Abstract
Head injury in children accounts for a large number of emergency department visits and hospital admissions. Falls are the most common type of injury, followed by motor-vehicle-related accidents. In the present study, we discuss the evaluation, neuroimaging and management of children with head trauma. Furthermore, we present the specific characteristics of each type of pediatric head injury.
Keywords: Children, head, trauma
INTRODUCTION
Head injury in children accounts for a large number of emergency department visits and hospital admissions each year and remains a major cause of death and disability in children over 1 year of age. Falls are the most common type of injury, followed by motor-vehicle–related accidents.[1] Furthermore, child abuse remains a major cause of head trauma in children under 2 years of age.
Head trauma may be responsible for primary and secondary brain damage. Primary brain injury results from a direct mechanical damage at the time of injury, whereas secondary injury is caused by further cellular damage that develops hours or days post injury. Although head trauma in children and adults has several similarities, children should not be considered as young adults, given that pediatric patients have a more susceptible cranial vault due to thinner bones, large head-to-torso ratio, late development of air sinuses and differences in the immune system and in their capability of maintaining body temperature. Furthermore, severe head trauma in children is less frequent than in adults, and the mortality rate is also lower.[2]
In order to determine the severity of pediatric head trauma, detailed history about the injury mechanism, loss of consciousness, seizures and amnesia should be obtained. Physical examination involves the assessment of airway, breathing and circulation; complete neurological examination, including the grading of traumatic brain injury according to glasgow coma scale (GCS) score, pupils’ size, inspection of the head and spine, fundoscopic and ear evaluation. Additionally, the examination of the anterior fontanel in infants is of paramount importance. Further, patient's management varies according to the degree of compromise. In general, the goal should be the identification of life-threatening conditions and prevention of secondary brain injury.
Skull X-ray is usually limited to the identification of skull fracture. computed tomography (CT) provides indispensable information that guides patient's management.[3] Nevertheless, although CT is routinely performed in moderate and severe head injuries, there is still an uncertainty over which children with minor head trauma require CT, since fewer than 10% of these children suffer from a traumatic brain injury. CT is not risk free because of the radiation exposure.[4] Rice et al. reported that there may be as high as 1 case of lethal cancer for every 1000 CT scans performed in a young child.[5] Thus identification of children having low risk after head trauma is of paramount importance. In a series of 1000 pediatric patients with minor head trauma, 65 patients had a positive CT and 6 out of the 65 required neurosurgical intervention.[6] A recent study suggested that high-risk patients that require CT scan are those with failure to reach GCS score of 15 within 2 hours, suspicion of open skull fracture, worsening headache and irritability; whereas large scalp hematoma, signs of skull base fracture and dangerous injury mechanism were identified as medium risk factors.[7] Kuppermann et al. in a prospective study of 42,412 children with minor head trauma developed prediction rules for clinically important traumatic brain injury that can provide help in the identification of children in whom CT can be omitted.[8]
Brain damage markers
Various markers have been evaluated for possible use in the diagnosis and prognosis of brain damage in children.[9] S100 calcium-binding protein B, or S100B, is a biomarker of acute neurological disorder. S100B is usually elevated in children after traumatic brain injury.[10] Hallén et al. reported that S100B elevates within 6 hours after head trauma in patients with intracranial pathologies, suggesting that this marker could serve as a diagnostic tool.[11] Nevertheless, S-100B cannot replace clinical examination and CT but may support selection of patients for CT.[12] However, in the presence of multiple trauma, S100B is less reliable[13]
