Abstract
Purpose:
To describe retinopathy of prematurity (ROP) among Jordanian preterm infants and evaluate the efficacy of applying current Western screening guidelines for Jordanian preterms.
Materials and Methods:
In this retrospective, descriptive hospital-based study, we collected data on preterm infants who were referred by their neonatologist for ROP screening at King Abdullah University Hospital between July 2006 and June 2007. Guidelines suggested by the American Academy of Pediatrics were followed. Additionally, older preterms considered at risk for ROP by the neonatal intensive care unit were screened. Any neonate with stage 1 ROP or higher in either eye was considered a positive case of ROP.
Results:
Ninety-one preterms were included in the study. The median birth weight was 1390 gm (range,730-1980 gms) and the gestational age ranged from 26 to 35 weeks with 64.8% of preterms ≤ 32 weeks. ROP occurred in 28.6% of all patients, in 20% of infants with birth weight greater than 1500 gms and in 9.4% of preterms with gestational age ≥ 32 weeks. Six patients (6.6%) required laser treatment, two with low birth weight greater than 1250 gm and one was 33 weeks of age. Consanguinity was identified in 19.2% of infants with ROP while consanguinity in infants who did not develop ROP was 1.9%. This difference was statistically significant (P<0.05).
Conclusion:
ROP occurs in premature infants in Jordan with gestational age above 32 weeks and birth weight above 1250 gm. Future guidelines for screening should incorporate the current study outcomes. A prospective, population-based is required to set national guidelines for ROP screening in the Jordanian population and similarly for different populations worldwide. Consanguinity may play a role in ROP development and further genetic studies may aid in elucidating the pathogenesis of ROP.
Keywords: Birth Weight, Jordan, Retinopathy of Prematurity, Screening
INTRODUCTION
Retinopathy of prematurity (ROP) is considered a leading cause of visual impairment in premature infants.1,2 Variations in ROP incidence and severity between different races and populations have been described.3–5 Data regarding ROP in Jordan is limited6 and there are no national guidelines to screen infants at high risk for ROP in this region. Currently we rely on the American7 and British8 guidelines.
Revised guidelines suggested by the American Academy of Pediatrics, the American association for Pediatric Ophthalmology and Strabismus and the American Academy of Ophthalmology recommend ROP screening of all infants with birth weight < 1500 gms or gestational age of 32 weeks or less.7 The British Association for Perinatal Medicine and the College of Ophthalmologists recommend screening all infants < 1500 gms at birth.8 However, these guidelines may not be suitable for other parts of the world as local ROP experience may dictate differing guidelines.
Reports of ROP in infants from the developed countries with birth weights > 1250 gms are limited. Hutchinson et al.9 reported only 8% of infants with birth weight between 1251 and 1500 gms who had undergone laser photocoagulation for threshold ROP. Goble et al.10 found that all the 2.7% infants with stage III ROP in Birmingham/England had a birth weight ≤ 1250 gms or a gestational age of ≤ 29 weeks, but two fell outside one criterion, indicating the need for both parameters to be used in screening guidelines. No ROP greater than stage 1 was observed in infants with gestational ages ≥ 32 weeks or birth weights ≥ 1500 gms in a study conducted by Wright et al. in the USA11 and all cases of threshold and stage 4 ROP were confined to infants with gestational ages ≤ 30 weeks or birth weights < 1200 gms.
