Abstract
SARS-CoV was the cause of the global pandemic in 2003 that infected over 8000 people in 8 months. Vaccines against SARS are still not available. We developed a novel method to produce high levels of a recombinant SARS virus-like particles (VLPs) vaccine containing the SARS spike (S) protein and the influenza M1 protein using the baculovirus insect cell expression system. These chimeric SARS VLPs have a similar size and morphology to the wild type SARS-CoV. We tested the immunogenicity and protective efficacy of purified chimeric SARS VLPs and full length SARS S protein vaccines in a mouse lethal challenge model. The SARS VLP vaccine, containing 0.8 μg of SARS S protein, completely protected mice from death when administered intramuscular (IM) or intranasal (IN) routes in the absence of an adjuvant. Likewise, the SARS VLP vaccine, containing 4 μg of S protein without adjuvant, reduced lung virus titer to below detectable level, protected mice from weight loss, and elicited a high level of neutralizing antibodies against SARS-CoV. Sf9 cell-produced full length purified SARS S protein was also an effective vaccine against SARS-CoV but only when co-administered IM with aluminum hydroxide. SARS-CoV VLPs are highly immunogenic and induce neutralizing antibodies and provide protection against lethal challenge. Sf9 cell-based VLP vaccines are a potential tool to provide protection against novel pandemic agents.
Keywords: Severe acute respiratory syndrome, Virus like particles, Lung virus titer, Neutralizing antibody, Baculovirus, Influenza
1. Introduction
Severe acute respiratory syndrome (SARS) is an emerging infectious disease [1]. From November 2002 to July 2003, the SARS global outbreak spread from Guang Dong province of China, to Southeast Asia and North America. The World Health Organization reported a total of 8098 SARS cases in 26 countries by July 2003, including 774 deaths and 9.6% mortality rate [2]. This wave of SARS pandemic was finally contained through international coordination and strict quarantine enforcement by local governments. In addition to the loss of life, the affected region suffered from significant social disruptions and economic turmoil [3], [4].
SARS causes flu like symptoms including high fever, cough, difficulty breathing and pneumonia, and can spread from person to person by close contact via respiratory droplets from coughing or sneezing. No specific anti-SARS treatments or vaccines are available [5]. SARS is caused by a newly identified virus, SARS-associated coronavirus (SARS-CoV) [6]. SARS-CoV is a ∼100 nm diameter, enveloped, single strand RNA virus containing a 30 kb genome with 14 open reading frames. SARS-CoV has four major structural proteins, the spike (S), membrane (M), envelope (E) and nucleocapsid (N) proteins [7]. The S protein is a type I transmembrane glycoprotein responsible for virus binding and virus penetration. It is the major inducer of neutralizing antibodies and cellular immunity [8], [9]. The S protein has been the main target antigen for most SARS vaccines being developed [1], [10], [11], [12], [13], [33].
Although we are in an inter-epidemic period with no reported SARS case worldwide, a safe and effective SARS vaccine remains an important public health need. There are natural reservoirs of SARS-like coronavirus in wild bats and palm civets [14], [15] and humans could be infected by close contact with other unknown wild animal reservoirs [16]. Also, there have been reported cases of laboratory acquired SARS virus infection of researchers in 2004 [17]. SARS-CoV is classified by the National Institute of Allergy and infectious diseases as a biodefense category C priority pathogen, with the potential for use as a biological weapon [18]. There are currently no approved SARS vaccines and only limited human clinical trials with candidate vaccines have been done [22].
Previous SARS vaccine developments fall into several categories: inactivated SARS-CoV based vaccines [19], [20], [21], DNA or other recombinant viruses expressing the S spike glycoprotein [10], [11], [22], [47], subunit vaccines containing S receptor binding domain or soluble ectodomain [23], [24], [52] and virus like particles (VLPs) based vaccines. Of these, SARS-CoV VLP vaccine candidates have shown considerable promise [30], [31], [32], [48]. Recombinant VLP vaccine development has drawn increasing attention because it has the potential to be safer than inactivated or attenuated viral vaccines and to be more immunogenic than subunit or DNA vaccines [25], [49], [50]. Recently, recombinant influenza VLP vaccines have been reported to be well tolerated and immunogenic in human trials [51]. SARS S proteins have been incorporated into VLPs composed of either M and E, or M and N structural proteins, but were shown to be produced at low levels in mammalian cells [26], [27]. In a baculovirus insect cell expression system, the SARS S proteins were incorporated into secreted and intracellular VLPs composed of SARS M and E [28], [29], [30], [31], but with low yields. In an effort to address the low yields of SARS-CoV VLPs, chimeric VLPs containing the S from SARS-CoV and M, E, N from mouse hepatitis virus were produced and showed increased yields relative to wild type VLPs when expressed in mammalian cells. In addition, immunization with these VLPs reduced lung virus titer in a mouse challenged model [32]. Although, SARS VLPs formation and its immunogenicity were shown to be promising from these studies, the expression levels remained less than what would be needed for a viable commercial vaccine candidate.
In this report, we described a novel method to produce high levels of SARS VLPs in insect cells infected with a recombinant baculovirus containing a chimeric SARS-CoV S protein containing the influenza hemagglutinin (HA) transmembrane and carboxyl terminus, and the avian influenza matrix 1 (M1) protein. These chimeric SARS VLPs are efficiently produced and secreted from infected Sf9 insect cells. Purified chimeric SARS S/M1 VLPs were shown to completely protect immunized mice against lethal challenge with SARS-CoV while immunization with recombinant purified SARS S protein alone produced only partial protection.
