Abstract
Objective
To describe an organization-wide disparity reduction strategy and to assess its success in quality improvement and reduction of gaps in health and health care.
Study Setting
Clalit Health Services, Israel's largest non-for-profit insurer and provider serving 3.8 million persons.
Study Design
Before and after design: quality assessment before and 12-month postinitiation of the strategic plan. A composite weighted score of seven quality indicators, measuring attainment of diabetes, blood pressure, and lipid control, lack of anemia in infants, and performance of mammography, occult blood tests, and influenza vaccinations.
Data Extraction Methods
Quality indicator scores, derived from Clalit's central data warehouse, based on data from electronic medical records.
Principal Findings
Low-performing clinics, of low-socioeconomic and minority populations, were targeted for intervention. Twelve months after the initiation of the project continuous improvement was observed coupled with a reduction of 40 percent of the gap between disadvantaged clinics, serving ∼10 percent of enrollees, and all other medium-large clinics.
Conclusion
The comprehensive strategy, following a quality improvement framework, with a top-down top-management incentives and monitoring, and a bottom-up locally tailored interventions, approach, is showing promising results of overall quality improvement coupled with disparity reduction in key health and health care indicators.
Keywords: Disparities, quality improvement, quality assessment, primary care
The role of health care organizations in reducing inequalities in health has recently drawn considerable interest from researchers and policy makers (McKee 2002; Smedley, Stith, and Nelson 2003;). It is clearly acknowledged that disparities in health are a result of interrelated factors external to the health care realm, such as socioeconomic status (SES), ethnicity, geography, and education (Chin et al. 2007; Starfield and Birn 2007; Benyamini et al. 2008; Riva et al. 2009;), yet health care organizations have an important role in reducing health disparities caused by these social factors, as well as by unequal access to quality medical care (Aaron and Clancy 2003). To address this need, the National Health Plan Collaborative was formed in 2004, aimed at reducing racial and ethnic disparities and improving the overall quality of care in the U.S. health care system. Early reports indicate that the plans have made significant headway in achieving coordination of disparities activities across the organization (Lurie et al. 2008). Yet data on programs' structures and the processes put in place, as well as achievements in disparity reduction, have not been reported to date. The means by which health care organizations can effectively achieve disparity reductions are yet to be unveiled (Fiscella 2007).
Israeli society has a diverse demographic profile in terms of its ethnic, religious, immigrant, and socioeconomic makeup. Recent reports show widening inequalities in economic status, as attested by the higher Gini coefficient (a marker of income variance) in Israel than in all OECD countries (Shmueli and Gross 2001). Recent studies report considerable differences in the health status of the Israeli population (Epstein and Horev 2007): differences in life expectancy according to geographical areas, minority status (mainly between the largest minority of Arab Muslims and the general Israeli Jewish population), and level of education (Shuval 1990; Chernichovsky and Anson 2005; Israeli Bureau of Statistics 2009;); large differences in infant mortality rates according to geographical area and minority status (Tarabeia et al. 2004); and disparities in the prevalence of chronic diseases according to minority status and education level in a variety of conditions, including osteoporosis (Nitzan-Kaluski et al. 2003), obesity (Keinan-Boker et al. 2005), and coronary artery disease (Salameh et al. 2008).
In Israel, all citizens, by law, are members of one of four health funds that serve as insurers and health care providers. Clalit Health Services is the largest health fund with over 3.8 million enrollees (53 percent market share), with <4 percent annual shifts between health funds, mainly of younger more affluent urban populations. Clalit has a significant overrepresentation of the underprivileged: low-socioeconomic groups, minorities, new immigrant (mainly overrepresentation of persons who immigrated from Ethiopia), residents of rural areas, the elderly, and people with disabilities (Horev and Kop 2008). Over the years, Clalit has gained experience in many sporadic efforts directed at improving the health status of these disadvantaged populations, including improving access to care, health education, health promotion, and cultural competency initiatives (Nirel, Pilpel, and Rosen 2000; Maislos, Weisman, and Sherf 2002;).
In recent years, Clalit has developed advanced quality measurement and quality improvement initiatives for better quality of care for its patient population (Goldfracht and Porath 2000; Peleg et al. 2008;). To further address the needs of diverse population groups, Clalit, with a network of over 1,500 primary and secondary care clinics, and 14 hospitals, unfolded in 2008 its first organization-wide strategic plan to reduce inequalities in health and health care. Jones, Trivedi, and Ayanian (2010) recently report on organizational factors that contribute to success in disparity reduction: organizational commitment, population health focus, use of data to inform solutions, and a comprehensive approach to quality improvement. These factors are in fact an integral part of the Clalit initiative, with strong leadership support (by the director general and all top management staff), and an integrative approach, which comprises many of the medical home attributes (Carrier, Gourevitch, and Shah 2009), including a unique data warehouse that contains detailed “cradle to crib” data (demographic, health indicators, and health care services utilization data); a large primary care—public-health-oriented workforce in the local communities; and an extensive set of quality measurement tools, based on data from a universal system of electronic medical records. Additionally, this new disparity-reduction strategy builds on Clalit's primary care orientation as a major force for driving disparity reduction (Shi et al. 2002).
