Abstract
Background:
The proximal phalanx (PP) of the fingers is fractured more frequently than the middle or even distal phalanges. The problems of malunion, stiffness and sometimes loss of skin or other soft tissues associated with PP fracture increases the disability. The optimum treatment depends on fracture location, fracture geometry and fracture stability. The objective of the study was to analyse the treatment outcome in a series of closed proximal phalangeal fractures of the hand.
Materials and Methods:
Eighty-four proximal phalangeal fractures in 68 patients were enrolled from 2007 to 2009. The treatment modalities were broadly categorised into two groups, Group A consisted of conservative treatment, and Group B consisted of surgical treatment. Group A included 47 digits treated with closed reduction (CR) with immobilization (n=43), extension block cast and dynamic traction (n=4), while 37 digits were treated in Group B, which included closed or open reduction (OR) and internal fixation (IF) with K-wires (n=31), OR and IF with stainless-steel wiring (n=2), and mini external-fixator (n=4). Belsky's criteria and Gingrass’ criteria were used for assessment of finger injuries and to assess the efficacy of conservative and surgical modalities for closed proximal phalangeal fractures of the hand.
Results:
Average period of follow-up was 1 year (range 10-14 months). The excellent to good results seen in Groups A and B were 89% and 92%, respectively. Six complications were seen in Group A, which included four cases with malunion and two cases with digital stiffness. Three complications were seen in Group B, which included one each of malunion, digital stiffness and extensor lag. Overall, maximum poor results (n=4) were seen with CR and buddy strapping.
Conclusion:
Conservative treatment is an inexpensive method, particularly suitable for stable fractures, and in patients who are poor candidates for surgery, Surgical modalities have distinct advantage of stable fixation, but with added risk of digital stiffness. Percutaneous pinning is a reliable, most commonly used surgical modality and technically easier. Both conservative and surgical modalities have good efficacy when used judiciously
Keywords: Proximal phalanx fracture, hand, closed reduction, open reduction
INTRODUCTION
Fractures of metacarpals and phalanges are the most common fractures of the upper extremity and account for 10% of total such cases.1 The outer rays of the hand are most commonly injured.1 Unfortunately, the metacarpal and phalangeal fractures are often neglected or regarded as trivial injuries.2 The proximal phalanx (PP) of the fingers is fractured more frequently than the middle or even distal phalanges. The deformity with considerable displacement is typical when the PP is fractured.3,4
Most fractures are functionally stable either before or after closed reduction (CR) and fare well with protective splintage and early mobilisation.1,2 The closed treatment has gained a poor reputation because of problems of malunion, stiffness, and sometimes loss of skin or other soft tissues.1,2 Certain fractures (angulation greater than 20° in anteroposterior view, and greater than 15° in lateral view, less than 50% bony contact, rotational deformity, collapse and multiple fractures) require operative fixation. Operative fixation must be used judiciously and with expectation that the ultimate outcome will be as good as, and optimally better than the outcome after nonoperative management.1 Selection of the optimum treatment depends on a number of factors, including fracture location, fracture geometry, deformity, whether they are open or closed, and fracture stability.3 The objectives of the study were to study causes, and types of fracture and to analyse the outcome from various treatment modalities for closed proximal phalangeal fractures of the hand.
MATERIALS AND METHODS
A prospective study was conducted of 84 consecutive closed proximal phalangeal fractures of hand in 68 patients, during a 2-year period of 2007-2009. Patients of all ages and both sexes were included in the study. Open fractures were excluded from the study.
After careful history taking and examination of the injured digit(s), antero-posterior and oblique radiographs were obtained. CR followed by fracture immobilization (buddy strapping/ cock up slab/ thumb spica, dorsal extension block cast, dynamic traction) was done. Check radiographs were taken. Fractures, which could not be reduced anatomically, eg, comminuted fractures and those that could be reduced, but unstable or got displaced on relieving the traction were labeled as unstable fractures and taken up for surgery [Figure 1]. The operative procedure and its advantages were explained in detail to each patient and an informed consent was obtained.
Figure 1.
