Abstract
Platelet derived growth factors have been shown to stimulate cell proliferation efficiently in vivo1,2 and in vitro. This effect has been reported for mesenchymal stromal cells (MSCs), fibroblasts and endothelial colony-forming cells with platelets activated by thrombin3-5 or lysed by freeze/thaw cycles6-14 before the platelet releasate is added to the cell culture medium. The trophic effect of platelet derived growth factors has already been tested in several trials for tissue engineering and regenerative therapy.1,15-17 Varying efficiency is considered to be at least in part due to individually divergent concentrations of growth factors18,19 and a current lack of standardized protocols for platelet preparation.15,16 This protocol presents a practicable procedure to generate a pool of human platelet lysate (pHPL) derived from routinely produced platelet rich plasma (PRP) of forty to fifty single blood donations. By several freeze/thaw cycles the platelet membranes are damaged and growth factors are efficiently released into the plasma. Finally, the platelet fragments are removed by centrifugation to avoid extensive aggregate formation and deplete potential antigens. The implementation of pHPL into standard culture protocols represents a promising tool for further development of cell therapeutics propagated in an animal protein-free system.
Protocol
1. Starting material
Start with platelet rich plasma (PRP) units prepared by cytapheresis or derived from buffy coats.
2. Sterility check
For sterility check take a sample of 20 mL from each PRP unit by transferring the volume to a connected small bag (Baxter). Disconnect this bag by welding.
3. Freezing of PRP units
Immediately after preparation, freeze the PRP units down to at least -20°C in the original storage bag without further manipulation.
4. Thawing of HPL units
When bacterial tests are negative, thaw human platelet lysate units, now called HPL units at 37°C (water bath) until the ice clots disappear. Do not warm the HPL.
5. Pooling of HPL units
Take at least ten to fifteen thawed HPL units for one platelet lysate pool to prepare a standardized product. Connect the HPL bags consecutively to the pooling double bag (MacoPharma) and transfer the HPL into these two bags. Disconnect the empty HPL bags by welding. Get a final volume of 3 to 4 L of pooled human platelet lysate (pHPL) by mixing the content of the two bags. Connect a small bag (Baxter) and take a sample of 20 mL pHPL for sterility check of the pooled product. Disconnect this bag by welding.
6. Portioning of the pHPL
Portion the pHPL to get suitable aliquots for further processing. Connect small bags (Baxter) to the pooling double bag (Macopharma) and transfer volumes of up to 250 mL to the small storage bags (Baxter). Disconnect the filled bags by welding.
7. Re-freezing of the pHPL aliquots
Increase the rate of platelet fragmentation and the amount of released growth factors by a further freeze/thaw step. Freeze the small bags of portioned pHPL again at least -20°C.
8. Re-thawing and portioning of the pHPL aliquots
Thaw the pHPL bags at 37°C (water bath). Transfer the content into 50 mL vials (Falcons BD) by cutting the tube of the bag using sterile scissors and pouring the pHPL into the vials. Perform this step in a laminar flow bench to avoid bacterial or fungal contamination.
9. Removal of platelet fragments
As platelet fragments tend to aggregate and may induce alloimmunization, remove them from the pHPL. Centrifuge the pHPL vials therefore at 4,000g (15 minutes, 4°C). In a laminar flow bench pipette the supernatant plasma into the final storage vials (Falcons BD) and discard the platelet pellets to avoid fragments in cell culture.
10. Storage of pHPL
Freeze aliquots of 50 mL pHPL vials again at least-20°C and store them for experimental use.
11. Use of pHPL in cell culture
Initially add preservative-free heparin to the medium to avoid gel formation. Thaw a pHPL aliquot at 37°C and supplement the culture medium by addition of 8 – 10%.
