Abstract
INTRODUCTION:
Pseudomonas aeruginosa (P. aeruginosa) is one of the primary opportunistic pathogens responsible for nosocomial infections. Aminoglycosides are an important component of antipseudomonal chemotherapy. The inactivation of drugs by modifying enzymes is the most common mechanism of aminoglycoside resistance.
OBJECTIVES:
The inactivation of aminoglycosides by modifying enzymes is the primary resistance mechanism employed by P. aeruginosa. The aim of the present study was to investigate the occurrence of aminoglycoside resistance and the prevalence of four important modifying enzyme genes (aac (6′)-I, aac (6′)-II, ant (2″)-I, aph (3′)-VI) in P. aeruginosa in Iran.
METHODS:
A total of 250 clinical isolates of P. aeruginosa were collected from several hospitals in seven cities in Iran. Antimicrobial susceptibility tests (using the disk diffusion method and E-tests) were performed for all 250 isolates. In addition, all isolates were screened for the presence of modifying enzyme genes by polymerase chain reaction.
RESULTS:
The resistance rates, as determined by the disk diffusion method, were as follows: gentamicin 43%, tobramycin 38%, and amikacin 24%. Of the genes examined, aac (6′)-II (36%) was the most frequently identified gene in phenotypic resistant isolates, followed by ant (2″)-I, aph (3′)-VI, and aac (6′)-I.
CONCLUSIONS:
Aminoglycoside resistance in P. aeruginosa remains a significant problem in Iran. Therefore, there is considerable local surveillance of aminoglycoside resistance.
Keywords: Pseudomonas aeruginosa, Antibiotic, Resistance, aac (6′)-II, ant (2″)-I
INTRODUCTION
Pseudomonas aeruginosa (P. aeruginosa) is one of the primary opportunistic pathogens responsible for nosocomial infections. The most important problem in the eradication of P. aeruginosa is the frequently observed multi-drug resistance of the species.1 In addition, P. aeruginosa can also acquire resistance to various antimicrobial agents, such as aminoglycosides, β-lactams2 and fluoroquinolones.3 Aminoglycosides are an important component of antipseudomonal chemotherapy,4 and they exhibit synergy with β-lactams.5 Resistance to aminoglycosides occurs via enzymatic modification, impermeability, the activity of efflux pumps (MexXY-OprM),6 the PhoP-PhoQ system,7 ndvB-dependent biofilm formation,8 and the activity of 16s rRNA methylases.9 Among these mechanisms, the inactivation of drugs by plasmid- or chromosome-encoded modifying enzymes is the most common. These modifying enzymes include aminoglycoside phosphoryl transferase (aph), aminoglycoside acetyltransferase (aac), and aminoglycoside nucleotidyl transferase (ant).10-12 Four of these enzymes, encoded by aac (6′)-I, aac (6′)-II, ant (2″)-I, and aph (3′)-VI, are of particular significance because they are among the most common modifying enzymes present in P. aeruginosa, and their substrates are the most important antipseudomonal aminoglycosides. aac (6′)-I confers resistance to tobramycin and amikacin, aac (6′)-II and ant (2″)-I inactivate tobramycin and gentamicin, and amikacin is the substrate of aph (3′)-VI.13,14
The aim of the present nationwide study was to investigate the occurrence of aminoglycoside resistance and the prevalence of the resistance-modifying enzyme genes, aac (6′)-I, aac (6′)-II, ant (2″)-I and aph (3′)-VI, in P. aeruginosa isolated from several hospitals in seven Iranian cities.
METHODS AND MATERIALS
Collection of bacterial isolates
A total of 250 non-duplicate, clinical isolates of P. aeruginosa were collected from a nationwide distribution of several hospitals in seven cities in Iran (Tehran, Shiraz, Zahedan, Tabriz, Sannandaj, Sari, and Ahvaz) between May 2007 and January 2008. Strain data and the demographic and clinical data for each patient were regularly forwarded to our laboratory. The study population was 62% male and 38% female. The specimens were isolated from urine (38%), wounds (18%), the trachea (18%), blood (10%), sputum (9%), and other sources (7%). Isolate confirmations were conducted using conventional biochemical tests, and then the isolates were stored at –76°C in glycerol skim milk broth.
