Abstract
Azithromycin is a potent macrolide antibiotic with poorly understood antiinflammatory properties. Long-term use of azithromycin in patients with chronic inflammatory lung diseases, such as cystic fibrosis (CF), results in improved outcomes. Paradoxically, a recent study reported that azithromycin use in patients with CF is associated with increased infection with nontuberculous mycobacteria (NTM). Here, we confirm that long-term azithromycin use by adults with CF is associated with the development of infection with NTM, particularly the multi-drug-resistant species Mycobacterium abscessus, and identify an underlying mechanism. We found that in primary human macrophages, concentrations of azithromycin achieved during therapeutic dosing blocked autophagosome clearance by preventing lysosomal acidification, thereby impairing autophagic and phagosomal degradation. As a consequence, azithromycin treatment inhibited intracellular killing of mycobacteria within macrophages and resulted in chronic infection with NTM in mice. Our findings emphasize the essential role for autophagy in the host response to infection with NTM, reveal why chronic use of azithromycin may predispose to mycobacterial disease, and highlight the dangers of inadvertent pharmacological blockade of autophagy in patients at risk of infection with drug-resistant pathogens.
Introduction
Azithromycin is a potent antibiotic and is frequently used in prophylaxis and treatment regimens for mycobacterial infections (1). Long-term use of azithromycin and other macrolide antibiotics has increased as a result of reports of improved clinical outcomes in patients with cystic fibrosis (CF) (2), chronic obstructive pulmonary disease (3), panbronchiolitis (4), asthma (5), and chronic transplant rejection (6). These benefits are believed to result from its antiinflammatory effects on macrophages and neutrophils mediated through unknown mechanisms (7).
Worryingly, several studies have identified a synchronous increase in mycobacterial infection of CF patients, predominantly with the multi-drug-resistant, highly pathogenic nontuberculous mycobacteria (NTM) Mycobacterium abscessus (8, 9), for which there is no reliable treatment (1). We therefore wondered whether azithromycin paradoxically impairs host immunity against mycobacteria. Macroautophagy (referred to herein as autophagy) appears crucial for an effective cellular response against mycobacteria (10). Since the macrolide bafilomycin disrupts autophagy in vitro (11), we examined whether azithromycin blocks autophagy and thereby impairs intracellular killing of NTM. Here we present clinical data suggestive of an association between long-term azithromycin treatment and development of NTM infection in CF patients. At concentrations achieved during therapeutic dosing, azithromycin impaired lysosomal degradation of both autophagosomes and phagosomes and led to failure of intracellular killing of mycobacteria and development of chronic infection with M. abscessus in mouse models.
Results
Long-term azithromycin use may predispose CF patients to NTM infection.
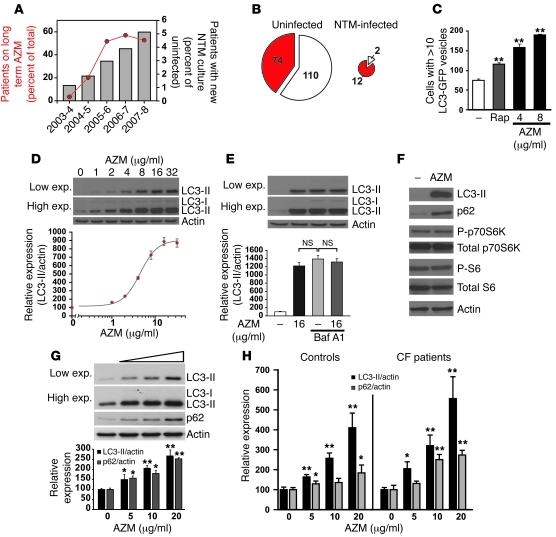
Escalating azithromycin use over the last 5 years has mirrored an increase in patients colonized or infected with NTM in our adult CF center (Figure 1A), not explicable by changes in sputum sampling (Supplemental Table 1; supplemental material available online with this article; doi: 10.1172/JCI46095DS1) or microbial culture methods. Long-term azithromycin use was associated with developing infection with NTM, particularly M. abscessus (P = 0.0009, 2-tailed uncorrected χ2; Figure 1B). When adjusted for age — which was identified, as in previous studies (9), as a significant covariate (P = 0.01; Supplemental Table 2) — azithromycin use remained significantly associated with NTM disease (P = 0.00046; odds ratio 9.80, 95% CI 2.09–45.87). Similar associations of chronic azithromycin use with NTM infection have been reported for an Israeli CF cohort (12), which suggests that azithromycin might impair host immunity against mycobacteria.
Figure 1. Azithromycin blocks autophagy by impairing autophagic flux.
(A) At Papworth Hospital, the numbers of adult CF patients on long-term azithromycin (AZM; red) and with new sputum cultures positive for NTM (gray) rose over the last 5 years. (B) Analysis of the 2007–2008 CF patient cohort. In patients currently or previously infected with NTM, long-term azithromycin use (current or within 6 months of first NTM culture) was significantly more common that in uninfected patients (P = 0.0009; 2-tailed uncorrected χ2). (C) In GFP-LC3+ COS7 cells, 24-hour treatment with azithromycin increased the number of cells containing 10 or more GFP-LC3+ vesicles more so than rapamycin (200 nM). (D) In HeLa cells, azithromycin caused a dose-dependent increase in LC3-II levels (EC50, 4.5 μg/ml). exp., exposure. (E) In the presence of 400 nM BafA1, azithromycin treatment of HeLa cells did not increase LC3-II compared with BafA1 alone. (F) Azithromycin treatment (16 μg/ml) of HeLa cells, while increasing LC3-II, did not alter mTOR-dependent signaling (monitored by changes in phosphorylation of S6 and p70S6 kinase); however, it did increase p62 levels. (G) Azithromycin dose-dependently increased LC3-II and p62 levels in primary human macrophages. (H) Similar effect of azithromycin, assessed by LC3-II and p62 levels, in primary macrophages derived from clinically stable CF patients and healthy controls (n = 3 per group). *P < 0.05; **P < 0.005.