The two main components of the strategy are (1) a top-down approach of disparity-reduction goal setting, continuous monitoring, and provision of incentives; and (2) use of tailored interventions to reduce disparities by a bottom-up approach in which each district and locality is empowered to plan interventions, policy changes, and shifts in workforce. Findings on the initial implementation efforts and their results are presented.
METHODS
The Disparity Reduction Strategy—Overview
Clalit's existing quality improvement processes were, to the point of the initiation of the disparity-reduction strategy, generic. The new strategy, aimed at closing quality gaps and not merely achieving improvement, began with the development of a set of targeted indicators to serve as the foci of the plan. The strategy involves the following main steps: selecting quality indicators, rating the primary care clinics, selecting target clinics for intervention, setting goals, providing feedback and support to district steering committees for suggested interventions, continuous monitoring, and incentives. Following is a detailed description of this process.
Selecting Quality Indicators
A panel of physicians, nurses, and senior public-health professionals examined the 70 health care quality indicators currently used at Clalit as part of ongoing quality measurement and improvement processes, to determine their inclusion as disparity indicators. Data on percent attainment of each indicator were based on annual percent attainment recorded at the second quarter of 2008. In the first phase of the selection process, the 70 indicators were ranked by level of disparity between high- and low-socioeconomic populations within Clalit. Disparity level was assessed by the ratio of high-to-low SES populations in the indicator score (percent attainment). SES levels were defined by means of geocoding techniques (Fremont et al. 2005), by linking the address of the primary care clinic serving the individual with the Census area-level SES data, based on the ratings of Israel's Central Bureau of Statistics (Israeli Bureau of Statistics 2009).
In the first stage, indicators for which the high-to-low SES ratio was above 1.1 (>10 percent difference) were included. In the second stage, the selected set of measures was further limited by several inclusion criteria: (1) reflect evidence-based high-impact medical care, (2) pertain to large segments of the population in various age groups, (3) focus on prevention (primary and secondary), and (4) are representative of processes and outcomes of care. The third stage involved the examination of other types of disparities in health care, namely differences according to minority status and overall differences in performance between high- and low-performing clinics.
Scoring of Primary Care Clinics
Each indicator selected was assigned a weight, through a consensus reached by the steering committee, to reflect its relative importance with respect to the organization's overall goals in quality improvement. For example, diabetes control was assigned the highest weight (25 percent) to reflect the over 10-year ongoing organizational focus on diabetes control (Goldfracht and Porath 2000). A composite weighted performance score, termed the Quality Indicator Disparity Scale (QUIDS), was constructed to reflect attainment of all selected indicators. Scale score was transformed to a 0–100 scale, with a higher score representing higher quality care. All 436 medium-large clinics, serving about 2.2 million persons, were rated on the QUIDS. The unit of analysis is the clinic as scores indicate average clinics' quality indicator attainment in the QUIDS measures.
Selection of Target Clinics for Intervention
We limited the selection and measurement process to include clinics with at least 25 persons for each of the QUIDS indicators. This resulted in selection of medium and large primary clinics, which each serve at least 1,500 enrollees—a total of 381 clinics that provide care to 60 percent of Clalit's enrollees. Each of the primary care clinics was assigned a QUIDS score.
The lowest performing clinics in each of Clalit's eight districts (10 percent lowest QUIDS score or 10 percent lowest scores in at least three individual measures) were designated as target clinics for intervention. After the selection process was set, a district steering committee at each of Clalit's eight districts reviewed the lists and ascertained that the selection of clinics was indeed representative of the main foci of quality care disparities in the district.
Setting Goals and Incentives
For each district, target QUIDS scores were set for the low-performing clinics as follows. Based on the preceding 2 years average QUIDS scores of the district's clinics, linear trend lines were calculated to predict the average future district QUIDS score for 2 years into the project, for each district. The ambitious goal of the low-performing clinics was set at this predicted district performance level, to be reached by the low-performing clinics 2 years hence (targeted at closing the quality gap in relation to all other clinics). Mid-term targets to be met within 12 months were also set. Financial incentives for reaching these annual goals were set at approximately 1 percent of the total district budget, to be divided by the districts according to the relative percentage of the goal achieved. An additional bonus was also affirmed for improvement over and above the set goals at the end of year 1 and year 2. It should be noted that unlike pay-for-performance schemes the incentives are provided at the district level and are not directly allotted to the clinics, nor are they designated for direct remuneration of the staff.
Intervention Programs Planning and Audit
The means by which low-performing clinics could achieve the preset quality improvement targets were determined by a bottom-up approach. The planning process was initiated at a conference for all district and subdistrict management-level administrators held in September 2008, at which the program was introduced. Each district, serving between 300,000 and 700,000 enrollees, received a report of their QUIDS scores, their 2-year goals, guidance on evidence-based approaches to disparity reduction, and peer presentations of successful implementation of such interventions to that date.