Neuron-specific enolase (NSE), a glycolytic isoenzyme in neurons and neuroendocrine cells, is also related to brain injury. Fridriksson et al. in a study of 50 children with blunt head trauma reported that NSE levels over 15.3 ng/mL could predict the presence of an intracranial lesion with 77% sensitivity and 52% specificity.[14] Bandyopadhyay and co-workers reported that NSE level of 21.2 ng/dL predicted poor outcome, with 86% sensitivity and 74% specificity, in children with closed traumatic brain injury.[15] Nevertheless, subsequent studies reported confounding results.[16,17]
Traumatic head injury predisposes to the development of coagulopathy. This has been considered as a manifestation of the disseminated intravascular coagulation (DIC) syndrome and has been associated with intravascular microthrombosis and neuronal death. Keller et al. reported that when GCS score was less than 9, 81% of children were coagulopathic.[18] Furthermore, children that developed coagulopathy had a worse prognosis. Incidence of development of DIC after pediatric severe head injury ranges between 14% and 25%. DIC occurrence is directly related to patient's outcome. Apart from that, D-dimer's cutoff of 500 pg/μL has been reported to predict a negative CT in patients with initial GCS score of 13 to 15 with a negative predictive value of 97%.[19]
Hyperglycemia after traumatic brain injury has also been associated with patient's outcome. Cochrane et al. reported that GCS score and serum glucose levels were independent predictors of mortality in children. In this study, serum glucose level greater than or equal to 300 mg/dL at admission was uniformly associated with death.[20] Inability for normalization of glucose blood levels within 48 hours has also been associated with worse prognosis.[21]
Scalp injury
Extensive skull lacerations can cause hypovolemic shock in small infants. Subgaleal hematoma is a blood collection between periosteum and galea aponeurotica, which thus passes the suture lines. It is usually related to vacuum extraction and trauma. Nevertheless, cases of spontaneous subgaleal hematomas due to coagulation disorders have been reported.[22] Subgaleal hematoma usually develops gradually. Prompt diagnosis is of paramount importance since patient may present with shock.[23] Subgaleal hematomas can be calcified [Figure 1].
Figure 1.
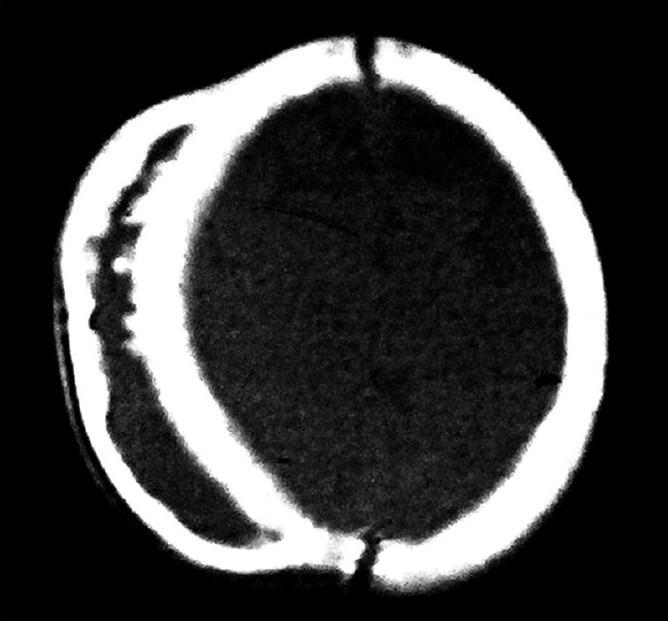
Calcified subgaleal hematoma
Cephalhematomas are rare and usually benign subperiosteal hemorrhagic collections of infancy and are usually limited by the sutures of the skull. This helps to differentiate cephalhematoma from subgaleal hematoma. A skull fracture may also be present. The treatment strategy of most cephalhematomas is usually conservative since they are gradually resolved in majority of the cases. Nevertheless, in cases of ossified cephalhematoma, surgical management is indicated for cosmetic reasons.[24,25]
Skull fracture
Skull fracture can be found in 2% to 20% of children that present with head trauma.[26] Bin et al. recently reported a clinical score based on patient's age, the scalp hematoma size, and the location of the hematoma that predicts the presence of skull fracture. Ninety percent of children with a score of 4 or greater had a skull fracture.[27] There are four major types of skull fractures: linear, depressed, diastatic and of skull base [Figure 2]. Linear skull fractures are the most common. Although not significant, they should be followed up for epidural hematoma, especially if they cross a major vessel. Depressed skull fractures may be open or closed. They usually require surgical treatment when the bone fragment is depressed deeper than the adjacent inner table. The deeper the depressed bone, the higher the risk of both dural tear and cortical laceration and the worse the prognosis.[28] Cases of elevated intracranial pressure due to compression of the superior sagittal sinus have been described.[29]
Figure 2.
