SUMMARY
Background
Umbilical cord blood (UCB) is increasingly considered as an alternative to peripheral blood progenitor cells (PBPC) or bone marrow (BM), especially when a HLA-matched adult unrelated donor is not available.
Methods
In order to establish the appropriateness of current graft selection practices, we retrospectively compared leukemia-free survival and other outcomes for each graft source in patients aged >16 years transplanted for acute leukemia using Cox regression. Data were available on 1525 patients transplanted between 2002 and 2006 using UCB (n=165), PBPC (n=888) and BM (n=472). UCB units were matched at HLA-A and B at antigen level and DRB1 at allele level (n=10) or mismatched at one (n=40) or two antigens (n=115). PBPC and BM grafts from unrelated adult donors were matched for allele-level HLA-A, B, C and DRB1 (n=632; n=332) or mismatched at one locus (n=256; n=140).
Findings
Leukemia-free survival after UCB transplantation was comparable to that observed after 8/8 and 7/8 allele-matched PBPC or BM transplantation. Transplant-related mortality, however, was higher after UCB transplantation compared to 8/8 allele-matched PBPC (HR 1.62, p<0.01) or BM (HR 1.69, p<0.01). Grades 2–4 acute and chronic graft-versus-host disease were lower in UCB recipients compared to allele-matched PBPC (HR 0.57, p<0.01 and HR 0.38, p<0.01, respectively), while chronic and not acute graft-versus-host disease was lower after UCB compared to allele-matched BM transplantation (HR 0.63, p=0.01).
Interpretation
Together, these data support the use of UCB for adults with acute leukemia when an HLA-matched unrelated adult donor is lacking and when transplant is urgently needed.
INTRODUCTION
Treatment of high-risk acute leukemia by allogeneic hematopoietic stem cell (HSC) transplantation is an accepted therapeutic strategy. However, lack of HLA compatible sibling donors is a major factor that limits its application in approximately 70% of patients who could otherwise benefit from this treatment. An unrelated HLA matched adult donor is generally considered to be the next best alternative if an HLA matched sibling is not available.1 HSC may be harvested from bone marrow or, after stimulation of the donor with hematopoietic growth factors, from peripheral blood. Over the past decade peripheral blood progenitor cells (PBPC) has surpassed the use of bone marrow (BM) as the preferred source of allogeneic HSC for adults. Worldwide PBPC collections from unrelated donors numbered 7260 (69%) and BM collections 3221 (31%) in 2008.2
As of 2008, over 14 million potential unrelated adult donors were registered with the unrelated donor registries worldwide.2 Still, only approximately 50% of patients of Caucasian descent will have an available and fully HLA matched unrelated adult donor; the probability is lower for non-Caucasians. Additionally, the search and procurement process for adult donors can take weeks to months. Consequently, UCB is increasingly attractive as an alternative to HLA-matched PBPC or BM.2,3
Numerous studies have clearly established the limitations and advantages of UCB, particularly in children.4–7 We previously performed a comparative analysis of UCB and BM in children with acute leukemia. In that study, we demonstrated that 4-6/6 HLA-matched UCB (HLA-A and -B matching at intermediate resolution and -DRB1 matching at allele-level) provided a similar probability of leukemia-free survival (LFS) relative to matched BM (HLA-A, -B, -C, -DRB1 matched at allele-level).7 As a result, we concluded that there was no reason to delay transplantation if a 4-6/6 HLA-matched UCB unit with an adequate cell dose was available, especially if an allele-matched unrelated adult donor could not be readily identified. The logical next question was to perform a similar analysis in adults with acute leukemia. While several prior reports have compared outcomes after UCB and BM in adults,8,9 these studies were based on less rigorous historical rather than current donor selection practices. Specifically, adult donors are now selected based on HLA matching using allele level typing at HLA-A, -B, -C and -DRB110 and a cell dose threshold of 2.5 × 107 total nucleated cells/kilogram recipient body weight is considered a standard for UCB grafts. The findings of these early reports differed in that one showed higher transplant-related mortality (TRM) and lower LFS after UCB compared to matched BM transplants8 and the other9 similar TRM and LFS after UCB and matched BM transplants. Further, these studies did not compare UCB with PBPC transplants. In the absence of a prospective clinical trial which would be logistically challenging, we used data reported to the Center for International Blood and Marrow Transplant Research (CIBMTR), the European Group for Blood and Marrow Transplantation (EBMT), the Eurocord-Netcord Registry and the National Cord Blood Program (NCBP) at the New York Blood Center for adults with acute leukemia who were transplanted with unrelated donor BM, PBPC or UCB. By evaluating LFS and other transplant outcomes for UCB relative to 8/8 HLA-matched BM or PBPC as the “gold standard” we sought to determine the optimal role of UCB grafts in transplantation for adults with acute leukemia. The results of this analysis could have profound effects on current donor selection practices and future research directions for overcoming identified obstacles.
METHODS
Collection of data
Data on transplantations in the United States were obtained from the CIBMTR (all HSC sources) and the NCBP (UCB only). Data on transplants in Europe were obtained from the Acute Leukemia Working Party of the EBMT (BM and PBPC) and the Eurocord-Netcord registry (UCB only). Two hundred and sixteen transplant centers contributed patients. UCB transplants were done at 76 transplant centers (with 73 centers contributing 1–5 patients). UCB transplants were distributed fairly equally over the 5 year period; 55% of transplantations occurred in 2002–2004 and 45% in 2005–2006. Adult donor graft transplants were done at 157 transplant centers (with 87 centers contributing 1–5 patients). Seventeen of 216 centers (8%) performed UCB and adult donor graft transplants. Subjects with outcome data reported to more than Registry were identified and counted only once. This study was approved by the Institutional Review Board of the Medical College of Wisconsin (HRRC# 056-87).
Inclusion criteria
Included are patients aged 16 years or older with acute lymphoblastic (ALL) or de novo myeloid leukemia (AML) transplanted with either a single UCB unit or unmanipulated PBPC or BM from an unrelated adult donor. Patients who had received prior autologous or allogeneic transplantation were excluded. Six hundred and thirty-two PBPC and 332 BM recipients were matched with their donors at the allele-level for HLA-A, HLA-B, HLA-C and HLA-DRB1 (8/8 HLA-match) and, 256 PBPC and 140 BM recipients were mismatched at a single allele or antigen (7/8 HLA-match), the accepted standard for these HSC.10 All UCB units were HLA-typed at the antigen-level (intermediate resolution) for HLA-A and HLA-B and at the allele-level for HLA-DRB1 (the current standard for UCB) and all UCB recipients received a single unit containing a minimum of 2.5 × 107/kg (total nucleated cells) at cryopreservation. Of the UCB donor-recipient pairs, 10 were HLA-matched, 40 were 5 of 6 HLA matched and 115 were 4 of 6 HLA matched. All transplantations were performed in 2002–2006 and used a myeloablative transplant conditioning regimen, identified by total busulfan dose ≥8 mg/kg or total body irradiation ≥1000 cGy.
