Abstract
Context
Coronary revascularization is among the most common hospital-based major interventional procedures performed in the United States. It is uncertain how new revascularization technologies, new clinical evidence from trials, and updated clinical guidelines have influenced the volume and distribution of coronary revascularizations over the past decade.
Objective
To examine national time trends in the rates and types of coronary revascularizations during 2001–2008.
Design
Serial cross-sectional study with time trends.
Setting
U.S. hospitals in the Healthcare Cost and Utilization Project's Nationwide Inpatient Sample providing coronary revascularization, supplemented by Medicare hospital claims.
Patients and Interventions
Patients undergoing coronary artery bypass grafting (CABG) or percutaneous coronary interventions (PCI) from 2001–2008.
Main Outcome Measure
Annual procedure rates.
Results
There was a 14% decrease (p<0.001) in the annual rate of coronary revascularizations between 2001 and 2008. The annual CABG rate decreased steadily from 1,742 CABGs per million adults per year in 2001–02 to 1,081 CABGs per million adults per year in 2007–08 (p<0.001), but PCI rates did not significantly change, from 3,827 PCI per million adults per year in 2001–02 to 3,667 PCI per million adults per year in 2007–08 (p=0.74). Between 2001 and 2008 the number of hospitals in the Nationwide Inpatient Sample providing CABG increased by 14% (p=0.03), while the number of PCI hospitals increased by 35% (p<0.001). The median CABG caseload per hospital declined by 28% (p<0.001), and the percentage of CABG hospitals providing fewer than 100 CABGs per year increased from 11% to 26% (p<0.001).
Conclusions
In U.S. hospitals from 2001–2008, there was a substantial decrease in CABG utilization rates, but PCI utilization rates remained unchanged.
Coronary revascularization, comprising coronary artery bypass surgery (CABG) and percutaneous coronary intervention (PCI), is among the most common major medical procedures provided by the U.S. healthcare system, with over 1 million procedures performed annually.1 It is also among the most costly: Medicare inpatient payments to hospitals for coronary revascularizations exceeded $3.2 billion in fiscal year 2006,2 an amount larger than the reimbursement for any other medical or surgical procedure except for hip/knee replacement.
Several innovations in coronary revascularization, such as drug-eluting stents, minimally invasive CABG, and "off-pump" CABG, have been adopted widely in the past decade,3–5 with the promise of improved clinical outcomes compared to older revascularization technologies and techniques.5–7 In addition, publication of randomized controlled trial results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial (2007)8 and the Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX) trial (2009)9 have provided important new information about both the potential clinical value of revascularization compared to pharmacotherapy, as well as the outcomes of CABG compared to PCI in the drug-eluting stent era. In addition, during the past decade updated appropriateness criteria for coronary revascularization have been issued and/or revised by the major cardiovascular societies.10–14
During this period of technological innovation, new published evidence, and updated guidelines, it is not well known whether or how the volume of coronary revascularization and its constituent types changed in the United States. Substantial changes in the overall volume of revascularizations and/or the relative use of CABG versus PCI would have important ramifications on clinical outcomes, healthcare costs, and the future organization and delivery of hospital-based cardiovascular care. Therefore, the goal of this study was to use a representative national sample of hospitalization claims to estimate temporal trends in the annual volume of coronary revascularization procedures during 2001–2008.
METHODS
Study Data
The University of Pennsylvania's Institutional Review Board approved the study protocol. Data were obtained from the Agency for Healthcare Research and Quality's (AHRQ's) Healthcare Cost and Utilization Project-Nationwide Inpatient Sample (NIS) files from 2001 through 2008. The NIS datasets contain patient-level hospital discharge data provided by states that participate in AHRQ's Healthcare Cost and Utilization Project (n=42 in 2008). The NIS includes data from approximately 1,000 hospitals and is designed as a stratified, 20% representative sample of all non-federal U.S. hospitals.15 Criteria used for stratified sampling of hospitals into the NIS include hospital ownership, patient volume, teaching status, urban/rural location, and geographic region. Weighting the patient-level observations in the NIS datasets to account for the complex sampling scheme provides estimates for the entire U.S. population of hospitalized patients. Each record in the NIS includes all procedure and diagnosis codes recorded on each patient's hospital discharge abstract. As the NIS is derived from state-mandated hospital discharge reports, it includes all claims from each selected hospital regardless of payer or insurance status.
Identifying Coronary Revascularizations
Coronary revascularizations were identified on NIS claims by the appearance of procedure codes 36.01–36.07, 36.09, or 00.66 for PCI, or by codes 36.1× for CABG. A claim was classified as a drug-eluting stent (DES) if procedure code 36.07 appeared or if the claim was assigned to diagnosis-related group (DRG) 526–527 during 4/1/2003–9/30/2005, DRG 557–558 during 10/1/2005–9/30/2007, or DRG 246–247 after 10/1/2007. The claim was designated as a bare metal stent (BMS) if there was no DES coding and if procedure code 36.06 or codes 00.45–00.48 combined with 00.66 appeared, or if the DRG assignment was 116 during 1/1/2001–9/30/2001, 517 during 10/1/2001–9/30/2005, 555–556 during 10/1/2005–9/30/2007, or 248–249 after 10/1/2007. The claim was assigned as a non-stent coronary angioplasty if codes 00.66, 36.01–36.05, or 36.09 appeared and were unaccompanied by any code indicating a DES or BMS.
