Abstract
This investigation compared a traditional behavioral weight loss program with a weight loss intervention emphasizing environmental modification and habit formation and disruption. Fifty-four overweight and obese adults (BMI ≥ 27 kg/m2) were randomly assigned to either a 14-week LEARN or TYL intervention. Forty-two participants completed the six-month follow-up assessment. Treatment outcomes between LEARN and TYL participants were equivalent. During the six-month no-treatment follow-up period, participants evidenced a 3.3 lb (SD = 9.2) weight gain. The TYL intervention appears to represent an attractive option for individuals seeking an alternative to the traditional behavioral approach to weight loss.
Introduction
Escalating rates of obesity in recent decades (Ogden et al., 2006) have coincided with significant changes in food and physical activity environments that encourage excess energy intake and discourage energy expenditure (Brownell & Horgen, 2004; Lowe, 2003; Nestle, 2004). These changes include increased portion sizes and availability of cheap, energy dense foods, as well as increased television, computer, and Internet use. Experts have concluded that the current ‘obesogenic’ environment continues to fuel the obesity epidemic while contributing to the widespread failure of weight loss attempts and maintenance (e.g. Brownell & Horgen, 2004; Lowe, 2003; Nestle, 2004).
Consistent with these conclusions, research indicates that the food environment has a significant impact on food consumption (e.g. Brownell & Horgen, 2004; French, Story, & Jeffrey, 2001; Harris, Bargh, & Brownell, 2009; Nestle, 2004; Sobal & Wansink, 2007; Wansink, 2004; Wansink & Sobal, 2007). It is believed, at least in part, that the obesogenic environment's impact on obesity rates is influenced by automatic processes, in which aspects of the environment regularly cue overeating and a sedentary lifestyle (Rothman, Sheeran, & Wood, 2010). For example, we speculate that it is not uncommon for an individual to automatically eat candy from a candy dish, even though s/he is not hungry, is unaware of the choice, and has the long-term goal of weight loss.
Models that explicate automatic or impulsive influences on behavior suggest that automatic processes often override more limited and effortful reflective systems (Hofmann, Friese, & Wiers, 2008). These dual process memory models, such as the Reflective Impulsive Model (RIM), suggest that individuals utilize two memory systems: impulsive and reflective. The impulsive system learns associations over an accumulated set of experiences and is constantly active, while the reflective system learns rules using language and logic, but competes for available cognitive resources (Hofmann et al., 2008).
These models and their emphasis on automatic processes are consistent with a growing body of research indicating that behaviors and goal pursuits can become activated upon the mere presence of relevant information in the person's environment (e.g. Bargh & Chartrand, 1999; Gollwitzer & Bargh, 2005). A principle underlying these observations (i.e. Auto-Motive Model), suggests that automatic associations are formed between representations in the environment (e.g. people, settings), and other representations, such as goal pursuits (Bargh & Chartrand, 1999). Thus, features of the context in which reflective goals have consistently been pursued over time become capable of automatically activating goal pursuits. In other words, seeing a treadmill at home has the potential to activate an individual's goal to exercise five days a week for 30 minutes each day, because over time, the treadmill becomes automatically linked in memory to the goal of exercising five days a week.
These findings emphasize the importance of creating an environment that maximizes the cueing of healthy behaviors and minimizes the cueing of unhealthy behaviors. Teaching individuals to create personal food environments that minimize unhealthy food-related decisions/exposure and maximize healthy food-related decisions/exposure may be critical to successful weight loss and maintenance.
As a way to capitalize on automatic processing, habit formation is critical to sustaining behavioral change and is often dependent on the environment in which the habits formed (Aarts & Dijksterhuis, 2000; Ouellette & Wood, 1998; Wood & Quinn, 2005). A habit is a behavioral tendency to repeat well-practiced acts in response to stable environmental cues (Ouellette & Wood, 1998). A number of health behaviors are independently predicted by the degree to which a behavior is habitually performed, even after controlling for important variables, such as the intention to perform the behavior (Ouellette & Wood, 1998). Once habits are developed, environmental cues automatically prompt habitual behaviors. Clearly, environmental modification is critical to habit formation and disruption. After developing a habit, an individual can forgo a laborious, rational, contemplative decision in favor of a quick, automatic, and effortless habitual response to engage in healthy behavior.