Endpoints
Neutrophil recovery was defined as achieving an absolute neutrophil count (ANC) of ≥500 cells per cubic millimeter for 3 consecutive days; and platelet recovery as achieving ≥20,000 platelets per cubic millimeter, unsupported by transfusion for 7 days. Both neutrophil and platelet counts were monitored daily until recovery was established. Incidences of grade 2–4 acute and chronic GVHD were based on reports using standard criteria from each transplant center.11,12 TRM was defined as death occurring in continuous complete remission and relapse defined as leukemia recurrence based on morphological evaluation supported by reappearance of abnormalities in cytogenetic or molecular analyses. LFS was defined as survival in a state of continuous complete remission.
Statistical analysis
Variables related to patients, disease and transplants (Table 1) were compared among the groups with the use of the chi-square statistic for categorical variables. The probability of LFS was calculated with Kaplan-Meier estimator.13 Probabilities of neutrophil and platelet recovery, acute and chronic GVHD, TRM and relapse were calculated with the cumulative incidence estimator.13 The cumulative incidence estimator is used when there are two events for the outcome of interest and the occurrence of one of the events precludes the occurrence of the other. For neutrophil and platelet recovery and acute and chronic GVHD, death without the event was the competing event. For TRM, relapse was the competing event, and for relapse, TRM was the competing event. For analysis of LFS, relapse or death from any cause (i.e., treatment failure) was considered an event. In all analyses, data on patients without an event was censored at last follow-up.
Table 1.
Patient, disease and transplant characteristics
| BM | PBPC | UCB | |
|---|---|---|---|
| Number | 472 | 888 | 165 |
| Male | 257 (54%) | 485 (55%) | 83 (50%) |
| Age | |||
| 16 – 20 years | 69 (15%) | 51 (6%) | 46 (29%) |
| 21 – 30 years | 134 (28%) | 218 (25%) | 44 (26%) |
| 31 – 40 years | 86 (18%) | 202 (23%) | 43 (26%) |
| 41 – 50 years | 105 (22%) | 230 (26%) | 23 (14%) |
| > 50 years | 78 (17%) | 187 (21%) | 9 (5%) |
| Disease | |||
| Acute myeloid leukemia | 276 (58%) | 528 (59%) | 76 (46%) |
| Acute lymphoblastic leukemia | 196 (42%) | 360 (41%) | 89 (54%) |
| Disease status at transplantation | |||
| 1st and 2nd complete remission | 352 (75%) | 618 (70%) | 123 (75%) |
| Relapse | 120 (25%) | 270 (30%) | 42 (25%) |
| Year, transplant | |||
| 2002 – 2004 | 227 (48%) | 323 (36%) | 91 (55%) |
| 2005 – 2006 | 245 (52%) | 565 (64%) | 74 (45%) |
| TBI-containing conditioning regimen | |||
| Yes | 321 (68%) | 583 (66%) | 90 (55%) |
| None | 151 (32%) | 305 (34%) | 75 (45%) |
| Addition of ATG to conditioning regimen | 131 (28%) | 161 (18%) | 119 (72%) |
| Donor-recipient HLA disparity | |||
| A, B, C, DRB1 (allele-level) | |||
| Matched (8/8) | 332 (70%) | 632 (71%) | N/A |
| 1- locus (allele or antigen) mismatch (7/8) | 140 (30%) | 256 (29%) | N/A |
| A, B (antigen-level), DRB1 (allele-level) | |||
| Matched (6/6) | N/A | N/A | 10 (6%) |
| 1-antigen mismatch (5/6) | N/A | N/A | 40 (24%) |
| 2-antigen mismatch (4/6) | N/A | N/A | 115 (70%) |
CB cell dose pre-freeze: 3.6 (range 2.5 – 9.3) × 107/kg
CB cell dose infused: 2.6 (range 1.0 – 6.1) × 107/kg
The number in parenthesis is the percent of the total; N/A = not applicable
BM=bone marrow; PBPC=peripheral blood progenitor cells; UCB=umbilical cord blood
TBI=total body irradiation; ATG=anti-thymocyte globulin
Before comparing outcomes by HSC source, we investigated the potential effect of cell dose on LFS (HR 1.09, 95% CI 0.91 – 1.29, p=0.36) and overall survival (HR 1.11, 95% CI 0.93 – 1.32, p=0.26) in UCB recipients and found none.14 As 70% of UCB donor-recipient pairs were 4/6 HLA-matched, it was not possible to examine the effect of number of mismatches on UCB transplant-outcomes. Therefore all UCB recipients were grouped together for multivariate analyses. Cox proportional hazard regression models were constructed for acute and chronic GVHD, TRM, relapse and LFS.15 Multivariate models were built with the use of stepwise forward selection, using a p-value ≤0.01 (Bonferroni correction) to include variables in the model. Proportional-hazards assumption was tested for each variable individually; all variables met this assumption.
The primary objective was to compare transplant-outcomes according to HSC source (UCB versus PBPC or BM). Results are expressed as hazard ratio [HR] with 95% confidence interval [CI]. The variable for HSC source was held in all steps of model building. The other patient, disease and transplant variables considered were patient age (≤40 vs. >40 years), serologic status with respect to cytomegalovirus in the recipient (yes vs. no), disease (ALL vs. AML), disease status at transplantation (complete remission vs. not in remission), transplant conditioning regimen (total body irradiation (TBI) regimens vs. non-TBI regimens, use of anti-thymocyte globulin (ATG) (yes vs. none vs. unknown). The only covariate with missing data was use of ATG (n=20) and an “unknown” group was created. We also considered year of transplantation (2002–2004 vs. 2005–2006) as supportive care has improved over time and felt it was important to examine for a period effect on transplantation outcomes. Individual covariates were entered as categorical variables (as shown above). Patient age was first tested by decade (Table 1). Age categories 16–40 years were collapsed to a single category as the age groups 16–30 and 31–40 years were not significantly different (HR 1.26, p=0.08). Similarly, age groups 41–50 and 51–60 years were collapsed (HR 1.01, p=0.96). Therefore, age was tested as ≤40 vs. >40 years. There were no interactions between the variable for HSC source and other significant variables in the final model. The effect of acute and chronic GVHD as time dependent covariates on TRM and relapse was explored using Cox proportional hazards regression to determine whether TRM or relapse risks vary amongst the HSC sources. There were no significant center effects detected using the random effect model.16 All p-values are two-sided. Analyses were done with SAS software (version 9.1, Cary NC).
