Abstract
OBJECTIVE
Caspase-1 is a component of the NALP3 inflammasome, a cytosolic multiprotein complex that mediates the processing of pro-inflammatory caspases and cytokines. The inflammasome represents the first line of defense against cellular stress and is a crucial component of innate immunity. Caspase-1 is the enzyme responsible for the cleavage and activation of interleukin-1β, which is a potent pro-inflammatory cytokine, and plays a central role in the mechanisms leading to labor (preterm and term) particularly in the context of intrauterine infection/inflammation. In addition, Caspase-1 cleaves IL-18 and IL-33. The objectives of this study were to determine whether there is a relationship between amniotic fluid concentrations of caspase-1 and gestational age, parturition (term and preterm) and intra-amniotic infection/inflammation (IAI).
STUDY DESIGN
A cross-sectional study was conducted including 143 pregnant women in the following groups: 1) mid-trimester of pregnancy (n=18); 2) term not in labor (n=25); 3) term in labor (n=28); 4) preterm labor (PTL) who delivered at term (n=23); 5) PTL without intra-amniotic infection and/or inflammation (IAI) who delivered preterm (n=32); 6) PTL with IAI who delivered preterm neonates (n=17). Caspase-1 concentrations in amniotic fluid were determined by a specific and sensitive immunoassay. Non-parametric statistics were used for analysis.
RESULTS
1) Caspase-1 was detected in amniotic fluid of women at term, but in none of the mid-trimester samples; 2) Patients in labor at term had a significantly higher median amniotic fluid concentration of caspase-1 than women at term not in labor [term in labor: 10.5 pg/ml, range (0.0–666.0) vs. term not in labor: 5.99 pg/ml, range (0.0–237.4); p<0.05]; 3) Among patients with spontaneous PTL, those with intra-amniotic infection and/or inflammation [median 41.4 pg/ml; range: (0.00–515.00)] had a significantly higher median amniotic fluid caspase-1 concentration than those without intra-amniotic infection and/or inflammation who delivered preterm [median 0.0 pg/ml; range: (0.0–78.4)] and than those who delivered at term [median 0.0 pg/ml, range (0.00–199.5)], (p<0.001 for both comparisons).
CONCLUSIONS
1) The presence and concentration of caspase-1 in the amniotic fluid varies as a function of gestational age; 2) Women with spontaneous labor at term had a higher median caspase-1 amniotic fluid concentration than women at term without labor. This suggests that the inflammasome may be activated in spontaneous parturition at term. Since most women with labor do not have intra-amniotic infection, we propose that cellular stress during labor accounts for activation of the inflammasome; 3) Preterm labor associated with infection/inflammation was also associated with a high concentration of caspase-1, suggesting that infection may induce caspase-1 production and activation of the inflammasome; 4) The sequential activation of the inflammasome and caspase-1, leading to interleukin-1β processing and secretion, is a candidate pathway leading to the activation of the common pathway of parturition.
Keywords: ICE, interleukin-1 converting enzyme, labor, delivery, preterm, intra-amniotic infection, intra-amniotic inflammation, chorioamnionitis, preterm birth, inflammasome
INTRODUCTION
Caspase-1,[1,2] also known as “Interleukin-1β Converting Enzyme” (ICE),[3,4] is a cysteine-aspartic protease,[5] promoting the processing, secretion and release of pro-inflammatory cytokines, including interleukin (IL)-1β, IL-18, and IL-33.[6–8] Caspase-1 is the prototype of the inflammatory caspases, and a key component of the inflammasome,[8–10] which has been recently defined as a first line of the immune response to cell stress,[10] as well as a “master switch of inflammation”.[11] The inflammasome, indeed, is an inducible multiprotein cytosolic complex,[8] assembling upon recognition of “danger signals” by intracellular sensors, including the NOD-like receptors,[12] or pathogen associated compounds.[10] The inflammasome, in turn, activates inflammatory caspases,[8] of which caspase-1 is the prototype, and promotes the processing, secretion and release of pro-inflammatory cytokines, including IL-1β, IL-18, and IL-33.[6–8,10]
Term and preterm labor are inflammatory processes,[13–21] in which inflammatory mediators including cytokines such as IL-1,[22–26] IL-6,[22,27–30] tumor necrosis factor,[27,31–36] IL-18,[37] IL-16,[38] and chemokines[39–45] play a central role. Of note, labor is associated with increased concentrations of IL-1β in both gestational tissues[46–48] and biological fluids.[13,49] and intra-amniotic and/or systemic administration of IL-1β to mice and monkeys induces preterm labor.[24,50,51]
Considering the pivotal role of caspase-1 as a link between the activation of the inflammasome and the processing of IL-1β, we conducted this study to determine whether there is a relationship between amniotic fluid concentrations of caspase-1 and gestational age, parturition (term and preterm) and intra-amniotic infection/inflammation (IAI).
MATERIALS AND METHODS
Study design
This cross-sectional study was designed to examine the relationship among amniotic fluid concentrations of caspase-1 and gestational age, spontaneous labor at term, preterm parturition and intra-amniotic infection/inflammation.
Amniotic fluid was collected by trans-abdominal amniocentesis from 143 singleton pregnancies in the following groups: 1) Patients undergoing mid-trimester amniocentesis for clinical indications who delivered at term (n=18); 2) women at term not in labor (n=25); 3) patients at term in labor (n=28); 4) women with preterm labor (PTL) and intact membranes who delivered at term (n=23); 5) women in PTL without IAI who delivered preterm (n=32); 6) women with PTL and IAI who delivered preterm (n=17).
Clinical definitions
Patients were considered to have a normal pregnancy if they did not have obstetrical, medical, or surgical complication of pregnancy, and delivered a term (≥37 weeks) neonate. PTL was defined in the presence of regular uterine contractions occurring at a frequency of at least 2 every 10 minutes, combined with documented cervical changes prior 37 weeks of gestation. Intra-amniotic infection was defined by a positive amniotic fluid culture for microorganisms. Intra-amniotic inflammation was defined in the presence of a white blood cell (WBC) count > 100 cells/mm3.
Amniotic fluid sample collection and analysis
Amniotic fluid was collected by trans-abdominal amniocentesis. Fluid not required for clinical purposes was centrifuged to remove cellular and particulate matter and aliquots stored at −70° C until analysis. Amniotic fluid WBC count, Gram stain, and glucose concentrations were used in the management of patients with preterm labor. Amniotic fluid samples from the term and preterm groups were cultured for aerobic, anaerobic species and genital mycoplasmas (Ureaplasma urealyticum and Mycoplasma hominis). Pregnant patients were enrolled at Hutzel Hospital, Detroit, MI, USA, Pennsylvania Hospital, Philadelphia, Pennsylvania, USA, and Sotero del Rio Hospital, Puente Alto, Cile. The collection of samples for research was approved by the Institutional Review Boards of Wayne State University, Pennsylvania Hospital, and Sotero del Rio Hospital, as well as the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services (NIH/DHHS). All participants provided written informed consent for collection of clinical data and biological materials. Many of these samples have been previously employed to study the biology of inflammation, hemostasis, angiogenesis regulation, and growth factor concentrations in non-pregnant women, normal pregnant women and those with complications.
Human caspase-1 immunoassays in amniotic fluid
A specific and sensitive immunoassay was used to determine the concentration of caspase-1 in amniotic fluid samples. Human caspase-1 immunoassay kits (Cistron Biotechnology, Pine Brook, NJ, USA) were validated for human amniotic fluid in our laboratory prior to the conduction of this study. Validation included spike and recovery experiments, which produced parallel curves indicating that amniotic fluid constituents did not interfere with antigen-antibody binding in this assay system. The inter-assay and intra-assay coefficients of variation for the caspase-1 immunoassay were 7.9% and 4.7%, respectively. The sensitivity was 3.54 pg/ml.
Statistical analysis
Data were tested for normality using the Kolmogorov-Smirnov test. Kruskal-Wallis was used for analysis of variance. Comparisons between two groups were performed using Mann-Whitney rank sum tests. A p value <0.05 was considered statistically significant. We used SPSS v.14.0 (SPSS Inc., Chicago, IL, USA) for analysis.
RESULTS
One-hundred and forty-three patients were included in this study. The demographic and clinical characteristics of patients with PTL are displayed in Table I.
Table I.
Demographic and clinical characteristics of patients with preterm labor
| Gestational Age at amniocentesis (weeks) | Gestational age at delivery (weeks) | Birthweight (grams) | Maternal age (years) | |
|---|---|---|---|---|
| PTL delivered at term | 31.8 (28.6–33.8) | 38.7 (37.9–40.1) | 3020 (2640–3317) | 20 (18–22) |
| PTL delivered preterm, no IAI | 28.4 (23.2–31.3) | 34.2 (31–35.7) | 1956 (1730–2570) | 24 (22–28) |
| PTL delivered preterm with IAI | 26.6 (24.4–32.2) | 26.9 (25.5–32.8) | 960 (795–1964) | 26 (23–32.5) |
PTL = preterm labor, IAI = intra-amniotic infection/inflammation. Results are median (inter-quartile range).
Caspase-1 in amniotic fluid
Caspase-1 was detectable in 56.6 % (81/143) of the amniotic fluid samples. Of interest, caspase-1 was detected in 76% (19/25) of women at term not in labor, whereas in none of the mid-trimester samples.
Spontaneous labor at term is associated with higher amniotic fluid concentrations of caspase-1
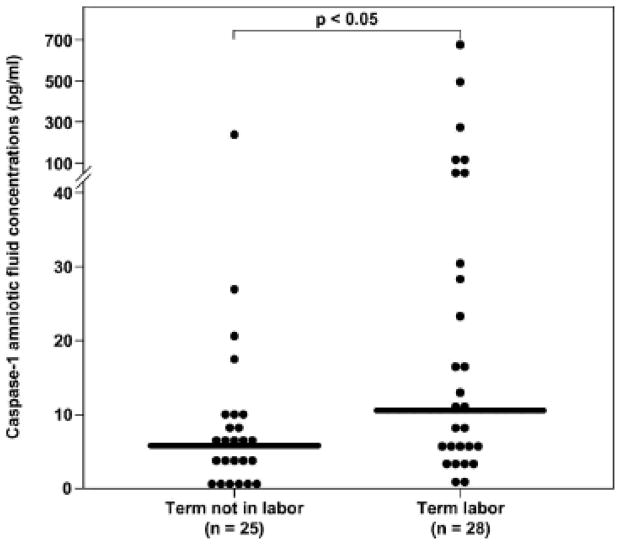
The median amniotic fluid caspase-1 concentration was significantly higher in women in spontaneous labor at term than in those not in labor at term 9term in labor: median 10.5 pg/mL; range (0–666) vs. term not in labor: median 5.99 pg/ml; range (0.0–237.4); p<0.05; Figure 1).
