Abstract
Opium is arguably one of the oldest herbal medicines, being used as analgesic, sedative and antidiarrheal drug for thousands of years. These effects mirror the actions of the endogenous opioid system and are mediated by the principal μ-, κ- and δ-opioid receptors. In the gut, met-enkephalin, leu-enkephalin, β-endorphin and dynorphin occur in both neurons and endocrine cells. When released, opioid peptides activate opioid receptors on the enteric circuitry controlling motility and secretion. As a result, inhibition of gastric emptying, increase in sphincter tone, induction of stationary motor patterns and blockade of peristalsis ensue. Together with inhibition of ion and fluid secretion, these effects cause constipation, one of the most frequent and troublesome adverse reactions of opioid analgesic therapy. Although laxatives are most frequently used to ameliorate opioid-induced bowel dysfunction, their efficacy is unsatisfactory. Specific antagonism of peripheral opioid receptors is a more rational approach. This goal is addressed by the use of opioid receptor antagonists with limited absorption such as oral prolonged-release naloxone and opioid receptor antagonists that do not penetrate the blood-brain barrier such as methylnaltrexone and alvimopan. Preliminary evidence indicates that peripherally restricted opioid receptor antagonists may act as prokinetic drugs in their own right.
Keywords: Alvimopan, Methylnaltrexone, Naloxone, Opioid peptides, Enteric nervous system, Opioid-induced bowel dysfunction, Constipation, Peripherally restricted opioid receptor antagonists, Prokinetic effects
1. Introduction
1.1. From opium to opioid receptors in the gut
Opium, the dried latex derived from the unripe seed capsules of the opium poppy, Papaver somniferum, is one of the oldest herbal medicines [1]. Its anesthetic and sedating properties are well described in “De Materia Medica” by Pedanius Dioscorides (Pedanios Dioskurides), a Greek physician in the service of the Roman emperor Nero in the 1st century AD [1]. “De Materia Medica” was compilated around 65 AD and is arguably the first textbook of pharmacology ever written. Dioscorides’ work has been copied and annotated uncounted times, and the oldest surviving copy is treasured in the Austrian National Library in Vienna and indexed as “Codex Vindobonensis Medicus Graecus 1”. Recognized by UNESCO as a World Heritage book, this so-called “Vienna Dioscorides” dates from about 512 AD and is a superb example of Byzantine book-painting [1].
Apart from its effects to facilitate sleep and remove pain, opium has also been used to treat diarrhea since ancient times. Paracelsus (1493–1541) had such a high opinion of opium that he called it “Laudanum”, and this name was later used to denote alcoholic preparations of opium introduced by Thomas Sydenham (1624–1689) [1]. His famous recipe contained 1 lb of sherry wine, 2 oz of opium, 1 oz of saffron, 1 oz of cinnamon powder and 1 oz of clove powder [2]. Importantly, Sydenham also confirmed the efficacy of Laudanum in the treatment of diarrhea associated with dysentery [2]. The active ingredients of opium (e.g., morphine, noscapine, codeine, thebaine, and papaverine) were isolated in the first half of the 19th century [1]. Although not all of these compounds are ligands of opioid receptors, they are able to affect the function of the gastrointestinal (GI) tract by various mechanisms.
Paul Trendelenburg was arguably the first to discover that morphine inhibits the peristaltic reflex in the gut [3], a finding that he reported in his classic text on “Physiologische und pharmakologische Versuche über die Dünndarmperistaltik”, now available in an English translation [4]. Ever since, investigators were intrigued by the physiologic meaning of this discovery, and Otto Schaumann interpreted the pharmacologic effects of exogenous opiates on pain and bowel function as indicative of an endogenous protective system [5]. Schaumann [5] and William D.M. Paton [6] showed that morphine inhibited the release of acetylcholine in the isolated guinea pig ileum, and electrophysiologic studies began to reveal that opiates inhibit the function of the enteric nervous system [7].
After the identification of opiate receptors by Solomon H. Snyder and other investigators [8] the search was out for their endogenous ligand. In 1975, Hans Kosterlitz, together with John Hughes, identified leucine-enkephalin and methionine-enkephalin as the first endogenous opioid receptor agonists [9]. These pentapeptides were also found to occur in the gut [10], and subsequent analysis of their functional implications revealed that opioid receptor agonists interact with pathways of the enteric nervous system that regulate GI motility and secretion [11–15]. In addition, there is evidence that some GI effects of opioid receptor agonists may be mediated by opioid receptors in the brain [16]. However, experimental and clinical studies with opioid receptor antagonists that are unable to enter the brain have shown that the GI effects of opioid analgesics arise from a peripheral site of action [16].
The current review starts by providing a brief overview of the neurobiologic mechanisms whereby opioids modify GI function. After addressing the use of opioid receptor agonists as antidiarrheal drugs, the article goes on to discuss emerging strategies to avoid opioid-induced bowel dysfunction (OBD) and the clinical utility of peripheral opioid receptor antagonists.
2. The endogenous opioid system in the gut
Independently of their plant, mammalian or synthetic origin, opioids are neuroactive substances, their actions being mediated by the principal μ-, κ- and δ-opioid receptors. Many neuroactive drugs act on the gut because the alimentary canal is equipped with the largest collection of neurons outside the brain, known as the enteric nervous system. Enteric neurons originating from the myenteric and submucosal plexuses supply all layers of the alimentary canal and thus are in a position to regulate virtually every aspect of digestion [17,18]. Many of the transmitters and neuropeptides occurring in the brain are also expressed by enteric neurons, and the same is true for transmitter and neuropeptide receptors. Thus, enteric neurons synthesize and release not only acetylcholine, substance P, nitric oxide, adenosine triphosphate, vasoactive intestinal polypeptide and 5-hydroxytryptamine but also opioid peptides as their transmitters.
