Abstract
The purpose of this study is to evaluate quantitative structural measures of the ventromedial prefrontal cortex (vmPFC) in boys with isolated clefts of the lip and/or palate (ICLP) relative to a comparison group and to associate measures of brain structure with quantitative measures of hyperactivity, impulsivity, and inattentiveness. A total of 50 boys with ICLP were compared to 60 healthy boys without clefts. Magnetic resonance imaging brain scans were used to evaluate vmPFC structure. Parents and teachers provided quantitative measures of hyperactivity, impulsivity, and inattentiveness using the Pediatric Behavior Scale. Boys with ICLP had significantly higher ratings of hyperactivity/impulsivity/inattention (HII) and significantly increased volume of the right vmPFC relative to the comparison group. There was a direct relationship between HII score and vmPFC volume in both the ICLP group and control group, but the relationship was in the opposite direction: in ICLP, the higher the vmPFC volume, the higher the HII score; for the comparison group, the lower the vmPFC volume, the greater the HII score. The vmPFC is a region of the brain that governs behaviors of hyperactivity, impulsivity and inattention (HII). In boys with ICLP, there are higher levels of HII compared to the controls and this is directly related to a significantly enlarged volume of the right vmPFC. Enlargement of this region of the brain is therefore considered to be pathological in the ICLP group and supports the notion that abnormal brain structure (from abnormal brain development) is the underlying etiology for the abnormal behaviors seen in this population.
Keywords: Ventromedial, Impulsivity, Orofacial cleft, Brain structure, Hyperactivity
Introduction
Orofacial clefts are the most common major birth defect in America, affecting over 6,800 births annually (Canfield et al. 2006). These oral clefts are developmental craniofacial abnormalities that result, at least in part, from a failure of neural crest cells to migrate properly. As a group, 70% of clefting disorders are comprised of those that are isolated to facial clefts only (non-syndromic), and 30% are those in which the facial cleft is part of a well-defined syndrome of additional anomalies (Jones 1988). Isolated oral clefts are further divided anatomically into clefts of the lip and/or palate (CLP) and clefts of the palate only (CPO).
In addition to the facial cleft, persons affected with isolated clefts of the lip and/or palate (ICLP) suffer from a constellation of other problems including persistent problems with speech (even after cleft repair), as well as cognitive and behavioral abnormalities. The cognitive deficits associated with ICLP are well documented and characterized with a lowering of overall intelligence quotient (IQ) (though not to mental retardation level) and specific deficits in language function (Richman and Eliason 2009; Richman and Eliason 2001). These deficits are severe enough that reading disabilities have been reported to be as common as 35% of children with ICLP (Richman et al. 1988; Broder et al. 1998).
In regard to behavior, an estimated 30% to 50% of children with ICLP experience at least some periods of behavioral abnormality (Richman and Millard 1997). Subjects with ICLP have been consistently shown to have increased internalizing behavior problems (social inhibition or shyness, depressed mood) (Endriga et al. 2003); however, very few studies have evaluated externalizing behaviors such as aggression, opposition, hyperactivity, impulsivity or inattention. A recent large study by Hunt et al. found that parent ratings of children with ICLP showed a significant increase in both internalizing and externalizing behaviors compared to children without ICLP (Hunt et al. 2007); however, the externalizing behaviors were not subdivided to isolate or characterize specific types.
The behavioral traits of hyperactivity/motor impulsivity, impulsivity/non-planning, and inattentiveness form a core dimension of personality that is heritable, emerges early in the course of development, and persists across developmental stages (McKay and Halperin 2001; Kochanska and Knaack 2003). Moreover, these behaviors can be elevated to pathological levels and are the hallmarks of the neuropsychiatric diagnosis of attention-deficit hyperactivity disorder (ADHD); however, they also occur at elevated levels (though often below diagnostic criteria for ADHD) in a multitude of developmental disorders.
In a previous study from our lab, we investigated the neural underpinnings of externalizing behaviors and found that in a sample of healthy normal boys (no psychiatric diagnosis including ADHD), the region of the brain that was directly related to behaviors of impulse control was the right ventromedial prefrontal cortex (vmPFC). Those boys with the highest ratings of hyperactivity and impulsivity had the lowest volumes of the right vmPFC (Boes et al. 2009). These findings are conceptualized as supporting the notion that the right vmPFC acts as a neuroanatomical correlate of impulse control in normal healthy boys, extending upon structure-function studies of pathologic samples with ADHD that have also highlighted the right vmPFC (Shaw et al. 2007a).
