Abstract
Background:
To better understand the longitudinal trend in the proportion of techniques employed for cerebral aneurysm treatment, we reviewed our experience with 2253 patients over the last 11 years.
Methods:
We reviewed data in our prospective aneurysm database for all consecutive patients treated from January 1998 through December 2009. Data regarding age, sex, aneurysm location, presence or absence of hemorrhage, Fisher grade, clinical grade, treatment methods, length of hospitalization, and mortality rates by the time of discharge were retrieved and retrospectively analyzed. The most common aneurysm types were subsequently classified and analyzed separately.
Results:
The patient population included 663 males (29%) and 1590 females (71%). A total of 2253 patients presented with 3413 aneurysms; 1523 (63%) of the aneurysms were diagnosed as aneurysmal subarachnoid hemorrhage. A total of 2411 (71%) aneurysms were treated. Overall, 645 (27%) of the 2411 aneurysms underwent endosaccular coiling and 1766 (73%) underwent clip ligation; 69 (3%) of these aneurysms required both treatment modalities. The percentage of all aneurysms treated by endosaccular coiling increased from 8% (21) in 1998 to 28% (87) in 2009. There was no statistical difference between the average length of hospitalization for patients who underwent endosaccular coiling and clip ligation for their ruptured (P = 0.19) and unruptured (P = 0.80) aneurysms during this time period.
Conclusions:
In our practice, endovascular treatment has continued to be more frequently employed to treat cerebral aneurysms. This technique has had the greatest proportional increase in the treatment of posterior circulation aneurysms.
Keywords: Cerebral aneurysm, clip ligation, endovascular coiling, trend
INTRODUCTION
Endosaccular coiling has revolutionized the care of cerebral aneurysms. Multiple landmark studies have documented the effectiveness and safety of endosaccular coiling as an alternative to clip ligation.[3,13,16] These studies have foreshadowed trends in the general application of these two methods for aneurysm treatment. The International Subarachnoid Aneurysm Trial (ISAT) is the only randomized control trial that has tested this coiling treatment and shown the safety of coiling versus clipping.[13] Since its introduction in the early 1990s, the number of aneurysms treated by endosaccular coiling has steadily increased, especially in academic medical centers. As newer technology has emerged and technique has been refined, coiling has become a standard treatment for intracranial aneurysms.[1,4,5,11,17] To better understand the longitudinal trend in the proportion of these techniques applied in a busy cerebrovascular practice, the authors reviewed their experience in the management of cerebral aneurysms from 1998 through 2009. These trends have not been previously reported for different aneurysm types in the United States.
MATERIALS AND METHODS
Goodman Campbell Brain and Spine maintains a comprehensive, prospective aneurysm database containing records from 4127 patients treated from 1976 to the present. This database was searched to obtain relevant data for all consecutive patients treated from January 1998 through December 2009. This time period was selected because we have routinely offered endosaccular coiling as an option for aneurysm treatment since 1997. Data regarding age, sex, aneurysm location, presence or absence of hemorrhage, Fisher grade, clinical grade, treatment methods, and mortality rates by the time of discharge were retrieved and retrospectively analyzed.
The potential for surgical or endovascular treatment was routinely discussed for most subarachnoid hemorrhage patients following their diagnostic study, and again for most elective aneurysm patients, at our biweekly, multidisciplinary, cerebrovascular conference. The approval of the Institutional Review Board at the Methodist Hospital was obtained.
RESULTS
General patient population
A total of 2253 patients (663 males, 1590 females) presented with 3413 aneurysms. Of these, 2411 aneurysms were treated. Upon detailed evaluation, treatment was determined to be not appropriate for the remaining aneurysms, which were found among patients with either poor neurologic or medical status or incidentally among patients with multiple aneurysms. Of the 2411 (71%) aneurysms that were treated, 1950 (81%) were located in the anterior circulation, and 461 (19%) were in the posterior circulation.
Of the 2411 aneurysms treated, 1523 (63%) were diagnosed as aneurysmal subarachnoid hemorrhage, and of these, 1105 (72%) were classified as Hunt–Hess grades I–III (42%, 10%, and 20%, respectively), and 412 (27%) were Hunt–Hess grades IV and V (19% and 8%, respectively). Hunt-Hess scores were not available for six patients.
