Diabetes mellitus (DM) has been recognized as a risk factor for the development of pulmonary tuberculosis (PTB). A recent meta-analysis showed that diabetic patients were 3.1 times (95% confidence interval 2.27–4.26) more likely to have tuberculosis than controls,[1] and a prospective study in elderly subjects revealed that this increased risk is limited to those not so well-controlled diabetic patients with hemoglobin A1c ≥ 7%.[2] Duration of symptoms before diagnosis of PTB does not seem to be affected by the presence of DM, but most authors agree with the fact that PTB in diabetics tends to develop presenting features which are somewhat different than in non-diabetic subjects. In this issue of Lung India, Rawat et al. provide further evidence that DM modifies not only the clinical presentation but also the chest X-rays images of PTB, including higher frequencies of lower lobe involvement and cavitations.[3] In countries with low PTB-incidence, this is important because such atypical radiological images may deviate diagnostic suspicion and erroneously be confused with community-acquired pneumonia, cancer, or other conditions.
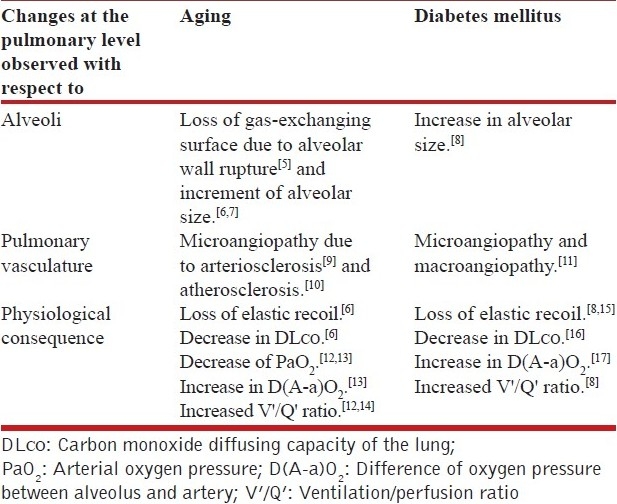
Some years ago, we found in Mexico that in non-diabetic subjects the frequency of tuberculous involvement of lower lung fields progressively increased from ~30% before age 30, to more than 80% at age 80 or older. Contrastingly, lower field involvement was very frequent (always >70%) among diabetics at any age group.[4] Thus, DM seemed to profoundly influence the lung in the same way as aging itself. A literature review corroborates that aging and DM indeed share a lot of morphological and functional consequences in the lung, as can be seen in the following Table 1. In the case of DM, advanced glycation end-products as well as glycosylation of serum and tissue proteins due to chronic hyperglycemia may constitute the bases for the alveolar wall changes and microangiopathic complications.
Table 1.
Similarities between abnormalities at the pulmonary level due to the aging process and those caused by diabetes mellitus
Structural modifications with increased alveolar size and microvascular damage, caused either by DM or aging, may be responsible of the increased ventilation/perfusiσn (V’/Q’) ratio and its well known consequence, a higher alveolar oxygen pressure (PAO2),[18] which should eventually favor multiplication of Mycobacterium tuberculosis. Since in normal conditions, the upper lung regions already have a relatively high V’/Q’ ratio (explaining the usual predominance of upper lung lesions in PTB), the aging- or DM-induced changes should mainly affect lower lung areas (explaining the atypical lower lung involvement of PTB in elders and diabetics).
Cavitary disease is frequently observed in tuberculous patients with DM, but is an uncommon feature in non-diabetic elderly patients.[4] This low frequency of cavitation in elders seems to be correlated to a deficient immune response, resulting in lower frequency of fever, hemoptysis or positive tuberculin skin-test, and lower blood leukocyte count. In contrast, the increased development of cavitation in diabetics and even in elderly people when they are diabetic, lead us to speculate that DM activates a mechanism(s) or factor(s) that promotes cavitation of the lung parenchyma. The nature of this putative cavitary factor sustained by diabetes is as yet unclear.
Experience has taught us that PTB is often manifested in different ways according to some conditions, including DM and aging. Although precise mechanisms by which they change the clinical or radiological features of PTB are largely unclear at present, clinicians must pay attention to these atypical features of PTB, especially because DM is increasingly becoming a worldwide epidemic.
