Abstract
Ebola virus is the etiologic agent of a lethal hemorrhagic fever in humans and nonhuman primates with mortality rates of up to 90%. Previous studies with Zaire Ebola virus (ZEBOV), mouse-adapted virus (MA-ZEBOV), and mutant viruses (ZEBOV-NPma, ZEBOV-VP24ma, and ZEBOV-NP/VP24ma) allowed us to identify the mutations in viral protein 24 (VP24) and nucleoprotein (NP) responsible for acquisition of high virulence in mice. To elucidate specific molecular signatures associated with lethality, we compared global gene expression profiles in spleen samples from mice infected with these viruses and performed an extensive functional analysis. Our analysis showed that the lethal viruses (MA-ZEBOV and ZEBOV-NP/VP24ma) elicited a strong expression of genes 72 h after infection. In addition, we found that although the host transcriptional response to ZEBOV-VP24ma was nearly the same as that to ZEBOV-NP/VP24ma, the contribution of a mutation in the NP gene was required for a lethal phenotype. Further analysis indicated that one of the most relevant biological functions differentially regulated by the lethal viruses was the inflammatory response, as was the induction of specific metalloproteinases, which were present in our newly identify functional network that was associated with Ebola virus lethality. Our results suggest that this dysregulated proinflammatory response increased the severity of disease. Consequently, the newly discovered molecular signature could be used as the starting point for the development of new drugs and therapeutics. To our knowledge, this is the first study that clearly defines unique molecular signatures associated with Ebola virus lethality.
INTRODUCTION
Ebola virus is the etiologic agent of a highly lethal hemorrhagic fever in human and nonhuman primates with mortality rates of up to 90% in humans (6, 47, 53). Because of its high mortality rate, the potential for human-to-human transmission, and the lack of an approved vaccine or therapy, the virus is classified as a category A pathogen (10) requiring biosafety level 4 (BSL-4) containment (51). Several groups have recently reported potential vaccine candidates (19, 44), and some have been tested in humans (33, 36); furthermore, a laboratory worker received an experimental live-attenuated vaccine on an emergency treatment protocol after being injured by a needle stick while handling Zaire Ebola virus (ZEBOV) (19, 50). Still, new insights into Ebola virus pathogenesis are required to aid in vaccine and antiviral drug development.
Severe disease outcome has previously been attributed to a combination of rapid uncontrolled viral replication, host immune suppression, and vascular dysfunction (19, 30, 38). Data collected from fatal human cases and from animal models indicates that the majority of organs, including the spleen, blood, liver, and lymph nodes, yield high virus titers, with immunohistochemistry showing multiple cell types, including hepatocytes, mononuclear, and endothelial cells, infected with Ebola virus (15, 22–24, 48). Data collected from fatal human cases and nonhuman primate studies have also shown that Ebola virus infection triggers a strong inflammatory response that likely contributes to disease progression (4, 23, 31). In addition, apoptosis of lymphocytes is a characteristic feature of Ebola virus infection (3, 21); however, it appears to be nonessential for Ebola virus disease progression (7). The current understanding of Ebola virus pathogenesis is that activation of proinflammatory cytokines and chemokines results in dysregulation of the immune, vascular, and coagulation systems, creating multiple organ failure and shock (19).
In an effort to understand the viral determinants of the high pathogenicity of ZEBOV, we previously generated recombinant viruses containing one or more genes from a lethal mouse-adapted variant (17). The mouse-adapted virus (MA-ZEBOV) differs from wild-type ZEBOV (WT-ZEBOV; nonlethal in mice) in 13 nucleotide positions, including eight amino acid changes and one amino acid insertion. Two of the recombinant viruses consisted of ZEBOV containing the mouse-adapted mutations found in either the nucleoprotein (NP) (ZEBOV-NPma) or viral protein 24 (VP24) (ZEBOV-VP24ma) genes; these viruses exhibited a nonlethal phenotype in mice. An additional recombinant virus consisted of ZEBOV containing the mouse-adapted mutations found in both the NP and VP24 genes (ZEBOV-NP/VP24ma); this virus exhibited a lethal phenotype in mice. Mutations acquired in the VP24 and NP genes are therefore sufficient for high virulence in mice.
In the present study, we used these genetically characterized viruses and global transcriptional profiling to gain new insights into the viral determinants and mechanisms underlying Ebola virus pathogenicity. Analysis of the host response elicited against WT-ZEBOV, MA-ZEBOV, and recombinant viruses revealed molecular signatures associated with pathogenesis. We found transcriptional signatures associated with proinflammatory and proapoptotic genes in response to both of the lethal viruses, MA-ZEBOV and ZEBOV-NP/VP24ma; furthermore, the induction of genes encoding specific metalloproteinases was associated with lethality. In addition, we found that although the host transcriptional response to ZEBOV-VP24ma was nearly the same as that to ZEBOV-NP/VP24ma, the contribution of a mutation in the NP gene was required for a lethal phenotype.
MATERIALS AND METHODS
Ethics statement.
All animal experiments were performed under an approved animal use document and according to the guidelines of the Canadian Council on Animal Care in the BSL-4 facility of the National Microbiology Laboratory of the Public Health Agency of Canada.
Viruses.
Five different recombinant viruses were used in this study. The mouse-adapted virus (MA-ZEBOV) and the double-mutant virus (ZEBOV-NP/VP24ma) were lethal in mice. The wild-type Zaire Ebola virus (WT-ZEBOV) and the single-mutant viruses (ZEBOV-NPma and ZEBOV-VP24ma) were not lethal in mice. All viruses used in the present study have been described previously by our group (17).