Azithromycin blocks autophagosome degradation.
Since autophagy appears crucial for an effective cellular response against mycobacteria (10), we investigated whether azithromycin blocks autophagy, thereby preventing autophagy-dependent intracellular killing of NTM. Autophagy is routinely assayed by quantifying autophagosomes, achieved either by measuring levels of LC3-II, a protein that specifically associates with autophagosomes, or by detection of LC3-II+ vesicles (13). In cell lines, azithromycin caused a dose-dependent increase in both the number of LC3+ vesicles and the amount of LC3-II protein (EC50, 4.5 μg/ml; Figure 1, C and D). This suggests an accumulation of autophagosomes, which could result from either their increased synthesis or their decreased degradation. We therefore examined the effect of azithromycin in the presence of the lysosomal inhibitor bafilomycin A1 (BafA1), which blocks LC3-II destruction (11). Cotreatment of azithromycin and BafA1 resulted in no significant increase in LC3-II levels compared with BafA1 alone (Figure 1E), which indicates that azithromycin does not induce autophagosome synthesis, but rather blocks LC3-II degradation. Moreover, the azithromycin-induced rise in LC3-II was not accompanied by decreases in mTOR-dependent signaling (monitored by phosphorylation of p70S6 kinase and S6), a major negative regulator of autophagosome synthesis (14), but was associated — in both HeLa cells and primary macrophages — with elevations in the endogenous autophagy substrate p62 (ref. 15 and Figure 1, F and G). Azithromycin treatment in vitro resulted in accumulation of LC3-II and p62 in primary macrophages from CF patients similar to that in cells from healthy controls (Figure 1H and Supplemental Figure 1).
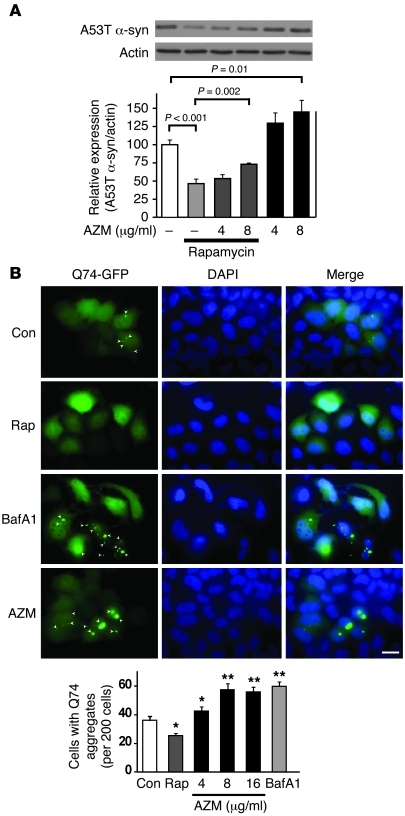
To confirm that azithromycin blocks autophagy-mediated degradation at, or below, concentrations achieved in clinical practice (between 12 μg/ml and 53 μg/ml in sputum, but several hundred–fold higher in phagocytic cells; refs. 7, 16), we examined the clearance of 2 known autophagy substrates: mutant (Q74) huntingtin (17) and A53T α-syncuclein (18). Azithromycin treatment retarded the basal and rapamycin-enhanced degradation of A53T α-synuclein and led to enhanced accumulation of intracellular aggregates of Q74 huntingtin (Figure 2, A and B). We next examined whether inhibition of LC3-II clearance by azithromycin was caused by failure of autophagosome-lysosome fusion, as seen with long-term treatment with BafA1 treatment (11), or failure of lysosomal function, a mechanism we recently reported (19). Confocal microscopy of HeLa cells coexpressing mCherry-LC3 and the lysosomal marker lgp120 revealed that although the number of LC3+ vesicles per cell increased with rapamycin, BafA1, or azithromycin treatment, the degree of LC3 colocalization with lgp120 was not significantly affected by azithromycin, but was, as expected, enhanced by rapamycin and inhibited by BafA1 (Figure 3A). However, azithromycin prevented acidification of autophagosomes. In HeLa cells stably expressing the mCherry-GFP-LC3 reporter, azithromycin treatment significantly increased nonacidified autophagosomes (i.e., mCherry+GFP+) and reduced acidified autophagosomes (mCherry+GFP–; Figure 3B).
Figure 2. Azithromycin blocks autophagic clearance and autophagosome acidification.
(A) Azithromycin reduced basal (black) and rapamycin-induced (gray) clearance of mutant (A53T) α-synuclein in stable inducible PC12 cells. The A53T α-synuclein transgene was induced with doxycycline for 48 hours and then switched off (by antibiotic removal) before cells were treated with vehicle alone, rapamycin (200 nM), and/or azithromycin for a further 24 hours. (B) Azithromycin reduced clearance of mutant (Q74) huntingtin. Aggregates of GFP-Q74 huntingtin were reduced by rapamycin treatment, but increased when autophagy was blocked by either BafA1 or azithromycin (4–16 μg/ml). Con, control. *P < 0.05; **P < 0.005. Scale bar: 10 μm.
