Abstract
Outbreaks of influenza A viruses are associated with significant human morbidity worldwide. Given the increasing resistance to the available influenza drugs, new therapies for the treatment of influenza virus infection are needed. An alternative approach is to identify products that enhance a protective immune response. In these studies, we demonstrate that infecting mice with the Th1-inducing parasite Toxoplasma gondii prior to highly pathogenic avian H5N1 influenza virus infection led to decreased lung viral titers and enhanced survival. A noninfectious fraction of T. gondii soluble antigens (STAg) elicited an immune response similar to that elicited by live parasites, and administration of STAg 2 days after H5N1 influenza virus infection enhanced survival, lowered viral titers, and reduced clinical disease. STAg administration protected H5N1 virus-infected mice lacking lymphocytes, suggesting that while the adaptive immune response was not required for enhanced survival, it was necessary for STAg-mediated viral clearance. Mechanistically, we found that administration of STAg led to increased production of gamma interferon (IFN-γ) from natural killer (NK) cells, which were both necessary and sufficient for survival. Further, administration of exogenous IFN-γ alone enhanced survival from H5N1 influenza virus infection, although not to the same level as STAg treatment. These studies demonstrate that a noninfectious T. gondii extract enhances the protective immune response against severe H5N1 influenza virus infections even when a single dose is administered 2 days postinfection.
INTRODUCTION
In April 2009, the swine-origin pandemic H1N1 influenza virus (pH1N1) emerged as the first pandemic strain of the 21st century (42). In contrast to the distantly related 1918 H1N1 influenza virus or the highly pathogenic avian H5N1 influenza viruses, which are associated with 60% mortality in infected individuals (52), the pH1N1 virus was associated with mild disease and low mortality (16, 51). Given the cocirculation of pH1N1 and H5N1 viruses in certain areas of the world, concerns have been raised that reassortants between these viruses may occur, leading to more-severe disease (3, 15). Although annual vaccination is the primary strategy for preventing infections, influenza virus antiviral drugs play an important role in a comprehensive approach to controlling illness and transmission. The two classes of approved antiviral drugs are the adamantane derivatives and neuraminidase inhibitors (19). For maximum benefits, the drugs must be administered within 48 h of symptom onset. However, the rate of drug resistance has increased significantly. Currently all A/H3N2 isolates and the human A/H5N1 isolates that emerged after 2003 are resistant to the adamantanes, with increasing resistance to neuraminidase inhibitors being identified (32).
Due to increasing drug resistance, limited efficacy against severe infections, and issues with vaccine development and supply, there is an urgent need for new therapies for the prevention and treatment of influenza virus infection (19, 21). Targeting an influenza virus protein is the typical approach in formulating new vaccines and antiviral therapies. Unfortunately, viral evolution outpaces therapeutic advances. An alternative therapeutic approach is to target the cellular responses required for productive viral replication (10, 24, 31) or employ beneficial microbes that act as immunomodulators boosting an antiviral Th1 response (34). For example, in the late 1960s one study demonstrated that chronic infection with the parasite Toxoplasma gondii protected mice from mengovirus infection (35). More recently, both live T. gondii infection and particular T. gondii proteins were shown to inhibit HIV-1 replication in human peripheral blood mononuclear cells (PBMCs) and lymphoid tissues ex vivo (17, 39), suggesting that T. gondii could influence the outcome of a viral infection.
T. gondii is an obligate intracellular parasite of warm-blooded animals that elicits a potent Th1 response (13). Within the intermediate host, acute infection peaks 7 to 10 days postinfection (dpi), after which T. gondii differentiates into a chronic lifelong cyst form within the striated muscle and the central nervous system (9). Recent work suggests that a noninfectious extract of soluble T. gondii antigens (STAg) and even individual T. gondii proteins stimulate cellular and innate immune responses similar to those induced by parasites, indicating that live T. gondii is not required for Th1 induction (11, 26). Given the ability of T. gondii to modulate the Th1 response, in these studies we asked whether T. gondii or STAg induced protective immune responses against influenza virus infection. Our studies demonstrate that chronic T. gondii infection protects mice from severe highly pathogenic avian H5N1 virus infection even 4 months after T. gondii infection. More importantly, a single dose of STAg can be administered 2 days after H5N1 viral infection and protects up to 70% of infected animals. Mechanistically, the STAg-mediated induction of gamma interferon (IFN-γ) from natural killer (NK) cells is required for protection. Finally, we found that, depending on the initial viral dose, exogenous IFN-γ also protects against severe influenza virus infection.
MATERIALS AND METHODS
Laboratory facilities.
All experiments using H5N1 viruses were conducted in a biosafety level 3 (BSL-3) enhanced containment laboratory (36). Investigators were required to wear appropriate respirator equipment (Racal Health and Safety Inc., Frederick, MD). Mice were housed in HEPA-filtered, negative-pressure, vented isolation containers.
Chronic infection with T. gondii prior to influenza virus infection.
Seven- to 8-week-old C57BL/6J mice (Jackson Laboratory, Bar Harbor, ME) were intraperitoneally (i.p.) inoculated with differing numbers of wild-type (WT), 73F9, or N28E2 T. gondii parasites grown under standard conditions (human foreskin fibroblasts [HFFs] in Dulbecco's modified Eagle's medium [DMEM] with 10% fetal bovine serum, pH 7.2, at 37°C in 5% CO2). To quantify the number of T. gondii cysts prior to influenza virus infection, brains were isolated from a subset of mice, ground with a mortar and pestle, fixed with 3.0% formaldehyde for 20 min, and then permeabilized and blocked in 0.2% Triton X-100 with 3.0% bovine serum albumin for 30 min. T. gondii cysts in brain homogenates were stained with fluorescein isothiocyanate (FITC)-labeled Dolichos biflorus agglutinin (Vector Labs), three 5-μl samples of homogenate were mounted on microscope slides, and cyst numbers were counted by fluorescence microscopy as described previously (27). Samples from four mice were counted per experiment, and experiments were repeated twice. After we ensured that the number of T. gondii cysts per brain had established a chronic infection (range from 1,000 to 9,000 T. gondii cysts), mice were transported into a CDC-APHIS-approved BSL-3 enhanced laboratory, lightly anesthetized, and intranasally infected with 103 50% tissue culture infectious doses (TCID50) A/Hong Kong/483/1997 (HK/483) H5N1 influenza virus (1 50% minimum lethal dose [MLD50]). Mice were monitored daily for weight loss and clinical signs of infection (29). Any animal losing greater than 25% of its initial body weight and reaching a clinical score of 3 was humanely euthanized. At 0, 3, and 7 dpi, sera and lungs were collected from 2 controls and 3 or 4 infected mice from each group and monitored for viral titers (4, 22) and cytokine levels by enzyme-linked immunosorbent assay (ELISA) (46).