An approach to weight loss that targets the detrimental impact of the obesogenic environment via modification of the personal eating and physical activity environment, combined with healthy habit formation and unhealthy habit disruption (Carels et al., 2009) has promise. In this investigation, a traditional behavioral weight loss program (LEARN; Brownell, 2004) was compared to a weight loss approach that emphasizes environmental modification as well as habit formation and disruption. It was hypothesized that a weight loss intervention that specifically focused on environmental modification and habit formation and disruption would result in comparable or superior weight loss outcomes when compared to a traditional behavioral weight loss program (i.e. LEARN).
Method
Participants
Fifty-four overweight and/or obese adults responded to advertisements for a weight loss intervention and met study criteria to participate. Participants were recruited through local newspapers, email, and a listserv at a Midwestern university. Participants were included if they were: (a) overweight/obese (BMI ≥ 27 kg/m2); (b) nonsmokers; and (c) free from cardiovascular disease and insulin dependent diabetes. Participants received no incentives for participating. This investigation received full human subjects review board approval and all participants received their physician's medical clearance prior to starting the intervention. Forty-nine participants completed the weight loss intervention, and 42 participants completed the six-month follow-up assessment.
Most participants were Caucasian (83.3%; N = 45) and female (79.6%; N = 43). Mean age of participants was 47.3 (SD = 11.2). Annual income exceeded $45,000 for approximately 66.6% (N = 36) of the participants and 79.7 % (N = 43) had at least a baccalaureate degree. Mean BMI at baseline was 37.2 (SD = 6.7).
Study design
Prior to the start of the investigation, participants were randomized to the newly developed Transforming Your Life (TYL) program (Carels et al., 2009) or the LEARN weight loss program (Brownell, 2004). The 14-week programs were administered in 90-minute, weekly sessions. All assessments and interventions were conducted by a licensed clinical health psychologist or psychology doctoral students with experience in leading weight loss interventions. Weight assessments were conducted at baseline, post-treatment (week 14), and six months post-treatment (follow-up). Both the TYL and LEARN programs included weekly weight assessments and utilized a combination of didactic instruction, individual activities, and out-of-class assignments. Body weight was measured using a digital scale (BF-350e; Tanita, Arlington Heights, IL) to the nearest 0.1lb. Height was measured to the nearest 0.5 inch using a height rod on a standard spring scale.
Weight loss interventions
LEARN program
The LEARN weight loss approach (Brownell, 2004) is a comprehensive, empirically-supported approach to weight management (Andersen et al., 1999; Wadden et al., 1994). The widely used LEARN program encourages gradually losing weight, progressively increasing physical activity, and decreasing energy and fat intake through permanent lifestyle changes. The program emphasizes: (a) self-monitoring of eating behavior; (b) controlling stimuli associated with eating; (c) physical activity; (d) nutrition education; (e) modifying self-defeating thoughts and negative emotions associated with dieting and body image; (f) setting realistic goals; (g) relationships; and (h) relapse prevention and weight maintenance.
Transforming Your Life (TYL)
The TYL program: (1) teaches participants how to strengthen and maintain healthy habits and disrupt unhealthy habits; (2) enables participants to create a personal food and exercise environment that minimizes exposure to unhealthy eating and sedentary behaviors, increases exposure to healthy eating and physical activity, and encourages automatic responding to goal-related cues; and (3) increases participants' weight loss motivation.