In an additional study from our lab, we have found that the structure of the brain in children with ICLP is substantially abnormal (Nopoulos et al. 2007). There are overall decrements in the size of the intracranial volume (ICV), and a proportional decrement in the frontal lobe, basal ganglia, and cerebellum after controlling for overall ICV. Moreover, there was a sex-specific finding in that for boys with ICLP, the cerebral cortex was proportionately enlarged compared to healthy boys—a tissue distribution abnormality.
Given the previous literature on elevated externalizing behavior in ICLP, our study of hyperactivity and impulsivity and its neuroanatomical correlate in healthy boys, and finally our study of brain structure in children with ICLP, the current study was designed to address the following questions: (1) Do boys with ICLP have elevations in hyperactivity/impulsivity/inattention (HII)? (2) Do boys with ICLP have structural abnormalities in the right vmPFC compared to healthy control boys? Finally, (3) what is the relationship between right vmPFC and HII in both healthy and ICLP boys?
Methods
Participants The current study uses samples from three previous studies from our lab. The ICLP boys (n = 50, age range 7.3–17.8 years) were previously analyzed for general brain morphology (Nopoulos et al. 2007) and the normal healthy boys (n = 60, age range 7.8–17.9 years) were previously assessed for impulse control and regional brain morphology associated with those behaviors (Boes et al. 2009). Both samples were sub-samples of a study on neuropsychological functioning in children with clefts (Conrad et al. 2009).All children with ICLP were recruited from our University of Iowa Cleft Clinic. Any child with ICLP in which there was a suspicion of genetic syndrome was evaluated by a clinical geneticist and included in the study only if the child was deemed non-syndromic based on that evaluation. Exclusion criteria for the ICLP subjects included presence of braces (creates artifact in magnetic resonance imaging (MRI) scan) and known IQ less than 70 (mental retardation). Cleft type was broken down into clefts of the lip only (CLO, n = 11), clefts of the lip and palate (CLP, n = 26) and cleft palate only (CPO, n = 13).The comparison group consisted of healthy boys recruited from the community via local newspaper advertisements. Exclusion criteria for this group included presence of braces, major medical, neurologic, or psychiatric illness or history of learning disability (information obtained from parents during screening process).The general measure of height was obtained by a trained research nurse and recorded in centimeters. Parental socioeconomic status (SES) of all participants was obtained using a modified Hollingshead Scale of 1 to 5, with the lower number corresponding to higher socioeconomic status (Hollingshead and Redlich 1958). Since SES is a factor that can significantly impact brain structure and function, it is accounted for in the statistical analyses (see “Statistical analysis” section). The race of both groups was mostly Caucasian (>95%), consistent with the geographic demographics. All participants (subjects and their parents) signed an informed consent prior to enrolling in the protocol which was approved by the local investigational review board.
IQ testing Wechsler Intelligence Scale for Children, 3rd Edition (WISC-III) (Wechsler 1991) The WISC-III is designed to assess the intellectual abilities of children ages 6 to 16 years. The children were administered the vocabulary, similarities, block design, and picture completion subtests, and the full scale IQ was prorated. The Wechsler Adult Intelligence Scale, 3rd Edition (Wechsler 1997) is a well-known test of adult intelligence. The subtests and scales are parallel to those in the children form. Adolescents who were 17 years old were administered this subtest because norms on the WISC-III only go up to 16 years. Two of the control subjects had missing IQ scores.