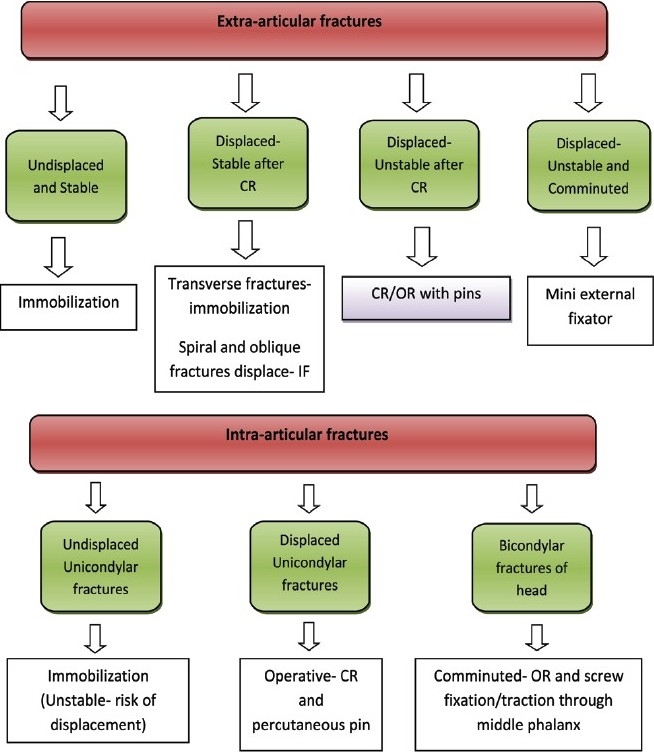
Flowchart for management of proximal phalangeal fractures
The patients were divided into two groups according to the type of treatment received. Group A consisted of cases that received conservative modalities like CR and immobilization with splinting by buddy strapping, aluminium splint, cock-up plaster of Paris (POP) slab, thermoplastic splint, and thumb spica for thumb fractures, dorsal extension block cast, or dynamic traction (based on fracture personality and surgeon's choice). Group B included cases of failed reductions and unstable fractures, which had undergone surgical procedures like CR/open reduction (OR) with Kirschner-wire (K-wire), OR with stainless steel (SS) wiring, or external-fixator (ex-fix) and augmentation with some kind of splinting. Results were analysed by Belsky's criteria4 for assessment of finger injuries to assess the efficacy of conservative and surgical modalities for closed proximal phalangeal fractures of the hand and were graded as 1) Excellent- pain-free union/no deformity/total active motion (TAM) > 215°, PIP motion > 100°; 2) Good - pain-free union/ minimal deformity/ TAM > 180°, PIP motion > 80°; 3) Poor- pain or non-union/ deformity affecting function or cosmesis/ TAM <180°, PIP motion <80°. Gingrass’ criteria4 were used for assessment of thumb injuries and were graded as 1) Excellent- palmar abduction (PAB) > 45°/ total flexion (TF) >100°; 2) Good- PAB >30°/ TF >75°; 3) Poor- PAB < 30°/ TF < 75°).
Group A: Nonsurgical procedure
The displaced or angulated, fractures were reduced1,6 under digital block. Reduction was achieved by giving longitudinal traction and using the thumb of the surgeon as a fulcrum. Metacarpophalangeal joint (MCP) was flexed maximally to stabilize the proximal fragment and the distal fragment was flexed to correct the volar angulation. Rotations were checked with reference to the curvature of the fingernails. On achieving satisfactory reduction, confirmed with check X-ray (angulation <20° in AP view, <150° in lateral view, >50 % bony contact, no rotational deformity or collapse) the digit was splinted6 either with POP in form of cock-up volar POP slab, where MCP joints were kept in 90° flexion, inter-phalangeal joints (IP joints) in extension and wrist in 30° dorsi-flexion (position of immobilization) or with dorsal extension block cast (in minimally displaced and stable fractures).6,7
Unstable fractures were treated by dynamic traction,1,8 where after achieving CR, a cloth hanger was molded in position of immobilization, and fixed to the forearm with POP. Suture bite was taken from the nail, and dynamic traction was secured with a rubber band.
Group B: Operative procedure
All surgeries were performed in 3-7 days of injury. Wrist block anesthesia was preferred because it allowed flexion of digits to assess rotational alignment. Reduction was checked under the C-arm guidance. Plates and screws were not used in our study.
For percutaneous pinning,1,9 after CR, one or two, longitudinal or crossed K-wires (1-2.5 mm) were inserted across the fracture. The most preferred entry point was mid-laterally through the head or base of the PP, with maximum flexion at MCP and proximal interphalangeal (PIP) joints. Wires were cut and bent at their ends, to be removed later on outpatient basis.