Role of funding source
The funding sources had no role in the study design, data analysis, data interpretation, or writing of this report. The corresponding author had full access to all data and final responsibility for decision to submit for publication.
RESULTS
Characteristics
Table 1 shows patient and transplant characteristics. Overall, UCB recipients were younger (median age 28 years versus 33 and 39 years for recipients of BM and PBPC, respectively, p<0.01). UCB recipients were more likely to have ALL (54%, p=0.01), receive a non irradiation-containing conditioning regimen (45%, p=0.01) and anti-thymocyte globulin (72%, p<0.01). Stage of disease at the time of transplant was similar between groups. After 2004, PBPC was the most commonly used HSC source. The median follow up of surviving BM, PBPC and UCB recipients was 26 months (range 3 – 68), 24 months (range 3 – 65) and 29 months (range 3 – 76), respectively.
Hematopoietic recovery
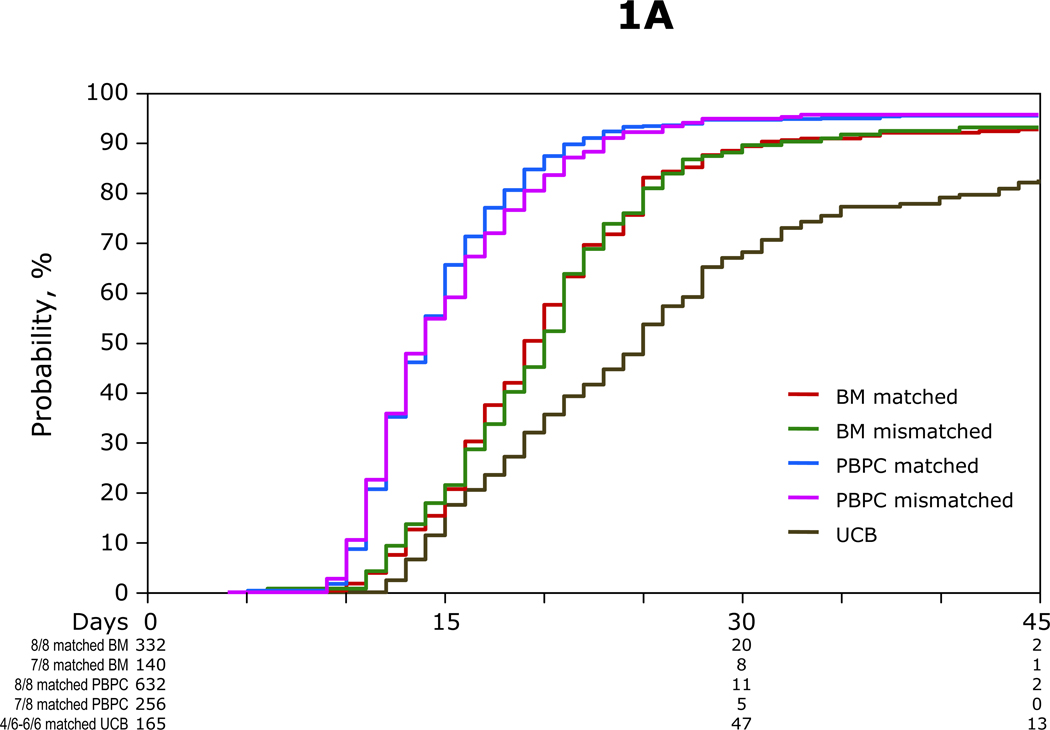
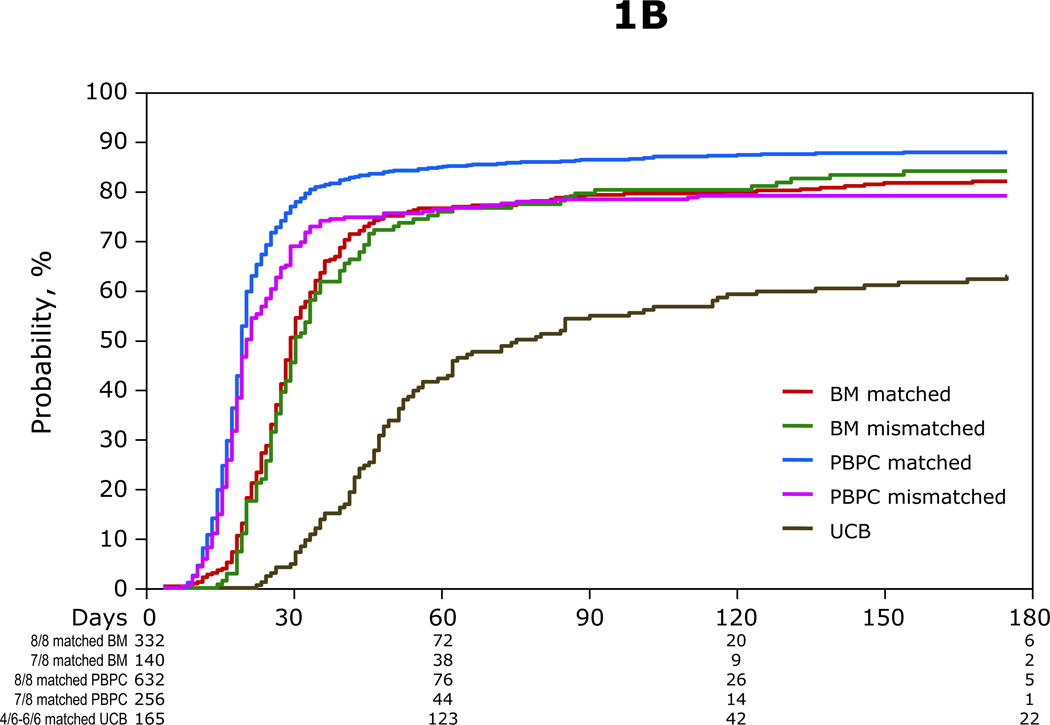
Recovery times in recipients of PBPC and BM were significantly faster that that observed in recipients of UCB (Figure 1A and 1B) and recovery times in recipients of PBPC faster than BM. Median times to neutrophil and platelet recoveries after PBPC transplant were 14 and 19 days, respectively and 19 and 28 days after BM transplant. Median times to neutrophil and platelet recoveries after UCB transplant were 24 days and 52 days, respectively. In all treatment groups, neutrophil recovery was slower with non-TBI regimens (HR 0.86, 95% CI 0.77 – 0.96, p=0.01). Neutrophil recovery by day-42 was inferior in recipients of UCB (80% p<0.0001) as compared to that in recipients of 8/8 and 7/8 HLA matched PBPC (96%) and BM (93%) which were similar to each other (p=0.02).
Figure 1.
