Abstract
Background
Despite the potential importance of nutrition to pregnancy outcomes, little is known about the factors influencing dietary quality, especially during the first trimester.
Objective
To examine the relationships among distress (an index of depression and stress), social support, and eating habits with dietary quality in low-income pregnant women.
Method
A cross-sectional design and path analytic methods was used in a clinic-based sample of low-income women (n = 118) in their first trimester of pregnancy. Women completed questionnaires and received training on estimating food portion sizes. Three 24-hour dietary recalls were collected over 2 weeks. Overall dietary quality was assessed using the Dietary Quality Index: Pregnancy.
Results
The final path model fit well (CFI = .97; RMSEA = .05) and revealed that distress had a direct effect on poor eating habits (β = .36), and a direct (β = −.23) and indirect effect on dietary quality (β = −.30). Poor eating habits had a direct effect on dietary quality (β = −.18). Social support had no effect on dietary quality. Age had significant direct effects on education (β = .39) and nutritional knowledge (β = .18) and an indirect effect on dietary quality (total effect, β = .19). Maternal age, education, and nutritional knowledge did not have significant effects on psychosocial variables.
Discussion
Psychosocial distress and poor eating habits contributed to inadequate dietary quality. Assessing for depression, stress, poor eating habits, and overall dietary quality during the crucial first trimester may identify women needing more intensive dietary monitoring and intervention throughout pregnancy.
A pregnant woman’s dietary quality, particularly in the first trimester of pregnancy, has a profound effect on subsequent pregnancy outcomes (Kind, Moore, & Davies, 2006). Emerging evidence strongly suggests that inadequate dietary quality during this critical period of fetal development may lead to reprogramming of the fetal phenotype, resulting in permanent physiological changes and predisposing the child to coronary heart disease, altered insulin metabolism, obesity, and hypertension as an adult (Barker, 1995, 1999; Godfrey & Barker, 2000; McMillen, Muhlhausler, Duffield, & Yuen, 2004). Data from the Dutch Famine Study signaled the critical nature of maternal nutrition in pregnancy (Susser & Stein, 1994) on the child’s subsequent health; infants who were exposed to maternal undernutrition in the first trimester had low birth weights (LBWs) and subsequently developed childhood obesity (Huang, Lee, & Lu, 2007) and cardiovascular disease (Painter, Roseboom, & Bleker, 2005). In addition, inadequate dietary quality in early pregnancy predisposes women to pre-eclampsia (Hofmeyer, Atallah, & Duley, 2006) and can affect infant birth weight at delivery adversely regardless of gestational weight gain or maternal nutritional status in the second and third trimesters of pregnancy (Baschat & Hecher, 2004).
Dietary quality is an integrative assessment of nutritional intake that is compared to the recommendations for pregnancy established by the United States Department of Agriculture and the Institute of Medicine (IOM; 2005). Initial assessment of low-income women’s dietary quality during pregnancy often occurs during their first prenatal visit to an obstetrical practitioner, opening a window of opportunity to modify women’s dietary quality that could enhance maternal and fetal outcomes. Dietary quality is a valuable measure of nutritional status (Bodnar & Siega-Riz, 2002), providing a summary measure of multiple dimensions of nutrient intake (i.e., protein intake, percent of energy from fats, and amount of folate and calcium). Each of these dimensions of nutrient intake are independently associated with one or more key sources of maternal and infant morbidity and mortality (Bhatia, 2005).
Women in low-income households are more likely to eat poor diets than their wealthier counterparts due in part to an inadequate understanding of nutritional requirements and limited ability to purchase healthy foods (Bhargava, 2004), predisposing them to delivering a LBW infant. However, little research has been used to assess low-income women’s dietary quality during pregnancy (Watts, Rockett, Baer, Leppert, & Colditz, 2007), particularly in the first trimester when the developing fetus is particularly susceptible to alterations in maternal nutrition. Examining the factors that support or inhibit dietary quality during the first trimester in low-income women, a population at substantial risk for perinatal complications, is an important but oftentimes neglected area of research.
Factors Affecting Dietary Quality
This study was based on a model derived from the literature describing the influence of unchangeable maternal contextual and potentially modifiable psychobehavioral factors on dietary quality during pregnancy. Variables of interest to this study are discussed below.
Contextual factors
The relationships among maternal age, educational level, and dietary quality during pregnancy is unclear. While older women in Europe were noted to have lower fat intake (healthier intake; Freisling, Elmadfa, & Gall, 2006) and consumed more fruits and vegetables than younger women (Groth, Fagt, & Brondsted, 2001), little is known about the influence of maternal age on dietary quality specifically during pregnancy. Similarly, years of education were related significantly to dietary quality in older White and African American adults (Raffensperger et al., 2011). One study of 1,777 pregnant women in the US reported better dietary quality in older and more educated women (Rifas-Shiman, Rich-Edwards, Kleinman, Oken, & Gillman, 2009); however, two-thirds of the women in this sample were older (> 25 years old), Caucasian, and college graduates. Little is known about the influence of maternal age and years of education on dietary quality in early pregnancy in low-income pregnant women and warrants exploration.
Psychobehavioral Factors
Stress and depression may diminish a woman’s ability to cope with barriers to healthy eating resulting in poor dietary quality (Arnow, Kenardy, & Agras, 1995). Low-income women may experience stress resulting from inadequate financial resources; emotional and financial demands of an impending pregnancy; and concern regarding a response to the pregnancy from their partner, friends, and other family members, which could influence their dietary intake. Hurley et al. (2005) reported that stressed pregnant women were more likely to consume energy-dense, nutrient-poor foods, thus decreasing their dietary quality during pregnancy. Additionally, Borders, Grobam, Amsden, and Holl (2007) reported that chronic stress experienced by low-income mothers was associated with low infant birth weight.