2. Materials and methods
2.1. Plasmids, baculovirus and cells
The amino acids sequences of SARS-CoV Urbani strain spike protein (S, #AAP13441), influenza A/Indonesia/5/2005 (H5N1) hemagglutinin (HA, #ABP51969) and matrix protein 1 (M1, #ABI36004) were obtained from the NCBI protein database. To construct a chimeric SARS S protein, the transmembrane and carboxyl terminus (TM/CT) of the SARS S protein (aa 1196-1255) were removed and replaced with the TM/CT from A/Indonesia/5/2005 HA (aa 531-568). Codon optimized DNA sequences of the SARS S protein, the chimeric S protein, and the M1 protein used for high level expression in insect cells were biochemically synthesized by Geneart AG (Regensburg, Germany). These coding sequences were individually cloned into BamHI and HindIII sites of pFastBac1 baculovirus transfer vector plasmid (Invitrogen, Carlsbad, CA). pFastBac1-M1 was digested with SnaBI and PvuI. The 2571 bp fragment containing M1 coding sequence was gel purified. pFastBac1-S was digested with HpaI and PvuI. The 6870 bp fragment containing S coding sequence was gel purified. The 2571 bp and 6870 bp fragments were ligated together with T4 DNA ligase (Roche, Indianapolis, IN). This process produced a tandem pFastBac1 plasmid that contained both the chimeric SARS S gene and the M1 gene with each gene under the control of its own polyhedrin promoter.
The tandem chimeric S/M1 and the wild type full length SARS S transfer vectors were transformed into DH10Bac competent cells (Invitrogen) to produce bacmids. The bacmids were transfected into Spodoptera frugiperda Sf9 insect cells (ATCC CRL-1711) to generate recombinant baculovirus using a Bac-to-Bac baculovirus expression system (Invitrogen). Sf9 cells were maintained as suspensions in HyQ-SFX insect serum free medium (HyClone, Logan, UT) at 27 ± 2 °C.
2.2. SARS S and VLPs expression, purification and characterizations
Sf9 cells were infected at 2 × 106 cells/mL cell density for 66 h with recombinant baculovirus encoding SARS S or S/M1 chimeric VLP proteins at a multiplicity of infection (MOI) of 1. The SARS S proteins were exacted from infected cell pellet with non-ionic detergent 0.5% Tergitol NP9 (Sigma–Aldrich, St. Louis, MO). The clarified supernatant after detergent extraction were purified with a Fractogel TMAE anion exchange capture column (EMD chemicals, Darmstadt, Germany), followed by a Lentil lectin sepharose 4B affinity column (GE healthcare, Piscataway, NJ) and finally polished with a Sephacryl S300 size exclusion column (GE healthcare). The chimeric SARS S/M1 VLPs (referred as VLPs in later text) were purified from infected cell culture medium by tangential filtration, anion exchange, and size exclusion chromatography, the same procedure reported for influenza VLPs purification [40].
Purified S proteins and chimeric VLPs were analyzed by SDS-PAGE (4–12% Bis-Tris NuPage, Invitrogen) stained with GelCode Blue stain (Pierce, Rockford, IL) and quantified by scanning densitometry using OneDscan software (BD Biosciences, Rockville, MD). For animal studies, purified S proteins and chimeric VLPs were normalized to have the same amount of SARS S protein concentration based on total protein by BCA assay (Pierce) and S protein content (purity) by densitometry. The identity of the SARS S protein and the influenza M1 protein were confirmed by Western blot using the following antibodies: rabbit anti-SARS S antibody (Imgnex, San Diego, CA), mouse anti-influenza M1 antibody (AbD Serotec, Oxford, UK), goat anti-mouse and goat anti-rabbit phosphatase labeled secondary antibody (KPL, Gaithersburg, MD). BCIP/NBT phosphatase substrate (KPL) was used to develop the Western blot. Particle size of the SARS S protein and VLP vaccine was measured by dynamic light scattering using ZETASizer Nano (Malvern Instrument, Worcestershire, UK).
2.3. Electron microscopy analysis
Chimeric SARS VLPs were adsorbed for 2 min by flotation onto a freshly discharged 400 mesh carbon parlodion-coated copper grid (Poly-Sciences, Warrington, PA). The grids were rinsed with 20 mM Tris, pH 7.4, and 120 mM KCl, negatively stained with 1% phosphotungstic acid, then dried by aspiration. VLPs were visualized on a Hitachi H-7600 transmission electron microscope (Hitachi High Technologies America, Schaumburg, IL) operating at 80 kV and digitally captured with a CCD camera at 1K × 1K resolution (Advanced Microscopy Techniques Corp., Danvers, MA). For immunoelectron microscopy (Immuno EM), rabbit anti-SARS S antibody (Imgnex) was used as primary antibody and 6 nm colloidal gold-affinity pure goat anti-rabbit IgG (Jackson Immuno Research, West Grove, PA) was used as secondary antibody as described previously [46].
2.4. Vaccination and challenge
A total of 14 groups of 6–8 weeks old female Balb/c mice, 15 animals per group, were used in this study. Nine groups were vaccinated intramuscularly (IM) through hind limb with vehicle (PBS), 0.8 μg or 4 μg of SARS S or VLP vaccine, with or without aluminum hydroxide (Brenntag AG, Mülheim, Germany) adjuvant. Five groups were vaccinated intranasally (IN) with vehicle, 0.8 μg or 4 μg of SARS S or VLP vaccine without adjuvant. The animals were vaccinated on day 0 and day 21. On day 42, mice were intranasally challenged with 2 lethal dose 50 (LD50) of mouse-adapted SARS-CoV strain v2163 (1 LD50 = 103.64 TCID50). On day 45, 3 days post challenge, 5 mice from each group were sacrificed to collect lung tissue, and assayed for SARS-CoV lung titer. For the remaining 10 mice per group, body weight, morbidity, and mortality were measured daily from day 42 to 63.
In a second animal study to measure SARS-CoV neutralizing antibody titers, a total of 9 groups of 6–8 weeks old female Balb/c mice, 5 mice per group, were immunized IM with vehicle, 0.8 μg or 4 μg of SARS S or VLP vaccine, with or without aluminum hydroxide adjuvant, on day 0 and day 21. The animals were bled on days 0, 21 and 42 to measure neutralizing antibody titers. All animals had undetectable level of SARS-CoV neutralizing antibody titers on day 0.
SARS-CoV Urbani strain (200300592) was obtained from the Centers for Disease Control and Prevention (Atlanta, GA) and routinely passed in Vero-76 cells. SARS-CoV v2163 was a lethal strain derived from the mouse adapted Urbani strain [45].
2.5. Lung virus titer determination
Each mouse lung was weighed and homogenized in MEM (minimum essential medium). Each lung homogenate was centrifuged at 2000 × g for 5 min and 10 fold serial dilutions of the supernatant was assayed, in triplicate, for infectious virus by plaque assay using Vero-76. Virus titers were measured as CCID50/g tissue and were calculated using the Reed–Muench method. A titer of 0.75 CCID50/g tissue was the minimum detection limit of the assay.