Figure 3. Azithromycin blocks acidification of autophagosomes without impairing lysosomal function.
(A) Azithromycin did not impair autophagosome-lysosome fusion. Confocal microscopy of HeLa cells coexpressing LC3-mCherry with the lysosomal marker lgp120-GFP revealed that although rapamycin, BafA1, and azithromycin (16 μg/ml) treatment increased the total number of LC3+ vesicles per cell, the colocalization of LC3+ vesicles with lgp120 (LC3+/lgp120+) was not significantly different from controls after azithromycin treatment, but increased with rapamycin and decreased with BafA1 treatment. (B) Azithromycin impaired autophagosome acidification. HeLa cells stably expressing the mCherry-GFP-LC3 construct were treated with either 8–16 μg/ml azithromycin or BafA1 for 24 hours and analyzed by confocal microscopy. Compared with the control, azithromycin caused a significant reduction in the number of acidified LC3+ vesicles, but increased total LC3+ vesicles per cell. Number of vesicles was normalized to control cells. **P < 0.005. Scale bars: 10 μm.
Azithromycin disrupts autophagosome and phagosome function in macrophages.
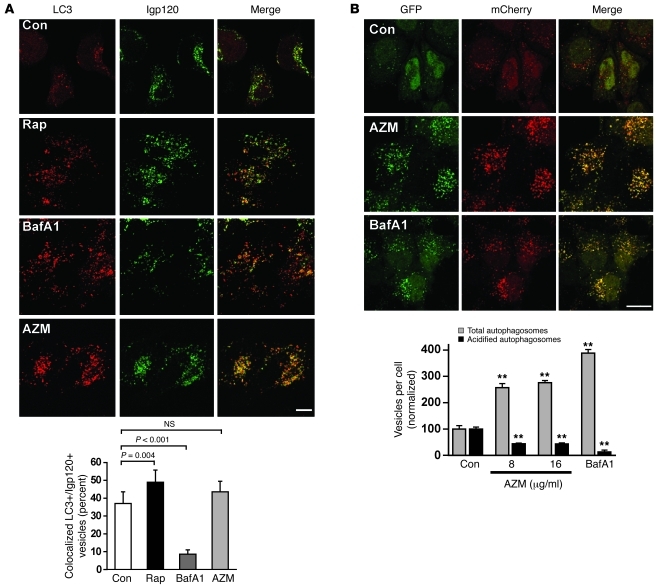
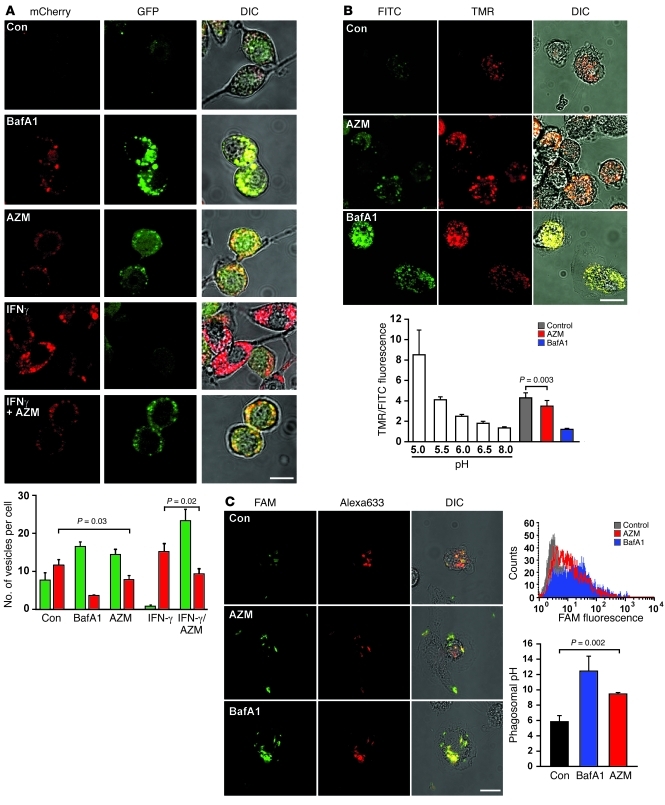
Since intracellular killing of mycobacteria by macrophages is critically enhanced by IFN-γ–induced autophagy (20), we examined the effect of azithromycin on autophagosomal flux triggered by this cytokine. Azithromycin blocked IFN-γ–induced as well as basal autophagosomal acidification in macrophages (Figure 4A), suggestive of impaired lysosomal function. Direct quantification of lysosomal pH, achieved by preloading human primary macrophages with dextran double-labeled with acid-sensitive (FITC) and resistant (TMR) fluorophores (21), indicated that 4 hours of treatment with azithromycin was sufficient to trigger significant alkalinization of lysosomes (Figure 4B). Azithromycin also blocked the acidification of phagosomes containing mycobacteria (Figure 4C and Supplemental Figure 2) or latex beads (Supplemental Figure 3). Using heat-killed M. abscessus labeled with both acid-quenchable (FAM) and pH stable (Alexa Fluor 633) fluorophores to report compartmental pH, we found that azithromycin pretreatment resulted in significant alkalinization of mycobacterial phagosomes (Figure 4C), to pH levels inhibitory to most lysosomal proteases. Similar azithromycin-induced phagosomal alkalinization was observed for cells ingesting PFA-killed M. tuberculosis (Supplemental Figure 2). As expected, azithromycin significantly reduced phagosomal protein degradation, as measured by time-dependent loss of surface-bound OVA from internalized latex beads (Figure 5A and Supplemental Figure 4). Although significant, phagosome-lysosome fusion was only impaired to a small extent by azithromycin (Figure 5B). Thus, it is likely that the block in phagosomal degradation results predominantly from a direct effect of azithromycin on compartmental pH. Azithromycin also reduced TNF-α release from macrophages in response to particulate but not soluble stimuli (Supplemental Figure 5), which suggests an inhibition of phagosome-triggered cytokine release. These data suggest that azithromycin treatment might compromise the host response to mycobacterial infection both by preventing degradation of mycobacteria within autophagosomes and phagosomes and by disrupting release of cytokines, such as TNF-α, that promote autophagy-dependent intracellular killing of mycobacteria.
