Abstract
AIM: To investigate gastric cancer screening and preventive behaviors among the relatives of patients with gastric cancer [i.e., gastric cancer relatives (GCRs)].
METHODS: We examined the Korean National Health and Nutrition Examination Survey 2005 (KNHANES III) database and compared the gastric cancer screening and preventive behaviors of GCRs (n = 261) with those of non-GCRs (n = 454) and controls without a family history of cancer (n = 2842).
RESULTS: The GCRs were more likely to undergo gastric cancer screening compared with the control group (39.2% vs 32.3%, adjusted odds ratio: 1.43, CI: 1.05-1.95), although the absolute screening rate was low. Dietary patterns and smoking rates did not differ significantly between the groups, and a high proportion of GCRs reported inappropriate dietary habits (i.e., approximately 95% consumed excessive sodium, 30% were deficient in vitamin C, and 85% were deficient in dietary fiber).
CONCLUSION: The gastric cancer screening and preventive behaviors of GCRs have yet to be improved. To increase awareness among GCRs, systematic family education programs should be implemented.
Keywords: Family history of cancer, Cancer relatives, Gastric cancer screening, Preventive behaviors, Cancer prevention
INTRODUCTION
Gastric cancer is the most common cancer, and the third leading cause of death from cancer, in Korea[1]. It is also the fourth most prevalent cancer in the world[2], although recent trends show stabilization of incidence rates and a continued decrease in cancer death rates[3].
Prevention of gastric cancer can be broadly divided into primary and secondary prevention. Primary prevention is essentially behavioral modification, which seeks to control the etiological agents of gastric cancer[4]. Several modifiable risk factors contribute to the development of gastric cancer. Infection with Helicobacter pylori (H. pylori) is a well-established risk factor[5], and the potential of preventing gastric cancer by eradicating H. pylori infection has been emphasized in the recent studies[6,7]. Salt intake levels of at least 10 g/d (4000 mg Na) significantly increase the risk of gastric cancer[8]. Fresh fruits and vegetables contain sufficient amounts of vitamin C and dietary fiber, which strongly reduce the risk of gastric cancer[4,9]. A previous study found that subjects in the bottom third of the distribution of vitamin C intake had a 2.5-fold higher risk of developing gastric cancer[10]. Additionally, there is a significant dose-dependent relationship between smoking and gastric cancer[11].
Secondary prevention relies on early detection, which can be achieved through regular cancer screenings[12]. This form of prevention is a priority in Korea, which has one of the highest incidence rates of stomach cancer in the world. The Korean National Cancer Screening Program (KNCSP) recommends that individuals aged 40 years or older undergo biennial gastric cancer screening (Table 1). Although the effect of mass screening remains controversial, it may help by identifying cancer at an early stage[13,14]. According to a study in Korea, the proportion of early gastric cancer (EGC) was 96% in a repeated screening group and 71% in an infrequent screening group, among patients with newly diagnosed gastric cancer[15]. The 5-year survival rate of EGC is greater than 90%[16].
Table 1.
The national cancer screening program in Korea
| Cancer | Target population | Frequency | Test or procedure | Co-payment1 (US $) |
| Stomach | 40 and over (adults) | Every 2 yr | Endoscopy or Upper Gastrointestinal Series | 7 |
| Colorectal | 50 and over (adults) | Every 1 yr2 | Fecal Occult Blood Test3 | 0.5 |
| Breast | 40 and over (women) | Every 2 yr | Mammography and Clinical breast exam | 3.5 |
| Cervix | 30 and over (women) | Every 2 yr | Pap smear | 0 |
Co-payments only applied to people with a higher income (i.e., upper 50%), and account for 20% of the total price. No co-payment is applied to the low-income population (i.e., lower 50%). There is no co-payment for cervical cancer screening regardless of income level;
Colorectal screening is provided every 2 years to most of the target population, with the exception of low-income people or manual laborers;
Colonoscopy or barium enema are performed if the fecal occult blood test is positive.
A positive family history of gastric cancer is one of the most important factors, increasing the risk of developing the disease by three-fold[17,18]. There is evidence that there may be a synergistic interaction between family history and H. pylori infection in the development of gastric cancer[18]. In addition, patients with a family history tend to have larger or more deeply infiltrated tumors[15]. As many risk factors of gastric cancer are modifiable, it is meaningful to investigate gastric cancer screening and preventive behaviors among high risk groups, such as the relatives of patients with gastric cancer [i.e., gastric cancer relatives (GCRs)] such that early detection and prevention can be achieved. The main purpose of this study is to investigate the current status of gastric cancer screening and preventive behaviors in GCRs.
MATERIALS AND METHODS
Study design
We performed a cross-sectional study of Koreans (n = 3557) who were at least 40 years old, with the aim of investigating the gastric cancer screening rates and preventive behaviors of GCRs compared with those of the general population. To differentiate the impact of family history of gastric cancer from that of other cancers, we studied subjects with a family history of cancer other than gastric cancer [i.e., non-GCRs (NGCRs)] and subjects without a family history of any cancer (controls).
