Abstract
Purpose
This study examined the relationship between level of treatment engagement through completion of homework and treatment outcomes within non-pharmacological interventions for participants with ME/CFS.
Methods
A sample of 82 participants with ME/CFS was randomly assigned to one of four non-pharmacological interventions. Each intervention involved 13 sessions over the course of six months. Change scores were computed for self-report measures taken at baseline and 12-month follow-up. Homework compliance was calculated as the percentage of completed assignments across the total number of sessions and grouped into three categories: minimum (0–25%), moderate (25.1–75%), or maximum (75.1–100%).
Results
Findings revealed that after controlling for treatment condition, those who completed a maximum amount of homework had greater improvement on a number of self-report outcome measures involving role, social and mental health functioning. There were no differential improvements in physical and fatigue functioning based on level of homework compliance.
Implications
Findings from this study suggest homework compliance can have a positive influence on some aspects of physical, social, and mental health functioning in participants with ME/CFS. It should be emphasized that these interventions do not cure this illness. The lack of significant changes in physical functioning and fatigue levels suggests a need for more multidisciplinary treatment approaches that can elicit improvement in these areas.
Keywords: Myalgic Encephalomyelitis, chronic fatigue syndrome, Non-pharmacological, Homework, Outcomes
Patients with Myalgic Encephalomyelitis/chronic fatigue syndrome (ME/CFS) have varying degrees of symptom severity and duration (Fukuda et al., 1994). The high levels of fatigue and impaired physical functioning experienced by individuals with ME/CFS can often result in drastic life changes affecting physical, social, and mental well being as well as overall quality of life (Anderson & Ferrans, 1997; Prins et al., 2001; Van Houdenhove & Luyten, 2008). While further research is exploring the multiple factors that contribute to the severity and duration of the illness, individuals with ME/CFS continue to have difficulty managing its debilitating effects.
In order to address both physical disability and coping skills, non-pharmacological interventions have been developed as palliative treatment approaches for a number of chronic illnesses. For example, behavioral interventions have demonstrated positive outcomes in coping with pain among individuals with cancer (Redinbaugh, Creola, Arnold, & Baum, 2004), and cognitive-behavioral stress management has been shown to reduce distress, improved quality of life, and increase cellular functioning in participants with HIV and different forms of cancer (Antoni et al., 2006a; Antoni et al., 2006b; Penedo et al., 2006). However, the use of these treatment approaches for ME/CFS has been extremely controversial.
Non-pharmacological interventions that involve increasing levels of physical activity can pose challenges for participants with ME/CFS who struggle to complete minimal activity due to their level of disability (Bazelmans, Prins, & Bleijenberg, 2006; Twisk & Maes, 2009). Further, participants with ME/CFS often experience post-exertional malaise, and exercise can actually worsen participants’ symptoms. For example, Black, O’Connor, and McCully (2005) found that after a four week period, participants with ME/CFS who increased their daily activity by an average of 28% experienced a worsening in overall mood, muscle pain intensity, and time spent each day with fatigue. Later reports by Black and McCully (2005) concluded that participants with ME/CFS developed exercise intolerance as demonstrated by a reduction in total daily activity after 4 to 10 days of increased activity.
Survey reports from individuals with ME/CFS have found that graded exercise protocols can influence symptom flare-ups (Cooper, 2001; Preliminary Report, 2001). Arecent review reported that different non-pharmacological interventions produce varying results for participants with ME/CFS and may not be well suited for many individuals with ME/CFS (Twisk & Maes, 2009). Similarly, some studies of behavioral interventions for ME/CFS have reported high dropout rates, which may indicate a lack of acceptability of the treatment among participants (Whiting et al., 2001). Price, Mitchell, Tidy, and Hunot (2008) reviewed 15 studies of cognitive behavioral therapy (CBT) with a total of 1,043 participants with ME/CFS. At treatment end, 40% of the CBT group showed clinical improvement in contrast to only 26% in usual care, but changes were not maintained at a 1 to 7 month follow-up when including people who had dropped out. Further research is needed to identify aspects of these interventions that might be related to outcomes.
