Abstract
Purpose
We analyzed the surgical and functional outcomes of 100 consecutive laparo-scopic radical prostatectomies (LRP) performed by a single surgeon.
Materials and Methods
Between October 2007 and May 2010, a total of 100 consecutive patients underwent LRP for prostate cancer at our institution. We retrospectively reviewed the medical records of these patients to determine surgical and functional results. We compared surgical and functional outcomes between three groups divided on the basis of operation period (Group 1; first 40 cases; Group 2; next 30 cases; Group 3; last 30 cases).
Results
The operative time decreased significantly as the surgeon's experience increased over time (P<0.01). The learning curve for operative time was surpassed after approximately 40 cases. The overall positive surgical margin (PSM) rate was 17.5% in Group 1, 16.7% in Group 2, and 10% in Group 3. For organ-confined disease, the PSM rate was 2.5%, 6.7%, and 3.3% in Groups 1, 2, and 3, respectively. The continence rate (absence of a pad) was 73.2% and the social continence rate was 94.7% at 12 months after surgery. There was a significant difference in continence (absence of pad) between the early (Group 1) and late group (Group 3) at 1, 3, and 6 months (P<0.0001). The continence rate was not affected by whether the pubic bone-anchoring procedure or the Rocco suture method was used. The overall potency rate was 16.7% and 48.6% at 6 and 12 months, respectively. For bilateral nerve-sparing cases, the potency rate was 20% and 57.1% at 6 and 12 months, respectively.
Conclusions
Our surgical and functional outcomes indicate that even in this 'robotic era', LRP is still an attractive treatment option for patients with localized prostate cancer, especially in areas with limited access to surgical robots.
Keywords: Laparoscopy, Prostatectomy, Prostate neoplasms, Urinary incontinence
INTRODUCTION
Laparoscopic radical prostatectomy (LRP) is known to be a technically challenging procedure. Improvements in laparoscopic equipment and techniques have led to lower morbidity, decreased postoperative pain, and a reduced length of hospital stay compared with open surgery. Furthermore, these improvements have yielded functional outcomes comparable to or better than those obtained with standard radical retropubic prostatectomy (RRP) [1-4]. However, laparoscopic surgery usually requires acquisition of new anatomical perspectives, excellent hand-to-eye coordination, and great manual dexterity. All these restrictions contribute to the steep learning curve of laparoscopic surgery [5]. Because of these technical difficulties associated with LRP, robot-assisted laparoscopic prostatectomy (RALP) has been used for prostate cancer treatment. However, the Korean national medical insurance system does not reimburse surgeons for the cost of RALP (which is 5-6 times the cost of LRP). LRP therefore remains a viable treatment option for patients with localized prostate cancer in Korea.
The aim of this study was to report the surgical and functional outcomes of 100 consecutive patients who underwent LRP by a single surgeon at our institution.
MATERIALS AND METHODS
Between October 2007 and May 2010, a total of 100 consecutive patients underwent LRP for prostate cancer at our institution. All procedures were performed by a single surgeon who was fellowship trained in laparoscopic urologic surgery. Eighty-nine patients were operated on by using a transperitoneal approach, whereas the remaining 11 patients were operated on by using an extraperitoneal approach according to the surgeon's preference.
All patients had prostate cancer as diagnosed by transrectal ultrasound-guided prostate needle biopsies. For work-up staging, a whole-body bone scan and prostate magnetic resonance imaging (MRI) were performed. The TNM 2002 classification was used to stage the operative specimens. Data including preoperative clinical and biological characteristics, patient demographics, surgical data, pathological features, and postoperative variables were collected retrospectively from a database. The operative time was defined as the time between CO2 gas on and off, and the estimated blood loss (EBL) was calculated by the anesthesiologist. Urinary continence was defined as the absence of a pad, and we also conducted an analysis of social continence, which was defined as the use of either no pad or one security pad daily. Potency was defined as the ability to achieve an erection sufficient for penetration with or without the use of phophodiesterase-5 enzyme inhibitor. Postoperative potency was evaluated in all patients who were sexually active and potent preoperatively and who had undergone a unilateral or bilateral nerve-sparing operation. The percentage of patients who were continent and the potency rate were evaluated at 1, 3, 6, and 12 months after surgery. Biochemical recurrence was defined as a serum PSA level ≥0.2 ng/ml in at least three consecutive measurements. The surgical techniques that we used are described in detail in a previous publication [6].