STAg treatment of influenza virus-infected mice.
STAg was prepared as described originally (7), except for the following changes. N28E2 parasites were grown in HFFs under mycoplasma-free (MycoAlert, Lonza, Switzerland) standard cell culture conditions. When the parasites were beginning to lyse the host cells, monolayers were scraped, passed twice through a 27-gauge needle, and pelleted at 420 × g. Parasites were washed in phosphate-buffered saline (PBS) without divalent cations and resuspended to 4 × 108 parasites per ml. After sonication with five 30-s pulses, parasites were centrifuged at 100,000 × g for 45 min and supernatants collected and stored at −70°C until use. An equal number of flasks containing HFFs without parasites were processed under the same conditions and resuspended to the same volume. Four- to 6-week-old female C57BL/6NCr, B6.129S7- Rag1tm1Mom/J, or B6.129S7-Ifngr1tm1Agt/J mice (National Cancer Institute, Frederick, MD, or Jackson Laboratory, Bar Harbor, ME) were infected with influenza virus as described above and treated at 2 and 4 dpi intravenously (i.v.) with 200 μg per mouse of PBS, HFF extract, or STAg. At 5 and 8 dpi, sera and lungs were collected from at least 2 controls and 3 infected mice from each group and monitored for viral titers (4, 22) and cytokine levels by ELISA (46).
NK cell depletion.
Natural killer (NK) cells were depleted similarly to procedures described in previous studies (8, 48). Briefly, at −1, 2, and 5 dpi, 100 μg of anti-NK1.1 monoclonal antibody or control IgG in 200 μl PBS (BioXCell, NH) was administered to mice by i.p. injection. To confirm depletion of NK cells, isolated spleens were analyzed for NK cell populations by flow cytometry on single-cell populations and whole tissue immunofluorescence detecting the presence of anti-NKp46 (NCR1; eBioscience, San Diego, CA)-positive splenocytes (47).
Administration of exogenous IFN-γ.
Exogenous IFN-γ treatment was administered to mice as previously described (48). Briefly, every 24 h for 4 days following influenza virus infection, mice were i.p. administered 200 μl PBS containing 2 × 104 specific activity units per dose of recombinant murine IFN-γ (PeproTech, Rocky Hill, NJ).
Statistical analysis.
Significance of the data was determined by using analysis of variance (ANOVA) or Student's t test on GraphPad Prism (San Diego, CA). The numbers of mice per group are given in the figure legends, and data are the averages from at least 2 independent experiments. Viral titers and IFN-γ levels are shown as results for individual mice from 2 independent experiments with either 3 or 4 mice per time point per group as noted in the figure legends.
RESULTS
Chronic T. gondii infection enhances survival from severe H5N1 influenza virus infection and decreases viral titers.
To determine if a chronic T. gondii infection protects against a lethal influenza virus infection, 7- to 8-week-old C57BL/6J mice were infected with a single dose of 5,000 wild-type (WT) T. gondii parasites. After 1 month, the number of T. gondii cysts per brain was quantified in a subset of the mice to ensure that the parasites had established a chronic infection (range from 1,000 to 9,000 T. gondii cysts). Mice chronically infected with T. gondii were then challenged with 103 TCID50 A/Hong Kong/483/1997 (HK/483, 1 MLD50) highly pathogenic avian H5N1 influenza virus. Mice were monitored daily for weight loss and clinical signs of infection for 20 days after influenza virus infection as described previously (4, 22, 29). Eighty percent of the mice infected with a single dose of WT T. gondii 1 month prior to H5N1 influenza virus infection survived, compared to 0% survival in the non-T. gondii-infected mice (Fig. 1A). T. gondii-mediated protection was independent of parasite inoculation dose, i.e., 50 to 5,000 parasites were similarly protective (Fig. 1A), demonstrating that a T. gondii preinfection protects mice from severe H5N1 virus infection.
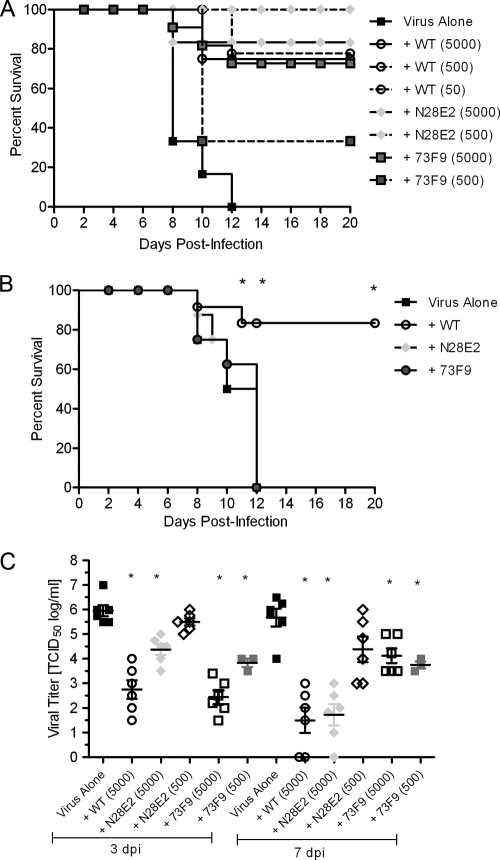
Fig. 1.
