Abstract
The aim of the study was to determine whether polymorphism in the GCM1 gene is associated with pregnancy induced hypertension (PIH) in a case-control study of mother-baby dyads. Predominantly Hispanic women, ages 15-45, with (n=136) and without (n=169) PIH were recruited. We genotyped four polymorphisms in the GCM1 gene and examined the association with PIH using both logistic regression and likelihood expectation maximization (LEM) to adjust for intra-familial correlation between genotypes. Maternal genotype was not associated with PIH for any polymorphisms examined. Fetal genotype, however, was associated with maternal risk of PIH. Mothers carrying a fetus with ≥1 copy of the minor (C) allele for rs9349655 were less likely to develop PIH than women carrying a fetus with the GG genotype (parity-adjusted OR=0.44, 95% Cl: 0.21, 0.94). The trend of decreasing risk with increasing C alleles was also statistically significant (ORtrend=0.41 95% Cl: 0.20, 0.85). The minor alleles for the other three SNPs also appear to be associated with protection. Multilocus analyses of fetal genotypes showed that the protective effect of carrying minor alleles at rs9349655 and rs13200319 (non-significant) remained unchanged when adjusting for genotypes at the other loci. However, the apparent (non-significant) effect of rs2816345 and rs2518573 disappeared when adjusting for rs9349655. In conclusion, we found that a fetal GCM1 polymorphism is significantly associated with PIH in a predominantly Hispanic population. These results suggest that GCM1 may represent a fetal-effect gene, where risk to the mother is conferred only through carriage by the fetus.
Keywords: GCM1, preeclampsia, hypertension, pregnancy, genetics
Introduction
Pregnancy induced hypertension (PIH) is responsible for 12% of maternal deaths worldwide and has the highest case fatality rate of all the major complications of childbirth [1]. The role of genetics in PIH is well-established but not well-defined. Most previous studies have focused on maternal genotype which may play a role in vulnerability to PIH via underlying susceptibility. However, because the initial pathology is widely believed to be deficient placentation and since the placenta is of fetal origin (and thus genotype), fetal, and possibly paternal genetics will likely play an important role in predisposing to PIH.
Many aspects of placental development are believed to be genetically determined and therefore genes responsible for placental development are obvious candidates for susceptibility to conditions associated with placental dysfunction, such as preeclampsia [2-4]. One placenta I ly-expressed candidate gene is a glial cells missing homologue 1 (GCM1), which encodes a transcription factor essential for the differentiation of syncytiotrophoblasts in mice [5] and in humans [6]. The expression pattern of GCM1 is the same among many species, including mice and humans [7]. In mice, Gcm1-expressing cells define the points where branching morphogenesis begins, forming placental villi [8].
Abnormal placental villi formation has been associated with the development of PIH in humans [9] and with fetal death and intrauterine growth restriction (IUGR) [10-11]. GCM1 expression has been shown to be decreased in the placentae of women with PIH [12], implicating GCM1 in the pathogenesis of this condition. As GCM1 is primarily expressed in the placenta, it is expected that fetal genotype will be the most relevant to the development of PIH.
Relatively few studies have been conducted among Hispanics, with some reporting higher rates of PIH among Hispanics [13-16] and others reporting lower rates compared to non-Hispanic Whites [13-14, 17-20]. Even fewer genetic studies have been conducted in Hispanics [21-24]. In the Los Angeles County (LAC) population where this study was conducted, the rate of PIH is between 7-9%, which may due to high rates of obesity, diet, or other social factors present in this population [25]. We opted to focus on this predominantly Hispanic population at LAC because the rates of PIH are higher than in the general population and because Hispanics, as a whole, are an understudied group.
We investigated four polymorphisms in the GCM1 gene in both mothers and offspring to determine if they are associated with PIH in a predominantly Hispanic population.
Materials and methods
Subjects: As described previously [21], cases of clinically-defined preeclampsia (n = 136) and controls (n = 169) were recruited retrospectively from delivery logs at the Los Angeles County (LAC) + University of Southern California (USC) Women's and Children's Hospital (WCH) from 1999-2006 (103 subjects) and during their postpartum hospital stay at the WCH from 2007-2008 (202 subjects). Controls were not matched to cases on any factors since the ethnic, racial and age distributions in the hospital population from which study subjects were drawn do not vary widely.
DNA was collected from both the mothers via blood (n=39), mouthwash (n=27), buccal swabs (n=13) or saliva (n=214) (Oragene, DNA Genotek, Kanata, Canada) and their infants via buccal swabs (n=92) or saliva (n=204) (Oragene, DNA Genotek, Kanata, Canada). There were no differences in genotyping success rates by method of DNA sampling. Information on known and suspected risk factors was obtained by structured questionnaire, modified for a Hispanic population from one used by the University of Pittsburgh (R. Ness, personal communication) and administered by trained interviewers using standardized prompts.
Medical charts were abstracted to collect information on prenatal care, clinical characteristics, comorbid conditions and to verify case diagnosis and absence of significant hypertension among controls. Cases identified as PE (preeclampsia) on delivery logs were classified as mild PE, severe PE, and gestational hypertension, eclampsia, or HELLP syndrome according to the following definitions. Mild preeclampsia (PE) was defined according to the Working Group on High Blood Pressure in Pregnancy [26] as blood pressure >=140 (systolic) or >= 90 (diastolic) on two or more occasions at least six hours apart plus proteinuria >= 300 mg/dL in a 24-hour urine collection or +1 on a dipstick in women who were normotensive in early pregnancy (less than 20 weeks gestation). Similarly, severe PE was defined as blood pressure >=160 (systolic) or >= 110 (diastolic) on two or more occasions at least six hours apart plus proteinuria >= 500 mg/dL in a 24-hour urine collection or +3 on a dipstick [26]. Gestational hypertension was defined as elevated blood pressure (mild or severe, as described above) without evidence of proteinuria. Eclampsia was defined as any PIH accompanied by seizure in a woman with no prior history of a seizure disorder and HELLP Syndrome was defined as evidence of hemolysis (abnormal peripheral smear or LDH≥600), ALT and/or AST≥70 and platelets ≤100,000. Women with two of the three signs of HELLP syndrome were deemed “partial HELLP Syndrome.” Women with lupus, chronic renal disease, multiple gestations, or sickle cell disease/trait were excluded.