1. Statistical analysis
Patient characteristics were calculated as means or medians and percentages for the overall population and procedural period. All data were analyzed by using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) by applying Student's t-test, the Chi-square test, Fisher's exact test, the Mann-Whitney test, the Kruskal-Wallis test, Spearman's rank correlation test, the log-linear model, and censored data analysis where appropriate.
RESULTS
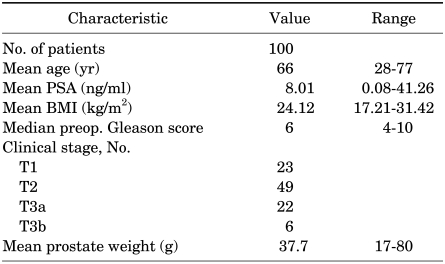
The patients' characteristics are listed in Table 1, 2. Briefly, the mean patient age was 66 years (range, 28-77 years), the mean PSA level was 8.01 ng/ml, and the distribution of clinical stages was as follows: 23% T1, 49% T2, 22% T3a, and 6% T3b.
TABLE 1.
Preoperative patient characteristics
PSA: prostate-specific antigen, BMI: body mass index
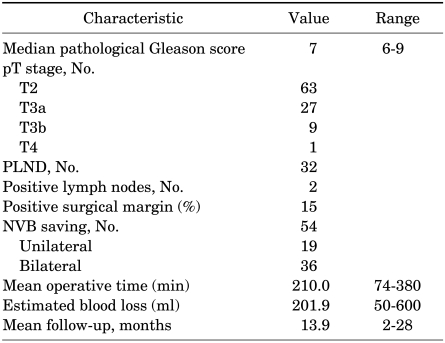
TABLE 2.
Intraoperative and postoperative patient characteristics
PLND: pelvic lymph node dissection, NVB: neurovascular bundle
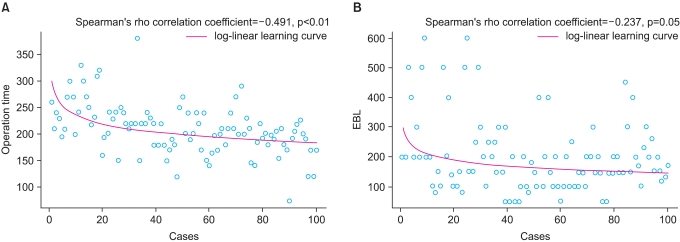
The overall mean operative time was 210 minutes (range, 74-380 minutes), and the operation time decreased as the number of cases increased (log-linear model, Spearman's rho -0.491, p<0.01) (Fig. 1A). According to the minimum p-value approach, there was a significant difference in the operative time cutoff at 40 cases; after 40 cases, the mean operative time reached a plateau. Thus, the surgeon's learning curve with regard to operative time was overcome after approximately 40 cases. The overall mean estimated blood loss was 201.9 ml (range, 50-600 ml). However, there was no significant correlation between EBL and the case number (log-linear model, Spearman's rho -0.237, p=0.05) (Fig. 1B).
FIG. 1.
Correlation between operative time and case number (A), and between EBL and case Number (B).
