Abstract
Purpose
The proximate use of illicit drugs or alcohol (substance use) is the most common precipitator of facial injuries among socioeconomically disadvantaged populations. Reducing these risky behaviors could minimize adverse health sequelae and potential reinjury. The objective of our study was to test whether a culturally competent, personalized motivational intervention incorporated into surgical care could significantly reduce existing substance use behaviors in facial injury patients.
Patients and Methods
Substance-using subjects (n = 218) presenting with facial injuries to a level 1 trauma center were randomly assigned to either a personalized motivational intervention (PMI) condition or a health-information (HI) control condition. After a brief assessment of the individual’s substance use severity and willingness to change these behaviors, both groups attended 2 counseling sessions with a trained interventionist. The PMI subjects (n = 118) received individualized, motivational interventions, whereas the HI subjects (n = 100) received only general health information. Both groups were reassessed at 6 and 12 months postinjury, and changes in substance-use patterns were measured to assess the effects of intervention.
Results
The PMI and HI groups were closely matched on their sociodemographic and substance use characteristics. Subjects in the PMI group showed statistically significant declines in drug use at both the 6- and 12-month assessments. The intervention’s effect on lowering illicit drug use was greatest at the 6-month assessment but had weakened by the 1-year follow-up. The efficacy of the PMI was moderated by an individual’s initial drug use severity; individuals with greater drug use dependency at baseline were seen to have larger intervention effects, as did individuals who were most aware of their drug problem and willing to change their substance use behaviors. Unlike illicit drug use, changes in alcohol use did not differ significantly between the intervention and control groups, irrespective of an individuals’ recognition of the alcohol problem or willingness to take steps to address it.
Conclusion
A culturally competent, motivational intervention integrated into the care of vulnerable patients with facial injury can reduce illicit drug use behaviors. Subgroups of injured patients appear to benefit most from such personalized motivational interventions. A better articulation of target populations, intervention content, and delivery would allow for directed interventions and an appropriate focusing of limited time and health care resources.
Oral and maxillofacial surgeons at regional trauma centers commonly treat patients with facial injuries resulting from interpersonal violence linked to the proximate use of illicit drugs or alcohol (substance use).1–6 Beyond the elevated risk for various health problems,7 these substance use behaviors also predispose an individual to repeat injury or recidivism.8 The causal relationships among substance use, violence, and injury are complex but organize along 2 dominant themes: violence related to attempts to procure drugs or substance use–induced disinhibition that leads to aggressive behavior. The strong linkage between substance use and injury is underscored by research documenting positive serum ethanol and urine toxicology screens in 80% of intentional trauma victims.9 Furthermore, individuals evidencing substance use at the time of initial injury are at a much greater risk for recurrent trauma.10,11 Similar themes are echoed by Sims and colleagues,12 who, in a 5-year longitudinal study of general trauma patients, determined that the incidence of substance abuse was 67% among those with recurrent injury. More specific to facial injuries, Murphy et al1 determined that 58% of individuals presenting to an urban trauma center with a jaw fracture qualified as problem drinkers, and 24% met the criteria for problem drug use. Because the associations among substance use, injury, and reinjury are so compelling, various organizations, including the American College of Surgeons, now recommend that all trauma center admissions be considered as an expression of underlying substance use problems and the basis for screening and behavioral interventions that address causal substance use behaviors.13
The use of the trauma center as an opportunistic setting for conducting behavioral interventions targeting risky behaviors is especially germane to the care of individuals presenting with intentional facial injury. Most orofacial injury patients treated at our urban trauma centers tend to be young, otherwise healthy, socioeconomically disadvantaged males, and the trauma center is frequently their only contact with the health care system.8 Because of their relative youth, this group is more likely to consist of at-risk/problem users or in the early stages of alcohol/drug dependence. For such patients, often unable or unwilling to access additional speciality care to address the underlying causes leading to the injury, integrating brief screenings and interventions into the surgical care may be the best means of minimizing continued risky behaviors and adverse outcomes, particularly reinjury. The conceptual appeal of these interventions draws from the feeling of vulnerability precipitated by the injury. Research indicates that the postinjury period of increased receptivity, or “teachable moment,” presents a unique opportunity to engage injured patients in secondary prevention efforts.14,15 Trauma center staff could capitalize on the effects of the recent injury to encourage at-risk patients to reflect on the relationship between their risky behavior and its consequences and increase their motivation to change the behavior.16 Designed as secondary prevention practices, these behavioral interventions investigate the underlying cause of injury (eg, substance use) and thereby motivate the individual to do something about it, either by natural, patient-directed means, or by seeking additional treatment. The content of the brief intervention varies depending on the type of risky behavior, the severity of the problem being addressed, and the desired outcome.
Motivational interventions have been evaluated in substance users in a variety of settings and using delivery modes raging from brief, stand-alone interventions to elaborate multisession interventions.17–24 Meta-analytical reviews suggest that this approach could be appropriate and effective in busy emergency care settings.25,26 Building on precursor research by Gentillo et al,15 investigators such as Sonderstrom et al27 have shown that targeted behavioral interventions can be effective in reducing drinking and health consequences in at-risk alcohol users treated in trauma settings. Specific to facial injury, the work of British injury researchers16,19 indicate that even brief motivational interventions can produce sustained reductions in risky alcohol use behaviors. However, there have been no published evaluations of such interventions when applied to the type of patients most commonly presenting with violence-related facial injuries to United States–based urban trauma centers—namely, young, socioeconomically disadvantaged, racial/ethnic minorities.4,5,8
To investigate whether a motivational intervention for substance use behaviors integrated into facial injury care would be effective in an urban trauma care setting, we developed a 2-session intervention that incorporated motivational techniques developed by Miller.28 The intervention derived from our earlier work29 that emphasized cultural competency in reaching and motivating racial/ethnic minorities with substance use problems. The primary aim of our study was to test whether a personalized motivational intervention incorporated into facial injury care could reduce substance (illicit drug/alcohol) use behaviors. Secondary aims were to determine whether the effectiveness of the intervention is moderated by the patient’s initial substance use severity and willingness to change the substance use behaviors. We hypothesized that a personalized, culturally congruent, substance use intervention integrated into surgical care would significantly reduce illicit drug/alcohol consumption in facial injury patients with a history of substance use.
Patients and Methods
STUDY DESIGN
We conducted a 2-arm randomized controlled study to test the efficacy of a personalized motivational intervention designed to reduce substance use in trauma patients. Recruited over a 3-year period, orofacial injury patients evidencing substance use and other risk behaviors were assigned randomly to either a personalized motivational intervention (PMI) condition or a health information (HI) control condition. In addition to standard surgical care, both groups attended 2 counseling sessions with a trained interventionist: individuals in the intervention group received individualized, motivational interventions along with a written health handout listing available resources for substance abuse and medical treatment along with active referrals; individuals in the control group received brief general health information along with a copy of a health handout listing resources for substance abuse and medical treatment.
SETTING
The study was conducted at the Los Angeles County/University of Southern California (LAC-USC) Medical Center, a publicly funded, level-1 trauma center serving east Los Angeles County. The LAC-USC Medical Center meets the health care needs of a large socioeconomically marginalized population, described as the uninsured, the working poor, homeless, and recent immigrants. The hospital catchment area encompasses large ethnic minority groups that are primarily Hispanic/Latino (64%) or African American (32%).
