Abstract
Apical membrane antigen 1 (AMA-1) is an invasion-related Plasmodium antigen that is expressed during both intracellular and extracellular asexual stages of the parasite's life cycle, making it an ideal target for induction of humoral and cellular immune responses that can protect against malaria. We show here that when it is administered as a recombinant protein (P) in Montanide ISA720 adjuvant, followed by a recombinant human type 5 adenovirus (Ad), intense and long-lasting Plasmodium vivax AMA-1-specific antibody responses (including both IgG1 and IgG2a), as well as proliferative memory T cell responses, can be detected in immunized mice. Memory T cells displayed both central (CD44hi CD62Lhi) and effector (CD44hi CD62Llo) phenotypes, with the central memory phenotype prevailing (56% of AMA-1-specific proliferating cells). Considering the main traits of the memory immune responses induced against AMA-1, this particular sequence of immunogens (P followed by Ad), but no others (Ad/Ad, Ad/P, or P/P), displayed an optimal synergistic effect. These results give further support to the need for preclinical studies of P. vivax vaccine candidate AMA-1 administered in prime/boost protocols that include recombinant proteins and adenoviral vectors.
INTRODUCTION
Plasmodium vivax is estimated to cause 80 to 310 million cases of human malaria annually, mainly in the Middle East, Asia, Western Pacific region, and Central and South America (35, 40). Although P. vivax is widely regarded as benign, in recent years there have been increasing reports describing severe manifestations of vivax malaria in Indonesia (56), Papua New Guinea (18), western India (26), and Brazil (49). Additionally, there has been renewed interest in the control of P. vivax because recent studies have shown the emergence and spread of drug-resistant strains in Asia, Brazil, and Africa (13, 23, 55). Thus, despite the fact that most malaria research groups have traditionally focused on the development of vaccines against Plasmodium falciparum, which is responsible for the most dangerous forms of malaria, there are good reasons to develop a P. vivax vaccine.
Malaria vaccine candidates can derive from preerythrocytic stages (free sporozoite or intracellular liver stage forms) or blood stages (asexual or sexual) of the Plasmodium parasite. At least in theory, if present in both stages, any antigen might have better chances of becoming a vaccine, since it could become a target for all known host protective immune mechanisms (cellular and humoral). Apical membrane antigen 1 (AMA-1) is present in both preerythrocytic and asexual blood-stage forms of the Plasmodium parasite. Antibodies against this molecule display inhibitory activities against sporozoite invasion of hepatocytes (52) and against merozoite invasion of erythrocytes (24, 42).
Montanide ISA720 is an oil-in-water synthetic adjuvant that has been repeatedly used in preclinical (4, 12, 15, 20) and clinical (17, 19, 21, 28, 32, 37, 38, 46, 50) trials of different malaria vaccine candidates and in particular of P. falciparum AMA-1 (11, 12, 15, 21, 32, 38, 46, 50). It is highly immunogenic and is able to induce significant humoral and cellular immune responses, even after a single immunization, although standard protocols consist of three doses of antigen in this adjuvant. Although it seems to be a safe adjuvant for human use, reactogenicity has been reported in some cases (21, 38, 46). If included in a prime/boost protocol in which two or more immunogens are sequentially administered, the number of doses of this adjuvant/antigen combination might be decreased, maintaining immunogenicity and increasing its safety.
Recombinant adenoviruses are efficient vectors to simultaneously induce antigen-specific humoral and cellular immune responses in immunized hosts. Our previous work has shown that homologous prime/boost protocols that use this vector to immunize mice are effective against Leishmania spp. (43), Toxo- plasma gondii (10), or Trypanosoma cruzi (31) infections; they are all highly dependent on the induction of T-cell immunity for protection. Parasite-specific antibodies were also induced in all those animals. More than a decade ago we also described a heterologous prime/boost protocol that combined recombinant adenoviral and poxviral (vaccinia virus) recombinants, which was able to induce potent humoral and cellular responses and completely protect mice against murine malaria caused by Plasmodium yoelii (8). To date, human adenovirus type 5 (Ad5) vectors have also demonstrated an exceptional ability to generate cellular immune responses against recombinant antigens in humans (9), although some authors have questioned the possibility of their use because of preexisting immunity detected in a some humans (33, 53). If included in a prime/boost protocol, a single dose of adenovirus(es) might be sufficient for vaccination, even in individuals with preexisting immunity.
Three recent reports have also shown good immunogenicity of P. falciparum AMA-1 when encoded by adenoviral vectors. Bruder et al. (7) were able to induce P. falciparum-specific antibodies in rabbits immunized with an AMA-1 recombinant adenovirus type 5 vector that inhibited 99% of parasite growth in vitro. Sedegah et al. (51) showed that human volunteers immunized with an equivalent vector generated CD8+ T cells that specifically recognized P. falciparum AMA-1 peptides in gamma interferon (IFN-γ) assays. Finally, Draper et al. (14) immunized monkeys using a simian adenoviral vector (AdCh63) in different prime/boost protocols and were able to induce P. falciparum AMA-1-specific T and B cell immune responses. However, the authors did not report any result of a protocol consisting of protein priming and an adenovirus booster.
In our current study we have pursued the idea that to achieve longer-lasting simultaneous B and T cell immune responses against P. vivax, a heterologous prime/boost immunization regimen that includes inoculation of the AMA-1 (PvAMA-1) protein in a purified form, preceded or followed by an adenovirus-vectored antigen (Ad5PvAMA-1), could be one of the best approaches. PvAMA-1 was administered as a recombinant protein purified from bacteria in Montanide ISA720, aiming mainly at the induction of a strong humoral response. The recombinant human type 5 adenovirus vector was used not only to induce a humoral response but also to generate an efficient T cell response. The antigen-specific effector and memory immune profiles detected after these immunizations are described below.
MATERIALS AND METHODS
Recombinant immunogens.
Recombinant PvAMA-1 represents a His6-tagged polypeptide (amino acids [aa] 43 to 487) of a P. vivax isolate from Belem, Brazil (named BEL 12), as previously described (45). Recombinant PvMSP-119 represents a His6-tagged C-terminal 19-kDa fragment (aa 1616 to 1704; GenBank accession number M60807) of Plasmodium vivax Belem strain merozoite surface protein 1. Both proteins were expressed in Escherichia coli and purified using Ni2+ columns (ProBond; Invitrogen). AMA-1 was purified under denaturing conditions and MSP-119 under native conditions.
The PvAMA-1-encoding sequence fused to that of the signal peptide of the hemagglutinin of influenza virus (HASS) was also cloned into an adenoviral shuttle vector (pAdCMV), which was further cotransfected with plasmid pJM17 into HEK-293 cells (CRL-1573; American Type Culture Collection [ATCC], Manassas, VA) as previously described (34), to generate replication-deficient human type 5 recombinant adenovirus Ad5PvAMA-1. Individual clones of this virus were analyzed for recombinant protein expression. Positive clones were purified using a Vivapure Adenopack kit (VivaScience) and kept frozen at −80°C. Viral concentrations were calculated as viral particles (vp) and PFU per milliliter, by spectrophotometry and plaque assays, respectively. vp/PFU ratios were equivalent for the two batches of viruses used in this study (90 to 95 for Ad5PvAMA-1 and 76 to 83 for Ad5lacZ).