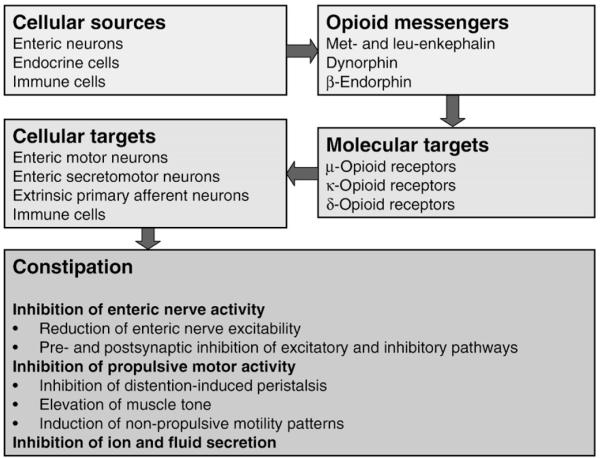
The presence of an elaborate opioid system (Fig.1) in the gut explains why exogenous opioid analgesics inhibit GI function. Met-enkephalin, leu-enkephalin, β-endorphin and dynorphin have been localized to both enteric neurons and mucosal endocrine cells [11,12,15,19,20]. Combined neuroanatomic and neurophysiologic analyses have shown that opioid peptides are expressed by distinct classes of enteric neurons, notably in myenteric neurons projecting to the circular muscle and in neurons of descending enteric pathways [15,18,20]. Opioid receptors of the μ-, κ- and δ-subtype have been localized to the GI tract of rodents and humans, but their relative distribution varies with GI layer, GI region and species [15,19,20]. In the human gut, μ-opioid receptors are present on myenteric and submucosal neurons and on immune cells in the lamina propria [20].
Fig. 1.
Overview of the gastrointestinal opioid system.
3. Opioid physiology and pharmacology in the gastrointestinal tract
Once released from enteric neurons, opioid peptides modify GI function by interaction with opioid receptors on the enteric circuitries that control motility and secretion. The inhibitory effect of opioid receptor agonists on peristalsis in the guinea pig small intestine is thought to arise primarily from interruption of neuroneuronal and neuroeffector transmission within enteric nerve pathways governing muscle activity [7,14,15,21,22]. Transmission is blocked both via presynaptic and postsynaptic sites of action on enteric neurons, whereby the release and action of transmitters are attenuated [7,12]. Importantly, opioid receptor agonists can interrupt both excitatory and inhibitory neural inputs to GI muscle [7]. Suppression of excitatory pathways inhibits the release of excitatory transmitters such as acetylcholine and blocks distention-induced peristaltic contractions, whereas blockade of inhibitory neural inputs results in depression of nitric oxide release from inhibitory motor neurons, disinhibition of GI muscle activity, elevation of resting muscle tone and nonpropulsive motility patterns [7,12,14,15,23].
The GI motor effects of opioids are complex because, depending on whether interruption of excitatory or inhibitory neural pathways prevails, muscle relaxation or spasm will be observed. In addition, opioids may directly activate the interstitial cell–muscle network [13,15]. As a result, μ-opioid receptor agonists inhibit gastric emptying, increase pyloric muscle tone, induce pyloric and duodenojejunal phasic pressure activity, disturb the migrating myoelectric complex, delay transit through the small and large intestine, and elevate the resting anal sphincter pressure [7,15,19]. The halt in propulsive motility combines with inhibition of GI ion and fluid transport. Through prolonged contact of the intestinal contents with the mucosa and interruption of prosecretory enteric reflexes, opioids attenuate the secretion of electrolytes and water and facilitate the net absorption of fluid [12,15,19,24,25]. The end result of all these effects is constipation.
Opioid receptors belong to the family of metabotropic membrane receptors that couple via the Gi/Go subtypes of G-proteins to cellular transduction processes. Once activated by agonists, μ-opioid receptors undergo endocytosis in a concentration-dependent manner [7,20]. The cellular effects of myenteric μ-opioid receptor activation are brought about by a multiplicity of transduction pathways including activation of potassium channels, membrane hyperpolarization, inhibition of calcium channels and reduced production of cyclic adenosine monophosphate [7]. Studies with isolated tissues from the human intestine show that δ-, κ- and μ-opioid receptors contribute to opioid-induced inhibition of muscle activity [15,19]. Propulsive motility in the rat intestine is blocked by δ- and μ-, but not κ-, opioid receptor agonists [12], whereas peristalsis in the guinea pig intestine is suppressed by activation of κ- and μ-, but not δ-, opioid receptors, much as opioid-induced inhibition of cholinergic transmission in the guinea pig gut is mediated by μ- and κ-opioid receptors [22,26].
Although the available evidence indicates that opioid-induced inhibition of GI transit is mediated by opioid receptors in the gut [15,19], there are experimental data to show that opioids acting within the brain can also influence GI function. For instance, intradural injection of opioid analgesics delays intestinal transit at doses that are considerably lower than equieffective intravenous doses [16]. However, opiate-induced blockade of gut motility correlates better with opiate concentrations in the gut than with opiate concentrations in the brain [27]. In addition, the N-methyl quaternary analogues of naloxone and naltrexone, which do not cross the blood-brain barrier, are able to fully antagonize the effects of morphine in the canine and rat intestine [16,19]. It follows that the adverse influence of opioids on GI function results primarily from interaction with opioid receptors in the gut. This conclusion is backed by the ability of opioid receptor antagonists with a peripherally restricted site of action to prevent the morphine-induced delay of GI transit [15,28,29].
4. Management of diarrhea by direct and indirect opioid receptor agonists
The actions of opioid receptor agonists to inhibit GI secretory activity and transit are therapeutically exploited in acute and chronic diarrhea as well as in irritable bowel syndrome associated with diarrhea [28]. Two therapeutic options are currently available: loperamide and racecadotril. The action of loperamide is predominantly mediated by μ-opioid receptors and restricted to the gut because the drug is poorly absorbed and fails to cross the blood-brain barrier at concentrations needed to produce analgesia [12,16,30]. While the antidiarrheal effect of loperamide arises from direct stimulation of μ-opioid receptors in the gut, racecadotril (acetorphan) inhibits enkephalinases which degrade endogenous opioids once they are released from neurons or other cells in the GI tract. While it does not penetrate the blood-brain barrier, racecadotril prolongs the presence, and increases the concentration, of endogenous opioid peptides at opioid receptors in the alimentary canal [31,32]. In this way the antisecretory and antitransit effects of endogenous opioid peptides are enforced, a result that is therapeutically used for the treatment of diarrhea in children and adults [33,34].
5. The problem of opioid-induced bowel dysfunction
Despite many attempts to develop alternative therapeutics, opioid analgesics remain the mainstay of therapy in many patients with moderate to severe pain. Unfortunately, the use of opioid analgesics is associated with a number of adverse effects among which those on the GI tract are most troublesome in terms of frequency and severity. The traditional approach to treat opioid-induced constipation is laxative comedication, although only about 50% of the patients experience satisfactory relief [19,35,36]. Due to the limited efficacy, rescue treatment requires frequent dose adjustments, combination therapy and laxative switching [19,35,37].