Chronic infection with T. gondii protects against H5N1 influenza virus infection and lowers viral titers. (A) C57BL/6 mice were inoculated with PBS (virus alone, n = 10 mice) or differing doses of the WT (n = 12), N28E2 (n = 12), or 73F9 (n = 12) strain of T. gondii and intranasally infected with 103 TCID50 (1 MLD50) HK/483 influenza virus 30 days later. Mice were then monitored for morbidity for 20 days after influenza virus infection. Results are from 2 independent experiments. (B) Four months after inoculation with PBS (virus alone, n = 8) or 5,000 WT (n = 8), 5,000 N28E2 (n = 8), or 5,000 73F9 (n = 8) T. gondii parasites, mice were infected with 103 TCID50 HK/483 influenza virus and monitored for morbidity for 20 dpi. Results are from 2 independent experiments. (C) C57BL/6 mice were inoculated with PBS (virus alone) or the WT, N28E2, or 73F9 strain of T. gondii and intranasally infected with 103 TCID50 HK/483 influenza virus 30 days later. Lungs were removed from 3 mice per group at 3 and 7 dpi, and viral titers were determined by TCID50 analysis. Results from one (lower-dose 73F9 infection) or two independent experiments are shown. Error bars represent standard errors of the means (SEM), and asterisks represent statistical significance at P values given in the text. Each point in panel C represents an individual mouse.
To determine if WT parasites were required, we examined the ability of attenuated T. gondii mutants to protect against H5N1 virus infection. The 73F9 mutant was previously found to be defective during acute infection and to have reduced numbers of brain cysts during chronic infection (12). For this study, the number of T. gondii cysts in mice infected with 5,000 73F9 parasites was significantly lower than the number in mice infected with the WT (only 30 to 50 cysts per brain). However, the 73F9 mutant was as protective as WT T. gondii but only with a high inoculum of parasites (compare 500 versus 5,000 73F9 parasites, Fig. 1A). In contrast, the N28E2 mutant, which is similar to WT T. gondii during acute infection but is unable to establish a persistent infection (5), produced similar numbers of cysts per brain as WT parasites, although the cysts were significantly smaller in size (data not shown), and induced 100% protection with the lower dose of parasites (500 N28E2 parasites, Fig. 1A). Not surprisingly, the mutant parasites failed to protect the mice at later times after T. gondii infection. At 4 months after T gondii infection, when mice have established a late chronic infection, only the mice infected with WT, but not 73F9 or N28E2, parasites survived H5N1 viral infection (Fig. 1B).
Survival from influenza virus infection can be achieved by reducing pathogen burden or limiting pathogen-induced immune damage (41). Therefore, we measured the levels of influenza virus in the lungs (4, 22). By 3 dpi, titers were already reduced by 3 log in mice inoculated with the WT and the higher dose of 73F9 T. gondii (Fig. 1C) (P < 0.001). The lower dose of 73F9 decreased viral load by ∼2 log (P < 0.001). In contrast, the most protective parasite, N28E2, had differential effects on viral titer. The higher inoculum (5,000 parasites) significantly decreased viral titers at 3 and 7 dpi (Fig. 1C) (P < 0.001). However, the lower dose of N28E2 (500 parasites), which protected 100% of the mice, failed to significantly decrease viral titers at either time postinfection (Fig. 1C). Finally, preinfection with T. gondii also protected from increased morbidity and mortality during infection with the mouse-adapted A/Puerto Rico/8/34 (PR/8) H1N1 virus, suggesting that these results are not specific to H5N1 influenza virus (data not shown).
Administration of STAg protects against H5N1 influenza virus infection.
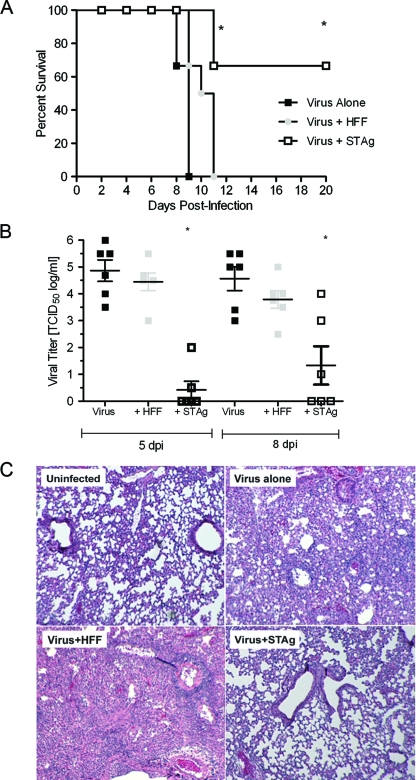
There are obvious concerns about the use of viable T. gondii as a protective therapy against influenza virus infection. Thus, we asked if the noninfectious extract of T. gondii called STAg, which stimulates cellular and innate immune responses similar to those induced by viable parasites (11, 26), was protective when administered after influenza virus infection. To examine this, mice were first intranasally inoculated with 103 TCID50 (1 MLD50) HK/483 H5N1 influenza virus. At 2 and 4 dpi, mice were intravenously administered PBS, STAg, or an equivalent dilution of human foreskin fibroblast (HFF) host cell extract and then monitored for weight loss and clinical signs of infection for 20 dpi. All of the mice administered PBS or HFF succumbed to influenza virus infection or had to be euthanized by 11 dpi (Fig. 2A). In contrast, 70% of mice administered STAg survived H5N1 virus infection. In addition, STAg administration dramatically decreased viral titers in the lungs. By 5 dpi (1 day after the second STAg administration), lung titers were below the limit of detection (P < 0.001) (Fig. 2B), and titers remained significantly decreased at 8 dpi compared to those for influenza virus-infected mice not treated with STAg (P < 0.003). Histopathology at 5 dpi showed that lungs of STAg-treated mice had less inflammation in the bronchium and alveolus, similar to lungs from control, noninfected animals (Fig. 2C). This result was in direct contrast to that for H5N1 virus-infected mice given PBS or HFF. These studies show that STAg administration 2 days after an H5N1 influenza virus infection significantly decreases viral titers and lung inflammation. This is exciting given that our current antiviral therapies must be administered within 48 h of exposure to be effective and require continual dosing (37).
Fig. 2.
T. gondii extract protects against H5N1 influenza virus infection, lowers viral titers, and reduces lung pathology when administered postinfection. (A) C57BL/6 mice were intranasally infected with 103 TCID50 (1 MLD50) HK/483 influenza virus; treated at 2 and 4 dpi with PBS (virus alone, n = 12 mice), HFF extract (virus + HFF, n = 12), or STAg (virus + STAg, n = 12); and monitored for morbidity for 20 dpi. (B) At 5 and 8 dpi, lungs were removed from 3 mice per group, and viral titers were determined by TCID50 analysis. Results from 2 independent experiments are shown. Error bars represent SEM, and asterisks represent statistical significance at P values given in the text. Each point represents an individual mouse. (C) Hematoxylin and eosin staining of the lungs from mice not infected with HK/483 influenza virus (uninfected) or mice infected with HK/483 virus and then treated with PBS (virus alone), HFF extract (virus+HFF), or STAg (virus+STAg) at 5 dpi. Magnification, ×10.