Data from the Eastern part of the globe differs as ROP has been reported in older and/or heavier premature infants. In Saudi Arabia, Binkhathlan et al.12 reported ROP incidence of 56% among infants with gestational age of ≤ 36 weeks (birth weight ≤ 2000 gms). Although the incidence was higher in infants < 32 weeks, ROP was still identified in infants with higher gestational age. Hence, these authors recommended changing current screening criteria to include premature infants with gestational age ≤ than 34 weeks. Karkhaneh et al.13 reported an 11.9% incidence of ROP among Iranian preterms with gestational age greater than 32 weeks. Dogra et al.14 reported that 15.3% of Indian babies with threshold ROP treated with cryotherapy were > 1500 gms at birth. In a study from Southern India, Deshpande et al.15 reported that 21.7% of South-Indian infants with threshold ROP had birth weight > 1500 gms. Phan et al.16 reported 61.9% of Vietnamese babies with threshold ROP of which 13 babies were > 1250 gms at birth. Chen and Li17 studied the medical records of all stage 3, 4 and 5 ROP infants and found 8.8% had gestational age greater than 32 weeks of which 27.2% birth weight greater than 1500 gms. A recent report from Basmah et al.18 on Turkish subjects found that 56.2% of infants with a gestational age of 32-35 weeks who were referred for ROP screening developed ROP. In their study, Basmah et al. report the mean birth weight was 1857.9 (range 1060-3200) gms of the infants with ROP and found that 7% developed threshold ROP that required laser treatment.
The aim of this study is to describe ROP among Jordanian preterm infants. Incidence in relationship to birth weight, gestational age and hospital course was evaluated. Incidence of ROP with severe disease that required laser therapy was also evaluated. This data will help guide future screening programs in this region.
MATERIAL AND METHODS
This study was conducted at the neonatal intensive care unit (NICU) at King Abdullah University Hospital. This is the main tertiary referral NICU in northern Jordan. This study was conducted between July 2006 and June 2007. Revised guidelines suggested by the American Academy of Pediatrics, the American Association for Pediatric Ophthalmology and Strabismus and the American Academy of Ophthalmology for ROP screening were followed.7 All patients admitted to the unit with birth weight < 2000 gms and between 32 and 34 weeks of gestation who were considered to have an unstable hospital course and be at risk for ROP after a neonatology consult were included. During the study period, all ROP screening was performed by the same ophthalmologist who was specially trained in ROP screening. ROP was classified into five different stages according to the International Classification of Retinopathy of Prematurity.19 Subjects with type 1 ROP according to the Early treatment for retinopathy of Prematurity Randomized Trial (any stage ROP with plus disease, zone 1 stage 3 ROP without plus disease; or zone II, stage 2 or 3 ROP with plus disease) or worse required laser treatment.
Screening was initiated once an infant reached 4 weeks of life or 32 weeks of corrected gestational age, whichever was later. ROP screening was performed using binocular indirect ophthalmoscopy after dilating the pupils using one drop of 2.5% phenylphrine and two drops of 0.5% cyclopentolate, 5 minutes apart. Follow-up exams were based on the initial findings. Treatment was performed by the same pediatric ophthalmologist or by a vitreoretinal surgeon.
We identified a total of 91 neonates who underwent ROP screening and all were included in this study. Data collected for each neonate included: gender, postconception age, postnatal age, birth weight, consanguinity, age of onset of ROP, days spent on a ventilator, total number of days spent on oxygen and the presence of consanguinity between parents. Other risk factors such as intraventricular hemorrhage (IVH), necrotizing enterocolitis, congenital heart disease, sepsis or anemia in the preterm were also collected though this was not the main objective of our study. Any neonate who had stage 1 ROP or higher in either eye was classified as having ROP disease. Any neonate who underwent treatment was considered an ROP-treated patient.
The comparison between multiple variables was performed between ROP-positive and -negative neonates and using the χ2 test. A P-value 0.05 or less was considered statistically significant.
RESULTS
A total of 91 subjects (45 males and 46 females) comprised the study cohort. Birth weight of the cohort ranged from 730 to 1980 gms with a median of 1390 gm. Eleven patients (12.1%) had birth weight < 1000 gms. The gestational age of the cohort ranged from 26 to 35 weeks with 59 (64.8%) subjects ≤ 32 weeks. ROP was found in 26 (28.6%) subjects (16 males and 10 females), mean gestational age at which ROP was first considered was 33.9 weeks. ROP occurred in 9.4% of preterms with gestational birth ≥ 32 weeks. Six (6.6%) infants developed type 1 ROP, warranting laser treatment (two males and four females) with mean gestational age of 34.5 weeks when treatment was performed (time of maximum ROP). Table 1 presents characteristics of all infants enrolled in this study according to the degree of ROP. Patients who had ROP or required treatment had statistically significant lower birth weight, longer ventilation time and hospital stays (P<0.05, all cases, Table 1). Presence of anemia or IVH was a statistically significant risk factor for ROP occurrence (P<0.05, both cases, Table 1).