Also, prenatal depression may intensify the negative effect of maternal stress on dietary quality, resulting in a heightened sense of distress, and has been linked to inadequate intake of some crucial nutrients, such as essential fatty acids (Sontrop, Avison, Evers, Speechley, & Campbell, 2008). Although little is known about the specific relationship between depression and overall dietary quality during pregnancy, depression in pregnancy is associated with an inadequate [OR = 1.36, 95% CI (1.0, 1.90)] and excessive [OR = 1.12, 95% CI (1.0, 1.1)] gestational weight gain (Webb, Seiga-Riz, & Dole, 2009), as well as the degree of nausea and vomiting and fatigue (r = .32, p < .001; Chou, Lin, Cooney, Walker, & Riggs, 2003). Dietary quality was not assessed in these women. The relationship between stress and depression, and their combined effect on dietary quality in the first trimester of pregnancy, need further examination.
Social support from partners, family, and friends is associated with improved dietary quality in diverse populations (Larson, Story, Wall, & Neumark-Sztainer, 2006; Watters, Satia, & Galanko, 2007). Fowles, Hendricks, and Walker (2005) found that low-income women with more social support ate healthier meals during the first trimester of pregnancy than those without support. Emotional support from husbands and female relatives was found to be important for maintaining a healthy diet during pregnancy in Latina women (Thorton et al., 2006). Low-income women with support from a partner consumed more vegetables but less grains than women with less partner support (Fowles, Murphey, & Ruiz, 2010). These findings support the need to further study the influence of social support in enabling some women to eat balanced meals during the critical first trimester of pregnancy.
Eating habits, characterized for this study as the frequency and location of meals and snacks contributes to overall dietary quality. An eating habit of consuming small, frequent meals is associated with a lower risk of obesity, whereas eating habits characterized by skipping breakfast and eating breakfast, lunch, or dinner away from home more often were associated with an increase in obesity (Ma et al., 2003). Fowles and Gabrielson (2005) reported that changes in eating habits in the first trimester of pregnancy, specifically not skipping meals and reducing intake of junk foods, contributed to improved overall dietary quality. Poor eating habits can have a negative effect on pregnancy outcomes. Women who do not follow the IOM guidelinesof eating “small to moderate-sized meals at regular intervals, and eat(ing) nutritious snacks” (IOM, 1992, p. 45) had lower overall caloric intake (Siega-Riz, Evenson, & Dole, 2004), but a higher risk for preterm delivery (Siega-Riz, Herrmann, Savitz, & Thorp, 2001). Also, prolonged periods without food (i.e., 13 hours or more) during pregnancy are associated with elevated maternal levels of corticotrophin-releasing hormone and preterm delivery (Siega-Riz, Herrmann, Savitz, & Thorp, 2001); the frequency of meals and snacks is an important component of dietary quality in pregnancy.
Nutritional knowledge about nutrient values of foods and basic nutrition principles in the first trimester of pregnancy can influence dietary intake. Fowles and Gabrielson (2005) noted that low-income women had more accurate knowledge of the recommended number of servings of several food groups (e.g., fruits and vegetables, meats, dairy) and more accurate actual intake of meats and milk servings than did their more affluent counterparts. This difference could be due, in part, to differences in their obstetrical care providers. Fowles (2002) noted that low-income women reported frequent nutritional assessment and education received from their midwife, while affluent women who received prenatal care from a private obstetrician reported that their dietary intake was not assessed after the first prenatal visit (Fowles, 2002). Recently, pregnant women had an improved dietary intake of fruits and vegetables; decreased intake of sugary foods, high fat, and fried meats; and less fast food consumption after receiving nutritional knowledge and counseling via an interactive video format (Jackson, Stotland, Caughey, & Gerbert, 2011), supporting the importance of nutritional knowledge on quality of dietary intake.
Examining contextual and psychobehavioral factors that may support or diminish dietary quality during the first trimester in low-income women, a population at substantial risk for perinatal complications, is an important but neglected area of research that could guide the development of effective interventions and lead to improved perinatal outcomes in this vulnerable population. Further understanding of the dynamics of maternal contextual factors (age and educational level), stress, depression, social support, eating habits, and nutritional knowledge in relation to dietary quality in the first trimester of pregnancy is best achieved by testing a model of these relationships using path analysis (Figure 1). The purpose of this study was to develop a path model that shows the relationships among distress (an index of stress and depression), social support, nutritional knowledge, and eating habits with dietary quality during the first trimester of pregnancy in low-income women.
Figure 1. Theoretical Model.
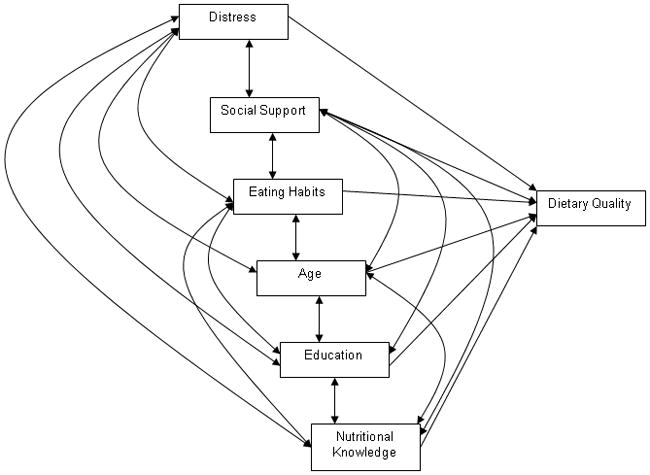
Full Theoretical Path Model
Method
A cross-sectional design was used to assess predictors of dietary quality in a convenience sample of low-income pregnant women. Women were included if they: (a) were underinsured or uninsured as determined by the recruitment facilities in the central Texas area, (b) were at least 16 years of age, (c) were able to read and speak English or Spanish, (d) had received confirmation of pregnancy, and (e) were in the first trimester of pregnancy (≤14 weeks from last menstrual date). Women were excluded if they were experiencing a pre-existing health condition, such as Type I or II diabetes, hypertensive disorders, cancer, heart disease, renal disease, a diagnosed eating disorder, milk or gluten allergies, or other conditions requiring special diets. From July 2009 to August 2010, 134 women were recruited into the study.