Calculation of Procedure Rates
The NIS was constructed as a 20% stratified random sample of U.S. hospitals. Accordingly, the population "at risk" for treatment at these hospitals was a 20% random sample of the U.S. population. Because our study excluded pediatric procedures, we calculated procedure rates as the number of CABG, DES, BMS, and non-stent coronary angioplasties reported in the NIS sample, weighted according to the NIS stratified sampling scheme,15 divided by 20% of the total number of U.S. adults during the same time periods. Estimates of the size of the U.S. adult population in each year 2001–2008 were obtained from the U.S. Census.16
Measuring Outpatient PCI
The NIS is assembled solely from hospital inpatient discharge data. While CABG is invariably an inpatient procedure, our prior work has determined that between 6–18% of PCI procedures were performed on outpatients, including low-risk elective procedures performed at hospitals in so-called "23-hour" stays.17 These outpatient PCI procedures would not be included in the NIS.18 For Medicare beneficiaries, however, outpatient procedure claims are available from the Centers for Medicare and Medicaid Services. We used these outpatient Medicare procedure claims to identify PCI by the appearance of Healthcare Common Procedure Coding System codes 92980, 92981, 92982, or 92984. Codes 92980–92981 on outpatient claims specifically indicated stent use, and the concurrent appearance of codes C1874, C1875, G0290, or G0291 further indicated use of a drug-eluting stent.
We estimated the ratio of outpatient to inpatient PCI claims, using a 100% national sample of Medicare claims, for beneficiaries ages 65 to 69 in each calendar quarter from 2001–2008 as a proxy measure for the national mean outpatient:inpatient PCI ratio. As prior reports of the demographics of PCI recipients indicate their mean age is in the mid 60's,3, 19, 20 the outpatient:inpatient PCI ratio of patients ages 65–69 would reasonably approximate the ratio for all PCI patients. Because the likelihood of obtaining outpatient PCI may be correlated with the type of PCI received, we separately calculated outpatient:inpatient ratios for DES, BMS, and non-stent angioplasty recipients. These outpatient:inpatient ratios derived from Medicare data then were multiplied by the quarterly inpatient PCI rates generated from NIS data to estimate the national outpatient PCI rate for each calendar quarter. Finally, the outpatient PCI rate was added to the inpatient PCI rate generated directly from the NIS to obtain the total PCI rate.
Validation of NIS Count Data
Because NIS hospitals were not designed specifically to represent the national provision of cardiovascular hospital services, it is possible that national rate estimates using the NIS may not perfectly approximate the rates in the full population of U.S. coronary revascularization hospitals. Therefore, to assess the level of agreement between the NIS and national claims data, we compared CABG and PCI quarterly national count estimates from NIS for Medicare beneficiaries over age 65 to the counts of CABG and PCI claims obtained from a 100% sample of Medicare inpatient claims for 2001–2008.
Differences in Revascularization Patients and Hospitals Between 2001 and 2008
To assess for differences between revascularization patients in 2001 compared to revascularization patients in 2008, we compared age, gender, and geographic distributions between CABG recipients in 2001 versus 2008, as well as PCI recipients in 2001 versus 2008. Because race is unreported for many hospitals in NIS data, we separately calculated the 2001–2008 difference in race percentages among CABG and PCI recipients using Medicare claims for CABG or PCI from 2001 and 2008. After excluding hospitals reporting fewer than 5 coronary revascularizations per year, we then examined changes over time in the number and case-volume of the hospitals performing CABG or PCI between 2001 and 2008.
Statistical Analyses
Trends in the annual rates of CABG and PCI were assessed using negative binomial regressions with procedure count as the dependent variable, and calendar quarter as the key independent variable, with the size of the population at risk as an offset term. Characteristics of patients undergoing CABG or PCI in 2001 versus 2008 were compared with chi-square tests, except age, which was compared with a t-test. Characteristics of hospitals providing CABG or PCI were compared using chi-square tests for categorical variables and the Wilcoxon rank-sum test for differences in hospital caseloads. All statistical analyses were performed using SAS 9.2 (Cary, NC) or STATA 11.1 (College Station, TX). All statistical tests were two-sided, with p<0.05 indicating statistical significance.