Behavioral measure The pediatric behavior scale, short version (PBS) is a tool for assessing emotional and behavioral problems and is derived from the PBS (Lindgren and Koeppl 1987), a measure with similar items as the Child Behavior Checklist (Achenbach 1991). For each participant, a parent and a teacher were asked to rate problems on a four-point Likert scale (0–3), with a lower score indicating fewer problems. For the current analysis all questions related to non-planning, motor impulsivity, and inattention were included. It is important to note that for our previous analysis of the healthy control boys, we limited the assessment to impulse control items, excluding the inattention items, thus a more restricted analysis. Individual questions for the current analysis included: (1) cannot concentrate, (2) easily distracted, (3) fails to finish things, (4) impulsive; acts without stopping to think, (5) cannot stand waiting; wants things right away, (6) interrupts, talks out of turn, or blurts things out, (7) hyperactive; always “on the go,” (8) squirms or fidgets, and (9) restless, cannot sit still. The parent and teacher response rate for the PBS was 100% and 97%, respectively for the ICLP boys and 86% and 88% for the healthy boys. Overall, 85% of the subjects had both a parent and a teacher score. As a means of data reduction, the PBS ratings were summed across these nine questions to get one sub-score each for parents and teachers, and then these two sub-scores were added together for one overall HII score (theoretical range of 0–54).The PBS scales were derived from factor analysis with varimax rotation from a sample of 600 children ages 6–12. The scales were obtained from a four-factor solution with all eigenvalues greater than one. All of the items on this scale do not cross load to any significant degree (less than 0.30) with other PBS scales. The reliability of the PBS impulse control scale was established using a longer version of the PBS, which estimated the internal consistency coefficient at 0.95 for the category including the HII questions (Lindgren and Koeppl 1987). The criterion for inclusion of items in the short PBS version is that items load on highly similar factors in the normal structure of the CBCL in both sexes across multiple age categories. The scale used in this study has a raw mean score of 3.82 from the normative sample (parent rating only). The PBS has been shown to be valuable in identifying symptoms of ADHD in a sample of children with cleft (Richman et al. 2004) as well as identifying attention deficits in a normal sample (Boes et al. 2009)The PBS was also used as a proxy to a formal evaluation for ADHD to identify participants that were likely to meet DSM-IV ADHD criteria. The criteria were met if the combined parent and teacher ratings exceeded the 90th percentile in two of the three ADHD-like scales (hyperactive\motor impulsivity, impulsiveness/non-planning, and inattentiveness), as described as a method of ADHD diagnosis (Richman et al. 2004). The 90th percentile was determined using normative data from 6 to 12-year-old boys, n = 300. Of the ICLP sample, nine of the 50 boys reached this criterion. In addition, parents filled out a medical history form which documents all medical and psychiatric diagnoses for each ICLP child. From that assessment, five boys with ICLP were identified as having been diagnosed with ADHD by a physician. None of the boys from the control fulfilled the criteria for ADHD by the PBS ratings and none had been diagnosed as ADHD by a clinician (which is one of our exclusionary criterion).
MRI acquisition Magnetic resonance imaging scans were obtained using a 1.5 Tesla General Electric SIGNA System (GE Medical Systems, Milwaukee, WI). Three-dimensional (3-D) T1-weighted images were acquired in the coronal plane using a spoiled grass sequence with the following parameters, 1.5-mm coronal slices, 40° flip angle, 24 ms repetition time (TR), 5 ms echo time (TE), two numbers of extinctions (NEX), a 26-cm field of view (FOV), and a 256 × 192 matrix. The proton density (PD) and T2-weighted images were acquired with the following parameters, 3.0-mm coronal slices, 36 ms TE (for PD) or 96 ms TE (for T2), 3,000 ms TR, one NEX, a 26-cm FOV, 256 × 192 matrix, and an echo train length = 1.
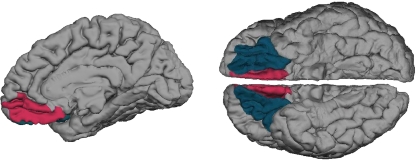
Image processing MRI data were processed using Brain Research: Analysis of Images, Networks, and Systems (BRAINS2), our locally developed software, described elsewhere (Magnotta et al. 2002) T1-weighted images were spatially normalized and re-sampled to 1.015625 mm3 voxels and the anterior–posterior axis of the brain was re-aligned parallel to the anterior commissure–posterior commissure line. The interhemispheric fissure was aligned by selecting points along the fissure in the coronal and axial views. T2 and PD images were co-registered to the final T1 image, and all images were intensity normalized and inhomogeneity corrected. A discriminant tissue classification was then performed, and a brain mask was created using an artificial neural network. Measures obtained include intracranial volume (all tissues from the dura mater on down), then separated into cerebrum and cerebellum. The cerebrum is then segmented into gray matter (cerebral cortex and sub-cortical), and white matter.The T1 acquisition was processed using FreeSurfer (http://www.martinos.org/freesurfer), an automated parcellation software program (Desikan et al. 2006). The output of interest was the predefined region of interest (ROI), the right vmPFC. The anatomical accuracy of each FreeSurfer ROI was visually inspected and those with unacceptable parcellation were excluded from all analyses (no scans were excluded). Figure 1 displays the anatomical ROI for the current study, derived from the standard FreeSurfer atlas. The vmPFC is composed of two regions defined by FreeSurfer, the medial orbitofrontal cortex (mOFC) and lateral orbitofrontal cortex (lOFC). The mOFC is composed of the ventral sector of the medial prefrontal cortex and the orbitofrontal cortex medial to the olfactory sulcus (i.e., straight gyrus). The lOFC is flanked by the olfactory sulcus medially and the lateral orbital sulcus laterally. Details of FreeSurfer parcellation, including reliability, validity, and anatomical boundaries, are described in detail elsewhere (Desikan et al. 2006).