T. gondii and STAg increase IFN-γ levels, which is crucial for protection.
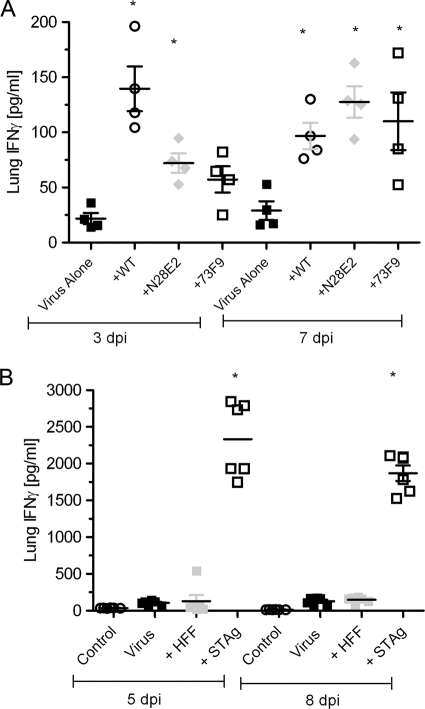
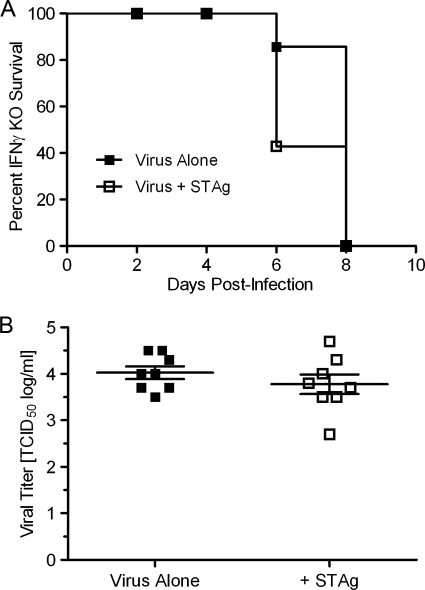
To begin defining the mechanism of T. gondii- and STAg-mediated survival, a panel of cytokines and chemokines were measured in the lungs of mice. While the levels of interleukin-1 (IL-1), IL-6, IL-10, tumor necrosis factor alpha (ΤΝF-α), transforming growth factor β (TGF-β), IFN-α, and IFN-γ were measured, only lung IFN-γ levels were significantly different in mice infected with T. gondii 1 month prior to H5N1 influenza virus infection. Within 3 dpi, mice chronically infected with T. gondii prior to influenza virus infection had significantly higher IFN-γ levels (Fig. 3A). This trend continued at 7 dpi (Fig. 3A). Similarly, cytokine analysis showed that H5N1 virus-infected mice administered STAg had significantly increased lung IFN-γ levels at 5 and 8 dpi (Fig. 3B). By 3 dpi, IFN-γ levels increased from 124 pg/ml in the mice given virus alone to over 2 ng/ml in the mice administered STAg (P < 0.01). To determine if this increased IFN-γ was important for STAg-mediated survival, IFN-γ receptor knockout (IFNgr1−/−) mice were infected with influenza virus and administered STAg. Unlike WT mice, IFN-γ receptor knockout mice did not survive H5N1 virus infection even with STAg (Fig. 4A), and there was no statistically significant decrease in viral titers at 5 dpi (Fig. 4B), suggesting that IFN-γ is necessary for STAg-mediated survival.
Fig. 3.
Lung IFN-γ levels are increased in influenza virus-infected mice receiving T. gondii. Lung IFN-γ levels were increased in the mice preinfected with 5,000 parasites of T. gondii (A) or administered STAg after HK/483 influenza virus infection (B). Results from 2 independent experiments are shown. Error bars represent SEM, and asterisks represent statistical significance at P values given in the text. Each point represents an individual mouse.
Fig. 4.
IFN-γ is required for STAg-mediated survival. (A) IFN-γ receptor knockout (KO) mice (B6.129S7-Ifngr1tm1Agt/J) were infected with 103 TCID50 (1 MLD50) HK/483 influenza virus, inoculated with PBS (virus alone, n = 8 mice) or STAg (virus + STAg, n = 8) at 2 and 4 dpi, and monitored for morbidity. Results represent two independent experiments. (B) At 5 dpi, lungs were isolated from 4 mice per group and viral titers were determined by TCID50 analysis. Results from 2 independent experiments are shown. Error bars represent SEM, and each point in panel B represents an individual mouse.
IFN-γ alone has therapeutic value against severe influenza virus infection depending on the viral dose administered.
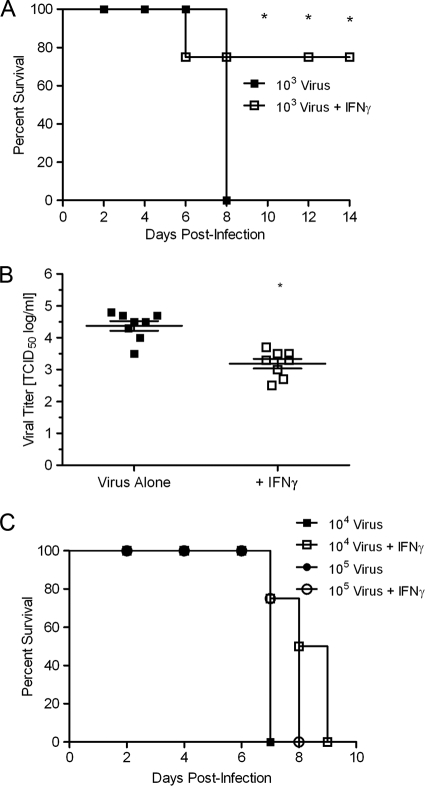
Our data suggest that IFN-γ is important for STAg-mediated protection against severe influenza virus infection. However, previous studies demonstrated that while IFN-γ is essential for the control of T. gondii infection (44), susceptibility to influenza A virus infection is not changed in mice with null mutations in the receptor for IFN-γ (33). Thus, to determine if IFN-γ was both necessary and sufficient for survival from H5N1 influenza virus infection, exogenous IFN-γ alone was administered. Briefly, mice were intranasally inoculated with 103 TCID50 (1 MLD50) H5N1 influenza virus, intravenously administered 2 × 104 specific activity units of IFN-γ every 24 h for 4 days, and then monitored for weight loss and clinical signs of infection for 14 dpi. Seventy-five percent of the mice administered IFN-γ survived H5N1 viral infection, compared to 0% of the untreated, infected mice (Fig. 5A). Viral titers were slightly reduced in the IFN-γ-treated mice (Fig. 5B), although not to the same levels as those in mice administered STAg (Fig. 2B). Additionally, the IFN-γ-mediated protection was dependent on the viral inoculation dose. Mice inoculated with 104 TCID50 (10 MLD50) or 105 TCID50 (100 MLD50) did have slightly prolonged survival when administered exogenous IFN-γ, although all of the mice ultimately succumbed to infection (data not shown). These studies suggest that while exogenous IFN-γ can be protective, the effects may be overcome by a high initial viral dose.