Following the conference, each district initiated an internal planning process, working with the subdistrict managers and clinic managers, each serving 5,000–14,000 persons, to construct a tailored set of interventions relevant to each targeted clinic. A managerial headquarters-level steering committee was nominated to review the plans and allow peer learning between the districts. Implementation of interventions began during November–December of 2008. Each district was asked to complete a detailed report on the types of interventions that were implemented. The reports were reviewed by two of the authors separately (R. B. and E. S.) and key types of interventions were extracted. Disagreements on classifications of types of interventions were discussed and resolved.
Continuous Monitoring and Analysis
Quality improvement and disparity reduction in each district are periodically assessed. The outcomes of the program, as measured by the changes in QUIDS scores between the preintervention stage (December 2008) to the 12-month follow-up (November 2009), and specific quality indicators at the district level and in each of the low-performing clinics, are periodically communicated to the districts. Trend line analysis of change in QUIDS scores between pre- and postintervention initiation periods is performed to assess statistically significant differences. This allows continuous monitoring and improvement according to feedback (a management-by-objectives approach) (Rodgers and Hunter 1991).
RESULTS
Selecting Quality Indicators
The indicator selection process resulted in the selection of seven quality indicators out of the 70 available measures. Table 1 shows the high-to-low SES ratio, demonstrating that large disparities existed between high- and low-SES populations in six of the seven indicators. The seventh measure, fecal occult blood tests, was selected due to wide variations among clinics in its performance, as well as a high mark in the other selection criteria. These results present that larger than 10 percent differences were observed between lower and higher SES populations, meeting the first criteria of the indicator selection process described above. The lipid control was determined as LDL<100 mg/dl for all patients in accordance with organizational medical guidelines at the time of the project. Anemia in infants was determined by the highest hemoglobin level if multiple measures were available. Target populations for influenza vaccination include all persons age 65 and older and younger persons with at least one of 34 chronic conditions, as indicated in Clalit's chronic disease registry. Assigned weights for each indicator ranged from 25 percent assigned to diabetes control to 10 percent assigned to performance of occult blood tests (Table 1).
Table 1.
Performance of Seven Selected Quality Indicators
| Performance Ratio in High- versus Low-SES Populations* | Assigned Weights (%) | |
|---|---|---|
| Diabetes control: Percentage of all known diabetes patients with HbA1c<9% | 1.43 | 25 |
| Blood pressure control: Percentage of all known hypertensive patients with blood pressure at or below 160/100 mmHg | 1.26 | 10 |
| Lipids control: Percentage of all known hyperlipidemia patients with LDL<100 mg/dl | 1.13 | 10 |
| Anemia prevalence in infants: Percentage of infants age 9–18 months with hemoglobin above 105 g/l | 1.34 | 15 |
| Influenza immunization rate: In target populations (>65 years of age or chronically ill) | 1.47 | 15 |
| Mammography tests rates: Once every 2 years, for women aged 50–75 | 1.19 | 15 |
| Occult blood tests: Once every year for persons aged 50–75 | 2.37† | 10 |
Performance in clinics with high- versus low-SES populations, adjusted for patients' age.
Performance ratio in clinics with 90% highest performance versus lowest 10% performance.
SES, socioeconomic status.
Selection and Scoring of Primary Care Clinics
Fifty-five low-performing clinics, which serve 10 percent of Clalit's total population (∼390,000 enrollees), were selected for the project. Average district QUIDS scores were, on a scale of 0–100, 56 points (standard deviation [SD]: 4) and 63 QUIDS points (SD: 4) for target clinics and all other clinics, respectively. The characteristics of the 55 target clinics versus all other medium-large clinics are presented in Table 2. As expected by the selection process, target clinics were significantly more likely to serve patients of low SES and to be clinics serving minority populations. Some clinics serving underprivileged populations, however, were high performers—in QUIDS score and in most other quality measures.
Table 2.
Sociodemographic Characteristics and Quality Indicator Score of Target Clinics Compared with All Other Medium-Large Clinics
| Target Clinics | All Other Clinics | p-Value† | |
|---|---|---|---|
| N | 55 | 326 | |
| Clinics serving low-SES populations* | 45 (82%) | 156 (48%) | <.001 |
| Clinics serving minority populations‡ | 41 (74%) | 108 (33%) | <.001 |
| Average QUIDS score (SD) | 56 (4) | 63 (4) | <.05 |
SES determined by linking the address of the primary care clinic serving the individual with the Census area-level SES data, based on the ratings of Israel's Central Bureau of Statistics.
p-Values derived from T-tests for continuous variables and χ2-test for categorical variables.
Minority status determined by Clalit clinic database characterizing the main catchment area of the clinic according to defined groups of populations residing in that area (particularly two types of minority groups are identified: clinics serving Arab or ultraorthodox Jewish minority populations).
QUIDS, Quality Indicator Disparity Scale; SD, standard deviation; SES, socioeconomic status.