Antimicrobial susceptibility testing
Antimicrobial susceptibility tests were performed using the disk diffusion method according to Clinical and Laboratory Standards Institute (CLSI) guidelines15 for three aminoglycosides [gentamicin (10 µg), amikacin (30 µg), and tobramycin (10 µg)] and for five other antibiotics [imipenem (10 µg), piperacillin (100 µg), ticarcillin (75 µg), ceftazidime (30 µg), and ciprofloxacin (5 µg)]. All drugs were obtained from Mast laboratories (Merseyside, United Kingdom). For all 250 isolates, the minimum inhibitory concentrations (MIC) of amikacin, gentamicin, and tobramycin were determined using the E-test (Biodisk, Dalvagen, Sweden) according to CLSI guidelines. P. aeruginosa (ATCC 27853) served as a control for the disk diffusion and E-tests.
Polymerase chain reaction amplification
Polymerase chain reaction (PCR) was used to screen all 250 isolates for the presence of the modifying enzyme genes, aac (6′)-I, aac (6′)-II, ant (2″)-I and aph (3′)-VI. The total template DNA for the PCR amplification was extracted from the supernatant of a mixture of P. aeruginosa cells produced by the boiling method. PCR amplification was performed using 2.5 µL of the template DNA, 1 µL of each primer,16 19.5 µL master mix, and 1 µL of Taq DNA polymerase (CinnaGen) in a total volume of 25 µL. A thermocycler (Mastercycler gradient; Eppendorf, Hamburg, Germany) was programmed with the appropriate conditions. Then, 5 µl of each PCR product was analyzed by electrophoresis on a 1% (w/v) TAE agarose gel (Fermentas UAB, Vilnius, Lithuania) containing 0.1 µl/ml ethidium bromide. The amplicons were then visualized on a UV transilluminator and photographed (BioDoc-Analyse; Biometra, Goettingen, Germany).
Statistical analysis
All statistical analyses were performed using Statistical Package for Social Sciences (SPSS) software (version 11.5) for Windows (χ2-test and Fisher's exact test). P-values of <0.05 were considered significant.
RESULTS AND DISCUSSION
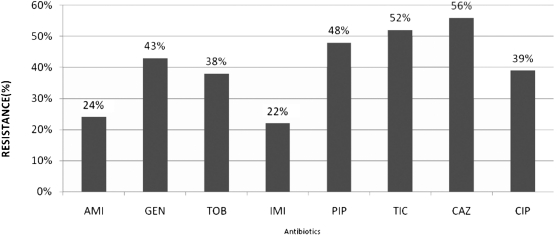
The resistance rates as determined using the disk diffusion method are presented in Figure 1. According to the disk diffusion method, 135 isolates were resistant to aminoglycosides. The resistance rates according to the E-test (base on MICs) were as follows: gentamicin 40%, tobramycin 36%, and amikacin 21%. The aminoglycoside susceptibility profiles according to the disk diffusion and E-test results for the 250 isolates are listed in Table 1.
Figure 1.
The antimicrobial resistance rate of 250 P. aeruginosa isolates as determined by the disk diffusion method AMI: amikacin, GEN: gentamicin, TOB: tobramycin, IMI: imipenem, PIP: piperacillin, TIC: ticarcillin, CAZ: ceftazidime, CIP: ciprofloxacin.
Table 1.