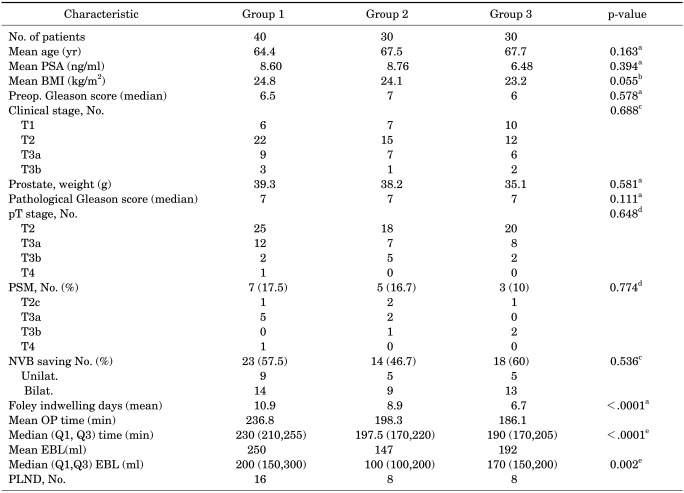
We divided the patients into three groups (first 40 cases vs. next 30 cases vs. last 30 cases). The early group (Group 1) consisted of the first 40 cases; this number of cases was chosen because after the 40th case, the learning curve in terms of operative time was surpassed. The middle and late groups (Groups 2, 3) constituted the next 30 cases in succession. Patient characteristics, the clinical stage, and pathological outcomes were comparable among the three groups. The positive surgical margin (PSM) rate was 6.3% (4/63) in pT2 and 27.8% (10/36) in pT3 tumors. An analysis of the overall PSM rate by group revealed that the PSM rate was 17.5% (7/40) in Group 1, 16.7% (5/30) in Group 2, and 10% (3/30) in Group 3 (Table 3). For organ-confined disease, the PSM rate was 2.5% (1/40) in Group 1, 6.7% (2/30) in Group 2, and 3.3% (1/30) in Group 3.
TABLE 3.
Comparisons of perioperative parameters according to groups divided on the basis of the operation period
PSM: positive surgical margin, NVB: neurovascular bundle, PLND: pelvic lymph node dissection, Q1: first quartile, Q3: third quartile, (Q1, Q3): inter quartile range, a: Mann-Whitney test, b: student's t-test, c: chi-square test, d: fisher's exact test, e: kruskal-wallis test
Of the 99 patients, 9 (9.1%) had a PSA level ≥0.2 ng/ml at their postoperative 3-month visit. Among 9 patients, 6 patients underwent adjuvant androgen deprivation therapy, 2 patients missed the follow-up, and 1 patient experienced a spontaneously decreased PSA level <0.2 ng/ml before 12 months postoperatively. Of the 100 patients, biochemical recurrence occurred in 7 patients during the follow-up period. These seven patients underwent salvage radiation therapy (one patient) or androgen deprivation therapy (six patients).
Two intraoperative and two postoperative complications required intervention. Intraoperative complications occurred only in Group 1 and consisted of a ureter injury and a rectal injury that resulted in a recto-urethral fistula. For the former, a stented ureteroneocystostomy was performed laparoscopically. For the latter, a temporary diverting sigmoidostomy and fistula repair were performed.
The postoperative complications that occurred in Groups 2 and 3 involved an anastomosis site stricture and inguinal hernia. These patients were treated by sound and herniorrhaphy.
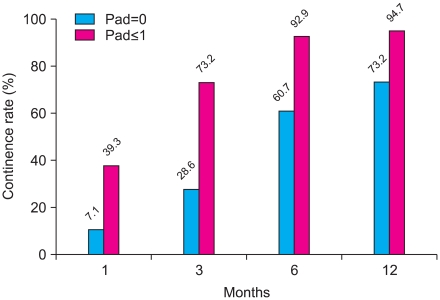
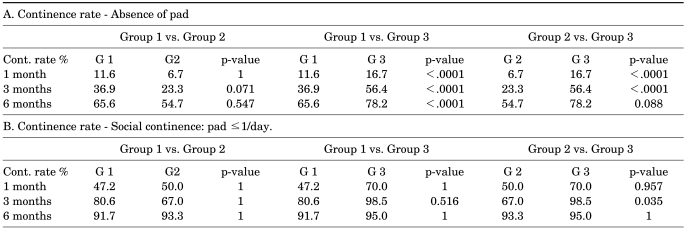
Continence (absence of a pad) was achieved in 73.2% of patients at 12 months after surgery. The social continence (0-1 pads per day) rate was 94.7% at 12 months after surgery (Fig. 2). The continence rate (absence of a pad) at 1, 3, and 6 months was 11.6%, 36.9%, and 65.6%, respectively, in Group 1 and 16.7%, 56.4%, and 78.2%, respectively, in Group 3, which was a significant difference (adjusted p-value for 1, 3, and 6 months, p<0.0001) (Table 4A).