Intervention Programs Review
District steering committees were presented with data on performance of each indicator in the target clinics as compared with all other clinics in their district. Each committee formulated a plan for quality improvement and disparity reduction. From the detailed reports provided by each district's medical manager three key types of interventions emerged: enhancement of teamwork and local leadership, improving access to services, and development of cultural competency programs. Teamwork and local leadership interventions include enhancement of managerial and leadership skills and designation of key personal to lead improvement in each (or several) of the target indicators. For example, clinic managerial teams participated in leadership skill building workshops, regular multidisciplinary team meetings were initiated in clinics where they were not an integral part of the clinics' routine, and clinic staff members were designated as champions of key health issues (e.g., promoting adherence to occult blood testing by the head nurse). Improved accessibility initiatives include increasing access to preventive services (e.g., mobile mammography units) and outreach initiatives to identify and summon patients for recommended preventive and follow-up services. Specifically, clinics scheduled 2–3-hour periods each week for proactive preventive and chronic care management visits, and some clinics prolonged opening times to allow for before and after hour services for working adults. Cultural competency interventions, including translation and cultural mediators' services and involvement of religious leaders in tailoring culturally appropriate health promotion messages. For example, some clinics serving minority Muslim populations created partnerships with local religious leaders who subsequently incorporated health promotion messages in their sermons, including direct calls for people to go get their influenza vaccination or on the importance of early cancer screening.
To enhance organizational peer-learning capabilities, high-performing clinics responsible for underprivileged populations were identified, and their key success stories and effective practices were communicated to low-performing clinics. Main challenges for implementation reported by regional and local managements on steering committee meetings were staff constraints (e.g., when a staff member is on leave there is no replacement and clinics need to adjust to periods of understaffing); lack of additional funding (districts had to initiate interventions within the limits of their current budgets); and burden of requirements for meeting all targets (additionally to the seven indicators on focus for the disparity reduction project clinics are still measured on their success in meeting the usual 70 quality indicators each of Clalit clinics is accounted for).
A comprehensive evaluation process to collect detailed data on the interventions used by each target clinic was initiated. Districts' steering committees and target clinics were asked to complete case-study reports on the features of each intervention. This detailed evaluation is currently ongoing.
Continuous Monitoring
For each district a target QUIDS score was set according to the above method. Targets for low-performing clinics were set at 3–6 percentage points improvement in QUIDS scores 24-month postprogram initiation in each district. Accordingly, 12-month mid-term targets for low-performing clinics were calculated for each district, and disparity reduction target scores were ascertained. These targets were set to reflect a trend toward closure of the quality gap, with the aim of closing the gap entirely within 2 years.
Figure 1 depicts the process of setting target scores. The average QUIDS scores during the 12-month period (fourth quarter 2007–fourth quarter 2008) in District I is presented by annual quarter. Point A reflects the time at which the indicator selection process, rating of clinics, and selection of target clinics for intervention occurred. Point B indicates the official organization-wide project initiation. Points C and D represent the average mid-term target scores for the target clinics and the predicted score for all other clinics in District I, respectively.
Figure 1.
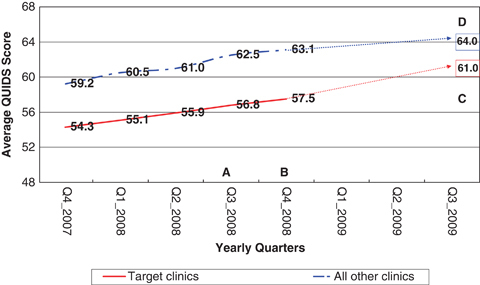
Target Setting for the Quality Indicator Disparity Scale (QUIDS) Score—District I
A, measurement selection—selection of indicators and targeted clinics for intervention; B, project initiation—presentation of measures, target clinics, and QUIDS goals; C, trend line mid-term (12 month) predicted QUIDS score in all (nontarget) medium-large clinics in the district. This value was used to determine the target scores for low-performing clinics; D, target mid-term QUIDS score for target clinics.
The figure shows that in this district, before the initiation of the project, a trend toward improvement in quality was observed for target clinics and for all other clinics. A trend of overall quality improvement with no significant narrowing of the gap was evident in five of Clalit's eight districts. In one of the remaining three districts, while overall quality scores improved for target and for all other clinics, a trend toward widening of the gap was observed. For the remaining two districts, before the initiation of the project, a modest decrease in the gap was observed, coupled with overall improvement in quality.
Initial Results
Figure 2 shows the average change in QUIDS score for July 2008–November 2009. Overall quality score improved in all nontarget clinics, from an average of 62.9 in July 2008 to 64.9 in November 2009. Target clinics improved at a faster rate—from a low of 56.3 in July 2008 to 60.8 in November 2009. The figure depicts change between two periods: before the interventions took effect and 12 months after the initiation of interventions. We allowed for a 3-month planning and implementation stage (between September 2008, project kickoff and December 2008 when clinics had begun full implementation of organizational changes and interventions). As evident from the figure, the average difference in QUIDS score between the target clinics and all other clinics remained constant between June 2008 and December 2008, at a 6.5–6.7 point difference. During the first 12 months of the intervention the average difference in QUIDS score narrowed to 4.07 QUIDS points; that is, at 12 months attainment of about 40 percent of the preset 24-month zero gap target. As depicted in Figure 2, average change (as indicated by trend line slope) for all nontarget clinics remained similar for the pre- and postproject initiation periods and ranged between 0.093 and 0.128. Conversely, target clinics improved at a 3.25 times faster rate in the post- versus preintervention periods (slope 0.348 and 0.107, respectively, p<.05).