Figure 1. Amniotic fluid concentrations of caspases-1 in patients at term.
The median amniotic fluid caspases-1 concentration was significantly higher in women in spontaneous labor at term than in those not in labor (term in labor: median 10.5 pg/ml; range (0–666) vs. term not in labor: median 5.99 pg/ml; range (0.00–237.4); p<0.05).
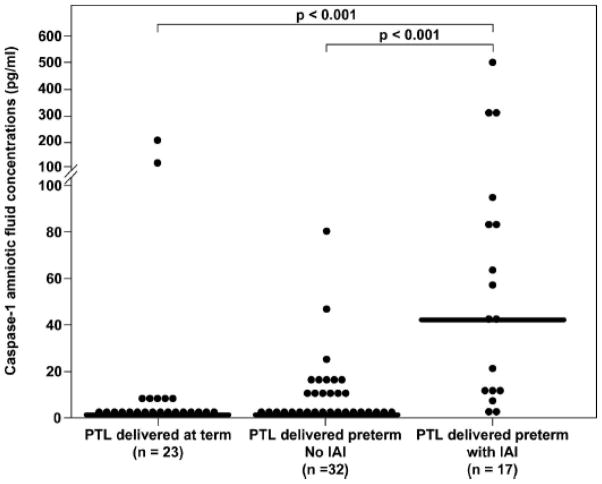
Caspase-1 is increased in the amniotic fluid of women with preterm labor in the presence of intra-amniotic infection/inflammation
Among patients with spontaneous PTL, those with intra-amniotic infection and/or inflammation (median 41.4 pg/ml; range: 0–515) had a significantly higher median amniotic fluid caspase-1 concentration than those without intra-amniotic infection and/or inflammation who delivered preterm (median 0. 0 pg/ml; range: 0.0–78.4) and than those who delivered at term (median 0.0 pg/ml, range 0.0–199.5), (p<0.001 for both comparisons; Figure 2).
Figure 2. Amniotic fluid concentrations of caspases-1 in women with preterm labor.
Among patients with spontaneous PTL, those with intra-amniotic infection and/or inflammation (median 41.4 pg/ml; range: 0.0–515) had a significantly higher median amniotic fluid caspase-1 concentration than those without intra-amniotic infection and/or inflammation who delivered preterm (median 0.0 pg/ml; range: 0.0–78.4) and than those who delivered at term (median 0.0 pg/mL, range 0.0–199.5), p<0.001 for both comparisons.
DISCUSSION
Principal findings of the study
1) Caspase-1 is detectable in amniotic fluid at term but not in the midtrimester; 2) Women in spontaneous labor at term have a higher median amniotic fluid concentration of caspase-1 than patients at term not in labor; 3) Among patients with preterm labor, those with intra-amniotic infection and/or inflammation had a significantly higher median amniotic fluid caspase-1 concentration than those without intra-amniotic infection and/or inflammation. These observations suggest that caspase-1 participates in the mechanisms leading to spontaneous term parturition and preterm labor associated with infection/inflammation.
Biology of Caspase-1
Caspase-1,[1,2] known as “Interleukin-1β Converting Enzyme” (ICE),[3,4] is a member of the cysteine-aspartic proteases family (“c-asp-ases”),[5] enzymes involved in inflammation, apoptosis, cellular proliferation and terminal differentiation.[52] Caspases have been classified as “inflammatory” (caspase-1, -4, -5 and the murine caspase-11 and -12), and “apoptotic” (“initiators”: caspase-2, -8, -9 and -10 ; and “executors”: caspase-3, -6 and -7),[7,53] according to their predominant pathway of involvement. However, this distinction is not absolute,[54] and differences between the in-vivo and in-vitro activity of these enzymes have been proposed.[7] Caspases process several proteins which are critical to major changes in cellular state, including nuclear proteins, transcription factors, cell cycle regulators, kinases, as well as cytoskeletal proteins.[52] Caspase-1 is the prototype of the inflammatory caspases, and a key component of the inflammasome.[8,11] Its central role in inflammation and the potentially harmful consequences of an inappropriate and/or unbalanced activation, justify the existence of tight regulatory mechanisms operating both before and after its synthesis.[55] Despite the existence of alternative pathways,[56,57] the major pathway leading to caspase-1 activation requires the assembly of the inflammasome,[8] and the active form of caspase-1 has only been detected in extracts of IL-1β producing cells.[58] With high resolution immunoelectron microscopy, performed on LPS stimulated human monocytes, both the active and the precursor domains of caspase-1 have been localized in the cytoplasmatic matrix and on the cell surface.[59] Of interest, only small amounts of the active form of caspase-1 are detectable in the intracellular milieu, even when IL-1β actively producing monocytes are tested.[60,61] It has been proposed that the Caspase-1 mediated processing of IL-1β, occurs during the transport of this cytokine across the plasma membrane, followed by rapid secretion in the extra-cellular milieu.[59]
Caspase-1 is initially synthesized as a 45 kDa catalytically inactive zymogen (pro-caspase).[62] Meager amounts of this inactive precursor protein are constitutively produced by monocytic cells,[60] and mainly localized in the cytoplasmatic compartment.[59] The active form of caspase-1 is heterodimeric in structure, and composed by the association of two polypeptides, p20 and p10.[2,3,55,63,64]
Monocytes constitutively express very low levels of caspase-1 mRNA,[60] and its transcripts are also detected in other cells of the immune system, including T and B lymphocytes, and cells of monocytic origin, such as microglia.[65] The transcription of caspase-1 gene, which maps on chromosome 11,[66] is increased upon lipopolysaccharide (LPS) and interferon (IFN)-γ stimulation; however, there is no evidence that higher intracellular mRNA levels result in increased pro-enzyme production.[67,68] In addition, there is recent evidence that leptin induces mRNA expression of caspase-1 in monocytes/macrophages,[69] and that also the pro-inflammatory response mediated by statins in mitogen-activated peripheral blood mononuclear cells is mediated by caspase-1 activation.[70]
Caspase-1 processes and activates proIL-1β
IL-1β is a pro-inflammatory cytokine whose inactive precursor, proIL-1β, is localized in the cytoplasm of monocytes.[71] Caspase-1[1,3–5,72] catalyzes the proteolytic cleavage of proIL-1β, between Asp116 and Ala117, which is necessary for functional activity.[73,74] Maturation and secretion of IL-1β occur in a coordinated fashion, with an unique kinetic.[73] Indeed, caspase-1, participates in both IL-1βprocessing and secretion.[58,59,75] Evidence in support of a role of caspase-1 in IL-1β cleavage and activation includes: 1) production of IL-1β and IL-18 is concordantly blocked in caspase-1 null mice;[76,77] and 2) a selective caspase-1 inhibitor blocks the LPS-induced IL-1β production from human mononuclear cells.[78] The critical role of IL-1β in the control of infections, and the harmful and potentially lethal consequences of an excessive cytokine production and release (i.e endotoxic shock),[79] deserves the existence of tight regulatory mechanisms controlling its transcription, processing, and secretion, as well as the presence of competitive inhibitors of its signaling.[80,81]
IL-1β is a potent pleiotropic pro-inflammatory cytokine, participates in the activation of nuclear factor-kB (NF-kB), mitogen-activated protein kinase (MAPK) pathways[82] and involves in the amplification of the inflammatory cascade.[53] Evidence has been accumulating in the past years on the role of IL-1β in the mechanisms leading to implantation,[83,84] term[13,46,47,49] and preterm labor.[23,50]
Caspase-1 processes IL-18
IL-18, also known as INF-γ-inducing factor, is a recently described cytokine sharing structural homology with the IL-1 family of proteins and functional properties with IL-12.[85–87] IL-18, like IL-1β, is synthesized as 24kDa inactive precursor lacking a signal peptide (proIL-18), which is cleaved after Asp35 by caspase-1 to yield an active 8kD molecule.[78,88] Evidence in support of a role of caspase-1 in IL-18 cleavage and activation includes: 1) caspase-1 deficient mice are defective in LPS induced IL-18 production;[78] 2) a selective caspase-1 inhibitor blocks LPS-induced IL-18 production from human peripheral blood mononuclear cells;[78] 3) Kupffer cells deficient in caspase-1, upon LPS stimulation synthesize the IL-18 precursor but fail to process it into its active form;[88] 4) caspase-1 inhibitors abolish the secretion of mature IL-18 by humans granulocyte macrophages infected with influenza or Sendai virus.[89] However, caspase-1 cleavage of proIL-18 is not exclusive and other proteases, such as proteinase-3, have been recently reported to generate biological activity from IL-18.[90]
IL-18 is an activator of the T helper (Th)-1 response,[91] mainly through the induction of IFN-γ production in both T cells and natural killer (NK) cells.[86] IL-18 enhances T and NK cells maturation and activation,[92] cytokine production,[93,94] and cytotoxicity,[85,95–99] as well as neutrophil activation, reactive oxygen intermediate intermediate synthesis, cytokine release and degranulation.[100,101] IL-18 is involved in the immune defense against bacteria (Chlamydiae,[102,103] Mycoplasmae,[104–106] Mycobacterium Tubercolosis,[107–109] and Leprae,[110] Salmonellae,[111] Shigella,[112] and Yersinia[113]), fungi,[114–116] protozoa[117,118] and viruses.[89,119] Of note, the role of IL-18 in implantation,[120–123] and in the context of microbial invasion of the amniotic fluid,[124] intra-amniotic inflammation[124] and preterm delivery[124,125] have been subject of research.