Apart from constipation, OBD comprises incomplete evacuation, abdominal distention, bloating, abdominal discomfort and gastroesophageal reflux [15,19]. In addition, OBD may lead to secondary complications such as pseudoobstruction of the bowel, anorexia, nausea, vomiting and interference with oral drug administration and absorption [19]. The symptoms associated with OBD can profoundly impair the quality of life and in some patients be so severe that they prefer to discontinue analgesic therapy rather than suffer from the discomfort arising from constipation [19]. Unlike other adverse effects of chronic opioid therapy such as sedation, nausea and vomiting, which often resolve with continued use, OBD generally persists throughout treatment [19]. However, tolerance to the effects of morphine on enteric neurons has been found to occur under experimental conditions [7]. Some of the initial gut-related adverse effects of opioid receptor antagonists with a peripherally restricted site of action, such as pain, flatulence and nausea, may also be interpreted as signs of opioid withdrawal.
6. Specific management of opioid-induced bowel dysfunction
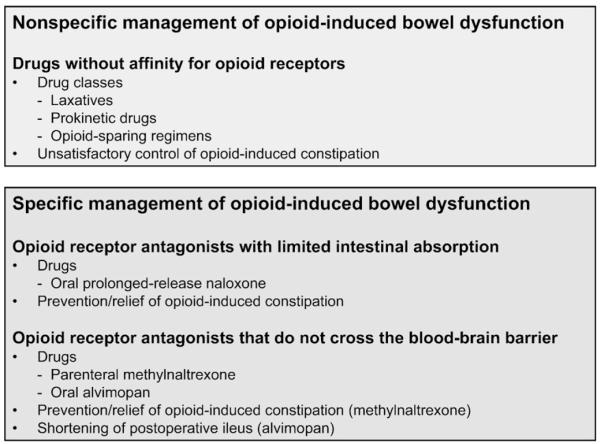
The pharmacologic management of OBD involves two approaches (Fig. 2): nonspecific treatment with laxatives and specific treatment with opioid receptor antagonists [19,35,38]. Since the nonspecific regimens often do not provide satisfactory relief, various opportunities in the specific treatment of OBD have been explored. The primary objective of these approaches is to prevent GI symptoms rather than treat established motor stasis due to opioid use [15,19,29,38]. Apart from attempts to introduce opioid-sparing regimens (Fig. 2), which had only limited success [15,19], the current approach is to selectively target opioid receptors outside the brain to prevent the peripheral adverse effects of opioid analgesics.
Fig. 2.
Nonspecific and specific management of opioid-induced bowel dysfunction.
Since opioid-induced analgesia is primarily mediated by μ-opioid receptors in the central nervous system, the rational approach to prevent OBD would be to combine opioid analgesics with opioid receptor antagonists that cannot penetrate the blood-brain barrier. As a result, the adverse effects of opioid analgesics on the GI system would be suppressed whereas their central analgesic action would be preserved. This strategy has been validated by the use of opioid receptor antagonists with limited systemic absorption such as prolonged-release (PR) naloxone and by the development of peripherally restricted opioid receptor antagonists such as methylnaltrexone and alvimopan [15,19,37–39].
6.1. Opioid receptor antagonists with limited systemic absorption: prolonged-release oral naloxone
The first attempt to selectively target opioid receptors in the periphery was made with naloxone and related tertiary opioid receptor antagonists such as nalmefene [19]. Naloxone is a pan-opioid receptor antagonist whose systemic bioavailability following oral administration is as low as 2% because of extensive first-pass metabolism in the liver [38,40]. Consequently, oral naloxone has been found to reduce constipation but not antinociception caused by morphine in rats [41]. One of the major metabolites of naloxone is naloxone-3-glucuronide which following oral administration to rodents is absorbed to a negligible degree but can counteract opiate-induced inhibition of GI motility [42,43]. A similar profile of action has been found in preclinical studies of nalmefene glucuronide, a metabolite of the μ-opioid receptor antagonist nalmefene [42], but a pilot trial in humans failed to prove a gut-selective action of the compound [44].
Several clinical studies have shown that oral naloxone is able to improve OBD without necessarily compromising opiate-induced analgesia [45–47]. Nevertheless, it need be realized that naloxone can easily cross the blood-brain barrier and hence reverse analgesia if given at sufficient doses [19]. Thus, the therapeutic range of immediate-release naloxone is rather narrow because of the need to titrate peripherally versus centrally active doses [45]. The situation is different, however, with a PR formulation of oral naloxone, which has been found to reduce OBD while preserving the analgesic efficacy of coadministered oxycodone [38].
Specifically, the combination of PR naloxone with PR oxycodone at a weight ratio of 2:1 has been reported to exert significantly less adverse effects on the gut than PR oxycodone alone [47,48]. As revealed in randomized, placebo-controlled trials in patients with moderate to severe chronic pain, increasing doses of PR naloxone were associated with improvements in bowel function, whereas the analgesic efficacy of oxycodone remained unabated [47,48]. A substantial decrease in the use of laxatives was also observed with the PR oxycodone/PR naloxone combination compared with oral PR oxycodone alone [47,48]. In addition, the patients’ assessment of the efficacy of their medication improved with increasing doses of PR naloxone, while the patients’ assessment of tolerability was similar across all treatment groups [49]. In view of these results, a combined formulation of PR naloxone and PR oxycodone has been approved in Europe for the oral treatment/prevention of OBD.
6.2. Peripherally restricted opioid receptor antagonists
Quaternary analogues of opioid receptor antagonists such as naloxone and naltrexone display a pharmacokinetic profile of limited absorption from the gut and inability to enter the brain [19,37]. Thus, intraluminal administration of N-methylnaloxone to an isolated vascularly perfused segment of the rat colon prevents intravascularly administered morphine from depressing motility, although the compound fails to penetrate the intestinal wall to a degree that it can be measured in the vasculature [43]. Similarly, N-methylnaloxone and N-methylnaltrexone attenuate morphine-evoked electrical activity in the canine duodenum at doses that are devoid of effects on the central nervous system [50]. N-methylnaltrexone and another highly polar opioid receptor antagonist, alvimopan, also fail to enter the brain in humans and have a promising potential to relieve OBD in a well-tolerated manner without compromising central analgesia [15,29,37,39,51–54]. Alvimopan and N-methylnaltrexone differ in their opioid receptor subtype selectivity and intrinsic activity on the isolated guinea pig ileum [55]. While N-methylnaltrexone reduces electrically induced contractions and spontaneous activity of the muscle, alvimopan increases these parameters. The action of alvimopan appears to involve both μ- and κ-opioid receptors [55].