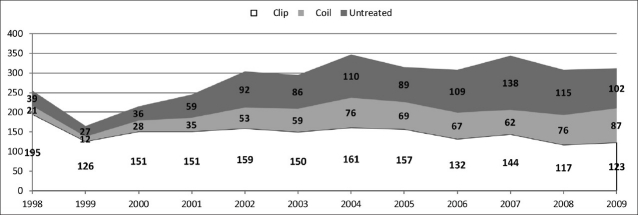
Of the 2411 aneurysms treated, 645 (27%) were treated with endosaccular coiling, and 1766 (73%) were managed with clip ligation. These numbers include 69 (3%) aneurysms that required both treatment modalities. The number of all aneurysms treated by endosaccular coiling increased from 21 (8%) in 1998 to 87 (28%) in 2009. However, the total number of aneurysms treated by clip ligation decreased from 195 (76%) in 1998 to 123 (39%) in 2009 [Figure 1].
Figure 1.
Total number of aneurysms showing the number untreated and treated by endosaccular coiling and clip ligation from 1998 to 2009
Patient subgroups
The percentage of basilar artery bifurcation aneurysms treated by endovascular methods increased from 22% in 1998 to 88% in 2009 [Figure 2]. During this same time, the proportion of anterior communicating artery aneurysms managed with endosaccular coiling increased from 6% to 38%, whereas the percentage of these aneurysms treated by clip ligation alone declined from 92% to 57% [Figure 3]. Of all posterior-communicating artery aneurysms, 5% were treated with coiling in 1998 compared with 31% in 2009. Furthermore, 93% of these aneurysms underwent clip ligation in 1998 versus 62% in 2009 [Figure 4]. The middle cerebral artery aneurysms were managed primarily through clip ligation during the study period.
Figure 2.
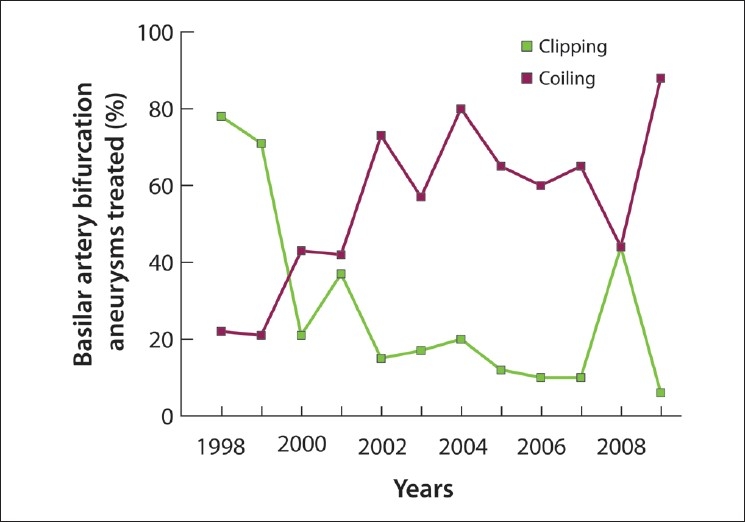
Percentage of basilar artery bifurcation aneurysms treated by endosaccular coiling versus clip ligation
Figure 3.
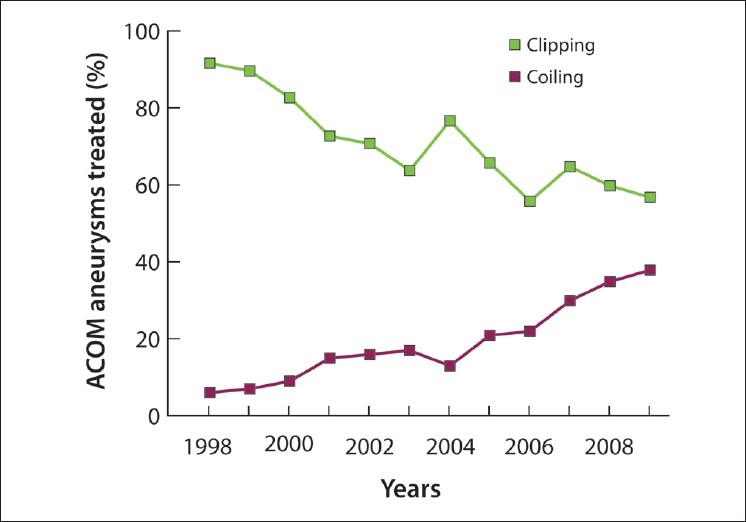
The percentage of anterior communicating artery aneurysms managed with endosaccular coiling increased, and the percentage of these aneurysms treated by clip ligation declined during the study period
Figure 4.