RESULTS
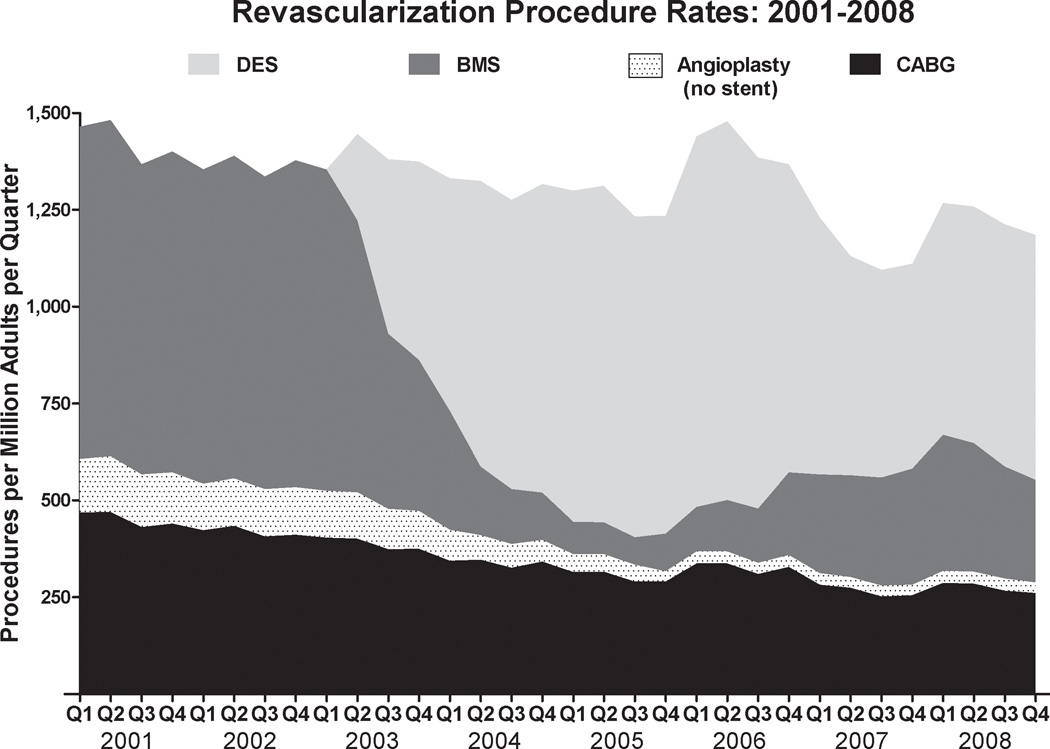
For each year between 2001 and 2008 the NIS dataset included all-payer inpatient discharge data from n=212 (2001) to n=241 (2008) hospitals per year that provided CABG and from n=246 (2001) to n=331 (2008) hospitals per year that provided PCI. Medicare PCI claims from patients ages 65–69 indicated outpatient PCI became more prevalent over time, rising from 7.5% (2001) to 17% (2008) of all PCI. The annual U.S. rate of coronary revascularizations declined by 14% (p<0.001) from 5,710 procedures per million adults in 2001 to 4,916 procedures per million adults per year in 2008 (Table 1). There was a 39% decrease (p<0.001) in the annual CABG rate between 2001 and 2008, with the CABG rate declining steadily throughout the 8-year period (Figure 1) from 1,808 per million adults in 2001 to 1,098 per million adults in 2008. However, the PCI rate changed minimally from 3,903 per million adults in 2001 to 3,818 per million adults in 2008, a 2% decrease (p=0.74). Projected to the entire U.S. population, these rate changes implied that 130,000 fewer CABGs were performed in 2008 compared to 2001, while the 2001–2008 decline in the total number of U.S. coronary revascularizations was 80,000 (7%) from a 2001 total volume of 1.21 million revascularizations.
Table 1.
Annual Rates of Coronary Revascularization Proceduresa
| Revascularization Procedure | Years | Trend p-valueb | |||
|---|---|---|---|---|---|
| 2001–02c (n=42.7) |
2003–04 (n=43.6) |
2005–06 (n=44.6) |
2007–08 (n=45.6) |
||
| Coronary artery bypass grafting | 1,742 (31) | 1,457 (27) | 1,261 (24) | 1,081 (23) | <0.001 |
| Percutaneous coronary interventions | 3,827 (69) | 3,873 (73) | 4,101 (76) | 3,667 (77) | 0.74 |
| Bare metal stents | 3,326 (60) | 1,557 (29) | 463 (9) | 1,167 (25) | <0.001 |
| Drug-eluting stents | - - | 2,040 (38) | 3,507 (65) | 2,383 (50) | N/Ad |
| Angioplasty (no stent) | 501 (9) | 276 (5) | 126 (2) | 117 (2) | <0.001 |
| TOTAL | 5,569 (100) | 5,330 (100) | 5,362 (100) | 4,748 (100) | <0.001 |
Data are average annual n procedures per million adults during the two-year period. Data in parentheses indicate the percentages of total revascularizations in the two-year period. Percentages may not add to 100, or to the subgroup total, due to rounding.
Trends tested with negative binomial regressions on quarterly count data from 2001–2008 reported in the 20% Nationwide Inpatient Sample, offset by catchment population size.
N indicates millions of adult patients at risk for inclusion in the NIS. The NIS is designed to represent the hospital services provided to a random 20% of the U.S. population. As this study excluded pediatric procedures, the NIS "at risk" population was therefore a 20% random sample of U.S. adults. Population size estimates for this sample were obtained from U.S. Census interim reports.16
There was a rising trend in DES rate from 2003–2006 (p=0.001), and a declining trend in DES rate from 2006–2008 (p=0.003).
Abbreviations: NIS—Nationwide Inpatient Sample; DES—drug-eluting stent.
Figure 1.
Area plot indicating the quarterly procedure rate (y-axis) of CABG (black area), BMS (dark gray area), non-stent angioplasty (dotted area), and DES (light gray area) from 2001–2008. The x-axis indicates time in calendar quarters. Abbreviations: CABG—coronary artery bypass grafting; BMS—bare metal stents; DES—drug-eluting stents.