This study was approved by the University of Southern California Health Sciences Campus Institutional Review Board. All participants signed an informed consent for both herself and her infant and, for women under the age of 18 at the time of recruitment (n=14), parental permission for participation was also obtained.
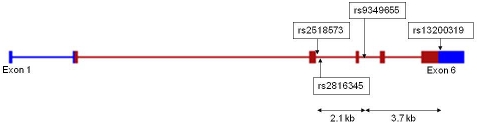
Selection of SNPs: We used a candidate SNP approach to select SNPs for genotyping. Potential candidate SNPs were identified using the SNPper Bioinformatics Tool (snpper.chip.org/) and by searching the NCBI SNP database (www.ncbi.nlm.nih.gov/snp). Specifically, SNPs were included if they had a minor allele frequency (MAF) of at least 5% and met one or more of the following criteria indicative of potential functionality: (1) were located in a coding region and resulted in an amino acid substitution (nonsynonymous SNPs), (2) were located in the 5' or 3' untranslated region or at an exon/ intron boundary, or (3) were located in an evolutionarily conserved region (ECR) highly conserved between humans and placental mammals. Four SNPs met these criteria and were included: one in the 3'UTR of exon 6, 2 bp downstream of the stop codon (rs13200319), one 15 bp downstream of exon 3 (rs2518573), one 37 bp downstream of exon 3 (rs2816345) and one 97 bp downstream of exon 4 (rs9349655) (www.ncbi.nlm.nih.gov/access date 6/22/2010) (Figure 1).
Figure 1.
Polymorphisms in GCM1 in relation to gene structure. The four candidate SNPs are shown in relation to their location in the GCM1 gene. The GCM1 gene has six exons; rs2518573 and rs2816345 are located downstream of exon 3, 15 and 37 bp from the exon respectively. rs9349655 is 97 bp downstream of exon 4 and rs13200319 is located in the 3'UTR of exon 6, 2 bp dowstream of the stop codon.
After the study was completed, a follow-up search was conducted using NCBI Entrez Gene (www.ncbi.nlm.nih.gov/gene/8521) to determine if any additional genotyping was warranted. The search identified 308 SNPs in the GCM1 gene, 282 of which had no information on allele frequency. Of those SNPs with MAF ≥ 5%, 17 were intronic and were not in ECRs and one was a synonymous coding SNP (rs76788361) and thus were not considered for genotyping. One was a nonsynonymous coding SNP (rs80332272) located in exon five with a reported MAF of 10%. However, this SNP could not be located in any other databases and had an unknown allele frequency outside of Asian populations. Since we had resequenced exon five in a multiethnic panel (see below) and did not find this polymorphism, we concluded that the SNP was likely rare in non-Asian populations and therefore did not genotype it.
Laboratory Methods: DNA was extracted from mouthwash specimens using a phenylchloroform protocol [27], from buccal swabs and buffy coat using QIAamp DNA Mini kits (Qiagen, Valencia, USA), and from saliva samples using ethanol precipitation per manufacturer's protocol (DNA Genotek, Kanata, Canada).
Sequences containing all six exons of the gene as well as 1000 bp upstream of the transcription start site were resequenced in 60 deidentified control samples from multiple ethnicities which are not part of the current study population. Regions of the gene were sequenced in both forward and reverse orientation using a standard BigDye Terminator v3.1 protocol (Applied Biosystems, Foster City, USA) and read on a 3700 ABI PRISM® 3700 DNA Analyzer.
SNPs were genotyped using TaqMan assays (7900HT Sequence Detection System, Applied Biosystems, Foster City, USA). All TaqMan primers and probes were designed using Primer Express 2.0 (Applied Biosystems, Foster City, USA). Five ng of genomic DNA was amplified in a 5 μl total reaction volume containing 2.2 μl of water, 2.5 μl of Universal Master Mix (Applied Biosystems, Foster City, USA), 0.1 μl of each primer (15 μM) and 0.05 μl of each probe (10 μM). Thermocycler conditions were as follows (rs2518573, rs2816345): one 10 min hold at 95 degrees C, and 60 cycles containing a 30 second denaturing cycle at 95 degrees C, followed by a 1 min annealing/extension cycle at 60 degrees C. Slight variations from the above conditions were made for rs13200319 and rs9349655, which included the following: (1) increased number of cycles to 65 and decreased annealing/extension temperature to 58 degrees C for rs13200319 and, (2) decreased number of cycles to 40 for rs9349655.
Statistical analysis
Mother-baby dyads were included in the descriptive analysis if they had non-missing genotype for both mom and baby for at least one of the four SNPs studied. One mother and six babies had missing data for at least 1 SNP, resulting in a final sample size of 297 dyads. Demographic characteristics of the analyzable study population were described using means and frequencies. Cases (n=130) and controls (n=167) were compared using either Pearson's or Fisher's chi-squared test (categorical variables) or Student's t-test (continuous variables).
We first analyzed each SNP separately, excluding mother/baby dyads that had a missing genotype for either the mother or the baby (17, 12, 11, and 7 dyads for rs13200319, rs9349655, rs2816345, and rs2518573, respectively). We collapsed heterozygotes with homozygous for the rare allele for rs13200319 and rs9349655. Unadjusted odds ratios (maternal genotype unadjusted for fetal genotype and vice versa) were estimated using unconditional logistic regression models, with and without adjustment for parity (parous vs. nulliparous) and maternal age. Genotypes were coded according to a log additive model to estimate allele dosage effects and to provide tests of trend. To compare individual genotypes to the reference group (homozygotes for the more common allele), the three genotypes were coded using two dummy variables, with the exception of rs9349655 and rs13200319 which, due to sparse data, was coded as dichotomous (carriers vs. non-carriers of the rare allele). To adjust for familial relationships, we fit log-linear models with non-linear constraints to account for Mendelian transmission, parental mating symmetry and allelic exchangeabilty as described by Shi et al. [28]. Odds ratios from log-linear models were not further adjusted because covariates could not be accommodated in the constrained model.