2.6. Neutralizing antibody titer determination
A 7 μL aliquot of serum was added to 63 μL of MEM + 50 μg/mL gentamicin, mixed, then serially diluted 2-fold to achieve a 1/20–1/5120 dilutions in 96-well round-bottom plates. SARS-CoV Urbani strain stock was diluted in MEM to 200 CCID50 per 60 μL. 60 μL of diluted virus was added to each well, the plates were vibrated for approximately 1 min, and incubated for 1 h at 37 °C. 100 μL of the virus/serum mixture from each well was transferred to each well of a 96-well plates containing sub-confluent Vero-76 cells and 100 μL of MEM + 4% fetal bovine serum (FBS). Plates were sealed with tape and incubated for 5 days at 37 °C in 5% CO2, then scored for the presence or absence of virus microscopically based on cytopathic effect (CPE). Neutralization titer was calculated as the inverse of the greatest dilution of serum where no CPE was detected. The assays were performed in duplicate and a serum titer of 1:20 was the lowest dilution tested in the assay.
2.7. Ethics regulation of laboratory animals
The animal studies were conducted in accordance with the approval of the Institutional Animal Care and Use Committee of Utah State University dated 21 September 2004. The study was conducted in the AAALAC-accredited Laboratory Animal Research Center of Utah State University. The U.S. Government (National Institutes of Health) approval was renewed 27 February 2002 (Assurance no. A3801-01) in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals (Revision 1996).
3. Results
3.1. Expression and characterization of SARS S and VLPs
Full length recombinant SARS S protein was produced in the baculovirus insect cell expression system (Fig. 1B). The SARS S protein was isolated from infected cells solublized with non-ionic detergent and purified by column chromatography. Purified full length SARS S protein had an apparent molecular weight of 160 kDa by SDS-PAGE (Fig. 1D). Purified SARS S protein formed ∼25 nm diameter particles consisting of multiple S protein molecules when observed by dynamic light scattering and electron microscopy (data not shown).
Fig. 1.
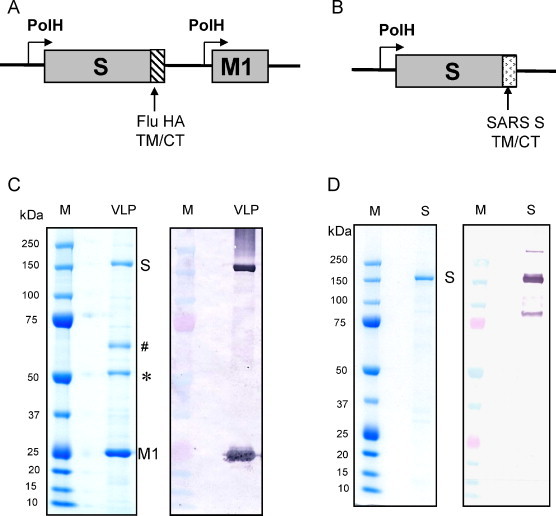
Expression and purification of SARS S and S/M1 chimeric VLP. (A) pFastBac1 baculovirus transfer vector for SARS S/Flu M1 chimeric VLP vaccine: SARS S protein with the influenza A/Indonesia/5/2005 hemagglutinin (HA) transmembrane and carboxyl terminus (TM/CT) and the M1 influenza matrix protein 1. Each gene is under the control of its own polyhedrin promoter; (B) pFastBac1 baculovirus transfer vector for wild type full length SARS S protein with its native TM/CT; (C) purified SARS VLP vaccine, left panel: coomassie blue stain, right panel: Western blot using anti-S and anti-M1 antibodies. Positions of the 160 kDa SARS S protein and the 25 kDa M1 protein are labeled. Bands labeled # and * were identified as baculovirus gp64 protein and insect cell β tubulin protein, respectively; (D) purified native SARS S protein, left panel: coomassie blue stain, right panel: Western blot using anti-SARS S antibody. Lane M contains precision plus protein molecular weight marker (Bio-Rad, Hercules, CA). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
We attempted to produce wild type SARS VLPs with homologous SARS S, M, and E proteins in insect cells but the process was inefficient and the VLP incorporated proteins could only be detected by Western blot. No S, M or E protein bands were observed in the coomassie blue stained gel (data not shown). This was probably due to the lack of an efficient matrix core protein needed for VLPs formation. Influenza matrix protein M1, especially the M1 from avian influenza A/Indonesia/5/2005 (H5N1) has been shown to support the production of high yield influenza VLPs even with hemagglutinin and neuraminidase from other heterologous influenza strains [34], [35]. As a result of those studies we decided to explore the possibility of forming a chimeric VLP containing the SARS S protein and the influenza M1 matrix protein. To maximize the interaction between the SARS S and the influenza M1, we replaced the wild type SARS S protein's transmembrane and carboxyl terminus (TM/CT) with the A/Indonesia/5/2005 influenza virus hemagglutinin TM/CT, and constructed a tandem transfer vector for chimeric S/M1 VLP production as shown in Fig. 1A.
Chimeric S/M1 VLPs were produced at high level from insect cells and were purified from the infected culture medium. The purified VLPs produced intense SARS S and influenza M1 protein bands on coomassie blue stained gel, at 14% and 51%, respective purity as measured by scanning densitometry (Fig. 1C). Two additional protein bands present in the VLPs were identified as baculovirus envelope protein gp64 (#) and insect cell skeleton protein β-tubulin (*) by Western blot (data not shown). These two proteins have been detected previously in some of the influenza VLPs we have produced in insect cells. Tubulin is likely to reside inside of VLPs since it may work together with actin to facilitate the baculovirus or VLPs transition to cell surface [53]. Glycoprotein gp64 is likely to be embedded in the VLPs envelope. Additional cell culture and purification development may help to reduce the level of these baculovirus and insect cell proteins in the SARS VLPs.
The average diameter of the chimeric S/M1 VLPs was 160 nm as measured by dynamic light scattering. The S/M1 VLPs contained spherical enveloped particles with a corona-like spike structure on the outer rim as determined by electron microscopy (EM) (Fig. 2A). The size and morphology of the S/M1 VLPs closely resembled the previously published SARS-CoV structures [36], [37], [38]. Immuno-EM using anti-SARS S protein primary antibody and 6 nm gold particles labeled secondary antibody showed that multiple S proteins were located on the surface of the spherical S/M1 VLPs (Fig. 2B).