A. The probabilities of neutrophil recovery by HSC source: the day-42 probability of neutrophil recovery after transplantation of 4-6/6 HLA matched UCB, 8/8 HLA matched PBPC, 8/8 HLA matched BM, 7/8 HLA matched PBPC and 7/8 HLA matched BM was 80%, 96%, 92%, 96% and 94%, respectively
B. The probabilities of platelet recovery by HSC source: the 6-month probability of platelet recovery after transplantation of 4-6/6 HLA matched UCB, 8/8 HLA matched PBPC, 8/8 HLA matched BM, 7/8 HLA matched PBPC and 7/8 HLA matched BM was 63%, 88%, 82%, 80% and 84%, respectively
Acute and chronic graft-versus-host disease
Grades 2–4 acute GVHD and chronic GVHD were significantly lower after transplantation of 4-6/6 HLA matched UCB compared to either 8/8 or 7/8 HLA matched PBPC (Table 2). Acute and chronic GVHD were also significantly lower after transplantation of 4-6/6 UCB compared to 7/8 HLA matched BM. In contrast, chronic GVHD but not acute GVHD was lower after transplantation of 4-6/6 HLA matched UCB compared to 8/8 HLA matched BM (Table 2). Regardless of HSC source, acute GVHD (HR 0.60, 95% CI 0.49 – 0.74, p<0.0001) and chronic GVHD (HR 0.47, 95% CI 0.38 – 0.58, p<0.0001) were lower in those treated with ATG as part of the conditioning regimen.
Table 2.
Multivariable analysis of leukemia-free survival, transplant-related mortality, relapse and acute and chronic graft-versus-host disease
| Number of events/number evaluable | Hazard Ratio (95% confidence interval) | p-value | |
|---|---|---|---|
| Leukemia-free survival | overall p=0.09 | ||
| 4-6/6 matched UCB vs.8/8 matched BM | 98/165 vs. 188/332 | 1.15 (0.90 – 1.47) | 0.25 |
| 4-6/6 matched UCB vs.7/8 matched BM | 98/165 vs. 80/140 | 0.93 (0.69 – 1.24) | 0.63 |
| 4-6/6 matched UCB vs.8/8 matched PBPC | 98/165 vs. 358/632 | 1.12 (0.89 – 1.39) | 0.18 |
| 4-6/6 matched UCB vs.7/8 matched PBPC | 98/165 vs. 170/256 | 0.91 (0.71 – 1.17) | 0.46 |
| Transplant-related mortality | overall p<0.0001 | ||
| 4-6/6 matched UCB vs.8/8 matched BM | 55/165 vs. 76/332 | 1.69 (1.19 – 2.39) | <0.01 |
| 4-6/6 matched UCB vs.7/8 matched BM | 55/165 vs. 46/140 | 1.06 (0.72 – 1.58) | 0.76 |
| 4-6/6 matched UCB vs.8/8 matched PBPC | 55/165 vs. 149/632 | 1.62 (1.18 – 2.23) | <0.01 |
| 4-6/6 matched UCB vs.7/8 matched PBPC | 55/165 vs. 93/256 | 0.95 (0.68 – 1.34) | 0.78 |
| Relapse | overall p=0.86 | ||
| 4-6/6 matched UCB vs.8/8 matched BM | 43/165 vs. 112/332 | 0.85 (0.59 – 1.20) | 0.35 |
| 4-6/6 matched UCB vs.7/8 matched BM | 43/165 vs. 42/140 | 0.84 (0.55 – 1.28) | 0.42 |
| 4-6/6 matched UCB vs.8/8 matched PBPC | 43/165 vs. 209/632 | 0.85 (0.61 – 1.17) | 0.31 |
| 4-6/6 matched UCB vs.7/8 matched PBPC | 43/165 vs. 77/256 | 0.91 (0.67 – 1.32) | 0.63 |
| Acute graft-versus-host disease | overall p<0.01 | ||
| 4-6/6 matched UCB vs. 8/8 matched BM | 49/162 vs.129/332 | 0.78 (0.56 – 1.08) | 0.13 |
| 4-6/6 matched UCB vs. 7/8 matched BM | 49/162 vs.64/139 | 0.59 (0.41 – 0.86) | 0.01 |
| 4-6/6 matched UCB vs. 8/8 matched PBPC | 49/162 vs.303/630 | 0.57 (0.42 – 0.77) | <0.01 |
| 4-6/6 matched UCB vs. 7/8 matched PBPC | 49/162 vs.134/256 | 0.49 (0.35 – 0.68) | <0.01 |
| Chronic graft-versus-host disease | overall p<0.0001 | ||
| 4-6/6 matched UCB vs. 8/8 matched BM | 39/161 vs. 132/332 | 0.63 (0.44 – 0.90) | 0.01 |
| 4-6/6 matched UCB vs. 7/8 matched BM | 39/161 vs. 51/140 | 0.59 (0.39 – 0.90) | 0.01 |
| 4-6/6 matched UCB vs. 8/8 matched PBPC | 39/161 vs. 327/632 | 0.38 (0.27 – 0.53) | <0.01 |
| 4-6/6 matched UCB vs. 7/8 matched PBPC | 39/161 vs. 113/256 | 0.46 (0.32 – 0.67) | <0.0001 |
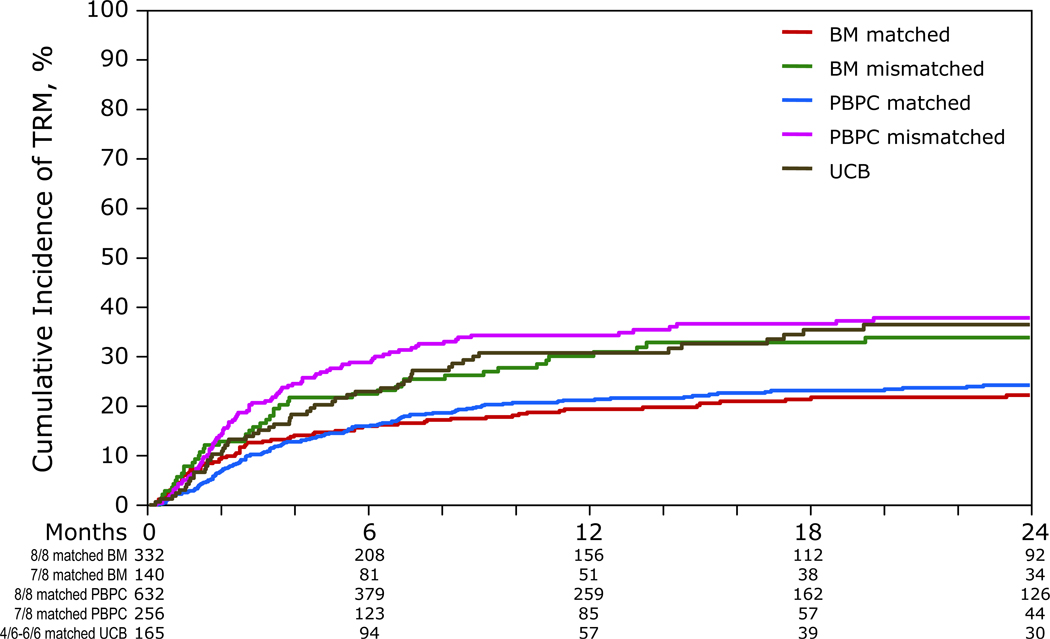
Transplant-related mortality
TRM was significantly higher after 4-6/6 HLA matched UCB transplants compared to 8/8 HLA-matched PBPC and BM transplants with most events in the UCB group occurring within 6 months after transplantation (Table 2, Figure 2). TRM risks were similar after transplantation of 4-6/6 HLA matched UCB and 7/8 HLA matched PBPC and BM. Independent of HSC source and HLA match, TRM risks were higher in patients who were not in remission compared to patients in remission at transplantation (HR 1.53, 95% CI 1.24 – 1.89, p<0.01) or aged >40 years compared to those aged ≤40 years (HR 1.33, 95% CI 1.09 – 1.61, p=0.01).