Instruction on forming healthy habits was accomplished by teaching participants how to: (1) develop predictable and sustainable weight loss-related routines; (2) anticipate and minimize potential disruptions to routines; (3) follow performance of weight loss-related behaviors with immediate positive reinforcement; and (4) form implementation intentions where habit-related cues are linked to performance of weight loss promoting behaviors (e.g. ‘If I am craving candy, then I will eat a piece of fruit instead’). Similarly, disruption of unhealthy habits was accomplished by teaching participants to: (1) disrupt/change established routines that support unhealthy habits; (2) make unhealthy behaviors less reinforcing (e.g. make sure unhealthy snacks require substantial preparation, time, and effort); (3) identify/remove triggers for unhealthy habits; and (4) form implementation intentions to perform healthy behaviors in response to cues that have historically signaled unhealthy behaviors.
In addition, individuals were taught to create their personal food and exercise environment in a manner that minimizes unhealthy eating and sedentary behavior cues/choices, maximizes healthy eating and exercise-related cues/choices, and encourages automatic responding to goal-related cues (Bell Roe, & Rolls, 2003; Brownell & Horgen, 2004; Della Valle Roe, & Rolls, 2005; French et al., 2001; Geier, Rozin, & Gheoghe, 2006; Harris et al., 2009; Kral & Rolls, 2004; Nestle, 2004; Rolls, Ello-Martin, & Tohill, 2004; Rolls, Roe, Kral, Meengs, & Wall, 2004b; Sobal & Wansink, 2007; Stroebele & De Castro, 2004; Wansink, 2004; Wansink, Painter, & Lee, 2006; Wansink, Painter, & North, 2005; Wansink & Sobal, 2007; Wansink, & Van Itternum, 2003). Each week, selected environmental factors that have been empirically recognized to influence eating (e.g. salience, variety, serving utensils, abundance, and convenience) were systematically targeted for modification (Bell et al., 2003; Brownell & Horgen, 2004; Della Valle et al., 2005; French et al., 2001; Geier et al., 2006; Harris et al., 2009; Kral & Rolls, 2004; Nestle, 2004; Rolls, Ello-Martin, & Tohill, 2004; Rolls, Roe et al., 2004; Sobal & Wansink, 2007; Stroebele & De Castro, 2004; Wansink, 2004; Wansink & Sobal, 2007; Wansink, & Van Itternum, 2003; Wansink et al., 2005; Wansink et al., 2006).
Finally, to increase and preserve motivation for weight loss through the application of principles from self-regulatory theory (Higgins, 2000), participants engaged in activities during group sessions where their trait regulatory fits (i.e. promotion-focus orientation; prevention-focus orientation) were matched to positive or negative role models, respectively. A promotion-focus orientation represents a concern with the presence and absence of positive outcomes (goal attainment focus), while a prevention-focus orientation represents a concern with the presence and absence of negative outcomes (failure prevention focus). For example, depending on the participant's self-regulatory orientation (promotion versus prevention) (Higgins, 2000), participants were asked to imagine how they might gain the benefits of a healthy lifestyle or avoid the consequences of an unhealthy lifestyle. Participants shared their insights with the group in order to promote group cohesion and adherence.
Self-monitoring
Participants in both the TYL and LEARN groups were instructed to self-monitor dietary intake and were provided with demonstrations of common food measurement procedures and instructions for estimating food portion sizes. Written instructions for measurement estimation were provided to participants as a reference. Participants used the food and beverage calorie guides or Internet dietary analysis programs, such as Calorie King (http://www.calorieking.com) and Nutrition Data (http://www.nutritiondata.com), to estimate energy intake from meals, snacks, and beverages. Participants were further instructed on how to electronically submit (or submit by paper and pencil) daily records of energy intake. Daily self-reported physical activity (type and duration of physical activity not including activity associated with daily living, such as occupational exertion or taking the stairs) and energy expenditure (accelerometer readings for total energy expended (kcal) during consecutive 24 hour periods) were also submitted. No objective assessments of physical exertion (i.e. sweating, heart rate) were performed, and participants were instructed to record all purposeful physical activity, regardless of intensity.