Multilocus models were fit using unconditional logistic regression, for fetal genotypes only, using all samples that had non-missing genotypes for all four SNPs (129 cases and 160 controls). Genotypes were coded as log-additive. Models included the locus found to be significant by univariate analysis (rs9349655), with adjustment for one or two of the remaining SNPs. The two highly correlated SNPs (rs2816345 and rs2518573) were not included together in the same model.
All models were adjusted for parity and maternal age, but not for body mass index (BMI) or the gender of the fetus since adjustment for these variables did not alter β by at least 10% and thus were not considered to be confound-ers. We also evaluated the possibility that BMI and/or baby's gender were effect measure modifiers, but did not find evidence of this in our data. We did not adjust for gestational age since it is an unnecessary adjustment, in other words, a variable whose only causal association with the variables of interest is that it is a result of the outcome [29]. Adjustment for a variable in this situation can result in significant bias and loss of precision. Moreover, this situation is particularly susceptible to collider-stratification bias [30]. For a minor allele frequency of 16% (the frequency of the variant haplotype) and 5% type I error rate, we had 80% to detect a protective odds ratio of 0.42.
To test for heterogeneity by disease severity, we fit multinomial logistic models with three outcome categories (control, gestational hypertension, preeclampsia), constraining the coefficients for the adjustment variable (parity) to be constant across severity strata. Likelihood ratio tests were conducted to compare models with genetic effects constrained to be equal across strata vs models with unconstrained genetic effects. We also evaluated the potential effects that the presence of chronic hypertensives, small for gestational age babies, diabetics, thyroid disease, seizure disorders, HIV positivity, and women with a history of PIH may have had by sequentially excluding women with these conditions from the analysis.
Haploview 4.0 [31] was used to estimate the linkage disequilibrium coefficient, D', between SNPs. Constrained log-linear models were fit using LEMDOS [32] and confidence intervals were generated by bootstrapping. All other analyses were conducted using Stata SE 11.0 (Statacorp LP, College Station, USA).
Results
Among the cases included in the analysis data set (n=130), 65 (50%) met the criteria for mild preeclampsia, 24 (18%) were severe preeclamptics, and 41 (32%) had gestational hypertension. However, among those classified as having gestational hypertension, 76% (n=31) had signs or symptoms of more severe disease, including elevated liver enzymes, uric acid, or lactose dehydrogenase and/or decreased platelets (n=14); symptoms of preeclampsia such as headache, right upper quadrant pain, epigastric pain or visual disturbances (n=16); and/or a history of preeclampsia in a previous pregnancy (n=11). Among the preeclamptics, 5 (4%) had PE superimposed on chronic hypertension, 4 (3%) had eclampsia, and 6 (5%) had HELLP Syndrome or partial HELLP Syndrome.
The patient population, as described previously [21] was 96% Hispanic, and cases and controls did not differ by race, maternal age or gravidity (Table 1). Controls in the study population delivered, on average, two weeks later than the cases in the study (p<0.01), indicating that controls, as a group, had sufficient opportunity to develop preeclampsia and be classified as cases. Not unexpectedly, cases were more likely to be nulliparous than controls, with 45% of preeclamptics being nulliparous compared to 31% among controls (p=0.02). Cases and controls also did not differ with respect to rates of most preexisting or comorbid conditions. Specifically, preeclamptics were no more likely than controls to have diabetes, thyroid disease, seizure disorder or be HIV+ [31]. However, preeclamptics were somewhat more likely to have chronic hypertension (5% vs. 1%, p=0.07), have a history of previous PIH (12% vs. 4%, p=0.01), and have small for gestational age babies (12% vs. 6%, p=0.06), defined as less than the 10th percentile of weight for gestational age.
Table 1.
Characteristics of the study population
| Variable | Controls (%) | Cases (%) | p-value |
|---|---|---|---|
| Maternal Age (%) | 167 (100) | 130 (100) | 0.92* |
| 15-20 | 35 (21) | 26 (20) | |
| 21-23 | 32 (19) | 22 (17) | |
| 24-28 | 38 (23) | 27 (21) | |
| 29-34 | 32 (19) | 30 (23) | |
| 35-45 | 30 (18) | 25 (19) | |
| Gestational Age | 167 (100) | 130 (100) | p<0.01* |
| <37 | 14(8) | 39 (30) | |
| 37-38 | 49 (29) | 42 (32) | |
| >=39 | 104 (62) | 49 (38) | |
| Gravidity | 167 (100) | 130 (100) | 0.25* |
| 1 | 43 (26) | 47 (36) | |
| 2 | 48 (29) | 31 (24) | |
| 3 | 30 (18) | 18 (14) | |
| 4-9 | 46 (28) | 34 (26) | |
| Parity | 167 (100) | 130 (100) | 0.02* |
| 0 | 52 (31) | 58 (45) | |
| 1 | 59 (35) | 30 (23) | |
| 2 | 31 (19) | 17 (13) | |
| 3-8 | 25 (15) | 25 (19) | |
| Race/ethnicity | 0.92* | ||
| Hispanic white | 161 (96) | 125 (96) | |
| Hispanic black | 1 (1) | 1 (1) | |
| non-Hispanic black | 3 (2) | 3 (2) | |
| Arab | 1 (1) | 1 (1) | |
| Phillipino | 1 (1) | 0 (0) |
Note: Percentages not totaling 100% are due to rounding errors.
P-value obtained by Pearson's chi-squared test.
During resequencing, no new variants were discovered that were not already reported in the NCBI database (http://www.ncbi.nlm.nih.gov/guide/). In fact, no variation in the exonic or 5' region of the gene was observed. In silico comparisons between the genomes of humans and other placental mammals, including rats, mice, cows, dogs, rhesus monkeys, and chimpanzees, found that the exons, intron/exon boundaries and 5' region of the gene were highly conserved, as were numerous intronic regions (http://ecrbrowser.dcode.org/xB.php?db=hg18&location=chr6:53099721-53121586 - access date 6/24/2010).