RECRUITMENT OF PARTICIPANTS
The study population consisted of patients presenting to the Oral and Maxillofacial Surgery Service for treatment of a recent facial injury that required follow-up care. All noncritically injured adults (18 years or older) with trauma resulting from interpersonal violence and a history of illicit drug and/or alcohol use were considered eligible. Subjects were excluded if they evidenced cognitive impairments or psychiatric problems, were in police custody or institutionalized, did not speak either English or Spanish, or were unwilling to return for long-term follow-up assessments. Research staff approached injured patients after initiation of surgical care and screened them for substance use behaviors (described subsequently). Individuals who screened positive for risky/harmful alcohol use or reported use of illicit drugs (ie, crack cocaine, heroin, marijuana) within the past 6 months were considered eligible. For interested patients, the staff obtained informed consent using a scripted recruitment approach and protocols approved by the Institutional Review Boards of the University of California—Los Angeles and the University of Southern California. All participants were compensated for assessments done at the baseline and follow-up visits (1, 6, and 12 months postinjury).
ASSESSMENT INSTRUMENTS
Enrolled subjects completed a comprehensive baseline assessment that elicited sociodemographic, substance use, and psychosocial information.
Illicit drug use was determined with the validated Texas Christian University Drug Screen—II (TCUDS). A self-report measure of drug use, the TCUDS is used as a brief screening for drug use frequency, treatment history, drug dependence, and motivation for treatment. The summary score can range from 0 to 9, with a score of 1 or higher indicating possible drug abuse and 3 or greater indicative of relatively severe drug-related problems. The TCUDS has a test–retest validity of 0.97 and an 82.1% overall accuracy rate in detecting substance use dependency disorders.30 Cronbach’s alpha in our sample ranged from 0.85 to 0.88 at each assessment. Additionally, the University of California—Los Angeles brief drug history form elicited details on the frequency and amount of illicit drug use (categories included inhalants, marijuana, hallucinogens, amphetamines, downers, heroin, other opiates, crack, cocaine, tranquilizers, PCP, and synthetic drugs) in the preceding 30 days.
The 10-item Alcohol Use Disorders Identification Test (AUDIT) screened for risky/harmful drinking over the previous 90 days.31 The AUDIT assesses 3 key dimensions: drinking pattern or quantity/frequency, symptoms of dependence, and problems caused by alcohol. It reliably distinguishes between patients with hazardous and harmful drinking histories and those without such histories. Cronbach’s alpha suggested good internal consistency in our sample, with values at each assessment ranging from 0.84 to 0.86.
In addition to these substance use measures, information was also collected on several other domains, including physical and psychological health status, resource utilization, available social support, and engagement with treatment and other support services.
RANDOMIZATION
After the research staff completed baseline screening and intake interviews, the project manager randomized the enrollees to the intervention or control group. A computer-generated randomization procedure guided assignment to the intervention or control condition. Health care providers and research staff involved in the follow-up assessments were blinded to randomization status.
INTERVENTION
All subjects attended 2 counseling sessions: the first occurred shortly after study entry and the second occurred 4 to 6 weeks later. Both sessions coincided with and immediately followed scheduled visits for surgical follow-up care. Depending on the study-arm assignment, the face-to-face sessions lasted from 15 to 60 minutes and were conducted by a bilingual (English and Spanish) interventionist with a master’s degree in social work. The interventionist was trained in motivational intervention techniques by a certified trainer and practitioner of motivational interviewing. Intervention fidelity was ensured through use of a script introducing the main themes of motivational interviewing and regular supervision meetings with the trainer who reviewed the interventionist’s technique and conducted random audit of tape recordings of the intervention sessions.
Whereas subjects in the control group received brief health information, subjects in the PMI group received an individualized behavioral intervention. Because the construct of readiness for change is a major component of motivational intervention techniques, subjects in the PMI group were evaluated at the outset with the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES)32 for both alcohol and drug use. The SOCRATES yields 3 reliable subscales: Ambivalence, which indicates the level of patients’ uncertainty about their substance use behaviors; Recognition, which indicates the level of patients’ willingness to acknowledge their problems; and Taking Steps, which indicates the level of patients’ readiness to change their behaviors. The SOCRATES scale has a high test–retest reliability (alpha >0.87) and satisfactory internal consistency (alpha >0.60) and has been validated among patients with comorbid mental and substance use disorders.33 In our sample, Cronbach’s alpha ranged from 0.89 to 0.98 for all subscales at all assessment time points.
The content and format of the intervention was derived from culturally congruent strategies described by Longshore et al29 and was tailored to the participant’s substance use behaviors and stage of readiness for change. Invoking relevant cultural values, the interventionist began the first session with feedback on the participant’s substance use patterns, comparison with national patterns, and a discussion of the consequences at both an individual and community level. Outside these methods of tailoring the MI to the individual, delivery of the protocol was standardized. The interventionist’s role was to encourage the participants to think differently about their substance use behaviors, raise awareness of the consequences, and generate an interest in quitting. For subjects at early stages of change (precontemplation or contemplation), the counselor emphasized techniques targeting the patient’s cognition about alcohol/drug use (developing discrepancy, avoiding argument, and rolling with resistance), and on the change processes most relevant at those early stages (consciousness raising, dramatic relief, and environmental reevaluation). For patients at later stages of change (preparation and action)—that is, patients already changing or preparing to change—the counselor emphasized action-oriented techniques that promoted self-efficacy. The change processes at these later stages are largely behavioral: counter-conditioning (finding behavioral alternatives to alcohol/drug use), stimulus control (avoiding people and places associated with alcohol/drug use), and contingency management (spending time with people who support the participant’s effort to change).
In the second counseling session conducted after 4 to 6 weeks, subjects assigned to the PMI group received a “booster” reinforcement. The interventionist began this session with a review of the change plan devised during the baseline PMI, initiated a dialogue about any recent negative consequences from substance use, and reviewed value priorities from the first session. Participants were encouraged to elaborate on change-promoting factors and any change-inhibiting factors presented opportunities for problem solving. The interventionist highlighted themes that emerged during the intervention and reinforced change-oriented talk. Finally, subjects were assisted in developing concrete, behavior-based goals, achievable within a 1-to 2-month time frame and provided with self-help materials for achieving these goals and active referrals for substance abuse and medical treatment.
OUTCOME MEASURES
Follow-up occurred at 6 and 12 months after hospital discharge. Research staff unaware of the subject’s assignment conducted follow-up assessments. Primary outcomes included changes in patterns of illicit drug use (TCUDS and number of drug-using days, for all drugs as well as for the primary drug of choice), and changes in patterns of alcohol use (AUDIT, days of alcohol use, use of alcohol to intoxication).
DATA ANALYSIS
The itinerant nature and lifestyle of our study population is reflected in the differential dropout rates at the 6-month (treatment group 48.3%; control group 38%) and 12-month (treatment group 56.8%; control group 43%) follow-ups. Data analysis was confined to the available cases; and demographic variables for age, gender, ethnicity, and employment were analyzed with independent-samples t tests and χ2 tests of independence to determine comparability of groups.