REFERENCES
- 1.Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: A systematic review of 13 observational studies. PLoS Med. 2008;5:e152. doi: 10.1371/journal.pmed.0050152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leung CC, Lam TH, Chan WM, Yew WW, Ho KS, Leung GM, et al. Diabetic control and risk of tuberculosis: A cohort study. Am J Epidemiol. 2008;167:1486–94. doi: 10.1093/aje/kwn075. [DOI] [PubMed] [Google Scholar]
- 3.Rawat J, Sindhwani G, Biswas D. Effect of age on presentation with diabetes: Comparison of nondiabetic patients with new smear-positive pulmonary tuberculosis patients. Lung India. 2011;28:187–90. doi: 10.4103/0970-2113.83975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perez-Guzman C, Torres-Cruz A, Villarreal-Velarde H, Vargas MH. Progressive age-related changes in pulmonary tuberculosis images and the effect of diabetes. Am J Respir Crit Care Med. 2000;162:1738–40. doi: 10.1164/ajrccm.162.5.2001040. [DOI] [PubMed] [Google Scholar]
- 5.Pump KK. Emphysema and its relation to age. Am Rev Respir Dis. 1976;114:5–13. doi: 10.1164/arrd.1976.114.1.5. [DOI] [PubMed] [Google Scholar]
- 6.Butler C, 2nd, Kleinerman J. Capillary density: Alveolar diameter, a morphometric approach to ventilation and perfusion. Am Rev Respir Dis. 1970;102:886–94. doi: 10.1164/arrd.1970.102.6.886. [DOI] [PubMed] [Google Scholar]
- 7.Niewoehner DE, Kleinerman J, Liotta L. Elastic behavior of postmortem human lungs: Effects of aging and mild emphysema. J Appl Physiol. 1975;39:943–9. doi: 10.1152/jappl.1975.39.6.943. [DOI] [PubMed] [Google Scholar]
- 8.Sandler M, Bunn AE, Stewart RI. Pulmonary function in young insulin-dependent diabetic subjects. Chest. 1986;90:670–5. doi: 10.1378/chest.90.5.670. [DOI] [PubMed] [Google Scholar]
- 9.Mackay EH, Banks J, Sykes B, Lee G. Structural basis for the changing physical properties of human pulmonary vessels with age. Thorax. 1978;33:335–44. doi: 10.1136/thx.33.3.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moore GW, Smith RR, Hutchins GM. Pulmonary artery atherosclerosis: Correlation with systemic atherosclerosis and hypertensive pulmonary vascular disease. Arch Pathol Lab Med. 1982;106:378–80. [PubMed] [Google Scholar]
- 11.Lysenko LV. Diabetic macro- and microangiopathy of the lungs. Arkh Patol. 1990;52:31–6. [PubMed] [Google Scholar]
- 12.Cardus J, Burgos F, Diaz O, Roca J, Barbera JA, Marrades RM, et al. Increase in pulmonary ventilation-perfusion inequality with age in healthy individuals. Am J Respir Crit Care Med. 1997;156:648–53. doi: 10.1164/ajrccm.156.2.9606016. [DOI] [PubMed] [Google Scholar]
- 13.Rossi A, Ganassini A, Tantucci C, Grassi V. Aging and the respiratory system. Aging (Milano) 1996;8:143–61. doi: 10.1007/BF03339671. [DOI] [PubMed] [Google Scholar]
- 14.Wagner PD, Laravuso RB, Uhl RR, West JB. Continuous distributions of ventilation-perfusion ratios in normal subjects breathing air and 100 per cent O2. J Clin Invest. 1974;54:54–68. doi: 10.1172/JCI107750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schuyler MR, Niewoehner DE, Inkley SR, Kohn R. Abnormal lung elasticity in juvenile diabetes mellitus. Am Rev Respir Dis. 1976;113:37–41. doi: 10.1164/arrd.1976.113.1.37. [DOI] [PubMed] [Google Scholar]
- 16.Agarwal AS, Fuladi AB, Mishra G, Tayade BO. Spirometry and diffusion studies in patients with type-2 diabetes mellitus and their association with microvascular complications. Indian J Chest Dis Allied Sci. 2010;52:213–6. [PubMed] [Google Scholar]
- 17.Ljubic S, Metelko Z, Car N, Roglic G, Drazic Z. Reduction of diffusion capacity for carbon monoxide in diabetic patients. Chest. 1998;114:1033–5. doi: 10.1378/chest.114.4.1033. [DOI] [PubMed] [Google Scholar]
- 18.West JB. Respiratory physiology: The essentials. Philadelphia: Lippincott Williams and Wilkins; 2008. [Google Scholar]