For the four genotyped SNPs (Figure 1), there were no Mendelian inconsistencies between maternal and fetal genotypes, and both maternal and fetal genotypes were in Hardy-Weinberg equilibruim among control subjects. Maternal genotype was not associated with PIH for any of the polymorphisms examined. Fetal genotype, however, was associated with PIH risk (Table 2). On the basis of the unadjusted (for maternal genotype) analyses, only one SNP (rs9349655; intron 4) was statistically significantly associated with risk. Women who carried a fetus with at least one copy of the minor (C) allele (16% of cases and 9% of controls) were less likely to develop PIH than women who carried a fetus with the GG genotype (parity-adjusted odd ratio=0.45, 95% Cl: 0.21, 0.97). The trend of decreasing risk with increasing number of C alleles was also statistically significant (ORtrend=0.44 95% Cl: 0.22, 0.90). While minor alleles of the other three SNPs appeared to be associated with protection as well, none were statistically significant, except for rs2816345, which showed a reduction in risk for homozygous carriers of the minor allele that became statistically significant only when adjusted for maternal genotype. However this finding was based on sparse data (only 1 case carrying a fetus homozygous for the minor allele). In general, adjustment for maternal genotype did not substantially alter any of the odds ratios.
Table 2.
GCM1 maternal and fetal genotypes and risk of PIH
| GCM1 locus | Maternal | Fetal | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N (%) | OR (95% Cl) | OR (95% Cl) | OR (95% Cl) | N (%) | OR (95% Cl) | OR (95% Cl) | OR (95% Cl) | |||
| Controls | Cases | Unadjusted | Adjusted* | Adjusted** | Controls | Cases | Unadjusted | Adjusted* | Adjusted** | |
| rs13200319 | ||||||||||
| CC | 139 (85%) | 116 (89%) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 139 (85%) | 117 (90%) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| CT | 22(14%) | 13 (10%) | 0.70 | 0.63 | 0.83 | 22(14%) | 13 (10%) | 0.62 | 0.63 | 0.71 |
| [0.35, 1.41] | [0.31, 1.28] | [0.40, 1.65) | [0.31, 1.22] | [0.31, 1.32] | [0.30, 1.41] | |||||
| TT | 2 (1%) | 1 (2%) | 2 (1%) | 0 (0%) | ||||||
| Trend | 0.72 | 0.65 | 0.89 | 0.64 | 0.61 | 0.66 | ||||
| [0.31, 1.37] | [0.34, 1.25] | [0.44, 1.64] | [0.31, 1.32] | [0.31, 1.21] | [0.30, 1.26] | |||||
| rs9349655 | ||||||||||
| GG | 144 (88%) | 114 (89%) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 137 (84%) | 117 (91%) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| GC | 20(12%) | 10 (8%) | 0.88 | 0.86 | 0.94 | 23(14%) | 11 (9%) | 0.48 | 0.45 | 0.54 |
| [0.43, 1.83] | [0.41, 1.80] | [0.47, 1.71] | [0.23, 1.00] | [0.21, 0.97] | [0.24, 0.98] | |||||
| CC | 0 (0%) | 4 (3%) | 4 (2%) | 0 (0%) | ||||||
| Trend | 1.14 | 1.13 | 1.31 | 0.47 | 0.44 | 0.45 | ||||
| [0.62, 2.11] | [0.60, 2.11] | [0.63, 2.31] | [0.23, 0.92] | [0.22, 0.90] | [0.22, 0.78] | |||||
| rs2816345 | ||||||||||
| AA | 121 (73%) | 92 (69%) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 112 (68%) | 96 (72%) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| AG | 39 (24%) | 34 (24%) | 1.15 | 1.09 | 1.02 | 47 (28%) | 37 (28%) | 0.92 | 0.93 | 0.84 |
| [0.67, 1.96] | [0.63, 1.87] | [0.59, 1.61] | [0.55, 1.53] | [0.55, 1.56] | [0.50, 1.40] | |||||
| GG | 5 (3%) | 8 (6%) | 2.10 | 2.30 | 2.94 | 6 (4%) | 1 (1%) | 0.19 | 0.16 | 0.16 |
| [0.67, 6.64] | [0.71, 7.47] | [0.76, 8.25] | [0.02, 1.64] | [0.02, 1.36] | [0.00, 0.58] | |||||
| Trend | 1.28 | 1.27 | 1.23 | 0.78 | 0.76 | 0.75 | ||||
| [0.85, 1.93] | [0.83, 1.93] | [0.80, 1.91] | [0.50, 1.22] | [0.48, 1.20] | [0.48, 1.14] | |||||
| rs2518573 | ||||||||||
| GG | 109 (66%) | 89 (66%) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 104(63%) | 92 (69%) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| GT | 49 (30%) | 38 (29%) | 0.95 | 0.94 | 0.93 | 54 (33%) | 40 (30%) | 0.84 | 0.87 | 0.78 |
| [0.57, 1.58] | [0.56, 1.58] | [0.59, 1.41] | [0.51, 1.37] | [0.53, 1.45] | [0.47, 1.23] | |||||
| TT | 6 (4%) | 7 (5%) | 1.43 | 1.49 | 2.06 | 6 (4%) | 2 (1%) | 0.38 | 0.30 | 0.34 |
| [0.46, 4.41] | [0.47, 4.71] | [0.60, 5.35] | [0.07, 1.31] | [0.06, 1.60] | [0.00, 1.26] | |||||
| Trend | 1.05 | 1.05 | 1.1 | 0.77 | 0.77 | 0.75 | ||||
| [0.70, 1.57] | [0.70, 1.59] | [0.73, 1.59] | [0.50, 1.19] | [0.50, 1.19] | [0.48, 1.06] | |||||
Adjusted for parity (nulliparous yes/no) and maternal age (<20, 20-32, >32) by logistic regression
Adjusted for fetal (or maternal) genotype at the same locus (LEM method)
The two SNPs in intron 3 were strongly linked with each other (D'=0.98) and were somewhat less strongly linked to the SNP in intron 4 (D'=0.90 for rs2816345 vs. rs9349655). There was little linkage disquilibrium between the 3'UTR SNP and any of the others (D'=0.21 for rs13200319 vs. rs2518573).
