Abstract
Traumatic neuromas are characterized by the presence of pain, burning, or paresthesia, associated with a history of trauma, normally surgery, in the same site. In the oral cavity, the most commonly affected sites are the lip, tongue, and mental nerve area. Pressure on the suspected area usually provokes pain. They microscopically consist of a proliferation of nerve fascicles embedded in a background of collagen. We present a case of a 42-year-old Latin American female patient complaining of a painful solitary nodule erupting on the lingual surface of the mandibular body. Histopathological analysis showed a traumatic neuroma associated with mature ganglion cells, which is an extremely unusual finding. After complete removal of the lesion the symptoms disappeared. To the best of our knowledge, this is the first case of a unique lesion with unusual clinical and histopathological features reported in the English language literature.
Keywords: Traumatic neuroma, ganglion cells, pseudoganglioneuroma, oral
INTRODUCTION
Traumatic neuroma is an exuberant, but non-neoplastic proliferation of a nerve occurring in response to an injury or surgery. The principal features of oral traumatic neuroma are similar to traumatic neuromas elsewhere in the body. Clinically, it presents as a firm nodule that is occasionally tender or painful on palpation.[1,2] Strangulation of the proliferating nerve caused by scar tissue, local trauma, or infection may be responsible for the pain. The most common oral sites are the lip, tongue, and mental nerve area. Microscopically, it consists of a haphazard proliferation of nerve fascicles, including axons, Schwann cells, fibroblasts embedded in the background of a collagen, and sometimes associated with chronic inflammation.[1,3] Eventually, it can present mature ganglion cells, being called pseudoganglioneuroma.[2] It is important to differentiate this condition, from ganglioneuroma, ganglioneuroblastoma, ganglioneuromatous tumor, subgemmal neurogenous plaque, and some neurofibromas,[4–6] in order to avoid misdiagnosis and consequently inadequate treatment.
This article describes a case of traumatic neuroma of the oral cavity containing a mature ganglion cell cluster with satellite cells. A search of the English language literature did not reveal cases with these clinical and histopathological features.
CASE REPORT
A 42-year-old Latin American female patient was referred to the Oral Diagnosis Clinic (OROCENTRO), Piracicaba Dental School – UNICAMP, complaining of a painful swelling in the right side of the mouth persisting for about three years, impairing her to use a complete lower denture. The patient denies trauma or surgery on the oral lesion site and her medical history was noncontributory. Intraoral examination showed a painful, submucous mass tumor with fibroelastic consistency, covered by normal mucosa, measuring 4.0 × 2.0 cm, located on the lingual face of the right mandibular body [Figure 1]. Our main clinical hypotheses of diagnosis were neural benign tumor or other benign mesenchymal tumor. Under local anesthesia, an excisional biopsy was carried out and the microscopical analysis showed a haphazard proliferation of prominent nerve fascicles, including axons with their investitures of myelin, Schwann cells, and fibroblasts, embedded in a fibrotic stroma, with focal areas of hyalinized collagen. Characteristic clefts-like spaces between the stroma and nervous component were also observed [Figure 2]. A large mature ganglion cell cluster surrounded by satellite cells and nerve fiber bundles was found within the stromal fibrosis [Figure 3]. These histological features corresponded to traumatic neuroma with mature ganglion cells. The patient has been in follow-up for three years without signs of recurrence.
Figure 1.
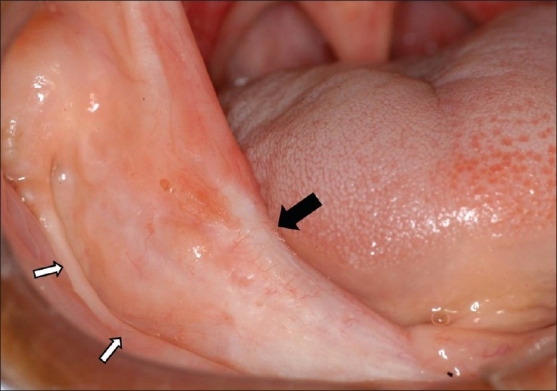
Panoramic view of a tumor mass on the lingual surface of the right mandibular body (black arrow). Note the extensive alveolar ridge resorption (white arrows)
Figure 2.
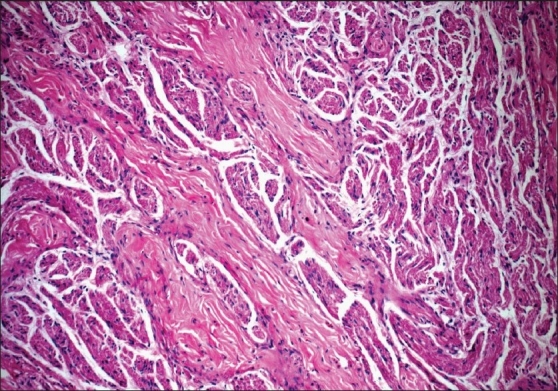
Nervous component intermingled with rich collagen bundles. Note the cleft-like spaces (H and E, ×10)
Figure 3.