Fig. 1.
Ventromedial prefrontal cortex (vmPFC). On the left is a medial view of the right hemisphere with the fuchsia color representing the medial orbitofrontal cortex. The image on the right is a ventral view of both hemispheres with the fuchsia color representing the medial orbitofrontal cortex and the blue color representing the lateral orbitofrontal cortex. These regions combine to form the vmPFC and are not visible from a lateral view
Statistical analysis
IQ and behavior scores The full scale IQ (FSIQ) and average PBS score for the HII section was compared between groups using a two-sample t test. Regarding the HII, there were 14 subjects who were missing the teacher component of the score and two subjects who were missing the parent component. Because the teacher component tended to be lower than the parent component (mean of 4.9 vs. 5.7), we used an imputation approach based on linear regression models fit on the complete data (n = 94) to estimate the missing components (n = 16). This approach resulted in mean HII scores that were similar in the complete cases and in the imputed cases (p = 0.782). To examine the potential confounding effects of SES, we included SES as a covariate in multiple linear regression models, and we also created and tested interaction terms involving SES in our models.
Brain morphology When evaluating regional measures of brain tissue (either total cortex or vmPFC), volumes were expressed as a percent of ICV. To measure laterality, an asymmetry coefficient (AC) for the vmPFC gray matter volume was calculated using the following formula: (right − left)/(right + left), with a negative value indicates a larger left-sided structure. Brain volumes, percents, and laterality were compared between groups using two-sample t tests. Since ICV is known to increase substantially with age, we used multiple linear regression to adjust between-group comparisons for age, as well as parental SES.
Relationship between brain morphology and behavior scores The vmPFC is a specific region of the cortex. In this analysis, to control for overall cortical volume, the vmPFC was expressed as a percent of total cortex volume. This also attempts to highlight specificity, by controlling for any potential relationship that the total cortex itself could have with the behavior scores. In addition, we focused this aim on the side (left or right) of the vmPFC with the most significant between-group differences. Multiple linear regression and scatter plots were used to examine the relationship between brain morphology and behavior in the two groups.
Results
Behavior scores
Demographic measures of age and parental SES are shown in Table 1. The mean age for the ICLP boys was 11.9 years (s.d. = 3.3) and for the healthy control boys was 12.1 years (s.d. = 2.7). Parental social class was significantly lower in the ICLP group (mean = 2.67, s.d. = 0.51) compared to the healthy control group (mean = 2.33, s.d. = 0.56), p = 0.001. Table 1 also displays the data for the IQ and behavioral scores compared between the two groups. The mean IQ scores for the ICLP group was in the average range (mean 105.3, s.d. 13.3), but significantly lower than the mean for the control group (mean 113.0, s.d. 16.6), p = 0.01; a finding previously reported (Richman and Eliason 2009). The average PBS score for the HII section was significantly elevated in the ICLP boys (mean 12.7, s.d. 10.2) compared to the healthy boys (mean 8.9, s.d. 6.7), p = 0.021.
Table 1.
Demographics, behavior scores, general, and regional morphometry
| Demographics | ICLP (n = 50) | Controls (n = 60) | P value for difference |
|---|---|---|---|
| Mean (SD), Median | Mean (SD), Median | ||
| Age (years) | 11.9 (3.3), 11.0 | 12.1 (2.7), 11.7 | 0.640 |
| Parental SES score | 2.67 (0.51), 3.0 | 2.33 (0.56), 2.0 | 0.001 |
| IQ and behavior scores | |||
| Full scale IQ (FSIQ) | 105.3 (13.3), 104 | 113 (16.6),110 | 0.010 |
| Hyperactivity/impulsivity/inattention (HII) | 12.7 (10.2), 9.3 | 8.9 (6.7), 7.0 | 0.021 |
| Brain measures | |||
| Intracranial volume (ICV) (cc) | 1,403 (148); 1,387 | 1,444 (111); 1,433 | 0.097 |
| Cortex volume (cc) | 746 (76), 740 | 758 (57), 758 | 0.368 |
| Cortex volume/ICV (%) | 53.3 (2.0), 53.1 | 52.5 (2.3), 52.4 | 0.083 |
| vmPFC/ICV (%) | 2.17 (0.18), 2.17 | 2.09 (0.13), 2.10 | 0.010 |
| Right vmPFC/ICV (%) | 1.08 (0.09), 1.08 | 1.03 (0.07), 1.04 | 0.008 |
| Left vmPFC/ICV (%) | 1.09 (0.10), 1.08 | 1.06 (0.07), 1.06 | 0.059 |
| Asymmetry coefficient (%) | −0.83 (3.4), −1.1 | −1.36 (4.1), −1.66 | 0.469 |
Brain morphology
General measures Table 1 also displays the results of the comparison across groups of both general and regional brain measures. After controlling for the smaller ICV, boys with ICLP had proportionately enlarged cortex volumes compared to healthy controls, though this did not reach statistical significance. In our previous publication (Nopoulos et al. 2007), this was significant; however, the current analysis uses a larger control sample (n = 60) than in the previous publication (n = 50).