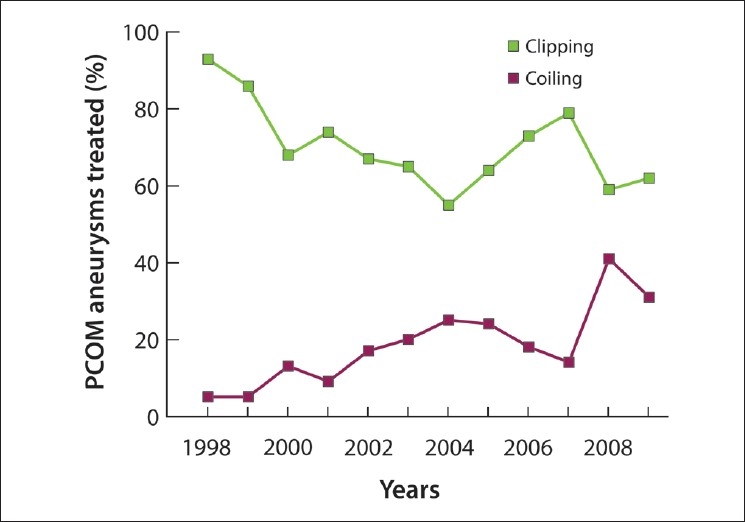
The percentage of posterior communicating artery aneurysms managed with endosaccular coiling increased and the percentage of these aneurysms treated by clip ligation declined during the study period
Of the 479 patients over age 60, 40% (190) were managed with endosaccular coiling, and 60% (289) were selected for clip ligation; however, these older patients have increasingly been treated by endosaccular coiling [Figure 5].
Figure 5.
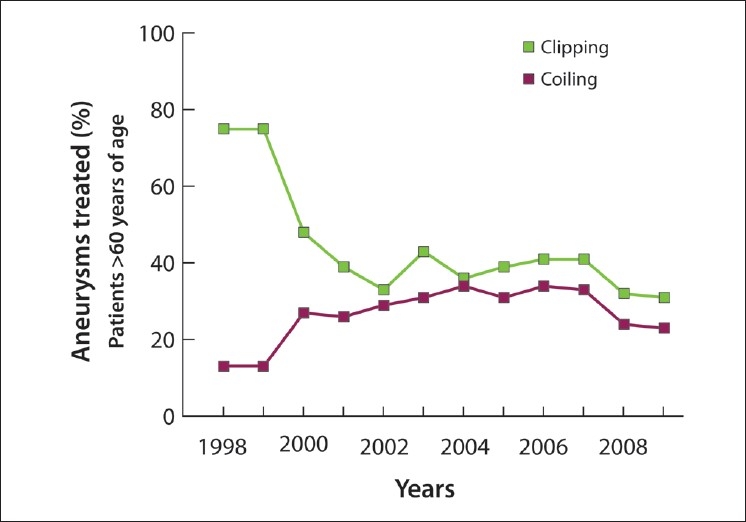
Older patients have increasingly been treated with endosaccular coiling
The proportion of patients with poor Hunt-Hess grades (grades IV and V) at the time of treatment who underwent endosaccular coiling increased from 15% in 1998 to 38% in 2009. The overall mortality rate for all the patients with cerebral aneurysms during their hospital stay has remained relatively constant during this time period (12% in 1998 to 11% in 2009).
There was no statistically significant difference between the average length of hospitalization for patients who underwent endosaccular coiling or clip ligation for their ruptured (average: 15 versus 14 days; P = 0.19) and unruptured (average: 3 versus 4.5 days; P = 0.80) aneurysms .
DISCUSSION
Overall, the number of cerebral aneurysms undergoing treatment is increasing.[1,4,5,11,17] This increase may be due to the more frequent discovery of incidental unruptured aneurysms when scans are performed for unrelated conditions.[1,4] Since the early 1990s, endosaccular aneurysm treatment has become an increasingly important part of aneurysm care. Participating surgeons and interventionists in major cerebrovascular centers have fostered their philosophy on the effectiveness and safety of endosaccular coiling versus clip ligation based on their center's experience with these treatment methods and interpretation of the available literature. This philosophy is dynamic, evolving, and affects the proportion of the patients who undergo each treatment paradigm. A detailed assessment of the utility of each method over time and the outcome from each technique will shape the future of aneurysm care. Our findings reflect our philosophy for treatment of cerebral aneurysms.