Data source
We analyzed data from the 2005 Korea National Health and Nutrition Examination Survey (KNHANES III), which was conducted by the Korea Centers for Disease Control to evaluate the health and nutrition status of the Korean population. The KNHANES III categorized the nation into 600 regions at the first stage, selecting 20 households from each region at the second stage. Data collected from the samples were adjusted to represent the entire population of Korea. The questionnaire consisted of four parts: a health interview survey, a health behavior survey, a health examination survey, and a nutrition survey. Information about family histories of cancer were obtained from the health examination survey, cancer screening behaviors and smoking behaviors were assessed using the health behavior survey, and 1 d food intake (i.e., for the last 24 h prior to the survey) was evaluated using the nutrition survey.
Study subjects
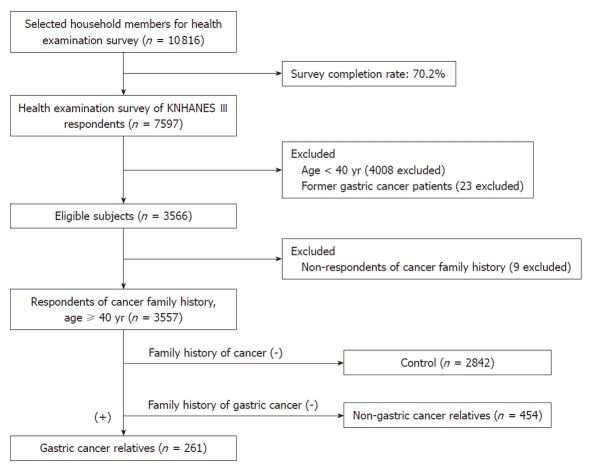
The completion rate of the health examination survey in KNHANES III was 70.2%. Of the 7597 subjects who responded to the health examination survey, we excluded respondents under the age of 40 years (n = 4008), former and current patients with stomach cancer (n = 23), and those who did not complete questions about their family history (n = 9). Data from the remaining 3557 respondents were analyzed (Figure 1). The following questions from the health examination survey supplement were used to categorize the subjects into three groups: (1) “Has your father, mother, brother or sister ever been clinically diagnosed with any form of cancer?” (responses included “yes” or “no”) and (2) “If you responded ‘yes’, write the type of the cancer.” These questions were asked three times to identify exactly which family member, if any, had a history of cancer. According to the answers, respondents were categorized into the following three groups: (1) GCRs; (2) NGCRs; and (3) controls. We defined “cancer family history” as subjects whose parents or siblings had a history of cancer.
Figure 1.
Selection of gastric cancer relatives and controls.
We compared the screening patterns for other common cancers (i.e., breast, cervical, and colon cancers) with those of gastric cancer. We excluded subjects with a history of breast, cervical, or colon cancer, respectively. Only females were included in the analysis of breast and cervical cancer. Only subjects 50 years and older were included in the analysis of colon cancer.
Variables
Factors known or thought to affect gastric cancer screening behavior were used as covariates, including socioeconomic factors (e.g., sex, age, education level, marital status, and income), health-related behaviors (e.g., smoking and alcohol consumption), and psychological factors (e.g., self-reported health status)[19].
Gastric cancer screening behaviors were assessed via the question, “When was the last time you were screened for gastric cancer (i.e., gastroscopy or upper gastrointestinal series)?” Responses included, “Less than 1 year ago”, “1 year to 2 years ago”, “More than 2 years ago” and “Never”. In accordance with the KNCSP guidelines, we distinguished screened and unscreened subjects based on whether they had undergone gastric cancer screening within the previous 2 years, and whether they had received a mammography or ultrasonography for breast cancer, a pap smear for cervical cancer, or a colonoscopy or barium enema for colon cancer within the past 2, 2, or 5 years, respectively (Table 1).
The 1 d intakes of sodium, vitamin C, and dietary fiber were calculated using the subjects’ responses to the interviewer-administered 24-h dietary recall, a tool that has been used in American surveys because of the accurate and complete self-reported information that it provides[20]. In our analyses, sodium, vitamin C, and dietary fiber were dichotomized according to current dietary recommendations, with a maximum recommended sodium intake of 2000 mg[21], a minimum recommended vitamin C intake of 60 mg[22], and a minimum recommended dietary fiber intake of 20 g[23].
Statistical analysis
The STATA program (version 10.0) was used to analyze the data. The chi-squared test was used to analyze the general characteristics, cancer screening, and preventive behaviors of each group. Adjusted means and adjusted rates of each group were analyzed via analysis of covariance, after adjustment for age, sex, education, marital status, smoking status, alcohol consumption, income, and self-reported health status. Crude odds ratios were analyzed via simple logistic regression, while adjusted odds ratios (aORs) were analyzed via multiple logistic regression, after adjustment for factors that affect gastric cancer screening behaviors, as mentioned above. Association analysis weights were used to minimize selection bias.
RESULTS
Characteristics of subjects
The socioeconomic environment, health behaviors, and psychological factors of the subjects are shown in Table 2. Of the 3557 subjects in the study population, 715 had a family history of cancer and 261 had a family history of gastric cancer. The factors listed in Table 2 were used as variables in subsequent multivariate logistic regression analyses.
Table 2.