Mediums
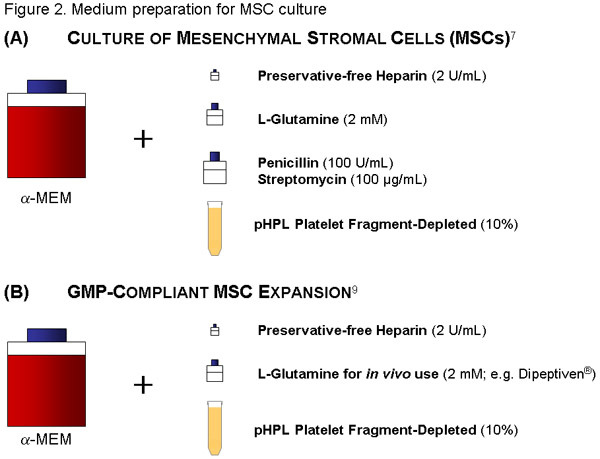
MSC-Medium:
Use 500 mL of a-MEM, add 56 mL of thawed pHPL (see also reference 1 for further details) and 2 IU/mL (=224 μl of stock solution) of preservative-free Heparin (avoids coagulation of the medium through clumping of the fibrinogen in the plasma) to reach a final concentration of 10% pHPL. Additionally add Penicillin (100U/mL) /Streptomycin (100μg/mL) solution and 2mM of L-Glutamin (both Sigma).
Filter the medium through a 20 μm-pore size vacuum filter (Millipore). Label the bottle appropriately (content, date).
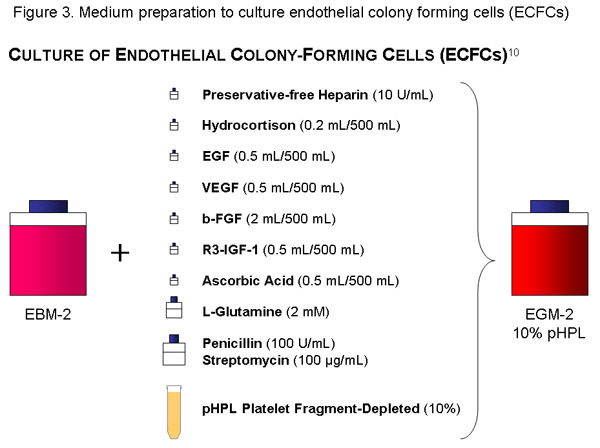
ECFC-Medium:
Use one bottle (500 mL) of EBM, add the cytokine-aliquots, 56 mL of pHPL, 10 IU/ml (=1120μl of stock solution) of preservative-free Heparin, Penicillin (100U/mL) /Streptomycin (100 g/mL) solution and 2mM of L-Glutamin to the basal medium and filter with a 20 μl-pore size vacuum filter (Millipore). Label the bottle appropriately (content, date).
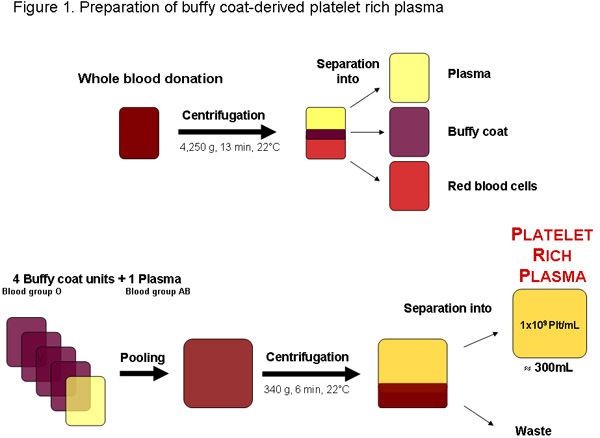 Figure 1:Preparation of platelet-rich plasma from a whole blood donation from a local blood bank or any other authorized provider. After centrifugation the blood can be separated into plasma, buffy coat and red blood cells. Four buffy coat units, blood group O and one blood group AB plasma can be pooled before centrifugation to separate the platelet rich plasma. A regular quality platelet-rich plasma unit of approximately 300mL should contain 1x109 platelets per mL or 3x1011 platelets total.
Figure 1:Preparation of platelet-rich plasma from a whole blood donation from a local blood bank or any other authorized provider. After centrifugation the blood can be separated into plasma, buffy coat and red blood cells. Four buffy coat units, blood group O and one blood group AB plasma can be pooled before centrifugation to separate the platelet rich plasma. A regular quality platelet-rich plasma unit of approximately 300mL should contain 1x109 platelets per mL or 3x1011 platelets total.