Table 1.
Infants characteristics in the retinopathy of prematurity and non-retinopathy of prematurity groups
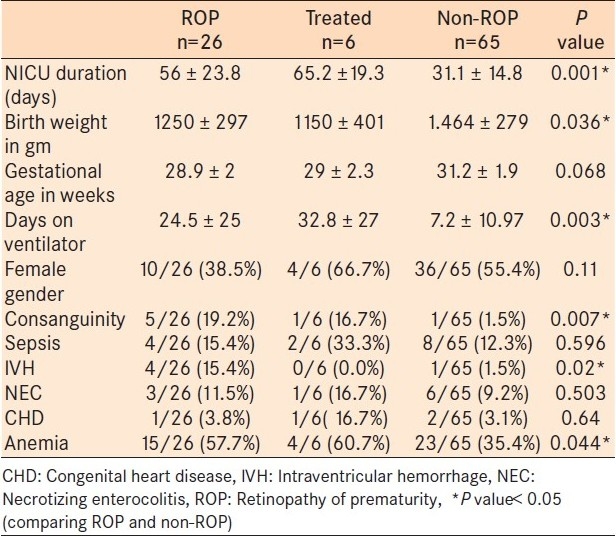
Consanguinity was identified in 19.2% (5/26) of infants who had ROP while consanguinity in infants who did not develop ROP was 1.9% (1/65). This difference in consanguinity was statistically significant (P=0.007). No significant association was found between consanguinity and the requirement for laser treatment (P>0.05).
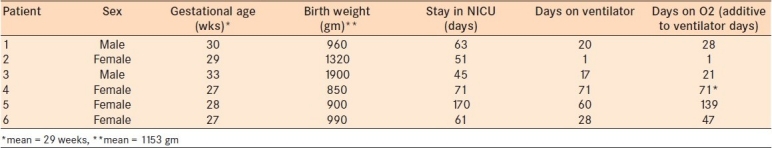
Table 2 describes the characteristics of ROP in relation to birth weight. Table 3 describes the characteristics of ROP in relation to gestational age. Out of 32 infants ≥ 32 weeks, three (9.4%) developed ROP one of whom required treatment. Figure 1 summarizes highest ROP stage reached in the 26 infants who developed ROP. Most patients developed stage 1 zone 3 ROP (38.5%) or stage 2 zone 2 ROP (30.8%). Table 4 presents the characteristics of the six treated subjects. The mean birth weight of treated subjects was 1153 gms and two subjects weighed more than 1250 gms. One of the treated subjects received 1 day of ventilation and the other one had a birth weight of 1.9 kg.
Table 2.
Retinopathy of prematurity according to birth weight
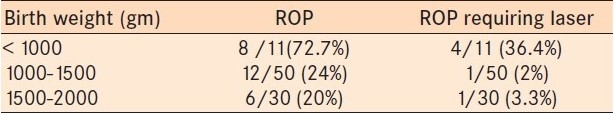
Table 3.
Retinopathy of prematurity according to gestational age
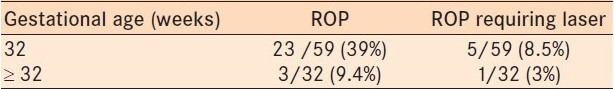
Figure 1.