Characteristics of gastric cancer relatives and controls n (%)
| Controls (n = 2842) | Non-gastric cancer relatives (n = 454) | Gastric cancer relatives (n = 261) | P1 | |
| Sex | ||||
| Male | 1258 (44.3) | 190 (41.9) | 105 (40.2) | 0.321 |
| Female | 1584 (55.7) | 264 (58.2) | 156 (59.8) | |
| Age (yr) | ||||
| 40-49 | 1024 (36.0) | 211 (46.5) | 104 (39.9) | < 0.001 |
| 50-59 | 710 (25.0) | 118 (26.0) | 85 (32.6) | |
| 60-69 | 665 (23.4) | 85 (18.7) | 51 (19.5) | |
| ≥ 70 | 443 (15.6) | 40 (8.8) | 21 (8.1) | |
| Education | ||||
| Elementary | 1136 (40.0) | 116 (25.6) | 79 (30.3) | < 0.001 |
| Middle to high school | 1271 (44.7) | 246 (54.2) | 146 (55.9) | |
| University and higher | 435 (15.3) | 92 (20.3) | 36 (13.8) | |
| Marital status | ||||
| Married | 2188 (77.0) | 387 (85.4) | 211 (80.8) | < 0.001 |
| Single | 653 (23.0) | 66 (14.6) | 50 (19.2) | |
| Smoking status | ||||
| Non-smoker | 1588 (57.3) | 260 (59.8) | 152 (59.6) | 0.657 |
| Ex-smoker | 582 (21.0) | 86 (19.8) | 45 (17.7) | |
| Current smoker | 602 (21.7) | 89 (20.5) | 58 (22.8) | |
| Alcohol drinking | ||||
| None | 1524 (55.0) | 241 (55.4) | 145 (56.9) | 0.841 |
| More than once a month | 1248 (45.0) | 194 (44.6) | 110 (43.1) | |
| Income (US $/mo)2 | ||||
| < 1000 | 801 (28.2) | 87 (19.2) | 48 (18.4) | < 0.001 |
| 1000-5000 | 1825 (64.2) | 315 (69.4) | 192 (73.6) | |
| ≥ 5000 | 216 (7.6) | 52 (11.5) | 21 (8.1) | |
| Self-reported health status | ||||
| Good | 873 (30.8) | 149 (33.0) | 82 (31.7) | 0.502 |
| Intermediate | 1017 (35.9) | 171 (37.8) | 96 (37.1) | |
| Bad | 946 (33.4) | 132 (29.2) | 81 (31.3) | |
| Stress | ||||
| Low | 1822 (65.7) | 294 (67.6) | 168 (65.9) | 0.703 |
| Moderate | 770 (27.8) | 120 (27.6) | 73 (28.6) | |
| High | 180 (6.5) | 21 (4.8) | 14 (5.5) | |
1P values were calculated by using a χ2 test;
1 US $ = 1000 won.
Gastric cancer screening behavior
Our analysis of gastric cancer screening rates revealed that GCRs were significantly more likely than the control group to undergo gastric cancer screening (39.2% vs 32.3%, aOR: 1.43, CI: 1.05-1.95). The gastric cancer screening rate of NGCRs was not significantly different from that of the control group (37.2% vs 32.3%, aOR: 1.08, CI: 0.83-1.41) (Table 3).
Table 3.
Prevalence of cancer screening n (%)
| Controls (n = 2842) | Non-gastric cancer relatives (n = 454) | Gastric cancer relatives (n = 261) | |
| Stomach cancer screening (within 2 yr) | |||
| Crude rate | 894 (32.3) | 162 (37.2) | 100 (39.2) |
| Adjusted rate (%, 95% CI)2 | 32.2 (30.5, 34.0) | 35.2 (30.8, 39.8) | 38.1 (32.3, 44.2) |
| Crude OR (95% CI) | 1 (referent) | 1.16 (0.89, 1.50) | 1.47 (1.08, 2.00)a |
| Adjusted OR (95% CI)1 | 1 (referent) | 1.08 (0.83, 1.41) | 1.43 (1.05, 1.95)a |
| Breast cancer screening (within 2 yr) | |||
| Crude rate | 456 (29.6) | 102 (40.8) | 61 (40.9) |
| Adjusted rate (%, 95% CI)2 | 28.9 (26.7, 31.4) | 36.5 (30.7, 42.8) | 38.5 (31.0, 46.7) |
| Crude OR (95% CI) | 1 (referent) | 1.68 (1.21, 2.33)a | 1.53 (1.05, 2.23)a |
| Adjusted OR (95% CI)1 | 1 (referent) | 1.42 (1.02, 2.00)a | 1.40 (0.95, 2.08) |
| Cervical cancer screening (within 2 yr) | |||
| Crude rate | 596 (39.9) | 133 (53.9) | 71 (47.7) |
| Adjusted rate (%, 95% CI)2 | 39.1 (36.5, 41.8) | 47.3 (40.7, 54.1) | 43.2 (35.1, 51.7) |
| Crude OR (95% CI) | 1 (referent) | 1.90 (1.35, 2.68)a | 1.33 (0.90, 1.97) |
| Adjusted OR (95% CI)1 | 1 (referent) | 1.51 (1.04, 2.20)a | 1.14 (0.76, 1.71) |
| Colon cancer screening (within 5 yr) | |||
| Crude rate | 309 (17.5) | 55 (23.6) | 33 (21.4) |
| Adjusted rate (%, 95% CI)2 | 17.2 (15.4, 19.0) | 22.6 (17.7, 28.5) | 20.2 (14.6, 27.3) |
| Crude OR (95% CI) | 1 (referent) | 1.17 (0.78, 1.74) | 1.48 (0.85, 2.56) |
| Adjusted OR (95% CI)1 | 1 (referent) | 1.10 (0.73, 1.67) | 1.41 (0.83, 2.41) |
P < 0.05.