Fig. 2.
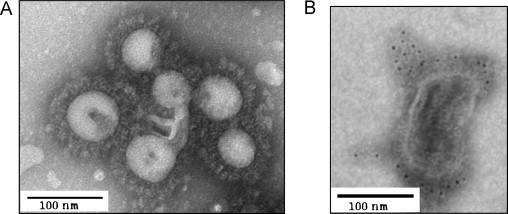
Transmission electron microscopy (EM) analysis of SARS VLPs. (A) Phosphotungstic acid negative stain of EM image of SARS VLPs; (B) immuno EM image of SARS VLPs using anti-SARS S protein primary antibody and 6 nm colloidal gold labeled secondary antibody. Black dots indicated gold labeled antibody binding to the SARS S protein. Bar: 100 nm.
3.2. Chimeric SARS VLPs protect mice from lethal challenge of SARS-CoV
The immunogenicity and protective efficacy of SARS S protein and S/M1 chimeric VLP vaccines were tested in a mouse lethal challenge model. Mice were intramuscularly (IM) or intranasally (IN) immunized with vehicle, 0.8 μg or 4 μg of SARS S protein or S/M1 VLPs, with or without aluminum hydroxide adjuvant, on days 0 and 21. The animals were challenged with SARS-CoV lethal strain v2163 on day 42. All mice in the vehicle control group died at 5.0 ± 0.9 days post challenge (Fig. 3A). In the IM immunization groups, 0.8 μg of purified SARS S protein without alum protected 7 out of 10 mice from death (Fig. 3B). In all other IM groups, 100% of the mice were protected from death (Fig. 3A and B). Mice immunized with 0.8 μg or 4 μg of purified SARS S protein, without alum, lost up to 15% and 7.5% of body weight, respectively before they fully recovered (Fig. 3C). All VLP groups and S + alum groups did not show any sign of weight loss (Fig. 3C) and the lung virus titers, at 3 days post challenge, appeared to correlate with the survival data (Fig. 3D): without adjuvant, 0.8 μg of the SARS S protein failed to significantly reduce lung virus titer, 4 μg of the SARS S protein reduced virus titer 2.5 log, 0.8 μg of the SARS VLPs reduced virus titer 6 logs, and 4 μg of the SARS VLPs reduced virus titer below the detectable limit. Likewise, in all groups containing SARS S protein with alum, lung virus titers were reduced below the detectable limit. This data indicated that as low as 0.8 μg of IM administered SARS VLP vaccine, without adjuvant, can fully protect mice from death and weight loss from a lethal virus challenge. IM administered SARS S protein vaccine can fully protect mice but only when co-administered with an alum adjuvant.
Fig. 3.
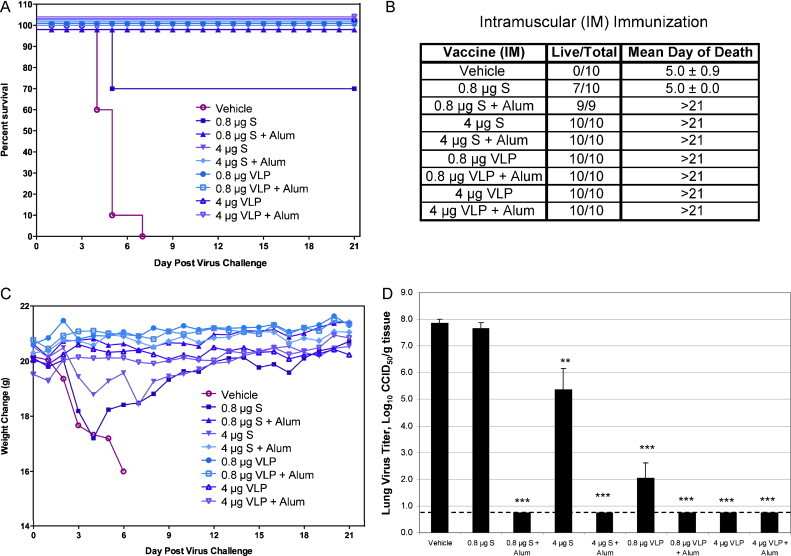
Survival rate and lung virus titer of mice intramuscularly (IM) immunized with SARS S protein vaccine or SARS VLP vaccine after SARS-CoV lethal challenge. Mice were immunized (IM) with vehicle, 0.8 μg or 4 μg of SARS S protein or SARS VLPs, with or without aluminum hydroxide, on days 0 and 21 (n = 14 or 15). Mice were challenged with 2 LD50 of SARS-CoV strain v2163 on day 42. Five mice per group were sacrificed on day 45. Lung tissues were collected, homogenized, and assayed for virus titer. The remaining mice were monitored for survival and body weight from day 42 to day 63. (A) Survival percentage curve; (B) survival table with the mean day of death; (C) animal weight change for 21 days post challenge; (D) lung SARS-CoV titer at day 45, 3 days post challenge. Virus titer was calculated as log10 CCID50/gram lung tissue with limit of detection as 0.75 (dashed line). Results were expressed as mean titer ± SEM. Statistical significance between the vehicle and vaccine groups was determined by the student t test. **p < 0.01, ***p < 0.001.
For IN immunization, no adjuvant was used. 0.8 μg or 4 μg of the SARS S protein failed to protect mice from lethal challenge and resulted in 100% death, same as the vehicle control group. Whereas, all mice immunized with 0.8 μg and 4 μg of the SARS VLPs survived virus challenge (Fig. 4A and B). The net weight loss for both of the VLP vaccine groups was as high as 3–4% but the animals completely recovered (Fig. 4C). Also, the SARS S protein failed to reduce lung virus titer. In the 0.8 μg and 4 μg VLP vaccine groups, lung virus titer were reduced 1 and 3.5 logs, respectively (Fig. 4D). The data show that without an effective adjuvant, the SARS S protein failed to protect when administered IN. The IN VLP vaccine without adjuvant protected 100% of mice from death, similar to when the vaccine is given IM. However, the lung virus titers in the IN VLP vaccine groups were 4 logs higher than the corresponding IM groups and the IN immunized animals suffered minor weight loss. The data from IM and IN lethal challenge studies indicate that the SARS S protein vaccine requires an effective adjuvant to be protective. For both vaccines, the IM route of administration worked better than IN for reducing lung virus titer. One possible explanation is that local immunity was mainly induced in the upper respiratory tract during IN immunization and not in the lower respiratory tract where the SARS-CoV replicates [41], [42], [43], [44] and where immunity was not fully established at the time of challenge. Whereas, after IM immunization, a broader systemic humoral immunity was developed that offer a better protection against SARS-CoV challenge through out the respiratory tract. IM immunization may also induce higher neutralizing antibody titers to help reduce lung virus titers.