Fig. 5.
Exogenous IFN-γ can protect mice from H5N1 virus infection depending on the initial viral dose. (A) Beginning 24 h after infection with 103 TCID50 (1 MLD50) HK/483 influenza virus, C57BL/6 mice were administered PBS (virus, n = 13 mice) or recombinant IFN-γ (virus + IFN-γ, n = 13) daily for 4 days; mice were then monitored for morbidity for 14 dpi. (B) At 5 dpi, lungs were isolated from 4 mice per group and viral titers were determined by TCID50 analysis. (C) Following the same IFN-γ treatment regimen described above, C57BL/6 mice were infected with 104 (n = 10) or 105 (n = 10) TCID50 HK/483 influenza virus and then monitored for morbidity for 10 dpi. Results from 2 independent experiments are shown. Error bars represent SEM, and asterisks represent statistical significance at P values given in the text. Each point in panel B represents an individual mouse.
NK cells are the source of STAg-induced IFN-γ.
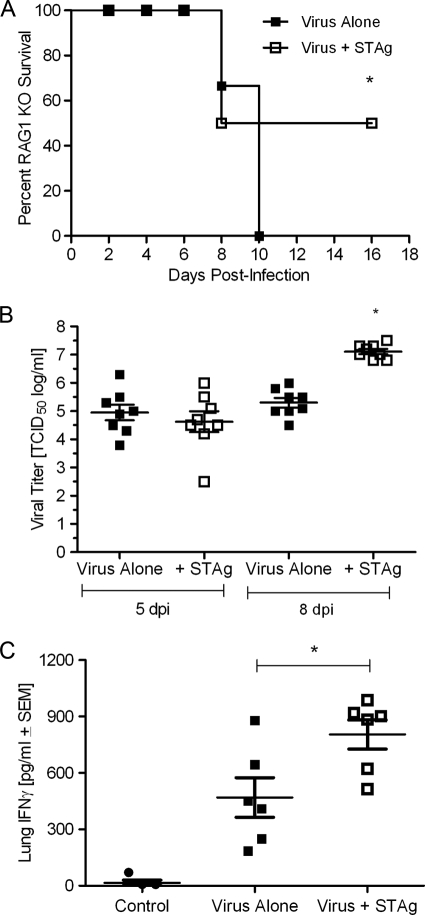
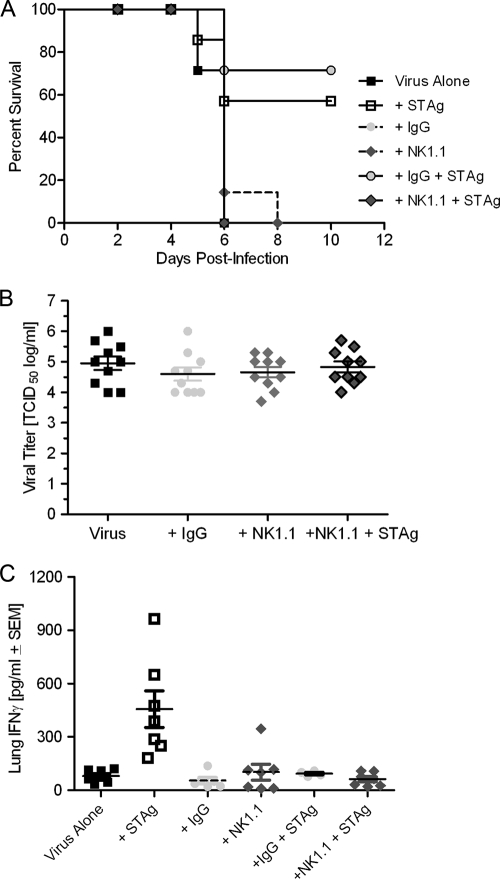
The primary sources of IFN-γ are T cells and NK cells (43, 45). To determine the source, RAG−/− mice (T and B cell deficient) or NK cell-depleted mice (anti-NK1.1-mediated depletion) were infected with influenza virus and administered STAg. Mortality of the RAG−/− mice was 50% with STAg administration and 100% without (Fig. 6A), compared to 70% protection in the WT mice (Fig. 2A). However, unlike WT mice, in which STAg administration reduced viral titers within 5 dpi (Fig. 2B), there was no statistically significant reduction in viral titers in STAg-treated RAG−/− mice compared to those in untreated, infected mice (Fig. 6B), and lung IFN-γ levels remain elevated compared to those for the group given virus alone (Fig. 6C). In fact, viral titers were ∼2-log higher in the STAg-treated group at 8 dpi (P < 0.002), suggesting that while T and/or B cells were not required for STAg-mediated protection, they may be important for the STAg-induced reduction in viral titers. In contrast to results for RAG−/− mice, STAg failed to protect influenza virus-infected mice depleted of NK cells by anti-NK1.1 antibody (Fig. 7A). Further, STAg administration failed to reduce viral titers (Fig. 7B), and no elevation of lung IFN-γ levels was observed compared to the level in WT mice (Fig. 7C and 2B). These results demonstrate that NK cells are necessary for the beneficial effects of STAg.
Fig. 6.