Calculated via multiple logistic regression and adjusted for age, sex, education, marital status, smoking, alcohol consumption, income, and self-reported health status;
Calculated via analysis of covariance adjusted for age, sex, education, marital status, smoking, alcohol consumption, income, and self-reported health status. OR: Odds ratio.
The rate of gastric cancer screening was higher among younger than older GCRs (42.4% vs 31.0%), and higher among younger GCRs than among controls (aOR 1.53 vs 1.08) Similarly, GCRs with a high income were screened more often than were GCRs with middle or low incomes (68.4% vs 41.8% and 17.0%, respectively), or controls (aOR: 2.70 vs 1.56 and 0.70, respectively). Gastric cancer screening did not vary according to education level (Table 4).
Table 4.
Gastric cancer screening prevalence by education level, age and income subgroups
| Controls (n = 2842) | Non-gastric cancer relatives (n = 454) | Gastric cancer relatives (n = 261) | |
| Education level | |||
| Elementary | |||
| n (%) | 322 (29.2) | 37 (32.5) | 27 (35.1) |
| aOR (95% CI)1 | 1 (referent) | 0.93 (0.57, 1.51) | 1.59 (0.85, 2.96) |
| Middle and higher | |||
| n (%) | 572 (34.3) | 125 (38.9) | 73 (41) |
| aOR (95% CI)1 | 1 (referent) | 1.13 (0.82, 1.55) | 1.36 (0.97, 1.92) |
| Age group (yr) | |||
| 40-59 | |||
| n (% | 585 (34.5) | 118 (37.7) | 78 (42.4) |
| aOR (95% CI)1 | 1 (referent) | 1.11 (0.82, 1.49) | 1.53 (1.07, 2.17)a |
| ≥ 60 | |||
| n (%) | 309 (28.8) | 44 (36.1) | 22 (31) |
| aOR (95% CI)1 | 1 (referent) | 0.99 (0.57, 1.69) | 1.08 (0.59, 1.98) |
| Income (US $/mo) | |||
| < 1000 | |||
| n (%) | 214 (27.1) | 22 (26.2) | 8 (17) |
| aOR (95% CI)1 | 1 (referent) | 0.86 (0.47, 1.57) | 0.70 (0.28, 1.77) |
| 1000-5000 | |||
| n (%) | 580 (32.8) | 113 (37.7) | 79 (41.8) |
| aOR (95% CI)1 | 1 (referent) | 1.16 (0.84, 1.60) | 1.56 (1.10, 2.21)a |
| ≥ 5000 | |||
| n (%) | 100 (47.4) | 27 (53.0) | 13 (68.4) |
| aOR (95% CI)1 | 1 (referent) | 1.02 (0.46, 2.26) | 2.70 (0.82, 8.88) |
P < 0.05.
Adjusted odds ratios (aOR) were calculated via multiple logistic regression.
Other cancer screening behaviors
The prevalence rates of cancer screening were slightly higher in GCRs and NGCRs compared with control subjects, although these differences were not consistently significant. Female NGCRs were more likely to undergo breast cancer screening (40.8% vs 29.6%, aOR: 1.42, CI: 1.02-2.00) and cervical cancer screening (53.9% vs 39.9%, aOR: 1.51, CI: 1.04-2.20) when compared with controls. Female GCRs were slightly more likely to undergo breast cancer screening compared with the control group (40.9% vs 29.6%, aOR: 1.40, CI: 0.95-2.08), although this difference was insignificant. The groups did not differ with regards to colon cancer screening.
Gastric cancer preventive behaviors
Gastric cancer preventive behaviors were similar among the three groups (Table 5). Sodium consumption was elevated in all three groups. The proportion of individuals with excessive sodium intake (i.e., more than 2000 mg per day) was more than 90% in all three groups, even in GCRs (94.6%). There was a tendency toward higher intake of vitamin C in GCRs and NGCRs compared with the control group [mean ± SE (mg): 110.0 ± 6.2 and 114.1 ± 4.9 vs 98.5 ± 1.6, respectively], but this difference was not statistically significant after adjustment. Approximately 30% of the subjects in each groups consumed less than 60 mg vitamin C per day. The average consumption of dietary fiber was not significantly different among the groups. The proportion of individuals with a deficient intake of dietary fiber (< 20 g/d) was approximately 85% in all three groups. The current smoking rate was similar in the three groups.
Table 5.