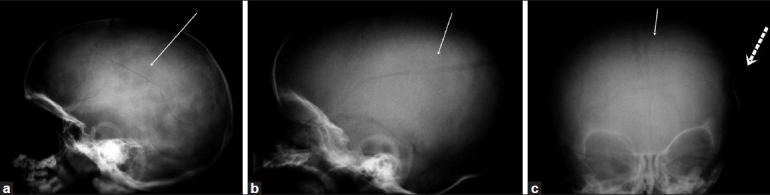
(a) Linear skull fracture (b) Diastatic skull fracture (c) Ping - Pong and linear fracture in an infant
Depressed skull fractures occurring in newborns and infants are called “ping pong” fractures and differ from those in older children since in infancy the bones are soft and resilient [Figure 2]. They usually occur during a difficult delivery. Surgical intervention has been proposed; however, cases of spontaneous resolution have also been reported.[30] Furthermore, nonsurgical procedures have been proposed, such as aspiration by breast milk extractor or by using an obstetrical vacuum extractor.[31,32] Growing skull fractures are rare, ranging from less than 0.05% to 1.6%, and are usually seen in children under 3 years of age [Figure 3].[33] All diastatic fractures should be followed up to timely identify the presence of a growing fracture. Late presented cases may be difficult to treat because autografts for reconstruction may be difficult to use, requiring alternative materials for cranioplasty.
Figure 3.
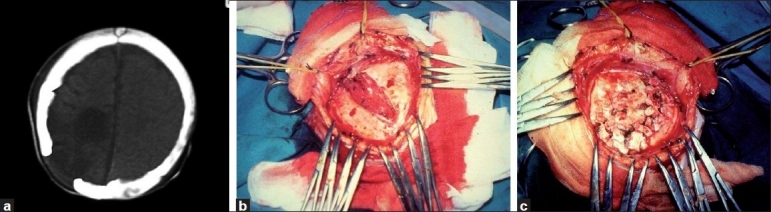
(a) CT scan of a patient with a growing fracture (b) Intraoperative photo revealing the growing fracture (c) Surgical treatment of the fracture
Skull base fractures are rare in children.[34] They can be suspected in the presence of specific signs such as periorbital ecchymosis (raccoon's eyes), mastoid ecchymosis (battle's sign), otorhagia and epistaxis. The most common physical findings are hemotympanum and bleeding in the ear canals.[34] Cerebrospinal fluid (CSF) leak may occur via the anterior cranial base or petrous bone, through the nose or ear. Usually CSF leaks stop spontaneously in nearly all children. In case of CSF fistula, surgical treatment is usually needed.
Epidural hematoma
Epidural hematoma is a collection of blood between the inner table of skull and the dura mater [Figure 4]. The hemorrhage usually originates from the middle meningeal artery, the venous cranial sinuses or from vessels that supply skull. In the majority of cases there is usually a fracture, and the blood vessels in the vicinity are usually responsible for the hemorrhage. The majority of epidural hematomas are located in the temporoparietal region. The lucid period may be absent; and in children, only in one third of the cases the clinical presentation is typical. The most dangerous period is the 4-hour period post trauma. Early diagnosis and surgical intervention via a craniotomy with hematoma evacuation is an appropriate treatment technique.[35] Patient's outcome is directly related to the patient's preoperative neurologic status and the presence of associated intracranial lesions.[36]
Figure 4.
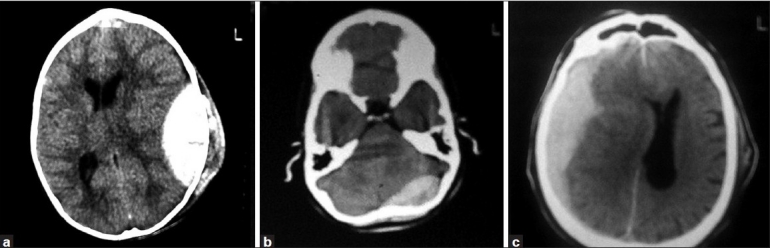
(a) Epidural hematoma (b) Posterior fossa epidural hematoma (c) Subdural hematoma
Epidural hematomas of the posterior fossa account for nearly 10% of all epidural hematomas and should be suspected in cases of occipital fall [Figure 4].[37] In about 80% of cases, there is an occipital fracture.[38] Because of the risk of rapid clinical deterioration due to brainstem compression, timely surgery can be life-saving.