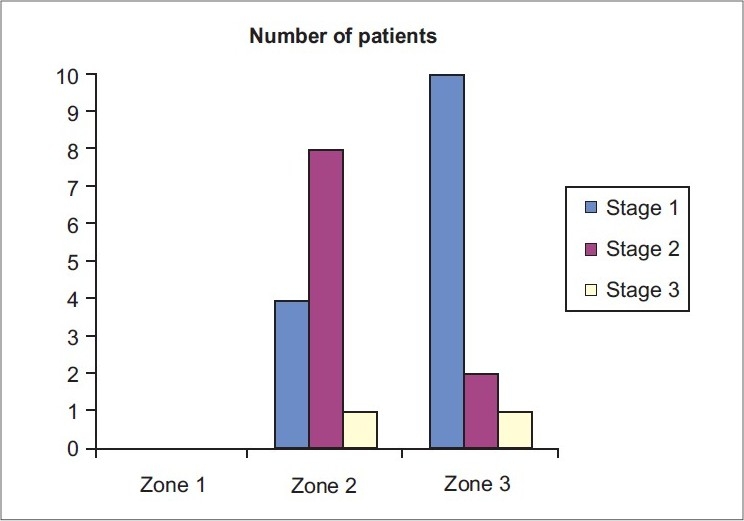
Distribution of Retinopathy of prematurity according to stages
Table 4.
Six of our patients needed treatment, Table 3 summarizes their data
DISCUSSION
This is the first study in Jordan that describes in detail both ROP-diseased infants and ROP in infants that required treatment intervention. This also is the first study where ROP screening was performed by a certified pediatric ophthalmologist. Previous work by Bdour et al.6 described the incidence of ROP without classifying the incidence based on gestational age or birth weight. We found that ROP disease occurred in 28.6% of screened infants. However, Bdour et al. reported an incidence of 44% in the 93 subjects screened in their study. This difference may reflect the difference in management in the two NICUs. However, the average gestational age for ROP-diseased patients in the Bdour et al. study and our study were was similar (29.4 and 28.9 weeks, respectively). The mean birth weight for ROP-diseased patients in the Bdour et al. study was 1320 gms; however, they did not comment on ROP occurring in infants with birth weight higher than 1500 gms. Average birth weight of ROP infants in our study was 1250 gms. The incidence of ROP was higher in infants with birth weight < 1000 gms. In this study the incidence of ROP was 20% among infants with more than 1500 gms. This clearly suggests that any screening program should recommend a higher cutoff for birth weight compared to data from the USA.
Six subjects in our cohort required laser treatment and two-thirds of these subjects were < 1000 gms at birth. Two subjects had birth weight above 1250 gms. The first subject's gestational age was 29 weeks (birth weight, 1350 gms) and required only 1 day of ventilation and 1 day of oxygen therapy. The second subject's gestational age was 33 weeks (birth weight, 1900 gms) and he required prolonged ventilation for more than 2 weeks with an extra 4 days of oxygen therapy. These results suggest that severe ROP that may need intervention still occur in infants above 1250 gms in the Jordanian population. This could be related to the management at NICU (oxygen exposure), or related to a genetic factor or a combination of both. Finding ROP that required intervention among the second infant who was 33 weeks (gestational age) strongly suggest that our screening program should be extended to all infants born at 34 weeks or less.
In the current study, consanguineous marriage was more likely to be found in infants with ROP disease. However, infants from a consanguineous marriage were not at a higher risk of developing severe ROP that required treatment. Although factors such as low birth weight and low gestational age are considered causative factors for ROP,20,21 and factors such as supplemental oxygen therapy are associated with ROP,22 there is indirect evidence suggesting a genetic component in the pathogenesis of ROP. The incidence of ROP is more frequent in white compared to black infants and in males compared to females.23,24 Genetic polymorphism may alter gene function that controls retinal vascularization, such as vascular endothelial growth factor,25,26 which may also be involved in ROP pathogenesis. The role of consanguinity on ROP incidence or severity has rarely been investigated and warrants further research. Investigation of the genetic basis of ROP and, whether genetic polymorphism alters the ROP pattern in different patients, is also required.
The CRYO-ROP study included infants weighing < 1251 gms at birth. There is no established policy on the screening infants larger than 1250 gms. The American screening guidelines for ROP suggests that infants ≤ 1500 gms at birth or ≤ 32 weeks gestational age must be screened and infants > 1500 gms or > 32 weeks be screened at the discretion of the attending neonatologist. However, developing countries likely need to modify these screening guidelines based on a recent report regarding ‘larger’ and ‘older’ infants from developing countries developing more ROP than their counterparts in the United States.