Figure 4. Azithromycin blocks autophagosome and phagosome acidification by impairing lysosomal function.
(A) Prevention of IFN-γ–induced autophagic flux. RAW 264.7 cells stably expressing mRFP-GFP-LC3 were treated with vehicle alone (as control), BafA1 (200 nM), azithromycin (40 μg/ml), IFN-γ (200 ng/ml), or azithromycin plus IFN-γ. Representative images are shown. Quantification of acidified (mCherry+GFP–; red) and nonacidified (mCherry+GFP+; green) vesicles revealed a significant reduction in basal and IFN-γ–induced autophagosomal acidification by azithromycin treatment. (B) Reduced acidification of lysosomes in primary human macrophages. Double-labeled (FITC and TMR) dextran was loaded into lysosomes before cells were treated for 4 hours with azithromycin (80 μg/ml) or BafA1 (400 nM). As determined by confocal fluorescence analysis, azithromycin significantly reduced lysosomal acidification compared with controls, as did BafA1. Intracellular pH calibrations were performed as described in Supplemental Methods. (C) Azithromycin decreased acidification of phagosomes containing M. abscessus. Patient-derived M. abscessus strains were heat-killed, double-labeled with FAM and Alexa Fluor 633, and incubated for 24 hours with primary human macrophages untreated or treated with azithromycin (20 μg/ml) or BafA1 (100 nM). Representative confocal/DIC images of macrophages with intracellular labeled M. abscessus show increased mycobacterial FAM fluorescence (indicating reduced acidification) after treatment with azithromycin or BafA1. Also shown is quantification by flow cytometry of FAM fluorescence of macrophages that have internalized M. abscessus (i.e., Alexa Fluor 633+). Corresponding phagosomal pH values (see Supplemental Methods) demonstrated significant alkalinization of phagosomes with azithromycin or BafA1 treatment. Scale bars: 10 μm.
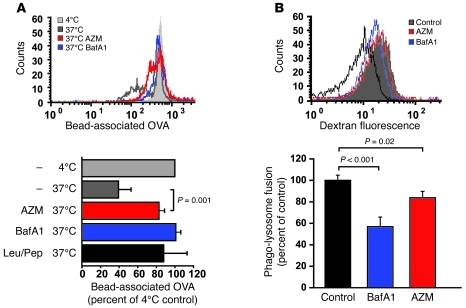
Figure 5. Azithromycin blocks phagosomal degradation and phagosome-lysosome fusion.
(A) OVA-coated beads were incubated with primary human macrophages (1-hour pulse, 23-hour chase). Internalized beads were released, and the amount of OVA coating was quantified by flow cytometry after incubation with fluorescent anti-OVA antibody. Treatment with azithromycin (20 μg/ml) significantly reduced OVA degradation compared with untreated cells, to levels close to those achieved by BafA1 (100 nM) or leupeptin/pepstatin. (B) Human primary macrophages were incubated (1-hour pulse, 4-hour chase) with TMR- and biotin-conjugated dextran to load lysosomes and then fed with IgG-coated streptavidin-conjugated fluorescent latex beads (30-minute pulse, 2-hour chase) with no treatment or in the presence of azithromycin (80 μg/ml) or BafA1 (400 nM). Beads were recovered by cell disruption, and the degree of bound dextran fluorescence was quantified by flow cytometry. Shown are a representative histogram and average geometric mean fluorescence of triplicate samples.
Intracellular killing of mycobacteria is impaired by azithromycin.
We therefore examined the effect of azithromycin on the survival of mycobacteria within primary human macrophages. Autophagy is critical for intracellular killing of M. tuberculosis and M. bovis BCG (10, 20), but also pathogenic NTM, including M. abscessus (Supplemental Figure 6). Over a wide range of concentrations, azithromycin blocked basal intracellular killing of M. bovis BCG and M. abscessus, as well as preventing the ability of the autophagy inducer rapamycin to enhance killing (Figure 6, A and B). The control of M. tuberculosis and NTM infection in vivo is crucially dependent on the inflammatory cytokines IFN-γ and TNF-α, which enhance intracellular killing of mycobacteria through the induction of autophagy (10). As expected, azithromycin treatment significantly blocked IFN-γ– and TNF-α–dependent killing of M. abscessus in primary human macrophages (Figure 6C). Furthermore, inoculation of whole blood with M. abscessus revealed that azithromycin pretreatment, while resulting in dose-dependent killing of presumably extracellular bacteria, blocked the ability of the autophagy inducers rapamycin and IFN-γ to enhance the clearance of mycobacteria (Figure 6D). These data suggest that the effect of azithromycin on NTM infection in vivo will depend on a balance between its direct antibiotic effects and its ability to enhance intracellular survival of mycobacteria through block of autophagosomal and phagosomal degradation.