Epidural hematomas in infants are rare because of the tight attachment between the dural membrane and periosteum and can occur after birth trauma.[39,40] Furthermore, in this age group, epidural hematoma may be difficult to diagnose due to the infants’ inability to communicate. Falls are the most common mechanism of injury.[41] The incidence of skull fracture has been reported to range between 54% and 79%. Tenderness in the anterior fontanel may be a sign of increased intracranial pressure. Besides that, lateralizing signs, irritability, pupillary abnormalities and scalp injuries should be explored in clinical examination.[42] In a series of 31 infants, the mortality rate was 6.5%, and the long-term morbidity rate was 3.2%. Interestingly, no neurophysiological sequela was noted.[43]
Subdural hematoma
Subdural hematomas result from injury to the bridging cortical veins or from extension of intracerebral contusion in the subarachnoid space [Figure 4]. The incidence is 20-25 cases per 100,000 children under 1 year of age.[44] These are usually classified as acute, subacute and chronic. Brain damage is more severe than in epidural hematoma. Subdural hematoma in children differs significantly from that in adults since it is usually associated with shaken-baby syndrome and less frequent with falls.[45] In case of suspected non-accidental head trauma, skeletal survey and ophthalmological examination for retinal hemorrhages should be performed.[46] Computed tomography is the examination of choice. Treatment depends on the extension and localization of the hematoma. Significant neurodisability and behavioral problems have been observed in children with subdural hematomas. Various prognostic factors have been identified, such as GCS score, early seizures, apnea, brain edema and diffuse axonal injury.[47–50]
Chronic subdural hematomas are usually observed in infants and result from an undiagnosed or conservatively treated acute subdural hematoma. Clinical findings are usually nonspecific. Evacuation of the hematoma through a single- or double-burr hole is usually performed.[51]
Intracerebral hematoma
Intracerebral hematomas are unusual in children and may be the result of focal brain injury or penetrating trauma. Most often they involve the temporal and frontal lobes. Many intracerebral hematomas can be treated conservatively. Those with significant mass effect or shift may require evacuation if clinically indicated. Repeated CT in high-risk lesions is recommended.[52]
Penetrating head trauma
Penetrating head injuries constitute only a small part of the total number of traumatic head injuries but belong to the class of most severe traumatic brain injuries [Figure 5]. In these cases, communication arises between the intracranial cavity and surrounding environment. Gunshot head wounds are the most frequent and are encountered with increasing frequency. Bihemispheric is the most common injury pattern in these cases.[53] Less frequent are injuries from knife, nails, pencils, chopsticks and scissors.[54–56]
Figure 5.
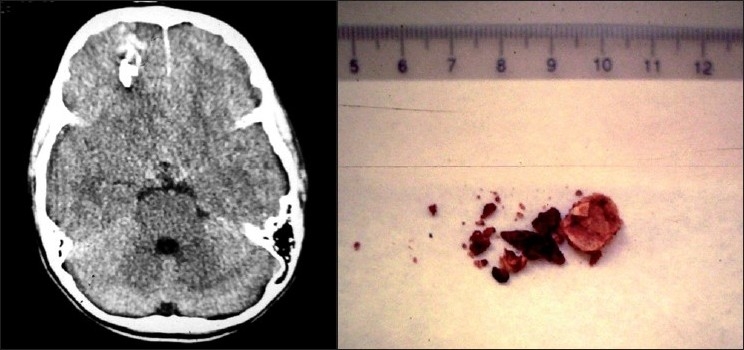
Penetrating head trauma following gunshot in a child
A wide variety of damage can be seen. CT and skull X-ray can demonstrate the extent of the damage. Surgery should be performed as soon as possible with debridement and proper wound closure.[57] Complications include CSF leak, diabetes insipidus, seizures, intracerebral abscess and hydrocephalus.[58,59]