Animals and immunization regimens.
Female BALB/c mice were bred at the CEBIO/UFMG animal facilities in Belo Horizonte, Brazil, and used according to our institutional ethical guidelines (certificate CETEA 140/2005). Purified recombinant proteins formulated in Montanide ISA720 (Seppic, France) were administered subcutaneously to BALB/c mice over 8 weeks old (20 μg of PvAMA-1 per animal) in a final volume of 100 μl. Ad5PvAMA-1 was administered subcutaneously (109 PFU/animal) to littermates into both sides of the tail in a final volume of 100 μl. When needed, animals were boosted within a 6-week interval with the same doses of recombinant adenovirus or protein in Montanide ISA720. A minimum of 6 animals per group were used in all experiments.
The subcutaneous route was chosen for administration of both immunogens because previous studies had shown similar efficiency and fewer harmful effects compared to other routes (29, 44).
IFA.
Indirect immunofluorescence assay (IFA) was performed on HEK-293 cells infected with Ad5PvAMA-1 or with a control virus (Ad5lacZ) at a multiplicity of infection (MOI) of 5 for 36 h. Cells were then fixed with 4% paraformaldehyde and permeabilized with 0.2% Triton X-100. Sera of mice (Ad5 preadsorbed) immunized with different vaccination protocols or of human patients (Ad5 negative) from areas where malaria is endemic (Ethics Committee on Research with Humans of Universidade Federal de Minas Gerais, Protocol ETIC 060/07) were diluted in phosphate-buffered saline (PBS) containing 3% bovine serum albumin (BSA) and used as sources of primary PvAMA-1-specific antibodies. Secondary Alexa Fluor 488-conjugated anti-mouse IgG or anti-human IgG antibodies (Invitrogen) were diluted 1:200 in PBS containing 3% BSA. Slides were finally washed, mounted, sealed with Prolong Gold antifade reagent containing 4′,6-diamidino-2-phenylindole (DAPI) (Invitrogen), and observed using a fluorescence microscope.
Samples of P. vivax-infected blood from malaria patients were collected after written informed consent (Ethics Committee of the Faculty of Tropical Medicine, Mahidol University, Thailand, certificate of ethical approval MUTM 2010-006-01 and University of Oxford, Centre for Clinical Vaccinology and Tropical Medicine, United Kingdom, OXTREC 027-025) was obtained and were processed within 5 h of collection at Shoklo Malaria Research Unit, Thailand. White blood cells and platelets were removed, and infected erythrocytes were cultured to the late schizont stage in 2% hematocrit (Hct)–McCoy's 5A medium supplemented with 2.4 g/liter d-glucose, 40 mg/ml gentamicin sulfate, and 20% heat-inactivated human AB serum in an atmosphere of 5% O2 at 37.5°C for 22 to 44 h (48). Thin-smear preparations of free merozoites and mature schizont-infected erythrocytes were fixed with cold acetone for 15 min and blocked with 3% BSA in PBS for 30 min at 37.5°C in a humidified incubator. PvAMA1-immunized or prebleed mouse serum (1:100) was then applied to the smear and incubated for 1 h before incubation with the secondary anti-mouse IgG antibody conjugated to Alexa Fluor 488 (Molecular Probes) or DAPI as described above. The presence of PvAMA1 was visualized using a Nikon TS100 epifluorescence microscope.
Enzyme-linked immunosorbent assay (ELISA).
Purified PvAMA-1 protein expressed in E. coli was used as plate-coating antigen (Nunc MaxiSorp) at a concentration of 0.5 μg/well. Nonspecific binding sites were blocked with 2% dry milk in PBS. Serial dilutions of individual sera (1:100 to 1:409,600) were added to the wells and incubated for 1 h. The reaction was developed using horseradish peroxidase-conjugated (Zymed, Life Technologies) secondary antibodies (anti-IgG, IgG1, and IgG2a) and 3,3′,5,5′-tetramethylbenzidine (TMB) (Pierce) substrate. Optical densities were measured at 450 nm in a Titertek microplate reader (McLean, VA).
T cell proliferation and cytokine detection.
Spleens were aseptically isolated from mice at the times indicated. Splenocytes (106 cells/well) were stained with 4μM carboxyfluorescein succinimidyl ester (CFSE) for 15 min at 37°C in 5% CO2 and then stimulated with PvAMA-1(1 μg/ml) or with an equivalent concentration of control protein (PvMSP-119) in Dulbecco modified Eagle medium (DMEM) (Invitrogen) supplemented with 5% fetal calf serum (FCS) and 4 μg/ml gentamicin. Cultures were incubated for 30 or 48 h (as indicated) before T cell proliferation was determined by flow cytometry. Analyses were performed with a FACScan flow cytometer (Becton Dickinson, Oxford, United Kingdom). CFSE-labeled splenocytes were stained before analyses with fluorochrome-conjugated antibodies against CD4 (allophycocyanin [APC], clone GK1.5) and CD62L (phycoerythrin [PE], clone MEL-14) or CD44 (PE, clone IM7) from BD Pharmingen.
Cytokines in cell culture supernatants were measured at 48 h after addition of 1 μg/ml of PvAMA-1 using anticytokine sandwich antibodies of the corresponding ELISA kits (R&D systems).
Statistical analyses.
Analysis of variance (ANOVA) was used for comparison of groups. For analysis of groups with a normal distribution of samples, we also used the Student t test. When data did not follow a normal distribution, nonparametric tests (Kruskal-Wallis or Mann-Whitney) were applied. Variances were compared using Bartlett and de Levene tests. A significance level of 5% was used in all cases. For nonhomogeneous variances, Welch's correction was applied for parametric analyses. For multiple comparisons (Student t test and Mann-Whitney test), Bonferroni's correction was applied to avoid overestimated global errors. For flow cytometry analyses, the Z test was used to compare two proportions.
RESULTS
Recombinant forms of PvAMA-1 used in this study and reactivity with anti-Plasmodium antibodies present in malaria patients or immunized mice.
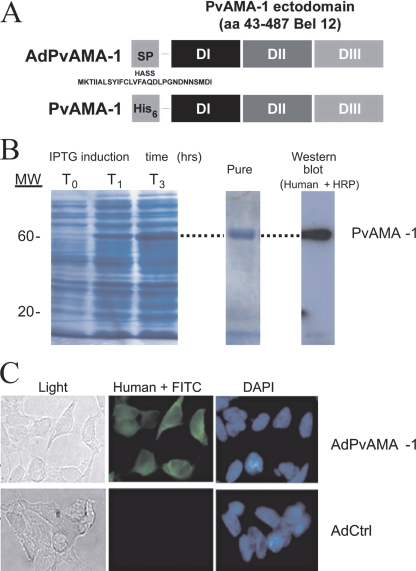
Two recombinant forms of the P. vivax vaccine candidate AMA-1 were used in our study (Fig. 1 A): a recombinant protein generated in recombinant E. coli bacteria and a recombinant human type 5 adenoviral vector. Expression of Pv-AMA-1 was efficiently induced in bacteria (Fig. 1B, left panel), being affinity purified to the point of displaying a single band of the expected molecular mass (around 60 kDa) after SDS-PAGE analysis (Fig. 1B, middle panel). Furthermore, a single reactive band of the same apparent molecular mass, which bound human antibodies raised after natural contact with P. vivax parasites, could be observed when the reactivity of the pure recombinant protein was tested by immunoblotting using sera of malaria patients (Fig. 1B, right panel).
