Abstract
Research has shown that black dialysis patients in the United States are significantly less likely than their white peers to be evaluated and listed for a kidney transplant. Extrapolating from social network theory, I hypothesize that a lack of access to social contacts with information about kidney transplantation may hinder information transaction regarding the benefits of, and pathway to, transplantation. In 2007–2008, the following research questions were addressed in an investigation in Chicago, USA: (1) What is the role of social networks in providing information about kidney transplantation to black hemodialysis patients? (2) What is the relationship between social networks and a patient’s likelihood of being seen at a kidney transplant center? From a stratified sample of dialysis units in the area, a purposive sample of 228 black patients were surveyed while they received treatment about their social networks and kidney transplant status. It was found that the odds of black hemodialysis patients being seen at a kidney transplant center increase with income, and patients who have people in their social network with information about kidney transplant were significantly more likely to be seen at a kidney transplant center. Specifically, black dialysis patients who get informational social support from their dialysis team and social networks were significantly more likely to be seen at kidney transplant centers. I conclude that considering black dialysis patients’ social milieu can be complementary to the existing research regarding this public health crisis.
Keywords: Kidney, transplant, social network, disparity, parity, kidney disease, USA, race, ethnicity
Introduction
In the United States, black End Stage Renal Disease (ESRD) patients are less likely to get a kidney transplant than white patients (Alexander & Sehgal, 2002). ESRD is a chronic illness that requires renal replacement therapy with dialysis or kidney transplantation, and is a significant public health issue in the United States. The total U.S. spending for ESRD care in 2007 was $32 billion and expenditures are expected to double by 2012 (U.S. Renal Data System, 2007). Compared to dialysis, kidney transplantation provides patients with better quality of life and improved health outcomes (Becker, et al., 2000; Dew, Goycoolea, Switzer, & Allen, 2000). Kidney transplantation is also the most cost-effective treatment for ESRD (Eggers, 1992). Despite a Healthy People 2010 target of 30% of ESRD patients receiving a kidney transplant within 3 years of diagnosis, only 10% of black patients achieved this goal (compared to 24% of white patients) (U.S. Department of Health and Human Services, 2000). Explanations for underutilization of transplantation as a treatment modality for black ESRD patients have focused primarily on socioeconomic, medical, and patient-preference factors. The contribution of the present study is to investigate previously unconsidered social network factors that might influence the racial composition of kidney transplant-patient populations in the United States (Arthur, 2002).
Social networks of black ESRD patients may not provide information about the benefits of and processes related to kidney transplantation, and this may partially explain why fewer black ESRD patients are listed on kidney transplant waiting lists. Social networks vary by race and socioeconomic status. In America, black individuals are more likely than white people to have dense, homophilous social networks and obtain social support from strong ties who have less access to novel information (Lee & Campbell, 1999; Malson, 1982; Taylor & Chatters, 1986).
In addition to differences in the composition of their social networks, black Americans are less likely to have access to information about kidney transplantation than are white Americans. Studies suggest that black Americans have less awareness and knowledge about kidney disease, transplantation, and the benefits and success rate of kidney transplantation (Callenderm, Bey, Miles, & Yeager, 1995; Ozminkowski, White, Hassol, & Murphy, 1997; Waterman et al., 2008). Likewise they are less likely than white people to know others who had signed organ donation cards or someone who had donated an organ for transplantation (Yuen et al., 1998). It is proposed that social-network theory and related concepts can be used to explain a portion of the racially disparate pursuit of kidney transplantation. White ESRD patients may have more heterogeneous social contacts than black ESRD patients, and these social contacts may serve as a bridge to enhanced information about transplantation and result in better patient outcomes (i.e., white patients pursue and ultimately receive kidney transplants more often than black patients). White patients may learn more about the benefits of, and process involved in, kidney transplantation from information received from their social networks (because their networks are more diverse and more knowledgeable about kidney transplantation), which makes them more likely to pursue a transplant.