Fig. 4.
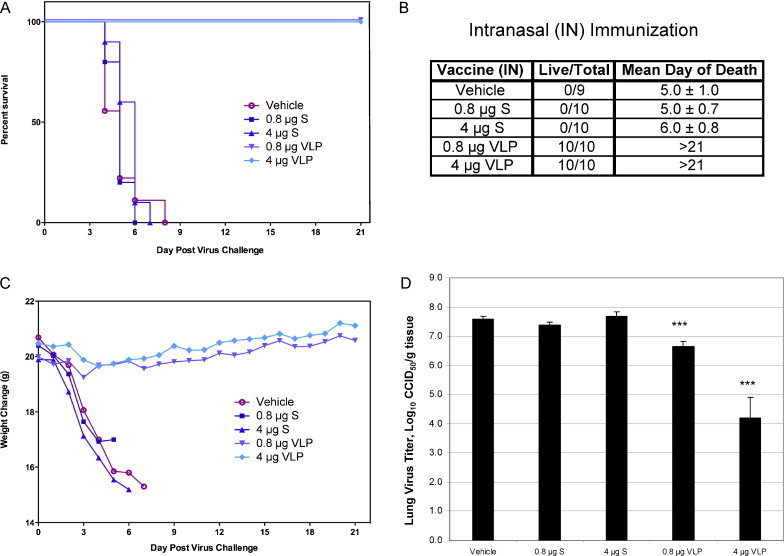
Survival rate and lung virus titer of mice intranasally (IN) immunized with SARS S protein vaccine or SARS VLP vaccine after SARS-CoV lethal challenge. Mice were immunized (IN) with vehicle, 0.8 μg or 4 μg of SARS S protein or SARS VLPs, without adjuvant, on day 0 and 21 (n = 14 or 15). Mice were challenged with 2 LD50 of SARS-CoV strain v2163 on day 42. Five mice per group were sacrificed on day 45. Lung tissues were collected and assayed for virus titer. The remaining mice were monitored for survival and body weight from day 42 to day 63. (A) Survival percentage curve; (B) survival table with the mean day of death; (C) animal weight change for 21 days after challenge; (D) lung SARS-CoV titer at day 45, 3 days post challenge. Virus titer was calculated as log10 CCID50/gram lung tissue. Results were expressed as mean titer ± SEM. Statistical significance between the vehicle and vaccine groups was determined by the student t test. ***p < 0.001.
To measure the humoral neutralizing antibody response, mice were immunized IM with vehicle, 0.8 μg or 4 μg of the SARS S protein or the chimeric SARS S/M1 VLPs, with or without aluminum hydroxide, on days 0 and 21. Mice were bled on days 21 and 42, and the sera samples were assayed for neutralizing antibodies against SARS-CoV (Fig. 5 ). Both the SARS S protein and the SARS VLPs need two vaccinations to elicit any neutralizing antibody titers > 250. The SARS S vaccine required alum adjuvant to induce neutralizing antibody titers above the base line, whereas 0.8 μg and 4 μg VLPs vaccine without alum can induce neutralizing antibody titer up to 878 and 1525, respectively. This result directly correlated with the survival rate and post challenge lung virus titer as shown in Fig. 3. The SARS S vaccine with alum and the SARS VLPs vaccine groups had neutralizing antibody geometry mean titer ranging from 878 to 2550, and they were not statistically different from each other. S with alum groups showed a trend of higher neutralizing antibody titer at day 42 than VLPs with alum. One explanation may be that S protein can absorb to alum more efficiently than VLPs, and the slow release of S from alum results a prolonged elevated antibody response at day 42.
Fig. 5.
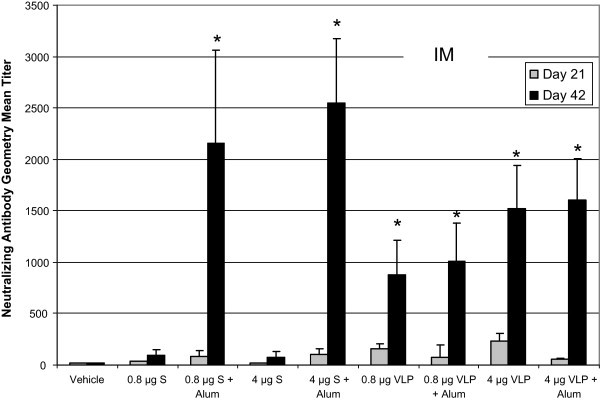
Neutralizing antibody titer of mice intramuscularly (IM) immunized with SARS S protein vaccine or SARS VLP vaccine. Mice were immunized (IM) with vehicle, 0.8 μg or 4 μg of SARS S protein or SARS VLPs, with or without aluminum hydroxide, on days 0 and 21. Mice were bled on day 21 (grey bar) and 42 (black bar). Sera samples were 2 fold serially diluted and assayed for neutralizing antibodies. SARS-CoV neutralizing antibody titer was defined as the inverse of the greatest dilution of serum that neutralized 100% and had no visible virus CPE. Results are expressed as the geometric mean titer ± SEM. A 1:20 dilution was the lowest dilution of serum tested. Statistical significance between vehicle and vaccine groups for day 42 sera samples was determined by the student t test. *p < 0.05.