Mouse experiments.
Six-week-old female BALB/c mice were obtained from a commercial supplier (Charles River Laboratories, Wilmington, MA). All mice were housed in microisolator cages and allowed to acclimatize for 5 days prior to use in experiments. To assess virus growth characteristics of mice, groups of 5 animals per time point for each virus (100 animals total) were inoculated intraperitoneally with 5 focus-forming units (FFU) of virus (corresponding to approximately 500 50% mouse lethal doses [MLD50] for MA-ZEBOV). At 12, 24, 48, and 72 h postinfection, the spleen and blood were collected from five infected mice, and the spleen samples were homogenized. Viral infectivity titers were determined by use of a focus-forming assay using Vero E6 cells (17).
RNA preparation and oligonucleotide microarray processing.
RNA was extracted from mouse spleens using a Qiagen RNeasy Minikit with RNAlater solution (Qiagen, Valencia, CA) according to the manufacturer's instructions. RNA was further purified using RNeasy columns (Qiagen, Valencia, CA). RNA samples were spectroscopically verified for purity, and the quality of the intact RNA was assessed using an Agilent 2100 Bioanalyzer. For each set of treatment conditions, three of the five RNA samples exhibiting the highest RNA integrity number (RIN) determined using the Bioanalyzer were used for microarray analysis. cRNA probes were generated from each sample by the use of an Agilent one-color LowInput Quick Amp labeling kit (Agilent Technologies, Santa Clara, CA). Individual cRNA samples were hybridized to Agilent mouse whole-genome oligonucleotide 4-by-44 microarrays (approximately 39,000 unique mouse genes) according to the manufacturer's instructions. To enable examination of animal-to-animal variation as part of the data analysis, samples from individual animals were not pooled; included were samples from three animals per time point for each virus (60 animals total). Select samples were hybridized a second time (n = 2 technical replicates) to verify the quality of the process. Slides were scanned with an Agilent DNA microarray scanner, and the resulting images were analyzed using Agilent Feature Extractor version 8.1.1.1. This software was used to perform image analysis, including significance of signal and spatial detrending and to apply a universal error model. For these hybridizations, the most conservative error model was applied. Raw data were then loaded into a custom-designed laboratory information management system (LIMS). Data were warehoused in a Labkey system (Labkey, Inc., Seattle, WA) and analyzed using GeneData Analyst 2.2.1 software (GeneData Solutions In Silico, San Francisco, CA), and Spotfire DecisionSite for Functional Genomics 9.1 software (Tibco Spotfire, Somerville, MA). Primary data are available (http://viromics.washington.edu) in accordance with proposed Minimum Information About a Microarray Experiment (MIAME) standards.
Microarray analysis and bioinformatics.
Global gene expression in infected spleens was compared to that in control RNA prepared from a pool of equal masses of total RNA from spleen tissue of five uninfected mice. Probe labeling and microarray slide hybridization were performed as described elsewhere (11).
Raw data from Agilent Feature Extractor was normalized by applying the central tendency algorithm with standard reference set at the 75th percentile of each microarray. Correlations between virus titers and gene expression were determined by Pearson's correlation coefficients. One- or two-way analysis of variance (ANOVA) was carried out for various groups of samples stratified by virus infection and/or time point (see Results for more grouping details). The Benjamini and Hochberg algorithm was used to control the false discovery rate (FDR) of multiple testing (5). All statistical analyses were performed using GeneData Analyst 2.2.1.
Functional and network analysis of statistically significant gene expression changes was performed using Ingenuity Pathways Analysis (IPA). The analysis considered all genes from statistical analysis results and those associated with biological functions in the IPA Knowledge Base. For all gene set enrichment analyses, Fisher's exact test was used to determine the probability that each biological function assigned to the genes within each statistical analysis result was due to chance alone.
qRT-PCR.
Quantitative real-time reverse transcription-PCR (qRT-PCR) was performed with samples from individual animals to validate specific cellular gene expression changes detected by microarray. A QuantiTect reverse transcription kit (Qiagen, Valencia, CA) was used to generate cDNA. qRT-PCR was run on an ABI 7500 PCR system, using TaqMan chemistry (Applied Biosystems, Foster City, CA). Gene expression assays specific to mouse cellular genes were purchased from Applied Biosystems. Differences in gene expression are represented as the quantification relative to a calibrator (log10 RQ) and normalized to a reference, using the 2−Ct method (35).
RESULTS
Virus titer has limited correlation with differential gene expression.