Discussion
In some regions platelet rich plasma (PRP) may be obtained from buffy-coats otherwise being a waste product of packed red blood cell production from tested blood donations (Figure 1). Optimally, PRP is used immediately for further preparation of pHPL, as in outdated platelet concentrates the availability of growth factors may be reduced due to platelet storage lesions and degradation20. It is further recommended to produce PRP by matching platelets of blood group O with plasma of blood group AB to avoid possible influences of ABH antigens and isoagglutinins. Up to now, cell cultures have mostly used fetal bovine serum (FBS) which bears the risk of xenoimmunization21 and transmission of known and unknown pathogens. Alternatives such as autologous serum or serum-free media did not yet succeed in replacing FBS in many applications.22 In previous studies we have compared the effects of pHPL and FBS on expansion of mesenchymal stromal cells revealing a higher efficiency of pHPL in cell propagation.7,8,23 The isolation and large scale expansion of endothelial progenitor cells under animal serum-free conditions in EGM-2 supplemented with pHPL has been shown by Reinisch et. al.11 and is further presented as a JoVE protocol by Nicole A. Hofmann. The protocols for preparing MSC and ECFC medium preparations are described in Figures 2 and 3.
The use of pHPL as a potent substitute for FBS represents an attractive step towards an animal serum-free Good Manufacturing Practice (GMP)-compliant development of cell therapeutics for clinical application.9,24
Acknowledgments
This work has been supported by the Austrian Research Foundation (FWF, grant N211-NAN to DS) and the Austrian Research Promotion Agency (FFG, grant N200 to DS). The authors thank Claudia Url for excellent technical assistance and Monica Farrell for linguistic editing.
References
- Nurden AT, Nurden P, Sanchez M, Andia I, Anitua E. Platelets and wound healing. Front Biosci. 2008;13:3532–3548. doi: 10.2741/2947. [DOI] [PubMed] [Google Scholar]
- Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M. Growth factors and cytokines in wound healing. Wound Repair Regen. 2008;16:585–601. doi: 10.1111/j.1524-475X.2008.00410.x. [DOI] [PubMed] [Google Scholar]
- Giacco F. Thrombin-activated platelets induce proliferation of human skin fibroblasts by stimulating autocrine production of insulin-like growth factor-1. FASEB J. 2006;20:2402–2404. doi: 10.1096/fj.06-6104fje. [DOI] [PubMed] [Google Scholar]
- Kocaoemer A, Kern S, Kluter H, Bieback K. Human AB serum and thrombin-activated platelet-rich plasma are suitable alternatives to fetal calf serum for the expansion of mesenchymal stem cells from adipose tissue. Stem Cells. 2007;25:1270–1278. doi: 10.1634/stemcells.2006-0627. [DOI] [PubMed] [Google Scholar]
- Kakudo N. Proliferation-promoting effect of platelet-rich plasma on human adipose-derived stem cells and human dermal fibroblasts. Plast Reconstr Surg. 2008;122:1352–1360. doi: 10.1097/PRS.0b013e3181882046. [DOI] [PubMed] [Google Scholar]
- Doucet C. Platelet lysates promote mesenchymal stem cell expansion: A safety substitute for animal serum in cell-based therapy applications. J Cell Physiol. 2005;205:228–236. doi: 10.1002/jcp.20391. [DOI] [PubMed] [Google Scholar]
- Schallmoser K. Human platelet lysate can replace fetal bovine serum for clinical-scale expansion of functional mesenchymal stromal cells. Transfusion. 2007;47:1436–1446. doi: 10.1111/j.1537-2995.2007.01220.x. [DOI] [PubMed] [Google Scholar]
- Reinisch A. Humanized system to propagate cord blood-derived multipotent mesenchymal stromal cells for clinical application. Regen Med. 2007;2:371–382. doi: 10.2217/17460751.2.4.371. [DOI] [PubMed] [Google Scholar]
