Abstract
Purpose
This study investigated HIV testing and risk behaviors in a longitudinal sample of young men who have sex with men (YMSM).
Design
Data come from the Healthy Young Men's (HYM) study, comprising five waves of non-experimental survey data collection every six months between February 2005 and January 2008.
Setting
Participants were recruited from public venues in Los Angeles County in which YMSM spend time.
Subjects
526 participants (24% African American, 37% Caucasian, 39% Latino; mean age = 20.14 years, range = 18 to 24 years) were enrolled. Retention was 93%.
Measures
Testing recency was assessed with a four-point ordinal scale. HIV-risk behaviors were operationalized as binary measures of unprotected anal intercourse (UAI) with multiple partners or partners with unknown or discordant serostatus, club drug use, and illicit drug use over the prior three months.
Analysis
Correlations, Cochran's Q tests, and repeated measures ANOVA were performed in SPSS. Analyses included all data available at each wave.
Results
No significant correlations emerged between testing recency and sex risk at any wave. Repeated measures ANOVA showed significant positive, linear change in HIV testing recency over time, but no significant changes emerged for sex risk or drug use.
Conclusion
Although participation in testing increased, there was no corresponding change in HIV-risk behavior. Initiatives may need to target risk behavior separately and specifically in order to reduce these behaviors among YMSM.
Keywords: HIV; Risk Behavior; Homosexuality, Male; Los Angeles
PURPOSE
HIV prevention remains a critical concern for health care service providers. In Los Angeles County alone, between 56,500 and 62,200 people are estimated to be living with HIV or AIDS, with an additional 2,000 infections occurring every year.1 Males represent over 85% of HIV infections in Los Angeles County, with exposure coming overwhelmingly from men who have sex with men (MSM; 79%).1
In response, recent funding has targeted prevention efforts related to HIV counseling and testing (HCT), including rapid HIV testing. Efforts have been particularly pronounced following a Centers for Disease Control and Prevention (CDC) investment in rapid testing in non-clinical settings such as bars, night clubs, and mobile vans.2 A focus on HCT serves to identify HIV-positive individuals, to connect seropositive individuals with care, and to educate and counsel seronegative individuals so they may remain HIV-negative. However, testing history and risk behaviors may not directly correspond: some studies find no relationship between testing and HIV risk,3,4 whereas others find that frequent testing is associated with higher HIV risk.5–6 Very few studies have investigated both HIV testing and risk behaviors specifically among young MSM (YMSM), and no research has focused on longitudinal changes in testing rates despite YMSM's continued high risk for contracting HIV. In a longitudinal study, we sought to ascertain the association, if any, between HIV testing and HIV-risk behaviors among a diverse cohort of YMSM in Los Angeles.
METHODS
Design
This research is a part of the Healthy Young Men's (HYM) study, which utilized quantitative and qualitative methods to explore the individual, familial, interpersonal, and community factors that may influence drug use, sexual risk, and mental health.7 This longitudinal study followed an ethnically diverse cohort of YMSM every six months between February 2005 and January 2008, culminating in five waves of data. At each wave, a survey was administered in both English and Spanish using computer-assisted interview (CAI) technologies that incorporated sound files, allowing the respondent to silently read questions on the computer screen and/or listen to the questions read through headphones and enter their responses directly into the computer. The survey required 1 to 1 1/2 hours to complete, and participants received $35 compensation for their time and effort. Additionally, participants received compensation for contact between waves, including $5 for each monthly check-in and $20 for updating their contact information. Incentives for monthly contact and updating contact information were provided at the participant's next scheduled interview. This research received approval from the Committee on Clinical Investigations at Children's Hospital Los Angeles.