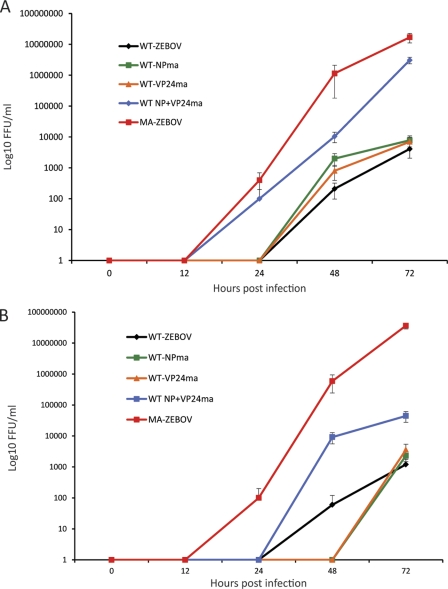
Our previous study indicated that mutations in the ZEBOV NP and VP24 proteins were responsible for the acquisition of virulence in mice; animals infected with MA-ZEBOV or the double mutant ZEBOV-NP/VP24ma succumbed to infection at 6.7 ± 1.7 days postinfection (p.i.) and 8.4 ± 0.5 days p.i., respectively, when inoculated with 100 MLD50 (1 FFU/animal) (17). Therefore, to elucidate molecular signatures associated with Ebola virus pathogenicity, we used a functional genomics approach to analyze global gene expression in the spleens of mice infected with different Ebola viruses. We investigated the global transcriptional changes in the spleen because this organ is a major target during Ebola virus infection (20, 24). As we previously reported, BALB/c mice were resistant to infection with WT-ZEBOV or the single mutants ZEBOV-NPma or ZEBOV-VP24ma. However, animals infected with MA-ZEBOV or the double mutant ZEBOV-NP/VP24ma succumbed to infection. The lethal viruses (MA-ZEBOV and ZEBOV-NP/VP24ma) replicated more efficiently than the nonlethal ones (WT-ZEBOV, ZEBOV-NPma, and ZEBOV-VP24ma) in spleen and blood (Fig. 1). Results from viral titration divided these viruses into distinct lethal and nonlethal groups. There was also a slight difference in replication between the lethal viruses MA-ZEBOV and ZEBOV-NP/VP24ma at 48 and 72 h after infection.
Fig. 1.
Lethal MA-ZEBOV and ZEBOV-NP/VP24ma viruses replicate more efficiently than nonlethal ZEBOV, ZEBOV-NPma, and ZEBOV-VP24ma viruses in mice. Mice were inoculated intraperitoneally with 5 FFU of virus (corresponding to approximately 500 MLD50 for MA-ZEBOV). At 12, 24, 48, and 72 h postinfection, spleens (A) and blood (B) were collected from three infected mice, and the spleen samples were homogenized. Viral infectivity titers were determined by use of a focus-forming assay using Vero E6 cells. Error bars indicate standard deviations.
Because lethality was correlated with viral titer, we explored whether viral titer also correlated with the level of differential gene expression. We therefore performed a correlation analysis between virus titer and gene expression with a Pearson's r of >0.85. Only 39 genes presented a positive correlation, indicating that differences in viral titer did not have a substantial impact on the number of differentially expressed genes. Genes correlated with a high viral titer were strongly upregulated by 48 and 72 h postinfection and encoded a variety of chemokines, colony stimulating factors, interleukins, matrix metallopeptidases, and C-type lectins (see Table S1 in the supplemental material).
Molecular signature associated with lethal Ebola virus infection.
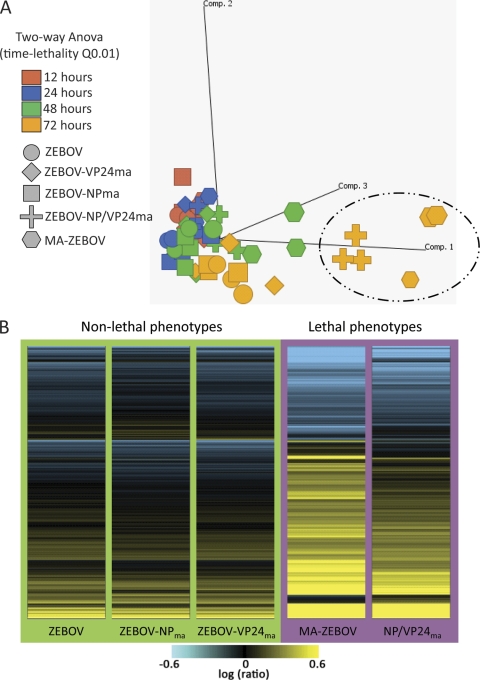
The main goal of the present study was to determine specific molecular signatures associated with pathogenicity. In order to address this point, we took advantage of the different disease phenotypes to divide these five viruses into two groups, the lethal group (MA-ZEBOV and ZEBOV-NP/VP24ma) and the nonlethal group (WT-ZEBOV, ZEBOV-NPma, and ZEBOV-VP24ma). We then used two-way ANOVA to identify differentially expressed genes between groups and performed principal component analysis (PCA) to identify subgroups within the data sets. This showed that the lethal subgroups (MA-ZEBOV and ZEBOV-NP/VP24ma) were the most different from the others at 72 h postinfection (Fig. 2A). Heat maps of the genes differentially expressed at 72 h showed that the nonlethal viruses elicited very weak activation of these genes (Fig. 2B), whereas infection with the lethal viruses elicited a much stronger response.
Fig. 2.
Lethal MA-ZEBOV and ZEBOV-NP/VP24ma viruses elicit stronger host responses than nonlethal viruses at 72 h postinfection. (A) Principal component analysis (PCA) was performed to identify subgroups within the data sets generated by the ANOVA approach, using a Benjamin and Hochberg algorithm-corrected false discovery rate (Q) of 0.01. Colors indicate the different time points of the experiment, and the shapes illustrate the different recombinant viruses. Highlighted are the most different subgroups. Comp., component. (B) Heat map generated using a two-way ANOVA method between the lethal and nonlethal groups relative to results for mock-infected control mice (fold change, ≥2) to identify differentially expressed genes between groups. Yellow indicates upregulated genes; blue indicates downregulated genes. Background colors indicate the lethal or nonlethal groups.