Energy expenditure
Caltrac accelerometers were provided to participants to assess total daily energy expenditure. The Caltrac accelerometer measures vertical acceleration and converts the measurement into an energy expenditure value. Although Caltrac accelerometers have been shown to mildly overestimate the absolute energy cost (i.e. measured VO2) of selected activities, they provide a reliable assessment of total energy expenditure (Balogun, Martin, & Clendenin, 1989; Fehling, Smith, Warner, & Dalsky, 1999).
Data analysis
Baseline differences between the treatment groups, as well as program attrition, were assessed using ANOVA and χ2. ANOVA was also used to compare self-monitoring frequency, energy intake, and energy expenditure between treatment groups. Baseline, post-treatment, and follow-up effects were evaluated using two-way repeated measures ANOVA with treatment group as the between group factor and weight loss as the dependent variable. Intent to treat analyses were performed with baseline weight carried forward to post-treatment and follow-up assessments for all program drop-outs. Data was analyzed using SPSS version 16.0.
Results
Baseline characteristics
Fifty-four participants were randomized to either the TYL (N = 26) or LEARN (N = 28) program. Forty-nine (90.7%) participants remained in the program through to post-treatment (TYL = 25; LEARN = 24), and 42 (77.8%) participants attended the six-month follow-up (TYL = 21; LEARN = 21). There were no significant differences between TYL and LEARN participants in attrition or baseline demographics (i.e., age, marital status, gender, education, income, race) including BMI. Similarly, there were no significant differences between program completers and drop-outs on any demographic factors, including baseline weight.
Treatment outcomes
Overall, participants provided, on average, 53.8 (SD = 39.1) of 98 potential caloric intake and physical activity diaries over 14 weeks (54.1%). Participants reported an average daily energy intake of 1736 kcal (SD = 473), an average energy expenditure of 2501 kcal (SD = 332), and an average energy expenditure from physical activity of 616 kcal (SD = 182). Participants reported an average exercise duration of 29.5 minutes (SD = 22.0) for each bout of purposeful exercise. There were no differences between TYL and LEARN participants on self-monitoring frequency or energy intake and expenditure (see Table 1).
Table I. Comparison of self-monitoring and energy intake and expenditure between TYL and LEARN participants.
| Factors | TYL M (SD) |
LEARN M (SD) |
Total M (SD) |
|---|---|---|---|
| Self-monitoring frequency (14 wks) | 53.3 (39.9) | 54.2 (39.3) | 53.8 (39.1) |
| Caloric intake (daily) | 1680 (433) | 1779 (504) | 1736 (473) |
| Caloric expenditure (kcal/daily) | 2490 (353) | 2509 (322) | 2501 (332) |
| Activity expenditure (kcal/daily) | 605 (182) | 624 (186) | 616 (182) |
| Exercise minutes | 31.5 (23.8) | 27.9 (20.9) | 29.5 (22.0) |
Notes: TYL=TransformingYour Life.
No significant differences between groups on any factors
Repeated measures ANOVA1 indicated a significant overall treatment effect for weight (lbs), F (1, 46) = 33.29, p < .001, (Fig. 1). Participants weighed significantly less at post-treatment, t(53) = 8.3, p < .001, (M = 11.9, SD = 10.5) and follow-up, t(53) = 6.3, p < .001, (M = 8.6; SD = 10.8) than at baseline. The increase in weight between post-treatment and follow-up was significant, t(53) = -2.6, p = .012, (M = -3.3, SD = 9.2).
Figure I.
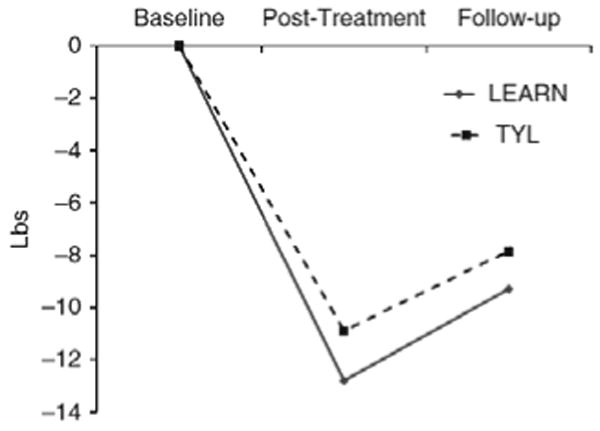
Weight change from baseline to follow-up in LEARN and TYL groups.