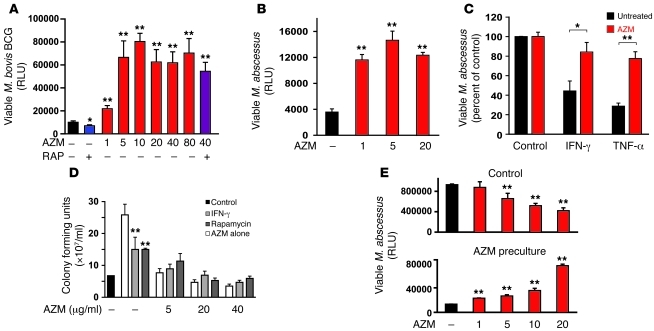
Figure 6. Azithromycin blocks intracellular killing of mycobacteria.
(A and B) Human macrophages were infected with luminescent mycobacteria — M. bovis BCG (A) and M. abscessus (B) — for 2 hours, washed, and exposed to the indicated concentrations of azithromycin (μg/ml) and/or 200 nM rapamycin for 24 hours. Viable intracellular mycobacteria were then assessed by measuring cell-associated luminescence after cell lysis. (C) IFN-γ and TNF-α enhanced intracellular killing of M. abscessus in human macrophages, and this was blocked by azithromycin pretreatment. Results were normalized to levels obtained without cytokine addition. (D) Patient-derived M. abscessus strains were incubated with peripheral blood from healthy subjects pretreated for 24 hours with vehicle alone or increasing concentrations of azithromycin. After 72 hours of incubation at 37°C, viable mycobacteria were quantified after sample lysis by counting CFUs. Addition of azithromycin, while reducing mycobacterial growth (white), prevented any additional autophagy-dependent killing achieved by coincubation with IFN-γ (200 U/ml) or rapamycin (100 nM). (E) Induction of macrolide resistance in M. abscessus. M. abscessus-lux was grown for 6 days in liquid culture (i.e., Middlebrook 7H9 plus ADC enrichment) in the presence of 0.1 μg/ml azithromycin or vehicle alone, washed, and resuspended in RPMI with 10% FCS with the indicated concentrations of azithromycin. Viable mycobacteria were assessed by measuring luminescence after 24 hours. *P < 0.05; **P < 0.005.
Azithromycin promotes chronic infection with M. abscessus in vivo.
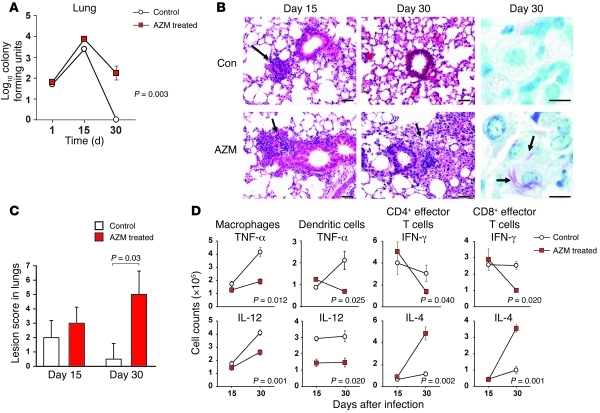
Although frequently sensitive to azithromycin in vitro, M. abscessus becomes highly macrolide resistant in vivo (Figure 6E) through inducible expression of the ribosomal methyltransferase erm(41) (22), equivalent to erm(37) found in M. tuberculosis, as well as through formation of a protective biofilm (23). To examine the effect of azithromycin treatment on the host response to mycobacteria in vivo, we infected mice via aerosol challenge with azithromycin-resistant M. abscessus (Figure 7). As previously described (24), lung infection in control mice peaked at day 15, with clearance of mycobacteria and resolution of peribronchiolar inflammatory infiltrates by day 30. In contrast, azithromycin treatment led to persistent lung infection associated with extensive granulomatous inflammation and failure of macrophage degradation of intracellular mycobacteria (Figure 7, A–C). As anticipated, azithromycin also influenced pulmonary cytokine levels during infection (Figure 7D). Lung macrophages (defined as CD11bhi) and dendritic cells (CD11b–CD11chiDEC205hi) produced less TNF-α and IL-12, whereas CD4+ and CD8+ effector T cells generated more IL-4 and less IFN-γ; the reasons for this are unclear, but may be associated with altered antigen presentation. This cytokine environment within the lung would be expected to further inhibit autophagic killing by macrophages (25, 26). These findings indicate that the ability of azithromycin to inhibit autophagy may outweigh any direct bactericidal properties and lead to chronic infection with NTM in vivo, explaining our own clinical observation and those of others (12).
Figure 7. Azithromycin promotes M. abscessus infection in vivo.
(A) C57BL/6 mice were infected by aerosol challenge with azithromycin-resistant M. abscessus. Treatment with azithromycin (100 mg/kg) by gavage for 5 days per week resulted in failure of M. abscessus clearance from lungs. (B) Representative lung histology demonstrating that azithromycin treatment led to persistent lung infection associated with extensive granulomas (arrows) and peribronchiolar inflammation at day 30. Ziehl-Neelsen staining confirmed the presence of large numbers of intracellular mycobacteria in azithromycin-treated, but not control, animals. Scale bars: 200 μm (histology); 10 μm (Ziehl-Neelsen). (C) Extent and severity of lung lesions in M. abscessus–infected mice at days 15 and 30 of treatment with vehicle alone or azithromycin. (D) Assessment of intracellular cytokine profiles for lung macrophages, dendritic cells, and CD4+ and CD8+ effector T cells during infection in the presence or absence of chronic azithromycin treatment.