Paired t tests were used to analyze changes from baseline in continuously scaled measures. Differences between changes from baseline in the PMI and control arms were compared with independent-samples t tests on the changes from baseline. To investigate whether the effectiveness of the PMI is moderated by initial substance use or readiness to change, we used analysis of variance models for changes from baseline with factors for intervention group, category of substance use or readiness to change, and their interaction.
Results
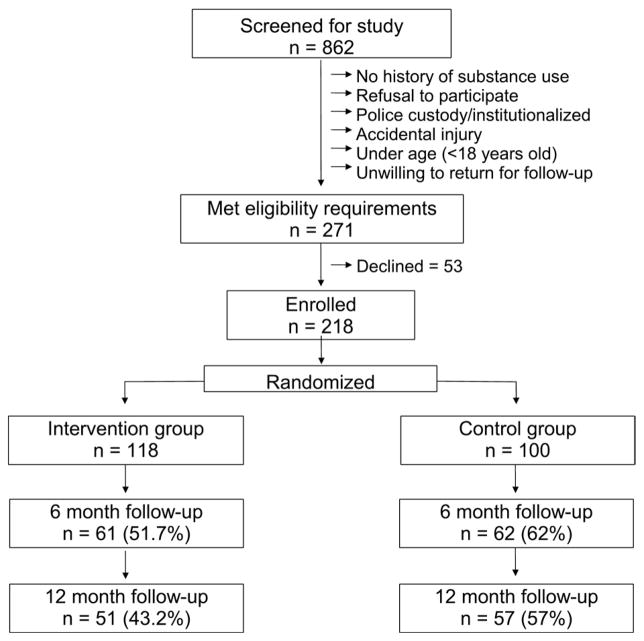
Of the 862 facial injury patients screened in the enrollment period (January 2005 to June 2008), 271 patients met eligibility criteria and 218 (80.4% of those eligible) were enrolled and randomized into the intervention (n = 118) and control (n = 100) groups. Of the enrolled subjects, 51.7% in the intervention group and 62.0% in the control group completed the 6-month follow-up, and 43.2% in the PMI group and 57.0% in the control group completed the 12-month follow-up (Fig 1).
FIGURE 1.
Study flow.
COMPARISON OF PARTICIPANT STATISTICS
Table 1 summarizes the sociodemographic characteristics of study cohort. The 2 groups were successfully balanced on all sociodemographic characteristics with the exception of employment status: the unemployment rate in the intervention group (71.8%) was significantly higher (P =.013 by χ2 test) than in the control group (55.6%).
Table 1.
SAMPLE DESCRIPTIVES (N = 218)*
| Variable | PMI (n = 118) | Control (n = 100) |
|---|---|---|
| Gender | ||
| Male | 92.4 | 91.0 |
| Female | 7.63 | 9.00 |
| Ethnicity | ||
| Black/African American | 27.1 | 24.0 |
| Mexican/Mexican American | 35.6 | 45.0 |
| Other Latino | 10.2 | 5.00 |
| White non-Latino | 8.47 | 13.0 |
| Native American/Alaskan | 2.54 | 0.00 |
| Asian/Pacific Islander | 2.54 | 1.00 |
| Multiethnic | 7.63 | 5.00 |
| Other | 5.93 | 7.00 |
| Country of birth | ||
| United States | 71.2 | 75.0 |
| Other | 28.8 | 25.0 |
| Marital status | ||
| Married | 8.47 | 10.0 |
| Cohabitating | 10.2 | 12.0 |
| Widowed | 0.00 | 1.00 |
| Separated | 9.32 | 10.0 |
| Divorced | 8.47 | 7.00 |
| Never married | 63.6 | 60.0 |
| Legal problems | ||
| Yes | 28.0 | 27.0 |
| No | 72.0 | 73.0 |
| Employment status | ||
| Employed | 28.2 | 44.4 |
| Unemployed | 71.8 | 55.6 |
| Highest level of education | ||
| Less than high school | 36.8 | 44.0 |
| High school graduate or GED | 28.2 | 23.0 |
| Some college or trade or tech or AA | 32.5 | 30.0 |
| 4-year college or more | 2.56 | 3.00 |
| Has or had family member with alcohol problem | ||
| Yes | 40.5 | 36.0 |
| No | 59.5 | 64.0 |
| Has or had family member with drug problem | ||
| Yes | 32.5 | 27.0 |
| No | 67.5 | 73.0 |
Abbreviations: AA, Associate of Arts degree; GED, General Educational Development.
Mean (range) age in personalized motivational intervention (PMI) group, 32.2 (19–62); control group, 31.1 (18–59).
Mean (range) number of days worked in past 30 for PMI = 5.8 (0–30); for control: 6.5 (0–30).
Some percentage values within category do not add up to 100% because of missing response.
As evidenced by Table 2, the 2 groups (PMI and control) did not differ significantly on any of their baseline substance-use characteristics.
Table 2.
SUMMARY OF SUBSTANCE USE AT BASELINE*
| Variable | Control Group | MI Group | P Value† |
|---|---|---|---|
| Any drugs in past 30 days | 38 (38%) | 52 (44%) | .442 |
| TCUDS ≥3 | 21 (21%) | 36 (31%) | .163 |
| Any alcohol in past 30 days | 78 (78%) | 92 (78%) | .874 |
| Alcohol to intoxication in past 30 days | 49 (49%) | 50 (42%) | .399 |
| AUDIT score ≥8 | 65 (66%) | 66 (58%) | .264 |
| Marijuana use in past 30 days | 31 (31%) | 43 (36%) | .483 |
| Any other drug use in past 30 days | 16 (16%) | 25 (21%) | .422 |
| TCUDS | 1.4 (2.4) | 1.8 (2.6) | .274 |
| Drug days in past 30 | 7.8 (14.3) | 8.7 (15) | .653 |
| Days used most frequent drug in past 30 | 6.3 (10.5) | 6.8 (10.7) | .742 |
| AUDIT score | 12.1 (9.3) | 11.2 (9) | .453 |
| Days used alcohol in past 30 | 7.3 (8.9) | 7.6 (9.6) | .812 |
| Days used alcohol to intoxication in past 30 | 3.6 (6.1) | 4.6 (7.9) | .329 |
Abbreviations: AUDIT, Alcohol Use Disorders Identification Test; TCUDS, Texas Christian University Drug Screen.
Table entries are n (5) or mean (SD).
P values for categorical outcomes are from χ2 tests of independence. P values for continuous outcomes are from independent-sample t test.