Figure 2.
The probabilities of leukemia-free survival by HSC source and donor-recipient HLA-match, adjusted for disease status at transplantation: the 2-year adjusted probability of leukemia-free survival after transplantation of 4-6/6 HLA matched UCB, 8/8 HLA matched PBPC, 8/8 HLA matched BM, 7/8 HLA matched PBPC and 7/8 HLA matched BM was 33%, 39%, 41%, 34% and 34%, respectively.
As UCB recipients tended to be younger than recipients of adult donor grafts we performed a subset analysis excluding the 83 patients who were aged 16–18 years at transplantation (BM matched n=30; BM mismatched n=8; PBPC matched n=15; PBPC mismatched n=4; UCB n=26). Consistent with the main analyses, TRM was higher after transplantation of UCB compared to 8/8 HLA matched BM and PBPC (Web Table 1).
Regardless of HSC source, TRM was higher in patients with acute (HR 2.09, 95% CI 1.71 – 2.55, p<0.01) and chronic GVHD (HR 1.59, 95% CI 1.91 – 2.13, p=0.02). Among those with acute GVHD, TRM risks were not different in UCB recipients compared to 8/8 HLA matched PBPC and BM (HR 1.37, 95% CI 0.82 – 2.32, p=0.22 and HR 1.75, 95% CI 0.30 – 0.96, p=0.07, respectively). Similarly, among those with chronic GVHD, TRM risks were not different in UCB recipients compared to 8/8 HLA matched PBPC (HR 1.67, 95% CI 0.84 – 3.29, p=0.14) and 8/8 HLA matched BM (HR 1.61, 95% CI 0.76 – 3.38, p=0.21).
Relapse
Leukemia relapse was similar in all treatment groups (Table 2). However, relapse was higher in patients who were not in complete remission compared to those in complete remission at transplantation (HR 3.67, 95% CI 3.06 – 4.40, p<0.0001). Patients with chronic GVHD had lower risks of relapse (HR 0.68, 95% CI 0.53 – 0.87, p<0.01), regardless of HSC source. Among those with chronic GVHD, relapse risks were similar after UCB and 8/8 HLA-matched PBPC and BM (HR 1.11, 95% CI 0.48 – 2.59, p=0.81 and HR 1.00, 95% CI 0.41 – 2.49, p=0.99, respectively).
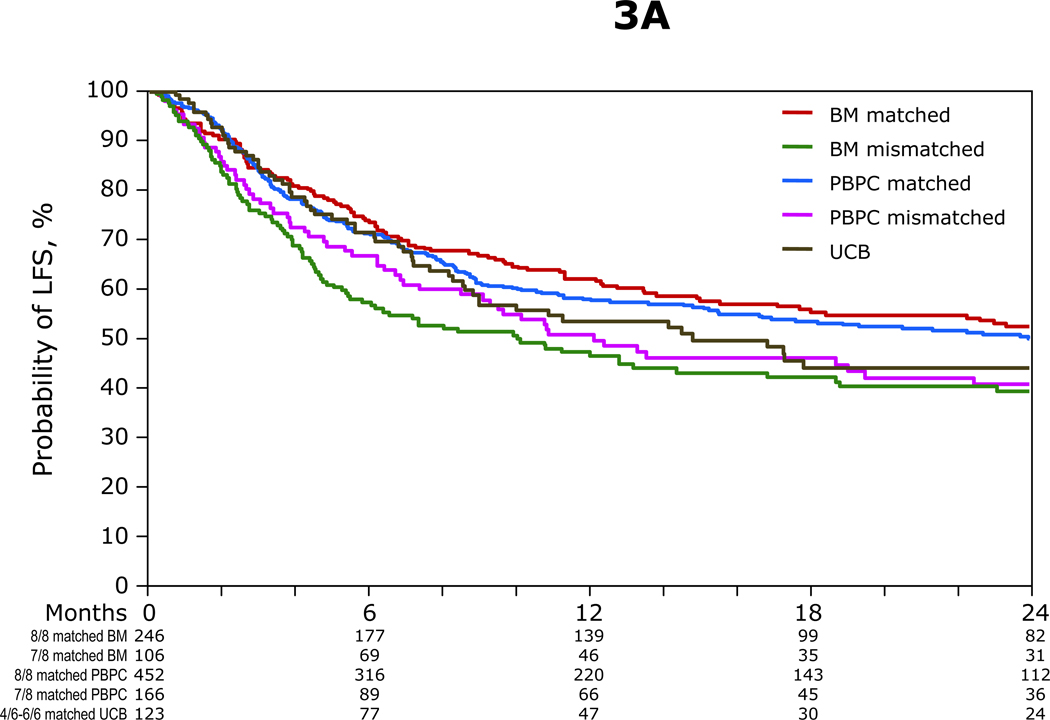
Leukemia-free survival
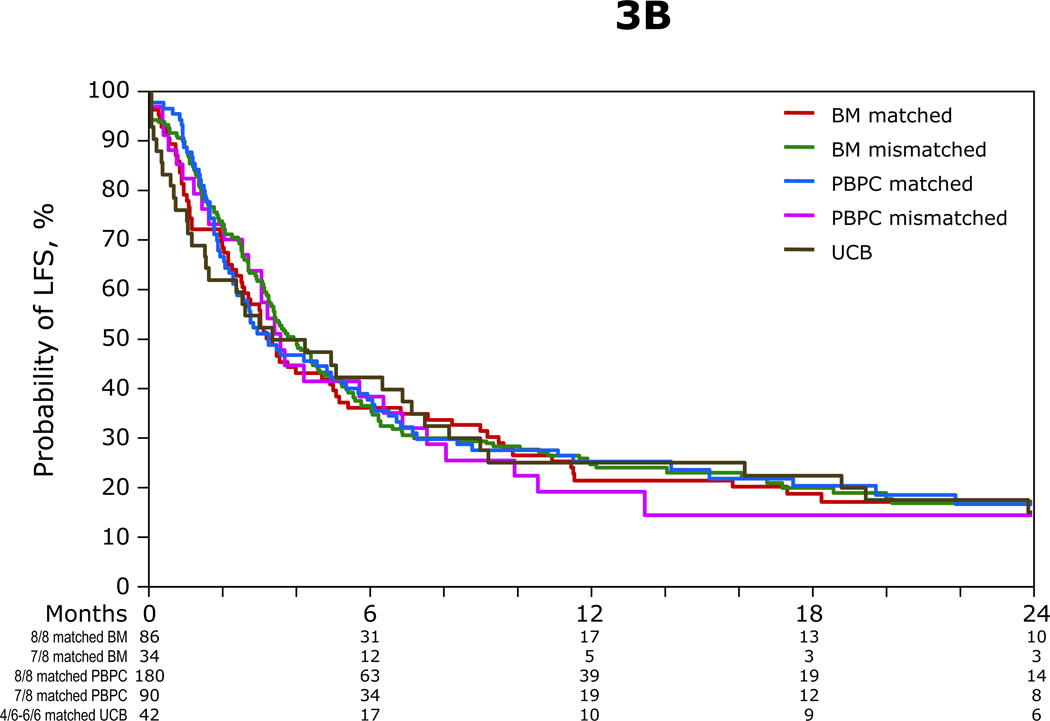
LFS was similar regardless of HSC source (Table 2, Figure 3A, 3B). This result also held when examined separately for each disease status (Web Table 2). Disease status was the only factor associated with LFS and independent of HSC source. Furthermore, outcomes were unchanged even if we restricted UCB recipients to those with a 4/6 HLA match, the dominant subset (Web Table 3). Patients who were not in complete remission had higher treatment failure compared to those in complete remission (HR 2.50, 95% CI 2.18 – 2.86, p<0.0001). LFS was also similar when we restricted the analysis to patients older than 18 years (Web Table 1). The causes of death that occurred during the first 100 days and thereafter are shown in Tables 3A, 3B. While 40–50% of early deaths were due to infections and organ failure, recurrent leukemia was the most common cause of death in all groups.
Figure 3.
A. The probabilities of leukemia-free survival by HSC source and donor-recipient HLA-match for patients in remission at transplantation: the 2-year probability of leukemia-free survival after transplantation of 4-6/6 HLA matched UCB, 8/8 HLA matched PBPC, 8/8 HLA matched BM, 7/8 HLA matched PBPC and 7/8 HLA matched BM was 44%, 50%, 52%, 39% and 41%, respectively
B. The probabilities of leukemia-free survival by HSC source and donor-recipient HLA-match for patients who were not in remission at transplantation: the 2-year probability of leukemia-free survival after transplantation of 4-6/6 HLA matched UCB, 8/8 HLA matched PBPC, 8/8 HLA matched BM, 7/8 HLA matched PBPC and 7/8 HLA matched BM was 15%, 17%, 17%, 17% and 14%, respectively