Fig. 1.
Recombinant immunogens used in this study and reactivity with human antibodies. (A) Scheme of the engineered extracellular domains I to III of P. vivax AMA-1 as expressed by an adenovirus (AdPvAMA-1) or E. coli (PvAMA-1). SP, signal peptide; HASS, influenza virus hemagglutinin signal sequence. (B) AMA-1-containing bacterial lysates after IPTG (isopropyl-β-d-thiogalactopyranoside) induction (left panel), pure protein (middle panel), and specific reactivity with a P. vivax-positive human serum in an immunoblot assay (serum dilution, 1:2,000) (right panel). (C) Reactivity of the same serum (1:200 dilution) with HEK-293 cells infected with AdPvAMA-1 or a control adenoviral vector. Cells were visualized by fluorescence microscopy or phase-contrast light microscopy at a magnification of ×600.
A recombinant adenovirus expressing the ectodomain of PvAMA-1 (regions I, II, and III) (45) was also constructed. As depicted in Fig. 1A, cells infected with this vector express the recombinant protein fused to the signal peptide of the influenza virus hemagglutinin protein (HASS) to facilitate secretion and thus antibody generation, as well as cross presentation of antigens to T cells.
Antibodies to AMA-1 are found in most people exposed to malaria, and the levels of IgG to PvAMA-1 increase with the time of exposure (36). To characterize the recombinant product generated by Ad5PvAMA-1-infected cells, immunofluorescence assays were performed using human sera of malaria patients (who tested Ad5 negative) as a source of primary antibodies (Fig. 1C). Figure 1C shows that HEK-293 cells infected with Ad5PvAMA-1 generate a recombinant product that resembles the parasite's native antigen, since it is strongly recognized by antibodies present in individuals naturally exposed to P. vivax parasites.
Antibodies are directly linked to protection against the blood stages of the malaria parasite. To determine whether immunization with the recombinant forms of P. vivax AMA-1 could induce antibodies with specificities similar to those induced against the parasite itself, we performed an indirect immunofluorescence assay using P. vivax parasites (free merozoites and infected erythrocytes) and also compared the cross-reactivity between AMA-1-specific immunization-induced (murine serum) and parasite-induced (human serum) antibodies.
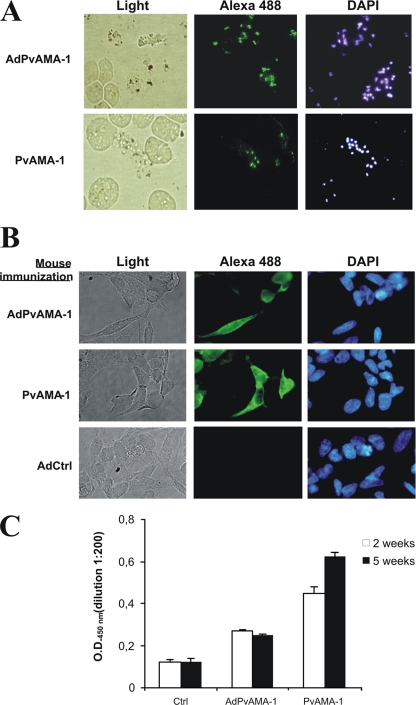
Initially, parasite isolates from infected patients were induced to mature in vitro before thin smears were prepared, fixed, and incubated with sera of BALB/c mice immunized with 109 PFU/animal of Ad5PvAMA-1 or 20 μg of PvAMA-1 protein in Montanide ISA720. Intense and specific fluorescence could be observed in free merozoites when incubated with sera of either adenovirus- or protein-immunized mice (Fig. 2 A) but not when incubated with control sera (not shown). Of interest, little or no fluorescence was observed inside infected erythrocytes within these preparations.
Fig. 2.
Reactivity of antibodies generated by immunization of BALB/c mice with a P. vivax AMA-1 recombinant adenovirus or with E. coli-produced AMA-1 protein in Montanide ISA720. (A) IFA images (magnification, ×1000) representing the immune reactivity of sera (1:100 dilution) of immunized mice (green) or the nucleic acid stain DAPI (blue) with P. vivax parasites or parasitized erythrocytes (light) obtained from infected individuals. (B and C) Cross-reactivity of mouse antibodies induced by immunization with either relevant immunogen (Ad or P) or with a control adenovirus against AdPvAMA-1-infected cells (IFA, 1:200 serum dilution; magnification, ×600) (B) or against PvAMA-1 protein used to coat an ELISA plate (1:400 serum dilution) (C). Results are representative of at least two equivalent experiments performed with pools of three animal sera.
Sera of the same groups of mice were also tested by immunofluorescence against Ad5PvAMA-infected cells (Fig. 2B) as well as by ELISA using PvAMA-1 coated plates (Fig. 2C). Antibodies induced in mice by Ad5PvAMA-1 or PvAMA-1 recognized the P. vivax antigen expressed by HEK-293 cells with a similar fluorescence pattern, suggesting an overall similarity in structure between both forms of the antigen and, together with the results shown above, a similarity between these antigens and the native parasite molecule.
To determine whether cross-reactivity also existed when using bacterially expressed PvAMA-1, we further analyzed by ELISA, using PvAMA-1-coated plates, the sera of control-, Ad5PvAMA-1-, and PvAMA-1-immunized mice at 2 and 5 weeks after immunization (Fig. 2C). The plot shows that, although the intensities were different (PvAMA-1 in Montanide ISA720 induced significantly higher levels of antibodies after a single immunization [P < 0.01 by Kruskal-Wallis test), reactivity was specific for PvAMA-1 independently of the immunogen used for inoculation.
Humoral immune responses induced by different PvAMA-1 immunization regimens.
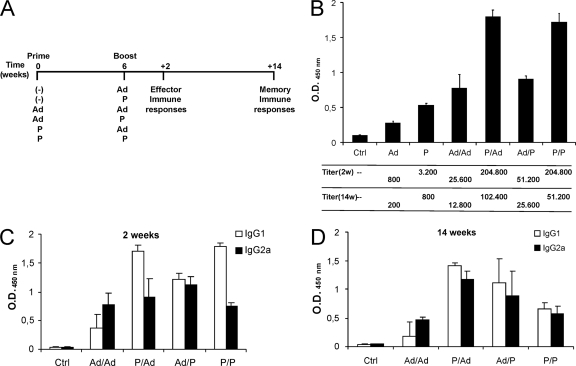
The intensities of AMA-1-specific humoral responses induced by immunization were subsequently determined in all groups of mice. We first measured, at 2 weeks after immunization, the antibody responses induced by different single-dose or prime/boost vaccination regimens. It has been repeatedly shown by many authors that different orders of administration of different immunogens may result in completely different immunization outcomes. Thus, our immunization protocols included inoculations of the recombinant protein and the adenoviral vector in different orders (Fig. 3 A). The immunization interval used was 6 weeks, because we previously determined that this interval is the minimum possible to avoid significant activation-induced cell death (AICD) mechanisms that could blunt immune responses before they reach maximal expansion (8).