Gastric cancer-preventive behaviors
| Controls (n = 2842) | Non-gastric cancer relatives (n = 454) | Gastric cancer relatives (n = 261) | ||||
| Crude | Adjusted | Crude | Adjusted | Crude | Adjusted | |
| Na (mg) | ||||||
| Mean intake (SE)2 | 5582 (66) | 5602 (64) | 5574 (166) | 5522 (162) | 5516 (213) | 5483 (212) |
| P value | 0.86 | 0.99 | 0.76 | 0.50 | ||
| High sodium intake (> 2000 mg) | ||||||
| Rate, n (%)2 | 2625 (92.4) | 93.8 | 429 (94.5) | 94.9 | 247 (94.6) | 95.1 |
| Odds ratio1 | 1 (referent) | 1 (referent) | 1.67 (1.04, 2.67)a | 1.56 (0.95, 2.57) | 1.34 (0.71, 2.54) | 1.17 (0.61, 2.26) |
| Vitamin C (mg) | ||||||
| Mean intake (SE)2 | 98.5 (1.6) | 100.0 (1.6) | 114.1 (4.9) | 109.7 (4.1) | 110.0 (6.2) | 107.2 (5.4) |
| P value | 0.03a | 0.15 | 0.07 | 0.19 | ||
| Low vitamin C intake (< 60 mg) | ||||||
| Rate, n (%)2 | 922 (32.4) | 30.7 | 129 (28.4) | 30.5 | 78 (29.9) | 30.8 |
| Odds ratio1 | 1 (referent) | 1 (referent) | 0.79 (0.59, 1.06) | 0.91 (0.67, 1.23) | 0.79 (0.55, 1.13) | 0.89 (0.62, 1.28) |
| Dietary fiber (g) | ||||||
| Mean intake (SE)2 | 8.0 (0.1) | 8.0 (0.1) | 8.4 (0.2) | 8.3 (0.2) | 8.3 (0.3) | 8.3 (0.3) |
| P-value | 0.20 | 0.30 | 0.08 | 0.14 | ||
| Low fiber intake (< 20 g) | ||||||
| Rate, n (%)2 | 2447 (86.1) | 87 | 383 (84.4) | 86.9 | 225 (86.2) | 87.4 |
| Odds ratio1 | 1 (referent) | 1 (referent) | 0.86 (0.44, 1.66) | 0.86 (0.44, 1.68) | 1.17 (0.50, 2.72) | 1.20 (0.50, 2.85) |
| Current smoking status | ||||||
| Rate, n (%)2 | 602 (21.7) | 12.9 | 89 (20.5) | 13.2 | 58 (22.8) | 15.4 |
| Odds ratio1 | 1 (referent) | 1 (referent) | 0.95 (0.69, 1.29) | 1.04 (0.73, 1.47) | 1.10 (0.78, 1.55) | 1.18 (0.76, 1.83) |
P < 0.05.
Adjusted odds ratios were calculated via multiple logistic regression and adjusted for age, sex, education, marital status, smoking, alcohol consumption, income, and self-reported health status;
Adjusted means and adjusted rates were calculated via analysis of covariance adjusted for age, sex, education, marital status, smoking, alcohol consumption, income, and self-reported health status.
DISCUSSION
To our knowledge, this is the first study of gastric cancer screening and preventive behaviors among GCRs. The strengths of this study are the use of a nationally representative sample and the inclusion of three comparison groups to more clearly reveal relationships. Our findings suggest that GCRs undergo gastric cancer screening more often than others, although the gastric cancer screening rate among GCRs was still relatively low (39.2%). The rates of breast cancer, cervical cancer, and colon cancer screening were not significantly higher in GCRs than in the control group. The dietary patterns and smoking behaviors of GCRs were similar to those of the other two groups.
The finding that GCRs undergo more frequent gastric cancer screening is consistent with previous reports for other cancers. Female relatives of patients with breast cancer are more likely to undergo mammogram screening than are females without a family history of breast cancer[24]. Similarly, men with a family history of prostate cancer are more likely to undergo prostate cancer screening. These findings suggest that a family history of cancer creates a greater sense of vulnerability and is an important factor in the decision to undergo screening[25]. Nonetheless, the screening rates for cancers other than gastric cancer were not different from those of the controls, suggesting that gastric cancer screening behaviors in GCRs is incidental and opportunistic, and not necessarily the result of a formal, systematic training on the importance of cancer screening in general. In addition, it is supposed that GCRs are motivated to undergo gastric cancer screening because of worries about possible cancer development rather than recognition of the benefits of screening. This hypothesis is also explained by the fact that individuals’ awareness of the benefits of screening, which is thought to be the result of educational campaigns, was no higher in GCRs than in the control group (63.9% vs 64.4%, Table 6). The diagnosis of cancer in a first-degree relative may spur a person into action, as suggested by the Health Belief Model[26], which might explain the increased rate of gastric cancer screening in GCRs.
Table 6.
Perception of the benefits of screening n (%)
| Controls (n = 2842) | Non-gastric cancer relatives(n = 454) | Gastric cancer relatives (n = 261) | |
| Beneficial | 1783 (64.4) | 292 (67.1) | 163 (63.9) |
| Not beneficial | 292 (10.5) | 47 (10.8) | 36 (14.1) |
| Have never received | 696 (25.1) | 96 (22.1) | 56 (22.0) |
More importantly, the absolute screening rate in GCRs was only 39.2%, indicating that more than half of the GCRs had not yet undergone regular gastric screening. Endoscopic mass screening for gastric cancer is effective in identifying cancer at an early stage and is cost-effective, especially in moderate- to high-risk populations[14,27]. In Korea, gastric cancer screening is provided as a part of the national cancer screening program, with virtually no economic barrier (Table 1). Therefore, the gastric cancer screening rate should theoretically be high, even in the general population, and GCRs should undergo at least biennial screening, barring a contraindication. Proper educational programs are needed to emphasize the benefits of screening to GCRs, especially those who are older and earn a lower income.