Amniotic fluid caspase-1 in normal pregnancy
This is the first study reporting that caspase-1 is detectable in the amniotic fluid of normal pregnant women. The sources of the intra-amniotic caspase-1 are still unclear. Caspase-1 may participate in the processing and activation of IL-1β and IL-18 which take place at the maternal-fetal interface, where these cytokines play an autocrine-paracrine role for successful human implantation, pregnancy mantainence,[84,120–122,126] and labor.[13,46–49,127]
Sources of IL-1β during pregnancy include cyto-, syncytio- and intermediate trophoblasts,[47,84,128] macrophages (Hofbauer cells),[47] amniochorionic membranes,[129] decidual stromal[84,128] and NK cells.[128] IL-1β regulates the activity of the matrix metalloproteinase (MMP)-9 which has been linked to cytotrophoblast invasion.[83]
IL-18 (both gene and protein) is constitutively expressed in human chorion and decidua, but not in the amniotic epithelium.[130] Evidence supports a role for IL-18 in modulating uterine NK cell, including their cytokine production and cytolytic activity, as well as in local vascular remodeling, through the induction of the IFN-γ production.[123]
Our finding that caspase-1 was not detectable in any of the mid-trimester samples, in contrast to 76% of amniotic fluid from women at term not in labor is unexpected. Indeed, previous studies have reported that placental IL-1β release, in which caspase-1 may play a role, is high in the first trimester and declines as term gestation approaches, reflecting the invasiveness of the cytotrophoblasts.[83] There are several explanations for this result. First, recent gene array studies have elucidated that during decidualization there is an up-regulation of the gene, mRNA and protein expression of IL-1β but this is not accompanied by a coincidental increase in the secretion of the bioactive form of this cytokine,[131] step requiring caspase-1. Second, it is possible that sources other than cytotrophoblast contribute to the amniotic fluid concentrations of caspase-1. Desquamated fetal epithelia (urinary tract, gastrointestinal or other cells found in normal amniotic fluid) have been proposed to be the major contributors to the amniotic fluid IL-1.[49] If this is true, fetal epithelial cells may contribute to the pool of caspase-1 present in amniotic fluid in greater amount as term approaches. Third, the detection of caspase-1 in the amniotic fluid at term, but not in mid-gestation, is in agreement with the previous report of cell associated IL-1 activity in the amniotic fluid collected in the third but not in second trimester,[49] as well as with the presence of higher IL-18 amniotic fluid concentrations as term approaches.[37]
Amniotic fluid caspase-1 in spontaneous labor at term
Women in spontaneous labor at term had a higher median amniotic fluid concentration of caspase-1 than patients at term not in labor. This finding is consistent with the view that labor at term is an event characterized by activation of the inflammatory cascade.[18,20,132] The pathways leading to the activation of the inflammasome in the context of labor require further investigation. Of note, the higher concentrations of caspase-1 during labor at term mirror the increase in IL-1β concentrations reported in gestational tissues (placenta,[47] chorion,[48] amniotic membranes,[48] decidua[46,48]) and biological fluids (amniotic fluid[13,22,49]), as well as the higher maternal serum[127] and amniotic fluid concentrations[37] of IL-18, when compared to normal term controls. In turn, IL-1β stimulates myometrial contractility by several mechanisms, including: 1) induction of prostaglandin (PG) synthesis (PGE2,[133–135] PGI2,[134] and PGF2[136]) in myometrial cells,[133,134] amnion,[135,136] and choriodecidua;[136] 2) activation of the transcription factor NF-kB, which is functionally linked to the expression of cyclo-oxygenase 2 messenger ribonucleic acid, protein, and PG synthesis;[137] 3) potentiation of the forskolin-promoted cAMP (cyclic-adenosine-monophosphate) production, resulting in cAMP accumulation.[134]
Amniotic fluid caspase-1 in preterm labor
Among patients with preterm labor, those with intra-amniotic infection and/or inflammation had a significantly higher median amniotic fluid caspase-1 concentration than those without intra-amniotic infection and/or inflammation. This finding is in agreement with previous reports supporting a role for two of the cytokines processed by caspase-1, IL-1β and IL-18, in the molecular mechanisms leading to the onset of preterm parturition.[23,37,49,50,124,125]
Evidence of the involvement of IL-1 in preterm labor
A solid body of evidence suggests that IL-1β is implicated in the mechanisms leading to preterm parturition, particularly in the context of intrauterine infection and/or inflammation. There is, indeed, an epidemiologic/causal link between the presence of intraamniotic infection, higher activity and/or concentrations of IL-1β in biological fluids, and higher concentrations of prostaglandins, as supported by the following observations. 1) Our group previously reported that the systemic administration (by subcutaneous injections) of recombinant human IL-1 to timed-pregnant C3H/HeJ inbred mice was followed by parturition within 24 hours in all of the treated mice, and that a premature delivery occurred in all IL-1-injected animals.[50] 2) An immunoradiometric assay, validated for amniotic fluid and with a sensitivity of 50 pg/ml, was capable of detecting IL-1β in the amniotic fluid of all (15/15) pregnant women with preterm labor and intraamniotic infection, versus 47.3% (10/21) of women in preterm labor, negative AF cultures and delivering prematurely, versus 47.2% (17/36) of samples from women with negative amniotic fluid cultures responding to tocolysis. All patients with histopathological signs of chorioamnionitis had detectable IL-1β in the amniotic fluid. Of interest, both IL-1α and IL-1β were significantly higher in women with microbial invasion of the amniotic cavity than in women who delivered prematurely but had negative amniotic fluid cultures (P=0.0001 and P=0.0006 respectively).[23] 3) Patients in preterm labor with intraamniotic infection had a fluid phase IL-1β activity which strongly correlated with the PGE2 and PGF2α amniotic fluid concentrations.[49] An increase in the fluid phase IL-1 activity is detectable also in amniotic fluid from women with spontaneous labor at term, but in this context it is predominantly attributable to IL-1α and not to IL-1β,[49] and only modest elevation in the amniotic fluid concentrations of prostaglandins and their metabolites.[138,139]
In summary, a microbial colonization of the amniotic cavity and the subsequent intra-uterine inflammation may lead to an increase in local production of IL-1β, followed by PG-mediated myometrial contractility. Both the fetus, the mother and the placenta may contribute to the higher amniotic fluid concentrations of IL-1β and caspase-1 in the context of preterm labor. A trans-membranous passage of IL-1 has been demonstrated in our laboratory (unpublished observation). In addition, experimental evidence indicates that supernatants from endotoxin-stimulated human decidua, contain a significantly higher IL-1 bioactivity (attributable both to IL-1α and IL-1β, than supernatants from unstimulated decidua.[140] Furthermore, production of IL-1 from placentas of women in labor, is seventeen-fold higher in the presence of chorioamnionitis.[47]
Evidence of the involvement of IL-18 in preterm labor
Previous investigations on the role of IL-18 in the context of preterm labor have yielded conflicting results. We have previously reported that: 1) both term and preterm parturition were associated with a modest increase in amniotic fluid IL-18 concentrations, although this trend did not reach statistical significance; and that 2) the microbial invasion of the amniotic cavity, in either preterm or term parturition, was associated with a significant increase in the amniotic fluid concentration of IL-18.[37] These findings are in agreement with another previous study in which it was reported that: 1) the median concentrations of IL-18 in cervical mucus and amniotic fluid were higher in women with preterm labor than in women not in labor at term;[124] 2) Among women with preterm labor, the median amniotic fluid concentrations of IL-18 were significantly higher in the presence of microbial invasion of the amniotic cavity and correlated with the indices of intra-amniotic inflammation [defined as increased levels of IL6 (≥1.5 ng/mL) and/or IL-8 (≥1.3 ng/mL)];[124] 3) Women with preterm labor and prompt delivery (delivery within seven days or <34 weeks of gestation) had significantly higher amniotic fluid concentrations of IL-18 than those delivering after several days or >34 weeks.[124] It is of note that the IL-18 gene is constitutively expressed (RT-PCR, in situ hybridization and immunohistochemistry) in human chorion and decidua, whereas the amniotic epithelium is devoid of IL-18 mRNA and protein.[130] However, whether a higher expression of IL-18 is associated with preterm labor is not clear yet, as mice lacking IL-18 (by disruption of the IL-18 gene and/or IL-18 neutralization with intraperitoneal administration of a specific inhibitor of IL-18) have been shown to be more sensitive to LPS-induced preterm delivery and preterm fetal losses than the wild-type counterparts.[125] The role of IL-18 as a negative regulator of TNF-α during sepsis (LPS challenge induces higher serum TNF-α concentrations in the IL-18 −/− mice than in the wild type),[141] may contribute to this unexpected finding.[125]
Caspase-1 inhibitors: implications for further research
Mice and rats deficient in caspase-1 (following administration of a caspase-1 inhibitor or gene deletion) display deficient maturation of pro-IL-1β[77,142–144] and pro-IL-18.[142,143] Of interest, there is evidence that these animals, which are three- to four-fold more sensitive to bacterial infection than wild-type controls,[145] have significantly lower serum concentrations of TNF-α,[144] are resistant to the lethal effects of endotoxins,[77] have a longer survival than controls during experimental pancreatitis,[144] and are less likely to die from E.Coli intraperitoneal injection induced sepsis.[146] Thus, administration of caspase-1 inhibitors has been proposed as a therapeutic strategy in the treatment of local and systemic inflammatory processes, particularly in the context of sepsis.[142,147] Caspase-1 inhibitors are the first orally active agents targeting cytokines, preventing the processing and release of the active forms for IL-1β and IL-18.[142] A blockage of lymphocyte apoptosis,[146] an event associated with the development of sepsis,[148–150] has been proposed as an further mechanism of action of caspase inhibitors, when tested in a model of cecal ligation and puncture.[147]
Of note, it has been proposed that caspase-1 inhibitors may be beneficial in the context of inflammation-related neurological damage. Administration of caspase-1 inhibitors to neonatally infected (E. Coli) rats followed by subsequent LPS challenge, prevented the expected LPS- induced memory impairment. These data suggest that IL-1β participates in the set of immune/inflammatory events resulting from neonatal infection and which likely to contribute to cognitive alterations.[151] In addition, caspase-1 inhibitors reduced apoptosis, increased proliferation and enhanced survival of transplanted stem cells.[152] This has considerable implications for the treatment of infection/inflammation induced perinatal brain injury.