6.2.1. Methylnaltrexone
N-methylnaltrexone (in brief methylnaltrexone) is a drug that has greater polarity and lower lipid solubility than naltrexone and, for this reason, exhibits low oral bioavailability due to limited absorption and does not cross the blood-brain barrier [29,37,52,54]. Consequently, this μ-opioid receptor-preferring antagonist (IC50 at human μ-opioid receptors=70 nM) offers the potential to prevent or reverse the undesired effects of opioids in the gut without compromising their therapeutic action in the central nervous system. This claim has been supported by several studies which show that, following parenteral administration of methylnaltrexone together with a centrally active opiate, the adverse effect of the opiate on GI function is prevented without a change of analgesia in dogs and humans, whereas in rats analgesia is appreciably attenuated [29,37,52,54]. This species-related difference in the peripheral selectivity of methylnaltrexone arises from its demethylation to naltrexone which readily penetrates the blood-brain barrier; demethylation occurs in mice and rats but is negligible in dogs and humans [56].
Methylnaltrexone has been formulated for intravenous, subcutaneous and oral administration and its pharmacodynamic, pharmacokinetic, therapeutic and safety profile evaluated in clinical trials [29,37,52,54,57]. Both the parenteral and oral formulations have been found efficacious in preventing the opioid-induced prolongation of gastric emptying and orocecal transit time in healthy volunteers [29,37,52,54]. It is noteworthy that methylnaltrexone is also able to ameliorate opioid-induced urinary retention [58].
The therapeutic efficacy of methylnaltrexone was first proved by the drug’s ability to relieve constipation in methadone-maintained, opioid-dependent volunteers without eliciting opioid withdrawal [59]. Two phase III trials of subcutaneous methylnaltrexone in patients with endstage diseases suffering from opioid-induced constipation revealed that methylnaltrexone is superior to placebo in causing laxation within 4 h after injection of a single drug dose [60,61]. When methylnaltrexone (0.15–0.30 mg/kg) was administered repeatedly every other day for two weeks, laxation was triggered in about 50% of the patients, compared with 8–15% of patients receiving placebo [61]. This response rate remained constant for more than 3 months [61]. The observation that only about 50% of the patients benefit from methylnaltrexone prompts the conjecture that part of the OBD occurring in patients with advanced illness is mediated through a central action of opioid analgesics.
Methylnaltrexone has been approved by the US Food and Drug Administration and the European Medicines Agency for the management of opioid-induced constipation in patients on palliative care for endstage disease, who receive opioid analgesics and do not appropriately respond to laxative therapy [29]. Since the long-term safety and tolerability of the drug has not yet been evaluated, the duration of methylnaltrexone therapy is limited to 4 months.
Another indication in which intravenous methylnaltrexone has been evaluated in clinical trials is postoperative ileus [29,52,54,62]. This condition is thought to involve activation of opioid mechanisms in the gut and to be exacerbated by postoperative therapy with opioid analgesics [63,64]. Patients undergoing open segmental colectomy were reported to benefit from treatment with methylnaltrexone, inasmuch as upper and lower bowel function recovered approximately 1 day earlier than in placebo-treated patients, whereas no difference in opioid use or mean pain scores was observed [52,62]. However, two subsequent phase III trials showed that methylnaltrexone was not better than placebo in shortening postoperative ileus [29,62].
At therapeutic doses (0.3–0.45 mg/kg intravenously and up to 19.2 mg/kg per os) methylnaltrexone is well tolerated, an outcome that is also true when methylnaltrexone is repeatedly administered [57]. Thus far, only two types of adverse reactions have been reported. One of them relates to the vascular system, given that transient orthostatic hypotension can occur at supratherapeutic doses [29,37,52,54]. This reaction may be related to facial flushing and mild light-headedness, symptoms that have occasionally been reported [54]. The other type of adverse effect comprises gut-related reactions such as abdominal cramps, flatulence and nausea [29,52,54,57,59].
6.2.2. Alvimopan
Alvimopan is a μ-opioid receptor-preferring antagonist with a peripherally restricted site of action and a potency (IC50 at human μ-opioid receptors=0.77 nM) considerably higher than that of methynaltrexone. Given its polar structure, alvimopan exhibits both low systemic absorption (oral bioavailability of 0.03% in dogs and 6% in humans) and a limited ability to enter the brain [15,28,37,51,53,65]. Since it is rapidly degraded after intravenous injection, alvimopan is formulated for oral intake, in which case it potently blocks μ-opioid receptors in the gut with a prolonged duration of action. Several studies have established the pharmacokinetics, safety, efficacy and selectivity of alvimopan in its antagonism of peripheral opioid receptors [15,19,28,37,51,53,60,65,66].
In patients on chronic opioid therapy for nonmalignant pain or opioid addiction, alvimopan (0.5 or 1 mg once daily for 21 days) was able to ameliorate constipation without attenuating opioid analgesia [66]. These observations were extended in a phase III trial involving more than 500 subjects taking opioids for non-cancer pain [67]. Alvimopan (0.5 or 1 mg twice daily for 6 weeks) increased spontaneous bowel movements during the initial 3 weeks of treatment and improved other symptoms of OBD (straining, stool consistency, incomplete evacuation, abdominal bloating and discomfort and decreased appetite) over the whole treatment period, while analgesia was not compromised [67].
Since opioid mechanisms and OBD are thought to contribute to postoperative ileus [19,63,64], several clinical trials have examined the ability of alvimopan to improve postoperative bowel function [15,19,37,39,51,53,68,69]. Four phase III trials conducted in North America showed that alvimopan (6 or 12 mg twice daily) accelerates GI recovery and shortens the duration of hospitalization after abdominal or pelvic surgery, whereas an international phase III trial failed to reveal a significant effect of alvimopan on postoperative ileus unless subjects were maintained on intravenous patient-controlled opioid analgesia [15,29,53,68–70]. The variability in the efficacy of alvimopan may be due to differences in dosage and pharmacokinetics, given that the rate of alvimopan absorption is slowed in surgical patients, relative to healthy controls [71]. Alvimopan has been approved by the US Food and Drug Administration for the short-term treatment of postoperative ileus following bowel resection in hospitalized patients aged 18 years or older. The recommended dosing is 12 mg just before surgery, and 12 mg twice daily post-surgery for up to 7 days [29].
Following acute or short-term (3–6 weeks) administration to patients with OBD alvimopan is well tolerated, the adverse effects being primarily bowel-related and including nausea, vomiting and abdominal discomfort [28,66,67]. However, the long-term safety of alvimopan remains to be established, given that a one-year phase III trial of patients on opiate therapy for chronic non-cancer pain revealed a numerical imbalance in the number of ischemic cardiovascular events, neoplasms and fractures in patients on alvimopan (0.5 mg perorally twice daily), relative to placebo [29,53]. A two-year carcinogenicity study in mice and rats showed that oral alvimopan significantly increased the incidence of cutaneous/subcutaneous fibroma, fibrosarcoma and sarcoma and of osteoma/osteosarcoma in female mice [29].