CONCLUSION
In conclusion, although general guidelines for managing head trauma in children are similar to those in adults, children are unique and have special characteristics. A careful history (time and mechanism of injury, loss of consciousness, seizure activity), thorough examination, observation and neuroimaging in selected cases should provide timely identification of the patients that require further treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Adirim TA, Wright JL, Lee E, Lomax TA, Chamberlain JM. Injury surveillance in a pediatric emergency department. Am J Emerg Med. 1999;17:499–503. doi: 10.1016/s0735-6757(99)90184-5. [DOI] [PubMed] [Google Scholar]
- 2.Kumar R, Mahapatra AK. The changing “epidemiology” of pediatric head injury and its impact on the daily clinical practice. Childs Nerv Syst. 2009;25:813–23. doi: 10.1007/s00381-009-0820-z. [DOI] [PubMed] [Google Scholar]
- 3.Halley MK, Silva PD, Foley J, Rodarte A. Loss of consciousness: When to perform computed tomography? Pediatr Crit Care Med. 2004;5:230–3. doi: 10.1097/01.pcc.0000123543.40224.73. [DOI] [PubMed] [Google Scholar]
- 4.King MA, Kanal KM, Relyea-Chew A, Bittles M, Vavilala MS, Hollingworth W. Radiation exposure from pediatric head CT: A bi-institutional study. Pediatr Radiol. 2009;39:1059–65. doi: 10.1007/s00247-009-1327-1. [DOI] [PubMed] [Google Scholar]
- 5.Rice HE, Frush DP, Farmer D, Waldhausen JH. APSA Education Committee. Review of radiation risks from computed tomography: Essentials for the pediatric surgeon. J Pediatr Surg. 2007;42:603–7. doi: 10.1016/j.jpedsurg.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 6.Atabaki SM, Stiell IG, Bazarian JJ, Sadow KE, Vu TT, Camarca MA, et al. A clinical decision rule for cranial computed tomography in minor pediatric head trauma. Arch Pediatr Adolesc Med. 2008;162:439–45. doi: 10.1001/archpedi.162.5.439. [DOI] [PubMed] [Google Scholar]
- 7.Osmond MH, Klassen TP, Wells GA, Correll R, Jarvis A, Joubert G, et al. CATCH: A clinical decision rule for the use of computed tomography in children with minor head injury. CMAJ. 2010;182:341–8. doi: 10.1503/cmaj.091421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuppermann N, Holmes JF, Dayan PS, Hoyle JD, Jr, Atabaki SM, Holubkov R, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: A prospective cohort study. Lancet. 2009;374:1160–70. doi: 10.1016/S0140-6736(09)61558-0. [DOI] [PubMed] [Google Scholar]
- 9.Sandler SJ, Figaji AA, Adelson PD. Clinical applications of biomarkers in pediatric traumatic brain injury. Childs Nerv Syst. 2010;26:205–13. doi: 10.1007/s00381-009-1009-1. [DOI] [PubMed] [Google Scholar]
- 10.Berger RP, Pierce MC, Wisniewski SR, Adelson PD, Kochanek PM. Serum S100B concentrations are increased after closed head injury in children: A preliminary study. J Neurotrauma. 2002;19:1405–9. doi: 10.1089/089771502320914633. [DOI] [PubMed] [Google Scholar]
- 11.Hallén M, Karlsson M, Carlhed R, Hallgren T, Bergenheim M. S-100B in serum and urine after traumatic head injury in children. J Trauma. 2010;69:284–9. doi: 10.1097/ta.0b013e3181ca060b. [DOI] [PubMed] [Google Scholar]
- 12.Müller K, Townend W, Biasca N, Undén J, Waterloo K, Romner B, et al. S100B serum level predicts computed tomography findings after minor head injury. J Trauma. 2007;62:1452–6. doi: 10.1097/TA.0b013e318047bfaa. [DOI] [PubMed] [Google Scholar]