This study focuses on the immunoreactive Caspase-1 concentrations in amniotic fluid. Further studies, investigating the functional or biological activity of Caspase-1 in the same milieu or in other maternal/fetal biological fluids, will contribute to clarifying the role of this enzyme in normal pregnancy, as well as in term and preterm parturition.
Acknowledgments
This research was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS.
Reference List
- 1.Cerretti DP, Kozlosky CJ, Mosley B, Nelson N, Van Ness K, Greenstreet TA, March CJ, Kronheim SR, Druck T, Cannizzaro LA, et al. Molecular cloning of the interleukin-1 beta converting enzyme. Science. 1992;256:97–100. doi: 10.1126/science.1373520. [DOI] [PubMed] [Google Scholar]
- 2.Miller DK, Ayala JM, Egger LA, Raju SM, Yamin TT, Ding GJ, Gaffney EP, Howard AD, Palyha OC, Rolando AM, et al. Purification and characterization of active human interleukin-1 beta-converting enzyme from THP.1 monocytic cells. J Biol Chem. 1993;268:18062–18069. [PubMed] [Google Scholar]
- 3.Thornberry NA, Bull HG, Calaycay JR, Chapman KT, Howard AD, Kostura MJ, Miller DK, Molineaux SM, Weidner JR, Aunins J, et al. A novel heterodimeric cysteine protease is required for interleukin-1 beta processing in monocytes. Nature. 1992;356:768–774. doi: 10.1038/356768a0. [DOI] [PubMed] [Google Scholar]
- 4.Kostura MJ, Tocci MJ, Limjuco G, Chin J, Cameron P, Hillman AG, Chartrain NA, Schmidt JA. Identification of a monocyte specific pre-interleukin 1 beta convertase activity. Proc Natl Acad Sci U S A. 1989;86:5227–5231. doi: 10.1073/pnas.86.14.5227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alnemri ES, Livingston DJ, Nicholson DW, Salvesen G, Thornberry NA, Wong WW, Yuan J. Human ICE/CED-3 protease nomenclature. Cell. 1996;87:171. doi: 10.1016/s0092-8674(00)81334-3. [DOI] [PubMed] [Google Scholar]
- 6.Mariathasan S, Newton K, Monack DM, Vucic D, French DM, Lee WP, Roose-Girma M, Erickson S, Dixit VM. Differential activation of the inflammasome by caspase-1 adaptors ASC and Ipaf. Nature. 2004;430:213–218. doi: 10.1038/nature02664. [DOI] [PubMed] [Google Scholar]
- 7.Matute-Bello G. Targeting caspase-1 in sepsis: a novel approach to an old problem. Intensive Care Med. 2007;33:755–757. doi: 10.1007/s00134-007-0589-z. [DOI] [PubMed] [Google Scholar]
- 8.Martinon F, Burns K, Tschopp J. The inflammasome: a molecular platform triggering activation of inflammatory caspases and processing of proIL-beta. Mol Cell. 2002;10:417–426. doi: 10.1016/s1097-2765(02)00599-3. [DOI] [PubMed] [Google Scholar]
- 9.Petrilli V, Dostert C, Muruve DA, Tschopp J. The inflammasome: a danger sensing complex triggering innate immunity. Curr Opin Immunol. 2007;19:615–622. doi: 10.1016/j.coi.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Ogura Y, Sutterwala FS, Flavell RA. The inflammasome: first line of the immune response to cell stress. Cell. 2006;126:659–662. doi: 10.1016/j.cell.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 11.Martinon F, Tschopp J. Inflammatory caspases and inflammasomes: master switches of inflammation. Cell Death Differ. 2007;14:10–22. doi: 10.1038/sj.cdd.4402038. [DOI] [PubMed] [Google Scholar]
- 12.Meylan E, Tschopp J, Karin M. Intracellular pattern recognition receptors in the host response. Nature. 2006;442:39–44. doi: 10.1038/nature04946. [DOI] [PubMed] [Google Scholar]
- 13.Romero R, Parvizi ST, Oyarzun E, Mazor M, Wu YK, Avila C, Athanassiadis AP, Mitchell MD. Amniotic fluid interleukin-1 in spontaneous labor at term. J Reprod Med. 1990;35:235–238. [PubMed] [Google Scholar]
- 14.Dudley DJ. Pre-term labor: an intra-uterine inflammatory response syndrome? J Reprod Immunol. 1997;36:93–109. doi: 10.1016/s0165-0378(97)00065-x. [DOI] [PubMed] [Google Scholar]
- 15.Hagberg H, Mallard C, Jacobsson B. Role of cytokines in preterm labour and brain injury. BJOG. 2005;112 (Suppl 1):16–18. doi: 10.1111/j.1471-0528.2005.00578.x. [DOI] [PubMed] [Google Scholar]
- 16.Chan EC, Fraser S, Yin S, Yeo G, Kwek K, Fairclough RJ, Smith R. Human myometrial genes are differentially expressed in labor: a suppression subtractive hybridization study. J Clin Endocrinol Metab. 2002;87:2435–2441. doi: 10.1210/jcem.87.6.8439. [DOI] [PubMed] [Google Scholar]
- 17.Bisits AM, Smith R, Mesiano S, Yeo G, Kwek K, MacIntyre D, Chan EC. Inflammatory aetiology of human myometrial activation tested using directed graphs. PLoS Comput Biol. 2005;1:132–136. doi: 10.1371/journal.pcbi.0010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Romero R, Espinoza J, Goncalves LF, Kusanovic JP, Friel LA, Nien JK. Inflammation in preterm and term labour and delivery. Semin Fetal Neonatal Med. 2006;11:317–326. doi: 10.1016/j.siny.2006.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haddad R, Tromp G, Kuivaniemi H, Chaiworapongsa T, Kim YM, Mazor M, Romero R. Human spontaneous labor without histologic chorioamnionitis is characterized by an acute inflammation gene expression signature. Am J Obstet Gynecol. 2006;195:394–24. doi: 10.1016/j.ajog.2005.08.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Norman JE, Bollapragada S, Yuan M, Nelson SM. Inflammatory pathways in the mechanism of parturition. BMC Pregnancy Childbirth. 2007;7 (Suppl 1):S7. doi: 10.1186/1471-2393-7-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Romero R, Espinoza J, Goncalves LF, Kusanovic JP, Friel L, Hassan S. The role of inflammation and infection in preterm birth. Semin Reprod Med. 2007;25:21–39. doi: 10.1055/s-2006-956773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keelan JA, Marvin KW, Sato TA, Coleman M, McCowan LM, Mitchell MD. Cytokine abundance in placental tissues: evidence of inflammatory activation in gestational membranes with term and preterm parturition. Am J Obstet Gynecol. 1999;181:1530–1536. doi: 10.1016/s0002-9378(99)70400-x. [DOI] [PubMed] [Google Scholar]
- 23.Romero R, Mazor M, Brandt F, Sepulveda W, Avila C, Cotton DB, Dinarello CA. Interleukin-1 alpha and interleukin-1 beta in preterm and term human parturition. Am J Reprod Immunol. 1992;27:117–123. doi: 10.1111/j.1600-0897.1992.tb00737.x. [DOI] [PubMed] [Google Scholar]
- 24.Romero R, Tartakovsky B. The natural interleukin-1 receptor antagonist prevents interleukin-1-induced preterm delivery in mice. Am J Obstet Gynecol. 1992;167:1041–1045. doi: 10.1016/s0002-9378(12)80035-4. [DOI] [PubMed] [Google Scholar]
- 25.Romero R, Sepulveda W, Mazor M, Brandt F, Cotton DB, Dinarello CA, Mitchell MD. The natural interleukin-1 receptor antagonist in term and preterm parturition. Am J Obstet Gynecol. 1992;167:863–872. doi: 10.1016/s0002-9378(12)80003-2. [DOI] [PubMed] [Google Scholar]
- 26.Winkler M, Kemp B, Fischer DC, Maul H, Hlubek M, Rath W. Tissue concentrations of cytokines in the lower uterine segment during preterm parturition. J Perinat Med. 2001;29:519–527. doi: 10.1515/JPM.2001.072. [DOI] [PubMed] [Google Scholar]
- 27.Fidel PL, Jr, Romero R, Wolf N, Cutright J, Ramirez M, Araneda H, Cotton DB. Systemic and local cytokine profiles in endotoxin-induced preterm parturition in mice. Am J Obstet Gynecol. 1994;170:1467–1475. doi: 10.1016/s0002-9378(94)70180-6. [DOI] [PubMed] [Google Scholar]
- 28.Romero R, Avila C, Santhanam U, Sehgal PB. Amniotic fluid interleukin 6 in preterm labor. Association with infection. J Clin Invest. 1990;85:1392–1400. doi: 10.1172/JCI114583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Romero R, Sepulveda W, Kenney JS, Archer LE, Allison AC, Sehgal PB. Interleukin 6 determination in the detection of microbial invasion of the amniotic cavity. Ciba Found Symp. 1992;167:205–220. doi: 10.1002/9780470514269.ch13. [DOI] [PubMed] [Google Scholar]
- 30.Romero R, Yoon BH, Kenney JS, Gomez R, Allison AC, Sehgal PB. Amniotic fluid interleukin-6 determinations are of diagnostic and prognostic value in preterm labor. Am J Reprod Immunol. 1993;30:167–183. doi: 10.1111/j.1600-0897.1993.tb00618.x. [DOI] [PubMed] [Google Scholar]
- 31.Romero R, Manogue KR, Mitchell MD, Wu YK, Oyarzun E, Hobbins JC, Cerami A. Infection and labor. IV. Cachectin-tumor necrosis factor in the amniotic fluid of women with intraamniotic infection and preterm labor. Am J Obstet Gynecol. 1989;161:336–341. doi: 10.1016/0002-9378(89)90515-2. [DOI] [PubMed] [Google Scholar]