Sample size was determined using a power analysis for a broader study using regression analysis and based on parameters recommended by Nunnally and Bernstein (1994; i.e., 10 subjects per predictor variable). There were 11 predictor variables (contextual and modifiable) in the model for the broader study, which suggests a sample size of 110 women. Allowing for a potential 20% attrition rate, an initial sample of 134 women was recruited. Three women miscarried during data collection, nine were lost to contact, and four were removed from data analysis due to significant outliers on essential variables, for a final sample size of 118.
Procedures
Prior to data collection, the study was reviewed and approved by the full Institutional Review Board of the sponsoring university. Women were recruited at four area clinics that offer free or low-cost pregnancy testing to low-income women. If the pregnancy test was positive, agency staff distributed a flyer to briefly explain the purpose of the study. Women interested in learning more about the study provided contact information on the recruitment form and placed the form in a sealed box in the agency. Two members of the research team retrieved the recruitment forms and contacted all the women by phone using a standard script to explain the study purpose in more detail, screen for eligibility, and schedule interested and eligible women to go to the data collection site. Initial data collection was then completed at a Family Wellness Clinic located in central Texas and operated by the sponsoring School of Nursing. Women ages 18 years and over completed written informed consent prior to study procedures. For participants 16 and 17 years of age, parental consent was obtained prior to the data collection appointment and signed child assent was completed during the visit. After obtaining informed consent for each participant, women completed a demographic form, the Eating Habits Scale, the Nutritional Knowledge Scale, the Edinburgh Postnatal Depression Scale, and the Prenatal Psychosocial Profile–Assessment of Support and Stress Evaluation subscales. Women also had their height and weight measured on a stadiometer (SECA 703, Hamburg, Germany). They were trained on portion estimation using the Food Amount Booklet followed by a 24-hour dietary recall using the Nutrition Data System for Research (NDSR) created by the Nutrition Coordinating Center at the University of Minnesota. Over the next 2 weeks, two additional nonconsecutive dietary recalls were conducted via telephone; during one of these, foods eaten on a weekend day were reviewed. Three unannounced 24-hour dietary recalls, which include one weekend day, is considered representative of usual intake (Willett, 1998). As a motivational benefit of the study, once data collection was complete, each participant received feedback comparing recommendations provided by MyPyramid.gov to her average dietary intake along with individualized suggestions for meeting the recommendations. Women also received financial compensation for their time and participation in the study. They received a total of $105 for their participation, $55 at the time of the initial visit ($50 for their time and $5 to offset travel costs) and $25 gift cards (mailed after each of the subsequent 24-hour dietary recalls, which took about 20–30 minutes).
Instruments
Outcome measure
Reflecting the nutritional recommendations outlined in the U.S. Food Guide Pyramid (MyPyramid.gov) and IOM (2005) guidelines for pregnancy, dietary quality was measured using the Dietary Quality Index–Pregnancy (DQI-P; Bodnar & Siega-Riz, 2002). This scale consists of eight components: percent of recommended intake for grains, vegetables, and fruits; percent of recommended intake for folate, iron, and calcium; percent of energy from fat; and meal and snack pattern. Each component has a score range from 0 to 10 with a total score (sum of all eight components) between 0 and 80. A component is scored 10 if the participant meets the minimum number of ounces or cups recommended for that food group or scored a 0 if no food from that group is consumed. Intermediate scores (0 to 9) are calculated proportionately; for example, a woman who consumes 1 cup of fruit instead of the recommended 2 cups is given a score of 5 for that food group component. Similarly, a score of 10 each is given if the woman’s intake of folate, iron, and calcium met the IOM requirements (600 ug/day, 27 mg/day, and 1,000 mg/day, respectively) during pregnancy and 0 if none were ingested. Intermediate scores also are calculated proportionately. The scoring for meal and snack patterns follows the developers’ guidelines: 3 meals and 2 snacks = 10; 3 meals and 0–1 snack or 2 meals and 2 snacks = 5; 2 meals and 0–1 snack or 1 meal or snack = 0 (Bodnar & Siega-Riz, 2002). The most desirable overall dietary quality is reflected by a total score of ≥70 (Bodnar & Siega-Riz, 2002).
The data needed to compute dietary quality was derived from the three dietary recalls collected and analyzed using the NDSR software (version 2009). Members of the research team were trained on using this program (it utilizes the Multiple Pass method, developed by the U.S. Department of Agriculture) to obtain more complete intake amounts (Moshfegh et al., 2001; Willett, 1998). The NDSR includes data on 18,000 foods (including ethnic and regional foods) and 8,000 brand name products; these data are analyzed into 160 nutrients, 9 food groups, food constituents, nutrient ratios, and indices (e.g., glycemic index).
Explanatory measures
A demographic form was used to collect data on maternal age and educational level. Maternal education was assessed by asking participants to provide the number of completed years of school and was considered a continuous variable for data analysis.
Eating habits were measured with the Eating Habits subscale from the Project EAT Survey (Neumark-Sztainer, Story, Hannan, Perry, & Irving, 2002). Though developed for a study of teen obesity, the items in this subscale are particularly useful in observing low-income pregnant women (personal communication, Dr. Neumark-Sztainer, March 2006). In this scale, the number of meals (breakfast, lunch, and dinner) skipped during the previous week and location of dinner are broken down into 9 items, along with the frequency of eating at fast-food restaurants, grocery shopping, snacking, and eating salty snack foods. For example, an item related to skipping a meal was “During the past week, how many days did you eat lunch?” with response options of never (score of 5), 1–2 days (4), 3–4 days (3), 5–67 days (2), every day (1). Frequency of eating at fast food restaurants was assessed using the item “In the past week, how often did you eat something from a fast food restaurant (like McDonald’s, Burger King, Jack in the Box, etc.)?” with response options of never (score of 1), 1–2 times (2), 3–4 times (3), 5–6 times (4), 7 or more times (5). All items were scored on a scale of 1 to 5 and summed; a higher score indicated less desirable eating habits. Because this tool is used to assess individual behaviors, which are assumed not to co-vary, measuring internal consistency is inappropriate (Munro, 2004).