Table 3.
Early causes of death (within 100 days after transplantation)
| A | |||
|---|---|---|---|
| Causes of death | BM | PBPC | CB |
| Total number | 95 | 180 | 37 |
| Recurrent leukemia | 25 (26%) | 56 (31%) | 11 (30%) |
| EBV associated lymphoma | __ | 1 (<1%) | 1 (3%) |
| Graft versus host disease | 8 (8%) | 35 (19%) | 3 (8%) |
| Interstitial pneumonitis | 9 (9%) | 11 (6%) | 2 (5%) |
| Infection | 21 (22%) | 30 (17%) | 10 (23%) |
| Organ failure | 31 (33%) | 47 (26%) | 10 (23%) |
| Other | 1 (2%) | 1 (<1%) | N/A |
| B Late causes of death (beyond 100 days after transplantation) | |||
|---|---|---|---|
| Causes of death | BM | PBPC | CB |
| Total number | 157 | 308 | 59 |
| Recurrent leukemia | 105 (67%) | 192 (62%) | 31 (53%) |
| EBV associated lymphoma | 1 (<1%) | 1 (<1%) | 2 (3%) |
| Graft versus host disease | 13 (8%) | 28 (9%) | 12 (20%) |
| Interstitial pneumonitis | 5 (3%) | 12 (4%) | 1 (2%) |
| Infection | 19 (12%) | 39 (13%) | 7 (12%) |
| Organ failure | 12 (8%) | 35 (11%) | 6 (10%) |
| Other | 2 (1%) | 1 (<1%) | N/A |
The number in parenthesis is the percent of the total
N/A = not applicable
Patient characteristics and HSC sources
Disease status was the only characteristic associated with relapse after transplantation and LFS. TRM was associated with age at transplantation and disease status. The sole potentially modifiable characteristic is disease status in that physicians may be able to perform transplantation in remission before disease progression. Age is not a modifiable factor. Therefore, when assessing the risk of TRM for any patient there are three potential risk categories, independent of HSC source. Low risk (patients aged ≤40 years and in remission; HR 1.00), intermediate risk (patients aged ≤40 years and not in remission or patients aged >40 years and in remission HR 1.23, p=0.05) and high risk (patients aged >40 years and not in remission HR 2.17, p<0.0001).
DISCUSSION
Our primary objective was to evaluate the three most commonly used sources of allogeneic HSC using standard donor selection criteria. After adjusting for differences between cohorts, to our knowledge this is the first analysis that demonstrates similar LFS in recipients of 4-6/6 HLA-matched UCB as compared to 8/8 HLA matched and 7/8 HLA matched PBPC and BM. These observations confirm UCB as an acceptable alternative to 8/8 and 7/8 HLA matched PBPC and BM. These results are particularly remarkable in view of the fact that 70% of UCB transplants were mismatched at two HLA-antigens. However, TRM is higher after 4-6/6 HLA matched UCB compared to 8/8 HLA matched PBPC and BM despite lower probabilities of acute and chronic GVHD. This report differs from previous reports in that it is focused on the way allogeneic adult and UCB HSC are selected in 2010 - namely, the use of allele-level HLA matching for adult donor allografts and a lower cell dose limit of 2.5 × 107/kg for a single UCB unit. Furthermore, we also evaluated outcomes in recipients of 8/8 and 7/8 HLA matched PBPC in addition to BM, as PBPC now represents the most commonly used graft source (approximately 70%) in Europe and U.S. Earlier reports8,9 that compared UCB and BM for adults with leukemia did not consider matching at the HLA-C locus which is now known to affect survival after BM transplantation and the more recent report17 did not evaluate UCB relative to 8/8 or 7/8 HLA matched PBPC or 7/8 HLA matched BM. Comparing transplant-outcomes after UCB to 7/8 HLA matched PBPC or BM, the accepted alternative to 8/8 HLA matched PBPC or BM is relevant, as 30% of unrelated adult donor transplantations use a mismatched adult donor.