For the OR techniques, dorsal approach was used.1 Full-thickness subcutaneous tissue and flaps were elevated, the extensor tendon retracted, and the PP was exposed. After OR, internal fixation (IF) with K-wire or SS-wire (26 or 28 gauze) was done, depending on the type of fracture. Retrograde technique for K-wire1,10 was the most preferred method. For the OR with stainless steel wire,11 a single loop was used to compress a smaller fragment against the larger one. Periosteum was closed with absorbable suture and the dorsal apparatus over the PP was re-approximated with nonabsorbable sutures. In a PP fracture of thumb, the interval between the extensor pollicis longus and brevis was developed.
Mini external fixator1,4,12,13 was mainly used for the displaced and comminuted fractures. Predrilling was done bicortically with a 1.5-mm drill bit and two 2-mm pins were inserted dorsolaterally, proximal and distal to the fracture. The connecting rods and swivel clamps were tightened after reducing the fractures.
Parental antibiotics were administered for 3 days followed by oral antibiotics for 5-7 days. Active finger and wrist movements were encouraged following surgery. Check radiographs were taken on the next day. Suture removal was done on day 10.
The patients were reviewed every 2 weeks for the first 2 months, and then monthly for next 4 months. At 4-6 weeks post operation, repeat radiographs were taken to look for fracture union and after confirmation of the same, external hardware was removed. The patient was encouraged for active finger movements. Improvements in the range of movements (ROM) were noted on every visit. Pain, tenderness, grip strength, pinch strength, and TAM and untoward complication of the treatment were also noted.
Results were based on Belsky's criteria for finger fractures and Gingrass’ criteria for thumb injuries.4 The frequencies and crosstabs procedure by which two-way and multi-way tables were made and statistics and graphical displays (values in ascending or descending order) created that were useful for describing variables, chart, and graphs. After tabulation, P-value was determined by applying standard χ2 and Gaussian test, P<0.05 was considered to be significant. All statistical methods were carried out through the SPSS for Windows (version 16.0) and Minitab (version 11.0) for windows.
RESULTS
A total of 84 fractures were seen in 68 patients after excluding seven patients from studied cases that were lost to follow-up (we have analysed 84 fractures in 68 patients, because 15 patients had multiple fractures, out of which 14 had two digits injured, and one had three digits injured).
Fifteen patients had multiple fractures (53 patients had single digit injury, 14 patients had two digits injured, and one had three digits injured). Each digit was considered as a separate entity in a multiple injured hand and treated as the same
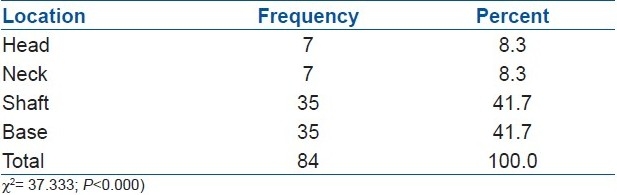
The mean age of patients was 34 years (range 17-40 years). There were 61 males compared to seven females. Almost equal percentage of right (44 phalanges, 52.3%) and left (40 phalanges, 47.7%) sided digits were affected. Road traffic accident (RTA) (20 cases, 29.4%) was the most common mode of injury followed by self-fall (19 cases, 27.9%) fall of object (n=16, 23.5%) sport (n=9, 13.2%) and assault (n=4, 5.9%). Little finger (24 digit, 28.6%) was the most common digit injured followed by middle finger (22 digit, 26.2%) ring (n=14,16.7%), thumb (n=13, 15.5 %) and index (n=11,13.1%) [Table 1]. Most common location of fracture was in the base and shaft region (35 digits, 41.7% each). With RTA and fall-related injuries, the most common location of fracture was in the base (13 digits, 48.1% and 14 digits, 66.7%, respectively), while with sports-related injuries, it was in the neck of phalanx (5 digits, 45.5%). The most common fracture pattern was transverse (n=29, 34.5%) while spiral (n=24, 28.6%), oblique (n=24, 4.8%), comminuted (n=23, 27.4%) and avulsion (n=24, 4.8%) [Table 2]. The ratio of extra-articular to intra-articular fractures was 2.8:1. Of extra-articular fractures, 31(50%) were present in the shaft, while 12(55%) of intra-articular fractures were present in the head of phalanx [Table 3].