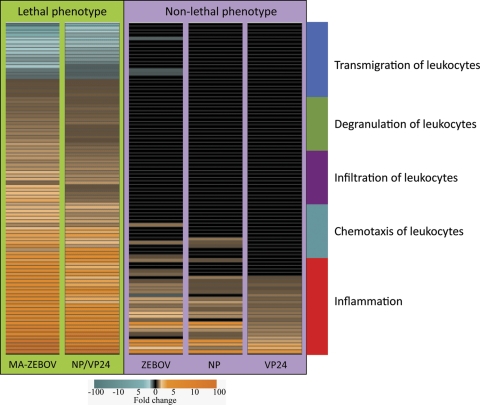
We next uploaded the 1,213 genes detected by two-way ANOVA into Ingenuity Pathways Analysis (IPA) for functional analysis. The top nine biological categories determined by IPA are presented in Table 1. By inspecting these categories and their associated functions, as well as identifying genes present in more than one category, we identified the inflammatory response as one of the most prominent functions differentially expressed at 72 h postinfection. The differential expression of these genes clearly distinguished the lethal and nonlethal groups (Fig. 3). To better illustrate these genes, we used IPA to subcategorize the genes according to their most specific functions within the inflammatory response; this resulted in the generation of five groups, labeled inflammation, chemotaxis of leukocytes, infiltration of leukocytes, degranulation of leukocytes, and transmigration of leukocytes, respectively. We also noted that the expression of some of these inflammatory genes had a positive correlation with virus titer. This suggests that although only 39 genes correlated with virus titer (see Table S1 in the supplemental material), many of these genes were strongly activated in response to infection with the lethal viruses.
Table 1.
Top nine biological categories determined by Ingenuity Pathways Analysisa
| Biological category | P value |
|---|---|
| Cellular movement | 3.76 × 10−21 to 3.41 × 10−5 |
| Cell-to-cell signaling and interaction | 1.08 × 10−18 to 4.44 × 10−5 |
| Tissue development | 1.08 × 10−18 to 2.55 × 10−5 |
| Immune cell trafficking | 7.17 × 10−16 to 4.44 × 10−5 |
| Connective tissue disorders | 2.07 × 10−15 to 1.89 × 10−5 |
| Inflammatory response | 3.27 × 10−15 to 4.62 × 10−5 |
| Hematological system development and function | 4.01 × 10−15 to 4.44 × 10−5 |
| Inflammatory disease | 2.38 × 10−14 to 2.12 × 10−5 |
| Skeletal and muscular disorders | 1.73 × 10−13 to 1.89 × 10−5 |
Categories were determined using Ingenuity Pathways Analysis of genes that were differentially expressed (ANOVA with corrected false discovery rate of 0.01) for each condition relative to results for mock-infected control mice (fold change, ≥2). Fisher's exact test correction P value was used to rank the significance associated for each category.
Fig. 3.
Differential regulation of inflammatory response genes by the lethal viruses. Heat map illustrates the transcriptional profile and categorization of the inflammatory genes identified as differentially expressed between the lethal and nonlethal groups 72 h after infection within cutoff values of a ≥2-fold change and an ANOVA P value with a Benjamini and Hochberg algorithm-corrected false discovery rate of 0.01. The genes shown in orange are upregulated, those in blue were downregulated, and those in black did not pass the statistical cutoff criteria for infected relative to mock-infected animals. Color legend at the bottom indicates the fold change spectrum of the results.
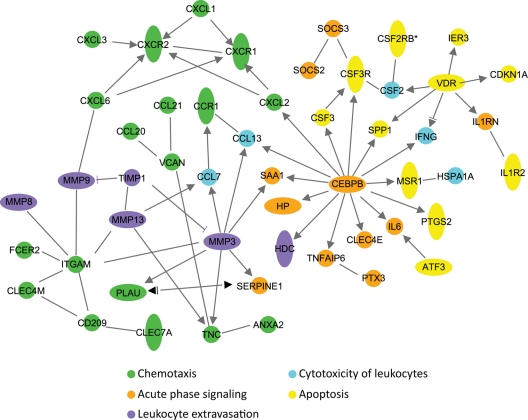
We also used IPA to identify functional relationships between the differentially regulated inflammatory genes associated with lethality. Results are illustrated in the functional network shown in Fig. 4. This network consists only of genes that showed a direct functional relationship; these genes are involved in chemotaxis (green), apoptosis (yellow), acute-phase signaling (orange), cytotoxicity of leukocytes (blue), and leukocyte extravasation (purple). Our results highlight the strong upregulation of genes related to the inflammatory response at 72 h postinfection as a consequence of lethal Ebola virus infection and the differential activation of metalloproteinases by the lethal viruses MA-ZEBOV and ZEBOV-NP/VP24ma. The identification of this molecular signature associated with lethality could open new avenues of research into novel targets for the development of new drug compounds.
Fig. 4.
Molecular signature associated with lethality. Biological network analysis determined by Ingenuity Pathways Analysis to identify functional relationships between the differentially regulated inflammatory genes associated with lethality. This analysis highlights five different subsets of genes that showed a direct functional relationship. These genes are involved in chemotaxis (green), apoptosis (yellow), acute-phase signaling (orange), cytotoxicity of leukocytes (blue), and leukocyte extravasation (purple). All these genes were strongly upregulated at 72 h postinfection as a consequence of lethal Ebola virus infection, with the exception of four chemotaxis genes (CCL21, CD209, CLEC4M, and FCER2) that were downregulated.
ZEBOV-VP24ma elicits a host transcriptional response similar to that of the lethal double mutant.