7. Opioid receptor antagonists as potential prokinetics
Endogenous opioid peptides are thought to play a role in the fine tuning of digestion [11,13,15]. Thus, distention-evoked peristalsis can be facilitated by naloxone in various preparations of the guinea pig, rabbit, cat and rat isolated small intestine [12,14,26]. In the guinea pig small intestine, the effect of naloxone is mimicked by selective antagonists at μ- and κ-opioid receptors, but not by antagonism at δ-opioid receptors [26]. It follows that endogenous opioid peptides released in the course of propulsive motility participate in the neural control of peristalsis as they dampen peristaltic performance via activation of μ- and κ-opioid receptors [15,26]. Naloxone has been found to accelerate transit in the colon but not small intestine of healthy human volunteers, this effect being shared by the μ-opioid receptor-preferring antagonists methylnaltrexone and alvimopan [57,72]. Thus, peripherally restricted opioid receptor antagonists have the potential to act as prokinetics and to alleviate intestinal motor stasis unrelated to opiate use, such as chronic idiopathic constipation and intestinal pseudoobstruction [13,15,28,52].
There is emerging evidence that pathologic GI motor inhibition is associated with upregulation and/or overactivity of the opioid system in the alimentary canal. For instance, experimental inflammation enhances the potency of μ-opioid receptor agonists to inhibit GI transit and enhances the expression of μ-opioid receptors in the intestine of mice [73,74]. Abdominal surgery leads to an increase in the circulating levels of endomorphin in humans [75] and causes internalization of μ-opioid receptors in the myenteric plexus of the guinea pig intestine [20]. These observations reflect a role of endogenous opioids in the pathophysiology of postoperative motor disturbances. In keeping with this concept, there is a limited number of small studies showing that naloxone can reverse idiopathic chronic constipation and have beneficial effects in patients with intestinal pseudoobstruction and constipation-predominant irritable bowel syndrome [15,37]. Peripherally restricted opioid receptor antagonists may hence be able to normalize pathologic inhibition of gut function that arises from an upregulation and/or overactivity of the opioid system in the GI tract [13,15].
8. Conclusions
Although its implications have not yet been disclosed in full detail, the GI opioid system is involved in the regulation of motor and secretory activity. While stimulation of GI opioid receptors by loperamide or racecadotril can be exploited to stop diarrhea, constipation is one of the most frequent and troublesome adverse effects of opioid analgesics. The development of opioid receptor antagonists with restricted access to the central nervous system has opened up a new avenue to selectively prevent the undesired effects of opioid analgesics outside the central nervous system. This concept has been validated by the clinical efficacy of PR oral naloxone, parenteral methylnaltrexone and oral alvimopan. In addition, peripherally restricted opioid receptor antagonists have the potential to act as prokinetic drugs.
Acknowledgements
Work in the author’s laboratory is supported by FWF – The Austrian Scientific Research Funds, the Austrian Federal Ministry of Science and Research, and the Zukunftsfonds Steiermark.
References
- [1].Holzer P, Lembeck F. Analgesia up to the twentieth century. In: Parnham MJ, Bruinvels, editors. Discoveries in Pharmacology. Psycho- and Neuro-pharmacology. Elsevier; Amsterdam: 1983. pp. 357–77. [Google Scholar]
- [2].Hamilton GR, Baskett TF. In the arms of Morpheus: the development of morphine for postoperative pain relief. Can J Anaesth. 2000;47:367–74. doi: 10.1007/BF03020955. [DOI] [PubMed] [Google Scholar]
- [3].Lammers WJ, Lammers-van den Berg AM, Morrison JF, Petroianu GA. Translating Trendelenburg; back to the future. Naunyn Schmiedebergs Arch Pharmacol. 2006;373:134–8. doi: 10.1007/s00210-006-0051-8. [DOI] [PubMed] [Google Scholar]
- [4].Trendelenburg P. Physiological and pharmacological investigations of small intestinal peristalsis. Arch Exp Pathol Pharmakol. 1917;81:55–129. doi: 10.1007/s00210-006-0052-7. [Translation of the article “Physiologische und pharmakologische Versuche über die Dünndarmperistaltik”] [DOI] [PubMed] [Google Scholar]; Naunyn-Schmiedeberg’s Arch Pharmacol. 1917;373:101–33. doi: 10.1007/s00210-006-0052-7. [DOI] [PubMed] [Google Scholar]
- [5].Schaumann O. Pain, the protective system and combinations with morphine-like effect. Wien Med Wschr. 1959;109:78–81. [PubMed] [Google Scholar]
- [6].Paton WDM. The action of morphine and related substances on contraction and on acetylcholine output of coaxially stimulated guinea-pig ileum. Br J Pharmacol. 1957;11:119–27. doi: 10.1111/j.1476-5381.1957.tb01373.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Wood JD, Galligan JJ. Function of opioids in the enteric nervous system. Neurogastroenterol Motil. 2004;16(Suppl 2):17–28. doi: 10.1111/j.1743-3150.2004.00554.x. [DOI] [PubMed] [Google Scholar]
- [8].Snyder SH. Opiate receptors in normal and drug-altered brain function. Nature. 1975;257:185–9. [Google Scholar]
- [9].Hughes J, Smith TW, Kosterlitz HW, Fothergill LA, Morgan BA, Morris HR. Identification of two related pentapeptides from the brain with potent opiate agonist activity. Nature. 1975;258:577–80. doi: 10.1038/258577a0. [DOI] [PubMed] [Google Scholar]