- 32.Romero R, Mazor M, Sepulveda W, Avila C, Copeland D, Williams J. Tumor necrosis factor in preterm and term labor. Am J Obstet Gynecol. 1992;166:1576–1587. doi: 10.1016/0002-9378(92)91636-o. [DOI] [PubMed] [Google Scholar]
- 33.Baumann P, Romero R, Berry S, Gomez R, McFarlin B, Araneda H, Cotton DB, Fidel P. Evidence of participation of the soluble tumor necrosis factor receptor I in the host response to intrauterine infection in preterm labor. Am J Reprod Immunol. 1993;30:184–193. doi: 10.1111/j.1600-0897.1993.tb00619.x. [DOI] [PubMed] [Google Scholar]
- 34.Maymon E, Ghezzi F, Edwin SS, Mazor M, Yoon BH, Gomez R, Romero R. The tumor necrosis factor alpha and its soluble receptor profile in term and preterm parturition. Am J Obstet Gynecol. 1999;181:1142–1148. doi: 10.1016/s0002-9378(99)70097-9. [DOI] [PubMed] [Google Scholar]
- 35.Fortunato SJ, Menon R, Lombardi SJ. Role of tumor necrosis factor-alpha in the premature rupture of membranes and preterm labor pathways. Am J Obstet Gynecol. 2002;187:1159–1162. doi: 10.1067/mob.2002.127457. [DOI] [PubMed] [Google Scholar]
- 36.Lonergan M, Aponso D, Marvin KW, Helliwell RJ, Sato TA, Mitchell MD, Chaiwaropongsa T, Romero R, Keelan JA. Tumor necrosis factor-related apoptosis-inducing ligand (TRAIL), TRAIL receptors, and the soluble receptor osteoprotegerin in human gestational membranes and amniotic fluid during pregnancy and labor at term and preterm. J Clin Endocrinol Metab. 2003;88:3835–3844. doi: 10.1210/jc.2002-021905. [DOI] [PubMed] [Google Scholar]
- 37.Pacora P, Romero R, Maymon E, Gervasi MT, Gomez R, Edwin SS, Yoon BH. Participation of the novel cytokine interleukin 18 in the host response to intra-amniotic infection. Am J Obstet Gynecol. 2000;183:1138–1143. doi: 10.1067/mob.2000.108881. [DOI] [PubMed] [Google Scholar]
- 38.Athayde N, Romero R, Maymon E, Gomez R, Pacora P, Yoon BH, Edwin SS. Interleukin 16 in pregnancy, parturition, rupture of fetal membranes, and microbial invasion of the amniotic cavity. Am J Obstet Gynecol. 2000;182:135–141. doi: 10.1016/s0002-9378(00)70502-3. [DOI] [PubMed] [Google Scholar]
- 39.Romero R, Ceska M, Avila C, Mazor M, Behnke E, Lindley I. Neutrophil attractant/activating peptide-1/interleukin-8 in term and preterm parturition. Am J Obstet Gynecol. 1991;165:813–820. doi: 10.1016/0002-9378(91)90422-n. [DOI] [PubMed] [Google Scholar]
- 40.Cherouny PH, Pankuch GA, Romero R, Botti JJ, Kuhn DC, Demers LM, Appelbaum PC. Neutrophil attractant/activating peptide-1/interleukin-8: association with histologic chorioamnionitis, preterm delivery, and bioactive amniotic fluid leukoattractants. Am J Obstet Gynecol. 1993;169:1299–1303. doi: 10.1016/0002-9378(93)90297-v. [DOI] [PubMed] [Google Scholar]
- 41.Romero R, Gomez R, Galasso M, Munoz H, Acosta L, Yoon BH, Svinarich D, Cotton DB. Macrophage inflammatory protein-1 alpha in term and preterm parturition: effect of microbial invasion of the amniotic cavity. Am J Reprod Immunol. 1994;32:108–113. doi: 10.1111/j.1600-0897.1994.tb01101.x. [DOI] [PubMed] [Google Scholar]
- 42.Athayde N, Romero R, Maymon E, Gomez R, Pacora P, Araneda H, Yoon BH. A role for the novel cytokine RANTES in pregnancy and parturition. Am J Obstet Gynecol. 1999;181:989–994. doi: 10.1016/s0002-9378(99)70337-6. [DOI] [PubMed] [Google Scholar]
- 43.Gonzalez BE, Ferrer I, Valls C, Borras M, Lailla JM. The value of interleukin-8, interleukin-6 and interleukin-1beta in vaginal wash as predictors of preterm delivery. Gynecol Obstet Invest. 2005;59:175–178. doi: 10.1159/000084279. [DOI] [PubMed] [Google Scholar]
- 44.Esplin MS, Romero R, Chaiworapongsa T, Kim YM, Edwin S, Gomez R, Mazor M, Adashi EY. Monocyte chemotactic protein-1 is increased in the amniotic fluid of women who deliver preterm in the presence or absence of intra-amniotic infection. J Matern Fetal Neonatal Med. 2005;17:365–373. doi: 10.1080/14767050500141329. [DOI] [PubMed] [Google Scholar]
- 45.Esplin MS, Peltier MR, Hamblin S, Smith S, Fausett MB, Dildy GA, Branch DW, Silver RM, Adashi EY. Monocyte chemotactic protein-1 expression is increased in human gestational tissues during term and preterm labor. Placenta. 2005;26:661–671. doi: 10.1016/j.placenta.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 46.Ammala M, Nyman T, Salmi A, Rutanen EM. The interleukin-1 system in gestational tissues at term: effect of labour. Placenta. 1997;18:717–723. doi: 10.1016/s0143-4004(97)90014-x. [DOI] [PubMed] [Google Scholar]
- 47.Taniguchi T, Matsuzaki N, Kameda T, Shimoya K, Jo T, Saji F, Tanizawa O. The enhanced production of placental interleukin-1 during labor and intrauterine infection. Am J Obstet Gynecol. 1991;165:131–137. doi: 10.1016/0002-9378(91)90241-i. [DOI] [PubMed] [Google Scholar]
- 48.Dudley DJ, Collmer D, Mitchell MD, Trautman MS. Inflammatory cytokine mRNA in human gestational tissues: implications for term and preterm labor. J Soc Gynecol Investig. 1996;3:328–335. [PubMed] [Google Scholar]
- 49.Romero R, Brody DT, Oyarzun E, Mazor M, Wu YK, Hobbins JC, Durum SK. Infection and labor. III. Interleukin-1: a signal for the onset of parturition. Am J Obstet Gynecol. 1989;160:1117–1123. doi: 10.1016/0002-9378(89)90172-5. [DOI] [PubMed] [Google Scholar]
- 50.Romero R, Mazor M, Tartakovsky B. Systemic administration of interleukin-1 induces preterm parturition in mice. Am J Obstet Gynecol. 1991;165:969–971. doi: 10.1016/0002-9378(91)90450-6. [DOI] [PubMed] [Google Scholar]
- 51.Sadowsky DW, Adams KM, Gravett MG, Witkin SS, Novy MJ. Preterm labor is induced by intraamniotic infusions of interleukin-1beta and tumor necrosis factor-alpha but not by interleukin-6 or interleukin-8 in a nonhuman primate model. Am J Obstet Gynecol. 2006;195:1578–1589. doi: 10.1016/j.ajog.2006.06.072. [DOI] [PubMed] [Google Scholar]
- 52.Nhan TQ, Liles WC, Schwartz SM. Physiological functions of caspases beyond cell death. Am J Pathol. 2006;169:729–737. doi: 10.2353/ajpath.2006.060105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Creagh EM, Conroy H, Martin SJ. Caspase-activation pathways in apoptosis and immunity. Immunol Rev. 2003;193:10–21. doi: 10.1034/j.1600-065x.2003.00048.x. [DOI] [PubMed] [Google Scholar]
- 54.Joshi VD, Kalvakolanu DV, Cross AS. Simultaneous activation of apoptosis and inflammation in pathogenesis of septic shock: a hypothesis. FEBS Lett. 2003;555:180–184. doi: 10.1016/s0014-5793(03)01271-7. [DOI] [PubMed] [Google Scholar]
- 55.Wilson KP, Black JA, Thomson JA, Kim EE, Griffith JP, Navia MA, Murcko MA, Chambers SP, Aldape RA, Raybuck SA, et al. Structure and mechanism of interleukin-1 beta converting enzyme. Nature. 1994;370:270–275. doi: 10.1038/370270a0. [DOI] [PubMed] [Google Scholar]
- 56.Hersh D, Monack DM, Smith MR, Ghori N, Falkow S, Zychlinsky A. The Salmonella invasin SipB induces macrophage apoptosis by binding to caspase-1. Proc Natl Acad Sci U S A. 1999;96:2396–2401. doi: 10.1073/pnas.96.5.2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hilbi H, Moss JE, Hersh D, Chen Y, Arondel J, Banerjee S, Flavell RA, Yuan J, Sansonetti PJ, Zychlinsky A. Shigella-induced apoptosis is dependent on caspase-1 which binds to IpaB. J Biol Chem. 1998;273:32895–32900. doi: 10.1074/jbc.273.49.32895. [DOI] [PubMed] [Google Scholar]
- 58.Tocci MJ. Structure and function of interleukin-1 beta converting enzyme. Vitam Horm. 1997;53:27–63. doi: 10.1016/s0083-6729(08)60703-7. [DOI] [PubMed] [Google Scholar]
- 59.Singer II, Scott S, Chin J, Bayne EK, Limjuco G, Weidner J, Miller DK, Chapman K, Kostura MJ. The interleukin-1 beta-converting enzyme (ICE) is localized on the external cell surface membranes and in the cytoplasmic ground substance of human monocytes by immuno-electron microscopy. J Exp Med. 1995;182:1447–1459. doi: 10.1084/jem.182.5.1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ayala JM, Yamin TT, Egger LA, Chin J, Kostura MJ, Miller DK. IL-1 beta-converting enzyme is present in monocytic cells as an inactive 45-kDa precursor. J Immunol. 1994;153:2592–2599. [PubMed] [Google Scholar]
- 61.Miossec C, Decoen MC, Durand L, Fassy F, Diu-Hercend A. Use of monoclonal antibodies to study interleukin-1 beta-converting enzyme expression: only precursor forms are detected in interleukin-1 beta-secreting cells. Eur J Immunol. 1996;26:1032–1042. doi: 10.1002/eji.1830260512. [DOI] [PubMed] [Google Scholar]