FIG. 2.
Recovery of continence according to postoperative period.
TABLE 4.
Comparison of the continence rate of groups 1, 2, 3 at 1, 3, and 6 months by censored data analysis
Cont.: continence
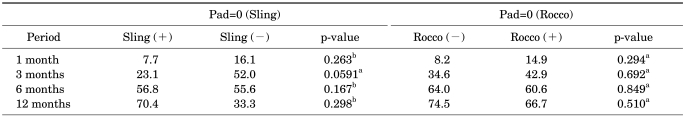
However, there was no significant difference in the social continence rate at 1, 3, and 6 months among the three groups (Table 4B). In terms of surgical technique, there was no significant difference in the continence rate related to the use of the pubic bone anchoring procedure or a Rocco suture (Table 5). Of 100 patients, artificial urethral sphincter insertion had to be performed in two patients because of post-prostatectomy incontinence.
TABLE 5.
Differences in the continence rate according to whether pubic bone anchoring or Rocco suturing were used
a: chi-square test, b: Fisher's exact test
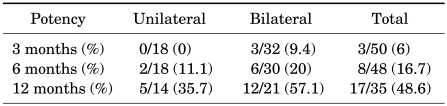
The overall potency rate was 16.7% and 48.6% at 6 and 12 months, respectively. This rate reached 20% at 6 months and 57.1% at 12 months for bilateral nerve-sparing cases, compared with 11.1% and 35.7% for unilateral nerve-sparing cases, respectively (Table 6).
TABLE 6.
Recovery of potency according to postoperative period
DISCUSSION
A recent study reported that a surgeon's experience with radical prostatectomy can have a great impact on clinical outcomes and complications [7]. Historically, the mastery of LRP has required a steep learning curve, with even experienced laparoscopic surgeons requiring nearly 60 cases to obtain proficiency [8]. The improvement in LRP techniques has decreased the length of the learning curve for LRP for laparoscopic-naïve surgeons [9]. For example, Guillonneau et al reported operative times of 4.6 hours for their first 50 cases, 4.0 hours for the next 50 cases, and 3.4 hours for their most recent 140 cases [8]. Ghavamian et al reported an operative time of 6.8 hours (411 min) for their first 10 cases and 3.3 hours (195 min) for their last 20 cases [10]; the learning curve for operative time was overcome after 35 cases. The operative time of our first 40 cases was 236.8 min compared with 186.1 min for the last 30 cases. Similarly, the learning curve in terms of operative time was overcome after approximately 40 cases; the mean operative times reached a plateau after that number.
Low blood loss is often considered one of the main advantages of laparoscopic surgery. In previous studies, the mean EBL for RRP ranged from 820 to 1,550 cc [11,12], whereas that for LRP was 380 to 800 cc [11,13] and that for RALP was 206 to 300 cc [14-16]. The overall EBL in our study was 202 cc, and there were no significant correlations between EBL and the number of cases. Rozet et al compared the clinical outcomes of LRP and RALP. They demonstrated that the mean EBL was 234 ml during RALP and 482 ml during LRP and that the mean operative time was 182 min for RALP and 234 min for LRP [17], consistent with our LRP results.
Ahlering et al reported a PSM rate of 27.3% for organ-confined disease after their first 50 robotic cases, but this decreased to 4.7% after experience with 150 cases [18]. Our PSM rate was 11% for organ-confined disease after our initial 31 cases [19], but this number decreased to 6.3% after 100 consecutive cases.