The treatment trends observed in our series reflect the nationwide movement toward using endovascular therapy more frequently.[1,4–6,17] Most patients in nonacademic hospitals with a lack of neurointervention support are still managed with clip ligation.[4,6] Certain types of aneurysms, such as middle cerebral artery bifurcation and giant aneurysms, as well as those with wide necks or intraluminal thrombus, may be best managed surgically.[15] We have retained a lower threshold to offer clip ligation to younger patients (<55 years of age) and those who harbor relatively accessible aneurysms (P-comm and MCA aneurysms).
Because the technique of endosaccular coiling is still relatively new, adequate long-term follow-up data are not yet available comparing the durability of endosaccular versus surgical aneurysm obliteration, especially among younger patients. However, the available studies have provided certain trends. In general, patients who undergo surgical clipping may have longer hospital stays following their procedure and an increased rate of complications.[11,18,20] Surgical clipping carries a greater durability, with fewer clipped aneurysms recanalizing and rebleeding, whereas coiled aneurysms may recanalize and, in some instances, rebleed.[5,11] The endovascular approach may be preferred for posterior circulation aneurysms because of the potentially high rates of morbidity following surgery.[18] The long-term outcome of small recurrent aneurysms that previously underwent endosaccular coiling is not clearly defined. Such recurrent aneurysms pose an important treatment dilemma, especially among our younger patients. Clip ligation of such recurrent aneurysms is associated with an increased risk. Johnston et al.[11] found that adverse outcomes were significantly more common in surgical cases (18.5%) compared to endovascular cases (0.6%).
In our study, the length of hospitalization did not differ between the patients who underwent clip ligation versus endosaccular coiling, regardless of their aneurysm rupture status. There was no statistically significant difference between the average length of hospitalization for the patients who underwent endosaccular coiling or clip ligation for their ruptured (average: 15 versus 14 days; P = 0.19) and unruptured (average 3 versus 4.5 days; P = 0.80) aneurysms. Our patients’ mortality rates during the decade studied did not decrease despite the more frequent use of endosaccular coiling. These results are likely to be affected by selection bias because the patients who harbored more risk factors for a poor outcome, including elderly patients and those with a poor Hunt-Hess grade, were likely selected for intervention therapies. A more sensitive battery of tests, such as detailed neuropsychological evaluation, may be necessary to assess the potential morbidity associated with clip ligation, especially among patients with unruptured aneurysms in comparison with endovascular occlusion. It is difficult to assess the superiority of one technique versus another using mortality rates alone. Randomized controlled trials are needed to account for confounding factors.
Other recent studies mirror our findings that currently at least one-third of aneurysms are managed through endovascular techniques. We have offered clip ligation to our patients as the preferred treatment option since the durability of clip ligation has been definitively established and this modality does not carry excessive risks. A survey of 100 neurosurgical departments in Germany revealed that 63% of aneurysms were selected for clip ligation versus 37% for endosaccular coiling.[19] Natarajan et al.[14] reported that among 195 consecutive patients, 55% underwent microsurgical clip ligation and 45% underwent endosaccular coiling between January 2005 and June 2006.[14] Other surgeons have favored clip ligation. Hoh et al.[10] reviewed 515 patients admitted between November 1995 and February 2003. Of these, 413 (80%) underwent clip ligation, whereas 79 (15%) underwent endosaccular coiling. Conversely, some centers have chosen to significantly increase the share of coiling procedures. Andaluz and Zuccarello[1] reported that in their center, the number of endovascular procedures doubled from 1993 to 2003.