Aminoglycoside susceptibility profiles according to the disk diffusion method and MIC results (E-test) for 250 P. aeruginosa isolates (according to CLSI guidelines).15
| Disk Diffusion1 | E-test2 | MIC 50% (ug/mL) | MIC 90% (ug/mL). | ||||||||
| Resistant | Intermediate | Susceptible | |||||||||
| No. (%) of isolates | MIC(µg/ml) | MIC(µg/ml) | MIC(µg/ml) | ||||||||
| Resistant | Intermediate | Susceptible | –1024128 | 64–128 | 16–64 | 8 | 2–4 | <2 | |||
| Gentamicin | 108(43.2) | 8(3.2) | 134(53.6) | 10 | 41 | 49 | 8 | 98 | 44 | 4 | 64 |
| Tobramycin | 95(38) | 7(2.8) | 148(59.2) | 8 | 45 | 37 | 5 | 103 | 52 | 4 | 64 |
| MIC(µg/ml) | MIC(µg/ml) | MIC(µg/ml) | MIC 50% (ug/mL) | MIC 90% (ug/mL). | |||||||
| >256 | –256128 | 64–128 | 32 | 4–16 | <4 | ||||||
| Amikacin | 59(23.6) | 7(2.8) | 184(73.6) | 4 | 17 | 32 | 6 | 134 | 57 | 8 | 128 |
1. Zone diameter (mm) for gentamicin and tobramycin, R:<12, I:13-14, S:>15; for amikacin, R:<14, I:15-16, S:>17.
2. MIC breakpoint(µg/ml) for gentamicin and tobramycin, R:>16, I:8; S:<4; for amikacin, R:>64, I:32, S:<16.
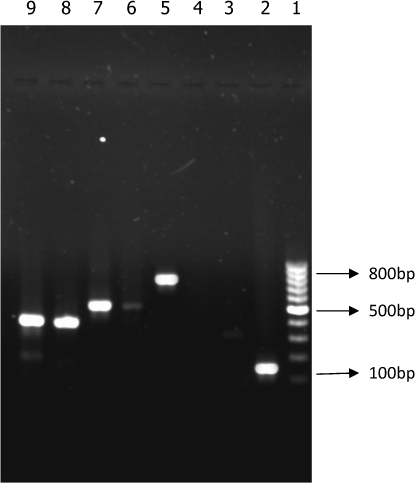
PCR analysis revealed the absence of resistance genes in susceptible isolates. The prevalence of aminoglycoside resistance genes in the 135 resistant isolates (as determined by the disk diffusion method) was as follows: aac (6′)-II was detected in 36% of the resistant isolates, ant (2″)-I was detected in 28%, aph (3′)-VI in 11%, and aac (6′)-I was found in 7% of the resistant isolates (Figure 2). Interestingly, individual aminoglycoside-resistant isolates carried multiple (two to four) modifying enzyme genes. Six isolates harbored ant(2″)-I and aac(6′)-II; three harbored aph(3′)-VI and ant(2″)-I; two harbored ant(2″)-I and aac(6′)-I; and three isolates harbored ant(2″)-I, aac(6′)-II and aph(3′)-VI. Only one isolate harbored all four genes.
Figure 2.
Lane 1, 1000 bp DNA size marker; Lane 2, aac(6′)-II (125 bp); Lane 5, aph(3′)-VI (800 bp); Lane 7, ant(2″)-I (524 bp); Lanes 8 and 9, aac(6′)-I (392 bp).
Several previous studies have examined the occurrence of aminoglycoside resistance mechanisms in P. aeruginosa isolated from different countries. The overall incidence of aminoglycoside resistance found in our study (according to the disk diffusion test and the E-test) was much higher than the incidence that has been reported previously in different countries worldwide.14,16,17 However, Estahbanati and co-workers reported that 53.3% of clinical isolates from Iranian burn patients were resistant to amikacin, and 90.7% were resistant to gentamicin, a result that reveals a high level of aminoglycoside resistance in their study.18
The aminoglycoside resistance rate was almost as high in our isolates, and most of the resistant isolates harbored modifying enzyme genes. In addition, none of the susceptible isolates harbored these resistance genes. These results highlight the importance of aminoglycoside-modification-related mechanisms in aminoglycoside resistance in P. aeruginosa. Two genes, aac (6′)-II and ant (2″)-I, were the most frequent resistance genes observed in these isolates. These results are similar to what has been observed in different studies in other countries.19-21 All isolates harboring the aac (6′)-II gene were resistant to gentamicin and tobramycin (100% concordance), which indicates that aac (6′)-II is a significant determinant of gentamicin and tobramycin resistance in P. aeruginosa. It is important to mention that we encountered an unexpected phenotype in some isolates (Table 2). For example, when an isolate harbored only the aph (3′)-VI gene, which has amikacin as a substrate, resistance to gentamicin, tobramycin, and amikacin was observed. We presume that the reason for this phenomenon might be the action of other resistance mechanisms, such as impermeability, efflux pumps, or other types of modifying enzymes. On the other hand, we detected 15 isolates which co-harbored two, three, or four aminoglycoside-modifying enzyme genes simultaneously, which is in contrast to several studies conducted in the USA and Europe, which reported that the majority of isolates exhibit only a single aminoglycoside modifying gene.22
Table 2.