Although GCRs underwent gastric cancer screening more often than other people, their dietary habits and smoking behaviors were not significantly different from those of the control group. Many members of the GCR group had inappropriate dietary habits, with 94.6% consuming excessive sodium, 29.9% deficient in vitamin C, and 86.2% deficient in dietary fiber. This finding was consistent with a previous study of breast cancer relatives, which found that female relatives were more likely to undertake medical actions but not lifestyle preventive behaviors[28]. However, another study suggested that relatives were motivated to change their consumption of fruits, vegetables, and fat once they understood that their behavior could increase their risk of cancer[29]. It is possible that a large proportion of the subjects did not completely understand the extent to which unhealthy behaviors increase the risk of gastric cancer. Healthy lifestyle changes are most successful when individuals believe that the changes will reduce their risk of adverse conditions[30]. For example, perceived vulnerability was a primary motivator for efforts to quit smoking among family members of lung cancer patients[31]. These findings suggest that GCRs should be made aware of the elevated risk of gastric cancer due to unhealthy behaviors. However, a survey has shown that the general Korean public did not clearly understand the risk factors for gastric cancer[32]. Therefore, family education programs should be developed to ensure that GCRs are aware of the risk factors for gastric cancer and the importance of regular screening and preventive behaviors. As the cancer diagnosis and treatment provide a teachable moment for family members as well as the patients themselves[26,31], hospital-based education programs involving both patients and family members could be considered as a potential method to deliver educational messages about gastric cancer screening and other preventive behaviors to them. In a similar example, a family-based health education and counseling intervention program was effective in changing health behaviors of children with a family history of cardiovascular diseases[33]. Another promising method of intervention is clinical treatment that is combined with computerized family-history tools, such as Family Healthware[34], which provides tailored preventive health messages focused on health behaviors and screening, not only for patients, but also for their doctors to offer appropriate recommendations.
This study had several limitations. First, we were unable to assess the prevalence of H. pylori existence in the subjects because of the retrospective nature of the study. H. pylori eradication is recommended for patients who are first degree relatives of patients with gastric cancer[6,7,35]. Second, the survey did not assess whether the subjects were aware of the causes of gastric cancer or the recommended biennial gastric cancer screening. Third, the statistical significance may have been limited by the relatively small number of GCRs. Fourth, as the design of this study is cross-sectional, we have no information regarding the gastric screening adherence at follow-up. Thus, further research is needed to determine how many subjects actually continue to undergo a 2-year screening procedure. Fifth, only 70.2% of the selected household members responded to the health examination survey. Therefore, it cannot be excluded that the other 29.8% of the household members who did not participate in the survey were less interested in health. As a result, preventive behaviors could be even worse than the findings of this study. Finally, the survey was based on self-reported data, which can potentially increase the risk of inaccuracy. However, the validity of self-reported cancer screening histories and interviewer-administered 24-h dietary recall have been shown to be accurate and reliable[20,36], although few studies have examined the validity of self-reported upper endoscopy history, which is still used in national surveys.
In conclusion, GCRs were found to be more likely to undergo gastric cancer screening compared with the control group. However, this behavior may be incidental, opportunistic, and motivated by concern rather than a true recognition of the benefits of screening by systematic education. The overall gastric cancer screening rate was relatively low in GCRs. The GCRs did not differ from controls with regards to the 1 d intake of sodium, vitamin C, and dietary fiber and a high proportion of GCRs reported inappropriate dietary habits. In addition, the smoking rate was similar in GCRs and controls. To promote awareness about gastric cancer screening and prevention in GCRs, family education programs should be developed and implemented in a systematic manner.
ACKNOWLEDGMENTS
We thank the staff of the Korean National Health Insurance Corporation for their cooperation.
COMMENTS
Background
These days, increasing emphasis is placed on early detection and prevention of cancers, as it is difficult to cure them when they develop. Gastric cancer is one of the cancers that are modifiable through lifestyle preventive behaviors and regular cancer screening. Currently, only a few Asian countries, including Korea, Japan, and Matsu Island in Taiwan, are conducting population-based screening for gastric cancer.
Research frontiers
Regular screening and health behaviors of high-risk groups have been always emphasized. However, it has not been unequivocally addressed as to how regularly or strictly gastric cancer relatives (GCRs), one of the high-risk groups for gastric cancer, are practicing these measures. In this study, the authors demonstrated that GCRs had much room for improvement in their cancer screening and preventive behaviors.
Innovations and breakthroughs
There have been previous reports that highlighted the low gastric cancer screening rate in the general public. This is the first study to use a nationally representative sample and report that GCRs were more likely to undergo gastric cancer screening, even though their lifestyle preventive behaviors did not show significant differences compared to controls. Furthermore, this study suggests that GCRs were not fully aware of the importance of screening and the potential impacts of risk factors for gastric cancer.
Applications
This study highlights the necessity of targeted intervention for GCRs and also proposes a future strategy through systematic family education programs.
Peer review
This is an interesting, well-written study.