Although this theoretical approach to explain health behaviors has not been previously used with kidney disease populations before, novel information transmitted through weak social-network ties has been systematically linked to: social mobility leading to employment (Granovetter, 1983, 1994); enhanced likelihood of an individual pursuing psychiatric treatment (Horwitz, 1977); information sharing about legislative changes (Roch, Scholz, & McGraw, 2000); information sharing about political knowledge and ideas (Huckfeldt, Beck, Dalton, and Levine, 1995; Huckfeldt & Sprague, 1987); and information sharing about where to find abortions before they were legalized (Lee, 1969).
I hypothesize that success in pursuing a kidney transplant may be influenced in part by the information that black ESRD patients receive from their social networks. The information gained from these contacts may inform patients about unfamiliar options like transplant. In addition, these social contacts may motivate, encourage, and facilitate a patient along the pathway to transplant. Social networks of black ESRD patients may provide less information about the benefits of, and processes related to, kidney transplantation. This approach may in part explain why fewer black ESRD patients are listed on kidney transplant waiting lists in the United States.
Method
Sample
The sample was 228 black, English-speaking hemodialysis patients between the ages of 18 and 65 years who have never received a kidney transplant and who receive hemodialysis at one of five Chicago-area dialysis units (all owned by the same company). In preparation for this study, de-identified information about the race and insurance status of patients in each dialysis unit in the U. S. Midwest was acquired from the U.S. Renal Data System 2004 Annual Data Report (U.S. Renal Data System, 2004). Using this data, hemodialysis units with the highest case mix of race and income (using insurance status as a proxy for income) were selected for the study. As the network effects of race and income may be endogenous, it was important to survey patients with income variability for this study. Due to the potential organizational differences between each dialysis unit (i.e. different policies and procedures may be responsible for different levels of patient education and assistance with kidney transplantation), the study was conducted only in dialysis units owned by the same company. Because of this, and the rarity of black dialysis patients with higher income in the Midwest U.S. area, this study purposively included all of the black patients age 18–65 at the units selected, rather than randomly sampling the patient population and rather than including white patients in the study. At each unit, 100% of the eligible patients were surveyed, unless they failed a cognitive screener (n= 7). Patients in the sample self identified as black ethnicity. Institutional-review-board (IRB) approval of the study was provided by the University of Chicago, and surveys were conducted by the author while the patients received hemodialysis. Patients provided verbal consent to the survey, so that no identifying information about the patient was recorded.
Measures and Analysis Strategy
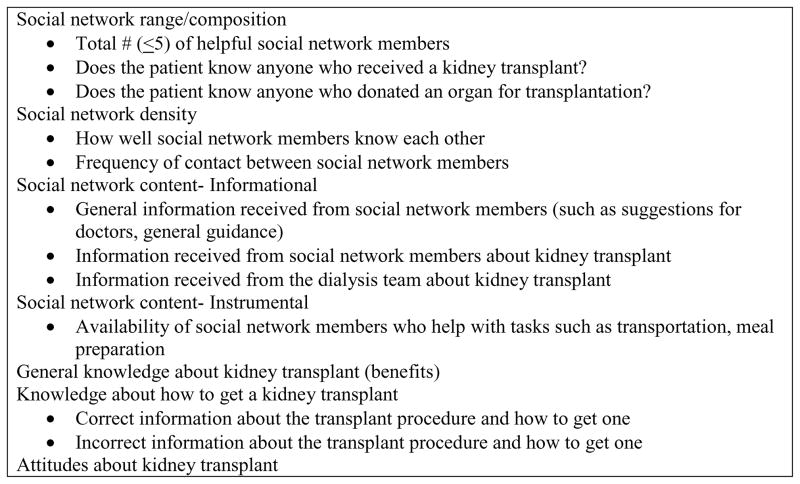
As this was a novel study, and there is no data base that captures social network information about kidney patients, the research instrument had to be created specifically for the survey. Figure 1 outlines the independent variables used in this analysis. The social network questions are from the National Health and Social Life Survey (Laumann, 1995), which has been administered to thousands of Chicago area individuals. Using these questions, patients identified a significant other, and generated up to 5 social network members that were helpful to them, and then answered questions about those social network members. The kidney transplant attitude questions had been previously used with dialysis populations (see Ayanian, J. Z., Cleary, P. D., Weissman, J. S., & Epstein, A. M., 1999), and the instrument as a whole was reviewed by kidney transplant disparity and social network experts (Alexander & Sehgal, 1998, 2001, 2002; Youm & Laumann, 2002) for face validity.