Region of interest Expressed as a ratio of ICV, the volume of the right vmPFC was significantly elevated in the ICLP boys (2.02, s.d. = 0.17) compared to the healthy control boys (1.97, s.d. 0.14), p = 0.008. This difference persisted after adjustment for age and parental SES (p = 0.007). The left vmPFC, however, was not quite significantly elevated (2.06, s.d. 0.18 in the ICLP boys compared to 2.02, s.d. = 0.17 in the healthy control boys; p = 0.059).
Laterality The AC was negative for both groups, indicating a slightly larger left vmPFC than the right. The ICLP and control groups did not differ. Within the ICLP group, subjects with unilateral cleft were identified and compared to each other to assess if unilateral clefting affected the AC. Unlilateral clefts are possible in CLO and CLP (CPO are not lateralized) giving a total of 37 subjects; however, five of these were bilateral, leaving 32 unilateral subjects, 13 with clefts on the right and 19 with clefts on the left. The AC was not significantly different between the right and left group (right cleft mean, −1.07; s.d., 2.64; left cleft mean, −1.48, s.d., 3.7; p = 0.730). In addition, the right cleft group did not differ from the left cleft group in HI scores (right cleft mean, 13.5; s.d., 12.6; left cleft mean, 13.4, s.d. 9.1; p = 0.984) or right vmPFC to ICV ratios (right cleft mean, 1.05%; s.d., 0.07%; left cleft mean, 1.08%; s.d., 0.11%; p = 0.511).
Effects of IQ Since IQ can potentially impact both behavior and/or brain function, we tested the relationship between FSIQ and brain morphology (the right vmPFC), and FSIQ and HII scores. Pearson correlation showed no relationship between FSIQ and the ratio of right vmPFC to ICV (r = 0.03, p = .798) and no significant relationship between FSIQ and HII score (r = −0.14, p = 0.155). Thus, the findings of increased HII and right vmPFC volume in the ICLP males are not confounded by the difference in FSIQ scores between the two groups.
Relationship between region of interest morphology and behavior scores
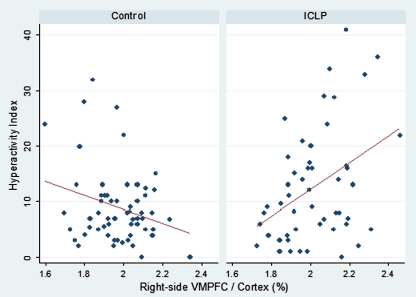
There was a robust interaction between group status and the right vmPFC when predicting HII scores (p < 0.001). When analyzed separately, there was a significant negative correlation (r = −0.26, p = 0.041) between HII and right vmPFC ratio in the control group, meaning those boys with the lowest proportional volume of the right vmPFC were those with the highest HII scores. This is in line with our previous analysis of this group looking at a slightly restricted behavior analysis of impulse control scores (as the current analysis also included inattention scores); however, in contrast, the relationship between the right vmPFC and HII scores in the ICLP boys was a significant positive correlation (r = 0.40, p = 0.005), indicating that those boys with the highest proportional volume of the right vmPFC were those with the highest HII scores. See Fig. 2 for an illustration of this interaction. These within-group associations remained significant after adjustment for parental SES. There was no significant interaction between parental SES and right vmPFC ratios within either group (p > 0.30 in each group).
Fig. 2.