- 13.Pelinka LE, Toegel E, Mauritz W, Redl H. Serum S 100 B: A marker of brain damage in traumatic brain injury with and without multiple trauma. Shock. 2003;19:195–200. doi: 10.1097/00024382-200303000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Fridriksson T, Kini N, Walsh-Kelly C, Hennes H. Serum neuron-specific enolase as a predictor of intracranial lesions in children with head trauma: A pilot study. Acad Emerg Med. 2000;7:816–20. doi: 10.1111/j.1553-2712.2000.tb02276.x. [DOI] [PubMed] [Google Scholar]
- 15.Bandyopadhyay S, Hennes H, Gorelick MH, Wells RG, Walsh-Kelly CM. Serum neuron-specific enolase as a predictor of short-term outcome in children with closed traumatic brain injury. Acad Emerg Med. 2005;12:732–8. doi: 10.1197/j.aem.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 16.Geyer C, Ulrich A, Gräfe G, Stach B, Till H. Diagnostic value of S100B and neuron-specific enolase in mild pediatric traumatic brain injury. J Neurosurg Pediatr. 2009;4:339–44. doi: 10.3171/2009.5.PEDS08481. [DOI] [PubMed] [Google Scholar]
- 17.Kövesdi E, Lückl J, Bukovics P, Farkas O, Pál J, Czeiter E, et al. Update on protein biomarkers in traumatic brain injury with emphasis on clinical use in adults and pediatrics. Acta Neurochir (Wien) 2010;152:1–17. doi: 10.1007/s00701-009-0463-6. [DOI] [PubMed] [Google Scholar]
- 18.Keller MS, Fendya DG, Weber TR. Glasgow Coma Scale predicts coagulopathy in pediatric trauma patients. Semin Pediatr Surg. 2001;10:12–6. doi: 10.1053/spsu.2001.19381. [DOI] [PubMed] [Google Scholar]
- 19.Swanson CA, Burns JC, Peterson BM. Low plasma D-dimer concentration predicts the absence of traumatic brain injury in children. J Trauma. 2010;68:1072–7. doi: 10.1097/TA.0b013e3181d7a6f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cochran A, Scaife ER, Hansen KW, Downey EC. Hyperglycemia and outcomes from pediatric traumatic brain injury. J Trauma. 2003;55:1035–8. doi: 10.1097/01.TA.0000031175.96507.48. [DOI] [PubMed] [Google Scholar]
- 21.Melo JR, Di Rocco F, Blanot S, Laurent-Vannier A, Reis RC, Baugnon T, et al. Acute hyperglycemia is a reliable outcome predictor in children with severe traumatic brain injury. Acta Neurochir (Wien) 2010;152:1559–65. doi: 10.1007/s00701-010-0680-z. [DOI] [PubMed] [Google Scholar]
- 22.Kirkpatrick JS, Gower DJ, Chauvenet A, Kelly DL., Jr Subgaleal hematoma in a child, without skull fracture. Dev Med Child Neurol. 1986;28:511–4. doi: 10.1111/j.1469-8749.1986.tb14291.x. [DOI] [PubMed] [Google Scholar]
- 23.Plauche WC. Subgaleal hematoma.A complication of instrumental delivery. JAMA. 1980;244:1597–8. [PubMed] [Google Scholar]
- 24.Brichtová E. Early neurosurgical treatment of cephalhaematomas-personal experience and review of the literature. Childs Nerv Syst. 2009;25:95–101. doi: 10.1007/s00381-008-0722-5. [DOI] [PubMed] [Google Scholar]
- 25.Chung HY, Chung JY, Lee DG, Yang JD, Baik BS, Hwang SG, et al. Surgical treatment of ossified cephalhematoma. J Craniofac Surg. 2004;15:774–9. doi: 10.1097/00001665-200409000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Schutzman SA, Greenes DS. Pediatric minor head trauma. Ann Emerg Med. 2001;37:65–74. doi: 10.1067/mem.2001.109440. [DOI] [PubMed] [Google Scholar]
- 27.Bin SS, Schutzman SA, Greenes DS. Validation of a clinical score to predict skull fracture in head-injured infants. Pediatr Emerg Care. 2010;26:633–9. doi: 10.1097/PEC.0b013e3181ef0440. [DOI] [PubMed] [Google Scholar]