4. Discussion
In this paper, we report a novel method to produce chimeric SARS VLPs containing the spike protein of SARS and the matrix protein of influenza virus using the baculovirus insect cell expression system. We obtained the level of 1 mg (S content) SARS VLPs per liter of Sf9 cell culture in shake flask. Upon further cell culture optimization such as stir tank reactor, high cell density, fed-batch or medium exchange and purification development, such yield is expected to increase several fold or more. We studied the immunogenicity and protective efficacy of the SARS S protein vaccine and the SARS VLP vaccine in a mice lethal challenge model. The VLP vaccine, without adjuvant, protected 100% of the immunized mice from death when given IM, reduced lung virus titer to undetectable levels, and elicited serum neutralizing antibody titer up to 1500. On the other hand, the S protein vaccine required alum adjuvant to effectively protect mice from lethal challenge, reduce lung virus titers, and elicit neutralizing antibodies. The data suggest that both the SARS S vaccine with alum and the SARS VLP vaccine are good candidates for protection against SARS-CoV infections when administered IM.
The recombinant VLP vaccines have been an attractive approach for vaccine development for the past decade. VLPs do not contain the viral genome, therefore cannot replicate in humans or revert to a pathogenic form. These characteristics make VLPs a safer vaccine for the recipient, and also a safer vaccine to manufacturing than inactivated or live attenuated viral vaccines, especially for a dangerous virus such as SARS-CoV that can cause high morbidity and death [25]. The repetitive antigen pattern represented on the surface of VLPs make them easier to be recognized by antigen presenting cells than subunit vaccines and therefore are able to induce a stronger and broader humoral and cellular immune response [34], [35], [39]. There are only three VLP vaccines approved for human use, the Hepatitis B vaccine and the two HPV vaccines. All three are composed of single protein particles without a lipid bilayer envelope. In addition, one of the commercial HPV vaccines (Cervarix) is produced in the baculovirus insect cell expression system [25]. The more complex version of VLPs, such as influenza VLPs that contain hemagglutinin, neuraminidase, M1 proteins, and a lipid bilayer envelope, are currently being evaluated in phase II human clinical trials by Novavax Inc. No other VLP vaccine is approved or in the late stage of clinical development, partially because VLPs are usually difficult to produce in high level due to the lack of an efficient viral core protein. In this report, we showed that influenza matrix M1 protein has the potential to become a universal core protein to support VLPs production for other viruses. It is not a coincidence that M1 can form VLPs with the SARS S protein. SARS-CoV and influenza virus share many common features: both have a RNA genome; both are 100–200 nm diameter spherical particles; both have a major surface spike glycoprotein (S or HA) that form trimers, and both spike glycoproteins contain a globular head domain and a stem region. The replacement of the SARS S TM/CT with the HA TM/CT may help to maximize the native interaction between core protein and surface antigen, and promote VLPs formation and secretion. The use of the influenza M1 as a core protein to form VLPs for other viruses is a promising approach that can be explored in the future. Besides of the potential yield increase, influenza M1 containing chimeric VLPs can quickly activated M1 specific memory CD4 T cells since most human population were infected multiple times with influenza virus during their lifetime. Activated M1 specific CD4 T cells can stimulate SARS S or other antigen specific B cells for differentiation and antibody secretion.
Our SARS chimeric VLP vaccine was manufactured by the same procedures as our influenza VLP vaccine that has been successfully tested in phase I and phase II clinical studies [51]. These two products share common infrastructure, equipment, supplies (medium, resin, filter, etc.) and utilize several identical standard operating procedures. In the unfortunate case of another SARS pandemic, countries or regions with existing influenza VLP vaccine manufacturing capacity will have the ability to quickly switch to the SARS vaccine production in the same facility, just like switching to another seasonal flu strain. The SARS VLP vaccine can be produced in an influenza VLP vaccine manufacturing facility within a short, 10–12 weeks period, after the pandemic virus is identified and sequenced or sooner if an Urbani-like strain reoccurs. A multi-use facility for seasonal flu, pandemic flu, and SARS may be desired for many countries because during another SARS pandemic the borders between countries may be closed and restrict vaccines from entering. Thus, pandemic vaccine manufacturing capacity within one's own borders may be critical for protecting their own citizens from infection.
Acknowledgements
We thank Peter Pushko, Jason Mantich, Attiya Ahmad, Maithili Kale, Yingyun Wu, Malgorzata Wisniewska, Jim Norton, Lou Potash, Travis Sadowski, Konnie Taylor, Sarathi Boddapati (Novavax Inc.) for their valuable contribution to this study. We thank Fredrick Cassels and Heather Greenstone (NIAID, NIH) for their helpful suggestions to the animal study. We thank Michael Delannoy for his electron microscopy service. We thank Shinji Makino (University of Texas) for providing SARS reagent and suggestions. The animal work was supported, in part, by contract NO1-AI-15345 from the Virology Branch, NIAID, National Institutes of Health. This work was supported by NIH grant 1U03AI06198801.
References
- 1.Enjuanes L., Dediego M.L., Alvarez E., Deming D., Sheahan T., Baric R. Vaccines to prevent severe acute respiratory syndrome coronavirus-induced disease. Virus Res. 2008;133(1):45–62. doi: 10.1016/j.virusres.2007.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. http://www.who.int/csr/sars/country/table2004_04_21/en/.