Because ZEBOV-VP24ma and ZEBOV-NPma were nonlethal in mice, whereas the recombinant virus containing the mouse-adapted mutations in both of these genes (ZEBOV-NP/VP24ma) was lethal, we used these viruses to gain insights into the relative contribution of the mutations in the individual VP24 and NP genes to lethality. We first identified genes that were differentially regulated between the double mutant and the viruses containing mutations only in VP24 or NP. To achieve this, we performed two-way ANOVAs using time and the virus strain as analysis factors. We identified only 8 differentially regulated genes between ZEBOV-VP24ma and ZEBOV-NP/VP24ma and 131 differentially regulated genes between ZEBOV-NPma and ZEBOV-NP/VP24ma. The small number of genes differentiating the host transcriptional response to the single- and double-mutant viruses was surprising, given the stark differences in phenotypic outcome. These results indicate that the generation of the lethal phenotype observed during infection with the double-mutant virus is due to a small number of gene expression changes not elicited by the viruses containing mutations only in VP24 or NP.
The next step of our analysis was to determine the specific contribution of these host gene expression changes to lethality. To accomplish this, we took advantage of the lethality signature identified earlier to compare the 8 and 131 differentially regulated genes identified by the ANOVA method. Results from this approach indicated that 7 of 8 genes (see Table S2 in the supplemental material) from the ZEBOV-VP24ma versus ZEBOV-NP/VP24ma ANOVA list were present in the identified lethality signature. On the other hand, 56 of 131 genes (see Table S3 in the supplemental material) from the ZEBOV-NPma versus ZEBOV-NP/VP24ma ANOVA list were found in the lethality signature. Thus, the VP24 mutation is responsible for inducing the majority of gene expression changes associated with lethality as evidenced by the high similarity in the host response elicited by the double-mutant and the VP24 mutant viruses. However, the lethal phenotype was only achieved during infection with the double-mutant virus, suggesting that there is an additive effect of the VP24 and NP mutations in order to generate this lethal phenotype. Of the identified 7 and 56 genes associated with lethality, the majority of these genes were unchanged during infection with the single-mutant viruses, but all of them were differentially expressed (up- or downregulated) during infection with the double-mutant virus.
We then performed a functional analysis of the detected genes associated with lethality. Among the most representative functions of the 56 genes associated with lethality were genes involved in the ubiquitination pathway (HSP90B1, HSPE1, and PARK2), activation of LXR/RXR (RXRG, MSR1, and ARG2), leukocyte extravasation signaling (MMP19, TIMP1), mitochondrial dysfunction (PARK2, SOD2), and integrin signaling (PARVA, RHOF), and the expression of these genes was activated by 72 h after infection with the double-mutant virus but not with the virus carrying only the NP mutation. From the 7 genes (CD209B, CILP, SHISA3, TIMD4, PLA2G2D, CPNE4, and MMP3) associated with lethality, the metalloproteinase gene MMP3 was not differentially expressed in response to the VP24 mutant but was almost 50-fold upregulated in response to the double mutant. Among the other genes, CD209B, also known as SIGNR1, encodes a C-type lectin that has been implicated in the humoral immune response to influenza virus infection (25), PLA2G2D encodes phospholipase A2 group IID that has been associated with apoptosis and chemotaxis (1, 9), and CPNE4 encodes copine IV, a calcium-dependent membrane-binding protein that may regulate events at the interface of cell membrane and cytoplasm (49). Our results suggest that the differential expression of these genes, especially that of the metalloproteinases, which recently have been linked to diverse pathological conditions such as inflammatory disorders and cancer (42, 45), is important for severe Ebola virus pathogenicity.
DISCUSSION
Lethal Ebola viruses elicit a specific molecular signature.
Our functional genomics study performed with spleens from Ebola virus-infected mice allowed us to identify a specific molecular signature associated with lethality. We acknowledge that analysis of different tissues may have yielded additional signatures; however, in a previous influenza virus study, we found that global expression profiles of the lung mirrored the profiles identified for blood (2). Although isolated cell populations may provide information on the response of specific cell types, the analysis of the whole organ nevertheless provides clear differences in molecular signatures between viruses and provides insight into pathogenesis.
At first glance, this functional signature illustrates the strong upregulation of proinflammatory genes 72 h after infection. Results from our study are therefore in agreement with the current knowledge of Ebola virus pathogenesis in humans, for whom a dysregulated inflammatory response is believed to contribute to disease progression (19, 31). Here, our results depict a scenario in which key genes related to the inflammatory response were strongly activated only during infection with the lethal viruses MA-ZEBOV and ZEBOV-NP/VP24ma. A similar activation of inflammatory genes was not observed in response to the nonlethal viruses WT-ZEBOV, ZEBOV-NPma, and ZEBOV-VP24ma, showing that an uncontrolled inflammatory response was an essential determinant of Ebola virus lethality.
Additional novel findings are the identification of specific inflammation-related components, such as classical chemokines (CCL7, CCL13, CXCL2, CXCL6, CXCL1, CCL21, CCL20, CXCL3, CCR1, CXCR2) and apoptosis-related genes (PTGS2, IL1R2, MSR1, ATF3, CSF3, SPP1, IER3, VDR, CDKN1A), in the identified lethality signature. We also observed the upregulation and direct functional connectivity of metalloproteinase-related genes (MMP3, MMP8, MMP9, MMP13, TIMP1) and acute-phase signaling molecules (CEBPB, HP, SAA1, CLEC4E, PTX3, TNFAIP6, SERPINE1, interleukin-6 [IL-6], IL1RN). Of particular relevance is our finding that metalloproteinase genes were upregulated only in lethal infections and not in response to the nonlethal wild-type or single-mutant viruses. Furthermore, the metalloproteinase gene MMP3 was one of 7 genes associated with lethality that was induced by the double mutant but not by the virus carrying the VP24 mutation. Metalloproteinases control chemokine activity (14, 34, 37, 43) and can regulate inflammation by controlling the activity of chemokines (13, 28), and MMP3-deficient mice are prone to severe inflammation (39). Additional studies have implicated metalloproteinases in inflammatory disorders, vasodilation, wound healing, and carcinogenesis (18, 40–42).