1. DID THE PERSONALIZED MOTIVATIONAL INTERVENTION DECREASE PARTICIPANTS’ USE OF ILLICIT DRUGS?
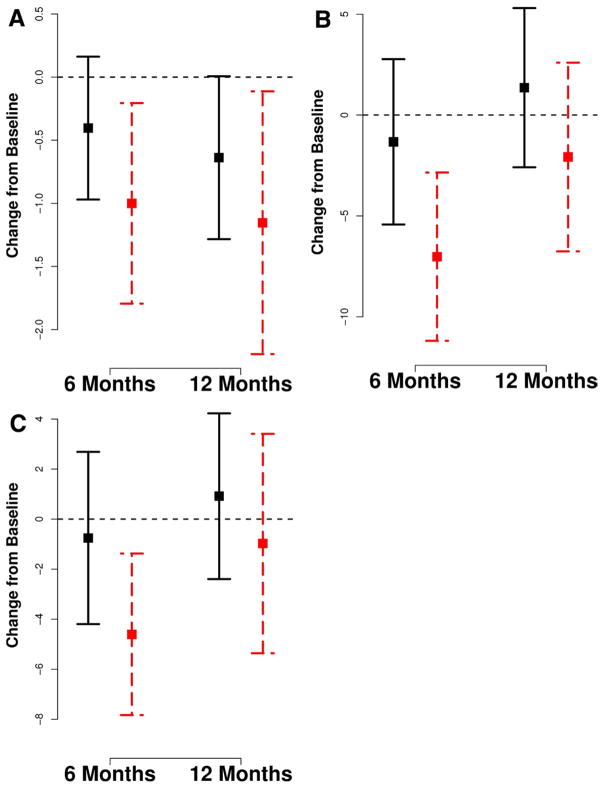
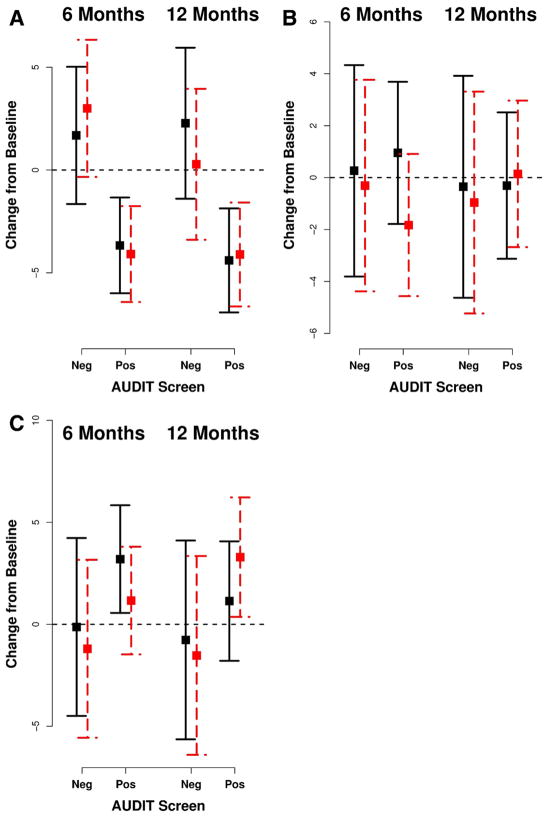
Figure 2 displays the distribution of the drug use measures, relative to the baseline (hospital intake) scores, at the follow-up assessments for the 2 groups. A score corresponding to 0 denotes no change from baseline, with negative numbers indicative of a decline in substance use. Subjects in the PMI group manifested statistically significant declines in their TCUDS scores (Fig 2A) at both the 6-month (mean decrease = −1.0, P =.015) and 12-month assessments (mean decrease = −1.15; P =.033). Although the TCUDS scores also declined in the control group, particularly at the 12-month assessment (mean decrease = −0.64; P =.054), the magnitude of the decline was not as great as that found in the intervention group; nonetheless, the difference in average change scores was not statistically significant. Changes in drug use patterns are further explored in Figure 2B, C, which show, relative to baseline, the changes in the number of drug-using days (for all drugs) as well the use of the primary illicit drug. The PMI group evidenced a larger decline in drug-using days at the 6-month assessment (mean decrease in all drug use = 7.02 days, P =.001; mean decrease in use of primary drug = 4.6 days, P =.006), and this decrease in use of all drugs (drug-days) was more pronounced than in the control group to an extent that approached conventional levels of statistical significance (interaction P =.054). At the 12-month follow-up, the drug use frequency in both groups appeared to regress back to baseline use patterns, although the PMI group continued to show greater average declines in drug use patterns compared with the control group.
FIGURE 2.
Plots of change scores from baseline (horizontal dotted line) for drug use outcomes at follow-up assessments. Error bars represent ± 2 SE. Solid vertical lines are for control group; dashed vertical lines are for personalized motivational intervention group. A, Texas Christian University Drug Screen—II (TCUDS) score. B, Drug-days. C, Primary drug.
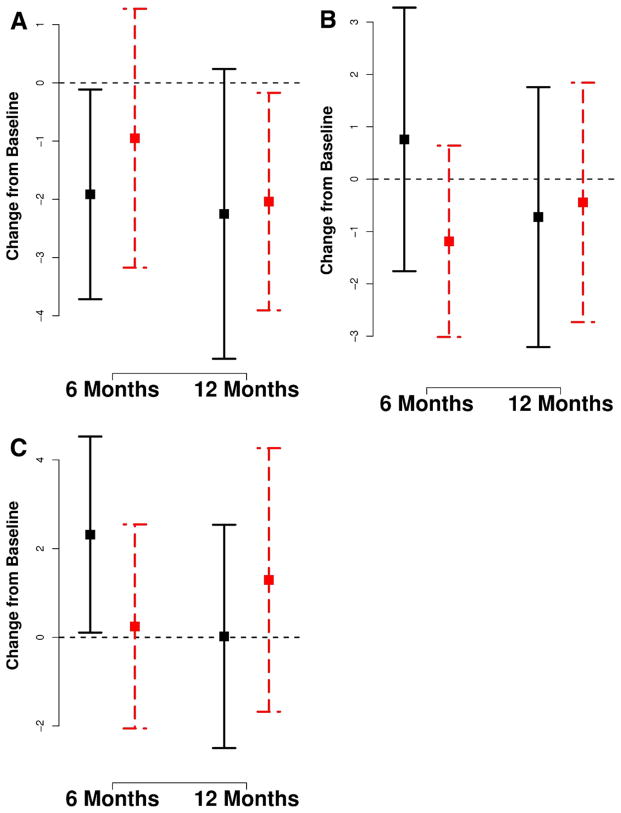
2. DID THE PERSONALIZED MOTIVATIONAL INTERVENTIONS DECREASE PARTICIPANTS’ ALCOHOL USE?
No significant between-group differences in alcohol use measures were found at any of the assessment time points (Fig 3). As can be seen from Figure 3A, the AUDIT scores declined significantly at 6 months in the control group (mean decrease = −1.9, P =.038). At 12 months, the intervention group (mean decrease = −2.03, P =.034) and the control group (mean decrease = −2.25, P =.076) shared a borderline, statistically significant decline. On the basis of the mean change scores at the 6-month or 12-month assessments, the intervention did not appear to have a significant effect on the number of days the subjects used alcohol (Fig 3B). The number of days subjects drank alcohol to intoxication (Fig 3C) increased significantly in the control group at 6 months (mean increase = 2.32, P = .041).
FIGURE 3.
Plots of change scores from baseline (horizontal dotted line) for alcohol use outcomes at follow-up assessments. Error bars represent ± 2 SE. Solid vertical lines for control group; dashed vertical lines are for personalized motivational intervention group. A, Alcohol Use Disorders Identification Test (AUDIT) score. B, Alcohol use. C, Alcohol to intoxication.