Relationship between behavior scores and right vmPFC structure
Finally, to evaluate further regional specificity, the rmvPFC to cortex ratio was broken down into its two components of medial orbitofrontal (MOF) and lateral orbitofrontal (LOF). Although both regions were enlarged in the ICLP group compared to the controls, this is only significant for the MOF (ICLP MOF mean = 0.79%; s.d., 0.09%; control mean = 0.75%; s.d., 0.08%; p = 0.048; ICLP LOF mean = 1.23%; s.d., 0.12; control mean = 1.21%; s.d., 0.11%, p = 0.351). Conversely, though both regions were positively correlated with HII in the ICLP group, this was only significant in the LOF (LOF r = 0.45, p = .001; MOF r = 0.16, p = 0.274).
Discussion
The current study finds that boys with ICLP have elevated levels of HII behaviors. Although externalizing behaviors have been documented as being elevated in ICLP children, no study to date has systematically evaluated HII behaviors in this population. One important exception is the study by Richman et al. that examined a sample of children with ICLP and diagnosed ADHD by an outside clinician (Richman et al. 2004). After careful examination to determine the accuracy of the ADHD diagnosis, they reported that many ICLP children that were diagnosed ADHD were actually misclassified and were manifesting learning disabilities instead.
The proportion of boys in our ICLP sample that carried a clinical diagnosis of ADHD (based on separate a assessment of local clinician) was five of 50 or 10%, somewhat higher than the ∼3–7% of all children in the general population (Richman et al. 2004); however, by ratings of parent and teacher’s assessment of HII behaviors, nine of 50 or 18% of the ICLP boys had clinically significant elevations of these behaviors. Even without consideration of what is deemed clinically significant or pathologically elevated, as a whole, boys with ICLP exhibit these behaviors more frequently or to a greater degree than their peer counterparts.
The region of the brain thought to be a neuroanatomic correlate of these behaviors, the ventromedial prefrontal cortex (vmPFC) was structurally abnormal in the boys with ICLP. Compared to healthy boys, the vmPFC was proportionately enlarged. This is despite the finding in our previous work that the frontal lobe of children with ICLP is proportionately smaller. Therefore, it is important to emphasize that despite the overall smaller volume of the frontal lobe in ICLP (both white and gray matter), the right vmPFC, a subregion within the frontal cortex, is enlarged. It is thought that an important function of this cortical region is to identify the emotional salience of stimuli and use that information to assign values to possible behavioral outcomes (Bechara 2005; Bechara and Van Der Linden 2005). In the context of a neurocognitive theory of impulse control, the amygdala (the impulsive system) tags stimuli as having immediate pain or pleasure. This is then countered by the reflective system (the vmPFC) which weighs the long-term consequences of any given action. Thus, impulsive behavior may be due to imbalance of the system with the amygdala having overactive or stronger than normal input compared to the vmPFC. Future studies are required to evaluate these relationships in subjects with ICLP.
Although the left vmPFC was slightly enlarged as well, this did not reach statistical significance. This is consistent with some functional lesion studies that show in males where right unilateral damage to the vmPFC results in substantially more severe behavioral impairment in males compared to damage in the left vmPFC (Tranel et al. 2005). This suggests that for males, it is the right hemisphere that is more important in relationship to behaviors and behavioral impairments.
The fact that the ICLP boys show excess HII and structural abnormalities in the right vmPFC seems in line with what is seen in the healthy controls. While the fact that the cortex is enlarged rather than smaller than normal may at first seem counterintuitive, the phenomenon of excess cortical tissue in males with ICLP has been previously well documented in our previous work. This phenomenon is also seen in other neurodevelopmental disorders, including autism (Piven et al. 1996). Moreover, the positive correlation between HII scores and vmPFC morphology in ICLP boys (the greater the volume, the more abnormal the behavior) support the notion that this is indeed pathological enlargement and not conceptualized as a compensatory mechanism of some type.
The spectrum of morphology of the vmPFC from abnormally small/thin to abnormally thick/large can be correlated with the same spectrum of severity of behavior. In ADHD, the vmPFC has been shown to be abnormally thin (Shaw et al. 2007b); however on the opposite side of the morphology spectrum, where the vmPFC is abnormally large (as in the current study), there are again higher levels of impulsivity. This relationship can be conceptualized as a U-shaped curve in which abnormally small or abnormally large volumes of vmPFC are correlated to pathologic elevations of HII, whereas intermediate volumes are associated with low levels of these types of behaviors. ICLP boys would thus be considered to not have the same pathoetiology of the typical ADHD, but instead a phenocopy in which the behaviors are descriptively the same as that of ADHD, and the region of the brain sub-serving impulse control is affected, but clearly by an altogether different pathologic process. This same phenomenon is seen in the context of total brain volume in which both microcephaly and macrocephaly are associated with mental retardation—again, a U-shaped curve in the relationship between IQ and total brain size.