In conclusion, ROP is common among premature infants in Jordan. Infants of higher gestational age and birth weight may also be affected in Jordan. Any national screening guidelines should incorporate the results of the current study. As populations of infants developing ROP differ in by country, a prospective, population-based is required to set national guidelines for ROP screening among Jordanian infants and similarly for different populations worldwide. Consanguinity may have a role in this disease and further genetic studies may add to understanding the pathogenesis of ROP.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Phelps DL. Retinopathy of prematurity. Pediatr Rev. 1995;16:50–6. doi: 10.1542/pir.16-2-50. [DOI] [PubMed] [Google Scholar]
- 2.Repka MX. Ophthalmological problems of the premature infant. Ment Retard Dev Disabil Res Rev. 2002;8:249–57. doi: 10.1002/mrdd.10045. [DOI] [PubMed] [Google Scholar]
- 3.Nødgaard H, Andreasen H, Hansen H, Sørensen HT. Risk factors associated with retinopathy of prematurity (ROP) in northern Jutland, Denmark 1990-1993. Acta Ophthalmol Scand. 1996;74:306–10. doi: 10.1111/j.1600-0420.1996.tb00098.x. [DOI] [PubMed] [Google Scholar]
- 4.Shah VA, Yeo CL, Ling YL, Ho LY. Incidence, risk factors of retinopathy of prematurity among very low birth weight infants in Singapore. Ann Acad Med Singapore. 2005;34:169–78. [PubMed] [Google Scholar]
- 5.Eliason KJ, Dane Osborn J, Amsel E, Richards SC. Incidence, progression, and duration of retinopathy of prematurity in Hispanic and white non-Hispanic infants. J AAPOS. 2007;11:447–51. doi: 10.1016/j.jaapos.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 6.Al-Bdour MD, Al-Till MI, Bin-Tarif RM, Shamayleh AK. Evaluation of risk factors for retinopathy of prematurity at Jordan University Hospital. Middle East J Ophthalmol. 2004;2:108–11. [Google Scholar]
- 7.Section on Ophthalmology American Academy of Pediatrics; American Academy of Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2006;117:572–6. doi: 10.1542/peds.2005-2749. [DOI] [PubMed] [Google Scholar]
- 8.Retinopathy of prematurity: Guidelines for screening and treatment. The report of a Joint Working Party of The Royal College of Ophthalmologists and the British Association of Perinatal Medicine. Early Hum Dev. 1996;46:239–58. [PubMed] [Google Scholar]
- 9.Hutchinson AK, Saunders RA, O’Neil JW, Lovering A, Wilson ME. Timing of initial screening examinations for retinopathy of prematurity. Arch Ophthalmol. 1998;116:608–12. doi: 10.1001/archopht.116.5.608. [DOI] [PubMed] [Google Scholar]
- 10.Goble RR, Jones HS, Fielder AR. Are we screening too many babies for retinopathy of prematurity? Eye. 1997;11:509–14. doi: 10.1038/eye.1997.136. [DOI] [PubMed] [Google Scholar]
- 11.Wright K, Anderson ME, Walker A, Lorch V. Should fewer premature infants be screened for retinopathy in managed care era? Pediatrics. 1998;102:31–4. doi: 10.1542/peds.102.1.31. [DOI] [PubMed] [Google Scholar]
- 12.Binkhathlan AA, Almahmoud LA, Saleh MJ, Srungeri S. Retinopathy of prematurity in Saudi Arabia: Incidence, risk factors, and the applicability of current screening criteria. Br J Ophthalmol. 2008;92:167–9. doi: 10.1136/bjo.2007.126508. [DOI] [PubMed] [Google Scholar]