The reason for the trend over time for each method's application has not been clearly defined. Gnanalingham et al.[7] reported an increase in the proportion of patients undergoing endovascular treatment from 35% to 68% between February 2001 and May 2003. The authors attributed this increase to the results of the ISAT trial published in 2002. The ISAT study affected the practice of vascular neurosurgery considerably, especially in some centers.[5] Ogungbo et al.[17] reported that from 1990 to 1998, the proportion of patients undergoing surgery decreased from 66.3% to 35.3%. An overall lower morbidity/mortality rate for endovascular treatment is a major factor in favor of endovascular treatment when either modality can be employed.[1,6]
In our practice, treatment of less surgically accessible aneurysms, such as those in the basilar artery bifurcation region, has undergone the most impressive transformation, especially around the years 2000–2002. At present, more than 80% of such aneurysms undergo endosaccular coiling. These trends are likely the result of the evolution of endovascular technology, including the introduction of stent-assisted and balloon-assisted aneurysm coiling, both of which show great potential to expand the role of endosaccular coiling in the treatment for wide-neck cerebral aneurysms previously considered “uncoilable.”[12]
We have also seen an overall increase in the number of Hunt–Hess grade IV and V patients treated. This is reflective of a general willingness by interventionists to treat poor-grade patients immediately, along with an increase in the admission of these patients.[17,21] Until recently, the prevailing standard of care has been to manage Hunt–Hess grade IV and V patients conservatively (medically) until they stabilize and reach a better grade (III or better) before initiating a more aggressive treatment. In general, these patients have very poor outcomes with surgical clipping.[22] However, Bailes et al.[2] found that grade IV and V patients who are treated only medically experience a high mortality rate. Ogungbo et al.[17] ascribe a 50/50 chance of survival as compared to poor-grade patients, regardless of the treatment used.[17] In addition to this study, other groups have evaluated outcomes among the patients who first undergo conservative management. Hoh et al.[10] found only a 15% favorable outcome rate for such patients , and Hijdra et al.[8] found 71% mortality in the patients whose treatment was delayed. Endovascular treatment, on the other hand, shows promise in the treatment of this population, and as such, it is now used much more frequently in our center as well as others.[22]
At the same time, elderly patients (over age 60) have been increasingly treated by endosaccular coiling [Figure 5]. This trend is seen in other centers as well.[1] This trend may be especially beneficial for this subset of patients as well as their younger counterparts since they generally may not tolerate surgery. The durability of the treatment is of less concern in the older population; therefore, endovascular treatment may be a preferred option because this modality seems to decrease mortality for the stated short follow-up intervals reported.[4,6]
The choice of whether to treat using surgical or endovascular methods has remained controversial and many authors have addressed this question.[4,5,11,15] There is no consensus, and each patient must be evaluated individually concerning the characteristics of his/her aneurysm, such as its location, size, and morphology. The age of the patient and clinical grade are also critical factors to tailor the optimal treatment choice.[4,5,11,15] A consultation for each patient should be undertaken involving, at the very least, clinicians with expertise in both microsurgical and endovascular techniques, to determine the best course of treatment.[4–6]
Each method carries its own advantages, and a multidisciplinary approach has become the standard of care. The determination of the exact criteria to select appropriate candidates for either treatment modality remains to be defined. Some situations in which surgery is warranted include patient preference toward surgery, the need for relief of the mass effect from a hemorrhage, and the lack of availability of timely (within 72 h) therapy with endovascular methods.[5] More sensitive large-scale studies using post-treatment neuropsychological evaluation and long-term durability trials will significantly influence the type of care that patients with cerebral aneurysms will receive.
The cost associated with the two procedures is another factor that may drive some centers to employ particular techniques.[1,11] Johnston et al.[11] found that the mean cost associated with clip ligation (the overall cost of therapy including any additional procedures after the initial coiling or clipping) was significantly higher than that of a patient treated with endosaccular coiling: $43,000 for clipping versus $30,000 for coiling. However, Hoh et al.[9] found that coiling was associated with higher hospital costs in both patients with unruptured and ruptured aneurysms, and attributed the higher cost to the higher cost of the coils themselves versus clipping devices.
Future considerations
The trend toward more endosaccular coiling will likely continue as higher generation of stents, including flow diverting and disrupting stents such as Pipeline (Chestnut Medical Technologies, Menlo Park, CA, USA) are popularized. Such stenting technology will further facilitate the occlusion of previously considered “broad-neck” aneurysms. Where is the ultimate plateau to be reached in terms of the proportion of aneurysms treated endovascularly versus surgically? The answer is not currently known. Similarly, the future of aneurysm surgery is not completely clear, but some speculations can be made.
Although the surgical technology has remained relatively unchanged during the past decade, the endovascular technology continues to evolve. This will decrease the number of aneurysms undergoing clip ligation. This phenomenon will place the art of aneurysm surgery only in the hands of selected groups of surgeons in the few specialized “aneurysm care centers” treating technically challenging aneurysms that are not amenable to other treatment methods. The exposure of neurosurgical residents and their hands-on experience to treat these challenging lesions will be minimized. Will this situation discourage residents from aggressively pursuing the art of microsurgical aneurysm care? The aneurysms that are not amenable to endovascular techniques will present enormous challenges that require surgeons with special skills, temperament, and dedication. Will future trainees be ready to take on the responsibility required to acquire the necessary skills?