The group by treatment interaction effect was not significant, F (1, 52) =.22, p = .80. There were no significant differences between TYL and LEARN participants in weight loss between baseline and post-treatment, F (1, 52) = .42, p = .52, (TYL: M = 10.9, SD = 10.8; LEARN: M = 12.8, SD = 10.4), baseline and follow-up, F (1, 52) = .29, p = .59, (TYL: M = 7.8, SD = 12.0; LEARN: M = 9.3, SD = 9.7), and post-treatment and follow-up, F (1, 52) = .01, p = .91, (TYL:M = -2.1, SD = 8.9; LEARN: M = -3.3, SD = 9.2).
Discussion
This investigation compared a traditional behavioral weight loss program with a weight loss intervention emphasizing environmental modification, healthy habit formation, and unhealthy habit disruption. Participants lost, on average, 5.3 percent total body weight during the 14-week programs. There was a 1.4 percent total body weight regain during the six-month post-treatment follow-up period. Weight loss during and following treatment were equivalent for the LEARN and TYL interventions.
Research suggests that individuals can and do lose weight utilizing interventions with varying modalities and intensities (Klem, Wing, McGuire, Seagle, & Hill, 1997). Therefore, a weight loss approach that emphasizes environmental modification, healthy habit formation, and unhealthy habit disruption, may offer an attractive option for individuals desiring an alternative approach to weight loss. While it is unlikely that one treatment approach will provide all individuals interested in losing weight with the tools they need to initiate and maintain successful weight control, it appears that programs such as TYL may be preferred or offer added benefits to participants.
Generally speaking, the LEARN program is a high quality behavioral weight loss program that broadly emphasizes a number of factors that may influence weight loss, including modifying self-defeating thoughts and negative emotions associated with dieting and body image, setting realistic goals, relationships, relapse prevention and weight maintenance, etc. In contrast, the TYL program is much narrower in focus, concentrating almost exclusively on modifying critical aspects of today's obesogenic environment. Anecdotally, participants mentioned that they appreciated the step-by-step guide to transforming their eating and physical activity environments as well as the support in breaking unwanted habits and replacing them with healthy habits.
The TYL program employs principles that are consistent with stimulus control and behavioral modification techniques found in the LEARN program as well as other behavioral weight loss programs. In addition, the TYL program employs principles that are consistent with models that explicate the conditions by which associations form between representations in the environment (e.g. situations, settings) and goal pursuits (Bargh & Chartrand, 1999), as well as how behavior is impacted by automatic or impulsive influences (Hofmann, Friese, & Wiers, 2008). The primary aim of the TYL intervention is to modify participants' personal obesogenic food and physical activity environments in a manner that encourages healthy eating and an active lifestyle. For example, participants learn how conscious and automatic aspects of the environment can greatly influence behavior, motivation, and self-regulatory resources. They are taught to thoroughly evaluate all aspects of their personal eating and physical activity environments and systematically modify the environment to encourage healthy behaviors and discourage unhealthy behaviors. Each week participants follow and complete an Environmental Modification checklist to transform aspects of their environments. In addition, participants are taught to systematically form healthy habits and disrupt unhealthy habits.
Several study limitations should be mentioned regarding the TYL intervention. For example, it is unclear whether participants were able to effectively modify their environments and which areas of environmental change were most effective at producing weight loss. Evidence of participants' environmental modification was based on anecdotal discussions that occurred during the treatment groups; therefore, it is possible that participants did not comply with program recommendations, thus limiting the intervention's potential effectiveness. It is also unclear if the strategies emphasized in the TYL intervention sufficiently or appropriately addressed the problems inherent in living within an obesogenic food and physical activity environment. Well validated measures of the personal food and physical activity environments are needed to answer these questions.
