Abstract
Background:
There are various anatomic variations in tracheobronchial system (tracheal bronchus, ectopic bronchus, and accessory bronchus). We aimed to investigate the bronchoscopic findings of the patients with tracheobronchial variations (TBVs) during bronchoscopy and to describe their clinical characteristics.
Materials and Methods:
A total of 3322 records of bronchoscopic examinations in university hospital and 1560 in chest disease hospital total 4882 were retrospectively analyzed and 198 (134 male, 64 female) patients were diagnosed as TBV.
Results:
Mean age of patients was 48.5 ± 17.8 (range, 15–78) years. Most of the tracheobronchial variations (n = 68, 33.1%) were localized at the right upper lobe bronchus. The most common type of TBVs at this region was right upper lobe with two segments. Symptoms were found in 21 (10.2%) patients with TBVs (7 accessory cardiac bronchus, 5 tracheal bronchus, 5 accessory segmental bronchus in left main bronchus and 4 accessory segmental bronchus in right main bronchus). Their symptoms cough, hemoptysis and recurrent pneumonia with unknown etiologies were thought as related to TBVs. No other potential causes leading these symptoms were found in these patients.
Conclusion:
According to our best of knowledge our study population is one of the largest series of bronchoscopy for investigate of TBVs. Although TBVs were usually reported as asymptomatic, nearly 10% of our patients with TBVs had symptoms such as recurrent pneumonia, cough and hemoptysis. TBVs should be taken into consideration in symptomatic patients before fiber-optic bronchoscopic examination.
Keywords: Bronchi, bronchoscopy, trachea, variation
INTRODUCTION
Recognition of tracheobronchial variations (TBVs) can provide important benefits in bronchoscopic processes, pulmonary resection, intubation process, and endobronchial therapy.[1]
Knowledge of tracheobronchial anatomy is a key factor in determining proper position of lung-isolation devices and double-lumen endotracheal tubes. Changes occur in tracheobronchial anatomy with age; therefore, it is very important that every anesthesiologist should be familiar with these anatomical variations in order to recognize anatomical landmarks and perform a successful placement of lung isolation devices.[2]
Although TBVs are rare clinical entity, its recognition and correct diagnosis is important because it can be associated with abnormalities that may require clinical, endobronchial, and in some instances surgical interventions.[3]
Bronchoscopy is frequently performed for diagnosis and treatment of pulmonary diseases. The diagnoses of TBVs are done by bronchoscopy and it is generally reported as asymptomatic. There are some case reports suggesting symptoms related to TBV.[3–5]
Various TBVs (tracheal bronchus, ectopic bronchus, accessory bronchus) can be found during bronchoscopy. These variations are reported as nearly 1%-12%.[1] Knowledge about these variations are needed to distinguish pathological findings and to do an accurate bronchoscopic diagnosis.
In this study, we aimed to evaluate the result of a large series of fiber optic bronchoscopic (FOB) examination reports including clinical features of TBVs patients and their type and localization of variations.
MATERIALS AND METHODS
In this study, we retrospectively evaluated 3475 consecutive FOB examination reports that was performed in Bronchoscopy Center of Pulmonary Diseases Department at Dicle University Medical School between from 1994 to May 2010. And 1603 FOB examination reports in chest disease hospital. No institutional review board approval was taken because of retrospective design of the study. Insufficient reporting and the second or third reports for the same patient (n = 153 in university 40 in chest disease hospital) were excluded. All of bronchoscopic examinations were performed for diagnostic purposes. These examinations were performed with fiber optic bronchoscope (Olympus KV-5) in the presence of two expert bronchoscopists. Lobar and segmental bronchus was visualized and variations were recorded for each, according to Miller's and Minnich anatomical classification [Table 1].[6,7]
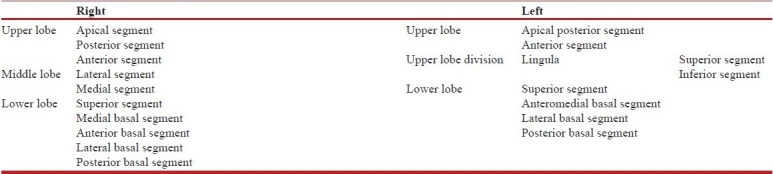
Table 1.
Topographic anatomy of the tracheobronchial tree Fishman et al.[6]
The hospital records of the patients diagnosed as TBVs were investigated. The data were recorded previously prepared on standard forms. The indications of bronchoscopy, demographic data of the patients, type and localization of abnormalities were evaluated.