The Nutritional Knowledge Questionnaire (Sherman, Alexander, Clark, Dean, & Welter, 1992) was used to measure a woman’s nutrition knowledge with questions about nutrient values of foods (i.e., calories, fats, and vitamins) and basic nutritional principles. This instrument was tested originally in a population of low-income Mexican American and White women in south Texas. A sample item is: “Which is the healthiest breakfast?” and response options are: (a) an Egg McMuffin and whole milk; (b) A doughnut, lowfat milk, and orange juice; (c) Cheerios, lowfat milk, orange juice, and a scrambled egg (correct answer); and (d) Two scrambled eggs, bacon, and orange juice. Another example question is: “Sweet potato, pumpkin, spinach, broccoli, carrots, apricots, cantaloupe, mangos, and papaya are ALL good sources of which vitamin?” with response options of: (a) Vitamin A (correct answer); (b) Vitamin B; (c) Vitamin C; and (d) Vitamin D. With permission, several items were reworded to delete references to children’s diets; for example, the question “A well-balanced meal for a child consists of…” was changed to “A well-balanced meal consists of…”. A total of 19 questions are marked either as correct or incorrect with a correct answer earning a score of one and incorrect answers earning zero for a total summated score of correct answers ranging from 0 to 19. Kuder-Richardson-20 measure of internal consistency was .70 in this study.
Depression was measured using the Edinburgh Postnatal Depression Scale (EPDS; Cox, Holden, & Sagovsky, 1987). Ten items are scored from 0 to 3, increasing in value based on the severity of the symptom. A cutoff score of ≥10 will be used to identify a possible depression. The Agency for Healthcare Research and Quality (2005) recommends using the EPDS or the Postpartum Depression Screening Scale to screen for depression during the prenatal period. Cronbach’s alpha coefficient of internal consistency in this study was .84.
The Prenatal Psychosocial Profile–Stress subscale (Curry, Burton, & Fields, 1998) was used to evaluate stress. Eleven items used to evaluate financial worries; friends; recent moves and/or losses; work difficulties; drug and/or alcohol use; current pregnancy; overall feelings of being overwhelmed; and current sexual, emotional, and/or physical abuse were scored from 1 to 4 (higher scores indicate higher levels of stress). Convergent validity, internal consistency reliabilities, and test-retest reliabilities of .70 have been reported (Curry, Campbell, & Christian, 1994). Cronbach’s alpha for the 11-item stress subscale was .67.
Support from partners, from others (family, friends, etc.), or both was measured using the Prenatal Psychosocial Profile–Support subscale (Curry et al., 1998). The social support subscale contains 11 items to assess partner support and 11 items to measure support from others. Women responded to either questions about support from partner, support from others or both. Each statement was rated on a scale of ‘very dissatisfied’ to ‘very satisfied’, with scores of 1 to 6 being given, respectively. Cronbach’s alpha for partner support was .96 and .94 for support from others.
An index of social support was created to evaluate the influence of overall social support experienced by the women equitably. Most participants responded to questions related to both support from a partner and support from others (n = 100), while 9 women responded only to questions related to support from a partner and 9 responded only to questions related to support from others. The Social Support Index was computed by using the ‘z score’ for raw score responses for partner support for women who only answered these questions or support from others for women who only evaluated the support they received from others. The average of the ‘z scores’ was used if women responded to questions for both sources of support. This index was used in subsequent data analysis.
Data analysis
Data analysis was conducted using SPSS (version 17). Descriptive statistics were used to summarize sample characteristics. All variables were examined and appeared to be distributed normally. Pearson product-moment coefficients were calculated for correlations. Only those contextual (age and education) and psychosocial variables with a significant relationship with dietary quality were used in further analysis. Pregnant body mass index was not related to dietary quality, and dietary quality did not differ between women who were partnered or single, so these contextual variables were not incorporated into the prediction analysis. Since standardized scores were used for social support, z-scores were computed for all psychosocial variables and were used in all analyses.
Although no evidence of multicollinearity among independent variables was noted (i.e., a variance inflation factor greater than 10; Myers, 1990), a strong positive relationship was noted between stress and depression (r = .52). Furthermore, stress and depression each had a significantly negative relationship with dietary quality (r = −.22 and 0.32, respectively). Therefore, an index of distress was calculated to diminish the influence of large standard errors among these variables (Tabachnick & Fidell, 2001). The index of distress was computed by adding the z-scores for individual scores on measures of stress and depression, and was used in regression and path analysis. Path analysis was conducted using the AMOS function within SPSS to identify direct, indirect, and total effects of predictor variables on dietary quality.
Results
The women were, on average, 25 years old, had completed high school, and 8.75 weeks pregnant at the time of initial data collection procedures (Table 1). Most were unmarried, uninsured or insured through Medicaid, and Hispanic. Scores on the Edinburgh Postnatal Depression Scale indicated that 38% of the participants had possible depression (score > 10); 82% had inadequate dietary quality (score < 60 on DQI-P; Table 2).
Table 1.
Sample Characteristics
| Variable
|
Mean
|
SD |
Minimum
|
Maximum
|
|---|---|---|---|---|
| Age | 25.30 | 5.34 | 16.00 | 40.00 |
| Pre-pregnant BMI | 26.65 | 7.11 | 16.40 | 54.60 |
| Gestational age (weeks) | 8.87 | 2.22 | 4.57 | 13.43 |
| n | % | ||
|---|---|---|---|
| Race | Anglo | 45 | 38.1 |
| African-American | 15 | 12.7 | |
| Hispanic | 55 | 46.6 | |
| Other | 3 | 2.5 | |
|
| |||
| Marital Status | Married | 30 | 25.4 |
| Single | 88 | 74.6 | |
|
| |||
| Socioeconomic Status | Minor Professional | 20 | 16.9 |
| Clerical/Sales/Skilled | |||
| Workers | 42 | 35.6 | |
| Semi-skilled Workers | 40 | 33.9 | |
| Unskilled/Service | |||
| Workers | 16 | 13.6 | |
|
| |||
| Body Mass Index | Underweight | 9 | 7.6 |
| Normal | 49 | 41.5 | |
| Overweight | 29 | 24.6 | |
| Obese | 31 | 26.3 | |
|
| |||
| Intended | Unintended | 77 | 65.3 |
| Pregnancy | Intended | 41 | 34.7 |
|
| |||
| Smoking during | Yes | 11 | 9.3 |
| pregnancy | No | 107 | 90.7 |
Table 2.