Table 1.
Digit injured
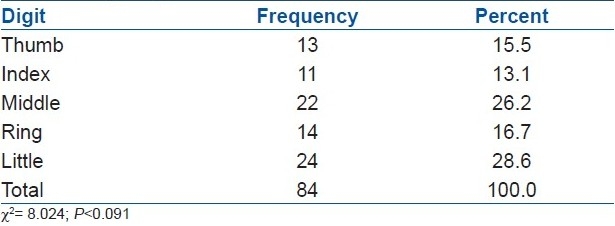
Table 2.
Type of the fracture
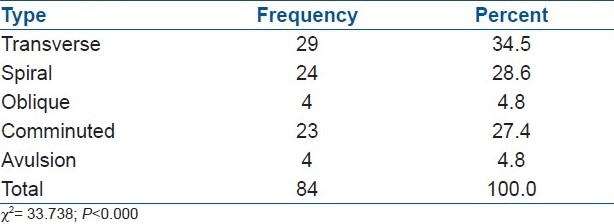
Table 3.
Location of the fracture
Group A (conservative) included, 47 fractures, while 37 were treated in group B (operative). A total of 38 (45.2%) digits were treated with buddy strapping and splinting, 18 digits (21.4%) with CR and IF with K-wire and splinting, and 13 digits (15.5%) with OR and IF with K-wire and splinting. Most fractures treated with buddy strapping were spiral (n= 18, 47.4%); with CR and IF with K-wire were comminuted (n=8, 44.4%); and with OR and IF with K-wire were transverse (n=9, 69.2%) [Figures 2–5] [Table 4].
Figure 2.

Closed reduction and buddy strapping and splint technique. (a) Radiograph of middle finger (anteroposterior view) showing fracture of PP of middle finger. (b and c) Buddy strapping after closed reduction with ice cream stick. (d) Post-strapping Cock-up slab. (e and f) Post-reduction radiograph (lateral and anteroposterior view) showing good position of fracture. (g and h) Clinical photograph of patient showing satisfactory range of movement at 6 weeks of follow-up
Figure 5.
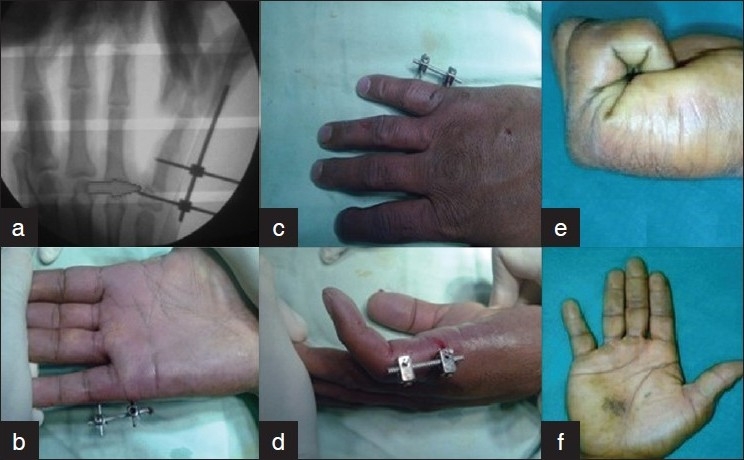
Mini external-fixation technique. (a) Intraoperative ‘C’ arm-assisted radiograph showing good fracture reduction of PP of little finger with external-fixator. (b-d) Postoperative clinical photographs. (e and f) Clinical photograph at 1 year followup showing full range of movement showing fixator in situ
Table 4.