Multilocus analyses of fetal genotypes (Table 3) showed that the protective effect of carrying minor alleles at the intron 4 locus (rs9349655) remained unchanged (odds ratio approximately 0.48) when adjusting for genotypes at the other loci. The apparent (non-significant) effect of the two SNPs in intron 3 (rs2816345 and rs2518573) however, disappeared (odds ratios changed from approximately 0.75 to 1.0) when adjusting for rs9349655. The non-significant protective effect of carrying minor alleles at the 3'UTR locus (rs13200319) remained unchanged (with odds ratio approximately 0.60) when adjusting for genotypes at the other loci.
Table 3.
GCM1 fetal genotypes and risk of PIH (multilocus and parity adjusted)
| GCM1 | Locus Odds Ratios and 95% Confidence Intervals† | |||||
|---|---|---|---|---|---|---|
| Single Locus | Multilocus Adjusted | |||||
| Model 1* | Model 2** | Model 3*** | Model 4**** | Model 5***** | ||
| rs13200319 | ||||||
| nT (trend) | 0.65 (0.33, 1.27) | 0.60 (0.30, 1.19) | 0.59 (0.30, 1.19) | 0.58 (0.28, 1.17) | ||
| rs9349655 | ||||||
| nC (trend) | 0.49 (0.24, 0.97) | 0.46 (0.23, 0.93) | 0.48 (0.21, 1.12) | 0.50 (0.22, 1.12) | 0.45 (0.20, 1.02) | 0.42 (0.18, 0.99) |
| rs2816345 | ||||||
| nG (trend) | 0.74(0.47, 1.18) | 1.00 (0.56, 1.78) | 1.13 (0.62, 2.07) | |||
| rs2518573 | ||||||
| nT (trend) | 0.75(0.48, 1.16) | 0.97 (0.57, 1.64) | 1.05 (0.61, 1.81) | |||
rs13200319 and rs9349655 mutually adjusted
rs9349655 and rs2816345 mutually adjusted
rs9349655 and rs2518573 mutually adjusted
rs13200319, rs9349655 and 2518573 mutually adjusted
rs13200319, rs9349655, and rs2816345 mutually adjusted
includes subjects (129 cases & 160 controls) for whom all 4 fetal genotypes are not missing; adjusted for parity (nulliparous yes/no) and maternal age (<20, 20-32, >32) by logistic regression
Note: SNPs which are highly correlated (rs2816345 and rs2518573 cannot be included in the same model.
Discussion
To our knowledge, this is the first report examining polymorphisms in the GCM1 gene in relation to PIH. The GCM1 gene is encoded by 6 exons on chromosome 6p, spanning 22 kb, with exons 1-5 lying in a separate LD (linkage disequilibrium) block from exon 6 (hapmap.org). We found that a variant in the 5' block (rs9349655), 97 bp downstream from exon 4, was significantly associated with reduced risk of PIH and that a variant in the 3' block (rs13200319), in the 3'UTR, 2 bp downsteam from the stop codon, was independently associated with reduced risk of PIH, though this latter association did not reach statistical significance.
The variant alleles were associated with reduced maternal risk only when carried by the fetus. GCM1 is now the second gene playing an important role in placental development that exhibits this pattern of genetic risk, with TGF-β3 being the first reported gene of this type [21]. Both GCM1 and TGF-β3 could aptly be called “fetal effect genes” since they appear to impact maternal disease risk via fetal carriage of the risk allele, but not when the mother herself carries the risk allele.
The finding that fetal GCM1 genotype impacted maternal risk of disease was not unexpected. GCM1 plays an important role in the maintenance and development of human trophoblasts [6], which are fetal cells and therefore of fetal genotype. The lack of association between maternal genotype and PIH was also anticipated, since GCM1 expression in the placenta far exceeds expression by any other (maternal) tissue. Given our understanding of GCM1 as a fetal effect gene, we believe that the appropriate statistical model to evaluate the effect of GCM1 genotype on the risk of PIH would be the model unadjusted for maternal genotype. Adjustment for a factor (maternal genotype) that is not a confounder, but is correlated with fetal genotype, would be an overadjustment, biasing odds ratios towards the null, due to collinearity [33-34]. Therefore, we have chosen to report odds ratios unadjusted for maternal genotype.
Fetal genetic and epigenetic mechanisms are responsible for the greater part of placental development [2-4, 35-37], for which GCM1 has been shown to play an essential role [3, 38]. GCM1 encodes a family of transcription factors [39-40] that are degraded under hypoxic conditions [41] experienced by the early placenta. Once the placenta reaches the maternal blood supply at approximately 12-14 weeks of gestation, GCM1 expression normally increases, resulting in upregulation of syncytin [41], PGF [42] and other target genes. Continuation of placental hypoxia beyond this period is characteristic of PIH, and continued GCM1 silencing results in alteration of many downstream genes, including those in the angiogenic pathway, that have been repeatedly shown to be altered in pregnancies affected by PIH [43-51]. Additional evidence for the role of GCM1 in predisposing to PIH comes from the observation that preeclamptic placentae have lower levels of GCM1 expression compared to placententae from gestational-age matched controls [12].
Interestingly, polymorphism in the GCM1 gene was recently associated with a common form of primary glomerulonephritis, IgA nephropathy (IgAN) [52]. In a genome-wide scan utilizing 10,204 SNPs, the strongest association was with an intronic SNP in GCM1. However, the sample size for the study was extremely small (30 IgAN patients and 28 controls), and the results have not been replicated. Nevertheless, the finding is intriguing since IgAN is characterized by the development of kidney lesions which are strikingly similar to those seen in women who have developed PIH.
Our study is limited by its relatively small sample size. While all study subjects were clinically diagnosed with preeclampsia by experienced clinicians at delivery, upon chart review, documentation of significant proteinura was not available for 32% of cases. Notwithstanding, 76% of women without documented proteinuria exhibited signs or symptoms of severe-range disease, suggesting that that they were well within the preeclamptic spectrum. Furthermore, the clinical utility of proteinuria as a reliable predictor of maternal or fetal outcomes has been questioned [53]. It seems reasonable, in light of this controversy, to consider other markers of disease when diagnosing preeclampsia or determining disease severity. While inclusion of women with less severe disease is expected to bias the results toward the null, in fact, we found that excluding the gestational hypertensives did not substantively alter the effect estimates. Nevertheless, our results should be considered preliminary until they are confirmed in a larger study.