Figure 2.
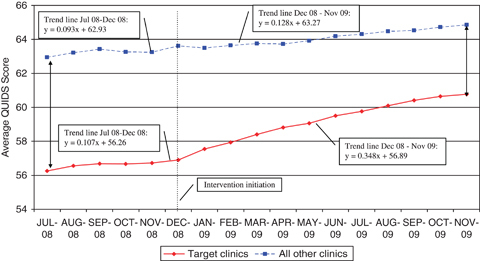
Change in QUIDS Score: Target Clinics and All Other Clinics
Vertical line indicating intervention initiation (after 3 months phase-in).
It should be noted that gaps were measured as the actual difference in score between the lowest performing clinics and all other clinics, rather than the difference between the lowest performing clinics and the target score (i.e., the predicted average future district QUIDS score for 2 years into the project, as described in “Methods”). Although all districts continued to improve in overall QUIDs score, for some districts, the trend line used to determine expected increase in overall performance in nontargeted clinics proved inaccurate, and these target scores were thus deemed by the steering committee as too ambitious of a goal (as these districts were the highest performers, they have reached a bend in the improvement curve).
For each of the individual quality indicators, greater improvement was observed in the target clinics than in all other clinics. The greatest improvement in individual quality indicators was observed for the performance indicators, in the target clinics and in all other clinics, respectively: performance of occult blood tests: 28.4 percent (SD: 10.2) and 13.3 percent (SD: 3.3); influenza immunization: 23.2 percent (SD: 28.3) and 1.3 percent (SD: 1.7); and performance of mammography tests: 9.8 percent (SD: 8.9) and 3.3 percent (SD: 5.1). Improvement in outcomes was more modest: diabetes control 4.0 percent (SD: 2.3) and 1.5 percent (SD: 1.1); blood pressure control: 3.4 percent (SD: 1.6) and 1.5 percent (SD: 0.8); and anemia in infants: 1.1 percent (SD: 1.4) and 0.0 percent (SD: 0.9) in target clinics and in all other clinics, respectively. Lipid control improved by 3.8 percent (SD: 11.3) in the target clinics and, on average, changed for the worse in all other clinics (−6.7 percent, SD: 4.4).
DISCUSSION
This study is unique in that it presents a large-scale organization-wide systematic process of disparity reduction based on quality improvement methodologies (General Accounting Office 2003; Fiscella 2007;). Previous studies have shown the benefits of organization-wide quality improvement strategies (Ornstein et al. 2008), yet universally applied quality improvement efforts do not necessarily reduce disparities (Trivedi et al. 2005; Sequist et al. 2006;) because strong populations tend to absorb the interventions earlier and to a larger extent, potentially increasing the care quality gap. The strategy presented here aimed to overcome this barrier by implementing a dual approach of focusing organizational efforts at the most challenged clinics. The initial 12 months of the intervention show that quality improvement coupled with disparity reduction is attainable.
Experience of other countries and health care systems shows that reducing disparities is much more than just a matter of access, and that even when universal access is available differences in processes and outcomes are found (Shih, Zhao, and Elting 2006; Schnittker and Bhatt 2008; Smedley 2008;). Data presented here for the period before the initiation of the project support the above claim and show that despite overall improvement of quality scores in all clinics (including target clinics), at the preintervention period gaps in quality remained constant. The initial results of Clalit's disparity reduction strategy show that reduction of disparities can be achieved by using an organization-wide plan. The principles of Clalit's strategy are in line with the framework depicted by Jones, Trivedi, and Ayanian (2010), who characterized the main organizational attributes of effective disparity reduction programs:
Organizational commitment: The strategic plan was declared one of the key strategies used by the organization, with progress reports provided to the director general and financial incentives provided to districts for meeting target goals.
Population health focus: To reach disadvantaged populations several approaches were implemented, including identifying and responding to health problems at a community level, and partnering with local religious and community leaders. Additionally, a focus on population health included using chronic disease registries to reach out to people and initiate preventive or care management visits.
Use of data to inform solutions: Measurable targets for disparity reduction were set, constituting a comprehensive, yet manageable set of measures that are aligned with organizational priorities and pertain to large segments of the population.
Comprehensive approach to quality: In line with lessons from other initiatives for reducing disparities (Chin et al. 2007), Clalit's districts and localities implemented multicomponent interventions, including culturally tailored quality improvement and local solutions for local challenges in improving access to and utilization of services. Additionally, ongoing assessment and learning took place; an organization-wide learning process was initiated, including cross-organizational learning through presentation of successful interventions at joint meetings as well as an ongoing comprehensive evaluation.