Subgroup Analyses and Temporal Changes in Patient and Hospital Characteristics
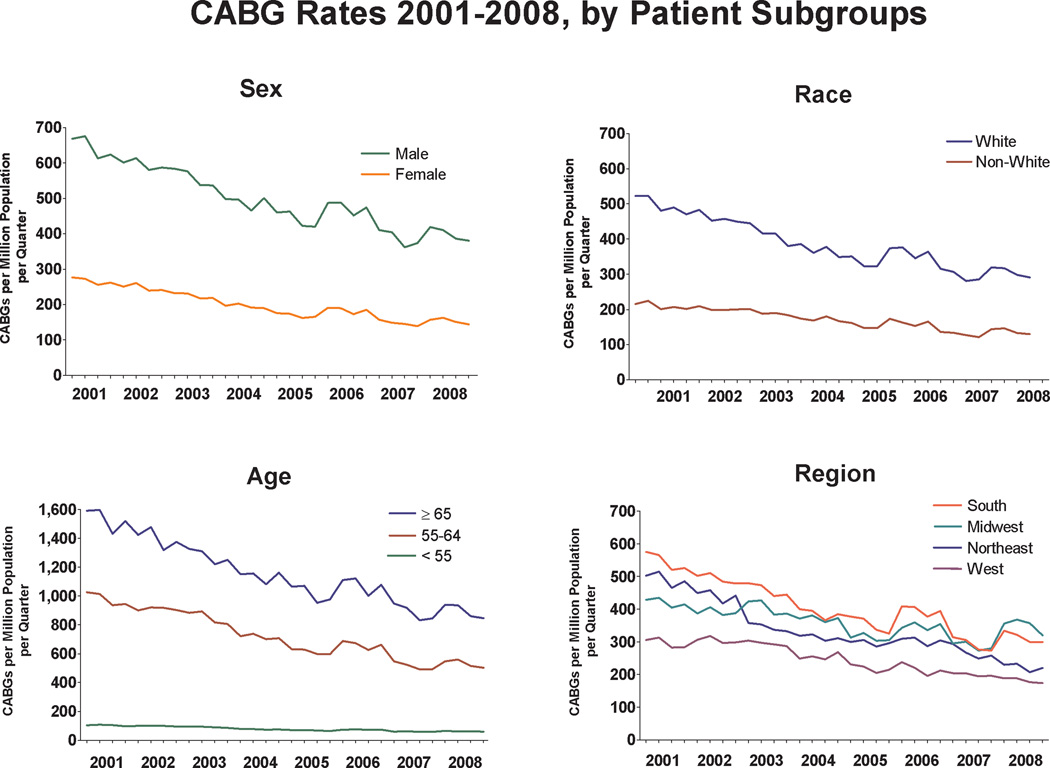
Statistically significant declines in CABG rates between 2001 and 2008 were observed across gender, age, racial, and regional subgroups (Figure 2). Comparison of the demographics of CABG recipients and PCI recipients between 2001 and 2008 revealed slight differences in age, gender, racial, and geographic distributions over time (Table 2). Fourteen percent more hospitals provided CABG in 2008 than in 2001 (p=0.03), and there was a 35% increase (p<0.001) between 2001 and 2008 in the number of PCI hospitals. The increase in the number of CABG hospitals combined with the decrease in national CABG rates resulted in a 28% decline in the median caseload per hospital (p<0.001) and a substantial increase in the number of hospitals that provided fewer than 100 CABGs per year (11% to 26%, p<0.001).
Figure 2.
Plots indicating the change in CABG rate from 2001–2008, by subgroups of CABG recipients (i.e., sex in upper left panel, race in upper right panel, age in lower left panel, U.S. Census region in lower right panel). The y-axes indicate quarterly procedure volumes. The x-axes indicate time in calendar quarters. Abbreviation: CABG—coronary artery bypass grafting.
Table 2.
Characteristics of U.S. Coronary Artery Bypass Grafting and Percutaneous Coronary Intervention Patients and Hospitals in 2001 and 2008a
| Characteristic | CABG | p-value | PCI | p-value | ||
|---|---|---|---|---|---|---|
| 2001 (n=77,952) |
2008 (n=53,483) |
2001 (n=151,893) |
2008 (n=153,800) |
|||
| Patient Characteristics | ||||||
| Female | 30.2 | 29.5 | <0.001 | 34.7 | 33.9 | 0.04 |
| Age, mean (SD) | 66 (10) | 66 (10) | 0.64 | 65 (12) | 65 (12) | 0.94 |
| Age groups | ||||||
| < 55 | 16 | 16 | <0.001 | 23 | 22 | 0.001 |
| 55–64 | 25 | 28 | 25 | 27 | ||
| 65–74 | 34 | 32 | 28 | 27 | ||
| ≥ 75 | 25 | 25 | 24 | 24 | ||
| Non-white raceb | 8 | 10 | <0.001 | 9 | 11 | <0.001 |
| United States Census region | ||||||
| Northwest | 21 | 15 | 0.01 | 20 | 18 | 0.68 |
| Midwest | 21 | 28 | 23 | 27 | ||
| South | 43 | 42 | 42 | 39 | ||
| West | 15 | 15 | 15 | 16 | ||
| Hospital Characteristics | ||||||
| Hospitals in Nationwide Inpatient Sample providing procedure, actual n | 212 | 241 | 0.03 | 246 | 331 | <0.001 |
| Estimated total number of U.S. hospitals providing procedurec, projected n | 1,059 | 1,188 | NA | 1,223 | 1,637 | NA |
| Procedure volume per year, median (IQR) | 253 (161, 458) | 183 (98, 292) | <0.001 | 446 (191, 777) | 318 (140, 631) | 0.001 |
| Procedure volume per year, by volume category, % of all hospitals providing procedure | ||||||
| 5–49d | 5 | 10 | <0.001 | 9 | 9 | 0.008 |
| 50–99 | 6 | 16 | 6 | 10 | ||
| 100–249 | 39 | 44 | 17 | 23 | ||
| 250–499 | 30 | 23 | 23 | 27 | ||
| ≥ 500 | 21 | 7 | 44 | 31 | ||
Data are percentages unless otherwise indicated. Percentages may not sum to 100 due to rounding.
Race identification was absent for a sizeable fraction of Nationwide Inpatient Sample data, thus race percentages are reported from Medicare beneficiaries over age 65 who underwent CABG or PCI in 2001 and 2008.