Instrument Descriptive
| Variable | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| Dietary Quality Index for Pregnancy | 50.01 | 10.11 | 24.96 | 76.28 |
| Social Support | 55.47 | 9.28 | 21 | 66 |
| Eating Habits | 19.84 | 3.64 | 12 | 29 |
| Stress | 21.07 | 4.64 | 11 | 36 |
| Depression | 8.19 | 4.96 | 0 | 22 |
| Nutritional Knowledge | 13.42 | 3.35 | 5 | 25 |
Correlational analysis uncovered significantly negative relationships between dietary quality and eating habits and distress (index of stress and depression), but a significantly positive relationship with social support, maternal age, and education (Table 3). Social support had a negative relationship with the index of distress and eating habits; women with more social support experienced less stress and depression and had better eating habits than women with less social support. The index of distress was related positively to eating habits; that is, women with more depression or stress had poorer eating habits.
Table 3.
Correlations Among Support, Eating Habits, Distress and Dietary Quality
| Social Support | Eating Habits | Distress | Age | Education | Nutritional Knowledge | |
|---|---|---|---|---|---|---|
| Dietary Quality Index-Pregnancy | .206* | −.320** | −.293** | .208* | .190* | .155 |
| Social Support | 1 | −.239** | −.483** | −.020 | .073 | .027 |
| Eating Habits | 1 | −.395** | −.183* | −.068 | −.112 | |
| Distress | 1 | .078 | .120 | .000 | ||
| Age | 1 | .387** | .330** | |||
| Education | 1 | .451** | ||||
| Nutritional Knowledge | 1 |
Notes.
p < .05,
p < .01
Dietary quality was regressed on the index of distress, social support, and standardized scores for eating habits. This combination of factors explained 19% of the variance in dietary quality when controlling for maternal age and years of education (F = 5.23, df = 5, 112, p < .001), with eating habits and distress making a significant contribution to the variance (Table 4).
Table 4.
Regression Analysis
| β | t | p | |
|---|---|---|---|
| Control Variables | |||
| Maternal Age | .12 | 1.25 | .213 |
| Education | .15 | 1.61 | .111 |
| Model Variables | |||
| Distress | −.21 | −2.00 | .048 |
| Social Support | .06 | .64 | .522 |
| Eating Habits | −.191 | −2.02 | .046 |
A full path model with all possible direct and indirect paths from predictors to dependent variables and among predictors was tested (Figure 2). Path analysis revealed that distress had a direct effect on poor eating habits and dietary quality and an indirect effect on dietary quality when combined with poor eating habits for a total effect of β = −.30. Poor eating habits had a direct effect of β = −.18 on dietary quality. The index of social support had a significant direct effect on distress and a nonsignificant direct effect on eating habits and dietary quality but a significant indirect effect on dietary quality, for a total effect of β = .19. Subsequent analysis revealed that support from others did not have any significant direct effects on any variable in the model, whereas support from partners demonstrated a significant direct effect on distress (β = −.42) and nonsignificant direct effect on dietary quality (β = .03).
Figure 2. Full Empirical Model.
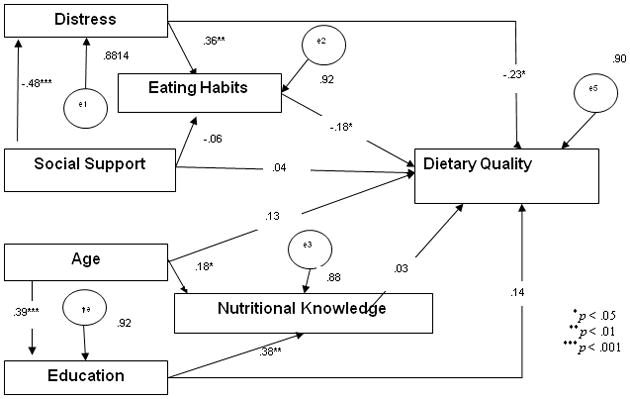
Empirical Path Model for Effects of Psychosocial Predictors on Dietary Quality (n = 118)
Maternal age had a significant direct effect on education and nutritional knowledge, a nonsignificant direct effect on dietary quality, and an indirect effect when combined with nutritional knowledge and education, for a total effect of β = .19. Maternal education had a significant direct effect on nutritional knowledge, a nonsignificant direct effect on dietary quality, and an indirect effect on dietary quality when combined with nutritional knowledge, for a total effect of β = .19 (Table 5). Maternal age, education, and nutritional knowledge did not have direct or indirect effects on distress, social support, or eating habits. The model was not significantly different from estimates (x2 = 12.02, df = 9, p = .21) and was a good fit (CFI = .97; RMSEA = .05, p = .4185); however, values for unexplained variance among endogenous variables were large (.88–.92).
Table 5.
Path Coefficients for Psychosocial Variable on Dietary Quality
| Predictor Variables | Effects
|
||
|---|---|---|---|
| Direct | Indirect | Total | |
| Social Support | 0.04 | 0.16 | 0.19 |
| Distress | −0.23 | −0.07 | −0.30 |
| Eating Habits | −0.18 | −0.18 | |
| Age | 0.13 | 0.06 | 0.19 |
| Education | 0.14 | 0.01 | 0.15 |
| Nutritional Knowledge | 0.04 | 0.03 | |
Discussion
This is one of the first studies to examine dietary quality in low-income women who were in the early weeks of their pregnancy, prior to enrolling in prenatal care or receiving food vouchers through the United States Special Supplemental Nutrition Program for Women, Infants and Children Program. Most of the women in this study did not have adequate dietary quality to ensure that they were meeting the nutritional recommendations for pregnancy in the US. These findings are similar to others that low-income pregnant women have inadequate intakes of iron, folate, fruits, and vegetables (Siega-Riz, Evenson, & Dole, 2004). Although Siega-Riz et al. did not compute a dietary quality index, nutrients and food that were examined are consistent with the DQI-P, and inadequate intake could have a negative impact on birth outcomes for these women.