- 62.Earnshaw WC, Martins LM, Kaufmann SH. Mammalian caspases: structure, activation, substrates, and functions during apoptosis. Annu Rev Biochem. 1999;68:383–424. doi: 10.1146/annurev.biochem.68.1.383. [DOI] [PubMed] [Google Scholar]
- 63.Nicholson DW, Ali A, Thornberry NA, Vaillancourt JP, Ding CK, Gallant M, Gareau Y, Griffin PR, Labelle M, Lazebnik YA, et al. Identification and inhibition of the ICE/CED-3 protease necessary for mammalian apoptosis. Nature. 1995;376:37–43. doi: 10.1038/376037a0. [DOI] [PubMed] [Google Scholar]
- 64.Walker NP, Talanian RV, Brady KD, Dang LC, Bump NJ, Ferenz CR, Franklin S, Ghayur T, Hackett MC, Hammill LD, et al. Crystal structure of the cysteine protease interleukin-1 beta-converting enzyme: a (p20/p10)2 homodimer. Cell. 1994;78:343–352. doi: 10.1016/0092-8674(94)90303-4. [DOI] [PubMed] [Google Scholar]
- 65.Moran LB, Duke DC, Graeber MB. The microglial gene regulatory network activated by interferon-gamma. J Neuroimmunol. 2007;183:1–6. doi: 10.1016/j.jneuroim.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 66.Cerretti DP, Hollingsworth LT, Kozlosky CJ, Valentine MB, Shapiro DN, Morris SW, Nelson N. Molecular characterization of the gene for human interleukin-1 beta converting enzyme (IL1BC) Genomics. 1994;20:468–473. doi: 10.1006/geno.1994.1202. [DOI] [PubMed] [Google Scholar]
- 67.Nett MA, Cerretti DP, Berson DR, Seavitt J, Gilbert DJ, Jenkins NA, Copeland NG, Black RA, Chaplin DD. Molecular cloning of the murine IL-1 beta converting enzyme cDNA. J Immunol. 1992;149:3254–3259. [PubMed] [Google Scholar]
- 68.Keane KM, Giegel DA, Lipinski WJ, Callahan MJ, Shivers BD. Cloning, tissue expression and regulation of rat interleukin 1 beta converting enzyme. Cytokine. 1995;7:105–110. doi: 10.1006/cyto.1995.1014. [DOI] [PubMed] [Google Scholar]
- 69.Ahmed M, Shaban Z, Yamaji D, Okamatsu-Ogura Y, Soliman M, Abd EM, Ishioka K, Makondo K, Saito M, Kimura K. Induction of proinflammatory cytokines and caspase-1 by leptin in monocyte/macrophages from holstein cows. J Vet Med Sci. 2007;69:509–514. doi: 10.1292/jvms.69.509. [DOI] [PubMed] [Google Scholar]
- 70.Coward WR, Marei A, Yang A, Vasa-Nicotera MM, Chow SC. Statin-induced proinflammatory response in mitogen-activated peripheral blood mononuclear cells through the activation of caspase-1 and IL-18 secretion in monocytes. J Immunol. 2006;176:5284–5292. doi: 10.4049/jimmunol.176.9.5284. [DOI] [PubMed] [Google Scholar]
- 71.Singer II, Scott S, Hall GL, Limjuco G, Chin J, Schmidt JA. Interleukin 1 beta is localized in the cytoplasmic ground substance but is largely absent from the Golgi apparatus and plasma membranes of stimulated human monocytes. J Exp Med. 1988;167:389–407. doi: 10.1084/jem.167.2.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Black RA, Kronheim SR, Sleath PR. Activation of interleukin-1 beta by a co-induced protease. FEBS Lett. 1989;247:386–390. doi: 10.1016/0014-5793(89)81376-6. [DOI] [PubMed] [Google Scholar]
- 73.Hazuda DJ, Lee JC, Young PR. The kinetics of interleukin 1 secretion from activated monocytes. Differences between interleukin 1 alpha and interleukin 1 beta. J Biol Chem. 1988;263:8473–8479. [PubMed] [Google Scholar]
- 74.Black RA, Kronheim SR, Cantrell M, Deeley MC, March CJ, Prickett KS, Wignall J, Conlon PJ, Cosman D, Hopp TP, et al. Generation of biologically active interleukin-1 beta by proteolytic cleavage of the inactive precursor. J Biol Chem. 1988;263:9437–9442. [PubMed] [Google Scholar]
- 75.Howard AD, Palyha OC, Griffin PR, Peterson EP, Lenny AB, Ding GJ, Pickup DJ, Thornberry NA, Schmidt JA, Tocci MJ. Human IL-1 beta processing and secretion in recombinant baculovirus-infected Sf9 cells is blocked by the cowpox virus serpin crmA. J Immunol. 1995;154:2321–2332. [PubMed] [Google Scholar]
- 76.Kuida K, Lippke JA, Ku G, Harding MW, Livingston DJ, Su MS, Flavell RA. Altered cytokine export and apoptosis in mice deficient in interleukin-1 beta converting enzyme. Science. 1995;267:2000–2003. doi: 10.1126/science.7535475. [DOI] [PubMed] [Google Scholar]
- 77.Li P, Allen H, Banerjee S, Franklin S, Herzog L, Johnston C, McDowell J, Paskind M, Rodman L, Salfeld J, et al. Mice deficient in IL-1 beta-converting enzyme are defective in production of mature IL-1 beta and resistant to endotoxic shock. Cell. 1995;80:401–411. doi: 10.1016/0092-8674(95)90490-5. [DOI] [PubMed] [Google Scholar]
- 78.Ghayur T, Banerjee S, Hugunin M, Butler D, Herzog L, Carter A, Quintal L, Sekut L, Talanian R, Paskind M, et al. Caspase-1 processes IFN-gamma-inducing factor and regulates LPS-induced IFN-gamma production. Nature. 1997;386:619–623. doi: 10.1038/386619a0. [DOI] [PubMed] [Google Scholar]
- 79.Beutler B, Cerami A. The endogenous mediator of endotoxic shock. Clin Res. 1987;35:192–197. [PubMed] [Google Scholar]
- 80.Mantovani A, Muzio M, Ghezzi P, Colotta C, Introna M. Regulation of inhibitory pathways of the interleukin-1 system. Ann N Y Acad Sci. 1998;840:338–351. doi: 10.1111/j.1749-6632.1998.tb09573.x. [DOI] [PubMed] [Google Scholar]
- 81.Burns K, Martinon F, Tschopp J. New insights into the mechanism of IL-1beta maturation. Curr Opin Immunol. 2003;15:26–30. doi: 10.1016/s0952-7915(02)00017-1. [DOI] [PubMed] [Google Scholar]
- 82.Dinarello CA. Interleukin-1 beta, interleukin-18, and the interleukin-1 beta converting enzyme. Ann N Y Acad Sci. 1998;856:1–11. doi: 10.1111/j.1749-6632.1998.tb08307.x. [DOI] [PubMed] [Google Scholar]
- 83.Librach CL, Feigenbaum SL, Bass KE, Cui TY, Verastas N, Sadovsky Y, Quigley JP, French DL, Fisher SJ. Interleukin-1 beta regulates human cytotrophoblast metalloproteinase activity and invasion in vitro. J Biol Chem. 1994;269:17125–17131. [PubMed] [Google Scholar]
- 84.Simon C, Frances A, Piquette G, Hendrickson M, Milki A, Polan ML. Interleukin-1 system in the materno-trophoblast unit in human implantation: immunohistochemical evidence for autocrine/paracrine function. J Clin Endocrinol Metab. 1994;78:847–854. doi: 10.1210/jcem.78.4.8157710. [DOI] [PubMed] [Google Scholar]
- 85.Okamura H, Tsutsi H, Komatsu T, Yutsudo M, Hakura A, Tanimoto T, Torigoe K, Okura T, Nukada Y, Hattori K, et al. Cloning of a new cytokine that induces IFN-gamma production by T cells. Nature. 1995;378:88–91. doi: 10.1038/378088a0. [DOI] [PubMed] [Google Scholar]
- 86.Dinarello CA. IL-18: A TH1-inducing, proinflammatory cytokine and new member of the IL-1 family. J Allergy Clin Immunol. 1999;103:11–24. doi: 10.1016/s0091-6749(99)70518-x. [DOI] [PubMed] [Google Scholar]
- 87.Ushio S, Namba M, Okura T, Hattori K, Nukada Y, Akita K, Tanabe F, Konishi K, Micallef M, Fujii M, et al. Cloning of the cDNA for human IFN-gamma-inducing factor, expression in Escherichia coli, and studies on the biologic activities of the protein. J Immunol. 1996;156:4274–4279. [PubMed] [Google Scholar]
- 88.Gu Y, Kuida K, Tsutsui H, Ku G, Hsiao K, Fleming MA, Hayashi N, Higashino K, Okamura H, Nakanishi K, et al. Activation of interferon-gamma inducing factor mediated by interleukin-1beta converting enzyme. Science. 1997;275:206–209. doi: 10.1126/science.275.5297.206. [DOI] [PubMed] [Google Scholar]
- 89.Pirhonen J, Sareneva T, Kurimoto M, Julkunen I, Matikainen S. Virus infection activates IL-1 beta and IL-18 production in human macrophages by a caspase-1-dependent pathway. J Immunol. 1999;162:7322–7329. [PubMed] [Google Scholar]
- 90.Sugawara S, Uehara A, Nochi T, Yamaguchi T, Ueda H, Sugiyama A, Hanzawa K, Kumagai K, Okamura H, Takada H. Neutrophil proteinase 3-mediated induction of bioactive IL-18 secretion by human oral epithelial cells. J Immunol. 2001;167:6568–6575. doi: 10.4049/jimmunol.167.11.6568. [DOI] [PubMed] [Google Scholar]
- 91.Takeda K, Tsutsui H, Yoshimoto T, Adachi O, Yoshida N, Kishimoto T, Okamura H, Nakanishi K, Akira S. Defective NK cell activity and Th1 response in IL-18-deficient mice. Immunity. 1998;8:383–390. doi: 10.1016/s1074-7613(00)80543-9. [DOI] [PubMed] [Google Scholar]
- 92.Gracie JA, Robertson SE, McInnes IB. Interleukin-18. J Leukoc Biol. 2003;73:213–224. doi: 10.1189/jlb.0602313. [DOI] [PubMed] [Google Scholar]
- 93.Hoshino T, Wiltrout RH, Young HA. IL-18 is a potent coinducer of IL-13 in NK and T cells: a new potential role for IL-18 in modulating the immune response. J Immunol. 1999;162:5070–5077. [PubMed] [Google Scholar]