Discussion
We found that azithromycin blocked lysosomal degradation of autophagosomes and phagosomes, which, while potentially contributing to its antiinflammatory effects seen clinically, impaired intracellular killing of mycobacteria and promoted chronic infection with NTM in vivo. Infection of CF patients with the multi-drug-resistant NTM M. abscessus is a growing clinical problem, leading to accelerated deterioration in lung function despite aggressive antibiotic therapy (8, 9). Previous epidemiological studies (12) and our current analysis suggest an association between long-term azithromycin use and development of M. abscessus infection, although definitive proof will require a prospective multicenter study with standardized sputum sampling and culture methods. Our findings provide a plausible mechanism for how chronic azithromycin use might predispose to NTM infection in CF patients and raise potential concerns about long-term macrolide treatment for other inflammatory lung diseases, use of macrolides in population-based eradication programs for trachoma and other infectious diseases (27), and clinical introduction of nonantibiotic macrolides as antiinflammatory agents.
The net effect of azithromycin during clinical NTM infection will depend on the balance between its direct antibiotic effect and its ability to block intracellular killing of mycobacteria. For slow-growing NTM species, such as the M. avium-intracellulare complex (MAC), which do not possess inducible macrolide resistance genes, azithromycin therapy (as part of multi-drug regimens) is usually highly effective. Whether it remains so during long-term, low-dose, intermittent treatment is unclear, particularly when concentrations of macrolides within MAC-containing phagosomes are likely to be reduced in vivo to below bacteriostatic levels (28). For rapid-growing NTM species, such as M. abscessus, that can acquire macrolide resistance (Figure 6E) through rapid induction of erm(41), single amino acid ribosomal mutation (1), and biofilm formation (23), the likely effect of long-term azithromycin therapy will be to promote infection, as seen in our mouse infection model. Azithromycin treatment also influenced cytokine production in vitro and in vivo, leading to reduced levels of macrophage- and dendritic cell–derived IL-12 and TNF-α and skewing T cell responses away from IFN-γ and toward IL-4. Although the mechanism underlying these effects remains to be elucidated, the net result will likely be further inhibition of autophagic killing (25, 26).
We demonstrated that azithromycin blocked autophagy in primary macrophages from stable CF patients as effectively as in those from healthy controls. Although basal levels of the autophagy substrate p62 were lower in CF macrophages, potentially as a result of transcriptional regulation (11), its levels were increased in both control and CF cells by azithromycin, indicative of blocked autophagic clearance.
Although the ability of azithromycin to block autophagy could be clinically exploitable in anticancer therapy, where tumor susceptibility to chemotherapy may be enhanced (29), our data suggest that its impairment of autophagic degradation in macrophages will compromise host immunity to mycobacteria and potentially block the efficacy of adjuvant IFN-γ therapy often used in patients with difficult NTM or M. tuberculosis infection. Our findings have profound implications for the treatment of multi-drug-resistant mycobacteria, including M. tuberculosis, in which the ability of azithromycin to block intracellular bacterial killing is not accompanied by a direct antibiotic effect.
Methods
Further information can be found in Supplemental Methods.
Culture of cell lines and generation of human macrophages
HeLa and COS-7 cells were grown as previously described. Human monocyte-derived macrophages were isolated from peripheral blood as previously described (30), obtained from healthy consented subjects (approved by Regional NHS Research Ethics Committee), or from patients with CF (clinically stable and not taking azithromycin).
Lysosomal and phagosomal pH measurements
Human primary macrophages were loaded with TMR-FITC dextran (1-hour pulse, 4-hour chase). Cells were then treated with compounds and visualized by live cell fluorescence/differential interference contrast (fluorescence/DIC) confocal imaging. To determine the phagosomal pH, primary macrophages were incubated (1-hour pulse, 23-hour chase) with albumin-coated, FAM-conjugated 645-nm (Far Red) latex beads, patient-derived heat-killed M. abscessus strains double-labeled with FAM and Alexa Fluor 633, or PFA-killed M. tuberculosis H37Rv double-labeled with FITC and Alexa Fluor 633. Macrophages were pretreated for 24 hours with compounds. Analysis was carried out by either live cell fluorescence/DIC confocal imaging or flow cytometry, in which the fluorescence of cells with internalized particles (FarRed or Alexa Fluor 633 for beads and mycobacteria, respectively) was measured. Intracellular calibration was achieved as detailed in Supplemental Methods.
Phagosomal degradation assays
Human macrophages were incubated (30-minute pulse, 2-hour chase) with OVA-conjugated fluorescent latex beads at 4°C, 37°C, or 37°C with 15-minute protease inhibitor pretreatment. Macrophages were pretreated with BafA1 or azithromycin for 24 hours prior to phagocytosis; treatment continued throughout the experiment. Beads were then recovered by cell disruption in the presence of proteases inhibitors, then incubated with OVA-specific biotinylated antibody and fluorescent streptavidin, which was quantified by flow cytometry.
Phagosome-lysosome fusion assays
Human macrophages were incubated (1-hour pulse, 4-hour chase) with TMR- and biotin-conjugated dextran to load lysosomes and then fed IgG-coated, streptavidin-conjugated fluorescent latex beads (30-minute pulse, 2-hour chase) with no treatment or in the presence of azithromycin (80 μg/ml) or BafA1. Beads were recovered by cell disruption, the degree of bound fluorescent dextran was quantified by flow cytometry, and average geometric mean fluorescence was determined.