The finding that stress and depression, elements of distress in this study, had a negative direct relationship with eating habits and overall dietary quality, is not surprising. Depression and stress together have been found to relate negatively to dietary quality and eating habits in low-income women during pregnancy (Larson, Story, Wall, & Neumark-Sztainer, 2006; Ma et. al., 2003; Tuffery & Scriven, 2005). The negative relationship between maternal mental stress and dietary quality is similar to others reporting poor dietary quality in stressed pregnant women (Borders et al., 2007; Larson et al., 2006).
Overall dietary quality among low-income women in the current study was related positively to support and is consistent with previous research (Fowles et al., 2005). The finding that support from a partner seemed to be more influential on improving dietary quality during early pregnancy than support from other family and friends is consistent with the works of Fowles et al. (2010); however, these results conflict with Thorton et al. (2006), who noted that support from female family friends or from a partner improved dietary intake in pregnant Latina women. Social support may serve to buffer the negative influence that psychosocial distress has on dietary quality. The influence of different types of social support on improving or hindering dietary quality during pregnancy requires further study.
As anticipated, poor eating habits, such as meal skipping and eating at fast food restaurants, had a very significant influence on dietary quality. This finding is similar to others reporting lower dietary quality in pregnant women who had poor eating habits by consuming less fruits and a high percent of total calories coming from fat (Siega-Riz et al., 2004).
Age and education were related independently to nutritional knowledge and to dietary quality, such that older women had more nutritional knowledge and a higher dietary quality score but less educated women had less nutritional knowledge and lower dietary quality scores. These findings are similar to those noted in a U.S. prospective cohort study (n = 1,777), in which Rifas-Shiman et al. (2009) noted that dietary quality in pregnancy differed by age and level of education. Also, the importance of nutritional knowledge on dietary quality supports previous research that suggests pregnancy may be an opportune time for health care providers to target nutrition education programs designed to improve maternal health and birth outcomes (Fowles & Gabrielson, 2005).
The current study has several limitations. First, the focus on low-income women in this study may limit the application of these findings to wealthier women. However, focusing on low-income women may be important since they are more vulnerable to experiencing adverse pregnancy outcomes. Understanding factors that influence their dietary intake may inform the development of food-based interventions designed to improve birth outcomes. Second, limitations to using dietary recalls include the under- or overreporting of intake, variations between foods eaten on weekends versus weekdays, and the possibility of participants providing socially desirable responses (Siega-Riz et al., 2004). Nonetheless, utilizing the multiple-pass method to obtain more complete intake amounts (Moshfegh et al., 2001) may minimize inherent dietary recall problems (Willett, 1998) by incorporating multiple, unannounced, nonconsecutive 24-hour recalls.
Findings from this study should be viewed with caution for several reasons. Although the sample size was adequate based on power analysis projections, responses from a larger number of women might alter the findings. Finally, the coefficient of internal consistency for the stress scale is just below the accepted value of .70; this may reflect lack of variability in participant responses to questions about stress following adverse life events (recent move, work difficulties, or drug abuse) that they have experienced.
Evaluating a woman’s dietary intake is an important component of the initial prenatal visit and dietary intake should be assessed frequently throughout pregnancy. In addition, health care providers should assess for factors that may enhance or pose as barriers to healthy eating, such as depression, presence of stressors, and eating habits, to identify women needing more intensive dietary monitoring and intervention throughout pregnancy. Frequent assessment of women’s dietary quality during pregnancy provides an opportunity to facilitate improvements in women’s dietary quality that could enhance maternal and fetal outcomes.
The lack of dietary quality in this sample supports the notion that low-income women are indeed a vulnerable, high-risk population. This requires further study to determine what contextual, behavioral, and psychosocial characteristics influence dietary quality so that evidenced-based, targeted interventions to promote dietary quality can be developed, potentially leading to improved birth outcomes.
Acknowledgments
Funding for this project was received from the National Institute of Nursing Research/National Institutes of Health, USA [1R21NR010592-01A1: Predictors of Dietary Quality in Low-Income Pregnant Women].
Contributor Information
Eileen R. Fowles, The University of Texas at Austin School of Nursing, Austin, Texas.
Miranda Bryant, Nutrition in Pregnancy Study, The University of Texas at Austin School of Nursing, Austin, Texas.
SungHun Kim, The University of Texas at Austin School of Nursing, Austin, Texas.
Lorraine O. Walker, The University of Texas at Austin School of Nursing, Austin, Texas.
Roberta Jeanne Ruiz, University of Texas at Austin, School of Nursing.
Gayle M. Timmerman, The University of Texas at Austin School of Nursing, Austin, Texas.
Adama Brown, The University of Texas at Austin School of Nursing, Austin, Texas.