Moreover, the Clalit strategy builds on the organization's strong primary care orientation and on the premise that health services can contribute to reductions in inequity in health care (Mackenbach 2003), particularly when primary care services are explicitly considered (Starfield, Shi, and Macinko 2005). The strategy focuses on key primary care enhancement interventions, including support for primary care clinics' initiatives, endorsement of primary care-level leadership building capacities and outreach programs.
The strategy developed and carried out by Clalit follows many of the principles suggested by researchers from the United States and other countries, as described above. Thus, we believe it is applicable to other health care organizations. As health care organization assume the roles of medical homes (Carrier, Gourevitch, and Shah 2009), many of the structures and processes put in place as part of the Clalit strategy are applicable to such settings and can be implemented as part of the organizations' overall quality improvement schemes. It should be noted that while different organization may chose to focus on different quality measures, the indicator selection process described here follows two important principles: First, the indicators were selected so as to reflect actual disparities between population groups. We selected health aspects for which there was a documented difference between clinics serving low- and high-socioeconomic populations. In that sense the project's core is reducing disparities and not merely improving the quality of care in low-performing clinics. Second, to address a wide array of health states, the project does not focus only on one disease (such as diabetes); rather it addresses several key conditions and preventable health states.
Limitations
There are several limitations to the disparity-reduction strategy reported here. First, although financial and organizational barriers reduce access to health care services and may significantly contribute to health care inequalities (Lasser, Himmelstein, and Woolhandler 2006), the strategy does not focus on major reallocation of health care resources. Nonetheless, targeted interventions for improving access to care are used at the local level (e.g., improved access to mammography testing units). Additionally, the measures at the foci of this strategy relate to services for which there are no copayments at the point of care (primary care services, immunizations, and screening tests that are included in the selected measures), yet significant disparities in their attainment by SES have been observed, indicating the importance of reasons other than direct financial access for the observed inequalities.
Our strategy combined both process and outcome measures, yet most of the observed improvements in the QUIDS scores are due to change in process indicators. Only modest improvement was observed in this early period following the intervention for diabetes, blood pressure, lipid control, or anemia in infants. It should be noted, however, that contrary to findings by others (Sequist et al. 2006) our results indicate greater change in target versus all other clinics in process as well as in outcome measures.
Another limitation is that this study did not examine the direct mechanisms by which disparity reductions are achieved. As cultural competency, as well as other types of interventions, vary greatly between groups and localities (Betancourt et al. 2005), the mechanism by which each intervention type is directly linked to improvement in outcomes is yet to be explored. To achieve this aim, a comprehensive program evaluation is currently ongoing, combining a mixed qualitative and quantitative approach to elicit case reports and to evaluate the underlying mechanisms for sustainable improvement.
Our report does not allow for direct statistical examination of the factors affecting the observed change in the targeted clinics. Also, we cannot preclude the effect of regression to the mean, which might have contributed to greater improvements among lowest performing clinics. Nonetheless, the study reports on all the target population (i.e., target clinics), which were low-performing clinics on the selected measures for an extended period of time (over a year before the inanition of the project), and for which a major change in quality improvement rate was observed only after the interventions were initiated. Additionally, the difference in rate of change between the pre- and postintervention initiation periods was observed for the target clinics but not for all other medium and large clinics in the organization.
Most important, assessment of the full impact of the strategy is not possible at this early point, as we can only show early trends toward disparity reduction. Still, as part of the continued organizational commitment to disparity reduction, ongoing improvement in all Clalit's districts will continue to be monitored and supported.