- [10].Hughes J, Kosterlitz HW, Smith TW. The distribution of methionine-enkephalin and leucine-enkephalin in the brain and peripheral tissues. Br J Pharmacol. 1977;61:639–47. doi: 10.1111/j.1476-5381.1977.tb07557.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kromer W. Endogenous and exogenous opioids in the control of gastrointestinal motility and secretion. Pharmacol Rev. 1988;40:121–62. [PubMed] [Google Scholar]
- [12].De Luca A, Coupar IM. Insights into opioid action in the intestinal tract. Pharmacol Ther. 1996;69:103–15. doi: 10.1016/0163-7258(95)02053-5. [DOI] [PubMed] [Google Scholar]
- [13].Holzer P. Opioids and opioid receptors in the enteric nervous system: from a problem in opioid analgesia to a possible new prokinetic therapy in humans. Neurosci Lett. 2004;361:92–5. doi: 10.1016/j.neulet.2003.12.004. [DOI] [PubMed] [Google Scholar]
- [14].Sanger GJ, Tuladhar BR. The role of endogenous opiates in the control of gastrointestinal motility: predictions from in vitro modelling. Neurogastroenterol Motil. 2004;16(Suppl 2):38–45. doi: 10.1111/j.1743-3150.2004.00556.x. [DOI] [PubMed] [Google Scholar]
- [15].Holzer P. Treatment of opioid-induced gut dysfunction. Expert Opin Investig Drugs. 2007;16:181–94. doi: 10.1517/13543784.16.2.181. [DOI] [PubMed] [Google Scholar]
- [16].Manara L, Bianchetti A. The central and peripheral influences of opioids on gastrointestinal propulsion. Annu Rev Pharmacol Toxicol. 1985;25:249–73. doi: 10.1146/annurev.pa.25.040185.001341. [DOI] [PubMed] [Google Scholar]
- [17].Holzer P, Schicho R, Holzer-Petsche U, Lippe IT. The gut as a neurological organ. Wien Klin Wochenschr. 2001;113:647–60. [PubMed] [Google Scholar]
- [18].Furness JB. The enteric nervous system. Blackwell; Oxford: 2006. [Google Scholar]
- [19].Kurz A, Sessler DI. Opioid-induced bowel dysfunction: pathophysiology and potential new therapies. Drugs. 2003;63:649–71. doi: 10.2165/00003495-200363070-00003. [DOI] [PubMed] [Google Scholar]
- [20].Sternini C, Patierno S, Selmer IS, Kirchgessner A. The opioid system in the gastrointestinal tract. Neurogastroenterol Motil. 2004;16(Suppl 2):3–16. doi: 10.1111/j.1743-3150.2004.00553.x. [DOI] [PubMed] [Google Scholar]
- [21].Tonini M, Waterman SA, Candura SM, Coccini T, Costa M. Sites of action of morphine on the ascending excitatory reflex in the guinea-pig small intestine. Neurosci Lett. 1992;144:195–8. doi: 10.1016/0304-3940(92)90748-v. [DOI] [PubMed] [Google Scholar]
- [22].Waterman SA, Costa M, Tonini M. Modulation of peristalsis in the guinea-pig isolated small intestine by exogenous and endogenous opioids. Br J Pharmacol. 1992;106:1004–10. doi: 10.1111/j.1476-5381.1992.tb14448.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Lenard L, Halmai V, Barthó L. Morphine contracts the guinea pig ileal circular muscle by interfering with a nitric oxide mediated tonic inhibition. Digestion. 1999;60:562–6. doi: 10.1159/000007707. [DOI] [PubMed] [Google Scholar]
- [24].Beubler E, Lembeck F. Inhibition of stimulated fluid secretion in the rat small and large intestine by opiate agonists. Naunyn-Schmiedeberg’s Arch Pharmacol. 1979;306:113–8. doi: 10.1007/BF00498980. [DOI] [PubMed] [Google Scholar]
- [25].Turnberg LA. Antisecretory activity of opiates in vitro and in vivo in man. Scand J Gastroenterol. 1983;84:79–83. [PubMed] [Google Scholar]
- [26].Shahbazian A, Heinemann A, Schmidhammer H, Beubler E, Holzer-Petsche U, Holzer P. Involvement of μ- and κ-, but not δ-, opioid receptors in the peristaltic motor depression caused by endogenous and exogenous opioids in the guinea-pig intestine. Br J Pharmacol. 2002;135:741–50. doi: 10.1038/sj.bjp.0704527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Bianchi G, Ferretti P, Recchia M, Rocchetti M, Tavani A, Manara L. Morphine tissue levels and reduction of gastrointestinal transit in rats. Correlation supports primary action site in the gut. Gastroenterology. 1983;85:852–8. [PubMed] [Google Scholar]
- [28].Camilleri M. Alvimopan, a selective peripherally acting μ-opioid antagonist. Neurogastroenterol Motil. 2004;17:157–65. doi: 10.1111/j.1365-2982.2005.00640.x. [DOI] [PubMed] [Google Scholar]
- [29].Holzer P. Methylnaltrexone for the management of unwanted peripheral opioid effects. Therapy. 2008;5:531–43. [Google Scholar]
- [30].Stacher G, Steinringer H, Schneider C, Vacariu-Granser GV, Castiglione F, Gaupmann G, Weber U, Stacher-Janotta G. Effects of the prodrug loperamide oxide, loperamide, and placebo on jejunal motor activity. Dig Dis Sci. 1992;37:198–204. doi: 10.1007/BF01308172. [DOI] [PubMed] [Google Scholar]
- [31].Matheson AJ, Noble S. Racecadotril. Drugs. 2000;59:829–35. doi: 10.2165/00003495-200059040-00010. [DOI] [PubMed] [Google Scholar]
- [32].Schwartz JC. Racecadotril: a new approach to the treatment of diarrhoea. Int J Antimicrob Agents. 2000;14:75–9. doi: 10.1016/s0924-8579(99)00151-x. [DOI] [PubMed] [Google Scholar]
- [33].Salazar-Lindo E, Santisteban-Ponce J, Chea-Woo E, Gutierrez M. Racecadotril in the treatment of acute watery diarrhea in children. New Engl J Med. 2000;343:463–7. doi: 10.1056/NEJM200008173430703. [DOI] [PubMed] [Google Scholar]
- [34].Prado D. Global Adult Racecadotril Study Group. A multinational comparison of racecadotril and loperamide in the treatment of acute watery diarrhoea in adults. Scand J Gastroenterol. 2002;37:656–61. doi: 10.1080/00365520212495. [DOI] [PubMed] [Google Scholar]
- [35].Herndon CM, Jackson KC, Hallin PA. Management of opioid-induced gastrointestinal effects in patients receiving palliative care. Pharmacotherapy. 2002;22:240–50. doi: 10.1592/phco.22.3.240.33552. [DOI] [PubMed] [Google Scholar]