Treatment modalities
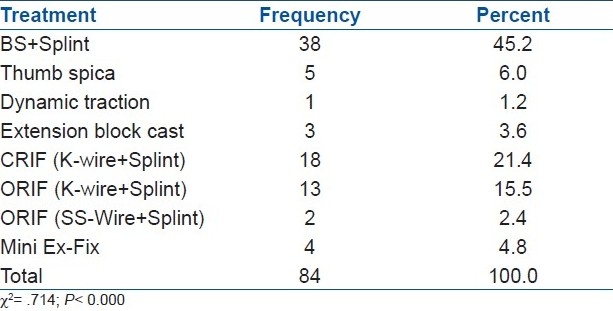
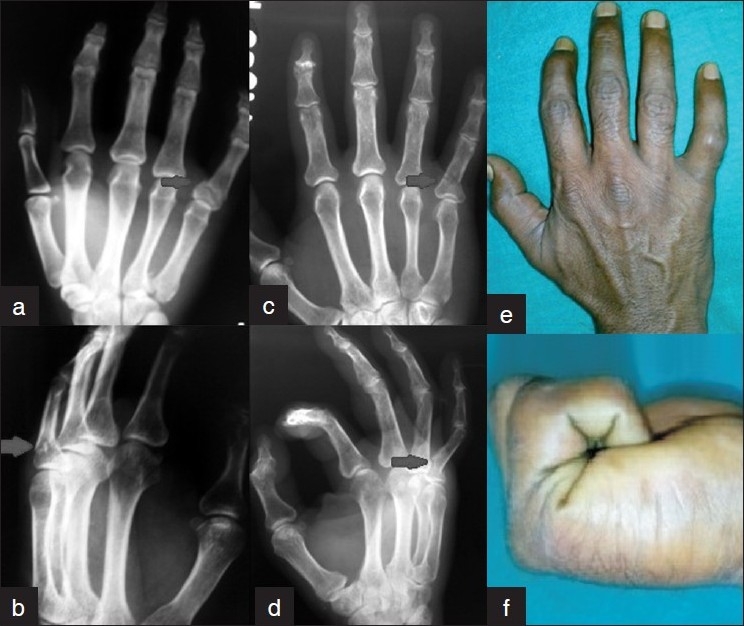
Figure 3.

Closed reduction and internal fixation technique. (a and b) Radiograph of hand (oblique and anteroposterior view) showing fracture of PP of ring finger. (c and d) Post-reduction radiograph of hand (oblique and anteroposterior view) with 2 K-wires in situ. (e) Post-reduction clinical picture at 2 weeks of followup. (f and g) Patient achieved full range of movement at 6 months of followup
Figure 4.

Open reduction and internal fixation technique. (a and b) Radiograph of hand (oblique and anteroposterior view) showing fracture of PP of little finger. (c to h) Peroperative photograph of surgical steps for fracture reduction. (i) Post-reduction radiograph of hand (oblique view) showing good position of fracture. (j and k) Clinical photograph of patient showing satisfactory range of movement at 6 weeks of follow-up
The mean duration of immobilization was average 4.26 weeks (range 3-5 weeks), and the mean union time was 5.95 weeks (range 4-7 weeks). In Group A, six complications were seen, which included malunions (n=3), digital stiffness with CR and immobilisation (n=2), malunion with thumb spica (n=1) [Figure 6]. Three complications were seen in group B, which included digital stiffness with CR and IF with K-wire (n=1), extension lag (n=1) and digital stiffness with OR and IF with K-wire and splinting (n=1) [Figure 7].
Figure 6.
Malunion following closed reduction and buddy strapping. (a and b) Radiograph showing fracture of PP of little finger. (c and d) Radiograph (anteroposterior and oblique view) showing malunited fracture at 6 months of follow-up. (e and f) Clinical photograph showing satisfactory range of movement with malunion at 6 months of follow-up
Figure 7.