One method for understanding outcomes of non-pharmacological interventions for ME/CFS is to evaluate treatment engagement. In particular, examining compliance with protocol that is assigned for completion outside of treatment (i.e., homework) can provide context for understanding intervention effects. Completion of homework assignments, such as at-home practice between sessions, is an important element to any psychotherapeutic intervention (Burns & Spangler, 2000). The implementation of at-home practice and homework assignments has been used for many illnesses in order to help individuals manage symptoms and regain control of their daily activities (Addis & Jacobson, 2000; Kazantzis, Whittington, & Dattilio, 2010; Neimeyer & Feixas, 1990). In a recent meta-analysis of non-pharmacological interventions, Kazantzis et al. (2010) reported that 68% of participants experience improvement in treatments that require homework while only 32% of participants improve in treatments that do not require any homework; suggesting that between-session assignments are an active component of treatment.
Although several studies have examined the efficacy of non-pharmacological interventions for ME/CFS, no studies have determined the role of homework compliance in study outcomes. The goal of this study was to explore the effect of homework compliance on treatment outcomes following participant involvement in non-pharmacological interventions for ME/CFS. This study examined homework compliance within a longitudinal study of participants with ME/CFS in order to determine whether regular completion of homework assignments contributed to positive outcomes. It was hypothesized that participants with ME/CFS who were more engaged in treatment through compliance with between-session homework and at-home practice would show significantly greater improvements in areas of functioning compared to those who were less engaged.
Methods
Participants
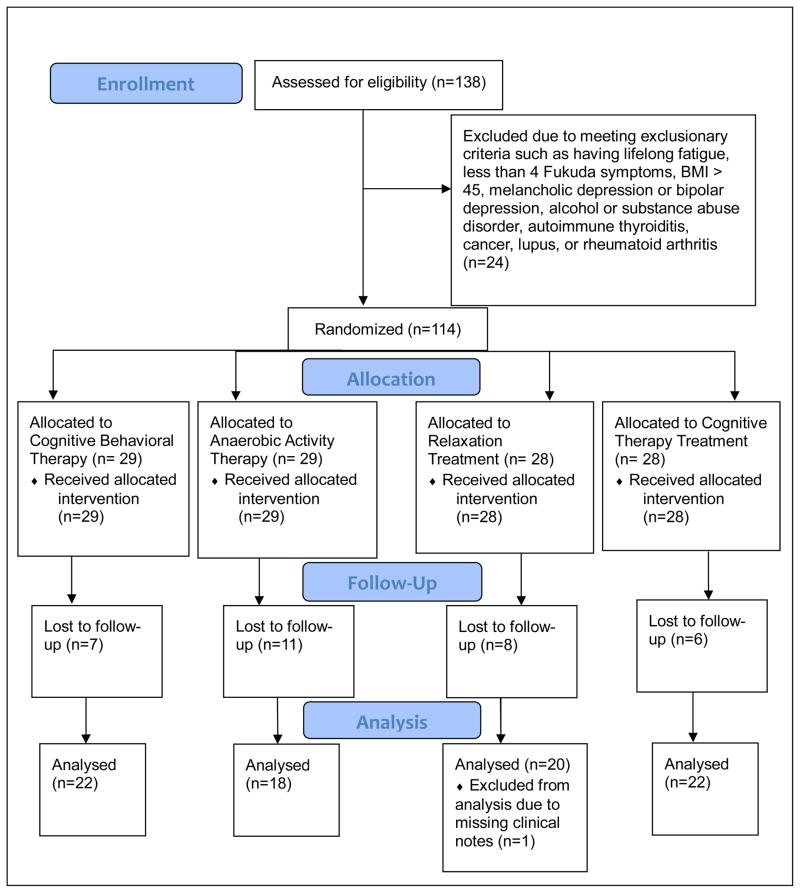
This study utilized data from a larger study of non-pharmacological interventions for ME/CFS (Jason et al., 2007). The original sample consisted of 114 participants with ME/CFS based on the criteria established by Fukuda et al. (1994). Participants completed a physical examination including lab tests, a psychiatric assessment, and a self-report health questionnaire (Komaroff et al., 1996) to assess symptomatology and rule out exclusionary physical or psychiatric conditions for an ME/CFS diagnosis (Fukuda et al., 1994). In order to test changes in functioning between baseline and the 12-month follow-up period, participants were required to have complete data at both time points. Due to one participant lacking therapy notes and 31 others missing 12-month follow-up data, 82 participants from the original sample were retained for analysis in the present investigation.