An additional limitation of this study is that we did not examine all variation in the GCM1 gene and, since not all of the SNPs studied were genotyped in the Hapmap Project, it is not possible to estimate the amount of variation in the GCM1 gene which is covered by these four SNPs. Although we chose SNPs on the basis of likely functionality, we may have missed some functionally important variation. Furthermore, it is likely that fetal and maternal genetic contributions to PIH are from distinct pathways and thus, future studies should investigate the possibility that different sets of candidate genes are important in the mother than in the offspring [54].
We also did not consider the possibility of alternate pathological pathways through which PIH could, and probably does, develop. We are aware that PIH is a complex disease with multiple etiologies and that each of those underlying physiological processes almost certainly involves complex interactions among multiple genes and environmental factors. This study is meant to address what we believe is one component in an important pathway underlying a large proportion of cases of PIH - insufficient placental development. Future studies will need to build on this preliminary work to address additional aspects of this pathway as well as entirely divergent pathways which are also likely to be involved in PIH.
Finally, our population was predominantly of Hispanic ethnicity; therefore, these results may not be generalizable to all racial or ethnic groups. However, the polymorphisms studied are not specific to Hispanic ethnicity and the underlying biological rationale for the putative role of GCM1 variants in predisposing to PIH remains intact in other ethnic groups. Still, confirmation of these results in other ethnic groups is needed.
This study has several important strengths. We performed extensive chart reviews for nearly all of the women in the study population and were able to confirm diagnoses for all study subjects. This allowed us to obtain reliable information on medical history, prenatal care, laboratory values and co-morbid conditions for the majority of the study population. By collecting fetal as well as maternal DNA samples, we were able to investigate a candidate gene involved in trophoblast cell differentiation, for which the fetal genotype is expected to be important. And last, gene variants, being present from birth, do not change over gestational age, thereby ruling out the possibility that the disease process may alter the exposure, as may be the case with changes in gene expression or protein levels.
In summary, these finding suggest that fetal genetics may play an important role in the development of PE. While the sample size is relatively small, this is the second study to have found that carriage of a fetal allele affects the risk of the mother developing PE. Additional research is warranted to confirm these results and to determine to what extent genes involved in placental development play a role in predisposing to maternal disease. Large studies will be needed to evaluate gene-gene interactions at separate loci.
Acknowledgments
We would like to thank the women and their children who participated in this study, without whom knowledge cannot be gained. We would also like to thank Aida Lozada for recruiting the vast majority of the women in the study and Clarice Weinberg for many helpful discussions regarding data analysis. We received funding from the NICHD, R21 HD046624-02.
References
- 1.Lerberghe W, Manual A, Matthews Z, Wolfheim C. Making Every Mother and Child count. In: Lerberghe WV, editor. Geneva: World Health Organization; 2005. [Google Scholar]
- 2.Knofler M, Kalionis B, Huelseweh B, Bilban M, Morrish DW. Novel genes and transcription factors in placental development-a workshop report Placenta. 2000;(21 Suppl A):S71–73. doi: 10.1053/plac.1999.0531. [DOI] [PubMed] [Google Scholar]
- 3.Cross JC, Baczyk D, Dobric N, Hemberger M, Hughes M, Simmons DG, Yamamoto H, Kingdom JC. Genes, development and evolution of the placenta. Placenta. 2003;24:123–130. doi: 10.1053/plac.2002.0887. [DOI] [PubMed] [Google Scholar]
- 4.Rawn SM, Cross JC. The evolution, regulation, and function of placenta-specific genes. Annu Rev Cell Dev Biol. 2008;24:159–181. doi: 10.1146/annurev.cellbio.24.110707.175418. [DOI] [PubMed] [Google Scholar]
- 5.Anson-Cartwright L, Dawson, Kerri, Holmyard, Doug, Fisher, Susan J, Lazzarini, Robert A, Cross, James C. The glial missing-1 protein is essential for branching morphogenesis in the chorioallantoic placenta. Nature Genetics. 2000;25:314–315. doi: 10.1038/77076. [DOI] [PubMed] [Google Scholar]
- 6.Baczyk D, Satkunaratnam A, Nait-Oumesmar B, Huppertz B, Cross JC, Kingdom JC. Complex patterns of GCM1 mRNA and protein in villous and extravillous trophoblast cells of the human placenta. Placenta. 2004;25:553–559. doi: 10.1016/j.placenta.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 7.de Mestre AM, Miller D, Roberson MS, Liford J, Chizmar LC, McLaughlin KE, Antczak DF. Glial cells missing homologue 1 is induced in differentiating equine chorionic girdle trophoblast cells. Biol Reprod. 2009;80:227–234. doi: 10.1095/biolreprod.108.070920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cross JC, Nakano H, Natale DR, Simmons DG, Watson ED. Branching morphogenesis during development of placental villi. Differentiation. 2006;74:393–401. doi: 10.1111/j.1432-0436.2006.00103.x. [DOI] [PubMed] [Google Scholar]