Nationwide Inpatient Sample weighted estimate.
Categories are ranges of procedure caseload per year.
Abbreviations: CABG—coronary artery bypass grafting; PCI—percutaneous coronary intervention; SD—standard deviation; NA—not applicable; IQR—interquartile range.
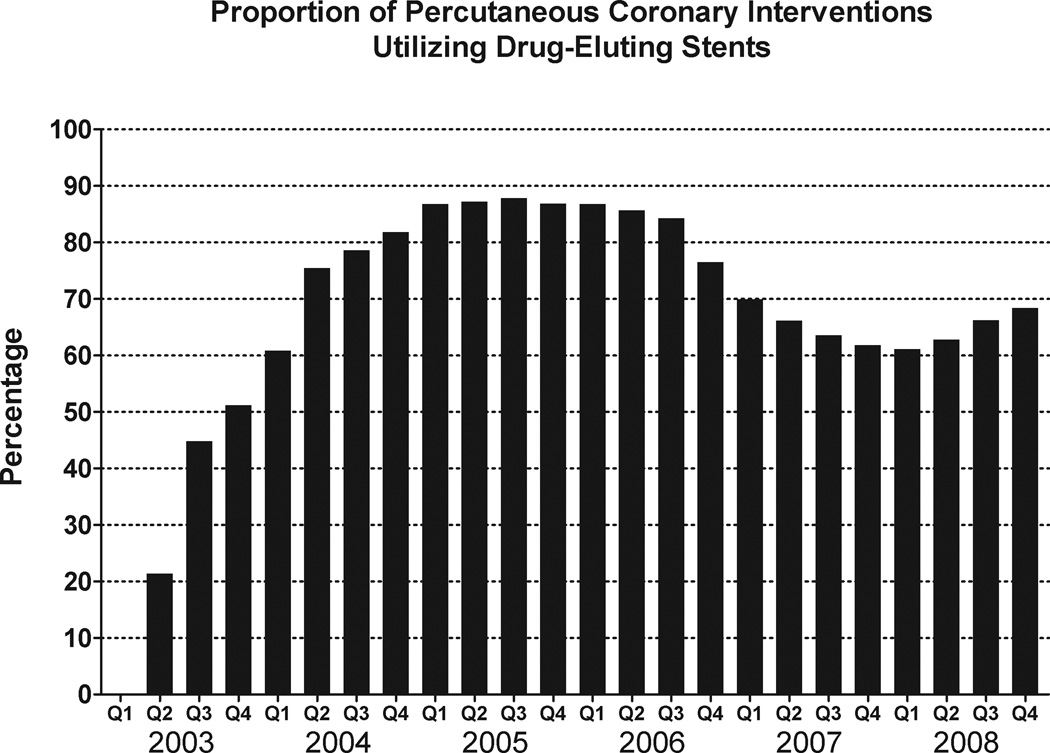
DES Percentage of PCI: 2001–2008
Drug eluting-stents were approved by the U.S. Food and Drug Administration in April, 2003. By the third quarter of 2005 the use of DES as a percentage of all PCI procedures peaked at nearly 90% (Figure 3). Percentage use of DES subsequently declined during 2006–2007 to 61% of all PCI procedures in the first quarter of 2008, followed by a sustained increase in DES use through the end of 2008. Data from the final calendar quarter in 2008 indicated DES were used in approximately 68% of PCI procedures.
Figure 3.
Bar chart indicating the percentage of all percutaneous coronary interventions that involved use of drug-eluting coronary stents between the first quarter of 2003 (FDA approval of drug-eluting stents occurred in April, 2003) and the last quarter of 2008. The y-axis indicates the percentage of all PCI procedures that involved a drug-eluting stent, and the x-axis indicates time in calendar quarters.
Validation of NIS Estimates with Medicare Claims Data
Comparisons of the counts of CABG and PCI estimated by NIS among Medicare beneficiaries over age 65 compared very closely to the actual counts of CABG and PCI claims submitted to Medicare between 2001 and 2008 (Technical Appendix). Quarterly CABG counts differed by a mean value of <1% (range: −14% to 13%), and quarterly PCI counts differed by a mean of <1% (range: −9% to 9%), between these two data sources. Medicare claims revealed similar trends in CABG and PCI rates from 2001 to 2008 as were observed in the NIS. Further analysis of Medicare PCI claims, which unlike NIS data include patient identifiers, also revealed that the percentage of all PCI procedures that were repeat PCIs (i.e., PCI performed within 365 days of a prior PCI) declined slightly from 16.1% (2001) to 12.9% (2008) (p=0.003 for trend).
COMMENT
We found that although there was only a modest decline in the annual rate of coronary revascularizations in the United States from 2001 to 2008, there was a substantial decrease in the rate of CABG surgery, with approximately 1/3rd fewer CABGs being performed in 2008 compared to 2001. This decline in CABG rate occurred as a roughly linear trend throughout the 8-year period. Hence, the data do not suggest that the decline was triggered by any single event occurring during the past decade, such as the introduction of competing technologies, advances in CABG surgical techniques, publication of clinical trials, or issuance of clinical guidelines. During the same eight-year period there was an increase in the number of U.S. hospitals providing CABG, thus there was a substantial decline in the median hospital CABG case volume and a marked increase in the number of U.S. hospitals with relatively low (i.e., less than 100 cases per year) annual CABG case volume.