- [36].Liu M, Wittbrodt E. Low-dose oral naloxone reverses opioid-induced constipation and analgesia. J Pain Symptom Manage. 2002;23:48–53. doi: 10.1016/s0885-3924(01)00369-4. [DOI] [PubMed] [Google Scholar]
- [37].DeHaven-Hudkins DL, DeHaven RN, Little PJ, Techner LM. The involvement of the μ-opioid receptor in gastrointestinal pathophysiology: therapeutic opportunities for antagonism at this receptor. Pharmacol Ther. 2008;117:162–87. doi: 10.1016/j.pharmthera.2007.09.007. [DOI] [PubMed] [Google Scholar]
- [38].Reimer K, Hopp M, Zenz M, Maier C, Holzer P, Mikus G, Bosse B, Smith K, Buschmann-Kramm C, Leyendecker P. Meeting the challenges of opioid-induced constipation in chronic pain management – a novel approach. Pharmacology. 2009;83:10–7. doi: 10.1159/000165778. [DOI] [PubMed] [Google Scholar]
- [39].Becker G, Galandi D, Blum HE. Peripherally acting opioid antagonists in the treatment of opiate-related constipation: a systematic review. J Pain Symptom Manage. 2007;34:547–65. doi: 10.1016/j.jpainsymman.2006.12.018. [DOI] [PubMed] [Google Scholar]
- [40].Greenwood-Van Meerveld B, Gardner CJ, Little PJ, Hicks GA, DeHaven-Hudkins DL. Preclinical studies of opioids and opioid antagonists on gastrointestinal function. Neurogastroenterol Motil. 2004;16(Suppl 2):46–53. doi: 10.1111/j.1743-3150.2004.00555.x. [DOI] [PubMed] [Google Scholar]
- [41].Jurna I, Kaiser R, Kretz O, Baldauf J. Oral naloxone reduces constipation but not antinociception from oral morphine in the rat. Neurosci Lett. 1992;142:62–4. doi: 10.1016/0304-3940(92)90620-m. [DOI] [PubMed] [Google Scholar]
- [42].Simpkins JW, Smulkowski M, Dixon R, Tuttle R. Evidence for the delivery of narcotic antagonists to the colon as their glucuronide conjugates. J Pharmacol Exp Ther. 1988;244:195–205. [PubMed] [Google Scholar]
- [43].Reber P, Brenneisen R, Flogerzi B, Batista C, Netzer P, Scheurer U. Effect of naloxone-3-glucuronide and N-methylnaloxone on the motility of the isolated rat colon after morphine. Dig Dis Sci. 2007;52:502–7. doi: 10.1007/s10620-006-9563-9. [DOI] [PubMed] [Google Scholar]
- [44].Cheskin LJ, Chami TN, Johnson RE, Jaffe JH. Assessment of nalmefene glucuronide as a selective gut opioid antagonist. Drug Alcohol Depend. 1995;39:151–4. doi: 10.1016/0376-8716(95)01153-p. [DOI] [PubMed] [Google Scholar]
- [45].Sykes NP. An investigation of the ability of oral naloxone to correct opioid-related constipation in patients with advanced cancer. Palliat Med. 1996;10:135–44. doi: 10.1177/026921639601000208. [DOI] [PubMed] [Google Scholar]
- [46].Meissner W, Schmidt U, Hartmann M, Kath R, Reinhart K. Oral naloxone reverses opioid-associated constipation. Pain. 2000;84:105–9. doi: 10.1016/S0304-3959(99)00185-2. [DOI] [PubMed] [Google Scholar]
- [47].Meissner W, Leyendecker P, Mueller-Lissner S, Nadstawek J, Hopp M, Ruckes C, Wirz S, Fleischer W, Reimer K. A randomised controlled trial with prolonged-release oral oxycodone and naloxone to prevent and reverse opioid-induced constipation. Eur J Pain. 2009;13:56–64. doi: 10.1016/j.ejpain.2008.06.012. [DOI] [PubMed] [Google Scholar]
- [48].Vondrackova D, Leyendecker P, Meissner W, Hopp M, Szombati I, Hermanns K, Ruckes C, Weber S, Grothe B, Fleischer W, Reimer K. Analgesic efficacy and safety of oxycodone in combination with naloxone as prolonged release tablets in patients with moderate to severe chronic pain. J Pain. 2008;9:1144–54. doi: 10.1016/j.jpain.2008.06.014. [DOI] [PubMed] [Google Scholar]
- [49].Nadstawek J, Leyendecker P, Hopp M, Wirz S, Ruckes C, Fleischer W, Reimer K. Patient assessment of a novel therapeutic approach for the treatment of severe, chronic pain. Int J Clin Pract. 2008;62:1159–67. doi: 10.1111/j.1742-1241.2008.01820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Russell J, Bass P, Goldberg LI, Schuster CR, Merz H. Antagonism of gut, but not central effects of morphine with quaternary narcotic antagonists. Eur J Pharmacol. 1982;78:255–61. doi: 10.1016/0014-2999(82)90026-7. [DOI] [PubMed] [Google Scholar]
- [51].Neary P, Delaney CP. Alvimopan. Expert Opin Investig Drugs. 2005;14:479–88. doi: 10.1517/13543784.14.4.479. [DOI] [PubMed] [Google Scholar]
- [52].Yuan CS, Israel RJ. Methylnaltrexone, a novel peripheral opioid receptor antagonist for the treatment of opioid side effects. Expert Opin Investig Drugs. 2006;15:541–52. doi: 10.1517/13543784.15.5.541. [DOI] [PubMed] [Google Scholar]
- [53].Leslie JB. Alvimopan: a peripherally acting μ-opioid receptor antagonist. Drugs Today (Barc) 2007;43:611–25. doi: 10.1358/dot.2007.43.9.1086176. [DOI] [PubMed] [Google Scholar]
- [54].Reichle FM, Conzen PF. Methylnaltrexone, a new peripheral μ-receptor antagonist for the prevention and treatment of opioid-induced extracerebral side effects. Curr Opin Investig Drugs. 2008;9:90–100. [PubMed] [Google Scholar]
- [55].Beattie DT, Cheruvu M, Mai N, O’Keefe M, Johnson-Rabidoux S, Peterson C, Kaufman E, Vickery R. The in vitro pharmacology of the peripherally restricted opioid receptor antagonists, alvimopan, ADL 08-0011 and methylnaltrexone. Naunyn-Schmiedeberg’s Arch Pharmacol. 2007;375:205–20. doi: 10.1007/s00210-007-0146-x. [DOI] [PubMed] [Google Scholar]
- [56].Kotake AN, Kuwahara SK, Burton E, McCoy CE, Goldberg LI. Variations in demethylation of N-methylnaltrexone in mice, rats, dogs, and humans. Xenobiotica. 1989;19:1247–54. doi: 10.3109/00498258909043176. [DOI] [PubMed] [Google Scholar]