In vitro mycobacterial infection assays
Primary human macrophages.
Macrophages were inoculated with mycobacteria (MOI 10:1) for 2 hours at 37°C, repeatedly washed, and then incubated for 24 hours at 37°C in the presence or absence of azithromycin or rapamycin, as indicated. Cells were finally lysed, and luminescence was measured.
Whole blood mycobacterial infection assays.
Patient-derived M. abscessus strains were grown to log phase in Middlebrook 7H9 media. Heparinized peripheral blood from healthy consented subjects was inoculated with M. abscessus after pretreatment for 24 hours with vehicle alone or azithromycin and incubated for 72 hours at 37°C. Viable mycobacteria were quantified (CFU) on microbial plates. Where indicated, IFN-γ or rapamycin were added to blood at the time of infection with mycobacteria.
Induction of macrolide resistance in vitro.
M. abscessus-lux was grown in liquid culture in the presence of 0.1 μg/ml azithromycin or vehicle alone, washed, and resuspended in RPMI with 10% FCS with the indicated concentrations of azithromycin. Viable mycobacteria were assessed by measuring luminescence after 24 hours.
In vivo mycobacterial infection
Mice were challenged with M. abscessus as previously described (24). Control (saline) and azithromycin groups (n = 5 per group) were treated 5 days per week at a concentration of 100 mg/kg by gavage. On days 15 and 30 after infection, bacterial loads in the lungs and spleen were determined by histological and flow cytometry analysis (see Supplemental Methods). Bacterial counts were determined by plating serial dilutions of homogenates of lungs after 3–7 days.
Statistics
Densitometric analysis on the immunoblots was done by Image J software. P values for the Cellomics array scan counting and for other experiments requiring multiple comparisons were determined by factorial ANOVA using STATVIEW software (version 4.53). P values for all other assays were determined using 2-tailed Student’s t test. A P value of 0.05 or less was considered significant. Experiments were performed on at least 3 separate occasions with at least triplicate samples for each condition and represented as mean ± sd.
To test for an association between NTM status and azithromycin, we used a logistic regression model adjusted for covariates. Forward logistic regression was used to select covariates associated with NTM status (P < 0.05) from age, forced expiratory volume in 1 second, BMI, sex, colonization with Pseudomonas aeruginosa, CF-related liver disease, CF-related diabetes, CF-related asthma, allergic bronchopulmonary aspergillosis, and gastroesophageal reflux disease. Analyses were performed in R ( http://www.r-project.org).
Study approval
All experimental protocols were approved by the Animal Care and Usage Committee of Colorado State University and complied with NIH guidelines.
Supplementary Material
Acknowledgments
This work was supported by grants from the Wellcome Trust (Senior Clinical Fellowships to R.A. Floto and D.C. Rubinsztein), the NIHR Biomedical Research Centre at Addenbrooke’s Hospital, Papworth Hospital NHS Trust, and the Jodi and Lucinda Dunmore Foundation. The authors thank Juliet Foweraker and Christian Laughton for help with microbiology and Jane Elliott and Judy Ryan for help with clinical data collection.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2011;121(9):3554–3563. doi:10.1172/JCI46095.
References
- 1.Griffith DE, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175(4):367–416. doi: 10.1164/rccm.200604-571ST. [DOI] [PubMed] [Google Scholar]
- 2.McArdle JR, Talwalkar JS. Macrolides in cystic fibrosis. Clin Chest Med. 2007;28(2):347–360. doi: 10.1016/j.ccm.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 3.Martinez FJ, Curtis JL, Albert R. Role of macrolide therapy in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2008;3(3):331–350. doi: 10.2147/copd.s681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poletti V, Casoni G, Chilosi M, Zompatori M. Diffuse panbronchiolitis. Eur Respir J. 2006;28(4):862–871. doi: 10.1183/09031936.06.00131805. [DOI] [PubMed] [Google Scholar]
- 5.Piacentini GL, et al. Azithromycin reduces bronchial hyperresponsiveness and neutrophilic airway inflammation in asthmatic children: a preliminary report. Allergy Asthma Proc. 2007;28(2):194–198. doi: 10.2500/aap.2007.28.2958. [DOI] [PubMed] [Google Scholar]
- 6.Yates B, et al. Azithromycin reverses airflow obstruction in established bronchiolitis obliterans syndrome. Am J Respir Crit Care Med. 2005;172(6):657–659. doi: 10.1164/rccm.2506011. [DOI] [PubMed] [Google Scholar]
- 7.Idris SF, Chilvers ER, Haworth C, McKeon D, Condliffe AM. Azithromycin therapy for neutrophilic airways disease: myth or magic? Thorax. 2009;64(3):186–189. doi: 10.1136/thx.2008.103192. [DOI] [PubMed] [Google Scholar]