Clinical Implications of the Decline in CABG Rate
While it is possible that the decline in CABG rate was entirely unrelated to PCI utilization, and while it cannot be known with certainty whether physicians were increasingly substituting PCI for CABG during the past decade for the treatment of coronary artery disease, our findings suggest the possibility that several thousand patients who underwent PCI in 2008 would have undergone CABG had patterns of care not changed markedly between 2001 and 2008. Our data imply a sizeable shift in cardiovascular clinical practice patterns away from surgical treatment toward percutaneous, catheter-based interventions. However, the results of the recent SYNTAX trial indicated CABG remains the better choice for coronary revascularization among patients with previously untreated three-vessel or left main coronary artery disease,9 even in the drug-eluting stent era. The clinical indications for CABG validated by the SYNTAX trial are virtually identical to the class IA indications for CABG published by the American College of Cardiology/American Heart Association in 1999,11 indicating stability in the published evidence supporting CABG use. The declining CABG rate during this period of stable evidence and guidelines implies either overuse of CABG in 2001 that has been progressively corrected by better patient selection, or increasing underuse of CABG between 2001 and 2008 as patients who would have been optimally treated with CABG were instead treated with PCI.
There are other published data suggesting CABG use decreased over time for treatment of coronary artery disease.12 Gogo et al. examined 2002–2005 data from 365 U.S. hospitals participating in an American College of Cardiology/American Heart Association Guidelines Quality Improvement Initiative and found that CABG was used in only 40% of 3-vessel-disease patients in late 2005 compared to nearly 50% in early 2002.19 Similarly, Frutkin et al. examined PCI indications from the National Cardiovascular Data Registry and determined that after the introduction of drug-eluting stents in 2003, increasing numbers of patients with class I clinical indications for CABG underwent PCI.21 Our results extend these findings by demonstrating that the trend in declining CABG rates was occurring in a broadly representative sample cohort of U.S. hospitals providing CABG, was persistent across 8 years, and resulted in a marked reduction in the rate of CABG procedures performed at the end of the decade compared to the beginning.
Potential Explanations for the Decline in CABG Rates
Because our data could not distinguish which revascularization patients were more appropriate candidates for CABG versus PCI, and because the data could not identify patients in later years who would have undergone CABG in prior years, it was not possible to measure the characteristics of the patients whose care was "shifted" toward PCI between 2001 and 2008. It is possible that this group included many patients with less compelling clinical indications for CABG over PCI, such as 2-vessel or non-left-main single-vessel coronary artery disease. It is also possible that the shift involved patients who were at very high risk for adverse perioperative outcomes from cardiac surgery, although it is unlikely that large numbers of such patients would have undergone CABG in 2001, as alternative treatments were available. Increasing use of primary PCI for the emergent treatment of acute myocardial infarction during 2001–2008 may have obviated the need for additional coronary revascularization and thus decreased the CABG rate. However, our observations combined with those of prior investigators strongly suggest that a sizeable fraction of patients who did not undergo CABG in 2007–2008 might have been appropriate CABG recipients.
Hospital Volume of CABG Surgery
The decline in the national case volume of CABG was accompanied by an increase in the number of U.S. hospitals providing CABG. The combination of these phenomena implies that over time, greater numbers of patients were obtaining CABG at hospitals with low volumes of CABG. While there is controversy in the literature on whether low-volume providers inherently have worse CABG outcomes,22, 23 our findings highlight the increasing role of low-volume hospitals in the provision of coronary artery bypass surgery.
Variation in Drug-Eluting Stent Use
Changes in PCI market share between DES and BMS have been previously reported among selected subsets of U.S. hospitals,3, 21, 24 and they possibly reflect a high level of clinician enthusiasm for DES in the years immediately following FDA approval, followed by a "cooling off" period after publication of data suggesting DES safety concerns (i.e., late in-stent thrombosis),25, 26 as well as increasing clinician awareness of the imperative for DES patients' adherence to long-duration anti-platelet therapy following DES implantation.27 Our results extend these prior findings to a national sample of hospitals and provide further evidence that PCI practice patterns involving the choice of DES or BMS were highly volatile in the years following DES approval. An important implication of this volatility is that thousands of patients may have received DES during the peak years (2004–2005) who would have instead received BMS in 2007–2008. Whether these patients were appropriately treated with DES instead of BMS during these years of high enthusiasm for DES is uncertain.
Stable PCI rates during 2001–2008 were unanticipated, as clinical trials consistently have reported that DES reduces a recipient's likelihood of repeat target vessel revascularization due to lower rates of subsequent restenosis.6, 7 Furthermore, our analysis of Medicare claims indicated the rate of repeat revascularization did in fact decline during the DES era, thus an overall decline in PCI rates subsequent to the introduction of DES would have been unsurprising. However, the stability of the PCI rate, combined with our findings from Medicare claims of declining rates of repeat PCI, suggests that there are increasing numbers of patients receiving PCI over time. PCI recipients in 2008 possibly included patients who would have been treated with CABG, not PCI, if the coronary revascularization practice patterns of 2001 had not subsequently changed.
Limitations
Our national estimates for CABG and PCI rates were derived from a 20% sample of U.S. hospitals, with the sample designed to approximate the national distribution of key hospital characteristics including location, ownership, volume, and academic status. Although the NIS sampling design is statistically sound, and the NIS has been used extensively in prior research to estimate national health care trends, it is possible that coronary revascularization or its subtypes were either over-represented or under-represented by the sample. However, the count of CABGs and PCI procedures among NIS patients who were Medicare beneficiaries closely approximated the volume of procedures indicated by 100% Medicare claims data. This agreement between independent data sources increases our confidence that the NIS accurately represented national rates of coronary revascularization procedures.