In the 56 patients followed up for 12 months, 73.2% of the patients were completely continent and 94.7% of the patients were socially continent. These figures are similar to those reported in previous RALP studies; a 73% continence rate was reported by Guillonneau et al (1999), whereas several groups have reported social continence rates of 90% to 95% after RALP [20-23]. In previous studies and our study, urinary continence and erectile function were subjectively determined by surgeon interviews and patient reports at postoperative visits [24-26]. However, to more objectively evaluate continence, we analyzed both pad-free continence and social continence (0-1 pads per day). We found a marked difference between pad-free and social continence. We therefore recommend that the absence of a pad should be taken into consideration when evaluating urinary continence after a prostatectomy.
According to our results, there was no significant difference in the recovery of continence whether a pubic bone anchoring procedure or a Rocco suture was used, but there was a significant improvement in the continence rate in the latest group at 1, 3, and 6 months compared with the earliest group. More meticulous and precise dissection of the prostatic apex and urethra may occur as the surgeon's experience increases; we attribute the improvement in the continence rate of the latest group to this improvement.
Preservation of the neurovascular bundles in both retropubic and laparoscopic prostatectomy has been demonstrated to significantly improve potency outcomes [27,28]. Herrmann et al reported a potency rate of 21% to 90% after RRP, 39% to 72% after LRP, and 36% to 84% after RALP [29]. Our potency rate was 57.1% in the bilateral neurovascular bundle-saved group.
As we stated above, our surgical and functional LRP outcomes are comparable with those reported for previous RALP series. In our opinion, the greatest disadvantage of RALP is the high cost associated with setting up and maintaining a robotic system. Furthermore, the volume-outcome relationship is an issue; smaller centers have found it difficult to overcome their learning curves. For this reason, we think that even in the "robotic era," in the case of surgeons who have some experience with laparoscopic surgery, the LRP technique might be offered to patients with prostate cancer as a viable, alternative treatment option, especially in areas with limited access to surgical robots.
One limitation of this study was the relatively small series (100 patients) and short follow-up duration (mean 13.9 months). The methods we used to evaluate functional outcomes were another limitation; patient and surgeon perceptions of functional impairment after radical prostatectomy can differ by up to 80% for urinary function and by up to 50% for sexual function [30]. This study was retrospective in nature and was limited to procedures performed by a single surgeon. Our LRP and previous RALP cohorts were also not identical. Therefore, we cannot generalize our results because of subjective variables such as the surgeon's experience.
CONCLUSIONS
Laparoscopic radical prostatectomy performed by a single surgeon yielded acceptable perioperative and early postoperative outcomes in a series of 100 patients with prostate cancer.
There was no significant difference in the recovery of continence whether a pubic bone anchoring procedure or a Rocco suture was used, but there was a significant improvement in the continence rate in the latest group at 1, 3, and 6 months compared with the earliest group. Our surgical and functional outcomes, especially with regard to continence, indicate that LRP remains an attractive treatment option for patients with localized prostate cancer, even in the robotic era.