References
- Agency for Healthcare Research and Quality. Publication No. 05-E006-2.171–174. Washington, DC: United States Department of Health and Human Services; 2005. Perinatal depression: Prevalence, screening accuracy, and screening outcomes. [Google Scholar]
- Arnow B, Kenardy J, Agras W. The Emotional Eating Scale: The development of a measure to assess coping with negative affect by eating. The International Journal of Eating Disorders. 1995;18:79–90. doi: 10.1002/1098-108x(199507)18:1<79::aid-eat2260180109>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Barker DJ. Fetal origins of coronary heart disease. BMJ. 1995;311(6998):171–174. doi: 10.1136/bmj.311.6998.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker DJ. The fetal origins of type 2 diabetes mellitus. Annals of Internal Medicine. 1999;130:322–324. doi: 10.7326/0003-4819-130-4-199902160-00019. [DOI] [PubMed] [Google Scholar]
- Baschat AA, Hecher K. Fetal growth restriction due to placental disease. Seminars in Perinatology. 2004;28:67–80. doi: 10.1053/j.semperi.2003.10.014. [DOI] [PubMed] [Google Scholar]
- Bhargava A. Socio-economic and behavioural factors are predictors of food use in the National Food Stamp Program Survey. The British Journal of Nutrition. 2004;92:497–506. doi: 10.1079/bjn20041210. [DOI] [PubMed] [Google Scholar]
- Bhatia J. Perinatal nutrition: Optimizing infant health and development. New York, NY: Marcel Dekker; 2005. [Google Scholar]
- Bodnar LM, Siega-Riz AM. A Diet Quality Index for Pregnancy detects variation in diet and differences by sociodemographic factors. Public Health Nutrition. 2002;5:801–809. doi: 10.1079/PHN2002348. [DOI] [PubMed] [Google Scholar]
- Borders AE, Grobam WA, Amsden LB, Holl JL. Chronic stress and low birth weight neonates in low-income population of women. Obstetrics and Gynecology. 2007;109:331–338. doi: 10.1097/01.AOG.0000250535.97920.b5. [DOI] [PubMed] [Google Scholar]
- Chou FH, Lin LL, Cooney A, Walker LO, Riggs MW. Psychosocial factors related to nausea, vomiting and fatigue in early pregnancy. Journal of Nursing Scholarship. 2003;35:119–125. doi: 10.1111/j.1547-5069.2003.00119.x. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: Development of the 10-Item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Curry MA, Burton D, Fields J. The Prenatal Psychosocial Profile: A research and clinical tool. Research in Nursing & Health. 1998;21:211–219. doi: 10.1002/(sici)1098-240x(199806)21:3<211::aid-nur4>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Curry MA, Campbell RA, Christian M. Validity and reliability testing of the Prenatal Psychosocial Profile. Research in Nursing and Health. 1994;17:127–135. doi: 10.1002/nur.4770170208. [DOI] [PubMed] [Google Scholar]
- Fowles ER. Comparing pregnant women’s nutritional knowledge to their actual dietary intake. MCN: The American Journal of Maternal-Child Nursing. 2002;27(3):171–177. doi: 10.1097/00005721-200205000-00009. [DOI] [PubMed] [Google Scholar]
- Fowles ER, Gabrielson M. First trimester predictors of diet and birth outcomes in low-income pregnant women. Journal of Community Health Nursing. 2005;22:117–130. doi: 10.1207/s15327655jchn2202_5. [DOI] [PubMed] [Google Scholar]
- Fowles ER, Hendricks JA, Walker LO. Identifying healthy eating strategies in low-income pregnant women: Applying a positive deviance model. Health Care for Women International. 2005;26:807–820. doi: 10.1080/07399330500230953. [DOI] [PubMed] [Google Scholar]
- Fowles E, Murphey C, Ruiz RJ. Exploring relationships among psychosocial status, dietary quality and measures of placental development during the first trimester in low-income women. Biological Research in Nursing. 2010 doi: 10.1177/1099800410378733. Available at http://brn.sagepub.com/content/early/2010/06/30/1099800410378733. [DOI] [PubMed]
- Freisling H, Elmadfa I, Gall I. The effect of socioeconomic status in dietary intake, physical activity and Body Mass Index in Austrian pregnant women. Journal of Human Nutrition and Dietetics. 2006;19:437–445. doi: 10.1111/j.1365-277X.2006.00723.x. [DOI] [PubMed] [Google Scholar]
- Godfrey KM, Barker DJ. Fetal nutrition and adult disease. The American Journal of Clinical Nutrition. 2000;71:1344S–1352S. doi: 10.1093/ajcn/71.5.1344s. [DOI] [PubMed] [Google Scholar]
- Groth MV, Fagt S, Bronsted L. Social determinants of dietary habits in Denmark. European Journal of Clinical Nutrition. 2001;55:959–966. doi: 10.1038/sj.ejcn.1601251. [DOI] [PubMed] [Google Scholar]
- Hofmeyr GJ, Atallah AN, Duley L. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database of Systematic Reviews. 2006;3:CD001059. doi: 10.1002/14651858.CD001059.pub2. [DOI] [PubMed] [Google Scholar]
- Huang JS, Lee TA, Lu MC. Prenatal programming of childhood overweight and obesity. Maternal and Child Health Journal. 2007;11:461–473. doi: 10.1007/s10995-006-0141-8. [DOI] [PubMed] [Google Scholar]
- Hurley KM, Caulfield LE, Sacco LM, Sacco LM, Costigan K, DiPeitro JA. Psychosocial influences in dietary patterns during pregnancy. Journal of the American Dietetic Association. 2005;105:963–966. doi: 10.1016/j.jada.2005.03.007. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Nutrition during pregnancy and lactation: An implementation guide. Washington, DC: National Academy Press; 1992. [Google Scholar]
- Institute of Medicine. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, DC: National Academy Press; 2005. [DOI] [PubMed] [Google Scholar]
- Jackson RA, Stotland NE, Caughey AB, Gerbert B. Improving diet and exercise in pregnancy with Video Doctor counseling: A randomized trial. Patient Education and Counseling. 2011;83:203–209. doi: 10.1016/j.pec.2010.05.019. [DOI] [PubMed] [Google Scholar]
