Abstract
Our aim was to assess whether a combination of seasonal climate forecasts, monitoring of meteorological conditions, and early detection of cases could have helped to prevent the 2002 malaria emergency in the highlands of western Kenya. Seasonal climate forecasts did not anticipate the heavy rainfall. Rainfall data gave timely and reliable early warnings; but monthly surveillance of malaria out-patients gave no effective alarm, though it did help to confirm that normal rainfall conditions in Kisii Central and Gucha led to typical resurgent outbreaks whereas exceptional rainfall in Nandi and Kericho led to true malaria epidemics. Management of malaria in the highlands, including improved planning for the annual resurgent outbreak, augmented by simple central nationwide early warning, represents a feasible strategy for increasing epidemic preparedness in Kenya.
A strategic aim advocated by Roll Back Malaria—a partnership founded by WHO, the United Nations Development Programme, the United Nations Children’s Fund (UNICEF), and the World Bank to help reduce the burden of malaria in Africa—is the implementation of malaria early warning systems (MEWS) to facilitate timely responses to prevent and contain malaria epidemics.1 Our goal was to examine what contribution the proposed methods for seasonal climate forecasting, early warning through the monitoring of meteorological conditions, and early detection (case surveillance) would have made to preparedness activities for the 2002 malaria emergency in western Kenya.
The highlands of western Kenya have seasonal mesoendemic malaria transmission with resurgent outbreaks2 in June and July after the long rains.3 The role of MEWS in these highland areas is often, therefore, to detect whether a seasonal resurgent outbreak is usual or has the potential to become a true epidemic.2 A joint UNICEF and Division of Malaria Control team was sent to four districts (Kisii Central, Gucha, Nandi, and Kericho) to examine the true extent of the media publicised emergency and to ascertain how existing surveillance mechanisms and available data could have assisted in epidemic preparedness.
A seasonal climate forecast for the March–May period was published in February, 2002, by the Greater Horn of Africa Climate Forum (http://www.cpc.ncep.noaa.gov/products/african_desk). The outlook for the Kenyan western highlands was for the highest likelihood (40%) of normal conditions, a 35% chance of higher than average rainfall, and a 25% chance of drier than average conditions. Although the long lead-time of a seasonal climate forecast can be useful for planning, in this case the information provided was inaccurate; exceptional rainfall occurred in May, 2002 (table). This skill, coupled with the limited temporal and spatial specificity of the information provided, compromises the usefulness of long-range weather forecasts in the health sector.
Rainfall estimates for 2002 expressed as a proportion of monthly average (1995–2001)
|
|
April |
May |
June |
|---|---|---|---|
| District | |||
| Kisii Central | 7·0% | −7·3% | −38·6% |
| Gucha | 1·0% | 1·0% | −26·4% |
| Nandi | 4·5% | 37·0% | −40·5% |
| Kericho | −8·4% | 40·6% | −32·1% |
Satellite and meteorological station data are combined to provide on-line rainfall estimates (RFE) for Africa in near-real time at an 8×8 km spatial resolution (http://edcsnw4.cr.usgs.gov/adds/). We retrieved these data for the duration of the archive and extracted district total rainfall estimates for the four districts. In Kisii Central and Gucha, the estimates for the months of April and May were not very different from average (table), suggesting a resurgent outbreak of normal proportions. By contrast, Nandi and Kericho received over a third more rain than is usual in May (table), indicating suitable conditions for true epidemics. Details for all the districts in the western highlands can be found in the UNICEF report cited in the Acknowledgments section. No equivalent sources of public-domain temperature data are available.
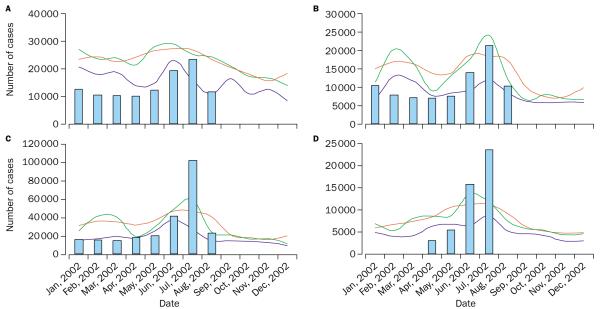
District Health Management Teams were visited in the four districts to collect information on malaria outpatients until the end of August, 2002, and for the preceding 5 years. We then used the WHO quartile, Cullen, and cumulative sum (C-SUM) epidemic detection techniques3 for objective quantification of the scale of the emergency. Resurgent outbreaks arose in Kisii Central and Gucha, compared with true epidemics in Nandi and Kericho (figure) in the months of June and July, as had been predicted on the basis of the rainfall estimates. The monthly temporal resolution of malaria outpatient reporting was not sufficient for the early detection of epidemics, since none of the techniques indicated unusual conditions in May. The routine health information and management systems were weak and did not provide timely information during the 2002 emergency.