Figure 1.
Independent Variables
Using SPSS version 15, data were analyzed at the univariate, bivariate and multivariate levels. Correlations between variables based on the relevant research questions were analyzed using either Spearman’s rank correlation coefficients or a Pearson chi-square test. Logistic regression analyses were conducted to determine if social network factors predict that a patient will be seen at a kidney transplant center, taking into account control variables of income, marital status, gender, age, and length of time on dialysis. Logistic regression analyses were also conducted to determine if social network factors predict whether or not a patient will have the correct information about how to get a kidney transplant based on consideration of the number of social network members identified, closeness of social network, frequency of contact of social network measures, and informational social support about kidney transplantation from the dialysis team and other social network members, (taking into account control variables of income, marital status, gender, and age). Only the final regression models, with the best goodness of fit and predicted probability, are discussed in this paper.
Results
Table 1 summarizes the frequencies of respondent attributes. Ninety-four percent of patients surveyed were interested in a kidney transplant, and 98% had insurance coverage that would pay for a kidney transplant, but only 9% were active on a kidney transplant waiting list. Despite including all eligible patients in the study, the final sample ended up being exactly 50% male and 50% female.
Table 1.
Frequencies for Study Variables
| n | % | |
|---|---|---|
| Sex (N = 228) | ||
| Male | 114 | 50.0 |
| Female | 114 | 50.0 |
| Marital status (N = 228) | ||
| Married | 79 | 34.6 |
| Separated | 30 | 13.2 |
| Divorced | 38 | 16.7 |
| Never been married | 73 | 32.0 |
| Education (N = 228) | ||
| Some high school or less | 76 | 33.3 |
| Graduated high school/GED | 138 | 60.5 |
| Graduated college | 14 | 6.1 |
| Income (N = 223) | ||
| < $15,000 | 91 | 40.8 |
| $15,000 – $34,999 | 39 | 17.5 |
| $35,000 – $49,999 | 45 | 20.2 |
| $50,000 – $99,999 | 21 | 9.4 |
| > $100,000 | 27 | 12.1 |
| Primary insurance (N = 228) | ||
| Medicaid | 92 | 40.4 |
| Medicare | 119 | 52.2 |
| Private insurance | 12 | 5.3 |
| None | 3 | 1.3 |
| Seen at transplant center (N = 228) | ||
| Yes | 83 | 36.4 |
| No | 145 | 63.6 |
| On transplant list (N = 228) | ||
| Yes | 20 | 8.8 |
| No | 208 | 91.2 |
| Do you want to get a kidney transplant? (N = 228) | ||
| Yes | 214 | 93.9 |
| No | 14 | 6.1 |
| Correct information about how to get a transplant (N = 228) | ||
| Yes | 83 | 36.4 |
| No | 145 | 63.6 |
| Know anyone who got a transplant? (N = 228) | ||
| Yes | 87 | 38.2 |
| No | 141 | 61.8 |
| Know anyone who donated an organ? (N = 228) | ||
| Yes | 13 | 5.7 |
| No | 215 | 94.3 |
| Good attitude towards getting a transplant? (N = 192) | ||
| Yes | 182 | 94.8 |
| No | 10 | 5.2 |
Social network variables
All but four respondents were able to identify a social network member who could provide general help and support, and the mean number of social network members identified by the total sample of respondents is 3.8 (SD = 1.4, see Table 2). Patients had social networks that were very close, with a mean score of 1.1 (SD = 0.4, see Table 2), with “1” indicating that the social network members know each other very well, “2” indicating that they know each other somewhat well, and “3” indicating that the social network members do not know each other well. The social network members were in frequent contact with one another, with contact averaging between a few times a week to once a week (mean = 2.2, SD = 1). Respondents identified more social network members who could provide instrumental social support (i.e. babysitting, transportation; M = 3.6, SD = 1.2) than who provided informational social support (M = 1.4, SD = 1.6).
Table 2.