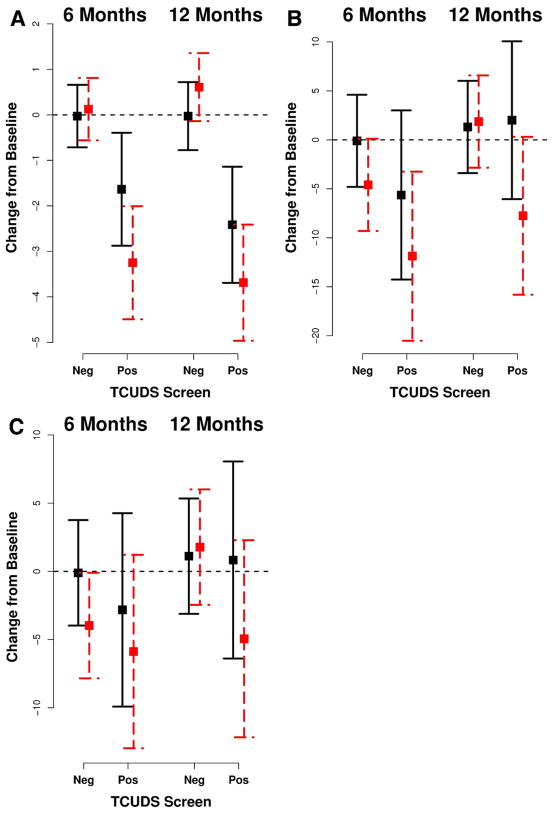
3. DID INITIAL DRUG USE SEVERITY MODERATE THE IMPACT OF THE PERSONALIZED INTERVENTION?
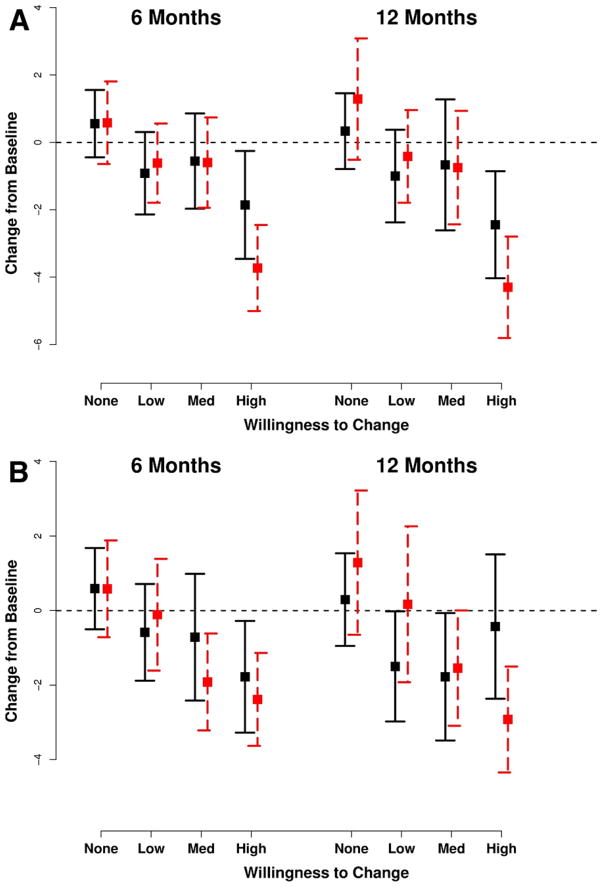
To better understand the effects of motivational intervention on illicit drug users, we dichotomized the drug use data into participants reporting drug use behaviors versus those evidencing drug dependency problems (composite TCUDS score ≥3). The differential changes in self-reported drug use patterns over time are shown in Figure 4. Decreases in TCUDS scores (Fig 4A) were more pronounced in subjects who were drug dependent at study intake (P < .0001 at 6 and 12 months), and there were borderline significant effects of the PMI on decreasing the TCUDS score when comparing patients in the PMI arm to control-arm patients (6-month P =.066, 12-month P =.068). Drug abusers experienced a differential effect on composite drug days (Fig 4B) at 12 months in the PMI arm only (P =.036). Changes in primary-drug use (Fig 4C) did not significantly differ between those positive and negative for drug abuse at baseline.
FIGURE 4.
Plots of change scores from baseline (horizontal dotted line) for drug use outcomes at follow-up assessments for different categories of baseline drug use. Error bars represent ± 2 SE. Solid vertical lines for control group; dashed vertical lines for personalized motivational intervention group. A, Texas Christian University Drug Screen—II (TCUDS) score. B, Drug-days. C, Primary drug.
4. DID INITIAL ALCOHOL USE SEVERITY MODERATE THE EFFECTS OF THE PERSONALIZED INTERVENTION?
At the 6- and 12-month follow-ups, subjects who screened positive for alcohol abuse at baseline (AUDIT ≥8), irrespective of their group assignment, had decreases in their AUDIT scores (Fig 5A) that were significantly different from subjects who did not screen positive for alcohol abuse (6-month P < .0001, 12-month P < .0005). However, subjects with abuse problems at intake did not differ significantly from those without abuse problems in their report of the number of days using alcohol (Fig 5B). At 12 months, subjects with alcohol-abuse problems used alcohol to intoxication more frequently, on average (Fig 5C), compared with subjects without abuse problems at baseline (P =.034).
FIGURE 5.
Plots of change scores from baseline (horizontal dotted line) for drug use outcomes at follow-up assessments for different categories of baseline alcohol use. Error bars represent ± 2 SE. Solid vertical lines for control group; dashed vertical lines for personalized motivational intervention group. A, Alcohol Use Disorders Identification Test (AUDIT) score. B, Alcohol use. C, Alcohol to intoxication.