STAg-induced protection requires the adaptive immune response for viral clearance but not protection. (A) RAG1 knockout mice (B6.129S7- Rag1tm1Mom/J) were infected with 103 TCID50 (1 MLD50) HK/483 influenza virus and then treated at 2 and 4 dpi with either PBS (virus alone, n = 12 mice) or STAg (virus + STAg, n = 12) and monitored for morbidity. (B) At 5 and 8 dpi, lungs were isolated from 4 mice per group and viral titers were determined by TCID50 analysis. (C) Lung IFN-γ levels were measured from 3 mice per group by ELISA. Results from 2 independent experiments are shown. Error bars represent SEM, and asterisks represent statistical significance at P values given in the text. Each point in panels B and C represents an individual mouse.
Fig. 7.
STAg fails to protect NK cell-depleted mice and does not increase lung IFN-γ levels. (A) Prior to infection, C57BL/6 mice were treated with PBS (virus alone, n = 6 to 8 mice), isotype control IgG (n = 6 to 8), or anti-NK1.1 antibody to deplete NK cells (n = 6 to 8). Mice were then infected with 103 TCID50 (1 MLD50) HK/483 influenza virus, treated with STAg, and monitored for morbidity for 10 dpi. (B and C) At 5 dpi, lungs were isolated from 3 or 4 mice per group. Viral titers were determined by TCID50 analysis (B), and lung IFN-γ levels were determined by ELISA (C). Results from 3 independent experiments are shown. Error bars represent SEM. Each point in panels B and C represents an individual mouse.
DISCUSSION
These studies demonstrate that an underlying infection with the apicomplexan parasite T. gondii lessens the severity of influenza virus infection in mice. More importantly, a noninfectious extract of T. gondii (STAg) is protective even when administered 2 days after infection. Both chronic T. gondii infection and STAg administration resulted in reduced viral titers in the lungs, suggesting that the mechanism of protection was modulation of viral replication. However, we also saw increased survival in the mice preinfected with a low inoculum of the N28E2 mutant. N28E2 consistently afforded the best survival against influenza virus-induced mortality (Fig. 1A), and yet viral titers in the lungs were differentially modulated; a high-dose inoculum (5,000 parasites) significantly lowered viral titers, but a low dose (500 parasites) had no effect (Fig. 1C). Further, RAG−/− mice were also protected from H5N1 viral infection and yet viral titers were actually increased in these mice, suggesting that T. gondii-induced survival may not be completely dependent on lowering viral titers, highlighting that the disease severity of influenza virus infection does not necessarily correlate with viral load.
To begin to define the mechanism of protection, we performed cytokine/chemokine analyses that led us to investigate the role of IFN-γ. A great deal is known about the regulation of IFN-γ by T. gondii (reviewed in reference 6), and IFN-γ is recognized as the major mediator of host resistance against T. gondii (40, 44). Much less is known about the role of IFN-γ in influenza virus infection. Several studies using antibody-mediated depletion (1), targeted disruption of the IFN-γ gene (18), and IFN-γ receptor knockout mice (33) demonstrated that IFN-γ was not essential for recovery from a sublethal dose of influenza virus. However, a study by Baumgarth and Kelso elegantly demonstrated that IFN-γ exerted a marked effect on the local immune responses in the lung parenchyma and was required for optimal effector leukocyte migration and/or recruitment into the inflamed tissue site (1). In support of this work, it was recently shown that early administration of exogenous IFN-γ during influenza virus infection stimulates NK cell proliferation and function in the infected lungs (48). Although this treatment did not lead to significant decreases in lung viral titers, it protected mice from a lethal H1N1 A/Puerto Rico/8/34 (PR/8) influenza virus infection in an NK cell-dependent manner, results similar to our findings. One caveat is that the protective ability of IFN-γ was dependent on the initial viral inoculum. This result suggests that there is a balance between IFN-γ-mediated protection and overwhelming viral infection. Although our work suggests that IFN-γ is required for STAg-mediated protection, at this time we cannot definitively rule out a role for other, as yet unidentified cellular factors.
IFN-γ is arguably one of the most broadly acting antimicrobial-inducing and host defense-enhancing cytokines described with widespread antiparasitic, antifungal, and antibacterial activities (30). However, less is known about its antiviral activities. Treatment of cells with IFN-γ induces a cascade of inducible genes with varied functions, many of which could be directly antiviral. Human lung epithelial cells treated with exogenous IFN-γ show marked increases in intracellular signaling and antiviral components, including phosphorylated signal transducer and activator of T cells 1 (STAT-1), interferon regulatory factor 9 (IRF-9), myxovirus resistance protein 1 (MxA, or Mx1), protein kinase R (PKR, or EIF2AK2), and 2′-5′-oligoadenylate synthetase 1 (OAS1) (28). Not surprisingly, exogenous administration of IFN-γ resulted in reduced replication of encephalomyocarditis virus (ECMV) and hepatitis B virus in vitro (2), and vesicular stomatitis virus (VSV) had enhanced replication when propagated in IFN-γ receptor-deficient primary embryonic fibroblasts (20). An alternative mechanism for increased protection that is under investigation is modulation of the lung inflammatory responses. IFN-γ is known to inhibit a Th2 response, which could be immunopathogenic. Indeed, the absence of IFN-γ leads to increased Th2 responses in the lungs during influenza virus infection (50) and can influence the development of pulmonary immunopathology (49). A study by Wiley et al. demonstrated that CD8-Tc2 effector cells lacking IFN-γ induced significantly more lung damage and dysfunction (49). IFN-γ is also required for protease-activated receptor 2 (PAR2)-mediated protection against influenza virus pathogenesis, although the precise mechanism of action is unclear (23). Clearly, more information on IFN-γ diverse antiviral activities is needed.
Studies from the late 1960s and early 1970s demonstrated that mice colonized with T. gondii were protected from bacterial (Listeria monocytogenes and Salmonella enterica serovar Typhimurium [38]), helminth (Schistosoma mansoni [14, 25]), fungus (Cryptococcus neoformans [14]), and even viral (mengovirus [35]) infections. Although a specific mechanism for protection was not identified, these were among the first studies to suggest that T. gondii could elicit an innate immune response that could reduce the pathogenicity of other microbes. To our knowledge, these are the first studies to describe a parasite extract that generates a protective immune response against H5N1 influenza virus infection. Given that T. gondii can enhance survival without a significant modulation of viral titers, these studies demonstrate that in this model, viral titers are severable from disease pathogenesis. Overall, T. gondii infection and STAg are important tools for understanding the immune responses necessary for survival against highly pathogenic avian H5N1 influenza virus infection and may lead to new therapies that specifically upregulate these responses.