Prevalence of aminoglycoside modifying enzymes genes and the correlation between these genes and phenotypic patterns in aminoglycoside resistant P. aeruginosa isolates.
| Gene | no. of isolates (%)1 | Expected resistance2 | Observed resistance phenotypes (no. of isolates)3 |
| aac(6′)-I | 9(7%) | TOB,AMI | Unexpected resistance to GEN(2) |
| aac(6′)-II | 49(36%) | GEN,TOB | Unexpected resistance to AMI(16) |
| ant(2″)-I | 38(28%) | GEN,TOB | As expected(38) |
| aph(3′)-VI | 15(11%) | AMI | Unexpected resistance to GEN and TOB(2) |
| aac(6′)-II+ ant(2″)-I | 6(4%) | GEN,TOB | As expected(6) |
| ant(2″)-I+ aph(3′)-VI | 3(2%) | AMI,GEN,TOB | As expected(3) |
| aac(6′)-I+ ant(2″)-I | 2(1%) | AMI,GEN,TOB | As expected(2) |
| ant(2″)-I + aac(6′)-II +aph(3′)-VI | 3(2%) | AMI,GEN,TOB | As expected(3) |
| aac(6′)-II ant(2″)-I+ + aph(3′)-VI + aac(6′)-I | 1(∼1%) | AMI,GEN,TOB | As expected(1) |
1. According to the disk diffusion method, a total of 135 resistant isolates were identified.
2. AMI: amikacin, GEN: gentamicin, TOB: tobramycin.
3. Described in greater detail in the text.
Miller et al. brought together the results of several studies of aminoglycoside resistance in P. aeruginosa carried out worldwide.22 Their results indicated that in Europe, aac(6′)-II was the most prevalent resistance gene (32.5%), followed by ant(2″)-I (16.9%). These results are in concordance with our study. In contrast to our results, a Korean nationwide study of 250 isolates of P. aeruginosa reported that aph(3′)-VI, ant(2″)-I, and aac(6′)-I were all prevalent, but none harbored aac(6′)-II.16 The difference in the distribution of modifying enzymes may derive from differences in aminoglycoside prescription patterns, the selection of bacterial population or geographical differences in the occurrence of aminoglycoside resistance genes.
CONCLUSIONS
In conclusion, although aminoglycosides remain useful antipseudomonal agents, resistance to these drugs continues to be a major issue, especially in Iran. Because these aminoglycoside resistance genes are usually located on mobile genetic elements (i.e., plasmid, transposon, or integrons),23,24 there is a growing concern that they could easily spread and be disseminated among other bacteria. Integrons that carry gene cassettes encoding both aacs and carbapenemases will only exacerbate this problem.25 The design of novel aminoglycosides with stronger affinity for their targets and resistance to these modifying enzymes is inevitable,26 and the new generation of anti-Pseudomonas therapy is forthcoming.27 Aminoglycoside resistance among clinical isolates of P. aeruginosa promises to become a major clinical concern in the future, and continuous local surveillance of aminoglycoside resistance is crucial.
ACKNOWLEDGEMENTS
This study was funded by a M.Sc. grant from the Tarbiat Modares University, Tehran, Iran.