Fig. 3.
Effector and memory humoral immune responses elicited in BALB/c mice after prime/boost immunizations with combinations of AdPvAMA-1 (Ad) and PvAMA-1 (P) or with the control formulation (Ctrl). (A) Scheme of immunizations and sample collection times. (B) ELISA results (both optical densities at 2 weeks after immunization and antibody titers at 2 and 14 weeks after inoculation of the last dose of either experimental vaccine) as determined in the sera of mice. (C and D) IgG1 and IgG2a responses in the sera of immunized mice at 2 (C) and 14 (D) weeks after inoculation of the last immunizing dose. Results are representative of three different experiments performed with 6 animals per group individually analyzed.
An ELISA was used to evaluate the humoral immunogenicities of the different immunization protocols in the different groups of mice. Optical densities were measured and total IgG antibody titers determined after endpoint dilutions of the sera of immunized BALB/c mice, at 2 weeks after inoculation of the last dose of experimental vaccine, using plates coated with PvAMA-1. The results (Fig. 3B) show that homologous and heterologous prime/boost protocols were able to elicit specific humoral responses that were in all cases more immunogenic than single-dose immunization protocols (P < 0.01 by Kruskal-Wallis test). Not all relevant protocols were equivalently immunogenic. Thus, reactivity (measured as total optical density in arbitrary units) and antibody titers were significantly higher (all P values < 0.01 by Mann-Whitney test) in sera of animals immunized with PvAMA-1 (P) alone or initially presented as a recombinant protein followed by either the adenoviral vector (P/Ad) or the same protein (P/P) than in groups of animals that received an initial dose of Ad5PvAMA-1 (Ad, Ad/Ad, or Ad/P). Antibody levels induced by P/Ad and P/P were not statistically different.
Memory antibody titers were also determined, at 14 weeks after inoculation of the last dose of experimental vaccine. By that time, we could observe significantly higher (P < 0.05 by Mann-Whitney test compared to primed-only mice) long-term (memory) responses still present in prime/boost-immunized animals. The highest antibody titers were displayed by sera of mice immunized with the P/Ad protocol.
PvAMA-1-specific antibody subclasses during effector and memory responses.
To explore the immune profiles induced in mice by the different immunization protocols, we first measured the levels of IgG1 and IgG2a antibodies in the sera of the different groups of mice. Total reactivity was higher for IgG1 than for IgG2a in all groups except Ad/Ad-immunized mice at both 2 (Fig. 3C) and 14 (Fig. 3D) weeks after immunization. However, although less intense in most groups, significant IgG2a reactivity was detected in all animals, suggesting a mixed Th1 and Th2 response. At 3 months after immunization, high levels of circulating IgG1 and IgG2a antibodies were still present in the blood, which indicated that immune memory had been potently induced for both subtypes. However, memory IgG1 responses decreased proportionally faster than IgG2a in the groups that received protein in Montanide as the first immunogen.
Of interest, a comparison of IgG isotype reactivities also showed significant differences in memory generation between immunization protocols. Thus, the protocol that used Ad5PvAMA-1 as a booster immunogen for PvAMA-1 (P/Ad) induced significantly (P = 0.0016 by Mann-Whitney test) more potent memory immune responses (both IgG1 and IgG2a) than a booster dose of the same protein (P/P).
Cellular immune responses induced in mice by vaccination with recombinant forms of P. vivax AMA-1.
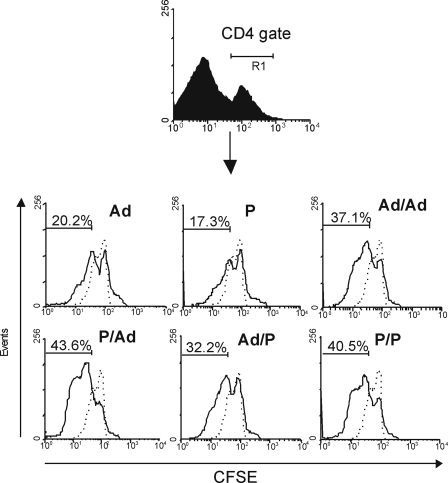
Antibodies that block red blood cell invasion seem to be the main mediators of protection against the blood stages of Plasmodium. However, the generation of AMA-1-specific T cells in the immunized host could also be relevant, both for long-term maintenance of the humoral response (memory cytokine-producing T helper cells) and for a possible induction of protection against the liver stages of the parasite (mainly through antigen-specific production of IFN-γ). To address this, splenocytes of mice immunized with the different prime/boost protocols were stained with CFSE and CD4-APC 2 weeks after receiving the last immunizing dose, and their proliferation rates were analyzed by flow cytometry. The specificity of the responses was assessed by comparing proliferation rates of cells from AMA-1-immunized mice with those of cells from mice inoculated with an irrelevant antigen (β-galactosidase administered as recombinant adenovirus Ad5lacZ), as well as by restimulating splenocytes of AMA-1-immunized mice with PvAMA-1 or with a different P. vivax antigen, MSP-119.
As illustrated in Fig. 4, when splenocytes were analyzed 30 h after ex vivo antigenic stimulation, CD4+ T lymphocyte proliferation was observed in all groups of mice immunized with recombinant forms of AMA-1 (comparison of proportions, P < 0.05 by Z test). Lymphocytes of animals that received two immunizations of either form of the antigen proliferated more intensely than those from animals that received a single immunizing dose (P < 0.05 by Z test), confirming that prime/boost protocols are more efficient at inducing not only antibodies but also T cell responses. No statistically significant differences could be observed among different prime/boost protocols, although higher percentages of proliferating cells were always detected in the groups that were inoculated with PvAMA-1 in Montanide ISA720 as the priming formulation (P/Ad and P/P).
Fig. 4.
Proliferation assay performed on CFSE-labeled splenocytes of BALB/c mice immunized with P. vivax recombinant immunogens. The percentage of proliferation was calculated by flow cytometry on CD4+ gated splenocytes of mice immunized 2 weeks before with AMA-1 (continuous lines) administered as a recombinant adenoviral vector (Ad), as a protein in Montanide ISA720 (P), or as sequential inoculations of both immunogens in prime/boost protocols, compared to mice immunized with two doses of an irrelevant adenovirus control (dotted lines). CFSE-labeled splenocytes were induced to proliferate ex vivo for 30 h by adding PvAMA-1 to the cell culture. Plots are representative of two different experiments that included a total of six animals per group, analyzed in pools of three. Numbers represent mean values of the results.