MMP3 was also among the 39 genes whose expression correlated with the viral titers of the MA-ZEBOV and ZEBOV-NP/VP24ma viruses. Many of these genes were part of the identified lethality signature, and 11 of these genes had the highest fold changes in the signature. The top three genes whose expression correlated with viral titer (CCL7, MMP3, and CCL13) had almost a 100-fold increases in gene expression, indicating that although the number of genes correlated with viral titer was small, these genes likely play relevant roles in disease outcome.
The increased inflammatory response is similar to the observed upregulation of the inflammatory response in studies using the mouse and macaque models of highly pathogenic influenza viruses (11, 12), further highlighting the relevance of homeostatic control of inflammation. In human cases of fatal Ebola virus infection, the dysregulated expression of inflammatory mediators, including interferon, interleukins, monocyte chemoattractant protein 1, tumor necrosis factor alpha (TNF-α), and reactive oxygen species, are thought to contribute to disease progression (19, 31, 47). However, an early and controlled inflammatory response has been associated with recovery, suggesting that a well-regulated innate immune response is critical for control of Ebola virus infection (4).
Contributions of VP24 and NP mutations to lethality.
In the present paper and in a previous study (17), we found that a combination of two specific mutations in VP24 and NP increased Ebola virus pathogenicity in a mouse model. We therefore took advantage of this group of viruses to gain insights into the contributions of the VP24 and NP genes to pathogenesis. Somewhat surprisingly, the host response to each single-mutant virus was similar to the response against the lethal double-mutant virus, indicating that the additive effect of mutations on both genes is required to generate the lethal phenotype. Indeed, the virus containing only the VP24 mutation induced the majority of gene expression changes associated with lethality. While metalloproteinase genes were not induced in response to viruses containing mutations only in VP24 or NP, these genes were highly induced by the lethal viruses MA-ZEBOV and ZEBOV-NP/VP24ma. The lack of induction of these genes by the single mutants was one of the few and most striking differences between the host responses to single- and double-mutant viruses.
Other studies have also implicated metalloproteinases in Ebola virus pathogenesis. Dolnik et al. identified TNF-α/α-disintegrin and metalloproteinase (ADAM 17) as responsible for Ebola virus glycoprotein ectodomain release, suggesting a possible viral escape mechanism from the host immune response (16). In addition, ADAM 17 was among the genes upregulated in blood from macaques infected with ZEBOV (46). Although we did not observe an upregulation of ADAM 17 in the mouse model, we used very stringent statistical criteria for the analysis of gene expression profiles by using a corrected Benjamini and Hochberg false discovery rate of 0.01.
We previously compared the host transcriptional response of human liver cells to ZEBOV, Reston Ebola virus, and Marburg virus infection (32). That study suggested that ZEBOV and Marburg virus antagonize the activation of the innate antiviral response and prompt the overall downregulation of coagulation. In addition, Hartman et al. performed a microarray analysis of human liver cells infected with ZEBOV and a recombinant virus, recEbo-VP35/R312A, containing the R312A mutation within VP35 (29). That study indicated that both viruses induced the expression of death receptor signaling, RNA processing, and hematological system- and development-related genes, suggesting that altered expression of these genes may contribute to severity of disease. In the present study, we did not observe major differences in the expression of genes in the coagulation system. One likely explanation for these differences is the model systems used for these studies. Mice infected with MA-ZEBOV do not show coagulation abnormalities, and in general, coagulopathy is not seen in this model (8, 20, 24). Although the mouse model differs in this aspect from human infections, the model nevertheless provides a relevant system to study pathogenicity and the host response (26, 27, 52), and mice have been used successfully for the screening of antiviral drugs and candidate vaccines against Ebola virus (19). An analysis of the host transcriptional response using blood samples from cynomolgus macaques infected with ZEBOV found a strong expression of cytokine, chemokine, and apoptotic genes 4 to 6 days after infection (46). Our present results add to these findings not only with additional chemokine- and apoptosis-related genes but also with the association of metalloproteinases and acute-phase signaling molecules strongly activated late during infection. To our knowledge, this specific molecular signature associated with Ebola virus lethality is the first report of this nature and should open new avenues for research and suggest targets for the development of new drugs aimed at modulating the inflammatory response.
Supplementary Material
ACKNOWLEDGMENTS
We thank Sarah Belisle and Sean Proll (Department of Microbiology, University of Washington) for helpful discussions and reviews of the manuscript.
This study was funded in part by a Contract Research Fund for the Program of Founding Research Centers for Emerging and Reemerging Infectious Diseases, by Exploratory Research for Advanced Technology (ERATO), and by the Special Coordination Funds for Promoting Science and Technology from the Ministry of Education, Culture, Sports, Science, and Technology of Japan. Additional funding was provided by the National Microbiology Laboratory of the Public Health Agency of Canada, by Public Health Service grants U54AI057153 (Great Lakes Regional Center of Excellence) and U54AI081680 (Pacific Northwest Regional Center of Excellence), and by grant R01AI077593 from the National Institute of Allergy and Infectious Diseases.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the funding agencies.
Footnotes
Supplemental material for this article may be found at http://jvi.asm.org/.
Published ahead of print on 6 July 2011.