Summary
This paper describes a successful process of planning and execution of an organizational strategy for disparity reduction based on the framework of health care quality improvement. The strategy builds on available evidence of best practices for reducing disparities in health and health care, and on key organizational leverage points. Our early results indicate that the strategy can bring to closure of gaps in health and health care. Future studies will continue to assess long-term sustainability of the strategy as well as determine which specific interventions and pathways are deemed most effective.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: A special recognition to the members of the Health Disparity Reduction Steering Committee, for their roles in strategy development and consultation throughout the process. Finally, our highest appreciation goes to all Community Division, District, and local community teams for their roles in planning and their daily dedicated work that allowed the strategy's implementation.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Aaron KF, Clancy CM. Improving Quality and Reducing Disparities: Toward a Common Pathway. Journal of the American Medical Association. 2003;289(8):1033–4. doi: 10.1001/jama.289.8.1033. [DOI] [PubMed] [Google Scholar]
- Benyamini Y, Blumstein T, Boyko V, Lerner-Geva L. Cultural and Educational Disparities in the Use of Primary and Preventive Health Care Services among Midlife Women in Israel. Women's Health Issues: Official Publication of the Jacobs Institute of Women's Health. 2008;18(4):257–66. doi: 10.1016/j.whi.2007.12.009. [DOI] [PubMed] [Google Scholar]
- Betancourt JR, Green AR, Carrillo JE, Park ER. Cultural Competence and Health Care Disparities: Key Perspectives and Trends. Health Affairs (Project Hope) 2005;24(2):499–505. doi: 10.1377/hlthaff.24.2.499. [DOI] [PubMed] [Google Scholar]
- Carrier E, Gourevitch MN, Shah NR. Medical Homes: Challenges in Translating Theory into Practice. Medical Care. 2009;47(7):714–22. doi: 10.1097/MLR.0b013e3181a469b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chernichovsky D, Anson J. The Jewish Arab Divide in Life Expectancy in Israel. Economics and Human Biology. 2005;3(1):123–37. doi: 10.1016/j.ehb.2005.01.002. [DOI] [PubMed] [Google Scholar]
- Chin MH, Walters AE, Cook SC, Huang ES. Interventions to Reduce Racial and Ethnic Disparities in Health Care. Medical Care Research and Review. 2007;64(5, suppl):7S–28S. doi: 10.1177/1077558707305413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein L, Horev T. Inequality in Health and in the Health System [in Hebrew] Jerusalem: Taub Center for Social Policy Studies in Israel; 2007. [Google Scholar]
- Fiscella K. Eliminating Disparities in Health Care through Quality Improvement. In: Williams RA, editor. Eliminating Healthcare Disparities in America: Beyond the IOM Report. Totowa, NJ: Humana Press; 2007. pp. 1–2. [Google Scholar]
- Fremont AM, Bierman A, Wickstrom SL, Bird CE, Shah M, Escarce JJ, Horstman T, Rector T. Use of Geocoding in Managed Care Settings to Identify Quality Disparities. Health Affairs. 2005;24(2):516–26. doi: 10.1377/hlthaff.24.2.516. [DOI] [PubMed] [Google Scholar]
- General Accounting Office. Health Care: Approaches to Address Racial and Ethnic Disparities. Washington, DC: US General Accounting Office; 2003. [Google Scholar]
- Goldfracht M, Porath A. Nationwide Program for Improving the Care of Diabetic Patients in Israeli Primary Care Centers. Diabetes Care. 2000;23(4):495–9. doi: 10.2337/diacare.23.4.495. [DOI] [PubMed] [Google Scholar]
- Horev T, Kop Y. Allocation of Resources for Social Services [in Hebrew] Jerusalem: Taub Center for Social Policy Studies in Israel; 2008. Available at http://www.taubcenter.org.il/files/H2009_Health_System.pdf. [Google Scholar]
- Israeli Bureau of Statistics. le: Characterization and Classification of Local Authorities by the Socio-Economic Level of the Population. Israel: Israeli Bureau of Statistics; 2009. Available at http://www.cbs.gov.il/www/publications/local_authorities2003/local_authorities_e.htm. [Google Scholar]
- Jones RG, Trivedi AN, Ayanian JZ. Factors Influencing the Effectiveness of Interventions to Reduce Racial and Ethnic Disparities in Health Care. Social Science and Medicine. 2010;70(3):337–41. doi: 10.1016/j.socscimed.2009.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keinan-Boker L, Noyman N, Chinich A, Green MS, Nitzan-Kaluski D. Overweight and Obesity Prevalence in Israel: Findings of the First National Health and Nutrition Survey (MABAT) Israel Medical Association Journal. 2005;7(4):219–23. [PubMed] [Google Scholar]
- Lasser KE, Himmelstein DU, Woolhandler S. Access to Care, Health Status, and Health Disparities in the United States and Canada: Results of a Cross-National Population-Based Survey. American Journal of Public Health. 2006;96(7):1300–7. doi: 10.2105/AJPH.2004.059402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie N, Fremont A, Somers SA, Coltin K, Gelzer A, Johnson R, Rawlins W, Ting G, Wong W, Zimmerman D. The National Health Plan Collaborative to Reduce Disparities and Improve Quality. Joint Commission Journal on Quality and Patient Safety. 2008;34(5):256–65. doi: 10.1016/s1553-7250(08)34032-x. [DOI] [PubMed] [Google Scholar]
- Mackenbach JP. An Analysis of the Role of Health Care in Reducing Socioeconomic Inequalities in Health: The Case of the Netherlands. International Journal of Health Services: Planning, Administration, Evaluation. 2003;33(3):523–41. doi: 10.2190/C12H-NBA4-7QWE-6K3T. [DOI] [PubMed] [Google Scholar]
- Maislos M, Weisman D, Sherf M. Western Negev Mobile Diabetes Care Program: A Model for Interdisciplinary Diabetes Care in a Semi-Rural Setting. Acta Diabetologica. 2002;39(1):49–53. doi: 10.1007/s005920200012. [DOI] [PubMed] [Google Scholar]
- McKee M. What can Health Services Contribute to the Reduction of Inequalities in Health? Scandinavian Journal of Public Health. 2002;59(suppl 59):54–8. [PubMed] [Google Scholar]
- Nirel N, Pilpel D, Rosen B. 2000. The Accessibility and Availability of Health Services in the South of Israel: Has the Gap between the South and Other Regions in Israel Been Reduced in the Wake of the National Health Insurance Law? Research Report 354-00 [in Hebrew]. Jerusalem: JDC-Brookdale Institute.