Footnotes
The authors have nothing to disclose.
References
- 1.Stolzenburg JU, Rabenalt R, Do M, Kallidonis P, Liatsikos EN. Endoscopic extraperitoneal radical prostatectomy: the University of Leipzig experience of 2000 cases. J Endourol. 2008;22:2319–2325. doi: 10.1089/end.2008.9714. [DOI] [PubMed] [Google Scholar]
- 2.Salomon L, Levrel O, de la Taille A, Anastasiadis AG, Saint F, Zaki S, et al. Radical prostatectomy by the retropubic, perineal and laparoscopic approach: 12 years of experience in one center. Eur Urol. 2002;42:104–110. doi: 10.1016/s0302-2838(02)00263-4. [DOI] [PubMed] [Google Scholar]
- 3.Bhayani SB, Pavlovich CP, Hsu TS, Sullivan W, Su LM. Prospective comparison of short-term convalescence: laparoscopic radical prostatectomy versus open radical retropubic prostatectomy. Urology. 2003;61:612–616. doi: 10.1016/s0090-4295(02)02416-0. [DOI] [PubMed] [Google Scholar]
- 4.Dahl DM, He W, Lazarus R, McDougal WS, Wu CL. Pathologic outcome of laparoscopic and open radical prostatectomy. Urology. 2006;68:1253–1256. doi: 10.1016/j.urology.2006.08.1054. [DOI] [PubMed] [Google Scholar]
- 5.Poulakis V, Dillenburg W, Moeckel M, de Vries R, Witzsch U, Zumbé J, et al. Laparoscopic radical prostatectomy: prospective evaluation of the learning curve. Eur Urol. 2005;47:167–175. doi: 10.1016/j.eururo.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 6.Park JW, Lee HW, Kim W, Jeong BC, Jeon SS, Lee HM, et al. Comparative assessment of a single surgeon's series of laparoscopic radical prostatectomy: conventional versus robot-assisted. J Endourol. 2011;25:597–602. doi: 10.1089/end.2010.0229. [DOI] [PubMed] [Google Scholar]
- 7.Hu JC, Gold KF, Pashos CL, Mehta SS, Litwin MS. Role of surgeon volume in radical prostatectomy outcomes. J Clin Oncol. 2003;21:401–405. doi: 10.1200/JCO.2003.05.169. [DOI] [PubMed] [Google Scholar]
- 8.Guillonneau B, Rozet F, Barret E, Cathelineau X, Vallancien G. Laparoscopic radical prostatectomy: assessment after 240 procedures. Urol Clin North Am. 2001;28:189–202. doi: 10.1016/s0094-0143(01)80021-5. [DOI] [PubMed] [Google Scholar]
- 9.Martina GR, Giumelli P, Scuzzarella S, Remotti M, Caruso G, Lovisolo J. Laparoscopic extraperitoneal radical prostatectomy--learning curve of a laparoscopy-naive urologist in a community hospital. Urology. 2005;65:959–963. doi: 10.1016/j.urology.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 10.Ghavamian R, Schenk G, Hoenig DM, Williot P, Melman A. Overcoming the steep learning curve of laparoscopic radical prostatectomy: single-surgeon experience. J Endourol. 2004;18:567–571. doi: 10.1089/end.2004.18.567. [DOI] [PubMed] [Google Scholar]
- 11.Rassweiler J, Seemann O, Schulze M, Teber D, Hatzinger M, Frede T. Laparoscopic versus open radical prostatectomy: a comparative study at a single institution. J Urol. 2003;169:1689–1693. doi: 10.1097/01.ju.0000062614.56629.41. [DOI] [PubMed] [Google Scholar]
- 12.Hsu EI, Hong EK, Lepor H. Influence of body weight and prostate volume on intraoperative, perioperative, and postoperative outcomes after radical retropubic prostatectomy. Urology. 2003;61:601–606. doi: 10.1016/s0090-4295(02)02422-6. [DOI] [PubMed] [Google Scholar]
- 13.Guillonneau B, Vallancien G. Laparoscopic radical prostatectomy: the Montsouris technique. J Urol. 2000;163:1643–1649. doi: 10.1016/s0022-5347(05)67512-x. [DOI] [PubMed] [Google Scholar]
- 14.Joseph JV, Vicente I, Madeb R, Erturk E, Patel HR. Robot-assisted vs pure laparoscopic radical prostatectomy: are there any differences? BJU Int. 2005;96:39–42. doi: 10.1111/j.1464-410X.2005.05563.x. [DOI] [PubMed] [Google Scholar]
- 15.Park SY, Ham WS, Choi YD, Rha KH. Robot-assisted laparoscopic radical prostatectomy: clinical experience of 200 cases. Korean J Urol. 2008;49:215–220. [Google Scholar]