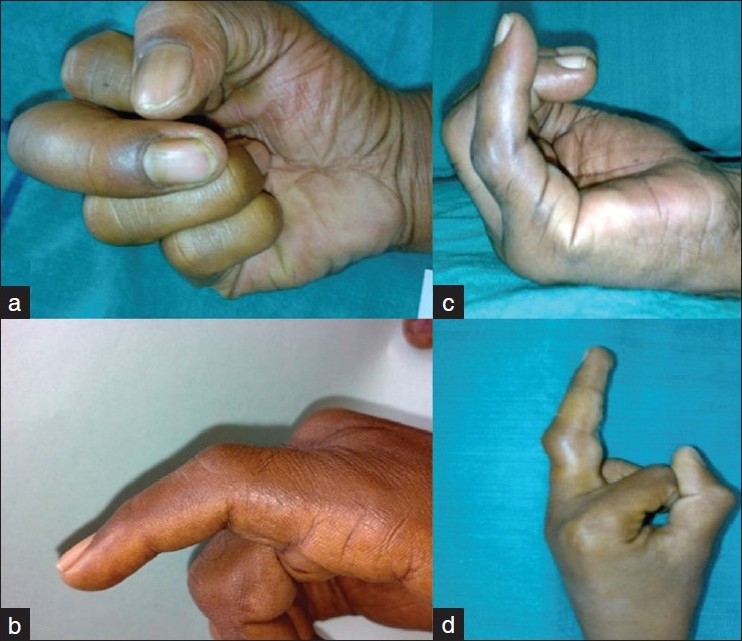
Post-treatment complications. (a) Clinical photograph with rotational deformity of middle finger. (b) Clinical photograph with extension lag of little finger. (c and d) Clinical photograph with malunion of little and middle fingers, respectively
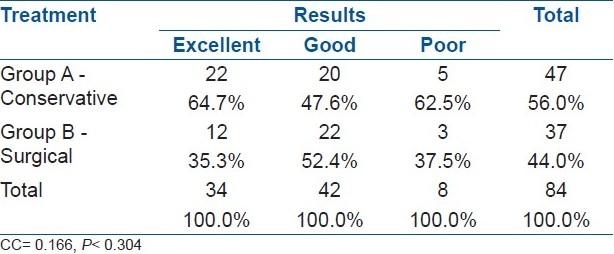
In group A, 89.4% (42/47 digits) excellent to good results were seen, while 91.9% (34/37 digits) of excellent to good results were seen in group B. Four poor results were seen with CR and immobilisation, two with OR and IF with K-wire and splinting, one with thumb spica, and one with CR and IF with K-wire. Overall best results were seen in shaft fractures, while most poor results were seen in basal fractures [Table 5].
Table 5.
Results
Mean TAM for fingers with all modalities of treatment was 210° (range 100°-265°), while mean total flexion (TF) for thumb fractures was 108.08° (range 60°-140°). Mean grip strength was 51.59 (range 25-75) pounds, while mean pinch strength was 13.37 (range 8-17) pounds.
DISCUSSION
The incidence of metacarpal and phalangeal fractures is most common in males and peaks at the age of 10-40 years14 – a time when the athletic injury and industrial exposure is the greatest. It is most commonly seen as fractured hand bone in children, especially the base, due to high incidence of Salter-Harris type 2 injuries.1 Of the 68 cases, 22% (15) of the patients had multiple digital fractures. Such combination fracture patterns were seen most commonly in the middle and ring finger and in the ring and little finger. Combination patterns have not been reported earlier. The mean patient age was comparable to that in other studies.4,10,15 In our study, the male to female ratio was 8.7:1, while Muhammad et al.15 reported this ratio to be 6:1. Almost equal percentage of right- and left-sided digit involvement was seen in our study and other studies as well.15 Consistent with the study by Kar et al.6 we also found RTA as the most common mode of injury. We found equal percentage of basal and shaft fractures (42% each). Transverse fracture pattern (29 phalanges, 35%) was most common and was consistent with the findings in other studies.6,10,15
The overall average duration of immobilization was 4.26 weeks (range 3-5 weeks), and the average time for fracture union was 5.95 weeks (range 4-7 weeks). Patankar et al.10 observed that all fractures united radiologically at 6 weeks. The excellent to good results were 89% in Group A and 92% in Group B. Muhammad et al.15 reported similar results. When compared to the study by Hornbach et al.9 83% of the patients had excellent results, while 100% of the patients treated by Patankar et al.10 had excellent results. The sample size for treatment with extension block cast (3), dynamic traction (1), mini external-fixator (4), and OR and IF with SS-wire (2) was extremely small to compare the results with other studies.6,7,9,11,13,16 Our study had an average TAM of 210°, and mean grip strength of 52 pounds. Hornbach et al.9 reported an average TAM of 265°. Average grip strength reported by Patankar et al.10 was 70.5 pounds.
With our best of knowledge, no study in the past has elaborated on the comparative results of conservative versus surgical treatment for only the closed fractures of proximal phalanges of the hand. Most of them considered all tubular bones of the hand together, both open and closed fractures together and involve only the adult age group. This might be a confounding factor for the purpose of comparison.