5. DID A SUBJECT’S STAGE OF CHANGE AT BASELINE MODERATE THE EFFECTS OF THE PERSONALIZED INTERVENTION?
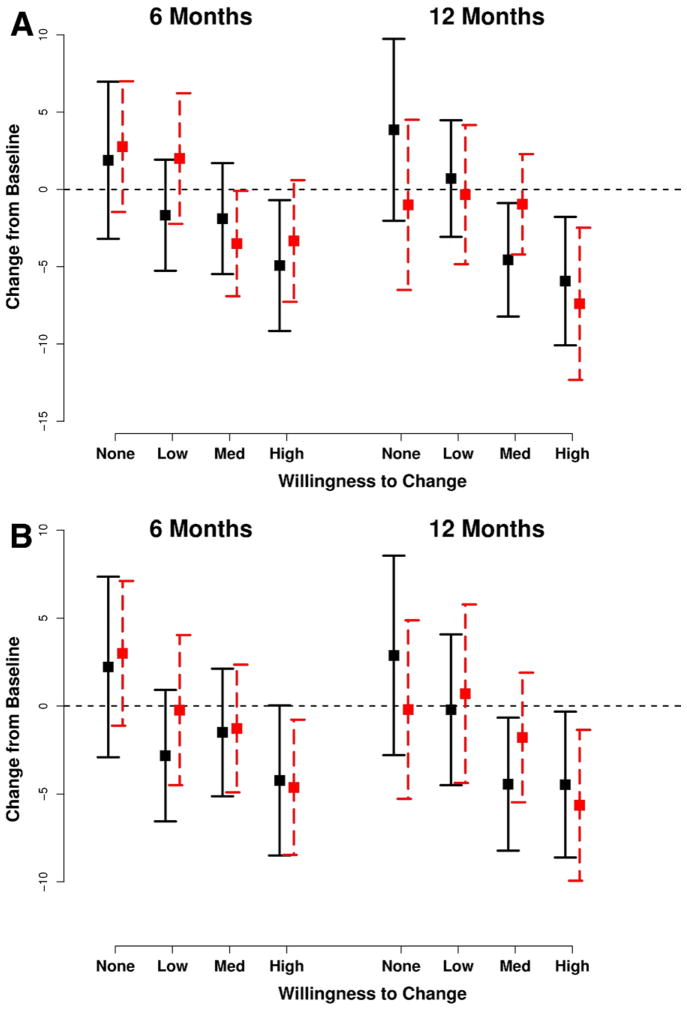
Figures 6 and 7 explore the relationship between the participants’ motivation to change their substance use behaviors and the actual changes observed at the follow-up assessments. Subjects were sorted into 4 groups based on their SOCRATES subscale score: no willingness to change, low willingness to change, medium willingness to change, or high willingness to change. The changes from baseline in the TCUDS and AUDIT scores for the intervention and control groups (Figs 6, 7) appeared to be based on their willingness to change score for the Recognition and Taking Steps Sub-scales of the Socrates. A higher recognition of the substance use problem and a greater willingness to take steps toward improvement were individually associated with larger decreases in TCUDS and AUDIT scores in both intervention and control groups (P values for all comparisons <.025). Contrasts indicated that PMI subjects with a high recognition of their drug problem had lower average TCUDS scores at both 6 and 12 months when compared with similar subjects in the control group (6-month P =.0714, 12-month P =.0941). A similar pattern was noted at 12 months in patients most willing to take steps to address their drug use problem (P =.0413). However, there were no significant differences in AUDIT scores between the intervention and control group, irrespective of the subject’s recognition of the alcohol problem or willingness to take steps to address it.
FIGURE 6.
Plots of change scores from baseline (horizontal dotted line) for drug use outcomes at follow-up assessments for subjects at different stages of change at baseline. Error bars represent ± 2 SE. Solid vertical lines for control group; dashed vertical lines for personalized motivational intervention group. A, Texas Christian University Drug Screen—II (TCUDS) by Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) D, Recognition. B, TCUDS by SOCRATES D, Taking Steps.
FIGURE 7.
Plots of change scores from baseline (horizontal dotted line) for alcohol use outcomes at follow-up assessments for subjects at different stages of change at baseline. Error bars represent ± 2 SE. Solid vertical lines for control group; dashed vertical lines for personalized motivational intervention group. A, Alcohol Use Disorders Identification Test (AUDIT) score by Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) D, Recognition. B, ADUIT by SOCRATES D, Taking Steps.
Discussion
MAIN FINDINGS
Our study results indicate that a culturally competent counseling intervention, integrated into the care of facial injury patients, has a differential impact on reducing substance use (illicit drugs/alcohol) behaviors. The 2-session intervention was significantly better than health information only in reducing illicit drug use behaviors; however, the magnitude and duration of the effect varied. The intervention’s effect on lowering illicit drug use was greatest at the 6-month follow-up but decayed by the 1-year follow-up assessment. The efficacy of the PMI was moderated by an individual’s initial drug use severity; individuals who were drug dependent at study intake appeared to be most responsive to the intervention. Similarly, individuals most aware of their drug problem and willing to change their behaviors showed larger declines in their drug use. Contrary to our expectation, the individualized intervention did not appear to influence alcohol use any more than the information-only control condition. We did not find any significant between-group effects for changes in the frequency and amount of alcohol used at both follow-up assessments. Unlike illicit drug use, the alcohol use scores did not differ significantly between the intervention and control groups, irrespective of an individuals’ recognition of the alcohol problem or willingness to take steps to address it.
Although both experimental and control groups showed an overall decrease in illicit drug use following the injury, the decline in drug use indexes (eg, TCUDS, days of drug use) tended to be greater for subjects in the experimental group over the short-term (6 month). The lack of a persistent protective effect over the long-term (12-month follow-up) suggests the need for repeat, booster interventions to have a sustained effect on drug use behaviors in trauma patients. The trajectory of substance use change was most prominent in subjects who evidenced drug dependency at study intake. In drug-dependent individuals, the PMI intervention produced greater decreases in drug use compared with similar control participants who received conventional care and health information only. We are unaware of similar studies of the effectiveness of motivational interventions in trauma populations with drug use histories. Nonetheless, our findings echo comparable trends reported in other settings that demonstrate an association between behavioral interventions and reductions in the use of marijuana, amphetamine-type stimulants, cocaine, and heroin.34–37
We included alcohol use for comparative purposes and to probe the intervention effects on stimulant use in general. The high-intensity, 2-session intervention notwithstanding, we did not find significant between-group differences in alcohol use measures at any of the assessment time points. Individuals who screened positive for alcohol abuse at admission tended to have significantly greater declines in alcohol use than those without alcohol abuse problems; however, this finding applied to both the experimental and the control condition. Our equivocal findings with a more intensive intervention differ from the significant effects reported by other groups16,19 for single-session, brief interventions targeting alcohol use among adult patients with facial injuries. If anything, we found greater declines in risky/harmful drinking (ie, AUDIT) in the control group at the 6-month assessment and no meaningful between-group differences at the 12-month follow-up. Irrespective of their assignment to the experimental or control condition, all subjects who screened positive for alcohol abuse at baseline (AUDIT ≥8) showed decreases in their AUDIT scores. Our observation echoes the findings of other investigators25,38 who attributed the decline in alcohol use following injury to regression-to-mean and Hawthorne-like effects.
Consistent with literature, we found a clear association between an individual’s readiness-to-change substance use behaviors and intervention outcome (ie, decreases in substance use). Components of readiness to change measured by the SOCRATES questionnaire (“Recognition” and “Taking Action”) appeared to operate similarly for both illicit drug as well as alcohol use. Individuals in the highest quartile for “problem awareness” and “willingness to take action” were much more likely to reduce their drug use behaviors following the PMI in our study, although the PMI impact was much less distinctive when alcohol use was concerned. Our findings add to the evidence linking problem recognition to PMI effect and underscore the importance of ascertaining a patient’s commitment to change and change-related actions and incorporating the information into individualized behavioral interventions.39 To the extent that disadvantaged racial/ethnic minorities with substance use problems comprise a significant subset of patients presenting with facial injury to our urban trauma centers, the integration of culturally tailored interventions supporting self-efficacy and action plans appears to be particularly relevant.