Footnotes
Supported by The research program was funded by the National Health Insurance Corporation
Peer reviewers: Angelo Zullo, MD, Department of Gastroenterology and Digestive Endoscopy, “Nuovo Regina Margherita” Hospital, Via E. Morosini 30, 00153 Rome, Italy; Maria de Fátima Gärtner, DVM, PhD(Med), ECVP(Dipl.), Full Professor of Veterinary Pathology, Carcinogenesis Group, IPATIMUP, Rua Dr. Roberto Frias s/n, 4200-456 Porto, Portugal
S- Editor Sun H L- Editor Stewart GJ E- Editor Zheng XM
References
- 1.Jung KW, Park S, Kong HJ, Won YJ, Boo YK, Shin HR, Park EC, Lee JS. Cancer statistics in Korea: incidence, mortality and survival in 2006-2007. J Korean Med Sci. 2010;25:1113–1121. doi: 10.3346/jkms.2010.25.8.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10. Lyon: International Agency for Research on Cancer; 2010. [Google Scholar]
- 3.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ. Cancer statistics, 2008. CA Cancer J Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 4.Correa P. The epidemiology of gastric cancer. World J Surg. 1991;15:228–234. doi: 10.1007/BF01659057. [DOI] [PubMed] [Google Scholar]
- 5.Peleteiro B, Lunet N, Figueiredo C, Carneiro F, David L, Barros H. Smoking, Helicobacter pylori virulence, and type of intestinal metaplasia in Portuguese males. Cancer Epidemiol Biomarkers Prev. 2007;16:322–326. doi: 10.1158/1055-9965.EPI-06-0885. [DOI] [PubMed] [Google Scholar]
- 6.Malfertheiner P, Megraud F, O’Morain C, Bazzoli F, El-Omar E, Graham D, Hunt R, Rokkas T, Vakil N, Kuipers EJ. Current concepts in the management of Helicobacter pylori infection: the Maastricht III Consensus Report. Gut. 2007;56:772–781. doi: 10.1136/gut.2006.101634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fock KM, Katelaris P, Sugano K, Ang TL, Hunt R, Talley NJ, Lam SK, Xiao SD, Tan HJ, Wu CY, et al. Second Asia-Pacific Consensus Guidelines for Helicobacter pylori infection. J Gastroenterol Hepatol. 2009;24:1587–1600. doi: 10.1111/j.1440-1746.2009.05982.x. [DOI] [PubMed] [Google Scholar]
- 8.Shikata K, Kiyohara Y, Kubo M, Yonemoto K, Ninomiya T, Shirota T, Tanizaki Y, Doi Y, Tanaka K, Oishi Y, et al. A prospective study of dietary salt intake and gastric cancer incidence in a defined Japanese population: the Hisayama study. Int J Cancer. 2006;119:196–201. doi: 10.1002/ijc.21822. [DOI] [PubMed] [Google Scholar]
- 9.Mayne ST, Risch HA, Dubrow R, Chow WH, Gammon MD, Vaughan TL, Farrow DC, Schoenberg JB, Stanford JL, Ahsan H, et al. Nutrient intake and risk of subtypes of esophageal and gastric cancer. Cancer Epidemiol Biomarkers Prev. 2001;10:1055–1062. [PubMed] [Google Scholar]
- 10.Block G. Vitamin C and cancer prevention: the epidemiologic evidence. Am J Clin Nutr. 1991;53:270S–282S. doi: 10.1093/ajcn/53.1.270S. [DOI] [PubMed] [Google Scholar]
- 11.Sjödahl K, Lu Y, Nilsen TI, Ye W, Hveem K, Vatten L, Lagergren J. Smoking and alcohol drinking in relation to risk of gastric cancer: a population-based, prospective cohort study. Int J Cancer. 2007;120:128–132. doi: 10.1002/ijc.22157. [DOI] [PubMed] [Google Scholar]
- 12.Adami HO, Day NE, Trichopoulos D, Willett WC. Primary and secondary prevention in the reduction of cancer morbidity and mortality. Eur J Cancer. 2001;37 Suppl 8:S118–S127. doi: 10.1016/s0959-8049(01)00262-3. [DOI] [PubMed] [Google Scholar]
- 13.Lee KJ, Inoue M, Otani T, Iwasaki M, Sasazuki S, Tsugane S. Gastric cancer screening and subsequent risk of gastric cancer: a large-scale population-based cohort study, with a 13-year follow-up in Japan. Int J Cancer. 2006;118:2315–2321. doi: 10.1002/ijc.21664. [DOI] [PubMed] [Google Scholar]
- 14.Tashiro A, Sano M, Kinameri K, Fujita K, Takeuchi Y. Comparing mass screening techniques for gastric cancer in Japan. World J Gastroenterol. 2006;12:4873–4874. doi: 10.3748/wjg.v12.i30.4873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nam SY, Choi IJ, Park KW, Kim CG, Lee JY, Kook MC, Lee JS, Park SR, Lee JH, Ryu KW, et al. Effect of repeated endoscopic screening on the incidence and treatment of gastric cancer in health screenees. Eur J Gastroenterol Hepatol. 2009;21:855–860. doi: 10.1097/MEG.0b013e328318ed42. [DOI] [PubMed] [Google Scholar]
- 16.Lo SS, Wu CW, Chen JH, Li AF, Hsieh MC, Shen KH, Lin HJ, Lui WY. Surgical results of early gastric cancer and proposing a treatment strategy. Ann Surg Oncol. 2007;14:340–347. doi: 10.1245/s10434-006-9077-x. [DOI] [PubMed] [Google Scholar]
- 17.Fock KM, Talley N, Moayyedi P, Hunt R, Azuma T, Sugano K, Xiao SD, Lam SK, Goh KL, Chiba T, et al. Asia-Pacific consensus guidelines on gastric cancer prevention. J Gastroenterol Hepatol. 2008;23:351–365. doi: 10.1111/j.1440-1746.2008.05314.x. [DOI] [PubMed] [Google Scholar]