For most stable fractures, conservative treatment modalities are sufficient, but for most unstable fractures, surgical treatment gives the better results. Conservative treatment is a reliable, inexpensive modality, especially in children and in elderly age groups, but is associated with complication of malunion, secondary to loss of reduction. Closed pining is the most commonly done surgical procedure for a reducible, unstable fracture. It is a cost-effective, simple, and rapid procedure, and is well tolerated. It has added advantages of early bone healing, lesser infection rate, and decreased incidence of malunion. Strict adherence to post-treatment physiotherapy and rehabilitation is must to achieve the treatment objective and best possible outcome.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Stern PJ. Factures of metacarpals and phalanges. In: Green DP, Hotchkiss RN, Pederson WC, editors. Green's operative hand surgery. 4th ed. Vol. 1. Philadelphia, US: Churchill Livingstone; 1999. pp. 711–57. [Google Scholar]
- 2.Watson-Jones R, Barton NJ. Fractures and Joint Injuries of the hand. In: Wilson JN, editor. Watson-Jones fractures and joint Injuries. 7th ed. Noida: Elsevier Publishers; 2009. pp. 650–95. [Google Scholar]
- 3.Barton N. Internal fixation of the hand. J Hand Surg Br. 1989;14:139–42. doi: 10.1016/0266-7681_89_90113-7. [DOI] [PubMed] [Google Scholar]
- 4.Margic K. External fixation of closed metacarpal and phalangeal fractures of digits: A prospective study of one hundred consecutive patients. J Hand Surg Br. 2006;31:30–40. doi: 10.1016/j.jhsb.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Burkhalter WE. Closed treatment of hand fractures. J Hand Surg Am. 1989;14:390–3. doi: 10.1016/0363-5023(89)90120-2. [DOI] [PubMed] [Google Scholar]
- 6.Kar A, Patni P, Dayama RL, Meena DS. Treatment of closed unstable extra-articular proximal phalangeal fractures of hand by closed reduction and dorsal extension block cast. Indian J Orthop. 2005;39:158–62. [Google Scholar]
- 7.Rajesh G, Ip WY, Chow SP, Fung BK. Dynamic treatment for proximal phalangeal fracture of the hand. J Orthop Surg (Hong Kong) 2007;15:211–5. doi: 10.1177/230949900701500218. [DOI] [PubMed] [Google Scholar]
- 8.Collins AL, Timlin M, Thornes B, O’Sullivan T. Old principles revisited-traction splinting for closed proximal phalangeal fractures. Injury. 2002;33:235–7. doi: 10.1016/s0020-1383(01)00138-3. [DOI] [PubMed] [Google Scholar]
- 9.Hornbach EE, Cohen MS. Closed reduction and percutaneous pinning of fractures of the proximal phalanx. J Hand Surg Br. 2001;26:45–9. doi: 10.1054/jhsb.2000.0524. [DOI] [PubMed] [Google Scholar]
- 10.Patankar H, Meman FW. Multiple intramedullary nailing of proximal phalangeal fractures of hand. Indian J Orthop. 2008;42:342–6. doi: 10.4103/0019-5413.39573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greene TL, Noellert RC, Belsole RJ, Simpson LA. Composite wiring of metacarpal and phalangeal fractures. J Hand Surg Am. 1989;14:665–9. doi: 10.1016/0363-5023(89)90188-3. [DOI] [PubMed] [Google Scholar]
- 12.Godwin Y, Arnstein PM. A cheap, disposable external fixator for comminuted phalangeal fractures. J Hand Surg Br. 1998;23:84–5. doi: 10.1016/s0266-7681(98)80227-1. [DOI] [PubMed] [Google Scholar]
- 13.Pennig D, Gausepohl T, Mader K, Wulke A. The use of minimally invasive fixation in fractures of the hand - the minifixator concept. Injury. 2000;31:102–12. doi: 10.1016/s0020-1383(99)00268-5. [DOI] [PubMed] [Google Scholar]
- 14.De Jorge JJ, Kingman J, van der Lei B, Klasen HJ. Fractures of the metacarpals: A retrospective analysis of incidence and aetiology and a review of the English-language literature. Injury. 1994;25:365–9. doi: 10.1016/0020-1383(94)90127-9. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad M, Hussain SS, Rafiq Z, Tariq F, Khan MI, Malik SA. Management of phalangeal fractures of hand. J Ayub Med Coll Abbottabad. 2006;18:38–41. [PubMed] [Google Scholar]
- 16.Tan V, Beredjiklian PK, Weiland AJ. Intra-articular fractures of the hand treatment by open reduction and internal fixation. J Orthop Trauma. 2005;19:518–23. doi: 10.1097/01.bot.0000163440.71156.8e. [DOI] [PubMed] [Google Scholar]