- 3.Ahmad A., Krumkamp R., Reintjes R. Controlling SARS: a review on China's response compared with other SARS-affected countries. Trop Med Int Health. 2009;14(Suppl. 1):36–45. doi: 10.1111/j.1365-3156.2008.02146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beutels P., Jia N., Zhou Q.Y., Smith R., Cao W.C., de Vlas S.J. The economic impact of SARS in Beijing, China. Trop Med Int Health. 2009;14(Suppl. 1):85–91. doi: 10.1111/j.1365-3156.2008.02210.x. [DOI] [PubMed] [Google Scholar]
- 5.Chan-Yeung M., Ooi G.C., Hui D.S., Ho P.L., Tsang K.W. Severe acute respiratory syndrome. Int J Tuberc Lung Dis. 2003;7(12):1117–1130. [PubMed] [Google Scholar]
- 6.Drosten C., Günther S., Preiser W., van der Werf S., Brodt H.R., Becker S. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med. 2003;348(20):1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- 7.Masters P.S. The molecular biology of coronaviruses. Adv Virus Res. 2006;66:193–292. doi: 10.1016/S0065-3527(06)66005-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li W., Moore M.J., Vasilieva N., Sui J., Wong S.K., Berne M.A. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426(6965):450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qiu M., Shi Y., Guo Z., Chen Z., He R., Chen R. Antibody responses to individual proteins of SARS coronavirus and their neutralization activities. Microbes Infect. 2005;7(5–6):882–889. doi: 10.1016/j.micinf.2005.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bisht H., Roberts A., Vogel L., Bukreyev A., Collins P.L., Murphy B.R. Severe acute respiratory syndrome coronavirus spike protein expressed by attenuated vaccinia virus protectively immunizes mice. Proc Natl Acad Sci USA. 2004;101(17):6641–6646. doi: 10.1073/pnas.0401939101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang Z.Y., Kong W.P., Huang Y., Roberts A., Murphy B.R., Subbarao K. A DNA vaccine induces SARS coronavirus neutralization and protective immunity in mice. Nature. 2004;428(6982):561–564. doi: 10.1038/nature02463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vogel L.N., Roberts A., Paddock C.D., Genrich G.L., Lamirande E.W., Kapadia S.U. Utility of the aged BALB/c mouse model to demonstrate prevention and control strategies for severe acute respiratory syndrome coronavirus (SARS-CoV) Vaccine. 2007;25(12):2173–2179. doi: 10.1016/j.vaccine.2006.11.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bai B., Lu X., Meng J., Hu Q., Mao P., Lu B. Vaccination of mice with recombinant baculovirus expressing spike or nucleocapsid protein of SARS-like coronavirus generates humoral and cellular immune responses. Mol Immunol. 2007;45:868–875. doi: 10.1016/j.molimm.2007.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rihtaric D., Hostnik P., Steyer A., Grom J., Toplak I. Identification of SARS-like coronaviruses in horseshoe bats (Rhinolophus hipposideros) in Slovenia. Arch Virol. 2010;155(4):507–514. doi: 10.1007/s00705-010-0612-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson L.J., Tong S. Update on SARS research and other possibly zoonotic coronaviruses. Int J Antimicrob Agents. 2010;36(November (Suppl. 1)):S21–S25. doi: 10.1016/j.ijantimicag.2010.06.016. Epub 2010 (August 30) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guan Y., Zheng B.J., He Y.Q., Liu X.L., Zhuang Z.X., Cheung C.L. Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science. 2003;302(5643):276–278. doi: 10.1126/science.1087139. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. China's latest SARS outbreak has been contained, but biosafety concerns remain-Update 7, 18 May 2004. http://www.who.int/csr/don/2004_05_18a/en/.
- 18.NIAID Category A, B, and C Priority Pathogens. http://www.niaid.nih.gov/topics/biodefenserelated/biodefense/research/pages/cata.aspx.
- 19.Spruth M., Kistner O., Savidis-Dacho H., Hitter E., Crowe B., Gerencer M. A double-inactivated whole virus candidate SARS coronavirus vaccine stimulates neutralising and protective antibody responses. Vaccine. 2006;24(5):652–661. doi: 10.1016/j.vaccine.2005.08.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marshall E., Enserink M. Medicine. Caution urged on SARS vaccines. Science. 2004;303(5660):944–946. doi: 10.1126/science.303.5660.944. [DOI] [PubMed] [Google Scholar]
- 21.Qin E., Shi H., Tang L., Wang C., Chang G., Ding Z. Immunogenicity and protective efficacy in monkeys of purified inactivated Vero-cell SARS vaccine. Vaccine. 2006;24(7):1028–1034. doi: 10.1016/j.vaccine.2005.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martin J.E., Louder M.K., Holman L.A., Gordon I.J., Enama M.E., Larkin B.D. A SARS DNA vaccine induces neutralizing antibody and cellular immune responses in healthy adults in a phase I clinical trial. Vaccine. 2008;26(50):6338–6343. doi: 10.1016/j.vaccine.2008.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bisht H., Roberts A., Vogel L., Subbarao K., Moss B. Neutralizing antibody and protective immunity to SARS coronavirus infection of mice induced by a soluble recombinant polypeptide containing an N-terminal segment of the spike glycoprotein. Virology. 2005;334(2):160–165. doi: 10.1016/j.virol.2005.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou Z., Post P., Chubet R., Holtz K., McPherson C., Petric M. A recombinant baculovirus-expressed S glycoprotein vaccine elicits high titers of SARS-associated coronavirus (SARS-CoV) neutralizing antibodies in mice. Vaccine. 2006;24(17):3624–3631. doi: 10.1016/j.vaccine.2006.01.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roy P., Noad R. Virus-like particles as a vaccine delivery system: myths and facts. Hum Vaccine. 2008;4(1):5–12. doi: 10.4161/hv.4.1.5559. [DOI] [PubMed] [Google Scholar]