Of the 82 participants, 81.7% were female and 18.3% were male, and their ages ranged from 18 to 65 (M=45.26, SD=10.92). The ethnic diversity of the sample ranged with 87.8% white, 4.9% African American, 4.9% Latino or Hispanic, and 2.4% Asian participants. The work status of participants was split with 61% not working and 39% working. Further, individuals varied on employment status with 57.3% retired, unemployed, or on disability, 37.9% working full or part time, 3.6% full or part time students, and 1.2% working part time and on disability. In addition, of the participants, 50% were married or had a domestic partner, 30.5% were never married, and 19.5 % were divorced or separated. The educational level of the participants varied in degree completion with 92.7% having completed a college degree or more and 7.3% having completed less than a college degree. There were no significant differences between gender (χ2 [1, n = 113] = .47, p = .49), ethnicity (χ2 [3, n = 113]=1.30, p = .73), work status (χ2 [1, n = 113] = .08, p = .78), employment status (χ2 [7, n = 113] = 7.36, p = .39), marital status (χ2 [4, n = 112] = 2.38, p = .67), and educational level (χ2 [4, n = 113] = 4.82, p = .31) among those who were part of this sample compared to those who were lost to follow-up. In addition, the age of participants within the utilized sample did not significantly differ from those who were lost to follow-up (overall M=40.97, SD=12.76), (t [111] =1.78, p=.43).
Measures
Homework compliance
Compliance was determined by analyzing completion of homework assigned at treatment sessions. Therapy notes for each session indicated whether or not homework and at-home practice were completed based on therapist reports. In most cases, therapists used yes/no checkboxes indicating homework completion for each session. In some cases the checkboxes were unmarked, and in this instance the session narrative was examined for indication of homework completion. The therapists were generally flexible about turning in assignments and allowed participants who utilized phone sessions to fax or email the assignments. If a participant did not attend an in-person or phone session, their assignments for that session were considered incomplete unless otherwise stated by the therapist. Two types of homework were assigned within this study. “Homework” consisted of assignments such as readings, sleep diaries, activity diaries, etc., while “at-home-practices” consisted of activity goals, relaxation exercises, use of coping skills, etc. Homework was assigned at each session beginning at session one, for a total of 12 homework assignments. At-home practices were assigned at each session beginning at session two, for a total of 11 at-home practices. Between homework and at-home practices, there were a total of 23 assignments administered over the course of treatment. For each participant, the number of completed assignments was divided by 23 in order to measure the percentage of homework compliance.
Medical Outcomes Study-Short Form36-Item Health Survey (SF-36)
The SF-36 consists of 36 self-report items of health status effects on functioning (Ware & Sherbourne, 1992). For this measure, higher scores demonstrate improved or less detriment of health on functioning. Studies of test construction on the SF-36 have shown high internal consistency and significant discriminate validity between subscales, and substantial differences in score pattern between patient and control samples (McHorney, Ware, Lu, & Sherbourne, 1994). The SF-36 has also been validated in a sample of participants with CFS as sufficiently measuring psychometric properties of functional status (Buchwald, Pearlman, Umali, Schmaling, & Katon, 1996). The SF-36 consists of eight subscales including: Role Physical, Role Emotional, Mental Health, General Health, Bodily Pain, Social Functioning, Vitality, and Physical Functioning.