This report differs from the one in children7 in that we could not evaluate the effect of UCB HLA match on the various outcomes as too few patients had a close HLA match (i.e. 6/6 HLA match). While the prior analysis suggested that 6/6 HLA matched UCB was associated with lower risks of TRM, the findings here are consistent with those in children who received 4–5/6 HLA matched UCB. Furthermore, as in other reports in adults, no specific cell dose could be identified that resulted in a survival advantage.8,9,17 It is possible that this reflects the relatively narrow range of cell doses with a single UCB unit. Future studies with larger numbers of patients with greater numbers of matched and mismatched donor-recipient pairs and wider range in cell doses infused might permit a more refined analysis on the effects of HLA match and cell dose in adults as well as children.
Consistent with others18 we observed a protective effect of chronic GVHD in preventing recurrent leukemia. To our knowledge, this is the first time such an association has been made with UCB as the HSC source. Though, acute and chronic GVHD are relatively uncommon after UCB transplantation, particularly when compared with allogeneic PBPC, this complication accounted for approximately 20% of deaths after UCB and PBPC transplants implying the severity of GVHD does not differ by HSC source. Whether the absence of chronic GVHD offers a difference in long term survival or health quality of life are topics for future studies.
A major limitation to the use of UCB is the availability of sufficient numbers of hematopoietic precursor cells for hematopoietic recovery.4,5,7–9,17,19,20 Several strategies for reducing the period of neutropenia being explored may lead to lower early mortality and potentially improved LFS.21 These include transplantation of two UCB units if a single UCB unit with an adequate cell dose cannot be identified, ex-vivo expansion culture to augment the number of HSC and progenitors in the UCB graft, co-infusion of T-cell depleted haploidentical PBPC to bridge the period of neutropenia, injection of UCB cells directly into the patient’s bone marrow to reduce non-specific losses of HSC as well as improve homing of HSC and progenitor cells. If successful, the effectiveness of UCB as a source of HSC for allogeneic transplantation could be enhanced.22–27 As the number of double UCB transplants increase over time, it is likely that future studies will address the relative risks and benefits of single versus double UCB transplantation.
As with all observational studies, this study has limitations. Choice of intervention, in this case HSC source, is often governed by a complex list of unmeasured factors that can potentially influence outcome, such as time to transplant that may be delayed for recipients of unrelated adult donor grafts. Although we adjusted for known risk factors, only a randomized trial comparing the different allogeneic HSC sources could exclude potential selection bias. While several groups have seriously considered such a trial, the logistics are formidable. Whereas UCB is principally limited by cell dose criteria, use of PBPC or BM is limited by HLA matching requirements and urgency of transplantation. Only an estimated 25% of adults will be able to find a suitable single UCB unit and studies on the safety and effectiveness of double UCB unit transplants are underway to address the cell dose obstacle. Therefore, in the absence of a randomized clinical trial, these data support the use of 4-6/6 HLA matched unrelated UCB and use of 7/8 HLA matched unrelated adult donor in the treatment of adults with acute leukemia when an 8/8 HLA-matched unrelated adult donor is lacking and use of UCB as first line therapy when transplant is urgently needed.
Acknowledgement
Supported by a Public Health Service grant (U24-CA76518) from the National Cancer Institute, National Heart Lung and Blood Institute and National Institute of Allergy and Infectious Disease; Health Resources and Services Administration (HHSH234200637015C); the Office of Naval Research, Department of Navy to the National Marrow Donor Program (N00014-08-1-1207), the Children’s Leukemia Research Association and a Scholar in Clinical Research Award from the Leukemia and Lymphoma Society (ME). Grant U24-CA76518 and HHSH234200637015C support the Center for International Blood and Marrow Transplant Research, including data collection. Grant N00014-06-01-0704 support donor-recipient histocompatibility typing. Opinions, findings, and conclusions or recommendations expressed herein are those of the authors and do not reflect the views of the Office of Naval Research or the National Marrow Donor Program.
Funding: National Cancer Institute, National Heart Lung and Blood Institute, National Institute of Allergy and Infectious Disease (U24-CA76518); Health Resources and Services Administration (HHSH234200637015C); Office of Naval Research, Department of Navy (N00014-08-1-1207); Children’s Leukemia Research Association; a Scholar in Clinical Research Award, the Leukemia and Lymphoma Society (ME).
Footnotes
Conflict of interest statement: We declare we have no conflict of interest.
Contributors: M Eapen, V Rocha, E Gluckman, MM Horowitz and JE Wagner designed the study. M Eapen, V Rocha and MJ Zhang prepared and analyzed data. M Eapen and JE Wagner had primary responsibility for drafting the manuscript. V Rocha, E Gluckman and MM Horowitz participated in data interpretation and critically reviewed the manuscript. G Sanz, A Scaradavou, W Arcese, A Sirvent, RE Champlin, N Chao, AP Gee, L Isola, MJ Laughlin, DI Marks, S Nabhan, A Ruggeri and R Soiffer interpreted data and critically reviewed the manuscript. All co-authors contributed equally to interpretation of data, manuscript preparation and approval of final report.