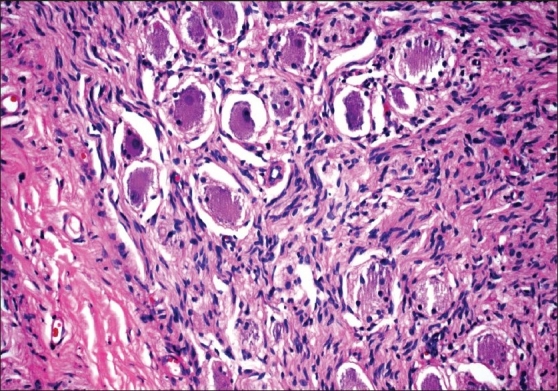
Mature ganglion cell cluster surrounded by satellite cells and nerve fiber bundles (H and E, ×20).
DISCUSSION
Although traumatic neuroma may form on any damaged nerve, it occurs more commonly in small nerves than in large nerves. Etiological factors particularly include previous surgical procedures, however, other events such as pressure, ischemia, crushing injuries, lacerations, stretching, cuts, bleeding to the surrounding tissue have also been considered. The most common sites in the mouth are the lip, tongue, and mental nerve area. Pain can be present in about 25% of the cases, and perhaps may be due to the constriction of nerves by stromal fibrosis.[1,2] The relation between the presence of inflammatory cell infiltrate in the injured nerve and pain is uncertain.[3] Once a neuroma is formed, removal is indicated specially when it becomes symptomatic. Interestingly, our case showed a painful, submucous nodular lesion in an unusual location, on the ramus and body of the mandible, following the route of the inner oblique line, probably associated with constant trauma caused by the pressure of the overextended denture borders. Some authors have reported that disturbances such as paresthesia and anesthesia can be related to the nerve size.[1,3] Our patient did not reveal any sensorial alteration, which implies that probably the lesion developed in the small nerves. After removal of the lesion, the patient reported complete cessation of oral symptoms.
Microscopically, the fact that some of these lesions contain ganglion cells should not come as a surprise, as this process may represent the involvement of a pre-existing ganglion in this region or involvement of a ganglionized nerve fiber.[3] Smith and Harn[7] demonstrated the presence of nerve cell bodies in 40 / 44 (91%) lingual nerves in the third molar area after studying the heads of 22 adult human cadavers. Because of the relationship of the lingual nerve with the submandibular ganglion it is believed that these cell bodies are parasympathetic. In our case, the possibility that the ganglion cells represent the involvement of these lingual nerve cell bodies cannot be discarded. Daneshvar et al.[2] showed that 6 / 14 cases (43%) of pharyngeal traumatic neuroma contained mature ganglion cells, which denominated pseudoganglioneuroma. Thus, pseudoganglioneuroma should be distinguished from other neural lesions presenting ganglion cells, and probably our case represents this same entity.
Ganglioneuromas occur in patients between 10 and 30 years of age, are well-circumscribed and encapsulated, and are most frequently located in the posterior mediastinum, retroperitoneum, and adrenal glands, being uncommon in the alimentary tract. Histologically it is composed of clusters of mono, bi, or multinucleate-ganglion cells deposited in a fibrillar neuromatous stroma.[8] Ganglioneuroma in the jaws is exceptional; to date only five cases have been reported, occurring centrally in the mandible.[5] Ganglioneurofibroma presents with more spindled-cell stroma and the number of axons are decreased. Ganglioneuroblastoma most commonly occurs in infants and young children and almost never occurs after the age of 10. Histologically, they are considered malignant because they contain primitive neuroblasts along with mature ganglion cells.[4] Pseudoganglioneuroma differs histologically from these tumors because the two components, ganglion cells surrounded by satellite cells and the neuroma, do not intermingle and are contained within a fibrous stroma.
Lee et al.[4] report a combined heterotopia of ganglion cells and hamartomatous neuroma. This was a cutaneous soft-tissue polypoid lesion, and microscopically displayed many isolated ganglion-like cells without satellite cells in the papillary dermis, and fascicles of unmyelinated axons in the lower dermis.
Subgemmal neural plaques are aggregates of nerve plexus and ganglion cells, usually organized in a neural tumor-like pattern, which incidentally, can be found in specimens of the lateral border of the tongue. Clinically, it may be associated with the erythematous area, ulcer, white patch, or hyperplasic papule. The lesions could be reactive, representing neuronal dysplasias, or be a result of trophic influences from gustatory nerve fibers.[6]
Traumatic neuromas are sometimes confused with neurofibromas. Participation of all elements of the nerve fascicles and identification of a damaged nerve distinguish a traumatic neuroma of neurofibroma. Neurofibroma is usually found to be deep-rooted, does not have a predilection for a specific site, and persistently grows causing expansion. Microscopically, the cells are arranged in short fascicles, whorls, or even in a storiform pattern.[6] In some patients with von Recklinghausen's disease, scattered, solitary, or clustered mature ganglion cells are observed within the plexiform neurofibromas.[9] There was no history or sign of von Recklinghausen's disease in our patient.