- Schallmoser K. Rapid large-scale expansion of functional mesenchymal stem cells from unmanipulated bone marrow without animal serum Tissue Eng Part. C Methods. 2008;14:185–196. doi: 10.1089/ten.tec.2008.0060. [DOI] [PubMed] [Google Scholar]
- Lange C. Accelerated and safe expansion of human mesenchymal stromal cells in animal serum-free medium for transplantation and regenerative medicine. J Cell Physiol. 2007;213:18–26. doi: 10.1002/jcp.21081. [DOI] [PubMed] [Google Scholar]
- Reinisch A. Humanized large-scale expanded endothelial colony-forming cells function in vitro and in vivo. Blood. 2009;113:6716–6725. doi: 10.1182/blood-2008-09-181362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardo ME. Optimization of in vitro expansion of human multipotent mesenchymal stromal cells for cell-therapy approaches: further insights in the search for a fetal calf serum substitute. J Cell Physiol. 2007;211:121–130. doi: 10.1002/jcp.20911. [DOI] [PubMed] [Google Scholar]
- Carrancio S. Optimization of mesenchymal stem cell expansion procedures by cell separation and culture conditions modification. Exp Hematol. 2008;36:1014–1021. doi: 10.1016/j.exphem.2008.03.012. [DOI] [PubMed] [Google Scholar]
- Muller AM. Platelet lysate as a serum substitute for 2D static and 3D perfusion culture of stromal vascular fraction cells from human adipose tissue. Tissue Eng Part A. 2009;15:869–875. doi: 10.1089/ten.tea.2008.0498. [DOI] [PubMed] [Google Scholar]
- Anitua E, Sanchez M, Orive G, Andia I. The potential impact of the preparation rich in growth factors (PRGF) in different medical fields. Biomaterials. 2007;28:4551–4560. doi: 10.1016/j.biomaterials.2007.06.037. [DOI] [PubMed] [Google Scholar]
- Anitua E. New insights into and novel applications for platelet-rich fibrin therapies. Trends Biotechnol. 2006;24:227–234. doi: 10.1016/j.tibtech.2006.02.010. [DOI] [PubMed] [Google Scholar]
- Martinez-Zapata MJ. Efficacy and safety of the use of autologous plasma rich in platelets for tissue regeneration: a systematic review. Transfusion. 2009;49:44–56. doi: 10.1111/j.1537-2995.2008.01945.x. [DOI] [PubMed] [Google Scholar]
- Weibrich G, Kleis WK, Hafner G, Hitzler WE. Growth factor levels in platelet-rich plasma and correlations with donor age, sex, and platelet count. J Craniomaxillofac Surg. 2002;30:97–102. doi: 10.1054/jcms.2002.0285. [DOI] [PubMed] [Google Scholar]
- Frechette JP, Martineau I&, Gagnon G. Platelet-rich plasmas: growth factor content and roles in wound healing. J Dent Res. 2005;84:434–439. doi: 10.1177/154405910508400507. [DOI] [PubMed] [Google Scholar]
- Seghatchian J, Krailadsiri P. The platelet storage lesion. Transfus Med Rev. 1997;11:130–144. doi: 10.1053/tm.1997.0110130. [DOI] [PubMed] [Google Scholar]
- Selvaggi TA, Walker RE, Fleisher TA. Development of antibodies to fetal calf serum with arthus-like reactions in human immunodeficiency virus-infected patients given syngeneic lymphocyte infusions. Blood. 1997;89:776–779. [PubMed] [Google Scholar]
- Tonti GA, Mannello F. From bone marrow to therapeutic applications: different behaviour and genetic/epigenetic stability during mesenchymal stem cell expansion in autologous and foetal bovine sera. Int J Dev Biol. 2008;52:1023–1032. doi: 10.1387/ijdb.082725gt. [DOI] [PubMed] [Google Scholar]
- Bieback K. Human Alternatives to Fetal Bovine Serum for the Expansion of Mesenchymal Stromal Cells from Bone Marrow. Stem Cells. 2009 doi: 10.1002/stem.139. [DOI] [PubMed] [Google Scholar]
- Rohde E, Schallmoser K, Bartmann C, Reinisch A. GMP-Compliant Propagation of Human Multipotent Mesenchymal Stromal Cells. In: Gad SC, editor. Pharmaceutical Manufacturing Handbook: Regulations and Quality. John Wiley and Sons, Inc; 2008. pp. 97–115. [Google Scholar]