- Kind KL, Moore VM, Davies MJ. Diet around conception and during pregnancy: Effects on fetal and neonatal outcomes. Reproductive Biomedicine Online. 2006;12:532–541. doi: 10.1016/s1472-6483(10)61178-9. [DOI] [PubMed] [Google Scholar]
- Larson NI, Story M, Wall M, Neumark-Sztainer D. Calcium and dairy intakes of adolescents are associated with their home environment, taste preferences, personal health beliefs, and meal patterns. Journal of the American Dietetic Association. 2006;106:1816–1824. doi: 10.1016/j.jada.2006.08.018. [DOI] [PubMed] [Google Scholar]
- Ma Y, Bertone ER, Stanek EJ, 3rd, Reed GW, Hebert JR, Cohen NL, et al. Association between eating patterns and obesity in a free-living US adult population. American Journal of Epidemiology. 2003;158:86–92. doi: 10.1093/aje/kwg117. [DOI] [PubMed] [Google Scholar]
- McMillen IC, Muhlhausler BS, Duffield JA, Yuen BS. Prenatal programming of postnatal obesity: Fetal nutrition and the regulation of leptin synthesis and secretion before birth. The Proceedings of the Nutrition Society. 2004;63:405–412. doi: 10.1079/pns2004370. [DOI] [PubMed] [Google Scholar]
- Moshfegh A, Raper N, Ingwersen L, Cleveland J, Anand J, Goldman J, LaComb R. An improved approach to 24-hour dietary recall methodology. Annals of Nutrition and Metabolism. 2001;45(Suppl 1):156. [Google Scholar]
- Munro B. Statistical methods for health care research. 5. Philadelphia, PA: Lippincott, Williams & Wilkins; 2004. [Google Scholar]
- Myers R. Classical and modern regression with applications. 2. Boston, MA: Duxbury; 1990. [Google Scholar]
- Neumark-Sztainer D, Story M, Hannan PJ, Perry CL, Irving LM. Weight-related concerns and behaviors among overweight and nonoverweight adolescents: Implications for preventing weight-related disorders. Archives of Pediatrics & Adolescent Medicine. 2002;156:171–178. doi: 10.1001/archpedi.156.2.171. [DOI] [PubMed] [Google Scholar]
- Nunnally J, Bernstein I. Psychometric theory. 3. New York, NY: McGraw-Hill; 1994. [Google Scholar]
- Painter RC, Roseboom TJ, Bleker OP. Prenatal exposure to the Dutch famine and disease later in life: An overview. Reproductive Toxicology. 2005;20:345–352. doi: 10.1016/j.reprotox.2005.04.005. [DOI] [PubMed] [Google Scholar]
- Raffensperger S, Kuczmarski MF, Hotchkiss L, Cotugna N, Evans MK, Zonderman AB. Effect of race and predictors of socioeconomic status on diet quality in the HANDLS Study sample. Journal of the National Medical Association. 2011;102:923–930. doi: 10.1016/s0027-9684(15)30711-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rifas-Shiman SL, Rich-Edwards JW, Kleinman KP, Oken E, Gillman MW. Dietary quality during pregnancy varies by maternal characteristics in Project Viva: A US cohort. Journal of the American Dietetic Association. 2009;109:1004–1011. doi: 10.1016/j.jada.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman JB, Alexander MA, Clark L, Dean A, Welter L. Instruments measuring maternal factors in obese preschool children. Western Journal of Nursing Research. 1992;14:555–575. doi: 10.1177/019394599201400502. [DOI] [PubMed] [Google Scholar]
- Siega-Riz AM, Evenson KR, Dole N. Pregnancy-related weight gain--a link to obesity? Nutrition Reviews. 2004;62(7 Pt 2):S105–S111. doi: 10.1111/j.1753-4887.2004.tb00079.x. [DOI] [PubMed] [Google Scholar]
- Siega-Riz AM, Herrmann TS, Savitz DA, Thorp JM. Frequency of eating during pregnancy and its effect on preterm delivery. American Journal of Epidemiololgy. 2001;153:647–652. doi: 10.1093/aje/153.7.647. [DOI] [PubMed] [Google Scholar]
- Sontrop J, Avison WR, Evers SE, Speechley KN, Campbell MK. Depressive symptoms during pregnancy in relation to fish consumption and intake of n-3 polyunsaturated fatty acids. Paedriatic and Perinatal Epidemiology. 2008;22:389–399. doi: 10.1111/j.1365-3016.2008.00941.x. [DOI] [PubMed] [Google Scholar]
- Susser M, Stein Z. Timing of prenatal nutrition: A reprise of the Dutch Famine Study. Nutrition Reviews. 1994;52(3):84–94. doi: 10.1111/j.1753-4887.1994.tb01395.x. [DOI] [PubMed] [Google Scholar]
- Tabachnick B, Fidell L. Using multivariate statistics. 4. Boston, MA: Allyn & Bacon; 2001. [Google Scholar]
- Thorton PL, Kieffer EC, Salabarria-Pena Y, Odoms-Young A, Willis SK, Kim H, et al. Weight, diet, and physical activity-related beliefs and practices among pregnant and postpartum Latino women: The role of social support. Maternal and Child Health Journal. 2006;10:95–104. doi: 10.1007/s10995-005-0025-3. [DOI] [PubMed] [Google Scholar]
- Tuffery O, Scriven A. Factors influencing antenatal and postnatal diets in primigravid women. The Journal of the Royal Society for the Promotion of Health. 2005;125:227–231. doi: 10.1177/146642400512500515. [DOI] [PubMed] [Google Scholar]
- Watters JL, Satia JA, Galanko JA. Associations of psychosocial factors with fruit and vegetable intake among African-Americans. Public Health Nutrition. 2007;10:701–711. doi: 10.1017/S1368980007662284. [DOI] [PubMed] [Google Scholar]
- Watts V, Rockett H, Baer H, Leppert J, Colditz G. Assessing diet quality in a population of low-income pregnant women: A comparison between Native Americans and Whites. Maternal and Child Health Journal. 2007;11:127–136. doi: 10.1007/s10995-006-0155-2. [DOI] [PubMed] [Google Scholar]
- Webb JB, Seiga-Riz AM, Dole N. Psychosocial determinants of adequacy of gestational weight gain. Obesity. 2009;17:300–309. doi: 10.1038/oby.2008.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willett W. Nutritional epidemiology. 2. New York, NY: Oxford University Press; 1998. [Google Scholar]