REFERENCES
- 1.Lambert PA. Mechanisms of antibiotic resistance in Pseudomonas aeruginosa. J R Soc Med. 2002;95(suppl 41):22–6. [PMC free article] [PubMed] [Google Scholar]
- 2.Park YJ. Prevalence of Ambler class A and D β-lactamases among clinical isolates of Pseudomonas aeruginosa in Korea. J Antimicrob Chemother. 2005;56:122–7. doi: 10.1093/jac/dki160. 10.1093/jac/dki160 [DOI] [PubMed] [Google Scholar]
- 3.Jalal S, Ciofu O, Høiby N, Gotoh N, Wretlind B. Molecular mechanisms of fluoroquinolone resistance in Pseudomonas aeruginosa isolates from cystic fibrosis patients. Antimicrob Agents Chemother. 2000;44:710–2. doi: 10.1128/aac.44.3.710-712.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Giamarellou H. Therapeutic guidelines for Pseudomonas aeruginosa infections. Int J antimicrob Agen. 2000;16:103–6. doi: 10.1016/s0924-8579(00)00212-0. 10.1016/S0924-8579(00)00212-0 [DOI] [PubMed] [Google Scholar]
- 5.Dubois V, Arpin C, Dupart V, Scavelli A, Coulange L, Andre C, et al. β-lactam and aminoglycoside resistance rates and mechanisms among Pseudomonas aeruginosa in French general practice (community and private healthcare centres) J Antimicrob Chemother. 2008;62:316–23. doi: 10.1093/jac/dkn174. 10.1093/jac/dkn174 [DOI] [PubMed] [Google Scholar]
- 6.Islam S, Oh H, Jalal S, Karpati F, Ciofu O, Høiby N, et al. Chromosomal mechanisms of aminoglycoside resistance in Pseudomonas aeruginosa isolates from cystic fibrosis patients. Clin Microbiol Infect. 2009;15:60–6. doi: 10.1111/j.1469-0691.2008.02097.x. 10.1111/j.1469-0691.2008.02097.x [DOI] [PubMed] [Google Scholar]
- 7.Macfarlane E, Kwasnicka A, Hancock R. Role of Pseudomonas aeruginosa PhoP-PhoQ in resistance to antimicrobial cationic peptides and aminoglycosides. Microbiol. 2000;146:2543–54. doi: 10.1099/00221287-146-10-2543. [DOI] [PubMed] [Google Scholar]
- 8.Sadovskaya I, Vinogradov E, Li J, Hachani A, Kowalska K, Filloux A. High-level antibiotic resistance in Pseudomonas aeruginosa biofilm: the ndvB gene is involved in the production of highly glycerol-phosphorylated β-(1→3)-glucans, which bind aminoglycosides. Glycobiol. 2010;20:895–904. doi: 10.1093/glycob/cwq047. 10.1093/glycob/cwq047 [DOI] [PubMed] [Google Scholar]
- 9.Doi Y, Ghilardi AC, Adams J, de Oliveira GD, Paterson DL. High prevalence of metallo- β-lactamase and 16S rRNA methylase coproduction among imipenem- resistant Pseudomonas aeruginosa isolates in Brazil. Antimicrob Agents Chemother. 2007;51:3388–90. doi: 10.1128/AAC.00443-07. 10.1128/AAC.00443-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shaw KJ, Rather PN, Hare RS, Miller GH. Molecular genetics aminoglycoside resistance genes and familial relationship of the aminoglycoside modifying enzymes. Microbiol Rev. 1993;57:138–63. doi: 10.1128/mr.57.1.138-163.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith CA, Baker EN. Aminoglycoside antibiotic resistance by enzymatic deactivation. Curr Drug Targets Infect Disord. 2002;2:143–60. doi: 10.2174/1568005023342533. 10.2174/1568005023342533 [DOI] [PubMed] [Google Scholar]
- 12.Yamane K, Wachino J, Doi Y, Kurokawa H, Arakawa Y. Global spread of multiple aminoglycoside resistance genes. Emerg Infect Dis. 2005;11:951–3. doi: 10.3201/eid1106.040924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller GH, Sabatelli FJ, Naples L, Hare RS, Shaw KJ. The most frequently occurring aminoglycoside resistance mechanisms— combined results of surveys in eight regions of the world. J Chemother. 1995;7((Suppl. 2)):17–30. [PubMed] [Google Scholar]