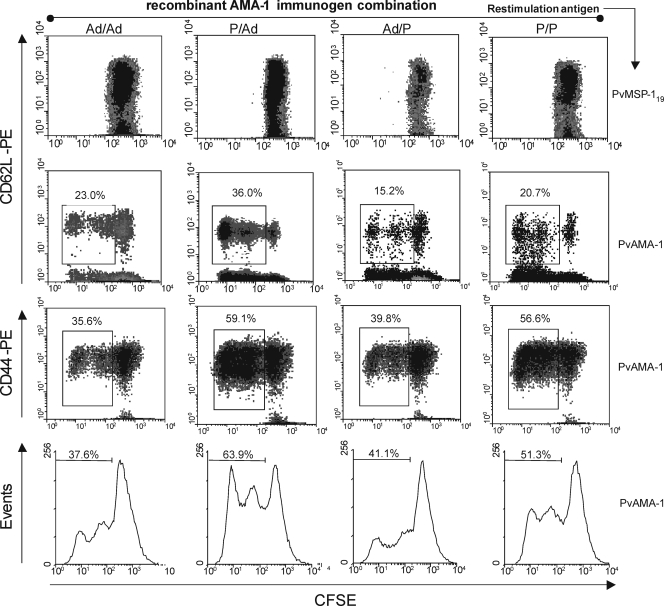
Lymphocytes were also stained with CFSE and antibodies to surface markers CD4, CD62L, and CD44, at 14 weeks after the last immunization, to determine the type and fate of the memory T cells that could had been generated in BALB/c mouse littermates. Figure 5 shows that CD4+ splenocytes from all groups of mice that received prime/boost immunizations also proliferated intensely at this time point in the presence of AMA-1 (compare top and second rows of panels). Proliferation was significantly more intense (P < 0.05 by Z test) for the groups of mice that received PvAMA-1 in Montanide ISA720 as the priming immunogen (P/Ad and P/P in the fourth row of panels) than for groups that received Ad5PvAMA-1 adenoviruses (Ad/Ad or Ad/P, same row).
Fig. 5.
Memory phenotypes of AMA-1-specific mouse lymphocytes generated after prime/boost vaccination. The percentage of CD62L- or CD44-positive proliferating cells (as indicated) was determined by flow cytometric analyses of splenocytes of BALB/c mice immunized according to the most relevant prime/boost protocols defined in this study and tested 14 weeks after the final immunization. CFSE-labeled splenocytes were induced to proliferate ex vivo for 48 h by adding PvAMA-1 (three lower rows of panels) or PvMSP-119 (negative controls, upper row of panels) to the cell cultures. Results are representative of two different experiments involving a total of six animals per group, individually analyzed.
According to the literature, central memory (CM) and effector memory (EM) T cell phenotypes may be defined, respectively, as CD44hi CD62Lhi and CD44hi CD62Llo (6). When memory phenotype cell surface markers were analyzed in mice at 14 weeks after immunization, it could be observed that the vast majority (mean ± standard deviation = 95% ± 2%) of the proliferating cells were CD44hi (compare the third and fourth rows of panels in Fig. 5). The second activation marker analyzed, CD62L, however, was not expressed in all proliferating cells. Figure 5 shows that mean values of CD62Lhi proliferating cells (second row) versus total proliferating cells (fourth row) were 61, 56, 37, and 40%, respectively, for the Ad/Ad, P/Ad, Ad/P, and P/P groups. This indicates that a significant proportion of proliferating cells were CD62Llo and suggests the induction of immune responses with a mixed memory phenotype, with the CM phenotype prevailing (significant difference with a confidence level of 99% by the Z test) when the Ad vector is used to boost immunes responses and the EM phenotype prevailing when the P is given as booster.
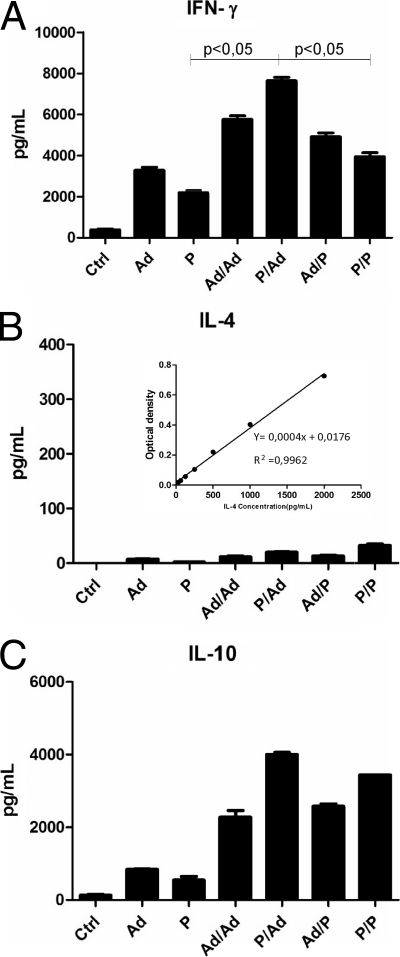
Cytokine secretion profiles of splenocytes of mice vaccinated with recombinant forms of P. vivax AMA-1.
Supernatants of splenocyte cultures from mice that had been immunized 14 weeks before with the different protocols mentioned above were analyzed by sandwich ELISA to determine their cytokine secretion profiles after in vitro restimulation with recombinant PvAMA-1. Figure 6 A shows that splenocytes of all groups of animals that received booster doses of either immunogen were capable of secreting higher levels of IFN-γ than those of animals that received a single dose. However, highly significant differences were observed only when using the P/Ad immunization protocol. The amounts of IFN-γ secreted by splenocytes of mice immunized with this protocol were repeatedly found to be at least two times higher than those secreted by splenocytes from animals immunized with P/P and up to three times higher than those of animals that received a single dose of protein in Montanide ISA720. Figure 6B shows that, opposite to that observation, interleukin-4 (IL-4) secretion was not significantly increased by administration of a booster dose of either immunogen, though the technique was performed with a range of values that would have detected those differences. Finally, Fig. 6C shows that IL-10 was produced at significantly higher levels by splenocytes of mice that had received booster doses of either immunogen, being significantly higher in animals immunized with either the homologous (P/P) or the heterologous (P/Ad) protocol.
Fig. 6.
Cytokine secretion profiles of splenocytes of BALB/c mice immunized with P. vivax recombinant immunogens. The cytokines IFN-γ (A), IL-4 (B), and IL-10 (C) were analyzed by ELISA in cell culture supernatants after in vitro restimulation with recombinant PvAMA-1 of splenocytes of the different groups of mice (as indicated) immunized 14 weeks before. Plots are representative of two different experiments that included a total of six animals per group, analyzed in pools of three. Numbers represent means ± standard errors of the means (SEM).
DISCUSSION
We have used two different systems (E. coli and a human type 5 adenovirus vector) to express P. vivax AMA-1. Ad5 was chosen because in the absence of preexisting immunity (which is the case for most children during the first months of life, when they would be considered primary targets for the vaccine), it is the most immunogenic among several adenoviral vectors tested to date (1, 2). Additional adjuvants were avoided in the adenoviral formulation to maintain the immune traits characteristic of the Ad5 vector. Our results indicate that both systems generated AMA-1 successfully, since recombinant products of the expected molecular weight specifically reacted with antibodies from individuals previously exposed to P. vivax parasite antigens.