Descriptive Statistics for Continuously Measured Variables
| n | Mean | Standard Deviation | Range | |
|---|---|---|---|---|
| Age | 228 | 44.8 | 13.1 | 20 – 64 |
| # of years on dialysis | 228 | 3.9 | 3.1 | 0.5 – 15 |
| Information from teama | 225 | 3.3 | 3.2 | 0 – 9 |
| Instrumental social supportb | 228 | 3.6 | 1.2 | 0 – 5 |
| Informational social supportc | 228 | 1.4 | 1.6 | 0 – 5 |
| Total number of social network membersd | 228 | 3.8 | 1.4 | 0 – 6 |
| How well members know each other e | 228 | 1.1 | 0.4 | 0 – 5 |
| Frequency of contact with membersf | 228 | 2.2 | 1.0 | 0 – 6 |
Range from 0 (=no information given) to 9 (=most information given)
Range from 0 (=no social members provide instrumental support) to 5 (=5 social network members provide instrumental support)
Range from 0 (=no social members provide instrumental support) to 5 (=5 social network members provide instrumental support)
Range from 1 network member to 6 network members (including significant other)
Range from 1 (=very well) to 3 (=not too well)
Range from 1 (=daily) to 6 (=less than once a month)
Information and attitude about kidney transplant
Just over one-third of the sample (n=83, 36%) had correct information about how to get a kidney transplant. The majority of patients (64%) either did not know how to get a kidney transplant or had incorrect information about how to get a kidney transplant. The majority of patients surveyed indicated that they wanted to get a kidney transplant (n = 214, 94%). Of the 14 patients who did not want a kidney transplant, three (21%) were not interested because of age, and eleven (79%) were not interested because they were satisfied with dialysis as a treatment modality.
With regard to the bivariate analysis of the first research question, “What is the role of social networks in providing information about kidney transplantation to black dialysis patients?” a correlation was found between having a social network that includes content about kidney transplants (individuals who provide informational social support or who are knowledgeable about kidney transplantation) and having the correct information about how to get a kidney transplant. Correct information about how to get a kidney transplant was significantly and strongly correlated with informational social support from the dialysis team (ρ = .68, p < .001), informational social support about kidney transplant from others in the social network (ρ = .46, p < .001), knowing someone who received a kidney transplant (ρ = .70, p < .001), and knowing someone who donated a kidney (ρ = .25, p < .001).
Looking further at the first research question, the multivariate regression model in Table 3 was able to correctly predict 91% of those patients who do not have the correct information about how to get a kidney transplant and 80% of those patients who do have the correct information about how to get a kidney transplant, for an overall success rate of 87%. This model implies that correct information about a kidney transplant can be differentiated on the basis of considering social network informational attributes. In this model, total number of social network members, higher income, and informational social support from the dialysis team have a significant effect (p<.05).
Table 3.
Summary of adjusted logistic regression analysis for predicting whether a patient has correct information about how to get a kidney transplant
| Predictors | B | SE B | Significance | Odds Ratio | 95.0% C.I. | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Total # of network members | −.41 | .17 | .02* | .67 | .47 | .94 |
| Close social network | .70 | .69 | .31 | 2.02 | .52 | 7.81 |
| Social network members in frequent contact | .11 | .21 | .60 | 1.12 | .73 | 1.71 |
| Female | .55 | .43 | .21 | 1.76 | .74 | 4.08 |
| ≥ 55 years old | .00 | .01 | .83 | 1.00 | .97 | 1.04 |
| Married | .73 | .49 | .14 | 2.07 | .78 | 5.45 |
| Annual income ≥ $50,000 | .31 | .12 | .01* | 1.36 | 1.07 | 1.74 |
| Patient received informational social support from social network | .19 | .16 | .25 | 1.21 | .87 | 1.69 |
| Patient received informational social support from dialysis team | .57 | .09 | .00*** | 1.76 | 1.47 | 2.10 |
Note: the constant for the regression equation = 4.142
p<.05.
p<.01.
p<.001
With regard to the second research question, “What is the relationship between social networks and a patient’s likelihood of being seen at a kidney transplant center?” correct information about kidney transplantation was significantly and strongly correlated with being seen at kidney transplant center (ρ = .28, p < .001), and with wanting a transplant (ρ = .19, p < .01), indicating that patients who had more information from their social network about how to get a kidney transplant were more likely to desire a transplant, be seen at a transplant center, and be placed on a kidney transplant list (see Table 4). This regression model indicates that the odds of being seen at a kidney transplant center increase by a factor of 1.763 for every unit increase in informational social support from the dialysis team about kidney transplant when the other two variables in the equation are held constant. Likewise, the regression model indicates that the odds of being seen at a kidney transplant center increase by a factor of 1.6 for every unit increase in informational social support from network ties, holding dialysis team social support and income constant. Finally, the model suggests that the odds of being seen at a kidney transplant center increase by a factor of 1.4 for every unit increase in income, or by 40% for every additional point in income, holding informational social support from the team and networks constant.