- 14.Poole K. Aminoglycoside resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2005;49:479–87. doi: 10.1128/AAC.49.2.479-487.2005. 10.1128/AAC.49.2.479-487.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Clinical and Laboratory Standards Institute Performance standards for antimicrobial susceptibility testing; seventeenth informational supplement. CLSI document M100-S17. CLSI, 2007 Wayne, PA
- 16.Kim JY, Park YJ, Kwon HJ, Han K, Kang MW, Woo GJ. Occurrence and mechanisms of amikacin resistance and its association with β-lactamases in Pseudomonas aeruginosa: a Korean nationwide study. J Antimicrob Chemother. 2008;62:479–83. doi: 10.1093/jac/dkn244. 10.1093/jac/dkn244 [DOI] [PubMed] [Google Scholar]
- 17.Cavallo J, Hocquet D, Plesiat P, Fabre R, Roussel-Delvallez M. Susceptibility of Pseudomonas aeruginosa to antimicrobials: a 2004 French multicentre hospital study. J Antimicrob Chemother. 2007;59:1021–4. doi: 10.1093/jac/dkm076. 10.1093/jac/dkm076 [DOI] [PubMed] [Google Scholar]
- 18.Estahbanati H, Kashani P, Ghanaatpisheh F. Frequency of Pseudomonas aeruginosa serotypes in burn wound infections and their resistance to antibiotics. Burns. 2002;28:340–8. doi: 10.1016/s0305-4179(02)00024-4. 10.1016/S0305-4179(02)00024-4 [DOI] [PubMed] [Google Scholar]
- 19.Busch-Sorensen C, Sonmezoglu M, Frimodt-Moller N, Hojbjerg T, Miller GH, Espersen F. Aminoglycoside resistance mechanisms in Enterobacteriaceae and Pseudomonas spp. from two Danish hospitals: correlation with type of aminoglycoside used. APMIS. 1996;104:763–8. [PubMed] [Google Scholar]
- 20.Over U, Gur D, Unal S, Miller GH. The changing nature of aminoglycoside resistance mechanisms and prevalence of newly recognized resistance mechanisms in Turkey. Clin Microbiol Infect. 2001;7:470–8. doi: 10.1046/j.1198-743x.2001.00284.x. [DOI] [PubMed] [Google Scholar]
- 21.Phillips I, King A, Shannon K. Prevalence and mechanisms of aminoglycoside resistance. A ten-year study. Am J Med. 1986;80:48–55. doi: 10.1016/0002-9343(86)90479-1. [DOI] [PubMed] [Google Scholar]
- 22.Miller GH, Sabatelli FJ, Hare RS, Glupczynski Y, Mackey P, Shlaes D, et al. The most frequent aminoglycoside resistance mechanisms changes with time and geographic area: a reflection of aminoglycoside usage patterns. Clin Infect Dis. 1997;24:S46–62. doi: 10.1093/clinids/24.supplement_1.s46. 10.1093/clinids/24.Supplement_1.S46 [DOI] [PubMed] [Google Scholar]
- 23.Park YJ. Aminoglycoside Resistance in Gram-negative Bacilli. Korean J Clin Microbiol. 2009;12:57–61. [Google Scholar]
- 24.Ramirez MS, Tolmasky ME. Aminoglycoside modifying enzymes. Drug Resist. 2010;13:151–71. doi: 10.1016/j.drup.2010.08.003. 10.1016/j.drup.2010.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strateva T, Yordanov D. Pseudomonas aeruginosa – a phenomenon of bacterial resistance. J Medic Microbiol. 2009;58:1133–48. doi: 10.1099/jmm.0.009142-0. 10.1099/jmm.0.009142-0 [DOI] [PubMed] [Google Scholar]
- 26.Haddad J, Kotra LP, Llano-Sotelo B, Kim C, Azucena EF, Liu M, et al. Design of novel antibiotics that bind to the ribosomal acyltransfer site. J Am Chem Soc. 2002;124:3229–37. doi: 10.1021/ja011695m. 10.1021/ja011695m [DOI] [PubMed] [Google Scholar]
- 27.Page M, Heim J. Prospects for the next anti-Pseudomonas drug. Curr Opin Pharmacol. 2009;9:558–65. doi: 10.1016/j.coph.2009.08.006. 10.1016/j.coph.2009.08.006 [DOI] [PubMed] [Google Scholar]