In immunized mice, the recombinant protein, as well as the adenoviral vector, induced specific antibody responses against P. vivax parasites. Of interest, antibodies raised by our immunizations reacted strongly with free merozoites but not detectably with intraerythrocytic parasites, a phenomenon already described by members of our group (16). Cross-reactivity between the protein produced in bacteria and the antigen expressed in adenovirus-infected cells suggests that the structure of the polypeptide is largely conserved between the two recombinant products. Moreover, the immune reactivity and fluorescence patterns displayed by adenovirus-infected cells incubated with sera of human malaria patients or immunized mice suggest that the overall structure must also be conserved between the recombinant and the native parasite antigens.
We next compared the humoral and cellular immune responses induced in mice immunized with different homologous or heterologous prime/boost protocols involving the recombinant purified AMA-1 protein produced in bacteria and the nonreplicative recombinant adenoviral vector. A single immunization with the purified protein in Montanide ISA720 or with the recombinant adenovirus induced readily detectable IgG antibodies. Antibody titers were higher when using PvAMA-1 in Montanide ISA720. In all cases, booster immunizations were able to increase the antibody titers detected after a single administration of either immunogen. When the efficiencies of different prime/boost protocols were compared, the results demonstrated that immunizations with P/P (homologous) and P/Ad (heterologous) protocols were the most efficient at enhancing antibody responses. These responses not only were high at the active phase of the immune response (2 weeks after immunization) but also remained high for over 3 months (14 weeks) after the boost. It is worth noting that, at any time point considered, vaccination generated parasite-specific antibodies more efficiently than repeated natural human infections (45).
The prime/boost protocol P/Ad described here is particularly attractive not only because it displayed higher immunogenicity but also because it could represent a significant step up in vaccine safety. Previous human vaccination protocols, such as the administration of three doses of a protein or peptide in Montanide ISA720 (19, 32, 37, 38, 46, 50) or three doses of a recombinant adenovirus (9), could be improved by using only one dose of each immunogen, and this would eliminate the possibility of adverse effects resulting from administration of repeated doses. In addition, it has been suggested (5) that a heterologous protocol could overcome preexisting immunity to adenovirus type 5 vectors present in human populations as well as avoid the altered immune responses to the recombinant antigens observed in these populations when immunized with a homologous Ad5 prime/boost protocol (39).
Our results in mice indicate that immunization with PvAMA-1 was capable of inducing long-lasting mixed humoral responses, with production of both IgG1 and IgG2a antigen-specific antibodies. ELISA reactivity suggested that IgG1 was initially produced more than IgG2a, though levels were very similar at week 14 after boost. Other authors have also observed a preferential induction of antibodies of the IgG1 subclass when vaccinating with Montanide ISA720, in both mice (41) and humans (3). The induction of not only IgG1 but also IgG2a responses is important, since in malaria, as in all infectious diseases, antibody isotypes affect pathogen neutralization and clearance, and it is widely accepted that cytophilic antibodies (such as mouse IgG2a) are involved in protective immunity against Plasmodium AMA-1 and other blood-stage antigens (22, 36).
The generation of antigen-specific T cells was also analyzed, and the results showed that not-yet-described T cell epitopes for the mouse H-2d/major histocompatibility complex (MHC) background must be present in the P. vivax AMA-1 antigen, since intense T cell proliferation was observed when splenocytes of immunized BALB/c mice were restimulated in vitro with this antigen. Although a description of mouse T cell epitopes is not very relevant for human studies because of the significant differences in MHCs between the two species, it is a good indicator of the capacity of the adenoviral vector to induce efficient T cell responses. In fact, a recently published paper (51) describes for the first time the induction in humans of CD8 T cells against nine epitopes of P. falciparum AMA-1 after immunization of volunteers with an adenoviral vector equivalent to the one described here.
Contrary to what has been previously described for adenovirus-induced T cells, we could detect the preferential induction of CM T cells after immunization with P/Ad or Ad/Ad. Since the preferential induction of CD8+ T cell EM responses has been attributed to the fact that the recombinant adenoviral vector may persist in the host organism for long times (54), it could be the case that a previous immunization with the recombinant protein or with the same vector may have acted as an adenovirus clearance stimulus, permitting the preferential induction of a different type of memory cells. Alternatively, slight differences in adenovirus backbones, i.e., deletions of genes encoding products that may interfere with immune responses against the vector, may result in different persistence of the resulting vectors, affecting the profile of memory generation.
As expected from the literature (30, 57), the order of administration of the immunogens affected the humoral and cellular responses elicited. Thus, when Ad was used as a priming vaccine, the antibody titers and proliferative T cell rates were lower than when the same vector was used as a booster. A recent study by Radosevic et al. (41) explored the use of a recombinant P. falciparum antigen (the circumsporozoite protein) expressed in yeast for priming and two adenoviruses (Ad35 and Ad26) as boosters. Although the parasite, the antigen, and the viruses studied were different, results were similar to those shown here for PvAMA-1. A recent report by Draper et al. (14) suggests that an adenovirus priming followed by a protein booster (Ad/P) would be the most efficient protocol to induce B cell responses against PfAMA-1; however, no final conclusions can be extracted from these data since the authors did not include P/Ad among the prime/boost protocols compared. In any case, all three studies with recombinant adenoviruses encoding PfAMA-1 reported to date (7, 14, 51) have reported antibody titers capable of significantly inhibiting P. falciparum growth in culture, greatly supporting our current approach to develop a vaccine against P. vivax.
This is the first time to our knowledge that any recombinant virus encoding P. vivax AMA-1 has been described and used to induce immune responses specific against this parasite. Few studies on experimental vaccination with PvAMA-1 have been performed. In summary, researchers have described high antibody titers following immunization with recombinant proteins (16, 27) and lower titers when using plasmid DNA vaccines (25, 47). In none of these studies did the authors compare two or more different protocols or use a recombinant adenovirus vector. Therefore, to date it is not possible to compare our results with others. Additionally, this lack of sufficient data also impedes any conclusion on the important relationship between allelic polymorphism and immune recognition of AMA-1. Despite that, our results suggest that both humoral and cellular memory responses are potently induced in mice when the P/Ad immunization protocol is used. Not only were antibody levels (both IgG1 and IgG2a) potently induced, but also more memory (CM and EM) T cells were present nearly 4 months after this immunization. Simultaneous induction of B and T cell responses against AMA-1 is important, since this liver- and blood-stage antigen may be target of both immune-effector arms, which can help in neutralizing/clearing Plasmodium parasites. Monkey experiments are underway to define the safety, immunogenicity, and protective efficacy of this prime/boost protocol.