The general decrease in key measures of stimulant use (eg, TCUDS and AUDIT scores) in the months following injury provokes several interesting explanations. The decrease may be attributed to the injury itself and/or the experience of being in a trauma care setting. It may well be that the screening for substance use behaviors could itself have an intervention effect by making the patients more aware of their substance use and its negative consequences. Alternatively, the multiple contacts with research staff for symptom monitoring may also have an impact. Our findings are consistent with intervention studies conducted in acute care settings showing that patients tend to reduce their level of substance use after hospital visits regardless of whether they receive a brief intervention.40,41
METHODOLOGICAL FEATURES
Beyond the prospective, randomized, controlled, repeated-measures design, our study has several specific strengths. We were able to access a relatively large sample of vulnerable individuals with facial injuries, an underserved population of great interest because they constitute most patients seeking care at urban trauma centers in the United States but are disproportionately excluded from clinical studies for the very reasons (eg, racial/ethnic background, behavioral and substance use problems; noncompliance; and social, financial and residential instability) that render them vulnerable. There was careful development of a manual-guided motivational intervention, which was supported by ongoing training, supervision, and monitoring. The evaluation of the intervention took place within the context of regular care within a large, level-1 trauma center service. The intervention and control groups were well balanced on baseline characteristics, thus reducing the risk that differences in unadjusted mean outcomes could be attributed to baseline differences. We believe that these qualities serve to support the internal and external validity of our study results.
Our findings should be considered in the context of limitations of the study. First, our subjects agreed to participate in a study in which they could receive substance use counseling. This sample could have been predisposed to change, even though the change rates did vary. Second, given the specific nature of the patient sample and culturally congruent PMI, our findings might not generalize to other cultures, ethnic groups, or settings. Third, the high attrition rates in our cohort of vulnerable patients’ raise the possibility that those least likely to benefit from some positive effects of the PMI might have dropped out, leaving more patients in the sample available for analysis who would exhibit a favorable response to intervention. Fourth, the multiple contacts of the research staff with enrolled subjects raises the possibility of potential participant reactivity effects with the unintended consequence of diminishing group differences through a form of therapeutic input. Fifth, our investigation of potential intervention effects was complicated by signs of changes in the comparison group. Change scores within an intervention group can be significantly different from baseline, but if the control group also improves, it is harder for between-group comparisons to emerge as significant.
The heterogeneity across studies of motivational interventions makes it difficult to compare our findings with other studies or to draw simple conclusions about the effectiveness of motivational interventions in trauma-care settings. The umbrella of “motivational interventions” covers a multitude of approaches with considerable variation in contextual factors, such as the study setting, screening methods used, recruitment and eligibility criteria, nature and severity of injury, substance use patterns, content and duration of the motivational intervention, and outcome time points. Furthermore, even a range of intervention approaches that share some common components can have different effects across populations.
CLINICAL IMPLICATIONS
Our study shows that a culturally competent, motivational intervention targeting substance use behaviors can be successfully integrated into the care of vulnerable patients presenting with facial injury. The differential impact of the PMI in modulating substance use behaviors suggests that there might be subgroups of injured patients who would benefit most from such a personalized motivational intervention. The effect of the PMI was more pronounced for individuals with drug dependency problems who were aware of their problem and willing to change. Individuals with alcohol use behaviors or a lower drug problem severity did not appear to benefit as much from the interventions, especially if they evidenced little willingness to change. As our findings indicate, the effect of the PMI can attenuate over time; repeated “booster” sessions may be required to extend the PMI’s benefits.
Although advocated by the American College of Emergency Physicians and American College of Surgeons, the integration of motivational interventions into trauma care needs to be better articulated in terms of target population, content, and delivery. Busy trauma care settings facing ever-present financial constraints require pragmatic mechanisms for intervention delivery. Through a combination of standardized screening and assessment instruments, medical history, and self-reports administered within the context of facial injury management, underlying risky behaviors can be identified along with the patient’s interest in and readiness to change such behaviors. Previously, we highlighted the poor quality of substance use information collected by surgical residents providing care for facial-injury patients.42 Persuading surgeons to integrate screening and intervention strategies into their practice would require quick and easy methods for assessing substance use behaviors and identifying at-risk patients. Our study indicates that the TCUDS (for illicit drugs) and AUDIT (for alcohol use) are straightforward screening questionnaires that can be used to identify patients who are at risk for (or clearly have) problematic substance use behaviors. The SOCRATES can assist clinicians with necessary information about the patient’s motivation for change, thus allowing selective referrals for targeted interventions and an appropriate focusing of limited time and resources. Finally, the opportunity costs of a motivational intervention could be mitigated by adopting a shared-services model in which the interventions and counseling are provided by an interventionist who supports all trauma subspecialties.
Acknowledgments
The project described was supported by Grant No. R01 DA016850 from the National Institutes of Health/National Institute on Drug Abuse (Principal Investigator V. Shetty). We acknowledge the assistance of the project directors (Ms. Judith Resell and Ms. Rachel Fintzy), research staff, and the surgical residents who made the study possible. We dedicate this article to the memory of our collaborator Dr Douglas Longshore, who helped initiate the study and whose untimely death is a great loss to the field of substance abuse research.
References
- 1.Murphy DA, Shetty V, Resell J, et al. Substance use in vulnerable patients with orofacial injury: Prevalence, correlates, and unmet service needs. J Trauma. 2009;66:477. doi: 10.1097/TA.0b013e318164773a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Snape L. Angry young men, interpersonal violence, alcohol, and broken faces. N Z Med J. 2005;118:U1534. [PubMed] [Google Scholar]
- 3.Lee KH. Interpersonal violence and facial fractures. J Oral Maxillofac Surg. 2009;67:1878. doi: 10.1016/j.joms.2009.04.117. [DOI] [PubMed] [Google Scholar]
- 4.Scherer M, Sullivan WG, Smith DJ, et al. An analysis of 1,423 facial fractures in 788 patients at an urban trauma center. J Trauma. 1989;29:388. doi: 10.1097/00005373-198903000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Ogundare BO, Bonnick A, Bayley N. Pattern of mandibular fractures in an urban major trauma center. J Oral Maxillofac Surg. 2003;61:713. doi: 10.1053/joms.2003.50118. [DOI] [PubMed] [Google Scholar]