Table 4.
Summary of adjusted logistic regression analysis for predicting whether a patient will be seen at a kidney transplant center
| Predictors | B | SE B | Significance | Odds Ratio | 95.0% C.I. | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Informational social support from social network | .57 | .09 | .00*** | 1.76 | 1.48 | 2.09 |
| Informational social support from dialysis team | .49 | .17 | .00** | 1.63 | 1.18 | 2.25 |
| Incomea | .32 | .12 | .01** | 1.38 | 1.09 | 1.76 |
Note: the constant for the regression equation = 4.283
p<.05.
p<.01.
p<.001
Refers to a 1-unit change in annual income between < $15,000, $15,000 – $34,999, $35,000 – $49,999, $50,000 – $99,999, > $100,000
Discussion
This study is a first step in exploring the relationship between social network information transaction and kidney transplant parity, and expanding the social network literature in the area of informational social support as it relates to medical behaviors. The results of the present study suggest that social network attributes are associated with information about how to get a kidney transplant as well as success in being seen at a kidney transplant center. These associations, however, relate primarily to the content of the social networks, rather than to their structure. This study suggests that it is not the density or strength of a social network that matters when looking at kidney transplant success, but the fact that the social network has members with information about kidney transplant in it. That is to say, when thinking about why black dialysis patients get stuck on the pathway to kidney transplant, it is alright for a patient to have a small, or close, social network, as long as someone in this social network can provide the patient with information about kidney transplant. Seminal social network research by Granovetter (1983, 1994) and others related to employment opportunities may need further expansion as related to health behaviors to include attention to the content of informational social support in addition to structural social network attributes.
Indeed, this study found that the relationship between the total number of social network members and likelihood of being seen at a transplant center is inverse, with patients with smaller social networks being more likely to be seen at a kidney transplant center. These findings are novel both in the field of kidney disease, and in social network research, and merit further study.
The major limitations to this study are: non-random sampling of participants; using a Black-only sample; inability of the study to capture possible provider discrimination; reliance on a patient self-reported dependent variable; and cross-sectional design of the study. For this particular study, random sampling of both black and white dialysis patients was not possible because an analysis of the ethnic and income composition of all dialysis units in Illinois, Indiana, and Wisconsin indicated that there were no dialysis units that had both black and white patients, who were both lower and upper income. It was important for the integrity of this study that the fewest possible dialysis units be used to select respondents, as patients’ propensity to successfully navigate the transplant pathway may be due to organizational differences rather than social network attributes. Using only dialysis units with common management controlled for possible organizational factors, however precluded the use of randomized selection of the sample because of the smaller pool of dialysis patients to survey. This study was not able to rule out discriminatory practices by the medical team. Since some patients in this study were successful in being seen at a transplant center, and the patients in each unit had common physicians, nurses, and social workers, it unlikely that within this sample, the other patients’ lack of success is dependent on wholesale provider negligence or discrimination. Another limitation to this study is the fact that the dependent variable “seen at transplant center” is a self-reported variable that was not confirmed independently (because there were no patient identifiers documented). However, in the United States, at the time of this survey, there were no commonly used reports by dialysis units to capture this milestone. Future longitudinal research is needed to fully explore patients’ success in navigating pathways to kidney transplantation.