Sample
Five hundred twenty-six subjects were recruited into the study between February of 2005 and January of 2006. Young men were eligible to participate in the study if they were: a) 18 to 24 years old; b) self-identified as gay, bisexual, or uncertain about their sexual orientation and/or reported having had sex with a man; c) a resident of Los Angeles County and anticipated living in this area for at least six months; and d) self-identified as Caucasian, African American, or Latino of Mexican descent. Using a stratified probability sampling design, participants were recruited from 36 different public venues that had previously been identified as settings in which YMSM spend time and/or “hang out”, including bars/clubs (50%); Pride festivals (14%); special events/private parties (14%); social service agencies (11%) and high-traffic street locations (11%). The survey was administered at a location convenient to the participant, at either the project office or a public venue that provided Internet connectivity. Before administering the survey, the interviewer reviewed the purpose of the study and the participation requirements and obtained the respondent's written informed consent. Retention in the study was 93% from the first to the last wave.1
Measures
In addition to collecting demographic information such as age and ethnicity, we investigated HIV testing recency, HIV status, and three binary indicators of HIV risk at each wave: sex risk, use of any club drug, and use of any illicit drug. Testing recency was assessed with a four-point ordinal scale (never tested, tested greater than one year ago, tested between six months and one year ago, and tested within the past six months). HIV status was self-reported as positive, negative, or unknown. Sex risk was characterized as engaging in any unprotected anal intercourse (UAI) with a partner whose HIV status was serodiscordant or unknown or engaging in UAI with multiple partners over the prior three months. Club drug use included prior three months use of ecstasy, cocaine, crystal/methamphetamine, poppers, GHB, Ketamine, and other forms of speed. Illicit drug use included prior three months use of any club drug(s) as well as crack, LSD, PCP, heroin, mushrooms, and prescription drugs without a physician's order.
Analysis
We first considered cross-sectional correlations between demographic variables, testing recency, and HIV-risk indicators. Next, we conducted a repeated measures analysis of variance (ANOVA) on the HIV testing recency measure and Cochran's Q tests on the binary risk measures to ascertain the presence or absence of quantifiable change in these variables over time. All analyses were performed in SPSS and included all participants present at each wave, regardless of their participation in other waves.
RESULTS
At baseline, the sample was 24% African American, 37% Caucasian, and 39% Latino of Mexican descent; their mean age was 20.1 years (range 18 to 24 years); 50% had been tested for HIV recently (within the past 6 months); 3% were HIV-positive; 24% had engaged in high-risk sex in the past three months; and 28% had used illicit drugs in the past three months.2 Descriptive statistics for the study sample at each wave are presented in Table 1. In waves 1 and 2, age was correlated with testing recency (wave 1: r = .10, p = .03; wave 2: r = .11, p = .02), indicating that older participants were more likely to have been tested recently than younger participants. However, no age effects were found in subsequent waves. In wave 2 only, there was a significant correlation between illicit drug use and testing recency (r = .10, p = .03). There were no significant correlations between any demographic variable or HIV-risk outcome and testing recency in waves 3, 4, or 5, and in particular, there were no significant correlations at any time point between testing recency and sex risk.
Table 1.
Descriptive statistics.
| Variable | Categories | Wave 1 N (%) | Wave 2 N (%) | Wave 3 N (%) | Wave 4 N (%) | Wave 5 N (%) |
|---|---|---|---|---|---|---|
| Sample size | Number of participants | 526 | 499 | 483 | 482 | 487 |
| Age | Mean (SD) | 20.1 (1.6) | 20.7 (1.7) | 21.2 (1.6) | 21.7 (1.7) | 22.2 (1.6) |
| Ethnicity | African American | 126 (24) | 115 (23) | 115 (24) | 115 (24) | 115 (24) |
| Latino of Mexican descent | 205 (39) | 196 (39) | 192 (40) | 191 (40) | 195 (40) | |
| Caucasian | 195 (37) | 188 (38) | 176 (36) | 176 (37) | 177 (36) | |
| HIV testing group (among sexually active respondents only) | Tested within past 6 months | 168 (32) | 188 (36) | 215 (41) | 220 (42) | 223 (47) |
| Tested 6 months to 1 year ago | 97 (18) | 109 (21) | 88 (17) | 123 (23) | 151 (32) | |