CONCLUSIONS
Endosaccular coiling has been established to play an important role in the treatment of cerebral aneurysms. This method is surpassing clip ligation for posterior circulation aneurysms in our practice. The aneurysms referred for clip ligation will be more technically challenging with further advances in endovascular care. More sensitive tools in large-scale studies with adequate long-term follow-up are necessary to define the role of clip ligation versus endovascular techniques for the treatment of cerebral aneurysms.
ACKNOWLEDGMENT
The authors acknowledge the involvement of Elaine Bammerlin in the preparation of this manuscript.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2011/2/1/110/83728
Contributor Information
Troy D. Payner, Email: TPayner@goodmancampbell.com.
Itay Melamed, Email: imelamed@goodmancampbell.com.
Shaheryar Ansari, Email: sfansari@iupui.edu.
Thomas J. Leipzig, Email: TLeipzig@goodmancampbell.com.
John A. Scott, Email: JScott@goodmancampbell.com.
Andrew J. DeNardo, Email: ADeNardo@goodmancampbell.com.
Terry G. Horner, Email: THorner@goodmancampbell.com.
Kathleen Redelman, Email: kathrede@iupui.edu.
Aaron A. Cohen-Gadol, Email: acohenmd@gmail.com.
REFERENCES
- 1.Andaluz N, Zuccarello M. Recent trends in the treatment of cerebral aneurysms: Analysis of a nationwide inpatient database. J Neurosurg. 2008;108:1163–9. doi: 10.3171/JNS/2008/108/6/1163. [DOI] [PubMed] [Google Scholar]
- 2.Bailes JE, Spetzler RF, Hadley MN, Baldwin HZ. Management morbidity and mortality of poor-grade aneurysm patients. J Neurosurg. 1990;72:559–66. doi: 10.3171/jns.1990.72.4.0559. [DOI] [PubMed] [Google Scholar]
- 3.Byrne JV, Sohn MJ, Molyneux AJ, Chir B. Five-year experience in using coil embolization for ruptured intracranial aneurysms: Outcomes and incidence of late rebleeding. J Neurosurg. 1999;90:656–63. doi: 10.3171/jns.1999.90.4.0656. [DOI] [PubMed] [Google Scholar]
- 4.Cowan JA, Jr, Ziewacz J, Dimick JB, Upchurch GR, Jr, Thompson BG. Use of endovascular coil embolization and surgical clip occlusion for cerebral artery. J Neurosurg aneurysms. 207;107:530–5. doi: 10.3171/JNS-07/09/0530. [DOI] [PubMed] [Google Scholar]
- 5.Crocker M, Corns R, Hampton T, Deasy N, Tolias CM. Vascular neurosurgery following the International Subarachnoid Aneurysm Trial: modern practice reflected by subspecialization. J Neurosurg. 2008;109:992–7. doi: 10.3171/JNS.2008.109.12.0992. [DOI] [PubMed] [Google Scholar]
- 6.Flett LM, Chandler CS, Giddings D, Gholkar A. Aneurysmal subarachnoid hemorrhage: Management strategies and clinical outcomes in a regional neuroscience center. AJNR Am J Neuroradiol. 2005;26:367–72. [PMC free article] [PubMed] [Google Scholar]
- 7.Gnanalingham KK, Apostolopoulos V, Barazi S, O’Neill K. The impact of the international subarachnoid aneurysm trial (ISAT) on the management of aneurysmal subarachnoid haemorrhage in a neurosurgical unit in the UK. Clin Neurol Neurosurg. 2006;108:117–23. doi: 10.1016/j.clineuro.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Hijdra A, van Gijn J, Nagelkerke NJ, Vermeulen M, van Crevel H. Prediction of delayed cerebral ischemia, rebleeding, and outcome after aneurysmal subarachnoid hemorrhage. Stroke. 1988;19:1250–6. doi: 10.1161/01.str.19.10.1250. [DOI] [PubMed] [Google Scholar]
- 9.Hoh BL, Chi YY, Dermott MA, Lipori PJ, Lewis SB. The effect of coiling versus clipping of ruptured and unruptured cerebral aneurysms on length of stay, hospital cost, hospital reimbursement, and surgeon reimbursement at the University of Florida. Neurosurgery. 2009;64:614–9. doi: 10.1227/01.NEU.0000340784.75352.A4. [DOI] [PubMed] [Google Scholar]