In multiple endocrine neoplasia MEN2b, mucosal neuromas involve the mucosal surfaces of the lips, mouth, eyelids, and intestines. The patients usually present with medullary carcinoma of the thyroid, pheochromocytoma of the adrenal glands, and skeletal anomalies. Histologically, the oral lesions present tortuous bundles of nerves, with a prominent perineurium within a fibrous stroma. Rare cases can present mature ganglion cells within enlarged lingual nerves. Differently, in the gastrointestinal tract both submucosal and myenteric plexus appear to be hyperplastic, showing Schwann cells and ganglion cells. This ganglioneuromatous proliferation can also occur in different settings as von Recklinghausen’s neurofibromatosis, Cowden's disease, or juvenile polyposis coli.[9,10] The clinical and histopathological features of our patient excluded these possible diagnoses.
Unusual cellular types, in association with traumatic neuroma were also described. Giménez-Bascuñana and Piqueras-Pérez[11] reported a case that disclosed features of both granular cell tumor and traumatic neuroma affecting the submandibular salivary gland, called granular cell traumatic neuroma. Ide and Umemura analyzing the surgical specimen of squamous cell carcinoma of the floor of the mouth, showed a case of traumatic neuroma with intralesional glandular structures, localized in the submucosal tissue of the alveolar mucosa. In this case, probably the residual salivary ducts of the minor salivary glands became incorporated during the development of a traumatic neuroma.
CONCLUSION
We report a case of oral traumatic neuroma with mature ganglion cells and unusual clinical features. It is important to recognize this condition in order to avoid misdiagnosis with other neural tumors associated with ganglion cells. All these conditions may present a clinical diagnostic challenge and inadequate treatment may be administered if they are not adequately recognized.
Footnotes
Source of Support: The National Council for Scientific and Technological Development (CNPq)
Conflict of Interest: Non declared.
REFERENCES
- 1.Sist TC, Jr, Greene GW. Traumatic neuroma of the oral cavity: report of thirty-one new cases and review of the literature. Oral Surg Oral Med Oral Pathol. 1981;51:394–402. doi: 10.1016/0030-4220(81)90149-3. [DOI] [PubMed] [Google Scholar]
- 2.Daneshvar A. Pharyngeal traumatic neuromas and traumatic neuromas with ganglion cells (pseudoganglioneuromas) Am J Surg Pathol. 1990;14:565–70. doi: 10.1097/00000478-199006000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Vora AR, Loescher AR, Craig GT, Boissonade FM, Robinson PP. A light microscopical study on the structure of traumatic neuromas of the human lingual nerve. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:395–403. doi: 10.1016/j.tripleo.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Lee JY, Martinez AJ, Abell E. Ganglioneuromatous tumor of the skin: a combined heterotopia of ganglion cells and hamartomatous neuroma: report of a case. J Cutan Pathol. 1988;15:58–61. doi: 10.1111/j.1600-0560.1988.tb00518.x. [DOI] [PubMed] [Google Scholar]
- 5.Oeppen R, Brennan P, Stutley J. Ganglioneuroma of the mandible: radiologic and pathologic findings of a rare tumor. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:259–62. doi: 10.1067/moe.2000.103646. [DOI] [PubMed] [Google Scholar]
- 6.Triantafyllou A, Coulter P. Structural organization of subgemmal neurogenous plaques in the foliate papillae of tongue. Hum Pathol. 2004;35:991–9. doi: 10.1016/j.humpath.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 7.Smith EE, Harn SD. Presence of nerve cell bodies in the lingual nerve in the third molar area. J Oral Maxillofac Surg. 1989;47:931–5. doi: 10.1016/0278-2391(89)90376-5. [DOI] [PubMed] [Google Scholar]
- 8.McDaniel RK. Subepithelial nerve plexus (with ganglion cells) associated with taste buds. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:605–9. doi: 10.1016/s1079-2104(99)70142-3. [DOI] [PubMed] [Google Scholar]
- 9.Pham BN, Villanueva RP. Ganglioneuromatous proliferation associated with juvenile polyposis coli. Arch Pathol Lab Med. 1989;113:91–4. [PubMed] [Google Scholar]
- 10.Sallai A, Hosszu E, Gergics P, Racz K, Fekete G. Orolabial signs are important clues for diagnosis of the rare endocrine syndrome MEN 2B.Presentation of two unrelated cases. Eur J Pediatr. 2008;167:441–6. doi: 10.1007/s00431-007-0532-x. [DOI] [PubMed] [Google Scholar]
- 11.Gimenez-Bascunana A, Piqueras-Perez FM. Granular cell traumatic neuroma of salivary gland. Arch Pathol Lab Med. 2001;125:1000–1. doi: 10.5858/2001-125-1000-GCTNOS. [DOI] [PubMed] [Google Scholar]