- 6.Lee K. Trend of alcohol involvement in maxillofacial trauma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:e9. doi: 10.1016/j.tripleo.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 7.Charbonney E, McFarlan A, Haas B, et al. Alcohol, drugs and trauma: Consequences, screening and intervention in 2009. Trauma. 2010;12:5. [Google Scholar]
- 8.Black E, et al. The relationship of substance abuse to orofacial injuries in an inner city population. Int J Oral Biol. 1998;23:47. [Google Scholar]
- 9.Madan AK, Yu K, Beech DJ. Alcohol and drug use in victims of life-threatening trauma. J Trauma. 1999;47:568. doi: 10.1097/00005373-199909000-00026. [DOI] [PubMed] [Google Scholar]
- 10.Rivara FP, Koepsell TD, Jurkovich GJ, et al. The effects of alcohol abuse on readmission for trauma. JAMA. 1993;270:1962. [PubMed] [Google Scholar]
- 11.Laski R, Ziccardi VB, Broder HL, et al. Facial trauma: A recurrent disease? The potential role of disease prevention. J Oral Maxillofac Surg. 2004;62:685. doi: 10.1016/j.joms.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 12.Sims DW, Bivins BA, Obeid FN, et al. Urban trauma: A chronic recurrent disease. J Trauma. 1989;29:940. discussion: 946. [PubMed] [Google Scholar]
- 13.Gentilello LM. Alcohol and injury: American College of Surgeons Committee on trauma requirements for trauma center intervention. J Trauma. 2007;62:S44. doi: 10.1097/TA.0b013e3180654678. [DOI] [PubMed] [Google Scholar]
- 14.Longabaugh R, Minugh PA, Nirenberg TD, et al. Injury as a motivator to reduce drinking. Acad Emerg Med. 1995;2:817. doi: 10.1111/j.1553-2712.1995.tb03278.x. [DOI] [PubMed] [Google Scholar]
- 15.Gentilello LM, et al. Detection of acute alcohol intoxication and chronic alcohol dependence by trauma center staff. J Trauma. 1999;47:1131. doi: 10.1097/00005373-199912000-00027. discussion: 1135. [DOI] [PubMed] [Google Scholar]
- 16.Smith AJ, Hodgson RJ, Bridgeman K, et al. A randomized controlled trial of a brief intervention after alcohol-related facial injury. Addiction. 2003;98:43. doi: 10.1046/j.1360-0443.2003.00251.x. [DOI] [PubMed] [Google Scholar]
- 17.Bernstein E, Edwards E, Dorfman D, et al. Screening and brief intervention to reduce marijuana use among youth and young adults in a pediatric emergency department. Acad Emerg Med. 2009;16:1174. doi: 10.1111/j.1553-2712.2009.00490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gentilello LM, Rivara FP, Donovan DM, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surg. 1999;230:473. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goodall C, Ayoub AF, Crawford A, et al. Nurse-delivered brief interventions for hazardous drinkers with alcohol-related facial trauma: A prospective randomised controlled trial. Br J Oral Maxillofac Surg. 2008;46:96. doi: 10.1016/j.bjoms.2007.11.014. [DOI] [PubMed] [Google Scholar]
- 20.Marsden J, Stillwell G, Barlow H, et al. An evaluation of a brief motivational intervention among young ecstasy and cocaine users: No effect on substance and alcohol use outcomes. Addiction. 2006;101:1014. doi: 10.1111/j.1360-0443.2006.01290.x. [DOI] [PubMed] [Google Scholar]
- 21.Mello MJ, Longabaugh R, Baird J, et al. DIAL: A telephone brief intervention for high-risk alcohol use with injured emergency department patients. Ann Emerg Med. 2008;51:755. doi: 10.1016/j.annemergmed.2007.11.034. [DOI] [PubMed] [Google Scholar]
- 22.Oakey F, Ayoub AF, Goodall CA, et al. Delivery of a brief motivational intervention to patients with alcohol-related facial injuries: Role for a specialist nurse. Br J Oral Maxillofac Surg. 2008;46:102. doi: 10.1016/j.bjoms.2007.11.013. [DOI] [PubMed] [Google Scholar]
- 23.Dunn C, Ostafin B. Brief interventions for hospitalized trauma patients. J Trauma Inj Infect Crit Care. 2005;59:S88. doi: 10.1097/01.ta.0000174682.13138.a3. [DOI] [PubMed] [Google Scholar]
- 24.Stern SA, Meredith LS, Gholson J, et al. Project CHAT: A brief motivational substance abuse intervention for teens in primary care. J Subst Abus Treat. 2007;32:153. doi: 10.1016/j.jsat.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 25.Nilsen P, et al. A systematic review of emergency care brief alcohol interventions for injury patients. J Subst Abus Treat. 2008;35:184. doi: 10.1016/j.jsat.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 26.Whitlock EP, Polen MR, Green CA, et al. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: A summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140:557. doi: 10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]
- 27.Soderstrom CA, et al. A controlled trial of brief intervention versus brief advice for at-risk drinking trauma center patients. J Trauma. 2007;62:1102. doi: 10.1097/TA.0b013e31804bdb26. discussion: 1111. [DOI] [PubMed] [Google Scholar]
- 28.Miller W. Treatment Improvement Protocol series 35. Bethesda, MD: National Center for Biotechnology Information, U.S. National Library of Medicine; 1995. Enhancing motivation for change in substance abuse treatment. Available at: http://www.ncbi.nlm.nih.gov/books/NBK14856. [Google Scholar]
- 29.Longshore D, Grills C, Annon K. Effects of a culturally congruent intervention on cognitive factors related to drug-use recovery. Subst Use Misuse. 1999;34:1223. doi: 10.3109/10826089909039406. [DOI] [PubMed] [Google Scholar]
- 30.Peters RH, et al. Effectiveness of screening instruments in detecting substance use disorders among prisoners. J Subst Abus Treat. 2000;18:349. doi: 10.1016/s0740-5472(99)00081-1. [DOI] [PubMed] [Google Scholar]
- 31.Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test (AUDIT): A review of recent research. Alcohol Clin Exp Res. 2002;26:272. [PubMed] [Google Scholar]
- 32.Miller W, Tonigan J. Assessing drinkers’ motivations for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) Psychol Add Behav. 1996;10:81. [Google Scholar]
- 33.Carey KB, Maisto SA, Carey MP, et al. Measuring readiness-to-change substance misuse among psychiatric outpatients: I. Reliability and validity of self-report measures. J Stud Alcohol. 2001;62:79. doi: 10.15288/jsa.2001.62.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bernstein J, Bernstein E, Tassiopoulos K, et al. Brief motivational intervention at a clinic visit reduces cocaine and heroin use. Drug Alcohol Depend. 2005;77:49. doi: 10.1016/j.drugalcdep.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 35.Copeland J, Swift W, Roffman R, et al. A randomized controlled trial of brief cognitive-behavioral interventions for cannabis use disorder. J Subst Abus Treat. 2001;21:55. doi: 10.1016/s0740-5472(01)00179-9. discussion: 65. [DOI] [PubMed] [Google Scholar]
- 36.McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: Results from a multi-site cluster randomized trial. Addiction. 2004;99:39. doi: 10.1111/j.1360-0443.2004.00564.x. [DOI] [PubMed] [Google Scholar]
- 37.The effectiveness of a brief intervention for illicit drugs linked to the alcohol, smoking, and substance involvement screening test (ASSIST) in primary health care settings: A technical report of Phase III findings of the WHO ASSIST Randomized control trial. World Health Organization. Available at: http://www.who.int/substance_abuse/activities/assist_technicalreport_phase3_final.pdf.
- 38.Daeppen J, Gaume J, Bady P, et al. Brief alcohol intervention and alcohol assessment do not influence alcohol use in injured patients treated in the emergency department: A randomized controlled clinical trial. Addiction. 2007;102:1224. doi: 10.1111/j.1360-0443.2007.01869.x. [DOI] [PubMed] [Google Scholar]
- 39.Amrhein PC, Miller WR, Yahne CE, et al. Client commitment language during motivational interviewing predicts drug use outcomes. J Consult Clin Psychol. 2003;71:862. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- 40.Forsberg L, Ekman S, Halldin J, et al. Brief interventions for risk consumption of alcohol at an emergency surgical ward. Addict Behav. 2000;25:471. doi: 10.1016/s0306-4603(99)00005-2. [DOI] [PubMed] [Google Scholar]
- 41.Monti PM, Colby SM, Barnett NP, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol. 1999;67:989. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- 42.Shetty V, Murphy DA, Zigler C, et al. Accuracy of data collected by surgical residents. J Oral Maxillofac Surg. 2008;66:1335. doi: 10.1016/j.joms.2008.01.065. [DOI] [PMC free article] [PubMed] [Google Scholar]