- 18.Shin CM, Kim N, Yang HJ, Cho SI, Lee HS, Kim JS, Jung HC, Song IS. Stomach cancer risk in gastric cancer relatives: interaction between Helicobacter pylori infection and family history of gastric cancer for the risk of stomach cancer. J Clin Gastroenterol. 2010;44:e34–e39. doi: 10.1097/MCG.0b013e3181a159c4. [DOI] [PubMed] [Google Scholar]
- 19.Kwon YM, Lim HT, Lee K, Cho BL, Park MS, Son KY, Park SM. Factors associated with use of gastric cancer screening services in Korea. World J Gastroenterol. 2009;15:3653–3659. doi: 10.3748/wjg.15.3653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thompson FE, Midthune D, Subar AF, Kipnis V, Kahle LL, Schatzkin A. Development and evaluation of a short instrument to estimate usual dietary intake of percentage energy from fat. J Am Diet Assoc. 2007;107:760–767. doi: 10.1016/j.jada.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 21.The Korean Nutrition Society. Dietary Reference Intakes for Koreans, 2005. Available from: http://www.kns.or.kr/
- 22.Levine M, Rumsey SC, Daruwala R, Park JB, Wang Y. Criteria and recommendations for vitamin C intake. JAMA. 1999;281:1415–1423. doi: 10.1001/jama.281.15.1415. [DOI] [PubMed] [Google Scholar]
- 23.Nakaji S, Sugawara K, Saito D, Yoshioka Y, MacAuley D, Bradley T, Kernohan G, Baxter D. Trends in dietary fiber intake in Japan over the last century. Eur J Nutr. 2002;41:222–227. doi: 10.1007/s00394-002-0379-x. [DOI] [PubMed] [Google Scholar]
- 24.Lerman C, Rimer B, Trock B, Balshem A, Engstrom PF. Factors associated with repeat adherence to breast cancer screening. Prev Med. 1990;19:279–290. doi: 10.1016/0091-7435(90)90028-i. [DOI] [PubMed] [Google Scholar]
- 25.Jacobsen PB, Lamonde LA, Honour M, Kash K, Hudson PB, Pow-Sang J. Relation of family history of prostate cancer to perceived vulnerability and screening behavior. Psychooncology. 2004;13:80–85. doi: 10.1002/pon.760. [DOI] [PubMed] [Google Scholar]
- 26.Humpel N, Magee C, Jones SC. The impact of a cancer diagnosis on the health behaviors of cancer survivors and their family and friends. Support Care Cancer. 2007;15:621–630. doi: 10.1007/s00520-006-0207-6. [DOI] [PubMed] [Google Scholar]
- 27.Leung WK, Wu MS, Kakugawa Y, Kim JJ, Yeoh KG, Goh KL, Wu KC, Wu DC, Sollano J, Kachintorn U, et al. Screening for gastric cancer in Asia: current evidence and practice. Lancet Oncol. 2008;9:279–287. doi: 10.1016/S1470-2045(08)70072-X. [DOI] [PubMed] [Google Scholar]
- 28.Madlensky L, Vierkant RA, Vachon CM, Pankratz VS, Cerhan JR, Vadaparampil ST, Sellers TA. Preventive health behaviors and familial breast cancer. Cancer Epidemiol Biomarkers Prev. 2005;14:2340–2345. doi: 10.1158/1055-9965.EPI-05-0254. [DOI] [PubMed] [Google Scholar]
- 29.Lemon SC, Zapka JG, Clemow L. Health behavior change among women with recent familial diagnosis of breast cancer. Prev Med. 2004;39:253–262. doi: 10.1016/j.ypmed.2004.03.039. [DOI] [PubMed] [Google Scholar]
- 30.Rabin C, Pinto B. Cancer-related beliefs and health behavior change among breast cancer survivors and their first-degree relatives. Psychooncology. 2006;15:701–712. doi: 10.1002/pon.1000. [DOI] [PubMed] [Google Scholar]
- 31.Patterson F, Wileyto EP, Segal J, Kurz J, Glanz K, Hanlon A. Intention to quit smoking: role of personal and family member cancer diagnosis. Health Educ Res. 2010;25:792–802. doi: 10.1093/her/cyq033. [DOI] [PubMed] [Google Scholar]
- 32.Oh DY, Choi KS, Shin HR, Bang YJ. Public awareness of gastric cancer risk factors and disease screening in a high risk region: a population-based study. Cancer Res Treat. 2009;41:59–66. doi: 10.4143/crt.2009.41.2.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salminen M, Vahlberg T, Ojanlatva A, Kivelä SL. Effects of a controlled family-based health education/counseling intervention. Am J Health Behav. 2005;29:395–406. doi: 10.5555/ajhb.2005.29.5.395. [DOI] [PubMed] [Google Scholar]
- 34.Ruffin MT, Nease DE, Sen A, Pace WD, Wang C, Acheson LS, Rubinstein WS, O’Neill S, Gramling R. Effect of preventive messages tailored to family history on health behaviors: the Family Healthware Impact Trial. Ann Fam Med. 2011;9:3–11. doi: 10.1370/afm.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim N, Kim JJ, Choe YH, Kim HS, Kim JI, Chung IS. [Diagnosis and treatment guidelines for Helicobacter pylori infection in Korea] Korean J Gastroenterol. 2009;54:269–278. doi: 10.4166/kjg.2009.54.5.269. [DOI] [PubMed] [Google Scholar]
- 36.Rauscher GH, Johnson TP, Cho YI, Walk JA. Accuracy of self-reported cancer-screening histories: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2008;17:748–757. doi: 10.1158/1055-9965.EPI-07-2629. [DOI] [PubMed] [Google Scholar]