Additional limitations in this investigation include the composition of the small sample (primarily Caucasian females), as well as potential redundancy between the LEARN and TYL intervention components (e.g. self-monitoring, nutrition education). It is possible that the small homogenous sample or the comparability of the two interventions on important features such as self-monitoring, masked potential group differences that might have otherwise emerged.
The current investigation has several clinical implications. The personal eating and physical activity environments that people frequently encounter likely contain numerous conscious and unconscious cues to eat or engage in sedentary behaviors. Similarly, unhealthy habits can be challenging to break and healthy habits challenging to establish. As such, individuals are likely to benefit from instruction on how to create personal food and physical activity environments that minimize unhealthy food-related decisions/exposure and maximize healthy food-related decisions/exposure. In addition, given the regularity in which individuals participate in food-related and sedentary activities, these behaviors are important targets for the establishment of healthy habits.
There is some evidence that alternative approaches to weight loss, such as environmental modification, habit formation, etc., might improve outcomes among individuals who are initially unsuccessful at losing weight on their own (Carels et al., 2009). Matching individuals based on pre-existing conditions, preference for type and modality of treatment, and likelihood for success with strategies that best fit a particular individual's weight loss needs and goals, may maximize therapeutic outcomes (Wadden, Brownell, & Foster, 2002). Future research is needed to determine whether specific baseline characteristics predispose people to benefit more from an environmental approach to weight loss versus a more traditional behavioral weight loss approach.
Despite the failure of the TYL intervention to demonstrate superior weight loss treatment outcomes as compared to the LEARN program, the TYL intervention may be viewed as an alternative approach to a traditional behavioral weight loss program. It is clear that the current obesogenic environment has the potential to hinder weight management efforts. Thus, individuals may benefit from programs, such as TYL, that address their interactions with and behaviors within the obesogenic food and physical activity environment.
Biographies
Robert A. Carels, PhD, MBA is Associate Professorand Vice Chair Graduate Studies in the Psychology Department at Bowling Green State University, Ohio. With his fellow authors, recent articles include ‘Implicit, explicit, and internalized weight bias and psychosocial maladjustment among treatment-seeking adults’, Eating Behaviors (in press, co-authored with Wott, Young, Gumble, Koball, and Oehlhof), ‘Weight bias and weight loss treatment outcomes in treatment-seeking adults’, Annals of Behavioral Medicine (2009, co-authored with Young, Wott, Harper, Gumble, Oehlof, and Clayton), and ‘Successful weight loss with self-help: A stepped-care approach’, Journal of Behavioral Medicine (2009, co-authored with Wott, Young, Gumble, Darby, Oehlof, Harper, and Koball).
Kathleen M. Young is a doctoral student in the Department of Psychology, Bowling Green State University
Afton Koball is a doctoral student in the Department of Psychology, Bowling Green State University
Amanda Gumble is a doctoral student in the Department of Psychology, Bowling Green State University
Lynn A. Darby is a Professor in the Departmentof Kinesiology, Bowling Green State University
Marissa Wagner Oehlhof is a doctoral student in the Department of Psychology, Bowling Green State University
Carissa B. Wott is a doctoral student in the Department of Psychology, Bowling Green State University
Nova Hinman is a doctoral student in the Department of Psychology, Bowling Green State University. Her interests focus on weight loss treatment outcome research and weight stigma research.
Footnotes
Competing Interests: None declared.
Some evidence suggests that General Linear Mixed Models may be slightly preferable for intent-to-treat clinical trial data. Therefore, we confirmed our findings using Generalized Estimating Equations in SPSS. The findings were essentially identical (i.e. a very strong within-person effect for weight change and a non-significant between-group effect for weight loss group). Given the widespread use of repeated-measures in weight loss treatment outcome research, its universal familiarity to readers, and its comparability to previous research, we elected to report the findings using repeated-measures ANOVA.