ACKNOWLEDGMENTS
We thank Alexander Klimov at the Centers for Disease Control and Prevention for A/Hong Kong/483/1997 (HK/483) H5N1 influenza virus; Rob Striker, Paul Thomas, and Anna Huttenlocher for critical reviews of the manuscript; and Gordon Brown, Ned Ruby, Margaret McFall-Ngai, and Richard Webby for insightful discussions.
This work was supported by an HHMI Gilliam fellowship (K.B.O.), AHA 0840059N and ACS RSG-07-202-01 awards (L.J.K.), and NIH AI059049 and U54 AI057157 from the Southeastern Regional Center of Excellence for Emerging Infections and Biodefense (S.S.-C.). This work was also partially supported by the American Lebanese Syrian Associated Charities (ALSAC).
Footnotes
Published ahead of print on 6 July 2011.
REFERENCES
- 1. Baumgarth N., Kelso A. 1996. Functionally distinct T cells in three compartments of the respiratory tract after influenza virus infection. Eur. J. Immunol. 26:2189–2197 [DOI] [PubMed] [Google Scholar]
- 2. Brunelle M. N., et al. 2010. Inhibition of hepatitis B virus DNA replication by a thermostable interferon-gamma variant. Antivir. Ther. 15:861–869 [DOI] [PubMed] [Google Scholar]
- 3. Capua I., Cattoli G. 2009. Flu: vaccinate to cut risk of chimaeric virus emerging. Nature 460:571. [DOI] [PubMed] [Google Scholar]
- 4. Carlson C. M., et al. 2010. Transforming growth factor-beta: activation by neuraminidase and role in highly pathogenic H5N1 influenza pathogenesis. PLoS Pathog. 6:e1001136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Craver M. P., Rooney P. J., Knoll L. J. 2010. Isolation of Toxoplasma gondii development mutants identifies a potential proteophosphoglycan that enhances cyst wall formation. Mol. Biochem. Parasitol. 169:120–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Denkers E. Y. 2003. From cells to signaling cascades: manipulation of innate immunity by Toxoplasma gondii. FEMS Immunol. Med. Microbiol. 39:193–203 [DOI] [PubMed] [Google Scholar]
- 7. Denkers E. Y., Gazzinelli R. T., Hieny S., Caspar P., Sher A. 1993. Bone marrow macrophages process exogenous Toxoplasma gondii polypeptides for recognition by parasite-specific cytolytic T lymphocytes. J. Immunol. 150:517–526 [PubMed] [Google Scholar]
- 8. Denkers E. Y., Gazzinelli R. T., Martin D., Sher A. 1993. Emergence of NK1.1+ cells as effectors of IFN-gamma dependent immunity to Toxoplasma gondii in MHC class I-deficient mice. J. Exp. Med. 178:1465–1472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dubey J. P. 1998. Advances in the life cycle of Toxoplasma gondii. Int. J. Parasitol. 28:1019–1024 [DOI] [PubMed] [Google Scholar]
- 10. Ehrhardt C., Ludwig S. 2009. A new player in a deadly game: influenza viruses and the PI3K/Akt signalling pathway. Cell. Microbiol. 11:863–871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Flores M., et al. 2008. Macrophage migration inhibitory factor (MIF) is critical for the host resistance against Toxoplasma gondii. FASEB J. 22:3661–3671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Frankel M. B., Mordue D. G., Knoll L. J. 2007. Discovery of parasite virulence genes reveals a unique regulator of chromosome condensation 1 ortholog critical for efficient nuclear trafficking. Proc. Natl. Acad. Sci. U. S. A. 104:10181–10186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gazzinelli R. T., Denkers E. Y., Sher A. 1993. Host resistance to Toxoplasma gondii: model for studying the selective induction of cell-mediated immunity by intracellular parasites. Infect. Agents Dis. 2:139–149 [PubMed] [Google Scholar]
- 14. Gentry L. O., Remington J. S. 1971. Resistance against Cryptococcus conferred by intracellular bacteria and protozoa. J. Infect. Dis. 123:22–31 [DOI] [PubMed] [Google Scholar]
- 15. Ghedin E., et al. 2009. Mixed infection and the genesis of influenza virus diversity. J. Virol. 83:8832–884119553313 [Google Scholar]
- 16. Girard M. P., Tam J. S., Assossou O. M., Kieny M. P. 2010. The 2009 A (H1N1) influenza virus pandemic: a review. Vaccine 28:4895–4902 [DOI] [PubMed] [Google Scholar]
- 17. Golding H., et al. 2003. Inhibition of HIV-1 infection by a CCR5-binding cyclophilin from Toxoplasma gondii. Blood 102:3280–3286 [DOI] [PubMed] [Google Scholar]
- 18. Graham M. B., et al. 1993. Response to influenza infection in mice with a targeted disruption in the interferon gamma gene. J. Exp. Med. 178:1725–1732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hayden F. 2009. Developing new antiviral agents for influenza treatment: what does the future hold? Clin. Infect. Dis. 48(Suppl. 1):S3–S13 [DOI] [PubMed] [Google Scholar]
- 20. Huang S., et al. 1993. Immune response in mice that lack the interferon-gamma receptor. Science 259:1742–1745 [DOI] [PubMed] [Google Scholar]
- 21. Ilyinskii P. O., Thoidis G., Shneider A. M. 2008. Development of a vaccine against pandemic influenza viruses: current status and perspectives. Int. Rev. Immunol. 27:392–426 [DOI] [PubMed] [Google Scholar]
- 22. Jones J. C., Turpin E. A., Bultmann H., Brandt C. R., Schultz-Cherry S. 2006. Inhibition of influenza virus infection by a novel antiviral peptide that targets viral attachment to cells. J. Virol. 80:11960–11967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Khoufache K., et al. 2009. Protective role for protease-activated receptor-2 against influenza virus pathogenesis via an IFN-γ-dependent pathway. J. Immunol. 182:7795–7802 [DOI] [PubMed] [Google Scholar]
- 24. Ludwig S., Planz O. 2008. Influenza viruses and the NF-kappaB signaling pathway—towards a novel concept of antiviral therapy. Biol. Chem. 389:1307–1312 [DOI] [PubMed] [Google Scholar]
- 25. Mahmoud A. A., Warren K. S., Strickland G. T. 1976. Acquired resistance to infection with Schistosoma mansoni induced by Toxoplasma gondii. Nature 263:56–57 [DOI] [PubMed] [Google Scholar]