| Tested more than 1 year ago | 100 (19) | 92 (17) | 105 (20) | 77 (15) | 70 (15) | |
| Never been tested | 127 (24) | 83 (16) | 55 (10) | 39 (7) | 30 (6) | |
| HIV status | Positive | 15 (3) | 17 (3) | 18 (4) | 18 (4) | 17 (3) |
| Negative | 420 (80) | 412 (83) | 395 (82) | 411 (85) | 417 (86) | |
| Don't know | 90 (17) | 69 (14) | 69 (14) | 49 (10) | 49 (10) | |
| Refused to answer | 1 (0) | 1 (0) | 1 (0) | 4 (1) | 4 (1) | |
| High sex risk | Single UAI serodiscordant / multiple partners | 125 (24) | 140 (27) | 139 (26) | 115 (22) | 121 (23) |
| Illicit drug use | Past 3 months | 148 (28) | 148 (30) | 152 (31) | 132 (27) | 136 (28) |
| Club drug use | Past 3 months | 117 (22) | 117 (23) | 120 (25) | 108 (22) | 110 (23) |
A repeated measures analysis of variance showed evidence of significant overall change in HIV testing recency over time (multivariate F(4, 1608) = 31.14, p < .001), including a positive linear trend in testing recency over time (linear F(1, 402) = 79.47, p < .001). To illustrate, Figure 1 compares the percentage of participants in each HIV testing group to the percentage of participants who engaged in sex risk at each wave. Membership in the two most-recent testing groups (participants who tested within the past six months and those who tested between six months and one year ago) showed a marked increase over the course of the study, and the two least-recent testing groups (participants who last tested over a year ago and those who never tested) showed a corresponding decrease. However, the proportion of study participants engaging in sex risk remains flat at roughly a quarter of the sample per wave (Q(4) = 6.65, p = .16). Results are similar for both types of drug use, neither of which demonstrated significant change across the five waves of data collection (club drug use: Q(4) = 2.15, p = .22; illicit drug use: Q(4) = 5.70, p = .71). This provides converging evidence that in our sample, although recent HIV testing increased over time, it was consistently unrelated to HIV risk.
Figure 1.
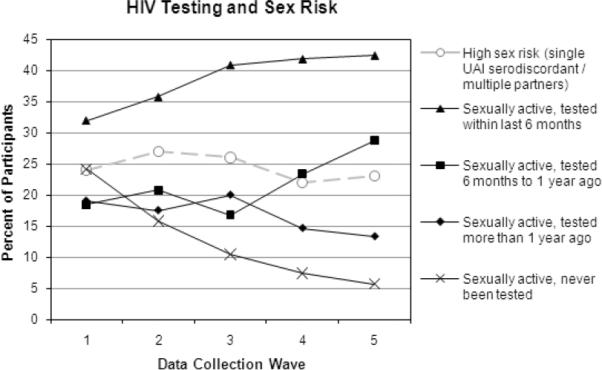
HIV testing and sex risk.
DISCUSSION
Summary
Results suggest that innovations in technology (e.g., rapid testing) and more accessible and targeted HCT services in Los Angeles County have been successful. By wave 5, 47% of sexually active participants had tested within the past 6 months and 79% had tested within the past year. Furthermore, the percentage of participants who reported never having tested for HIV dropped from 24% at the first wave to only 6% by the last wave. However, despite the marked increase in HIV testing, there was no corresponding change in HIV-risk behavior as measured by sexual risk or drug use. The testing message, though successful in its own right, does not appear to influence HIV-risk behaviors.
Limitations
Our chief limitation is that our principal finding – the relationship between HIV testing and risk – is a null result. With α = .05, power = .80, and n = 499 (the smallest sample size available, from wave 2), post-hoc sensitivity analyses confirmed that our study had adequate power to detect effect sizes as small as .125 for a two-tailed test, and thus we are confident the null results reflect a genuine lack of correspondence between testing and risk behaviors over time. Nonetheless, we are elucidating the absence of an effect in a hypothesis testing framework designed to test the presence of one, and the null results may simply be an artifact of low sample size. A secondary limitation is the inability to link HIV testing to HIV seropositivity. Although we did capture self-reported HIV serostatus, we did not conduct HIV testing with our sample, and self-reported seropositivity was so infrequent as to preclude statistical analysis. Self-reports may underestimate actual seropositivity for a number of reasons in this group of young men, including fear of disclosure and not being certain of diagnosis. Third, we are limited by data that required a binary operationalization of drug use. Although we measured multiple types and frequencies of drug use, only approximately 30% of our sample had used illicit drugs within the past three months at any given wave. This relatively low rate precluded investigation of effects based on different types of drugs used or frequency of use. Finally, our sample reflects the behavior of YMSM residing in Los Angeles County, a diverse, large urban area that receives substantial funding for HIV prevention. Studies conducted in dissimilar regions or targeting different populations may yield alternate patterns of testing and risk behavior.