To diminish the risk of aspiration, oral feeding of the patients was stopped in patients 8 h before FOB. Premedication by Xylocain spray was applied to the nasopharyngeal region with atomization method 15 min before the procedure. Methamisol was given intravenously to each patient in the dose of 2 mg. The patients were monitored throughout the procedure and observed for a cardiac or pulmonary problem. All of the FOB procedure was done via oral route. All of the patients were informed before the process and written consent were obtained.
RESULTS
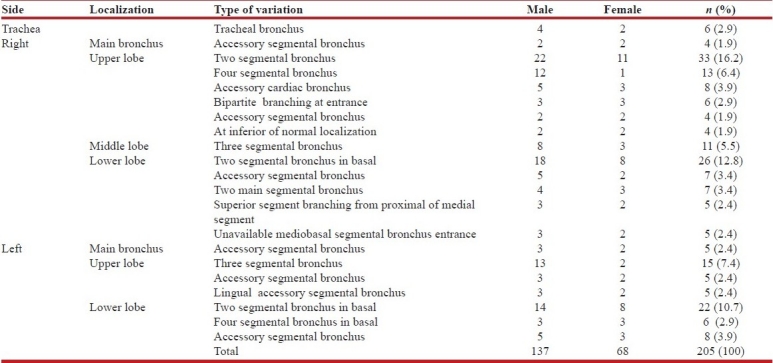
The mean age of TBVs patients were 48.5 ± 17.8 (15–78). A total of 205 TBVs were found in 198 patients. TBVs prevalence was 4.2% among our bronchoscopy series. Of the 198 TBV patients, 134 (68%) was male and 64 (32%) was female. TBVs were most frequently identified in the right upper lobe (n = 68, 33.1%). The most frequent TBVs were the right upper lobe consisting of two segmental bronchi. The second frequent TBVs were two segmental bronchi in lower lobe of left lung.
Seven (3.5%) cases had more than one TBV. Eight (3.9%) cases had accessory cardiac bronchus (ACB). Six cases (2.9%) had tracheal bronchus. The rate of the presence of TBVs in the right bronchial system (133.65%) was higher than that in the left (66.32%) [Table 2].
Table 2.
Detected tracheobronchial variations by bronchoscopy
TBVs had been considered before FOB in only four patients. Accessory segmental bronchus was found in 41 patients (23 (11.2%) right lung and 18 (8.8%) in left lung). Moreover, hemoptysis (n = 12) and recurrent pulmonary infection (n = 9) were detected in 21 (10.2%) patients with (7 have ACB, 5 have Tracheal bronchus, 4 accessory segmental bronchus in right main bronchus and 5 have accessory segmental bronchus in left main bronchus). No other disease, that possibly leading to recurrent pulmonary infection and hemoptysis were detected in these 21 patients.
Indications for FOB intervention were investigated in 198 patients with TBVs and 4684 patients without TBVs. The first indication for FOB was lung mass in both groups. The FOB indications in TBV group lung mass (75 patient (37.8%)), hemoptysis (56 patient (28.3%)) and bronchoalveoler lavage (BAL) for tuberculosis bacilli (21 patient (10.6%)). The FOB indications in non-TBV group lung mass (2056 patient (43.9%), hemoptysis (904 patients (19.3%)) and BAL for tuberculosis bacilli (815 patients (17.4%)).
Some detected TBVs examples are shown in Figure 1(a) and (b).
Figure 1.
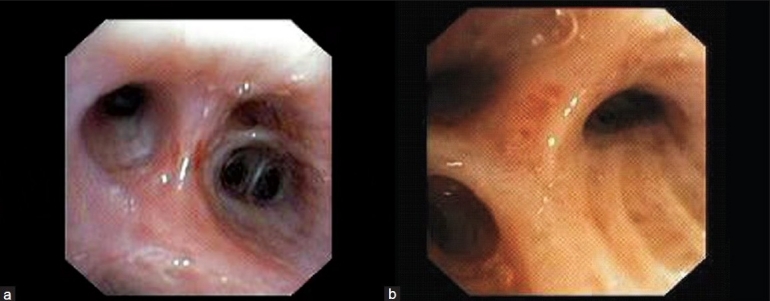
(a) Accessory cardiac bronchus; (b) Three segmental bronchus in the upper lobe of left lung
DISCUSSION
TBVs have developed among 3rd and 16th of gestational weeks.[8,9] Tracheobronchial variation is encountered most frequently in the right upper lobe.[9–13] In this study, most frequently TBVs were seen in the right upper lobe similar to previous publications.[9–13]
We evaluated a large series of FOB reports for TBVs. In literature, there are reports including 2550 and 1114 FOB evaluated for TBVs.[14,15] But we evaluated records of 3351 FOB reports. TBVs as a bronchoscopic diagnosis have been reported as asymptomatic. There are only few case reports suggested some symptoms related to TBVs, such as persistent cough and hemoptysis.[3–5,9,10] We determined in 13 (10.2%) patients symptoms (recurring infection and hemoptysis) which relationship between bronchial variations.