- 8.Esther CR, Jr, Esserman DA, Gilligan P, Kerr A, Noone PG. Chronic Mycobacterium abscessus infection and lung function decline in cystic fibrosis. J Cyst Fibros. 2010;9(2):117–123. doi: 10.1016/j.jcf.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roux AL, et al. Multicenter study of prevalence of nontuberculous mycobacteria in patients with cystic fibrosis in France. J Clin Microbiol. 2009;47(12):4124–4128. doi: 10.1128/JCM.01257-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vergne I, et al. Autophagy in immune defense against Mycobacterium tuberculosis. Autophagy. 2006;2(3):175–178. doi: 10.4161/auto.2830. [DOI] [PubMed] [Google Scholar]
- 11.Klionsky DJ, et al. Guidelines for the use and interpretation of assays for monitoring autophagy in higher eukaryotes. Autophagy. 2008;4(2):151–175. doi: 10.4161/auto.5338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levy I, et al. Multicenter cross-sectional study of nontuberculous mycobacterial infections among cystic fibrosis patients, Israel. Emerg Infect Dis. 2008;14(3):378–384. doi: 10.3201/eid1403.061405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kabeya Y, et al. LC3, a mammalian homologue of yeast Apg8p, is localized in autophagosome membranes after processing. EMBO J. 2000;19(21):5720–5728. doi: 10.1093/emboj/19.21.5720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ravikumar B, et al. Inhibition of mTOR induces autophagy and reduces toxicity of polyglutamine expansions in fly and mouse models of Huntington disease. Nat Genet. 2004;36(6):585–595. doi: 10.1038/ng1362. [DOI] [PubMed] [Google Scholar]
- 15.Moscat J, Diaz-Meco MT. P62 at the crossroads of autophagy, apoptosis, and cancer. Cell. 2009;137(6):1001–1004. doi: 10.1016/j.cell.2009.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilms EB, Touw DJ, Heijerman HG. Pharmacokinetics and sputum penetration of azithromycin during once weekly dosing in cystic fibrosis patients. Ther Drug Monit. 2006;28(2):219–225. doi: 10.1097/01.ftd.0000195617.69721.a5. [DOI] [PubMed] [Google Scholar]
- 17.Narain Y, Wyttenbach A, Rankin J, Furlong RA, Rubinsztein DC. A molecular investigation of true dominance in Huntington’s disease. J Med Genet. 1999;36(10):739–746. doi: 10.1136/jmg.36.10.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Webb JL, Ravikumar B, Atkins J, Skepper JN, Rubinsztein DC. Alpha-Synuclein is degraded by both autophagy and the proteasome. J Biol Chem. 2003;278(27):25009–25013. doi: 10.1074/jbc.M300227200. [DOI] [PubMed] [Google Scholar]
- 19.Jahreiss L, Renna M, Bittman R, Arthur G, Rubinsztein DC. 1-O-Hexadecyl-2-O-methyl-3-O-(2’-acetamido-2’-deoxy-β-D-glucopyranosyl)-sn-glycerol (Gln) induces cell death with more autophagosomes which is autophagy-independent. Autophagy. 2009;5(6):835–846. doi: 10.4161/auto.9120. [DOI] [PubMed] [Google Scholar]
- 20.Gutierrez MG, Master SS, Singh SB, Taylor GA, Colombo MI, Deretic V. Autophagy is a defense mechanism inhibiting BCG and Mycobacterium tuberculosis survival in infected macrophages. Cell. 2004;119(6):753–766. doi: 10.1016/j.cell.2004.11.038. [DOI] [PubMed] [Google Scholar]
- 21.Di A, et al. CFTR regulates phagosome acidification in macrophages and alters bactericidal activity. Nat Cell Biol. 2006;8(9):933–944. doi: 10.1038/ncb1456. [DOI] [PubMed] [Google Scholar]
- 22.Nash KA, Brown-Elliott BA, Wallace RJ. A novel gene, erm(41), confers inducible macrolide resistance to clinical isolates of Mycobacterium abscessus but is absent from Mycobacterium chelonae. Antimicrob Agents Chemother. 2009;53(4):1367–1376. doi: 10.1128/AAC.01275-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greendyke R, Byrd TF. Differential antibiotic susceptibility of Mycobacterium abscessus variants in biofilms and macrophages compared to that of planktonic bacteria. Antimicrob Agents Chemother. 2008;52(6):2019–2026. doi: 10.1128/AAC.00986-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ordway D, et al. Animal model of Mycobacterium abscessus lung infection. J Leukoc Biol. 2008;83(6):1502–1511. doi: 10.1189/jlb.1007696. [DOI] [PubMed] [Google Scholar]
- 25.Singh SB, Davis AS, Taylor GA, Deretic V. Human IRGM induces autophagy to eliminate intracellular mycobacteria. Science. 2006;313(5792):1438–1441. doi: 10.1126/science.1129577. [DOI] [PubMed] [Google Scholar]
- 26.Harris J, et al. T Helper 2 cytokines inhibit autophagic control of intracellular Mycobacterium tuberculosis. Immunity. 2007;27(3):505–17. doi: 10.1016/j.immuni.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 27.Mecaskey JW, Knirsch CA, Kumaresan JA, Cook JA. The possibility of eliminating blinding trachoma. Lancet Infect Dis. 2003;3(11):728–734. doi: 10.1016/S1473-3099(03)00807-7. [DOI] [PubMed] [Google Scholar]
- 28.Fréhel C, Offredo C, de Chastellier C. The phagosomal environment protects virulent Mycobacterium avium from killing and destruction by clarithromycin. Infect Immun. 1997;65(7):2792–2802. doi: 10.1128/iai.65.7.2792-2802.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kondo Y, Kanzawa T, Sawaya R, Kondo S. The role of autophagy in cancer development and response to therapy. Nat Rev Cancer. 2005;5(9):726–734. doi: 10.1038/nrc1692. [DOI] [PubMed] [Google Scholar]
- 30.Floto RA, et al. Loss of function of a lupus-associated FcgammaRIIb polymorphism through exclusion from lipid rafts. Nat Med. 2005;11(10):1056–1058. doi: 10.1038/nm1288. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.