- 9.Kingdom J, Huppertz B, Seaward G, Kaufmann P. Development of the placental villous tree and its consequences for fetal growth. Eur J Obstet Gynecol Reprod Biol. 2000;92:35–43. doi: 10.1016/s0301-2115(00)00423-1. [DOI] [PubMed] [Google Scholar]
- 10.Sagol S, Sagol O, Ozdemir N. Stereological quantification of placental villus vascularization and its relation to umbilical artery Doppler flow in intrauterine growth restriction. Prenat Diagn. 2002;22:398–403. doi: 10.1002/pd.323. [DOI] [PubMed] [Google Scholar]
- 11.Bane AL, Gillan JE. Massive perivillous fibri-noid causing recurrent placental failure. Bjog. 2003;110:292–295. [PubMed] [Google Scholar]
- 12.Chen CP, Chen CY, Yang YC, Su TH, Chen H. Decreased placental GCM1 (glial cells missing) gene expression in pre-eclampsia. Placenta. 2004;25:413–421. doi: 10.1016/j.placenta.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 13.Baraban E, McCoy L, Simon P. Increasing prevalence of gestational diabetes and pregnancy-related hypertension in Los Angeles County, California, 1991-2003. Prev Chronic Dis. 2008;5:A77. [PMC free article] [PubMed] [Google Scholar]
- 14.Wolf M, Shah A, Jimenez-Kimble R, Sauk J, Ecker JL, Thadhani R. Differential risk of hypertensive disorders of pregnancy among Hispanic women. J Am Soc Nephrol. 2004;15:1330–1338. doi: 10.1097/01.asn.0000125615.35046.59. [DOI] [PubMed] [Google Scholar]
- 15.Tanaka M, Jaamaa G, Kaiser M, Hills E, Soim A, Zhu M, Shcherbatykh IY, Samelson R, Bell E, Zdeb M, McNutt LA. Racial disparity in hypertensive disorders of pregnancy in New York State: a 10-year longitudinal population-based study. Am J Public Health. 2007;97:163–170. doi: 10.2105/AJPH.2005.068577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Velentgas P, Benga-De E, Williams MA. Chronic hypertension, pregnancy-induced hypertension, and low birthweight. Epidemiology. 1994;5:345–348. doi: 10.1097/00001648-199405000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Osterman MJ, Martin JA, Menacker F. Expanded health data from the new birth certificate, 2006. Natl Vital Stat Rep. 2009;58:1–24. [PubMed] [Google Scholar]
- 18.Yeo S, Wells PJ, Kieffer EC, Nolan GH. Preeclampsia among Hispanic women in a Detroit health system. Ethn Dis. 2007;17:118–121. [PubMed] [Google Scholar]
- 19.Brown HL, Chireau MV, Jallah Y, Howard D. The “Hispanic paradox”: an investigation of racial disparity in pregnancy outcomes at a tertiary care medical center. Am J Obstet Gynecol. 2007;197:e191–197. doi: 10.1016/j.ajog.2007.04.036. 197 discussion 197 e197-199. [DOI] [PubMed] [Google Scholar]
- 20.Goodwin AA, Mercer BM. Does maternal race or ethnicity affect the expression of severe preeclampsia? Am J Obstet Gynecol. 2005;193:973–978. doi: 10.1016/j.ajog.2005.05.047. [DOI] [PubMed] [Google Scholar]
- 21.Wilson ML, Desmond DH, Goodwin TM, Miller DA, Ingles SA. Maternal and fetal variants in the TGF-beta3 gene and risk of pregnancy-induced hypertension in a predominantly Latino population. Am J Obstet Gynecol. 2009;201:e291–295. doi: 10.1016/j.ajog.2009.05.038. 295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Landau R, Xie HG, Dishy V, Wood AJ, Stein CM, Smiley RM. No association of the Asp298 variant of the endothelial nitric oxide synthase gene with preeclampsia. Am J Hypertens. 2004;17:391–394. doi: 10.1016/j.amjhyper.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 23.Bashford MT, Hefler LA, Vertrees TW, Roa BB, Gregg AR. Angiotensinogen and endothelial nitric oxide synthase gene polymorphisms among Hispanic patients with preeclampsia. Am J Obstet Gynecol. 2001;184:1345–1350. doi: 10.1067/mob.2001.115048. discussion 1350-1341. [DOI] [PubMed] [Google Scholar]
- 24.Hefler LA, Tempfer CB, Gregg AR. Polymorphisms within the interleukin-1 beta gene cluster and preeclampsia. Obstet Gynecol. 2001;97:664–668. doi: 10.1016/s0029-7844(01)01128-0. [DOI] [PubMed] [Google Scholar]
- 25.Steinfeld JD, Valentine S, Lerer T, Ingardia CJ, Wax JR, Curry SL. Obesity-related complications of pregnancy vary by race. J Matern Fetal Med. 2000;9:238–241. doi: 10.1002/1520-6661(200007/08)9:4<238::AID-MFM10>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 26.Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol. 2000;183:S1–S22. [PubMed] [Google Scholar]
- 27.Lum A, Le Marchand L. A simple mouth-wash method for obtaining genomic DNA in molecular epidemiological studies. Cancer Epidemiol Biomarkers Prev. 1998;7:719–724. [PubMed] [Google Scholar]
- 28.Shi M, Umbach DM, Vermeulen SH, Weinberg CR. Making the most of case-mother/control-mother studies. Am J Epidemiol. 2008;168:541–547. doi: 10.1093/aje/kwn149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schisterman EF, Cole SR, Platt RW. Overad-justment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20:488–495. doi: 10.1097/EDE.0b013e3181a819a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glymour M. Using Causal Diagrams to Understand Common Problems in Social Epidemilogy. In: Oakes J KJ, editor. Methods in Social Epidemiology. San Francisco: Wiley & Sons; 2006. pp. 393–428. [Google Scholar]
- 31.Barrett JC, Fry B, Mailer J, Daly MJ. Hap-loview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21:263–265. doi: 10.1093/bioinformatics/bth457. [DOI] [PubMed] [Google Scholar]
- 32.Vermunt JK. Tilberg, Netherlands: 1997. LEM: A General Program for the Analysis of Categorical Data, T. Department of Methodology and Statistics and University, Editors. [Google Scholar]