In Turkey, researchers investigated result of 2550 consecutive reports of bronchoscopy retrospectively. Major variations of the tracheobronchial tree were found in 2.6% of patients examined by bronchoscopy. In that study, the most frequent finding was a bifurcate pattern in the right upper lobe (47.7%). The variations were localized in the right upper lobe in 71.6% of patients. Male predominance was observed in all anatomic variations except one.[14] In our study we determined male predominance for all TBVs.
In our study, TBVs prevalence was found as 4.2%. This result is in accordance with the results of previous studies.[1,16] True tracheal bronchus is a bronchus originating from trachea in the region up to 2 cm above to carina and its incidence was reported to be 0.2%.[1] In our series, it was detected in the 2.9% of bronchoscopy results.
True tracheal bronchus may cause some problems especially during intubation.[17] Intubation tube may lead to atelectasis by obstructing the entrance of tracheal bronchus or pneumothorax by entering into tracheal bronchus.[16,18,19] Tracheal bronchus should be taken into consideration in differential diagnosis of recurrent pneumonia in the right upper lobe or the problems such as persistent non homogenous infiltration, bronchiectasis hypoxia, and atelectasis that occurred during anesthesia.[10,17,19] In symptomatic cases, surgical therapy may be needed. Additionally, the cases with bronchial carcinoma originating from tracheal bronchus have been reported.[19,20] In our study, five cases with tracheal bronchus were symptomatic.
Although ACB is generally a sole abnormality, it can be associated with other anomalies of tracheobronchial tree.[11] Spiral computerized tomography is an acceptable method to diagnose ACB.[11,12] Surgery may be needed for the cases with recurring pulmonary infections and hemoptysis. Small case report series have reported.[3–5] In our study these were eight cases with ACB and seven of ACB cases were symptomatic.
Other variations of tracheobronchial tree have also been defined in the literature.[1,14] A left bronchial system identical with the right bronchial system (right isomerism) and a right bronchial system identical with the left bronchial system (left isomerism) can be seen, but in our series such kinds of abnormalities were not. We think that bronchial variations may be more frequent than that we determined since some cases might not have been diagnosed during bronchoscopy.
It was reported that such kind of variations could be determined with virtual bronchoscopy.[21] In another study, it was reported that these variations could be determined during FOB processes in childhood.[22] In another study, a total of 999 TBVs in 475 patients were observed and 71.3% of TBVs were detected in males. In that study, 49.6% of the TBVs were observed in the right bronchial system, 49.2% in the left, and 1.2% in the trachea.[15] The frequency of tracheobronchial variations was higher in that study compared our report. This difference may be related to regional and genetic factors.
One limitation of this study was its retrospective characteristics. In present study we review the FOB examination reports. Tracheobronchial variations were usually reported as asymptomatic; however, we found that 10.2% of our patients with tracheal bronchus and accessory cardiac bronchus had symptoms such as recurrent pneumonia, cough and hemoptysis. Therefore, TBVs should be taken into consideration in symptomatic patients before FOB examination.
A thorough knowledge on bronchial variations is needed to distinguish the pathological findings. Knowledge on TBVs may be needed in bronchoscopy, bronchoalveolar lavage, biopsy and endobronchial therapy processes for pulmonary diseases specialists, in pulmonary resection and transplantation surgery for surgeons and tracheal intubation.