ACKNOWLEDGMENTS
This work was financially supported by the Oswaldo Cruz Foundation (FIOCRUZ, PDTIS program RVR01-Malaria Vaccine), the Brazilian National Research Council (CNPq/INCTV, National Institute of Science and Technology in Vaccines), and the Fundação de Amparo a Pesquisa do Estado de São Paulo (FAPESP). Leoneide Bouillet was supported by a Ph.D. fellowship from Fundação de Amparo a Pesquisa do Estado de Minas Gerais (FAPEMIG). E. M. Braga, R. T. Gazzinelli, M. M. Rodrigues, I. S. Soares, and O. Bruna-Romero were also supported by CNPq fellowships. F.N. and the SMRU are supported by the Wellcome Trust of Great Britain.
L.E.M.B., R.T.G., M.M.R., I.S.S., and O.B.-R. are named inventors on patent applications covering malaria vectored vaccines and immunization regimens.
Footnotes
Published ahead of print on 5 July 2011.
REFERENCES
- 1. Abbink P., et al. 2007. Comparative seroprevalence and immunogenicity of six rare serotype recombinant adenovirus vaccine vectors from subgroups B and D. J. Virol. 81:4654–4663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Adams W. C., et al. 2011. Adenovirus type-35 vectors block human CD4+ T-cell activation via CD46 ligation. Proc. Natl. Acad. Sci. U. S. A. 108:7499–7504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Arevalo-Herrera M., et al. 2011. Antibody-mediated and cellular immune responses induced in naive volunteers by vaccination with long synthetic peptides derived from the Plasmodium vivax circumsporozoite protein. Am. J. Trop. Med. Hyg. 84:35–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Arevalo-Herrera M., et al. 2011. Preclinical vaccine study of Plasmodium vivax circumsporozoite protein-derived synthetic polypeptides formulated in montanide ISA 720 and montanide ISA 51 adjuvants. Am. J. Trop. Med. Hyg. 84:21–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Asefa B., Korokhov N., Lemiale F. 2010. Heterologous HIV-based lentiviral/adenoviral vectors immunizations result in enhanced HIV-specific immunity. Vaccine 28:3617–3624 [DOI] [PubMed] [Google Scholar]
- 6. Bjorkdahl O., et al. 2003. Characterization of CC-chemokine receptor 7 expression on murine T cells in lymphoid tissues. Immunology 110:170–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bruder J. T., et al. 2010. Adenovectors induce functional antibodies capable of potent inhibition of blood stage malaria parasite growth. Vaccine 28:3201–3210 [DOI] [PubMed] [Google Scholar]
- 8. Bruna-Romero O., Gonzalez-Aseguinolaza G., Hafalla J. C., Tsuji M., Nussenzweig R. S. 2001. Complete, long-lasting protection against malaria of mice primed and boosted with two distinct viral vectors expressing the same plasmodial antigen. Proc. Natl. Acad. Sci. U. S. A. 98:11491–11496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Buchbinder S. P., et al. 2008. Efficacy assessment of a cell-mediated immunity HIV-1 vaccine (the Step Study): a double-blind, randomised, placebo-controlled, test-of-concept trial. Lancet 372:1881–1893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Caetano B. C., et al. 2006. Vaccination with replication-deficient recombinant adenoviruses encoding the main surface antigens of Toxoplasma gondii induces immune response and protection against infection in mice. Hum. Gene Ther. 17:415–426 [DOI] [PubMed] [Google Scholar]
- 11. Coley A. M., et al. 2001. Rapid and precise epitope mapping of monoclonal antibodies against Plasmodium falciparum AMA1 by combined phage display of fragments and random peptides. Protein Eng. 14:691–698 [DOI] [PubMed] [Google Scholar]
- 12. Collins W. E., et al. 1994. Protective immunity induced in squirrel monkeys with recombinant apical membrane antigen-1 of Plasmodium fragile. Am. J. Trop. Med. Hyg. 51:711–719 [DOI] [PubMed] [Google Scholar]
- 13. de Santana Filho F. S., et al. 2007. Chloroquine-resistant Plasmodium vivax, Brazilian Amazon. Emerg. Infect. Dis. 13:1125–1126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Draper S. J., et al. 2010. Enhancing blood-stage malaria subunit vaccine immunogenicity in rhesus macaques by combining adenovirus, poxvirus, and protein-in-adjuvant vaccines. J. Immunol. 185:7583–7595 [DOI] [PubMed] [Google Scholar]
- 15. Dutta S., et al. 2009. High antibody titer against apical membrane antigen-1 is required to protect against malaria in the Aotus model. PLoS One 4:e8138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gentil F., et al. 2010. A recombinant vaccine based on domain II of Plasmodium vivax apical membrane antigen 1 induces high antibody titres in mice. Vaccine 28:6183–6190 [DOI] [PubMed] [Google Scholar]
- 17. Genton B., et al. 2003. Safety and immunogenicity of a three-component blood-stage malaria vaccine (MSP1, MSP2, RESA) against Plasmodium falciparum in Papua New Guinean children. Vaccine 22:30–41 [DOI] [PubMed] [Google Scholar]
- 18. Genton B., et al. 2008. Plasmodium vivax and mixed infections are associated with severe malaria in children: a prospective cohort study from Papua New Guinea. PLoS Med. 5:e127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Herrera S., et al. 2011. Phase I safety and immunogenicity trial of Plasmodium vivax CS derived long synthetic peptides adjuvanted with montanide ISA 720 or montanide ISA 51. Am. J. Trop. Med. Hyg. 84:12–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hodder A. N., Crewther P. E., Anders R. F. 2001. Specificity of the protective antibody response to apical membrane antigen 1. Infect. Immun. 69:3286–3294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hu J., et al. 2008. Safety and immunogenicity of a malaria vaccine, Plasmodium falciparum AMA-1/MSP-1 chimeric protein formulated in montanide ISA 720 in healthy adults. PLoS One 3:e1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Iriemenam N. C., et al. 2009. Antibody responses to a panel of Plasmodium falciparum malaria blood-stage antigens in relation to clinical disease outcome in Sudan. Vaccine 27:62–71 [DOI] [PubMed] [Google Scholar]
- 23. Karunajeewa H. A., et al. 2008. A trial of combination antimalarial therapies in children from Papua New Guinea. N. Engl. J. Med. 359:2545–2557 [DOI] [PubMed] [Google Scholar]
- 24. Kennedy M. C., et al. 2002. In vitro studies with recombinant Plasmodium falciparum apical membrane antigen 1 (AMA1): production and activity of an AMA1 vaccine and generation of a multiallelic response. Infect. Immun. 70:6948–6960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kim H. J., et al. 2011. CD8 T-cell activation in mice injected with a plasmid DNA vaccine encoding AMA-1 of the reemerging Korean Plasmodium vivax. Korean J. Parasitol. 49:85–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kochar D. K., et al. 2005. Plasmodium vivax malaria. Emerg. Infect. Dis. 11:132–134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kocken C. H., et al. 1999. High-level expression of Plasmodium vivax apical membrane antigen 1 (AMA-1) in Pichia pastoris: strong immunogenicity in Macaca mulatta immunized with P. vivax AMA-1 and adjuvant SBAS2. Infect. Immun. 67:43–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lawrence G. W., Saul A., Giddy A. J., Kemp R., Pye D. 1997. Phase I trial in humans of an oil-based adjuvant SEPPIC MONTANIDE ISA 720. Vaccine 15:176–178 [DOI] [PubMed] [Google Scholar]