Significance
In line with previous research on at-risk MSM,3,4 results from our study did not support an association between HIV testing and significant reductions in HIV-risk behavior. Our results suggest that HCT alone may not be sufficient to reduce risk, and risk behavior may need to be targeted separately and specifically in order to promote behavioral change. Our findings reinforce the need for funding agencies to support alternate HIV-prevention efforts such as behavioral-change interventions along with HCT, as findings from our studies and others suggest that complex psychosocial processes underlie the adoption of risk behaviors.8–10 If the same energy and innovation supporting HCT is brought to individual- or group-level interventions, we may hope for similar success in reducing risk behaviors.
Acknowledgments
Support for the original research was provided by a grant from the National Institute on Drug Abuse of the National Institutes of Health (R01 DA015638-03).
Footnotes
Participants who remained in the study did not significantly differ in their baseline sexual risk, recency of HIV testing, illicit drug use, or club drug use compared to participants who did not continue after the first wave of data collection.
Participants' risk behaviors did not differ as a function of ethnicity or sexual identity. Therefore, all results presented are based on the entire sample for each wave.
REFERENCES
- 1.LA County Public Health Office of AIDS Programs and Policy [Accessed December 25, 2008];Prevention plan 2009–2013. Available at: http://www.lapublichealth.org/aids/PPC/Prevention%20Plan%2009/Chapter2SanFernandoValley.pdf.
- 2.Centers for Disease Control and Prevention [Accessed December 30, 2008];Advancing HIV prevention: New strategies for a changing epidemic. Available at http://www.cdc.gov/hiv/resources/reports/hiv3rddecade/chapter5.htm.
- 3.Dodge B, Jeffries WL, 4th, Sandfort TG. Beyond the down low: sexual risk, protection, and disclosure among at-risk Black men who have sex with both men and women (MSMW) Arch Sex Behav. 2008;37:683–696. doi: 10.1007/s10508-008-9356-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sumartojo E, Lyles C, Choi K, et al. Prevalence and correlates of HIV testing in a multi-site sample of young men who have sex with men. AIDS Care. 2008;20:1–14. doi: 10.1080/09540120701450425. [DOI] [PubMed] [Google Scholar]
- 5.MacKellar DA, Valleroy LA, Secura GM, et al. Repeat HIV testing, risk behaviors, and HIV seroconversion among young men who have sex with men: a call to monitor and improve the practice of prevention. J Acquir Immune Defic Syndr. 2002;29:76–85. doi: 10.1097/00042560-200201010-00011. [DOI] [PubMed] [Google Scholar]
- 6.Sifakis F, Hylton JB, Flynn C, et al. Prevalence of HIV infection and prior HIV testing among young men who have sex with men: The Baltimore Young Men's Survey. AIDS Behav. 2007 Oct 30; doi: 10.1007/s10461-007-9317-5. [DOI] [PubMed] [Google Scholar]
- 7.Kipke MD, Kubicek K, Weiss G, et al. The health and health behaviors of young men who have sex with men. J Adolescent Health. 2007;40:342–350. doi: 10.1016/j.jadohealth.2006.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kipke MD, Weiss G, Wong CF. Residential status as a risk factor for drug use and HIV risk among young men who have sex with men. AIDS Behav. 2007;11(6 Suppl):56–69. doi: 10.1007/s10461-006-9204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong CF, McDavitt B, Weiss G, Kipke MD. Emotion regulation as predictors of depression and HIV-risk behaviors among YMSM. Adolescence. In press. [Google Scholar]
- 10.Harper GW. Sex isn't that simple: culture and context in HIV prevention interventions for gay and bisexual male adolescents. Am Psychol. 2007;62:803–819. doi: 10.1037/0003-066X.62.8.806. [DOI] [PubMed] [Google Scholar]