- 28.Erşahin Y, Mutluer S, Mirzai H, Palali I. Pediatric depressed skull fractures: Analysis of 530 cases. Childs Nerv Syst. 1996;12:323–31. doi: 10.1007/BF00301021. [DOI] [PubMed] [Google Scholar]
- 29.Forbes JA, Reig AS, Tomycz LD, Tulipan N. Intracranial hypertension caused by a depressed skull fracture resulting in superior sagittal sinus thrombosis in a pediatric patient: Treatment with ventriculoperitoneal shunt insertion. J Neurosurg Pediatr. 2010;6:23–8. doi: 10.3171/2010.3.PEDS09441. [DOI] [PubMed] [Google Scholar]
- 30.Lim CT, Koh MT, Sivanesaratnam V. Depressed skull fracture in a newborn successfully managed conservatively: A case report. Asia Oceania J Obstet Gynaecol. 1991;17:227–9. doi: 10.1111/j.1447-0756.1991.tb00265.x. [DOI] [PubMed] [Google Scholar]
- 31.Mastrapa TL, Fernandez LA, Alvarez MD, Storrs BB, Flores-Urueta A. Depressed skull fracture in Ping Pong: Elevation with Medeva extractor. Childs Nerv Syst. 2007;23:787–90. doi: 10.1007/s00381-007-0354-1. [DOI] [PubMed] [Google Scholar]
- 32.de Paul Djientcheu V, Njamnshi AK, Ongolo-Zogo P, Ako S, Essomba A, Sosso MA. Dpressed skull fractures in children: Treatment using an obstetrical vacuum extractor. Pediatr Neurosurg. 2006;42:273–6. doi: 10.1159/000094061. [DOI] [PubMed] [Google Scholar]
- 33.Ersahin Y, Gülmen V, Palali I, Mutluer S. Growing skull fractures (craniocerebral erosion) Neurosurg Rev. 2000;23:139–44. doi: 10.1007/pl00011945. [DOI] [PubMed] [Google Scholar]
- 34.Liu-Shindo M, Hawkins DB. Basilar skull fractures in children. Int J Pediatr Otorhinolaryngol. 1989;17:109–17. doi: 10.1016/0165-5876(89)90086-4. [DOI] [PubMed] [Google Scholar]
- 35.Gerlach R, Dittrich S, Schneider W, Ackermann H, Seifert V, Kieslich M. Traumatic epidural hematomas in children and adolescents: Outcome analysis in 39 consecutive unselected cases. Pediatr Emerg Care. 2009;25:164–9. doi: 10.1097/PEC.0b013e31819a8966. [DOI] [PubMed] [Google Scholar]
- 36.Rocchi G, Caroli E, Raco A, Salvati M, Delfini R. Traumatic epidural hematoma in children. J Child Neurol. 2005;20:569–72. doi: 10.1177/08830738050200070501. [DOI] [PubMed] [Google Scholar]
- 37.Costa Clara JM, Claramunt E, Ley L, Lafuente J. Traumatic extradural hematomas of the posterior fossa in children. Childs Nerv Syst. 1996;12:145–8. doi: 10.1007/BF00266818. [DOI] [PubMed] [Google Scholar]
- 38.Ciurea AV, Nuteanu L, Simionescu N, Georgescu S. Posterior fossa extradural hematomas in children: Report of nine cases. Childs Nerv Syst. 1993;9:224–8. doi: 10.1007/BF00303574. [DOI] [PubMed] [Google Scholar]
- 39.Gama CH, Fenichel GM. Epidural hematoma of the newborn due to birth trauma. Pediatr Neurol. 1985;1:52–3. doi: 10.1016/0887-8994(85)90010-4. [DOI] [PubMed] [Google Scholar]
- 40.Leggate JR, Lopez-Ramos N, Genitori L, Lena G, Choux M. Extradural hematoma in infants. Br J Neurosurg. 1989;3:533–9. doi: 10.3109/02688698909002844. [DOI] [PubMed] [Google Scholar]
- 41.Ersahin Y, Mutluer S, Guzelbag E. Extradural hematoma: Analysis of 146 cases. Childs Nerv Syst. 1993;9:96–9. doi: 10.1007/BF00305316. [DOI] [PubMed] [Google Scholar]
- 42.Beni-Adani L, Flores I, Spektor S, Umansky F, Constantini S. Epidural hematoma in infants: A different entity? J Trauma. 1999;46:306–11. doi: 10.1097/00005373-199902000-00018. [DOI] [PubMed] [Google Scholar]
- 43.Ciurea AV, Kapsalaki EZ, Coman TC, Roberts JL, Robinson JS, 3rd, Tascu A, et al. Supratentorial epidural hematoma of traumatic etiology in infants. Childs Nerv Syst. 2007;23:335–41. doi: 10.1007/s00381-006-0230-4. [DOI] [PubMed] [Google Scholar]