- 16.Frota R, Turna B, Barros R, Gill IS. Comparison of radical prostatectomy techniques: open, laparoscopic and robotic assisted. Int Braz J Urol. 2008;34:259–268. doi: 10.1590/s1677-55382008000300002. [DOI] [PubMed] [Google Scholar]
- 17.Rozet F, Harmon J, Cathelineau X, Barret E, Vallancien G. Robot-assisted versus pure laparoscopic radical prostatectomy. World J Urol. 2006;24:171–179. doi: 10.1007/s00345-006-0065-3. [DOI] [PubMed] [Google Scholar]
- 18.Ahlering TE, Eichel L, Edwards RA, Lee DI, Skarecky DW. Robotic radical prostatectomy: a technique to reduce pT2 positive margins. Urology. 2004;64:1224–1228. doi: 10.1016/j.urology.2004.08.021. [DOI] [PubMed] [Google Scholar]
- 19.Lee HW, Lee HM, Seo SI. Comparison of initial surgical outcomes between laparoscopic radical prostatectomy and robot-assisted laparoscopic radical prostatecomy performed by a single surgeon. Korean J Urol. 2009;50:468–474. [Google Scholar]
- 20.Guillonneau B, Cathelineau X, Cour F, Veillon B, Vallancien G. Update of the morbidity of radical retropubic prostatectomy: retrospective analysis of 100 consecutive operations during the period. Prog Urol. 1999;9:662–667. [PubMed] [Google Scholar]
- 21.Badani KK, Kaul S, Menon M. Evolution of robotic radical prostatectomy: assessment after 2766 procedures. Cancer. 2007;110:1951–1958. doi: 10.1002/cncr.23027. [DOI] [PubMed] [Google Scholar]
- 22.Patel VR, Palmer KJ, Coughlin G, Samavedi S. Robot-assisted laparoscopic radical prostatectomy: perioperative outcomes of 1500 cases. J Endourol. 2008;22:2299–2305. doi: 10.1089/end.2008.9711. [DOI] [PubMed] [Google Scholar]
- 23.Zorn KC, Gofrit ON, Steinberg GP, Taxy JB, Zagaja GP, Shalhav AL. Planned nerve preservation to reduce positive surgical margins during robot-assisted laparoscopic radical prostatectomy. J Endourol. 2008;22:1303–1309. doi: 10.1089/end.2008.0009. [DOI] [PubMed] [Google Scholar]
- 24.Bianco FJ, Jr, Scardino PT, Eastham JA. Radical prostatectomy: long-term cancer control and recovery of sexual and urinary function ("trifecta") Urology. 2005;66:83–94. doi: 10.1016/j.urology.2005.06.116. [DOI] [PubMed] [Google Scholar]
- 25.Eastham JA, Scardino PT, Kattan MW. Predicting an optimal outcome after radical prostatectomy: the trifecta nomogram. J Urol. 2008;179:2207–2210. doi: 10.1016/j.juro.2008.01.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pierorazio PM, Spencer BA, McCann TR, McKiernan JM, Benson MC. Preoperative risk stratification predicts likelihood of concurrent PSA-free survival, continence, and potency (the trifecta analysis) after radical retropubic prostatectomy. Urology. 2007;70:717–722. doi: 10.1016/j.urology.2007.06.639. [DOI] [PubMed] [Google Scholar]
- 27.Katz R, Salomon L, Hoznek A, de la Taille A, Vordos D, Cicco A, et al. Patient reported sexual function following laparoscopic radical prostatectomy. J Urol. 2002;168:2078–2082. doi: 10.1016/S0022-5347(05)64300-5. [DOI] [PubMed] [Google Scholar]
- 28.Quinlan DM, Epstein JI, Carter BS, Walsh PC. Sexual function following radical prostatectomy: influence of preservation of neurovascular bundles. J Urol. 1991;145:998–1002. doi: 10.1016/s0022-5347(17)38512-9. [DOI] [PubMed] [Google Scholar]
- 29.Herrmann TR, Rabenalt R, Stolzenburg JU, Liatsikos EN, Imkamp F, Tezval H, et al. Oncological and functional results of open, robot-assisted and laparoscopic radical prostatectomy: does surgical approach and surgical experience matter? World J Urol. 2007;25:149–160. doi: 10.1007/s00345-007-0164-9. [DOI] [PubMed] [Google Scholar]
- 30.Litwin MS, Pasta DJ, Stoddard ML, Henning JM, Carroll PR. Epidemiological trends and financial outcomes in radical prostatectomy among Medicare beneficiaries, 1991 to 1993. J Urol. 1998;160:445–448. [PubMed] [Google Scholar]