- Nitzan-Kaluski D, Chinich A, Ifrah A, Merom D, Green MS. Correlates of Osteoporosis among Jewish and Arab Women Aged 45–74 in Israel: National Women's Health Interview Survey. Journal of Gender-Specific Medicine: The Official Journal of the Partnership for Women's Health at Columbia. 2003;6(1):17–23. [PubMed] [Google Scholar]
- Ornstein S, Nietert PJ, Jenkins RG, Wessell AM, Nemeth LS, Rose H. Improving the Translation of Research into Primary Care Practice: Results of a National Quality Improvement Demonstration Project. Joint Commission Journal on Quality and Patient Safety/Joint Commission Resources. 2008;34(7):379–90. doi: 10.1016/s1553-7250(08)34048-3. [DOI] [PubMed] [Google Scholar]
- Peleg R, Press Y, Asher M, Pugachev T, Glicensztain H, Lederman M, Biderman A. An Intervention Program to Reduce the Number of Hospitalizations of Elderly Patients in a Primary Care Clinic. BMC Health Services Research. 2008;8:36–43. doi: 10.1186/1472-6963-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riva M, Curtis S, Gauvin L, Fagg J. Unraveling the Extent of Inequalities in Health across Urban and Rural Areas: Evidence from a National Sample in England. Social Science and Medicine. 2009;68(4):654–63. doi: 10.1016/j.socscimed.2008.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers R, Hunter JE. Impact of Management by Objectives on Organizational Productivity. Journal of Applied Physiology. 1991;76:322–36. [Google Scholar]
- Salameh S, Hochner-Celnikier D, Chajek-Shaul T, Manor O, Bursztyn M. Ethnic Gap in Coronary Artery Disease: Comparison of the Extent, Severity, and Risk Factors in Arab and Jewish Middle-Aged Women. Journal of the Cardiometabolic Syndrome. 2008;3(1):26–9. doi: 10.1111/j.1559-4572.2008.07315.x. [DOI] [PubMed] [Google Scholar]
- Schnittker J, Bhatt M. The Role of Income and Race/Ethnicity in Experiences with Medical Care in the United States and United Kingdom. International Journal of Health Services: Planning, Administration, Evaluation. 2008;38(4):671–95. doi: 10.2190/HS.38.4.f. [DOI] [PubMed] [Google Scholar]
- Sequist TD, Adams A, Zhang F, Ross-Degnan D, Ayanian JZ. Effect of Quality Improvement on Racial Disparities in Diabetes Care. Archives of Internal Medicine. 2006;166(6):675–81. doi: 10.1001/archinte.166.6.675. [DOI] [PubMed] [Google Scholar]
- Shi L, Starfield B, Politzer R, Regan J. Primary Care, Self-Rated Health, and Reductions in Social Disparities in Health. Health Services Research. 2002;37(3):529–50. doi: 10.1111/1475-6773.t01-1-00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shih YC, Zhao L, Elting LS. Does Medicare Coverage of Colonoscopy Reduce Racial/Ethnic Disparities in Cancer Screening among the Elderly? Health Affairs (Project Hope) 2006;25(4):1153–62. doi: 10.1377/hlthaff.25.4.1153. [DOI] [PubMed] [Google Scholar]
- Shmueli A, Gross R. Income-Related Inequality in Health in Israel during the 90's [in Hebrew] Social Security Journal of Welfare and Social Security Study. 2001;59:64–75. [Google Scholar]
- Shuval JT. Health in Israel: Patterns of Equality and Inequality. Social Science and Medicine. 1990;31(3):291–303. doi: 10.1016/0277-9536(90)90276-x. [DOI] [PubMed] [Google Scholar]
- Smedley BD. Moving beyond Access: Achieving Equity in State Health Care Reform. Health Affairs (Project Hope) 2008;27(2):447–55. doi: 10.1377/hlthaff.27.2.447. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Institute of Medicine: The National Academies Press; 2003. [PubMed] [Google Scholar]
- Starfield B, Birn AE. Income Redistribution Is Not Enough: Income Inequality, Social Welfare Programs, and Achieving Equity in Health. Journal of Epidemiology and Community Health. 2007;61(12):1038–41. doi: 10.1136/jech.2006.054627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starfield B, Shi L, Macinko J. Contribution of Primary Care to Health Systems and Health. Milbank Quarterly. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarabeia J, Amitai Y, Green M, Halpern GJ, Blau S, Ifrah A, Rotem M, Jaber L. Differences in Infant Mortality Rates between Jews and Arabs in Israel, 1975–2000. Israel Medical Association Journal. 2004;6(7):403–7. [PubMed] [Google Scholar]
- Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Trends in the Quality of Care and Racial Disparities in Medicare Managed Care. New England Journal of Medicine. 2005;353(7):692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