As affirmative action is a policy and practice solution to minority exclusion from social networks which can help them get jobs, targeted interventions with black dialysis patients may help black patients get transplants even if they do not have anyone in their social network who can help them with that process. These findings may also have relevance to improving the access of other disadvantaged patients to health care. As in kidney disease, health and health care disparities exist for every chronic illness (Smedley, Stith, & Nelson, 2002). Augmenting disadvantaged patients’ social networks with individuals who are knowledgeable about how to best access recommended health services may address disparities in illnesses beyond kidney disease. Interventions such as patient navigation (Freeman, 2006) that help disadvantaged patients navigate the barriers to seeking treatment for chronic illnesses such as cancer is one example of such an intervention, and may be a way to address other health care disparities through informational and instrumental social support. This study also has international implications for further research, as kidney transplant racial disparities exist in Canada (Yeates et al., 2004), Australia (Cass, Cunningham, Snelling, Wang, & Hoy, 2003), France, Spain, and the United Kingdom (Koizumi, 2010). Considering dialysis patients’ social milieu can be complementary to the existing research regarding kidney transplant disparity in the United States and beyond.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alexander G, Sehgal A. Variation in access to kidney transplantation across dialysis facilities: Using process of care measures for quality improvement. American Journal of Kidney Diseases. 2002;40(4):824–831. doi: 10.1053/ajkd.2002.35695. [DOI] [PubMed] [Google Scholar]
- Alexander G, Sehgal A. Why hemodialysis patients fail to complete the transplantation process. American Journal of Kidney Diseases. 2001;37(2):321–328. doi: 10.1053/ajkd.2001.21297. [DOI] [PubMed] [Google Scholar]
- Alexander G, Sehgal A. Barriers to cadaveric renal transplantation among blacks, women, and the poor. Journal of the American Medical Association. 1998;280:1148–1152. doi: 10.1001/jama.280.13.1148. [DOI] [PubMed] [Google Scholar]
- Arthur T. The role of social networks: A novel hypothesis to explain the phenomenon of racial disparity in kidney transplantation. American Journal of Kidney Diseases. 2002;40:678–681. doi: 10.1053/ajkd.2002.35672. [DOI] [PubMed] [Google Scholar]
- Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. The effect of patients’ preferences on racial differences in access to renal transplantation. New England Journal of Medicine. 1999;341:1661–1669. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- Becker BN, Becker YT, Pintar T, Collins BH, Pirsch JD, Friedman A, et al. Using renal transplantation to evaluate a simple approach for predicting the impact of End-Stage Renal Disease therapies on patient survival: Observed/expected life span. American Journal of Kidney Diseases. 2000;35:653. doi: 10.1016/s0272-6386(00)70012-6. [DOI] [PubMed] [Google Scholar]
- Callender CO, Bey AS, Miles PV, Yeager CL. A national minority organ/tissue transplant education program: The first step in the evolution of a national minority strategy and minority transplant equity in the USA. Transplantation Proceedings. 1995;27(1):1441–1443. [PubMed] [Google Scholar]
- Cass A, Cunningham J, Snelling P, Wang Z, Hoy W. Renal transplantation for indigenous Australians: Identifying the barriers to equitable access. Ethnicity & Health. 2003;8(2):111–119. doi: 10.1080/13557850303562. [DOI] [PubMed] [Google Scholar]
- Cohen SD, Sharma T, Acquaviva K, Peterson RA, Patel SS, Kimmel P. Social support and chronic kidney disease: An update. Advances in Chronic Kidney Disease. 2007;14(4):335–344. doi: 10.1053/j.ackd.2007.04.007. [DOI] [PubMed] [Google Scholar]
- Dew M, Goycoolea J, Switzer G, Allen A. Quality of life in organ transplantation: Effects on adult recipients. In: Trzepacz P, DiMartini A, editors. The transplant patient: Biological psychiatric and ethical issues in organ transplantation. Cambridge MA: Cambridge University; 2000. pp. 67–145. [Google Scholar]
- Eggers PW. Comparison of treatment costs between dialysis and transplantation. Seminars in Dialysis. 1992;12:284–289. [PubMed] [Google Scholar]