- [57].Yuan CS, Doshan H, Charney MR, O’Connor M, Karrison T, Maleckar SA, Israel RJ, Moss J. Tolerability, gut effects, and pharmacokinetics of methylnaltrexone following repeated intravenous administration in humans. J Clin Pharmacol. 2005;45:538–46. doi: 10.1177/0091270004273491. [DOI] [PubMed] [Google Scholar]
- [58].Rosow CE, Gomery P, Chen TY, Stefanovich P, Stambler N, Israel R. Reversal of opioid-induced bladder dysfunction by intravenous naloxone and methylnaltrexone. Clin Pharmacol Ther. 2007;82:48–53. doi: 10.1038/sj.clpt.6100164. [DOI] [PubMed] [Google Scholar]
- [59].Yuan CS, Foss JF, O’Connor M, Osinski J, Karrison T, Moss J, Roizen MF. Methylnaltrexone for reversal of constipation due to chronic methadone use: a randomized, controlled trial. J Am Med Assoc. 2000;283:367–72. doi: 10.1001/jama.283.3.367. [DOI] [PubMed] [Google Scholar]
- [60].Portenoy RK, Thomas J, Boatwright ML Moehl, Tran D, Galasso FL, Stambler N, Von Gunten CF, Israel RJ. Subcutaneous methylnaltrexone for the treatment of opioid-induced constipation in patients with advanced illness: a double-blind, randomized, parallel group, dose-ranging study. J Pain Symptom Manage. 2008;35:458–68. doi: 10.1016/j.jpainsymman.2007.12.005. [DOI] [PubMed] [Google Scholar]
- [61].Thomas J, Karver S, Cooney G Austin, Chamberlain BH, Watt CK, Slatkin NE, Stambler N, Kremer AB, Israel RJ. Methylnaltrexone for opioid-induced constipation in advanced illness. N Engl J Med. 2008;358:2332–43. doi: 10.1056/NEJMoa0707377. [DOI] [PubMed] [Google Scholar]
- [62].Kraft MD. Methylnaltrexone, a new peripherally acting μ-opioid receptor antagonist being evaluated for the treatment of postoperative ileus. Expert Opin Investig Drugs. 2008;17:1365–77. doi: 10.1517/13543784.17.9.1365. [DOI] [PubMed] [Google Scholar]
- [63].Fukuda H, Suenaga K, Tsuchida D, Mantyh CR, Pappas TN, Hicks GA, DeHaven-Hudkins DL, Takahashi T. The selective μ opioid receptor antagonist, alvimopan, improves delayed GI transit of postoperative ileus in rats. Brain Res. 2006;1102:63–70. doi: 10.1016/j.brainres.2006.02.092. [DOI] [PubMed] [Google Scholar]
- [64].Schmidt J, Stoffels B, Nazir A, Dehaven-Hudkins DL, Bauer AJ. Alvimopan and COX-2 inhibition reverse opioid and inflammatory components of postoperative ileus. Neurogastroenterol Motil. 2008;20:689–99. doi: 10.1111/j.1365-2982.2007.01078.x. [DOI] [PubMed] [Google Scholar]
- [65].Schmidt WK. Alvimopan (ADL 8-2698) is a novel peripheral opioid antagonist. Am J Surg. 2001;182(Suppl):27S–38S. doi: 10.1016/s0002-9610(01)00784-x. [DOI] [PubMed] [Google Scholar]
- [66].Paulson DM, Kennedy DT, Donovick RA, Carpenter RL, Cherubini M, Techner L, Du W, Ma Y, Schmidt WK, Wallin B, Jackson D. Alvimopan: an oral, peripherally acting, μ-opioid receptor antagonist for the treatment of opioid-induced bowel dysfunction – a 21-day treatment-randomized clinical trial. J Pain. 2005;6:184–92. doi: 10.1016/j.jpain.2004.12.001. [DOI] [PubMed] [Google Scholar]
- [67].Webster L, Jansen JP, Peppin J, Lasko B, Irving G, Morlion B, Snidow J, Pierce A, Mortensen E, Kleoudis C, Carter E. Alvimopan, a peripherally acting μ-opioid receptor (PAM-OR) antagonist for the treatment of opioid-induced bowel dysfunction: results from a randomized, double-blind, placebo-controlled, dose-finding study in subjects taking opioids for chronic non-cancer pain. Pain. 2008;137:428–40. doi: 10.1016/j.pain.2007.11.008. [DOI] [PubMed] [Google Scholar]
- [68].Delaney CP, Wolff BG, Viscusi ER, Senagore AJ, Fort JG, Du W, Techner L, Wallin B. Alvimopan, for postoperative ileus following bowel resection: a pooled analysis of phase III studies. Ann Surg. 2007;245:355–63. doi: 10.1097/01.sla.0000232538.72458.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Tan EK, Cornish J, Darzi AW, Tekkis PP. Meta-analysis: alvimopan vs. placebo in the treatment of post-operative ileus. Aliment Pharmacol Ther. 2007;25:47–57. doi: 10.1111/j.1365-2036.2006.03150.x. [DOI] [PubMed] [Google Scholar]
- [70].Büchler MW, Seiler CM, Monson JR, Flamant Y, Thompson-Fawcett MW, Byrne MM, Mortensen ER, Altman JF, Williamson R. Clinical trial: alvimopan for the management of postoperative ileus after abdominal surgery: results of an international randomised, double-blind, multicentre, placebo-controlled clinical study. Aliment Pharmacol Ther. 2008;28:312–25. doi: 10.1111/j.1365-2036.2008.03696.x. [DOI] [PubMed] [Google Scholar]
- [71].Foss JF, Fisher DM, Schmith VD. Pharmacokinetics of alvimopan and its metabolite in healthy volunteers and patients in postoperative ileus trials. Clin Pharmacol Ther. 2008;83:770–6. doi: 10.1038/sj.clpt.6100292. [DOI] [PubMed] [Google Scholar]
- [72].Gonenne J, Camilleri M, Ferber I, Burton D, Baxter K, Keyashian K, Foss J, Wallin B, Du W, Zinsmeister AR. Effect of alvimopan and codeine on gastrointestinal transit: a randomized controlled study. Clin Gastroenterol Hepatol. 2005;3:784–91. doi: 10.1016/s1542-3565(05)00434-9. [DOI] [PubMed] [Google Scholar]
- [73].Puig MM, Pol O. Peripheral effects of opioids in a model of chronic intestinal inflammation in mice. J Pharmacol Exp Ther. 1998;287:1068–75. [PubMed] [Google Scholar]
- [74].Pol O, Alameda F, Puig MM. Inflammation enhances μ-opioid receptor transcription and expression in mice intestine. Mol Pharmacol. 2001;60:894–9. doi: 10.1124/mol.60.5.894. [DOI] [PubMed] [Google Scholar]
- [75].Yoshida S, Ohta J, Yamasaki K, Kamei H, Harada Y, Yahara T, Kaibara A, Ozaki K, Tajiri T, Shirouzu K. Effect of surgical stress on endogenous morphine and cytokine levels in the plasma after laparoscopoic or open cholecystectomy. Surg Endosc. 2000;14:137–40. doi: 10.1007/s004649900085. [DOI] [PubMed] [Google Scholar]