- 10.Hoh BL, Topcuoglu MA, Singhal AB, Pryor JC, Rabinov JD, Rordorf GA, et al. Effect of clipping, craniotomy, or intravascular coiling on cerebral vasospasm and patient outcome after aneurysmal subarachnoid hemorrhage. Neurosurgery. 2004;55:779–86. doi: 10.1227/01.neu.0000137628.51839.d5. [DOI] [PubMed] [Google Scholar]
- 11.Johnston SC, Dudley RA, Gress DR, Ono L. Surgical and endovascular treatment of unruptured cerebral aneurysms at university hospitals. Neurology. 1999;52:1799–805. doi: 10.1212/wnl.52.9.1799. [DOI] [PubMed] [Google Scholar]
- 12.Koebbe CJ, Veznedaroglu E, Jabbour P, Rosenwasser RH, et al. Endovascular management of intracranial aneurysms: Current experience and future advances. Neurosurgery. 2006;59:S93–102. doi: 10.1227/01.NEU.0000237512.10529.58. [DOI] [PubMed] [Google Scholar]
- 13.Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005;366:809–17. doi: 10.1016/S0140-6736(05)67214-5. [DOI] [PubMed] [Google Scholar]
- 14.Natarajan SK, Sekhar LN, Ghodke B, Britz GW, Bhagawati D, Temkin N. Outcomes of ruptured intracranial aneurysms treated by microsurgical clipping and endovascular coiling in a high-volume center. AJNR Am J Neuroradiol. 2008;29:753–9. doi: 10.3174/ajnr.A0895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nussbaum ES, Madison MT, Myers ME, Goddard J. Microsurgical treatment of unruptured intracranial aneurysms. A consecutive surgical experience consisting of 450 aneurysms treated in the endovascular era. Surg Neurol. 2007;67:457–64. doi: 10.1016/j.surneu.2006.08.069. [DOI] [PubMed] [Google Scholar]
- 16.Ogilvy CS, Hoh BL, Singer RJ, Putman CM. Clinical and radiographic outcome in the management of posterior circulation aneurysms by use of direct surgical or endovascular techniques. Neurosurgery. 2002;51:14–21. doi: 10.1097/00006123-200207000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Ogungbo B, Gregson BA, Blackburn A, Mendelow AD. Trends over time in the management of subarachnoid haemorrhage in Newcastle: review of 1609 patients. Br J Neurosurg. 2001;15:388–95. doi: 10.1080/02688690120082387. [DOI] [PubMed] [Google Scholar]
- 18.Peluso JP, Van Rooij WJ, Sluzewski M, Beute GN. Coiling of basilar tip aneurysms: Results in 154 consecutive patients with emphasis on recurrent haemorrhage and re-treatment during mid- and long-term follow-up. J Neurol Neurosurg Psychiatry. 2008;79:706–11. doi: 10.1136/jnnp.2007.127480. [DOI] [PubMed] [Google Scholar]
- 19.Sakowitz OW, Raabe A, Vucak D, Kiening KL, Unterberg AW. Contemporary management of aneurysmal subarachnoid hemorrhage in Germany: Results of a survey among 100 neurosurgical departments. Neurosurgery. 2006;58:137–45. doi: 10.1227/01.neu.0000194532.47239.7c. [DOI] [PubMed] [Google Scholar]
- 20.Schaafsma JD, Sprengers ME, van Rooij WJ, Sluzewski M, Majoie CB, Wermer MJ, et al. Long-term recurrent subarachnoid hemorrhage after adequate coiling versus clipping of ruptured intracranial aneurysms. Stroke. 2009;40:1758–63. doi: 10.1161/STROKEAHA.108.524751. [DOI] [PubMed] [Google Scholar]
- 21.van Rooij WJ, Sluzewski M. Endovascular treatment of large and giant aneurysms. AJNR Am J Neuroradiol. 2009;30:12–8. doi: 10.3174/ajnr.A1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weir RU, Marcellus ML, Do HM, Steinberg GK, Marks MP. Aneurysmal subarachnoid hemorrhage in patients with Hunt and Hess grade 4 or 5: Treatment using the Guglielmi detachable coil system. AJNR Am J Neuroradiol. 2003;24:585–90. [PMC free article] [PubMed] [Google Scholar]