- 26. Mason N. J., Liou H. C., Hunter C. A. 2004. T cell-intrinsic expression of c-Rel regulates Th1 cell responses essential for resistance to Toxoplasma gondii. J. Immunol. 172:3704–3711 [DOI] [PubMed] [Google Scholar]
- 27. Mordue D. G., Scott-Weathers C. F., Tobin C. M., Knoll L. J. 2007. A patatin-like protein protects Toxoplasma gondii from degradation in activated macrophages. Mol. Microbiol. 63:482–496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Morrow A. N., Schmeisser H., Tsuno T., Zoon K. C. 2011. A novel role for IFN-stimulated gene factor 3II in IFN-γ signaling and induction of antiviral activity in human cells. J. Immunol. 186:1685–1693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Morton D. B. 2000. A systematic approach for establishing humane endpoints. ILAR J. 41:80–86 [DOI] [PubMed] [Google Scholar]
- 30. Murray H. W. 1996. Current and future clinical applications of interferon-gamma in host antimicrobial defense. Intensive Care Med. 22(Suppl. 4):S456–S461 [DOI] [PubMed] [Google Scholar]
- 31. Pleschka S. 2008. RNA viruses and the mitogenic Raf/MEK/ERK signal transduction cascade. Biol. Chem. 389:1273–1282 [DOI] [PubMed] [Google Scholar]
- 32. Poland G. A., Jacobson R. M., Ovsyannikova I. G. 2009. Influenza virus resistance to antiviral agents: a plea for rational use. Clin. Infect. Dis. 48:1254–1256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Price G. E., Gaszewska-Mastarlarz A., Moskophidis D. 2000. The role of alpha/beta and gamma interferons in development of immunity to influenza A virus in mice. J. Virol. 74:3996–4003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pulendran B. 2004. Modulating TH1/TH2 responses with microbes, dendritic cells, and pathogen recognition receptors. Immunol. Res. 29:187–196 [DOI] [PubMed] [Google Scholar]
- 35. Remington J. S., Merigan T. C. 1969. Resistance to virus challenge in mice infected with protozoa or bacteria. Proc. Soc. Exp. Biol. Med. 131:1184–1188 [DOI] [PubMed] [Google Scholar]
- 36. Richmond J. Y., McKinney R. W., III (ed.). 1993. Biosafety in microbiological and biomedical laboratories. U.S. Department of Health and Human Services, Washington, DC, and Centers for Disease Control, Atlanta, GA [Google Scholar]
- 37. Ruf B. R., Szucs T. 2009. Reducing the burden of influenza-associated complications with antiviral therapy. Infection 37:186–196 [DOI] [PubMed] [Google Scholar]
- 38. Ruskin J., Remington J. S. 1968. Immunity and intracellular infection: resistance to bacteria in mice infected with a protozoan. Science 160:72–74 [DOI] [PubMed] [Google Scholar]
- 39. Sassi A., et al. 2009. Toxoplasma gondii inhibits R5 HIV-1 replication in human lymphoid tissues ex vivo. Microbes Infect. 11:1106–1113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Scharton-Kersten T. M., et al. 1996. In the absence of endogenous IFN-gamma, mice develop unimpaired IL-12 responses to Toxoplasma gondii while failing to control acute infection. J. Immunol. 157:4045–4054 [PubMed] [Google Scholar]
- 41. Schneider D. S., Ayres J. S. 2008. Two ways to survive infection: what resistance and tolerance can teach us about treating infectious diseases. Nat. Rev. Immunol. 8:889–895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schnitzler S. U., Schnitzler P. 2009. An update on swine-origin influenza virus A/H1N1: a review. Virus Genes 39:279–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Strehl B., et al. 2005. Interferon-gamma, the functional plasticity of the ubiquitin-proteasome system, and MHC class I antigen processing. Immunol. Rev. 207:19–30 [DOI] [PubMed] [Google Scholar]
- 44. Suzuki Y., Orellana M. A., Schreiber R. D., Remington J. S. 1988. Interferon-gamma: the major mediator of resistance against Toxoplasma gondii. Science 240:516–518 [DOI] [PubMed] [Google Scholar]
- 45. Tassi I., Klesney-Tait J., Colonna M. 2006. Dissecting natural killer cell activation pathways through analysis of genetic mutations in human and mouse. Immunol. Rev. 214:92–105 [DOI] [PubMed] [Google Scholar]
- 46. Tumpey T. M., Lu X., Morken T., Zaki S. R., Katz J. M. 2000. Depletion of lymphocytes and diminished cytokine production in mice infected with a highly virulent influenza A (H5N1) virus isolated from humans. J. Virol. 74:6105–6116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Walzer T., et al. 2007. Identification, activation, and selective in vivo ablation of mouse NK cells via NKp46. Proc. Natl. Acad. Sci. U. S. A. 104:3384–3389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Weiss I. D., et al. 2010. IFN-gamma treatment at early stages of influenza virus infection protects mice from death in a NK cell-dependent manner. J. Interferon Cytokine Res. 30:439–449 [DOI] [PubMed] [Google Scholar]
- 49. Wiley J. A., Cerwenka A., Harkema J. R., Dutton R. W., Harmsen A. G. 2001. Production of interferon-gamma by influenza hemagglutinin-specific CD8 effector T cells influences the development of pulmonary immunopathology. Am. J. Pathol. 158:119–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wohlleben G., Erb K. J. 2004. The absence of IFN-gamma leads to increased Th2 responses after influenza A virus infection characterized by an increase in CD4+ but not CD8+ T cells producing IL-4 or IL-5 in the lung. Immunol. Lett. 95:161–166 [DOI] [PubMed] [Google Scholar]
- 51. Writing Committee of the WHO Consultation on Clinical Aspects of Pandemic (H1N1) 2009 Influenza 2010. Clinical aspects of pandemic 2009 influenza A (H1N1) virus infection. N. Engl. J. Med. 362:1708–1719 [DOI] [PubMed] [Google Scholar]
- 52. Yen H. L., Webster R. G. 2009. Pandemic influenza as a current threat. Curr. Top. Microbiol. Immunol. 333:3–24 [DOI] [PubMed] [Google Scholar]