It is also possible that our method of estimating percentages of outpatient PCI was inaccurate, because this ratio was derived solely from a subset of Medicare beneficiaries ages 65–69 rather than from all patients undergoing PCI. However, as the mean age of U.S. patients undergoing PCI is approximately 64 years,28 it is likely that the national ratio of outpatient:inpatient PCI among all patients approximates the ratio observed among patients ages 65–69. Also, as outpatient PCI remains relatively infrequent, a systematic bias in our estimate of the outpatient PCI fraction would not have changed our findings substantially.
The NIS does not include detailed information about patient clinical characteristics, such as coronary anatomy, angina class, ejection fraction, medications, surgical risk, or smoking status, which could explain changes over time in utilization of CABG or PCI. Furthermore, the absence of these variables complicates comparisons of revascularization practices across hospitals, thus a detailed exploration of the drivers of the time trends we observed is beyond the scope of our study. Finally, the NIS does not report coronary revascularizations occurring in federal hospitals, such as those operated by the Department of Veterans Affairs, the Department of Defense, or the Indian Health Service. While these hospitals represent only a small fraction of the national health care system29 and thus exclusion of their procedures is unlikely to affect our primary findings, it is likewise unknown whether the trends we observed are applicable to patients in federal health care systems.
Summary
Although the total rate of U.S. coronary revascularization decreased modestly during 2001–2008, there was a substantial decline in the CABG rate. Conversely, despite the potential for drug-eluting stents to reduce the need for subsequent coronary revascularization procedures, during 2001–2008 the rate of PCI did not significantly decrease.
Supplementary Material
Acknowledgment
The authors gratefully acknowledge the contributions of Gina Pugliano, MA (research assistant, University of Pennsylvania School of Medicine) in the production of this manuscript. Dr. Groeneveld had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The study's sponsors had no role in the analysis of the data or in the writing or approval of the manuscript.
Research support: This research was supported by the National Heart, Lung, and Blood Institute (1R01HL086919) and by the Agency for Healthcare Research and Quality (1R01HS018403). This project was also funded, in part, under a grant from the Pennsylvania Department of Health, which specifically disclaims responsibility for any analyses, interpretations, or conclusions.
Footnotes
None of the authors had any personal or financial conflicts of interest in regard to this study.
REFERENCES
- 1.DeFrances CJ, Lucas CA, Vuie VC, Golosinskiy A. 2006 National Hospital Discharge Survey. Hyattsville, MD: National Center for Health Statistics; 2008. [PubMed] [Google Scholar]
- 2.Centers for Medicare and Medicaid Services; [Accessed February 24, 2010]. Inpatient Hospital Payment Information for Value-Driven Health Care. Available at: http://www.cms.hhs.gov/HealthCareConInit/02_Hospital.asp. [Google Scholar]
- 3.Roe MT, Chen AY, Cannon CP, et al. Temporal changes in the use of drug-eluting stents for patients with non-ST-Segment-elevation myocardial infarction undergoing percutaneous coronary intervention from 2006 to 2008: results from the can rapid risk stratification of unstable angina patients suppress ADverse outcomes with early implementation of the ACC/AHA guidelines (CRUSADE) and acute coronary treatment and intervention outcomes network-get with the guidelines (ACTION-GWTG) registries. Circ Cardiovasc Qual Outcomes. 2009;2(5):414–420. doi: 10.1161/CIRCOUTCOMES.109.850248. [DOI] [PubMed] [Google Scholar]
- 4.Hernandez AF, Li S, Dokholyan RS, O'Brien SM, Ferguson TB, Peterson ED. Variation in perioperative vasoactive therapy in cardiovascular surgical care: data from the Society of Thoracic Surgeons. Am Heart J. 2009;158(1):47–52. doi: 10.1016/j.ahj.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 5.Li Z, Yeo KK, Parker JP, Mahendra G, Young JN, Amsterdam EA. Off-pump coronary artery bypass graft surgery in California, 2003 to 2005. Am Heart J. 2008;156(6):1095–1102. doi: 10.1016/j.ahj.2008.07.020. [DOI] [PubMed] [Google Scholar]
- 6.Moses JW, Leon MB, Popma JJ, et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med. 2003;349(14):1315–1323. doi: 10.1056/NEJMoa035071. [DOI] [PubMed] [Google Scholar]
- 7.Stone GW, Ellis SG, Cox DA, et al. A polymer-based, paclitaxel-eluting stent in patients with coronary artery disease. N Engl J Med. 2004;350(3):221–231. doi: 10.1056/NEJMoa032441. [DOI] [PubMed] [Google Scholar]
- 8.Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356(15):1503–1516. doi: 10.1056/NEJMoa070829. [DOI] [PubMed] [Google Scholar]
- 9.Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961–972. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 10.Eagle KA, Guyton RA, Davidoff R, et al. ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery) J Am Coll Cardiol. 2004;44(5):e213–e310. doi: 10.1016/j.jacc.2004.07.021. [DOI] [PubMed] [Google Scholar]
- 11.Eagle KA, Guyton RA, Davidoff R, et al. ACC/AHA Guidelines for Coronary Artery Bypass Graft Surgery: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1991 Guidelines for Coronary Artery Bypass Graft Surgery). American College of Cardiology/American Heart Association. J Am Coll Cardiol. 1999;34(4):1262–1347. doi: 10.1016/s0735-1097(99)00389-7. [DOI] [PubMed] [Google Scholar]
- 12.Patel MR, Dehmer GJ, Hirshfeld JW, Smith PK, Spertus JA. ACCF/SCAI/STS/AATS/AHA/ASNC 2009 Appropriateness Criteria for Coronary Revascularization: a report by the American College of Cardiology Foundation Appropriateness Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, and the American Society of Nuclear Cardiology Endorsed by the American Society of Echocardiography, the Heart Failure Society of America, and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2009;53(6):530–553. doi: 10.1016/j.jacc.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Smith SC, Jr, Dove JT, Jacobs AK, et al. ACC/AHA guidelines of percutaneous coronary interventions (revision of the 1993 PTCA guidelines)--executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (committee to revise the 1993 guidelines for percutaneous transluminal coronary angioplasty) J Am Coll Cardiol. 2001;37(8):2215–2239. doi: 10.1016/s0735-1097(01)01344-4. [DOI] [PubMed] [Google Scholar]
- 14.Smith SC, Jr, Feldman TE, Hirshfeld JW, Jr, et al. ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention-Summary Article: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention) J Am Coll Cardiol. 2006;47(1):216–235. doi: 10.1016/j.jacc.2005.11.025. [DOI] [PubMed] [Google Scholar]
- 15.Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality; 2008. [Accessed March 8, 2010]. Introduction to the Nationwide Inpatient Sample (NIS) Available at: http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_2008_INTRODUCTION.pdf. [Google Scholar]
- 16.U.S. Census Bureau - Population Division. Annual estimates of the resident population by sex and selected age groups for the United States: April 1, 2000 to July 1, 2009 (NC-EST2009-02) [Accessed March 2, 2011]; Available at: http://www.census.gov/popest/national/asrh/NC-EST2009-sa.html.