Epidemic detection in Kisii Central (A), Gucha (B), Nandi (C), and Kericho (D).
In each graph, the blue bars represent the number of cases of malaria in 2002. If a bar exceeds the thin blue line the outbreak is a WHO defined epidemic, the green line a Cullen defined epidemic, and the red line a C-SUM defined epidemic3.
The highland populations are typical of those of the rest of Kenya, with poor access to, and use of, insecticide treated nets, emerging antimalarial drug resistance, supply of antimalarial products from the informal sector—which fail internationally acceptable quality assurance standards—poor case management, and inadequate prescription practices by formal health-service providers. The highlands of Kenya should, therefore, not be viewed as a distinct case, demanding great revisions to national policy. Increasing access to affordable, effective, preventative and curative strategies are as relevant in the highlands as they are in the more intense transmission areas of the country. We would, however, argue that emphasis should be given to improved planning cognisant of the seasonal epidemiology of risk, in view of the fact that every year about 25% of the annual case burden occurs in June and July. This planning should concentrate central, provincial, and particularly district level efforts at preparedness (indoor residual spraying, advocacy for the use of mosquito nets and re-treatment, community mobilisation and education, audits of drug stock, efficacy, and resistance, medical staff audits, retraining, etc) in the months of April and May before the predictable seasonal resurgence. Further considerations for the highlands might include modifications of national policies for malaria to allow for: proportionately more advocacy for indoor residual house spraying;4 routine suspension of cost sharing for malaria treatment in May, June, and July to encourage more prompt treatment of disease as a midway to mass drug administration, which has historically been shown to be very effective;5 the strict management of leave during the months of May, June, and July for key medical and administrative staff at the relevant districts, provinces, and central levels; and embracing the role of the media as an important component of the wider dissemination of public-health information through appointment of a press representative to assist in quality control of information reported.
Ironically, the national and international attention paid to the highland malaria emergency in western Kenya in 2002 ignored the fact that malaria is a leading cause of death in 65 of the 70 Kenyan administrative districts. In these districts those who die are generally voiceless, politically inert children. Although some aspects of MEWS are of potential benefit to the western highland districts, better utilisation of early warning potential within and beyond the highlands would help ensure equitable implementation of the national malaria control strategy in Kenya.
Acknowledgments
We thank Prof Sarah E Randolph and Prof David J Rogers for their comments. Funds were provided by UNICEF Kenya Country Office (Special Service Agreement 059—SSA/KENA/2002/00001290-0). The full report of this work, distributed to all relevant partners, can be requested for further details: Hay SI. The inter-sectoral response to the 2002 malaria outbreak in the highlands of western Kenya. Nairobi: UNICEF, Kenya Country Office (KCO), 2002. The opinions and assertions contained herein are private views of the authors and are not to be construed as official or as reflecting the views of UNICEF. SIH is supported as an Advanced Training Fellow by the Wellcome Trust (#056642) and affiliated to the Kenya Medical Research Institute/Wellcome Trust Collaborative Programme, PO Box 43640, Nairobi, Kenya. In respect of the term and conditions of this award, the consultancy for UNICEF was operated on an expenses only basis. RWS is a Senior Wellcome Trust Fellow (#058992) and acknowledges the support of the Kenya Medical Research Institute. This report is published with the permission of the director of the Kenyan Medical Research Institute (KEMRI). The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Footnotes
Conflict of interest statement None declared.
References
- 1.WHO . Malaria early warning systems, a framework for field research in Africa: concepts, indicators and partners. World Health Organization; Geneva: 2001. p. 80. [Google Scholar]
- 2.Nájera JA, Kouznetsov RL, Delacollete C. Malaria epidemics: detection and control, forecasting and prevention. World Health Organization; Geneva: 1998. p. 81. [Google Scholar]
- 3.Hay SI, Simba M, Busolo M, et al. Defining and detecting malaria epidemics in the highlands of Western Kenya. Emerg Infect Dis. 2002;8:555–62. doi: 10.3201/eid0806.010310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guyatt HL, Corlett SK, Robinson TP, Ochola SA, Snow RW. Malaria prevention in highland Kenya: indoor residual house-spraying vs. insecticide-treated bednets. Trop Med Int Health. 2002;7:298–303. doi: 10.1046/j.1365-3156.2002.00874.x. [DOI] [PubMed] [Google Scholar]
- 5.Roberts JMD. The control of epidemic malaria in the highlands of western Kenya, 3: after the campaign. J Trop Med Hyg. 1964;67:230–37. [PubMed] [Google Scholar]