- 33.Thompson WD. “Overadjustment in case-control studies”. Am J Epidemiol. 1982;115:797–801. doi: 10.1093/oxfordjournals.aje.a113364. [DOI] [PubMed] [Google Scholar]
- 34.Kalantar-Zadeh K, Kuwae N, Regidor DL, Kovesdy CP, Kilpatrick RD, Shinaberger CS, McAllister CJ, Budoff MJ, Salusky IB, Kopple JD. Survival predictability of time-varying indicators of bone disease in maintenance hemodialysis patients. Kidney Int. 2006;70:771–780. doi: 10.1038/sj.ki.5001514. [DOI] [PubMed] [Google Scholar]
- 35.Ferguson-Smith AC, Moore T, Detmar J, Lewis A, Hemberger M, Jammes H, Kelsey G, Roberts CT, Jones H, Constancia M. Epigenetics and imprinting of the trophoblast – a workshop report. Placenta. 2006;(27 Suppl A):S122–126. doi: 10.1016/j.placenta.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 36.Maccani MA, Marsit CJ. Epigenetics in the placenta. Am J Reprod Immunol. 2009;62:78–89. doi: 10.1111/j.1600-0897.2009.00716.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tabano S, Colapietro P, Cetin I, Grati FR, Zanutto S, Mando C, Antonazzo P, Pileri P, Rossella F, Larizza L, Sirchia SM, Miozzo M. Epigenetic modulation of the IGF2/H19 imprinted domain in human embryonic and extraembryonic compartments and its possible role in fetal growth restriction. Epigenetics. 5 doi: 10.4161/epi.5.4.11637. [DOI] [PubMed] [Google Scholar]
- 38.Baczyk D, Drewlo S, Proctor L, Dunk C, Lye S, Kingdom J. Glial cell missing-1 transcription factor is required for the differentiation of the human trophoblast. Cell Death Differ. 2009 doi: 10.1038/cdd.2009.1. [DOI] [PubMed] [Google Scholar]
- 39.Schubert SW, Lamoureux N, Kilian K, Klein-Hitpass L, Hashemolhosseini S. Identification of integrin-alpha4, Rb1, and syncytin a as murine placental target genes of the transcription factor GCMa/Gcm1. J Biol Chem. 2008;83:5460–5465. doi: 10.1074/jbc.M710110200. [DOI] [PubMed] [Google Scholar]
- 40.Chiang MH, Liang FY, Chen CP, Chang CW, Cheong ML, Wang LJ, Liang CY, Lin FY, Chou CC, Chen H. Mechanism of hypoxia-induced GCM1 degradation: Implications for the pathogenesis of preeclampsia. J Biol Chem. 2009 doi: 10.1074/jbc.M109.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yu C, Shen K, Lin M, Chen P, Lin C, Chang GD, Chen H. GCMa regulates the syncytinmediated trophoblastic fusion. J Biol Chem. 2002;277:50062–50068. doi: 10.1074/jbc.M209316200. [DOI] [PubMed] [Google Scholar]
- 42.Chang M, Mukherjea D, Gobble RM, Groesch KA, Torry RJ, Torry DS. Glial cell missing 1 regulates placental growth factor (PGF) gene transcription in human trophoblast. Biol Reprod. 2008;78:841–851. doi: 10.1095/biolreprod.107.065599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maynard S, Epstein FH, Karumanchi SA. Preeclampsia and angiogenic imbalance. Annu Rev Med. 2008;59:61–78. doi: 10.1146/annurev.med.59.110106.214058. [DOI] [PubMed] [Google Scholar]
- 44.Maynard MA, Qi H, Chung J, Lee EH, Kondo Y, Hara S, Conaway RC, Conaway JW, Ohh M. Multiple splice variants of the human HIF-3 alpha locus are targets of the von Hippel-Lindau E3 ubiquitin ligase complex. J Biol Chem. 2003;278:11032–11040. doi: 10.1074/jbc.M208681200. [DOI] [PubMed] [Google Scholar]
- 45.Aggarwal PK, Jain V, Sakhuja V, Karumanchi SA, Jha V. Low urinary placental growth factor is a marker of pre-eclampsia. Kidney Int. 2006;69:621–624. doi: 10.1038/sj.ki.5000075. [DOI] [PubMed] [Google Scholar]
- 46.Levine RJ, Thadhani R, Qian C, Lam C, Lim KH, Yu KF, Blink AL, Sachs BP, Epstein FH, Sibai BM, Sukhatme VP, Karumanchi SA. Urinary placental growth factor and risk of preeclampsia. JAMA. 2005;293:77–85. doi: 10.1001/jama.293.1.77. [DOI] [PubMed] [Google Scholar]
- 47.Levine RJ, Qian C, Maynard SE, Yu KF, Epstein FH, Karumanchi SA. Serum sFlt1 concentration during preeclampsia and mid trimester blood pressure in healthy nulliparous women. Am J Obstet Gynecol. 2006;194:1034–1041. doi: 10.1016/j.ajog.2005.10.192. [DOI] [PubMed] [Google Scholar]
- 48.Levine RJ, Lam C, Qian C, Yu KF, Maynard SE, Sachs BP, Sibai BM, Epstein FH, Romero R, Thadhani R, Karumanchi SA. Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med. 2006;355:992–1005. doi: 10.1056/NEJMoa055352. [DOI] [PubMed] [Google Scholar]
- 49.Levine RJ, Karumanchi SA. Circulating angiogenic factors in preeclampsia. Clin Obstet Gynecol. 2005;48:372–386. doi: 10.1097/01.grf.0000160313.82606.d7. [DOI] [PubMed] [Google Scholar]
- 50.Ahmad S, Ahmed A. Elevated placental soluble vascular endothelial growth factor receptor-1 inhibits angiogenesis in preeclampsia. Circ Res. 2004;95:884–891. doi: 10.1161/01.RES.0000147365.86159.f5. [DOI] [PubMed] [Google Scholar]
- 51.Lim JH, Kim SY, Park SY, Yang JH, Kim MY, Ryu HM. Effective prediction of preeclampsia by a combined ratio of angiogenesis-related factors. Obstet Gynecol. 2008;111:1403–1409. doi: 10.1097/AOG.0b013e3181719b7a. [DOI] [PubMed] [Google Scholar]
- 52.Woo KT, Lau YK, Wong KS, Zhao Y, Chan CM. Parallel genotyping of 10,204 single nucleotide polymorphisms to screen for susceptible genes for IgA nephropathy. Ann Acad Med Singapore. 2009;38:894–899. [PubMed] [Google Scholar]
- 53.Thangaratinam S, Coomarasamy A, O'Mahony F, Sharp S, Zamora J, Khan KS, Ismail KM. Estimation of proteinuria as a predictor of complications of pre-eclampsia: a systematic review. BMC Med. 2009;7:10. doi: 10.1186/1741-7015-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wilson ML, Goodwin TM, Pan VL, Ingles SA. Molecular epidemiology of preeclampsia. Obstet Gynecol Surv. 2003;58:39–66. doi: 10.1097/00006254-200301000-00022. [DOI] [PubMed] [Google Scholar]