- 17.Cohen MM, Wreford M, Barnes M, Voight P. Re-engineering surgical services in a community teaching hospital. Cost Qual Q J. 1997;3(2):48–57. [PubMed] [Google Scholar]
- 18.Groeneveld PW, Matta MA, Greenhut AP, Yang F. Drug-eluting compared with bare-metal coronary stents among elderly patients. J Am Coll Cardiol. 2008;51(21):2017–2024. doi: 10.1016/j.jacc.2008.01.057. [DOI] [PubMed] [Google Scholar]
- 19.Gogo PB, Jr, Dauerman HL, Mulgund J, et al. Changes in patterns of coronary revascularization strategies for patients with acute coronary syndromes (from the CRUSADE Quality Improvement Initiative) Am J Cardiol. 2007;99(9):1222–1226. doi: 10.1016/j.amjcard.2006.12.037. [DOI] [PubMed] [Google Scholar]
- 20.Dunlay SM, Rihal CS, Sundt TM, Gerber Y, Roger VL. Current trends in coronary revascularization. Curr Treat Options Cardiovasc Med. 2009;11(1):61–70. doi: 10.1007/s11936-009-0007-7. [DOI] [PubMed] [Google Scholar]
- 21.Frutkin AD, Lindsey JB, Mehta SK, et al. Drug-eluting stents and the use of percutaneous coronary intervention among patients with class I indications for coronary artery bypass surgery undergoing index revascularization: analysis from the NCDR (National Cardiovascular Data Registry) JACC Cardiovasc Interv. 2009;2(7):614–621. doi: 10.1016/j.jcin.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 22.Rathore SS, Epstein AJ, Volpp KG, Krumholz HM. Hospital coronary artery bypass graft surgery volume and patient mortality, 1998–2000. Ann Surg. 2004;239(1):110–117. doi: 10.1097/01.sla.0000103066.22732.b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vaughan-Sarrazin MS, Hannan EL, Gormley CJ, Rosenthal GE. Mortality in Medicare beneficiaries following coronary artery bypass graft surgery in states with and without certificate of need regulation. JAMA. 2002;288(15):1859–1866. doi: 10.1001/jama.288.15.1859. [DOI] [PubMed] [Google Scholar]
- 24.Krone RJ, Rao SV, Dai D, et al. Acceptance, panic, and partial recovery the pattern of usage of drug-eluting stents after introduction in the U.S. JACC Cardiovasc Interv. 2010;3(9):902–910. doi: 10.1016/j.jcin.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 25.Daemen J, Wenaweser P, Tsuchida K, et al. Early and late coronary stent thrombosis of sirolimus-eluting and paclitaxel-eluting stents in routine clinical practice: data from a large two-institutional cohort study. Lancet. 2007;369(9562):667–678. doi: 10.1016/S0140-6736(07)60314-6. [DOI] [PubMed] [Google Scholar]
- 26.Shuchman M. Trading restenosis for thrombosis? New questions about drug-eluting stents. N Engl J Med. 2006;355(19):1949–1952. doi: 10.1056/NEJMp068234. [DOI] [PubMed] [Google Scholar]
- 27.Eisenstein EL, Anstrom KJ, Kong DF, et al. Clopidogrel use and long-term clinical outcomes after drug-eluting stent implantation. JAMA. 2007;297(2):159–168. doi: 10.1001/jama.297.2.joc60179. [DOI] [PubMed] [Google Scholar]
- 28.Anderson HV, Shaw RE, Brindis RG, et al. A contemporary overview of percutaneous coronary interventions. The American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR) J Am Coll Cardiol. 2002;39(7):1096–1103. doi: 10.1016/s0735-1097(02)01733-3. [DOI] [PubMed] [Google Scholar]
- 29.Harrison JP, Coppola MN, Wakefield M. Efficiency of federal hospitals in the United States. J Med Syst. 2004;28(5):411–422. doi: 10.1023/b:joms.0000041168.28200.8c. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.