REFERENCES
- 1. Arcila M. L., et al. 2007. Activation of apoptosis, but not necrosis, during Mycobacterium tuberculosis infection correlated with decreased bacterial growth: role of TNF-alpha, IL-10, caspases and phospholipase A2. Cell. Immunol. 249:80–93 [DOI] [PubMed] [Google Scholar]
- 2. Baas T., et al. 2006. Integrated molecular signature of disease: analysis of influenza virus-infected macaques through functional genomics and proteomics. J. Virol. 80:10813–10828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Baize S., et al. 1999. Defective humoral responses and extensive intravascular apoptosis are associated with fatal outcome in Ebola virus-infected patients. Nat. Med. 5:423–426 [DOI] [PubMed] [Google Scholar]
- 4. Baize S., et al. 2002. Inflammatory responses in Ebola virus-infected patients. Clin. Exp. Immunol. 128:163–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Benjamini Y., Hochberg Y. 1995. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. B 57:289–300 [Google Scholar]
- 6. Bermejo M., et al. 2006. Ebola outbreak killed 5000 gorillas. Science 314:1564. [DOI] [PubMed] [Google Scholar]
- 7. Bradfute S. B., et al. 2010. Mechanisms and consequences of ebolavirus-induced lymphocyte apoptosis. J. Immunol. 184:327–335 [DOI] [PubMed] [Google Scholar]
- 8. Bray M., Hatfill S., Hensley L., Huggins J. W. 2001. Haematological, biochemical and coagulation changes in mice, guinea-pigs and monkeys infected with a mouse-adapted variant of Ebola Zaire virus. J. Comp. Pathol. 125:243–253 [DOI] [PubMed] [Google Scholar]
- 9. Carnevale K. A., Cathcart M. K. 2001. Calcium-independent phospholipase A(2) is required for human monocyte chemotaxis to monocyte chemoattractant protein 1. J. Immunol. 167:3414–3421 [DOI] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention Bioterrorism agents/diseases. http://www.bt.cdc.gov/agent/agentlist-category.asp#a Centers for Disease Control and Prevention, Atlanta, GA: Accessed 15 March 2011 [Google Scholar]
- 11. Cilloniz C., et al. 2010. Lethal dissemination of H5N1 influenza virus is associated with dysregulation of inflammation and lipoxin signaling in a mouse model of infection. J. Virol. 84:7613–7624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cilloniz C., et al. 2009. Lethal influenza virus infection in macaques is associated with early dysregulation of inflammatory related genes. PLoS Pathog. 5:e1000604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Corry D. B., et al. 2004. Overlapping and independent contributions of MMP2 and MMP9 to lung allergic inflammatory cell egression through decreased CC chemokines. FASEB J. 18:995–997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Corry D. B., et al. 2002. Decreased allergic lung inflammatory cell egression and increased susceptibility to asphyxiation in MMP2-deficiency. Nat. Immunol. 3:347–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Davis K. J., et al. 1997. Pathology of experimental Ebola virus infection in African green monkeys: involvement of fibroblastic reticular cells. Arch. Pathol. Lab Med. 121:805–819 [PubMed] [Google Scholar]
- 16. Dolnik O., et al. 2004. Ectodomain shedding of the glycoprotein GP of Ebola virus. EMBO J. 23:2175–2184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ebihara H., et al. 2006. Molecular determinants of Ebola virus virulence in mice. PLoS Pathog. 2:e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Egeblad M., Werb Z. 2002. New functions for the matrix metalloproteinases in cancer progression. Nat. Rev. Cancer. 2:161–174 [DOI] [PubMed] [Google Scholar]
- 19. Feldmann H., Geisbert T. W. 2011. Ebola haemorrhagic fever. Lancet 377:849–862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Geisbert T. W., Hensley L. E. 2004. Ebola virus: new insights into disease aetiopathology and possible therapeutic interventions. Expert Rev. Mol. Med. 6:1–24 [DOI] [PubMed] [Google Scholar]
- 21. Geisbert T. W., et al. 2000. Apoptosis induced in vitro and in vivo during infection by Ebola and Marburg viruses. Lab. Invest. 80:171–186 [DOI] [PubMed] [Google Scholar]
- 22. Geisbert T. W., et al. 2003. Pathogenesis of Ebola hemorrhagic fever in cynomolgus macaques: evidence that dendritic cells are early and sustained targets of infection. Am. J. Pathol. 163:2347–2370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Geisbert T. W., et al. 2003. Pathogenesis of Ebola hemorrhagic fever in primate models: evidence that hemorrhage is not a direct effect of virus-induced cytolysis of endothelial cells. Am. J. Pathol. 163:2371–2382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gibb T. R., et al. 2001. Pathogenesis of experimental Ebola Zaire virus infection in BALB/c mice. J. Comp. Pathol. 125:233–242 [DOI] [PubMed] [Google Scholar]
- 25. Gonzalez S. F., et al. 2010. Capture of influenza by medullary dendritic cells via SIGN-R1 is essential for humoral immunity in draining lymph nodes. Nat. Immunol. 11:427–434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gupta M., et al. 2005. CD8-mediated protection against Ebola virus infection is perforin dependent. J. Immunol. 174:4198–4202 [DOI] [PubMed] [Google Scholar]