- Freeman HP. Patient navigation: A community based strategy to reduce cancer disparities. Journal of Urban Health. 2006;83(2):139–141. doi: 10.1007/s11524-006-9030-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furth S, Garg P, Neu A, Hwang W, Fivush B, Powe N. Racial differences in access to kidney transplant waiting list for children and adolescents with end-stage renal disease. Pediatrics. 2000;106:756–761. doi: 10.1542/peds.106.4.756. [DOI] [PubMed] [Google Scholar]
- Granovetter M. The strength of weak ties: A network theory revisited. Sociological Theory. 1983;1:201–233. [Google Scholar]
- Granovetter M. Afterward 1994: Reconsiderations and a new agenda. In: Granovetter M, editor. Getting a Job: A Study of Contacts and Careers. 2. Chicago: University of Chicago; 1994. pp. 139–182. Rev. [Google Scholar]
- Horwitz A. Social networks and pathways to psychiatric treatment. Social Forces. 1977;56(1):86–105. [Google Scholar]
- Huckfeldt R, Beck P, Dalton R, Levine J. Political environments, cohesive social groups, and the communication of public opinion. American Journal of Political Science. 1995;39:1025–1054. [Google Scholar]
- Huckfeldt R, Sprague J. Networks in context: The social flow of political information. American Political Science Review. 1987;81:1197–1216. [Google Scholar]
- Kasiske BL, London W, Ellison MD. Race and socioeconomic factors influencing early placement on the kidney transplant waiting list. Journal of the American Society of Nephrology. 1998;9:2142–2147. doi: 10.1681/ASN.V9112142. [DOI] [PubMed] [Google Scholar]
- Koizumi N. Geographical disparity in access to organ transplant in the United States and other western countries: A prolegomenon to a solution. World Medical & Health Policy. 2010;2(2):111–131. [Google Scholar]
- Laumann EO. National Health and Social Life Survey. Chicago: University of Chicago and National Opinion Research Center; 1995. [Google Scholar]
- Lee N. The search for an abortionist. Chicago: University of Chicago; 1969. [Google Scholar]
- Lee BA, Campbell KE. Neighbor networks of black and white americans. In: Wellman B, editor. Networks in the global village. Boulder, CO: Westview Press; 1999. pp. 119–146. [Google Scholar]
- Malson M. The social-support systems of black families. Marriage and Family Review. 1982;5(4):37–57. [Google Scholar]
- Ozminkowski R, White A, Hassol A, Murphy M. Minimizing racial disparity regarding receipt of a cadaver kidney transplant. American Journal of Kidney Disease. 1997;30:749–759. doi: 10.1016/s0272-6386(97)90078-0. [DOI] [PubMed] [Google Scholar]
- Roch C, Scholz J, McGraw K. Social networks and citizen response to legal change. American Journal of Political Science. 2000;44:777–791. [Google Scholar]
- Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, D.C.: National Academies Press; 2002. [PubMed] [Google Scholar]
- Taylor R, Chatters L. Patterns of informal support to elderly black adults: Family friends and church members. Social Work. 1986;31:432–436. [Google Scholar]
- Yeates KE, Schaubel DE, Cass A, Sequist TD, Ayanian JZ. Access to renal transplantation for minority patients with ESRD in Canada. American Journal of Kidney Diseases. 2004;44:324–331. doi: 10.1053/j.ajkd.2004.08.031. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People 2010. Washington, DC: U.S. Government Printing; 2000. [Google Scholar]
- U.S. Renal Data System. Annual Data Report. Bethesda, MD: National Institutes of Health & National Institute of Diabetes and Digestive and Kidney Diseases; 2004. [Google Scholar]
- U.S. Renal Data System. Annual Data Report. Bethesda, MD: National Institutes of Health & National Institute of Diabetes and Digestive and Kidney Diseases; 2007. [Google Scholar]
- Waterman AD, Browne T, Waterman BN, Gladstone EH, Hostetter T. Attitudes and behaviors of African Americans regarding early detection of kidney disease. American Journal of Kidney Diseases. 2008;51(4):554–562. doi: 10.1053/j.ajkd.2007.12.020. [DOI] [PubMed] [Google Scholar]
- Youm Y, Laumann E. Social network effects on the transmission of sexually transmitted diseases. Sexually Transmitted Diseases. 2002;29(11):689–697. doi: 10.1097/00007435-200211000-00012. [DOI] [PubMed] [Google Scholar]
- Yuen CC, Burton W, Chiraseveenuprapund P, Elmore E, Wong S, Ozuah P, et al. Attitudes and beliefs about organ donation among different racial groups. Journal of the National Medical Association. 1998;90(1):13–20. [PMC free article] [PubMed] [Google Scholar]