- 94.Hoshino T, Yagita H, Ortaldo JR, Wiltrout RH, Young HA. In vivo administration of IL-18 can induce IgE production through Th2 cytokine induction and up-regulation of CD40 ligand (CD154) expression on CD4+ T cells. Eur J Immunol. 2000;30:1998–2006. doi: 10.1002/1521-4141(200007)30:7<1998::AID-IMMU1998>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 95.Tsutsui H, Nakanishi K, Matsui K, Higashino K, Okamura H, Miyazawa Y, Kaneda K. IFN-gamma-inducing factor up-regulates Fas ligand-mediated cytotoxic activity of murine natural killer cell clones. J Immunol. 1996;157:3967–3973. [PubMed] [Google Scholar]
- 96.Dao T, Ohashi K, Kayano T, Kurimoto M, Okamura H. Interferon-gamma-inducing factor, a novel cytokine, enhances Fas ligand-mediated cytotoxicity of murine T helper 1 cells. Cell Immunol. 1996;173:230–235. doi: 10.1006/cimm.1996.0272. [DOI] [PubMed] [Google Scholar]
- 97.Yoshimoto T, Takeda K, Tanaka T, Ohkusu K, Kashiwamura S, Okamura H, Akira S, Nakanishi K. IL-12 up-regulates IL-18 receptor expression on T cells, Th1 cells, and B cells: synergism with IL-18 for IFN-gamma production. J Immunol. 1998;161:3400–3407. [PubMed] [Google Scholar]
- 98.Micallef MJ, Ohtsuki T, Kohno K, Tanabe F, Ushio S, Namba M, Tanimoto T, Torigoe K, Fujii M, Ikeda M, et al. Interferon-gamma-inducing factor enhances T helper 1 cytokine production by stimulated human T cells: synergism with interleukin-12 for interferon-gamma production. Eur J Immunol. 1996;26:1647–1651. doi: 10.1002/eji.1830260736. [DOI] [PubMed] [Google Scholar]
- 99.Dao T, Mehal WZ, Crispe IN. IL-18 augments perforin-dependent cytotoxicity of liver NK-T cells. J Immunol. 1998;161:2217–2222. [PubMed] [Google Scholar]
- 100.Gracie JA, Forsey RJ, Chan WL, Gilmour A, Leung BP, Greer MR, Kennedy K, Carter R, Wei XQ, Xu D, et al. A proinflammatory role for IL-18 in rheumatoid arthritis. J Clin Invest. 1999;104:1393–1401. doi: 10.1172/JCI7317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Leung BP, Culshaw S, Gracie JA, Hunter D, Canetti CA, Campbell C, Cunha F, Liew FY, McInnes IB. A role for IL-18 in neutrophil activation. J Immunol. 2001;167:2879–2886. doi: 10.4049/jimmunol.167.5.2879. [DOI] [PubMed] [Google Scholar]
- 102.Hook CE, Matyszak MK, Gaston JS. Infection of epithelial and dendritic cells by Chlamydia trachomatis results in IL-18 and IL-12 production, leading to interferon-gamma production by human natural killer cells. FEMS Immunol Med Microbiol. 2005;45:113–120. doi: 10.1016/j.femsim.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 103.Lu H, Shen C, Brunham RC. Chlamydia trachomatis infection of epithelial cells induces the activation of caspase-1 and release of mature IL-18. J Immunol. 2000;165:1463–1469. doi: 10.4049/jimmunol.165.3.1463. [DOI] [PubMed] [Google Scholar]
- 104.Muneta Y, Minagawa Y, Shimoji Y, Nagata R, Markham PF, Browning GF, Mori Y. IL-18 expression in pigs following infection with Mycoplasma hyopneumoniae. J Interferon Cytokine Res. 2006;26:637–644. doi: 10.1089/jir.2006.26.637. [DOI] [PubMed] [Google Scholar]
- 105.Tanaka H, Narita M, Teramoto S, Saikai T, Oashi K, Igarashi T, Abe S. Role of interleukin-18 and T-helper type 1 cytokines in the development of Mycoplasma pneumoniae pneumonia in adults. Chest. 2002;121:1493–1497. doi: 10.1378/chest.121.5.1493. [DOI] [PubMed] [Google Scholar]
- 106.Narita M, Tanaka H, Abe S, Yamada S, Kubota M, Togashi T. Close association between pulmonary disease manifestation in Mycoplasma pneumoniae infection and enhanced local production of interleukin-18 in the lung, independent of gamma interferon. Clin Diagn Lab Immunol. 2000;7:909–914. doi: 10.1128/cdli.7.6.909-914.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kinjo Y, Kawakami K, Uezu K, Yara S, Miyagi K, Koguchi Y, Hoshino T, Okamoto M, Kawase Y, Yokota K, et al. Contribution of IL-18 to Th1 response and host defense against infection by Mycobacterium tuberculosis: a comparative study with IL-12p40. J Immunol. 2002;169:323–329. doi: 10.4049/jimmunol.169.1.323. [DOI] [PubMed] [Google Scholar]
- 108.Vankayalapati R, Wizel B, Weis SE, Samten B, Girard WM, Barnes PF. Production of interleukin-18 in human tuberculosis. J Infect Dis. 2000;182:234–239. doi: 10.1086/315656. [DOI] [PubMed] [Google Scholar]
- 109.Yamada G, Shijubo N, Shigehara K, Okamura H, Kurimoto M, Abe S. Increased levels of circulating interleukin-18 in patients with advanced tuberculosis. Am J Respir Crit Care Med. 2000;161:1786–1789. doi: 10.1164/ajrccm.161.6.9911054. [DOI] [PubMed] [Google Scholar]
- 110.Garcia VE, Uyemura K, Sieling PA, Ochoa MT, Morita CT, Okamura H, Kurimoto M, Rea TH, Modlin RL. IL-18 promotes type 1 cytokine production from NK cells and T cells in human intracellular infection. J Immunol. 1999;162:6114–6121. [PubMed] [Google Scholar]
- 111.Mastroeni P, Clare S, Khan S, Harrison JA, Hormaeche CE, Okamura H, Kurimoto M, Dougan G. Interleukin 18 contributes to host resistance and gamma interferon production in mice infected with virulent Salmonella typhimurium. Infect Immun. 1999;67:478–483. doi: 10.1128/iai.67.2.478-483.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sansonetti PJ, Phalipon A, Arondel J, Thirumalai K, Banerjee S, Akira S, Takeda K, Zychlinsky A. Caspase-1 activation of IL-1beta and IL-18 are essential for Shigella flexneri-induced inflammation. Immunity. 2000;12:581–590. doi: 10.1016/s1074-7613(00)80209-5. [DOI] [PubMed] [Google Scholar]
- 113.Bohn E, Sing A, Zumbihl R, Bielfeldt C, Okamura H, Kurimoto M, Heesemann J, Autenrieth IB. IL-18 (IFN-gamma-inducing factor) regulates early cytokine production in, and promotes resolution of, bacterial infection in mice. J Immunol. 1998;160:299–307. [PubMed] [Google Scholar]
- 114.Qureshi MH, Zhang T, Koguchi Y, Nakashima K, Okamura H, Kurimoto M, Kawakami K. Combined effects of IL-12 and IL-18 on the clinical course and local cytokine production in murine pulmonary infection with Cryptococcus neoformans. Eur J Immunol. 1999;29:643–649. doi: 10.1002/(SICI)1521-4141(199902)29:02<643::AID-IMMU643>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 115.Kawakami K, Qureshi MH, Zhang T, Okamura H, Kurimoto M, Saito A. IL-18 protects mice against pulmonary and disseminated infection with Cryptococcus neoformans by inducing IFN-gamma production. J Immunol. 1997;159:5528–5534. [PubMed] [Google Scholar]
- 116.Mencacci A, Bacci A, Cenci E, Montagnoli C, Fiorucci S, Casagrande A, Flavell RA, Bistoni F, Romani L. Interleukin 18 restores defective Th1 immunity to Candida albicans in caspase 1-deficient mice. Infect Immun. 2000;68:5126–5131. doi: 10.1128/iai.68.9.5126-5131.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cai G, Kastelein R, Hunter CA. Interleukin-18 (IL-18) enhances innate IL-12-mediated resistance to Toxoplasma gondii. Infect Immun. 2000;68:6932–6938. doi: 10.1128/iai.68.12.6932-6938.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Yap GS, Ortmann R, Shevach E, Sher A. A heritable defect in IL-12 signaling in B10.Q/J mice. II. Effect on acute resistance to Toxoplasma gondii and rescue by IL-18 treatment. J Immunol. 2001;166:5720–5725. doi: 10.4049/jimmunol.166.9.5720. [DOI] [PubMed] [Google Scholar]
- 119.Fujioka N, Akazawa R, Ohashi K, Fujii M, Ikeda M, Kurimoto M. Interleukin-18 protects mice against acute herpes simplex virus type 1 infection. J Virol. 1999;73:2401–2409. doi: 10.1128/jvi.73.3.2401-2409.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Tokmadzic VS, Tsuji Y, Bogovic T, Laskarin G, Cupurdija K, Strbo N, Koyama K, Okamura H, Podack ER, Rukavina D. IL-18 is present at the maternal-fetal interface and enhances cytotoxic activity of decidual lymphocytes. Am J Reprod Immunol. 2002;48:191–200. doi: 10.1034/j.1600-0897.2002.01132.x. [DOI] [PubMed] [Google Scholar]
- 121.Ostojic S, Dubanchet S, Chaouat G, Abdelkarim M, Truyens C, Capron F. Demonstration of the presence of IL-16, IL-17 and IL-18 at the murine fetomaternal interface during murine pregnancy. Am J Reprod Immunol. 2003;49:101–112. doi: 10.1034/j.1600-0897.2003.01150.x. [DOI] [PubMed] [Google Scholar]
- 122.Ledee-Bataille N, Dubanchet S, Coulomb-L'hermine A, Durand-Gasselin I, Frydman R, Chaouat G. A new role for natural killer cells, interleukin (IL)-12, and IL-18 in repeated implantation failure after in vitro fertilization. Fertil Steril. 2004;81:59–65. doi: 10.1016/j.fertnstert.2003.06.007. [DOI] [PubMed] [Google Scholar]