The current finding of pathological enlargement of cortex in ICLP boys is similar in some ways to a recent study of children with idiopathic epilepsy who, like the ICLP kids, also showed elevated rates of hyperactivity and inattention. Similar to the current study, they also found cortical thickening in association with these behaviors (Hermann et al. 2007); however the location was different—the dorsolateral prefrontal cortex (rather than the ventral prefrontal cortex) was enlarged in the children with epilepsy. Although ICLP and epilepsy both have elevated rates of hyperactivity and inattention, there is little else that is clinically similar between the two; however, they are both neurodevelopmental disorders. The children with idiopathic epilepsy example highlights the notion that developmental aberration in general can lead to structural abnormalities in the brain (for example, cortical thickening) and can be manifested in symptoms of hyperactivity and inattention, presenting as a phenocopy of ADHD.
The microstructure of the ICLP cortex is unknown, therefore the exact nature of the cortical enlargement is also unknown. Whether it be enlarged neurons, excess glia or neuropil, or excess dendrites, the end result suggests that whatever the mechanism, the functionality of this region is clearly compromised. Moreover, the connectivity of an abnormally structured region could also be impaired, a finding that future studies evaluating white matter integrity should focus on.
In sum, the current study identifies ICLP boys to have substantially elevated HII scores compared to a healthy comparison group. Moreoever, the quantitative measures of HII were directly related to the volume of the vmPFC, an area of the brain with an important role in these behaviors. Further studies will be needed to replicate and extend the findings in order to assess factors such as effects of clefting phenotype and whether these findings would also extend to females with ICLP.
Acknowledgements
This research was supported by the following grant: National Institute of Dental and Craniofacial Research “Brain structure and function in Children with Oral Clefts” 1 RO1 DE01 14399 01 A1.
References
- Achenbach TM. Manual for the child behavior checklist/4–18 and the 1991 profile. Burlington: University of Vermonst Department of Psychiatry; 1991. [Google Scholar]
- Bechara A. Decision making, impulse control and loss of willpower to resist drugs: a neurocognitive perspective. Nat Neurosci. 2005;8(11):1458–63. doi: 10.1038/nn1584. [DOI] [PubMed] [Google Scholar]
- Bechara A, Linden M. Decision-making and impulse control after frontal lobe injuries. Curr Opin Neurol. 2005;18(6):734–9. doi: 10.1097/01.wco.0000194141.56429.3c. [DOI] [PubMed] [Google Scholar]
- Boes AD, Bechara A, Tranel D, Anderson SW, Richman L, Nopoulos P. Right ventromedial prefrontal cortex: a neuroanatomical correlate of impulse control in boys. Soc Cogn Affect Neurosci. 2009;4(1):1–9. doi: 10.1093/scan/nsn035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broder HL, Richman LC, Matheson PB. Learning disability, school achievement, and grade retention among children with cleft: a two-center study. Cleft Palate Craniofac J. 1998;35(2):127–31. doi: 10.1597/1545-1569(1998)035<0127:LDSAAG>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- Canfield MA, Honein MA, Yuskiv N, et al. National estimates and race/ethnic-specific variation of selected birth defects in the United States, 1999–2001. Birth Defects Res A Clin Mol Teratol. 2006;76(11):747–56. doi: 10.1002/bdra.20294. [DOI] [PubMed] [Google Scholar]
- Conrad AL, Richman L, Nopoulos P, Dailey S. Neuropsychological functioning in children with non-syndromic cleft of the lip and/or palate. Child Neuropsychol. 2009;2:1–14. doi: 10.1080/09297040802691120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desikan RS, Segonne F, Fischl B, et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage. 2006;31(3):968–80. doi: 10.1016/j.neuroimage.2006.01.021. [DOI] [PubMed] [Google Scholar]
- Endriga MC, Jordan JR, Speltz ML. Emotion self-regulation in preschool-aged children with and without orofacial clefts. J Dev Behav Pediatr. 2003;24(5):336–44. doi: 10.1097/00004703-200310000-00004. [DOI] [PubMed] [Google Scholar]