- 29. Leenaars P. P., et al. 1998. Assessment of side effects induced by injection of different adjuvant/antigen combinations in rabbits and mice. Lab. Anim. 32:387–406 [DOI] [PubMed] [Google Scholar]
- 30. Li S., et al. 1993. Priming with recombinant influenza virus followed by administration of recombinant vaccinia virus induces CD8+ T-cell-mediated protective immunity against malaria. Proc. Natl. Acad. Sci. U. S. A. 90:5214–5218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Machado A. V., et al. 2006. Long-term protective immunity induced against Trypanosoma cruzi infection after vaccination with recombinant adenoviruses encoding amastigote surface protein-2 and trans-sialidase. Hum. Gene Ther. 17:898–908 [DOI] [PubMed] [Google Scholar]
- 32. Malkin E., et al. 2008. A phase 1 trial of PfCP2.9: an AMA1/MSP1 chimeric recombinant protein vaccine for Plasmodium falciparum malaria. Vaccine 26:6864–6873 [DOI] [PubMed] [Google Scholar]
- 33. McCoy K., et al. 2007. Effect of preexisting immunity to adenovirus human serotype 5 antigens on the immune responses of nonhuman primates to vaccine regimens based on human- or chimpanzee-derived adenovirus vectors. J. Virol. 81:6594–6604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. McGrory W. J., Bautista D. S., Graham F. L. 1988. A simple technique for the rescue of early region I mutations into infectious human adenovirus type 5. Virology 163:614–617 [DOI] [PubMed] [Google Scholar]
- 35. Mendis K., Sina B. J., Marchesini P., Carter R. 2001. The neglected burden of Plasmodium vivax malaria. Am. J. Trop. Med. Hyg. 64:97–106 [DOI] [PubMed] [Google Scholar]
- 36. Morais C. G., et al. 2006. Antibodies to Plasmodium vivax apical membrane antigen 1: persistence and correlation with malaria transmission intensity. Am. J. Trop. Med. Hyg. 75:582–587 [PubMed] [Google Scholar]
- 37. Oliveira G. A., et al. 2005. Safety and enhanced immunogenicity of a hepatitis B core particle Plasmodium falciparum malaria vaccine formulated in adjuvant Montanide ISA 720 in a phase I trial. Infect. Immun. 73:3587–3597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pierce M. A., et al. 2010. Phase 1 safety and immunogenicity trial of the Plasmodium falciparum blood-stage malaria vaccine AMA1-C1/ISA 720 in Australian adults. Vaccine 28:2236–2242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pine S. O., et al. 2011. Pre-existing adenovirus immunity modifies a complex mixed Th1 and Th2 cytokine response to an Ad5/HIV-1 vaccine candidate in humans. PLoS One 6:e18526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Price R. N., et al. 2007. Vivax malaria: neglected and not benign. Am. J. Trop. Med. Hyg. 77:79–87 [PMC free article] [PubMed] [Google Scholar]
- 41. Radosevic K., et al. 2010. The Th1 immune response to Plasmodium falciparum circumsporozoite protein is boosted by adenovirus vectors 35 and 26 with a homologous insert. Clin. Vaccine Immunol. 17:1687–1694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Remarque E. J., Faber B. W., Kocken C. H., Thomas A. W. 2008. Apical membrane antigen 1: a malaria vaccine candidate in review. Trends Parasitol. 24:74–84 [DOI] [PubMed] [Google Scholar]
- 43. Resende D. M., et al. 2008. Epitope mapping and protective immunity elicited by adenovirus expressing the Leishmania amastigote specific A2 antigen: correlation with IFN-gamma and cytolytic activity by CD8+ T cells. Vaccine 26:4585–4593 [DOI] [PubMed] [Google Scholar]
- 44. Rodrigues E. G., Zavala F., Eichinger D., Wilson J. M., Tsuji M. 1997. Single immunizing dose of recombinant adenovirus efficiently induces CD8+ T cell-mediated protective immunity against malaria. J. Immunol. 158:1268–1274 [PubMed] [Google Scholar]
- 45. Rodrigues M. H., et al. 2005. Antibody response of naturally infected individuals to recombinant Plasmodium vivax apical membrane antigen-1. Int. J. Parasitol. 35:185–192 [DOI] [PubMed] [Google Scholar]
- 46. Roestenberg M., et al. 2008. Safety and immunogenicity of a recombinant Plasmodium falciparum AMA1 malaria vaccine adjuvanted with Alhydrogel, Montanide ISA 720 or AS02. PLoS One 3:e3960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rogers W. O., Gowda K., Hoffman S. L. 1999. Construction and immunogenicity of DNA vaccine plasmids encoding four Plasmodium vivax candidate vaccine antigens. Vaccine 17:3136–3144 [DOI] [PubMed] [Google Scholar]
- 48. Russell B., et al. 2008. Determinants of in vitro drug susceptibility testing of Plasmodium vivax. Antimicrob. Agents Chemother. 52:1040–1045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Santos-Ciminera P. D., Roberts D. R., Alecrim M. G., Costa M. R., Quinnan G. V., Jr 2007. Malaria diagnosis and hospitalization trends, Brazil. Emerg. Infect. Dis. 13:1597–1600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Saul A., et al. 2005. A human phase 1 vaccine clinical trial of the Plasmodium falciparum malaria vaccine candidate apical membrane antigen 1 in Montanide ISA720 adjuvant. Vaccine 23:3076–3083 [DOI] [PubMed] [Google Scholar]
- 51. Sedegah M., et al. 2010. Identification and localization of minimal MHC-restricted CD8+ T cell epitopes within the Plasmodium falciparum AMA1 protein. Malar. J. 9:241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Silvie O., et al. 2004. A role for apical membrane antigen 1 during invasion of hepatocytes by Plasmodium falciparum sporozoites. J. Biol. Chem. 279:9490–9496 [DOI] [PubMed] [Google Scholar]
- 53. Sumida S. M., et al. 2004. Neutralizing antibodies and CD8+ T lymphocytes both contribute to immunity to adenovirus serotype 5 vaccine vectors. J. Virol. 78:2666–2673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Tatsis N., et al. 2007. Adenoviral vectors persist in vivo and maintain activated CD8+ T cells: implications for their use as vaccines. Blood 110:1916–1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Teka H., et al. 2008. Chloroquine-resistant Plasmodium vivax malaria in Debre Zeit, Ethiopia. Malar. J. 7:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Tjitra E., et al. 2008. Multidrug-resistant Plasmodium vivax associated with severe and fatal malaria: a prospective study in Papua, Indonesia. PLoS Med. 5:e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Vuola J. M., et al. 2005. Differential immunogenicity of various heterologous prime/boost vaccine regimens using DNA and viral vectors in healthy volunteers. J. Immunol. 174:449–455 [DOI] [PubMed] [Google Scholar]