References
- Aarts H, Dijksterhuis A. Habits as knowledge structures: Automaticity in Goal-Directed Behavior. Journal of Personality and Social Psychology. 2000;78:53–63. doi: 10.1037//0022-3514.78.1.53. [DOI] [PubMed] [Google Scholar]
- Andersen R, Wadden T, Bartlett S, Zemel B, Verde T, Franckowiak S. Effects of lifestyle activity vs. structured aerobic exercise in obese women. JAMA. 1999;281:335–340. doi: 10.1001/jama.281.4.335. [DOI] [PubMed] [Google Scholar]
- Balogun J, Martin D, Clendenin M. Calometric validation of the Caltrac Accelerometer during level walking. Physical Therapy. 1989;89:501–509. doi: 10.1093/ptj/69.6.501. [DOI] [PubMed] [Google Scholar]
- Bargh JA, Chartrand TL. The unbearable automaticity of being. American Psychologist. 1999;54:462–479. [Google Scholar]
- Bell EA, Roe LS, Rolls BJ. Sensory-specific satiety is affected more by volume than by energy content of liquid food. Physiology and Behavior. 2003;78:593–600. doi: 10.1016/s0031-9384(03)00055-6. [DOI] [PubMed] [Google Scholar]
- Brownell KD. The LEARN Program for weight management. 10th. Dallas, Texas: American Health Publishing Company; 2004. [Google Scholar]
- Brownell KD, Horgen KB. Food fight: The inside story of the food industry, America's obesity crisis, and what we can do about it. Chicago: Contemporary Books; 2004. [Google Scholar]
- Carels RA, Wott CB, Young KM, Gumble A, Darby LA, Oehlhof MW, et al. Successful weight loss with self-help: A stepped-care approach. Journal of Behavioral Medicine. 2009;32:503–509. doi: 10.1007/s10865-009-9221-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Della Valle DM, Roe LS, Rolls BJ. Does the consumption of caloric and non-caloric beverages with a meal affect energy intake? Appetite. 2005;44:187–193. doi: 10.1016/j.appet.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Fehling P, Smith D, Warner S, Dalsky G. Comparison of accelerometers with oxygen consumption in older adults during exercise. Medicine & Science in Sports & Exercise. 1999;31:171–175. doi: 10.1097/00005768-199901000-00026. [DOI] [PubMed] [Google Scholar]
- French SA, Story M, Jeffrey RW. Environmental influences on eating and physical activity. Annual Review of Public Health. 2001;22:309–335. doi: 10.1146/annurev.publhealth.22.1.309. [DOI] [PubMed] [Google Scholar]
- Geier AB, Rozin P, Gheoghe D. Unit bias: A new heuristic that helps explain the effect of portion size on food intake. Psychological Science. 2006;17:521–525. doi: 10.1111/j.1467-9280.2006.01738.x. [DOI] [PubMed] [Google Scholar]
- Gollwitzer PM, Bargh JA. Automaticity in goal pursuit. In: Elliot AJ, Dweck CS, editors. Handbook of competence and motivation. New York: The Guilford Press; 2005. pp. 624–646. [Google Scholar]
- Harris JL, Bargh JA, Brownell KD. Priming effects of television food advertising on eating behaviors. Health Psychology. 2009;28:404–413. doi: 10.1037/a0014399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ET. Making a good decision: Value from fit. American Psychologist. 2000;55:1217–1230. [PubMed] [Google Scholar]
- Hofmann W, Friese M, Wiers RW. Impulsive versus reflective influences on health behavior: A theoretical framework and empirical review. Health Psychology Review. 2008;2:111–137. [Google Scholar]
- Klem M, Wing RR, McGuire M, Seagle H, Hill J. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. American Journal of Clinical Nutrition. 1997;66:239–246. doi: 10.1093/ajcn/66.2.239. [DOI] [PubMed] [Google Scholar]