- 27. Gupta M., et al. 2004. Persistent infection with Ebola virus under conditions of partial immunity. J. Virol. 78:958–967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Haro H., et al. 2000. Matrix metalloproteinase-3-dependent generation of a macrophage chemoattractant in a model of herniated disc resorption. J. Clin. Invest. 105:133–141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hartman A. L., Ling L., Nichol S. T., Hibberd M. L. 2008. Whole-genome expression profiling reveals that inhibition of host innate immune response pathways by Ebola virus can be reversed by a single amino acid change in the VP35 protein. J. Virol. 82:5348–5358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hartman A. L., Towner J. S., Nichol S. T. 2010. Ebola and Marburg hemorrhagic fever. Clin. Lab. Med. 30:161–177 [DOI] [PubMed] [Google Scholar]
- 31. Hensley L. E., Young H. A., Jahrling P. B., Geisbert T. W. 2002. Proinflammatory response during Ebola virus infection of primate models: possible involvement of the tumor necrosis factor receptor superfamily. Immunol. Lett. 80:169–179 [DOI] [PubMed] [Google Scholar]
- 32. Kash J. C., et al. 2006. Global suppression of the host antiviral response by Ebola- and Marburgviruses: increased antagonism of the type I interferon response is associated with enhanced virulence. J. Virol. 80:3009–3020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ledgerwood J. E., et al. 2010. A replication defective recombinant Ad5 vaccine expressing Ebola virus GP is safe and immunogenic in healthy adults. Vaccine 29:304–313 [DOI] [PubMed] [Google Scholar]
- 34. Li Q., Park P. W., Wilson C. L., Parks W. C. 2002. Matrilysin shedding of syndecan-1 regulates chemokine mobilization and transepithelial efflux of neutrophils in acute lung injury. Cell 111:635–646 [DOI] [PubMed] [Google Scholar]
- 35. Livak K. J., Schmittgen T. D. 2001. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔC(T) method. Methods 25:402–408 [DOI] [PubMed] [Google Scholar]
- 36. Martin J. E., et al. 2006. A DNA vaccine for Ebola virus is safe and immunogenic in a phase I clinical trial. Clin. Vaccine Immunol. 13:1267–1277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. McQuibban G. A., et al. 2000. Inflammation dampened by gelatinase A cleavage of monocyte chemoattractant protein-3. Science 289:1202–1206 [DOI] [PubMed] [Google Scholar]
- 38. Mohamadzadeh M., Chen L., Schmaljohn A. L. 2007. How Ebola and Marburg viruses battle the immune system. Nat. Rev. Immunol. 7:556–567 [DOI] [PubMed] [Google Scholar]
- 39. Mudgett J. S., et al. 1998. Susceptibility of stromelysin 1-deficient mice to collagen-induced arthritis and cartilage destruction. Arthritis Rheum. 41:110–121 [DOI] [PubMed] [Google Scholar]
- 40. Nagase H., Visse R., Murphy G. 2006. Structure and function of matrix metalloproteinases and TIMPs. Cardiovasc. Res. 69:562–573 [DOI] [PubMed] [Google Scholar]
- 41. Page-McCaw A., Ewald A. J., Werb Z. 2007. Matrix metalloproteinases and the regulation of tissue remodelling. Nat. Rev. Mol. Cell Biol. 8:221–233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Parks W. C., Wilson C. L., Lopez-Boado Y. S. 2004. Matrix metalloproteinases as modulators of inflammation and innate immunity. Nat. Rev. Immunol. 4:617–629 [DOI] [PubMed] [Google Scholar]
- 43. Pruijt J. F., et al. 1999. Prevention of interleukin-8-induced mobilization of hematopoietic progenitor cells in rhesus monkeys by inhibitory antibodies against the metalloproteinase gelatinase B (MMP-9). Proc. Natl. Acad. Sci. U. S. A. 96:10863–10868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Reed D. S., Mohamadzadeh M. 2007. Status and challenges of filovirus vaccines. Vaccine 25:1923–1934 [DOI] [PubMed] [Google Scholar]
- 45. Roy R., Yang J., Moses M. A. 2009. Matrix metalloproteinases as novel biomarkers and potential therapeutic targets in human cancer. J. Clin. Oncol. 27:5287–5297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rubins K. H., et al. 2007. The temporal program of peripheral blood gene expression in the response of nonhuman primates to Ebola hemorrhagic fever. Genome Biol. 8:R174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sanchez A., Geisbert T. W., Feldmann H. 2007. Filoviridae: Marburg and Ebola viruses, p. 1409–1448 In Knipe D. M., et al. (ed.), Fields virology, 5th ed., vol. 2 Lippincott Williams and Wilkins, Philadelphia, PA [Google Scholar]
- 48. Schnittler H. J., Feldmann H. 1999. Molecular pathogenesis of filovirus infections: role of macrophages and endothelial cells. Curr. Top. Microbiol. Immunol. 235:175–204 [DOI] [PubMed] [Google Scholar]
- 49. Tomsig J. L., Snyder S. L., Creutz C. E. 2003. Identification of targets for calcium signaling through the copine family of proteins: characterization of a coiled-coil copine-binding motif. J. Biol. Chem. 278:10048–10054 [DOI] [PubMed] [Google Scholar]
- 50. Tuffs A. 2009. Experimental vaccine may have saved Hamburg scientist from Ebola fever. BMJ 338:b1223. [DOI] [PubMed] [Google Scholar]
- 51. U.S. Department of Health and Human Services 2007. Biosafety in microbiological and biomedical laboratories, 5th ed U.S. Government Printing Office, Washington, DC [Google Scholar]
- 52. Warfield K. L., et al. 2003. Ebola virus-like particles protect from lethal Ebola virus infection. Proc. Natl. Acad. Sci. U. S. A. 100:15889–15894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zampieri C. A., Sullivan N. J., Nabel G. J. 2007. Immunopathology of highly virulent pathogens: insights from Ebola virus. Nat. Immunol. 8:1159–1164 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.