References
- 1.Eapen M, Logan BR, Confer DL, et al. Peripheral blood grafts from unrelated donors are associated with increased acute and chronic graft-versus-host disease without improved survival. Biol Blood and Marrow Transplant. 2007;13:1461–1468. doi: 10.1016/j.bbmt.2007.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Marrow Donor Association Donor Registries Working Group. Stem Cell Donor Registries Annual Report. 12th ed. Leiden: World Marrow Donor Association; 2008. [Google Scholar]
- 3.Barker JN, Krepski TP, DeFor TE, et al. Searching for unrelated donor hematopoietic stem cells: Availability and speed of umbilical cord versus bone marrow. Biol Blood and Marrow Transplant. 2002;8:257–260. doi: 10.1053/bbmt.2002.v8.pm12064362. [DOI] [PubMed] [Google Scholar]
- 4.Rocha V, Cornish J, Sievers EL, et al. Comparison of outcomes of unrelated bone marrow and umbilical cord blood transplants in children with acute leukemia. Blood. 2001;97:2962–2971. doi: 10.1182/blood.v97.10.2962. [DOI] [PubMed] [Google Scholar]
- 5.Wagner JE, Barker JN, DeFor TE, et al. Transplantation of unrelated donor umbilical cord blood in 102 patients with malignant and non-malignant diseases: influence of CD34 cell dose and HLA disparity on treatment-related mortality and survival. Blood. 2002;100:1611–1618. doi: 10.1182/blood-2002-01-0294. [DOI] [PubMed] [Google Scholar]
- 6.Kurtzberg J, Prasad VK, Carter SL, et al. Results of the cord blood transplantation study (COBLT): clinical outcomes of unrelated donor umbilical cord blood transplantation in pediatric patients with hematologic malignancies. Blood. 2008;112:4318–4327. doi: 10.1182/blood-2007-06-098020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eapen M, Rubinstein P, Zhang M-J, et al. Outcomes of transplantation of unrelated umbilical cord blood and bone marrow in children with acute leukemia: A comparison study. Lancet. 2007;369:1947–1954. doi: 10.1016/S0140-6736(07)60915-5. [DOI] [PubMed] [Google Scholar]
- 8.Laughlin MJ, Eapen M, Rubinstein P, et al. Outcomes after transplantation of cord blood or bone marrow from unrelated donors in adults with leukemia. N Engl J Med. 2004;351:2265–2275. doi: 10.1056/NEJMoa041276. [DOI] [PubMed] [Google Scholar]
- 9.Rocha V, Labopin M, Sanz G, et al. Transplantation of umbilical cord blood or bone marrow from unrelated donors in adults with acute leukemia. N Engl J Med. 2004;351:2276–2285. doi: 10.1056/NEJMoa041469. [DOI] [PubMed] [Google Scholar]
- 10.Lee SJ, Klein JP, Haagenson M, et al. High resolution donor-recipient HLA matching contributes to the success of unrelated donor transplantation. Blood. 2007;110:4576–4583. doi: 10.1182/blood-2007-06-097386. [DOI] [PubMed] [Google Scholar]
- 11.Przepiorka D, Weisdorf D, Martin P, et al. 1994 Concensus conference on acute GVHD grading. Bone Marrow Transplant. 1995;15:825–828. [PubMed] [Google Scholar]
- 12.Flowers ME, Kansu E, Sullivan KM. Pathophysiology and treatment of graft-versus-host disease. Hematol Oncol Cln North Am. 1999;13:1091–1112. doi: 10.1016/s0889-8588(05)70111-8. [DOI] [PubMed] [Google Scholar]
- 13.Klein JP, Moeschberger ML. Survival Analysis: techniques of censored and truncated data. 2nd ed. New York, NY: Springer-Verlag; 2003. [Google Scholar]
- 14.Klein JP, Wu TJ. Handbook of Statistics: advances in survival analysis discretizing a continuous covariate in survival studies. Amsterdam: Elsevier; 2004. [Google Scholar]
- 15.Cox DR. Regression model and life tables. J R Stat Soc B. 1972;34:187–200. [Google Scholar]
- 16.Andersen PK, Klein JP, Zhang M-J. Testing for center effects in multi-center survival studies: a Monte Carlo comparison of fixed and random effects tests. Stat Med. 1999;18:1489–1500. doi: 10.1002/(sici)1097-0258(19990630)18:12<1489::aid-sim140>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 17.Atsuta Y, Suzuki R, Nagamura-Inoue T, et al. Disease-specific analyses of unrelated cord blood transplantation compared with unrelated bone marrow transplantation in adult patients with acute leukemia. Blood. 2009;113:1631–1638. doi: 10.1182/blood-2008-03-147041. [DOI] [PubMed] [Google Scholar]
- 18.Ringden O, Pavletic SZ, Anasetti C, et al. The graft-versus-leukemia effect using matched unrelated donors is not superior to HLA-identical siblings for hematopoietic stem cell transplantation. Blood. 2009;113:3110–3118. doi: 10.1182/blood-2008-07-163212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Heeckeren WJ, Fanning LR, Meyerson HJ, et al. Influence of human leukocyte antigen disparity and graft lymphocytes on allogeneic engraftment and survival after umbilical cord blood transplants in adults. B J Hematol. 2007;139:464–474. doi: 10.1111/j.1365-2141.2007.06824.x. [DOI] [PubMed] [Google Scholar]
- 20.Rocha V, Gluckman E. Improving outcomes of cord blood transplantation: HLA matching, cell dose and other graft- and transplantation-related factor. B J Haematol. 2009;147:262–274. doi: 10.1111/j.1365-2141.2009.07883.x. [DOI] [PubMed] [Google Scholar]
- 21.Rocha V, Broxymeyer HE. New approaches for improving engraftment after cord blood transplantation. Biol Blood Marrow Transplant. 2009;16:S126–S132. doi: 10.1016/j.bbmt.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 22.Brunstein CG, Barker JN, Wesidorf DJ, et al. Umbilical cord blood transplantation after non-myeloablative conditioning: impact on transplantation outcomes in 110 adults with hematologic disease. Blood. 2007;110:3064–3070. doi: 10.1182/blood-2007-04-067215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jaroscak J, Goltry K, Smith A, et al. Augmentation of umbilical cord blood (UCB) transplantation with ex-vivo expanded UCB cells: results of a phase 1 trial using the Asstrom Replicell System. Blood. 2003;101:5061–5067. doi: 10.1182/blood-2001-12-0290. [DOI] [PubMed] [Google Scholar]
- 24.Robinson SN, Ng J, Niu T, et al. Superior ex-vivo cord blood expansion following co-culture with bone marrow derived mesenchymal stem cells. Bone Marrow Transplant. 2006;37:359–366. doi: 10.1038/sj.bmt.1705258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bautista G, Cabrera JR, Regidor C, et al. Cord blood transplants supported by co-infusion of mobilized hematopoietic stem cells from a third party donor. Bone Marrow Transplant. 2009;43:365–373. doi: 10.1038/bmt.2008.329. [DOI] [PubMed] [Google Scholar]
- 26.Delaney C, Varnum-Finney B, Aoyama K, et al. Dose-dependent effects of the notch ligand delta1 on ex vivo differentiation and in vivo marrow repopulating ability of cord blood cells. Blood. 2005;106:2693–2699. doi: 10.1182/blood-2005-03-1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frassoni F, Gualandi F, Podesta M, et al. Direct intrabone transplant of unrelated cord blood cells in acute leukemia: a phase I/II study. Lancet Oncol. 2008;9:831–839. doi: 10.1016/S1470-2045(08)70180-3. [DOI] [PubMed] [Google Scholar]
- 28.Copelan EA. Hematopoietic stem cell transplantation. N J Engl Med. 2006;354:1813–1826. doi: 10.1056/NEJMra052638. [DOI] [PubMed] [Google Scholar]