- Kral TVE, Rolls BJ. Energy density and portion size: Their independent and combined effects on energy intake. Physiology & Behavior. 2004;82:131–138. doi: 10.1016/j.physbeh.2004.04.063. [DOI] [PubMed] [Google Scholar]
- Lowe MR. Self-regulation of energy intake in the prevention and treatment of obesity: Is it feasible? Obesity Research. 2003;11:44s–59s. doi: 10.1038/oby.2003.223. [DOI] [PubMed] [Google Scholar]
- Nestle M. Food politics. Berkeley: University of California Press; 2004. [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Ouellette JA, Wood W. Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychological Bulletin. 1998;124:54–74. [Google Scholar]
- Rolls BJ, Ello-Martin JA, Tohill BC. What can intervention studies tell us about the relationship between fruit and vegetable consumption and weight management? Nutrition Reviews. 2004;62:1–17. doi: 10.1111/j.1753-4887.2004.tb00001.x. [DOI] [PubMed] [Google Scholar]
- Rolls BJ, Roe LS, Kral TVE, Meengs JS, Wall DE. Increasing the portion size of a packaged snack increases energy intake in men and women. Appetite. 2004;42:63–69. doi: 10.1016/S0195-6663(03)00117-X. [DOI] [PubMed] [Google Scholar]
- Rothman AJ, Sheeran P, Wood W. Reflective and automatic processes in the initiation and maintenance of dietary change. Annals of Behavioral Medicine. 2010;38:S4–S17. doi: 10.1007/s12160-009-9118-3. [DOI] [PubMed] [Google Scholar]
- Sobal J, Wansink B. Kitchenscapes, tablescapes, platescapes, and food scapes: Influences of microscale built environments on food intake. Environment and Behavior. 2007;39:124–142. [Google Scholar]
- Stroebele N, De Castro JM. Effect of ambience on food intake and food choice. Nutrition. 2004;20:821–838. doi: 10.1016/j.nut.2004.05.012. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Brownell KD, Foster G. Obesity: Managing the global epidemic. Journal of Consulting and Clinical Psychology. 2002;70:510–525. doi: 10.1037//0022-006x.70.3.510. [DOI] [PubMed] [Google Scholar]
- Wadden T, Foster G, Letizia K. One-year behavioral treatment of obesity: Comparison of moderate and severe caloric restriction and the effects of weight maintenance therapy. Journal of Consulting and Clinical Psychology. 1994;62:165–171. doi: 10.1037//0022-006x.62.1.165. [DOI] [PubMed] [Google Scholar]
- Wansink B. Environmental factors that increase the food intake and consumptionvolume of unknowing consumers. Annual Review of Nutrition. 2004;24:455–479. doi: 10.1146/annurev.nutr.24.012003.132140. [DOI] [PubMed] [Google Scholar]
- Wansink B, Painter JE, Lee YK. The office candy dish: proximity's influence on estimated and actual consumption. International Journal of Obesity. 2006;30:871–875. doi: 10.1038/sj.ijo.0803217. [DOI] [PubMed] [Google Scholar]
- Wansink B, Painter JE, North J. Bottomless bowls: Why visual cues of portion size may influence intake. Obesity Research. 2005;13:93–100. doi: 10.1038/oby.2005.12. [DOI] [PubMed] [Google Scholar]
- Wansink B, Sobal J. Mindless eating: The 200 daily food decisions we overlook. Environment and Behavior. 2007;39:106–122. [Google Scholar]
- Wansink B, Van Itternum K. Bottoms up! The influence of elongation on pouring and consumption. Journal of Consumer Research. 2003;30(3):455–463. [Google Scholar]
- Wood W, Quinn JM. Habits and the structure of motivation in everyday life. In: Forgas JP, Williams KD, Laham SM, editors. Social Motivation: Conscious and unconscious processes. New York: Cambridge University Press; 2005. pp. 55–70. [Google Scholar]