- 44.Jayawant S, Rawlinson A, Gibbon F. Subdural haemorrhages in infants: Population based study. BMJ. 1998;317:1558–61. doi: 10.1136/bmj.317.7172.1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Matschke J, Voss J, Obi N, Görndt J, Sperhake JP, Püschel K, et al. Nonaccidental head injury is the most common cause of subdural bleeding in infants <1 year of age. Pediatrics. 2009;124:1587–94. doi: 10.1542/peds.2008-3734. [DOI] [PubMed] [Google Scholar]
- 46.Tzioumi D, Oates RK. Subdural hematomas in children under 2 years. Accidental or inflicted? A 10-year experience. Child Abuse Negl. 1998;22:1105–12. doi: 10.1016/s0145-2134(98)00093-3. [DOI] [PubMed] [Google Scholar]
- 47.Jayawant S, Parr J. Outcome following subdural haemorrhages in infancy. Arch Dis Child. 2007;92:343–7. doi: 10.1136/adc.2005.084988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bonnier C, Nassogne MC, Saint-Martin C. Neuroimaging of intraparenchymal lesions predicts outcome in shaken baby syndrome. Pediatrics. 2003;112:808–14. doi: 10.1542/peds.112.4.808. [DOI] [PubMed] [Google Scholar]
- 49.Kemp AM, Stoodley N, Cobley C, Coles L, Kemp KW. Apnoea and brain swelling in nonaccidental head injury. Arch Dis Child. 2003;88:472–6. doi: 10.1136/adc.88.6.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chung CY, Chen CL, Cheng PT, See LC, Tang SF, Wong AM. Critical score of Glasgow Coma Scale for pediatric traumatic brain injury. Pediatr Neurol. 2006;34:379–87. doi: 10.1016/j.pediatrneurol.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 51.Swift DM, McBride L. Chronic subdural hematoma in children. Neurosurg Clin N Am. 2000;11:439–46. [PubMed] [Google Scholar]
- 52.Durham SR, Liu KC, Selden NR. Utility of serial computed tomography imaging in pediatric patients with head trauma. J Neurosurg. 2006;105:365–9. doi: 10.3171/ped.2006.105.5.365. [DOI] [PubMed] [Google Scholar]
- 53.Irfan FB, Hassan RU, Kumar R, Bhutta ZA, Bari E. Craniocerebral gunshot injuries in preschoolers. Childs Nerv Syst. 2010;26:61–6. doi: 10.1007/s00381-009-0971-y. [DOI] [PubMed] [Google Scholar]
- 54.Pascual-Castroviejo I, Pascual-Pascual SI, Viaño J. Diplegia due to transcranial knife-blade injury in a 20-month-old child. J Child Neurol. 2006;21:340–1. doi: 10.1177/08830738060210040501. [DOI] [PubMed] [Google Scholar]
- 55.Karim T, Topno M. An unusual case of penetrating head injury in a child. J Emerg Trauma Shock. 2011;3:197–8. doi: 10.4103/0974-2700.62113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.van As AB, van Dijk J, Numanoglu A, Millar AJ. Assaults with a sharp object in small children: A 16-year review. Pediatr Surg Int. 2008;24:1037–40. doi: 10.1007/s00383-008-2211-z. [DOI] [PubMed] [Google Scholar]
- 57.Mackerle Z, Gal P. Unusual penetrating head injury in children: Personal experience and review of the literature. Childs Nerv Syst. 2009;25:909–13. doi: 10.1007/s00381-009-0901-z. [DOI] [PubMed] [Google Scholar]
- 58.Coşar A, Gönül E, Kurt E, Gönül M, Taşar M, Yetişer S. Craniocerebral gunshot wounds: Results of less aggressive surgery and complications. Minim Invasive Neurosurg. 2005;48:113–8. doi: 10.1055/s-2004-830222. [DOI] [PubMed] [Google Scholar]
- 59.Kim TW, Lee JK, Moon KS, Kwak HJ, Joo SP, Kim JH, et al. Penetrating gunshot injuries to the brain. J Trauma. 2007;62:1446–51. doi: 10.1097/01.ta.0000222909.31666.db. [DOI] [PubMed] [Google Scholar]