- 26.Hsieh P.K., Chang S.C., Huang C.C., Lee T.T., Hsiao C.W., Kou Y.H. Assembly of severe acute respiratory syndrome coronavirus RNA packaging signal into virus-like particles is nucleocapsid dependent. J Virol. 2005;79(22):13848–13855. doi: 10.1128/JVI.79.22.13848-13855.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang Y., Yang Z.Y., Kong W.P., Nabel G.J. Generation of synthetic severe acute respiratory syndrome coronavirus pseudoparticles: implications for assembly and vaccine production. J Virol. 2004;78(22):12557–12565. doi: 10.1128/JVI.78.22.12557-12565.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mortola E., Roy P. Efficient assembly and release of SARS coronavirus-like particles by a heterologous expression system. FEBS Lett. 2004;576:174–178. doi: 10.1016/j.febslet.2004.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ho Y., Lin P.H., Liu C.Y., Lee S.P., Chao Y.C. Assembly of human severe acute respiratory syndrome coronavirus-like particles. Biochem Biophys Res Commun. 2004;318(4):833–838. doi: 10.1016/j.bbrc.2004.04.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lu X., Chen Y., Bai B., Hu H., Tao L., Yang J. Immune responses against severe acute respiratory syndrome coronavirus induced by virus-like particles in mice. Immunology. 2007;122(4):496–502. doi: 10.1111/j.1365-2567.2007.02676.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bai B., Hu Q., Hu H., Zhou P., Shi Z., Meng J. Virus-like particles of SARS-like coronavirus formed by membrane proteins from different origins demonstrate stimulating activity in human dendritic cells. PLoS One. 2008;3(7):e2685. doi: 10.1371/journal.pone.0002685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lokugamage K.G., Yoshikawa-Iwata N., Ito N., Watts D.M., Wyde P.R., Wang N. Chimeric coronavirus-like particles carrying severe acute respiratory syndrome coronavirus (SCoV) S protein protect mice against challenge with SCoV. Vaccine. 2008;26(6):797–808. doi: 10.1016/j.vaccine.2007.11.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roper R.L., Rehm K.E. SARS vaccines: where are we? Expert Rev Vaccines. 2009;8(7):887–898. doi: 10.1586/erv.09.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bright R.A., Carter D.M., Crevar C.J., Toapanta F.R., Steckbeck J.D., Cole K.S. Cross-clade protective immune responses to influenza viruses with H5N1 HA and NA elicited by an influenza virus-like particle. PLoS One. 2008;3(1):e1501. doi: 10.1371/journal.pone.0001501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Song H., Wittman V., Byers A., Tapia T., Zhou B., Warren W. In vitro stimulation of human influenza-specific CD8+ T cells by dendritic cells pulsed with an influenza virus-like particle (VLP) vaccine. Vaccine. 2010;28(34):5524–5532. doi: 10.1016/j.vaccine.2010.06.044. [DOI] [PubMed] [Google Scholar]
- 36.Almeida J., Tyrell D. The morphology of three previously uncharacterized human respiratory viruses that grow in organ culture. J Gen Virol. 1967;2:175–178. doi: 10.1099/0022-1317-1-2-175. [DOI] [PubMed] [Google Scholar]
- 37.Zhang Q.F., Cui J.M., Huang X.J., Lin W., Tan D.Y., Xu J.W. Morphology and morphogenesis of severe acute respiratory syndrome (SARS)-associated virus. Acta Biochim Biophys Sin. 2003;35(6):587–591. [PubMed] [Google Scholar]
- 38.Drosten C., Lau A., Preiser W., So L., Yam L. In: SARS reference. 3rd ed. Kamps B.S., Hoffmann C., editors. Flying Publisher; 2003. p. 41. http://www.sarsreference.com. [Google Scholar]
- 39.Bright R.A., Carter D.M., Daniluk S., Toapanta F.R., Ahmad A., Gavrilov V. Influenza virus-like particles elicit broader immune responses than whole virion inactivated influenza virus or recombinant hemagglutinin. Vaccine. 2007;25(19):3871–3878. doi: 10.1016/j.vaccine.2007.01.106. [DOI] [PubMed] [Google Scholar]
- 40.Pushko P., Kort T., Nathan M., Pearce M.B., Smith G., Tumpey T.M. Recombinant H1N1 virus-like particle vaccine elicits protective immunity in ferrets against the 2009 pandemic H1N1 influenza virus. Vaccine. 2010;28(30):4771–4776. doi: 10.1016/j.vaccine.2010.04.093. [DOI] [PubMed] [Google Scholar]
- 41.Hall L.J., Clare S., Dougan G. Probing local innate immune responses after mucosal immunisation. J Immune Based Ther Vaccines. 2010;8(1):5. doi: 10.1186/1476-8518-8-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hamming I., Timens W., Bulthuis M.L., Lely A.T., Navis G.J., van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ding Y., He L., Zhang Q., Huang Z., Che X., Hou J. Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS-CoV) in SARS patients: implications for pathogenesis and virus transmission pathways. J Pathol. 2004;203(2):622–630. doi: 10.1002/path.1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen J., Subbarao K. The immunobiology of SARS. Annu Rev Immunol. 2007;25:443–472. doi: 10.1146/annurev.immunol.25.022106.141706. [DOI] [PubMed] [Google Scholar]
- 45.Day C.W., Baric R., Cai S.X., Frieman M., Kumaki Y., Morrey J.D. A new mouse-adapted strain of SARS-CoV as a lethal model for evaluating antiviral agents in vitro and in vivo. Virology. 2009;395(2):210–222. doi: 10.1016/j.virol.2009.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Murti K.G., Portner A., Thoughton K., Deshpande K. Localization of proteins on viral nucleocapsids using immunoelectron microscopy. J Electron Microsc Tech. 1985;2:139–146. [Google Scholar]
- 47.Feng Q., Liu Y., Qu X., Deng H., Ding M., Lau T.L. Baculovirus surface display of SARS coronavirus (SARS-CoV) spike protein and immunogenicity of the displayed protein in mice models. Immunology. 2007;122(4):496–502. doi: 10.1089/dna.2006.25.668. [DOI] [PubMed] [Google Scholar]
- 48.Lu B., Huang Y., Huang L., Li B., Zheng Z., Chen Z. Effect of mucosal and systemic immunization with virus-like particles of severe acute respiratory syndrome coronavirus in mice. Immunology. 2010;130(2):254–261. doi: 10.1111/j.1365-2567.2010.03231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ludwig C., Wagner R. Virus-like particles–universal molecular toolboxes. Curr Opin Biotechnol. 2007;18(6):537–545. doi: 10.1016/j.copbio.2007.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grgacic E.V., Anderson D.A. Virus-like particles: passport to immune recognition. Methods. 2006;40(1):60–65. doi: 10.1016/j.ymeth.2006.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.López-Macías C, Ferat-Osorio E, Tenorio-Calvo A, Isibasi A, Talavera J, Arteaga-Ruiz O, et al. Safety and immunogenicity of a virus-like particle pandemic influenza A (H1N1) 2009 vaccine in a blinded, randomized, placebo-controlled trial of adults in Mexico. Vaccine, under review. [DOI] [PMC free article] [PubMed]
- 52.Hu M.C., Jones T., Kenney R.T., Barnard D.L., Burt D.S., Lowell G.H. Intranasal protollin-formulated recombinant SARS S-protein elicits respiratory and serum neutralizing antibodies and protection in mice. Vaccine. 2007;25(34):6334–6340. doi: 10.1016/j.vaccine.2007.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ohkawa T., Volkman L.E., Welch M.D. Actin-based motility drives baculovirus transit to the nucleus and cell surface. J Cell Biol. 2010;190(2):187–195. doi: 10.1083/jcb.201001162. [DOI] [PMC free article] [PubMed] [Google Scholar]