- Hermann B, Jones J, Dabbs K, et al. The frequency, complications and aetiology of ADHD in new onset paediatric epilepsy. Brain. 2007;130(Pt 12):3135–48. doi: 10.1093/brain/awm227. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB, Redlich FC. Social class and mental illness. New York: Wiley; 1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt O, Burden D, Hepper P, Stevenson M, Johnston C. Parent reports of the psychosocial functioning of children with cleft lip and/or palate. Cleft Palate Craniofac J. 2007;44(3):304–11. doi: 10.1597/05-205. [DOI] [PubMed] [Google Scholar]
- Jones MC. Etiology of facial clefts: prospective evaluation of 428 patients. Cleft Palate J. 1988;25:16–20. [PubMed] [Google Scholar]
- Kochanska G, Knaack A. Effortful control as a personality characteristic of young children: antecedents, correlates, and consequences. J Pers. 2003;71(6):1087–112. doi: 10.1111/1467-6494.7106008. [DOI] [PubMed] [Google Scholar]
- Lindgren S, Koeppl G. Assessing child behavior problems in a medical setting: development of the pediatric behavior scale. Adv Behav Assess Child Fam. 1987;3:57–90. [Google Scholar]
- Magnotta V, Harris G, Andreasen NC, O’Leary DS, Yuh WT, Heckel D. Structural MR image processing using the BRAINS2 toolbox. Comput Med Imaging Graph. 2002;26(4):251–64. doi: 10.1016/S0895-6111(02)00011-3. [DOI] [PubMed] [Google Scholar]
- McKay KE, Halperin JM. ADHD, aggression, and antisocial behavior across the lifespan. Interactions with neurochemical and cognitive function. Ann N Y Acad Sci. 2001;931:84–96. doi: 10.1111/j.1749-6632.2001.tb05774.x. [DOI] [PubMed] [Google Scholar]
- Nopoulos P, Langbehn DR, Canady J, Magnotta V, Richman L. Abnormal brain structure in children with isolated clefts of the lip or palate. Arch Pediatr Adolesc Med. 2007;161(8):753–8. doi: 10.1001/archpedi.161.8.753. [DOI] [PubMed] [Google Scholar]
- Piven J, Arndt S, Bailey J, Andreasen NC. Regional brain enlargement in autism: an MRI study. J Am Acad Child Adolesc Psych. 1996;35(4):530–536. doi: 10.1097/00004583-199604000-00020. [DOI] [PubMed] [Google Scholar]
- Richman L, Eliason M. Disorders of communication: developmental language disorders and cleft palate. In: Walker CE, Roberts MC, editors. Handbook of clinical child psychololgy. New York: Wiley; 2001. pp. 603–617. [Google Scholar]
- Richman L, Eliason M. Psychological characteristics associated with cleft palate. In: Moller K, Glaze L, editors. Cleft lip and palate: inerdisciplinary issues and treatment. Austin: Pro-ed; 2009. pp. 453–480. [Google Scholar]
- Richman L, Millard T. Brief report: cleft lip and palate: longitudinal behavior and relationships of clef conditions to behavior and achievement. J Pediatr Psychol. 1997;22:487–494. doi: 10.1093/jpepsy/22.4.487. [DOI] [PubMed] [Google Scholar]
- Richman LC, Eliason MJ, Lindgren SD. Reading disability in children with cleft lip and/or palate. Cleft Palate J. 1988;25:21–25. [PubMed] [Google Scholar]
- Richman LC, Ryan S, Wilgenbusch T, Millard T. Overdiagnosis and medication for attention-deficit hyperactivity disorder in children with cleft: diagnostic examination and follow-up. Cleft Palate Craniofac J. 2004;41(4):351–4. doi: 10.1597/03-047.1. [DOI] [PubMed] [Google Scholar]
- Shaw P, Gornick M, Lerch J, et al. Polymorphisms of the dopamine D4 receptor, clinical outcome, and cortical structure in attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2007;64(8):921–31. doi: 10.1001/archpsyc.64.8.921. [DOI] [PubMed] [Google Scholar]
- Shaw P, Eckstrand K, Sharp W, et al. Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proc Natl Acad Sci U S A. 2007;104(49):19649–54. doi: 10.1073/pnas.0707741104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tranel D, Damasio H, Denburg NL, Bechara A. Does gender play a role in functional asymmetry of ventromedial prefrontal cortex? Brain. 2005;128(Pt 12):2872–81. doi: 10.1093/brain/awh643. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler intelligence scale for children. 3. Washington, D.C.: The Psychological Corporation; 1991. [Google Scholar]
- Wechsler D. Wechsler adult intelligence scale. 3. Washington, D.C.: The Psychological Corporation; 1997. [Google Scholar]