ACKNOWLEDGEMENTS
The research was not financially supported by any grants or any kind of funding from any pharmaceutical company or any other possible sources. All the authors had an active involvement in data collection and analysis, writing, preparation, and reviewing the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ghaye B, Szapiro D, Fanchamps JM. Congenital bronchial abnormalities revisited. Radiographics. 2001;21:105–19. doi: 10.1148/radiographics.21.1.g01ja06105. [DOI] [PubMed] [Google Scholar]
- 2.Campos JH. Update on tracheobronchial anatomy and flexible fiberoptic bronchoscopy in thoracic anesthesia. Curr Opin Anaesthesiol. 2009;22:4–10. doi: 10.1097/ACO.0b013e32831a43ab. [DOI] [PubMed] [Google Scholar]
- 3.Saad CP, Metha AC. Accessory cardiac bronchus. J Bronchol. 2002;9:311–2. [Google Scholar]
- 4.Bentala M, Grijm K, van der Zee JH, Kloek JJ. Cardiac bronchus: A rare cause of hemoptysis. Eur J Cardiothorac Surg. 2002;22:643–5. doi: 10.1016/s1010-7940(02)00431-1. [DOI] [PubMed] [Google Scholar]
- 5.Endo S, Saitoh N, Murayama F, Sohara Y, Fuse K. Symptomatic accessory cardiac bronchus. Ann Thorac Surg. 2000;69:262–4. doi: 10.1016/s0003-4975(99)01200-x. [DOI] [PubMed] [Google Scholar]
- 6.Fishman AP, Elias JA, Fishman JA, Grippi MA, Senior RM, Pack AI. Fishman's Pulmonary Diseases and Disorders. 4th ed. New York: McGraw-Hill; 2008. pp. 21–61. [Google Scholar]
- 7.Minnich DJ, Mathisen DJ. Anatomy of the trachea, carina and bronchi. Thorac Surg Clin. 2007;17:571–85. doi: 10.1016/j.thorsurg.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 8.McLaughlin FJ, Strieder DJ, Harris GB, Vawter GP, Eraklis AJ. Tracheal bronchus: Association with respiratory morbidity in childhood. J Pediatr. 1985;106:751–5. doi: 10.1016/s0022-3476(85)80348-6. [DOI] [PubMed] [Google Scholar]
- 9.Sanchez I, Navarro H, Mendez M, Holmgren N, Caussade S. Clinical characteristics of children with tracheobronchial anomalies. Pediatr Pulmonol. 2003;35:288–91. doi: 10.1002/ppul.10256. [DOI] [PubMed] [Google Scholar]
- 10.Barat M, Konrad HR. Tracheal bronchus. Am J Otolaryngol. 1987;8:118–22. doi: 10.1016/s0196-0709(87)80034-0. [DOI] [PubMed] [Google Scholar]
- 11.Keane MP, Meaney JF, Kazerooni EA, Whyte RI, Flint A, Martinez FJ. Accessory cardiac bronchus presenting with haemoptysis. Thorax. 1997;52:490–1. doi: 10.1136/thx.52.5.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghaye B, Kos X, Dondelinger RF. Accessory cardiac bronchus: 3D CT demonstration in nine cases. Eur Radiol. 1999;9:45–8. doi: 10.1007/s003300050625. [DOI] [PubMed] [Google Scholar]
- 13.Ritsema GH. Ectopic right bronchus: Indication for bronchography. AJR Am J Roentgenol. 1983;140:671–4. doi: 10.2214/ajr.140.4.671. [DOI] [PubMed] [Google Scholar]
- 14.Gonlugur U, Efeoglu T, Kaptanoglu T, Akkurt İ. Major anatomical variations of the tracheobronchial tree: Bronchoscopic observation. Anat Sci Int. 2005;80:111–5. doi: 10.1111/j.1447-073x.2005.00104.x. [DOI] [PubMed] [Google Scholar]
- 15.Beder S, Kupeli E, Karnak D, Kayacan O. Tracheobronchial variations in Turkish population. Clin Anat. 2008;21:531–8. doi: 10.1002/ca.20667. [DOI] [PubMed] [Google Scholar]
- 16.Ikeno S, Mitsuhata H, Saito K. Airway management for patients with a tracheal bronchus. Br J Anaesth. 1996;76:573–5. doi: 10.1093/bja/76.4.573. [DOI] [PubMed] [Google Scholar]
- 17.Conacher ID. Implications of a tracheal bronchus for adult anaesthetic practice. Br J Anaesth. 2000;85:317–21. doi: 10.1093/bja/85.2.317. [DOI] [PubMed] [Google Scholar]
- 18.Doolittle AM, Mair EA. Tracheal bronchus: Classification,endoscopic analysis, and airway management. Otolaryngol Head Neck Surg. 2002;126:240–3. doi: 10.1067/mhn.2002.122703. [DOI] [PubMed] [Google Scholar]
- 19.Aoun NY, Velez E, Kenney LA, Trayner EE. Tracheal bronchus. Respir Care. 2004;49:1056–8. [PubMed] [Google Scholar]
- 20.Tamura M, Murata T, Kurumaya H, Ohta Y. Leiomyoma of an accessory tracheal bronchus. Ann Thorac Surg. 2004;78:2163–5. doi: 10.1016/S0003-4975(03)01500-5. [DOI] [PubMed] [Google Scholar]
- 21.Osma E, Yilmaz E. Virtual bronchoscopy applications. J Int Med Sci. 2006;2:63–7. [Google Scholar]
- 22.Kut A, Karakoc F, Karadağ B, Bakaç S, Dağli E. Flexible bronchoscopy ın childhood: Evaluation of 169 patients. T Klin J Pediatr. 2001;10:197–201. [Google Scholar]