- 123.Laskarin G, Strbo N, Bogovic CT, Juretic K, Ledee BN, Chaouat G, Rukavina D. Physiological role of IL-15 and IL-18 at the maternal-fetal interface. Chem Immunol Allergy. 2005;89:10–25. doi: 10.1159/000087906. [DOI] [PubMed] [Google Scholar]
- 124.Jacobsson B, Holst RM, Mattsby-Baltzer I, Nikolaitchouk N, Wennerholm UB, Hagberg H. Interleukin-18 in cervical mucus and amniotic fluid: relationship to microbial invasion of the amniotic fluid, intra-amniotic inflammation and preterm delivery. BJOG. 2003;110:598–603. [PubMed] [Google Scholar]
- 125.Wang X, Hagberg H, Mallard C, Zhu C, Hedtjarn M, Tiger CF, Eriksson K, Rosen A, Jacobsson B. Disruption of interleukin-18, but not interleukin-1, increases vulnerability to preterm delivery and fetal mortality after intrauterine inflammation. Am J Pathol. 2006;169:967–976. doi: 10.2353/ajpath.2006.050207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Fazleabas AT, Kim JJ, Strakova Z. Implantation: embryonic signals and the modulation of the uterine environment--a review. Placenta. 2004;25 (Suppl A):S26–S31. doi: 10.1016/j.placenta.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 127.Ida A, Tsuji Y, Muranaka J, Kanazawa R, Nakata Y, Adachi S, Okamura H, Koyama K. IL-18 in pregnancy; the elevation of IL-18 in maternal peripheral blood during labour and complicated pregnancies. J Reprod Immunol. 2000;47:65–74. doi: 10.1016/s0165-0378(00)00058-9. [DOI] [PubMed] [Google Scholar]
- 128.Jokhi PP, King A, Loke YW. Cytokine production and cytokine receptor expression by cells of the human first trimester placental-uterine interface. Cytokine. 1997;9:126–137. doi: 10.1006/cyto.1996.0146. [DOI] [PubMed] [Google Scholar]
- 129.Menon R, Swan KF, Lyden TW, Rote NS, Fortunato SJ. Expression of inflammatory cytokines (interleukin-1 beta and interleukin-6) in amniochorionic membranes. Am J Obstet Gynecol. 1995;172:493–500. doi: 10.1016/0002-9378(95)90562-6. [DOI] [PubMed] [Google Scholar]
- 130.Menon R, Lombardi SJ, Fortunato SJ. IL-18, a product of choriodecidual cells, increases during premature rupture of membranes but fails to turn on the Fas-FasL-mediated apoptosis pathway. J Assist Reprod Genet. 2001;18:276–284. doi: 10.1023/A:1016626620137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.White CA, Dimitriadis E, Sharkey AM, Stoikos CJ, Salamonsen LA. Interleukin 1 beta is induced by interleukin 11 during decidualization of human endometrial stromal cells, but is not released in a bioactive form. J Reprod Immunol. 2007;73:28–38. doi: 10.1016/j.jri.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 132.Lindstrom TM, Bennett PR. The role of nuclear factor kappa B in human labour. Reproduction. 2005;130:569–581. doi: 10.1530/rep.1.00197. [DOI] [PubMed] [Google Scholar]
- 133.Hertelendy F, Rastogi P, Molnar M, Romero R. Interleukin-1beta-induced prostaglandin E2 production in human myometrial cells: role of a pertussis toxin-sensitive component. Am J Reprod Immunol. 2001;45:142–147. doi: 10.1111/j.8755-8920.2001.450304.x. [DOI] [PubMed] [Google Scholar]
- 134.Hertelendy F, Romero R, Molnar M, Todd H, Baldassare JJ. Cytokine-initiated signal transduction in human myometrial cells. Am J Reprod Immunol. 1993;30:49–57. doi: 10.1111/j.1600-0897.1993.tb00601.x. [DOI] [PubMed] [Google Scholar]
- 135.Romero R, Durum S, Dinarello CA, Oyarzun E, Hobbins JC, Mitchell MD. Interleukin-1 stimulates prostaglandin biosynthesis by human amnion. Prostaglandins. 1989;37:13–22. doi: 10.1016/0090-6980(89)90028-2. [DOI] [PubMed] [Google Scholar]
- 136.Mitchell MD, Chang MC, Chaiworapongsa T, Lan HY, Helliwell RJ, Romero R, Sato TA. Identification of 9alpha,11beta-prostaglandin F2 in human amniotic fluid and characterization of its production by human gestational tissues. J Clin Endocrinol Metab. 2005;90:4244–4248. doi: 10.1210/jc.2004-2496. [DOI] [PubMed] [Google Scholar]
- 137.Belt AR, Baldassare JJ, Molnar M, Romero R, Hertelendy F. The nuclear transcription factor NF-kappaB mediates interleukin-1beta-induced expression of cyclooxygenase-2 in human myometrial cells. Am J Obstet Gynecol. 1999;181:359–366. doi: 10.1016/s0002-9378(99)70562-4. [DOI] [PubMed] [Google Scholar]
- 138.Romero R, Emamian M, Wan M, Quintero R, Hobbins JC, Mitchell MD. Prostaglandin concentrations in amniotic fluid of women with intra-amniotic infection and preterm labor. Am J Obstet Gynecol. 1987;157:1461–1467. doi: 10.1016/s0002-9378(87)80245-4. [DOI] [PubMed] [Google Scholar]
- 139.Romero R, Wu YK, Sirtori M, Oyarzun E, Mazor M, Hobbins JC, Mitchell MD. Amniotic fluid concentrations of prostaglandin F2 alpha, 13,14-dihydro-15-keto-prostaglandin F2 alpha (PGFM) and 11-deoxy-13,14-dihydro-15-keto-11, 16-cyclo-prostaglandin E2 (PGEM-LL) in preterm labor. Prostaglandins. 1989;37:149–161. doi: 10.1016/0090-6980(89)90038-5. [DOI] [PubMed] [Google Scholar]
- 140.Romero R, Wu YK, Brody DT, Oyarzun E, Duff GW, Durum SK. Human decidua: a source of interleukin-1. Obstet Gynecol. 1989;73:31–34. [PubMed] [Google Scholar]
- 141.Sakao Y, Takeda K, Tsutsui H, Kaisho T, Nomura F, Okamura H, Nakanishi K, Akira S. IL-18-deficient mice are resistant to endotoxin-induced liver injury but highly susceptible to endotoxin shock. Int Immunol. 1999;11:471–480. doi: 10.1093/intimm/11.3.471. [DOI] [PubMed] [Google Scholar]
- 142.Dinarello CA. Therapeutic strategies to reduce IL-1 activity in treating local and systemic inflammation. Curr Opin Pharmacol. 2004;4:378–385. doi: 10.1016/j.coph.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 143.Boost KA, Hoegl S, Hofstetter C, Flondor M, Stegewerth K, Platacis I, Pfeilschifter J, Muhl H, Zwissler B. Targeting caspase-1 by inhalation-therapy: effects of Ac-YVAD-CHO on IL-1 beta, IL-18 and downstream proinflammatory parameters as detected in rat endotoxaemia. Intensive Care Med. 2007;33:863–871. doi: 10.1007/s00134-007-0588-0. [DOI] [PubMed] [Google Scholar]
- 144.Norman J, Yang J, Fink G, Carter G, Ku G, Denham W, Livingston D. Severity and mortality of experimental pancreatitis are dependent on interleukin-1 converting enzyme (ICE) J Interferon Cytokine Res. 1997;17:113–118. doi: 10.1089/jir.1997.17.113. [DOI] [PubMed] [Google Scholar]
- 145.Joshi VD, Kalvakolanu DV, Hebel JR, Hasday JD, Cross AS. Role of caspase 1 in murine antibacterial host defenses and lethal endotoxemia. Infect Immun. 2002;70:6896–6903. doi: 10.1128/IAI.70.12.6896-6903.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Sarkar A, Hall MW, Exline M, Hart J, Knatz N, Gatson NT, Wewers MD. Caspase-1 regulates Escherichia coli sepsis and splenic B cell apoptosis independently of interleukin-1beta and interleukin-18. Am J Respir Crit Care Med. 2006;174:1003–1010. doi: 10.1164/rccm.200604-546OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Hotchkiss RS, Chang KC, Swanson PE, Tinsley KW, Hui JJ, Klender P, Xanthoudakis S, Roy S, Black C, Grimm E, et al. Caspase inhibitors improve survival in sepsis: a critical role of the lymphocyte. Nat Immunol. 2000;1:496–501. doi: 10.1038/82741. [DOI] [PubMed] [Google Scholar]
- 148.Hotchkiss RS, Swanson PE, Cobb JP, Jacobson A, Buchman TG, Karl IE. Apoptosis in lymphoid and parenchymal cells during sepsis: findings in normal and T- and B-cell-deficient mice. Crit Care Med. 1997;25:1298–1307. doi: 10.1097/00003246-199708000-00015. [DOI] [PubMed] [Google Scholar]
- 149.Wang SD, Huang KJ, Lin YS, Lei HY. Sepsis-induced apoptosis of the thymocytes in mice. J Immunol. 1994;152:5014–5021. [PubMed] [Google Scholar]
- 150.Ayala A, Herdon CD, Lehman DL, Ayala CA, Chaudry IH. Differential induction of apoptosis in lymphoid tissues during sepsis: variation in onset, frequency, and the nature of the mediators. Blood. 1996;87:4261–4275. [PubMed] [Google Scholar]
- 151.Bilbo SD, Biedenkapp JC, Der-Avakian A, Watkins LR, Rudy JW, Maier SF. Neonatal infection-induced memory impairment after lipopolysaccharide in adulthood is prevented via caspase-1 inhibition. J Neurosci. 2005;25:8000–8009. doi: 10.1523/JNEUROSCI.1748-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Micci MA, Pattillo MT, Kahrig KM, Pasricha PJ. Caspase inhibition increases survival of neural stem cells in the gastrointestinal tract. Neurogastroenterol Motil. 2005;17:557–564. doi: 10.1111/j.1365-2982.2005.00702.x. [DOI] [PubMed] [Google Scholar]