- 13.Karkhaneh R, Mousavi SZ, Riazi-Esfahani M, Ebrahimzadeh SA, Roohipoor R, Kadivar M, et al. Incidence and risk factors of retinopathy of prematurity in a tertiary eye hospital in Tehran. Br J Ophthalmol. 2008;92:1446–9. doi: 10.1136/bjo.2008.145136. [DOI] [PubMed] [Google Scholar]
- 14.Dogra MR, Narang S, Biswas C, Gupta A, Narang A. Threshold retinopathy of prematurity: Ocular changes and sequelae following cryotherapy. Indian J Ophthalmol. 2001;49:97–101. [PubMed] [Google Scholar]
- 15.Deshpande DA, Chaturvedi M, Gopal L, Ramachandran S, Shanmugasundaram R. Treatment of threshold retinopathy of prematurity. Indian J Ophthalmol. 1998;46:15–9. [PubMed] [Google Scholar]
- 16.Phan MH, Nguyen PN, Reynolds JD. Incidence and severity of retinopathy of prematurity in Vietnam, a developing middle-income country. J Pediatr Ophthalmol Strabismus. 2003;40:208–12. doi: 10.3928/0191-3913-20030701-07. [DOI] [PubMed] [Google Scholar]
- 17.Chen Y, Li X. Characteristics of severe retinopathy of prematurity patients in China: A repeat of the first epidemic? Br J Ophthalmol. 2006;90:268–71. doi: 10.1136/bjo.2005.078063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Basmak H, Niyaz L, Sahin A, Erol N, Gürsoy HH. Retinopathy of prematurity: Screening guidelines need to be reevaluated for developing countries. Eur J Ophthalmol. 2010;20:752–5. doi: 10.1177/112067211002000417. [DOI] [PubMed] [Google Scholar]
- 19.An international classification of retinopathy of prematurity. The Committee for the Classification of Retinopathy of Prematurity. Arch Ophthalmol. 1984;102:1130–4. doi: 10.1001/archopht.1984.01040030908011. [DOI] [PubMed] [Google Scholar]
- 20.Darlow BA, Horwood LJ, Clemett RS. Retinopathy of prematurity: Risk factors in a prospective population-based study. Paediatr Perinat Epidemiol. 1992;6:62–80. doi: 10.1111/j.1365-3016.1992.tb00747.x. [DOI] [PubMed] [Google Scholar]
- 21.Karna P, Muttineni J, Angell L, Karmaus W. Retinopathy of prematurity and risk factors: A prospective cohort study. BMC Pediatr. 2005;5:18. doi: 10.1186/1471-2431-5-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ellsbury DL, Ursprung R. Comprehensive oxygen management for the prevention of retinopathy of prematurity: The pediatrix experience. Clin Perinatol. 2010;37:203–15. doi: 10.1016/j.clp.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 23.Saunders RA, Donahue ML, Christmann LM, Pakalnis AV, Tung B, Hardy RJ, et al. Racial variation in retinopathy of prematurity. The Cryotherapy for Retinopathy of Prematurity Cooperative Group. Arch Ophthalmol. 1997;115:604–8. doi: 10.1001/archopht.1997.01100150606005. [DOI] [PubMed] [Google Scholar]
- 24.Sabri K, Manktelow B, Anwar S, Field D, Woodruff G. Ethnic variations in the incidence and outcome of severe retinopathy of prematurity. Can J Ophthalmol. 2007;42:727–30. doi: 10.3129/i07-136. [DOI] [PubMed] [Google Scholar]
- 25.Dickinson JL, Sale MM, Passmore A, FitzGerald LM, Wheatley CM, Burdon KP, et al. Mutations in the NDP gene: Contribution to Norrie disease, familial exudative vitreoretinopathy and retinopathy of prematurity. Clin Experiment Ophthalmol. 2006;34:682–8. doi: 10.1111/j.1442-9071.2006.01314.x. [DOI] [PubMed] [Google Scholar]
- 26.Kwinta P, Bik-Multanowski M, Mitkowska Z, Tomasik T, Pietrzyk JJ. The clinical role of vascular endothelial growth factor (VEGF) system in the pathogenesis of retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol. 2008;246:1467–75. doi: 10.1007/s00417-008-0865-9. [DOI] [PubMed] [Google Scholar]