Fatigue Severity Scale (FSS)
The FSS (Krupp, LaRocca, Muir-Nash, & Steinberg, 1989) was used to assess level of fatigue in participants. The nine items, which are rated on a seven-point scale, understand fatigue severity as having different quality and intensity across participants. Also, many questions refer to the behavioral consequences of fatigue. Previous findings have utilized the FSS (Krupp et al., 1989) to differentiate between individuals with CFS, MS, and primary depression (Pepper, Krupp, Friedberg, Doscher, & Coyle, 1993). In a comparison between the Fatigue Scale (Chalder, Berelowitz, Pawlikowska, Watts, & Wessely, 1993) and the FSS (Krupp et al., 1989) on a sample of healthy controls and a CFS-like group (Taylor, Jason, & Torres, 2000), the CFS-like group showed more association with severity ratings for the eight Fukuda et al. (1994) CFS symptoms and fatigue related functional outcomes on the FSS (Krupp et al., 1989).
Beck Depression Inventory (BDI-II)
Due to the common comorbidity of depression with CFS (Friedberg, 1996), the BDI-II (Beck, Steer, & Brown, 1996) was used to measure depression severity. The BDI-II measures depressive symptoms through self-report across 21-items with validated psychometric properties. Compared to the earlier version, the BDI-II (Beck et al., 1996) is more congruent with the criteria for major depressive disorder as described in the DSM-IV. Due to overlapping symptoms of ME/CFS with items on the BDI-II (e.g., tiredness or fatigue, concentration difficulty), scores were evaluated for two BDI-II factors separately in order to evaluate somatic items separately. In a factor analysis by Arnau, Meagher, Norris, and Bramson (2001), Cognitive and Somatic-Affective factors were revealed for a primary care sample, and these two factors were evaluated separately in the present investigation.
Procedures
Upon enrollment, participants were randomized to four nurse-delivered, non-pharmacological interventions. Of the 82 participants examined in this study, 22 (26.8%) were randomized to CBT with graded activity (CBT), 22 (26.8%) were randomized to cognitive coping skills (COG), 20 (24.4%) were randomized to relaxation training (RELAX), and 18 (22%) were randomized to the anaerobic exercise condition (ACT). There were no significant differences in treatment assignment for those who comprised the sample of 82 in this study compared to those who were lost to follow-up (χ2 [3, n = 114] = 2.23, p = .50).
The CBT condition involved cognitive strategies for stress management and schedules of planned, graded activities. Participants were also instructed to keep record of activities, stressors, and sleep to develop appropriate daily target levels and reduce setbacks. In the COG condition, coping and stress reduction skills were taught through implementation of relaxation exercises and imagery and positive mood techniques. While the COG condition did not require mild activity increases, as the CBT condition did, participants were taught to pace activities and keep daily stress and fatigue diaries. The ACT condition aimed to educate participants on energy systems and prescribe and monitor low levels of exercise to increase functional gains. To reinforce slow, gradual progression, exercise records were kept by participants and assessed by the therapists to ensure suitability of goals and prevent symptom exacerbation. Despite similarities in activity increase between ACT and CBT conditions, the ACT condition did not incorporate any cognitive intervention. The RELAX condition involved teaching progressive muscle relaxation and autogenic training, that incorporated skills such as breathing exercises and yoga stretching. Although both COG and RELAX involved a relaxation component, the RELAX condition did not involve any cognitive therapeutic techniques. Participants were encouraged to keep daily records of stress and relaxation and implement learned techniques in strenuous situations. A more thorough description of individual interventions is detailed in (Jason et al., 2007).
A clear framework was used within each intervention, however, the intensity of homework assignments (e.g., duration of physical activity, number of repetitions, etc.) were tailored to the individual abilities of participants. For the purposes of the present investigation, the four treatment conditions were analyzed together, and are referred to more generally as non-pharmacological interventions. Across interventions, 13 biweekly sessions were completed over the span of six months with homework and at-home practices assigned at each session. Participants completed 10 sessions on average, with a range of one to 13 sessions attended. A battery of self-report measures was completed by participants at baseline and 12-months after treatment.
Since therapy notes did not always clearly indicate assignment completion, inter-rater scoring was used to code assignment completion to confirm accurate ratings of homework compliance. Twenty-two percent of the participants were randomly selected to be coded by a second rater to ensure reliable completion ratings. If the raters disagreed on the group designated for homework compliance, the treatment notes were revisited, and the final compliance group assignment was made once consensus was reached between the two raters. To determine the consistency of homework completion rating, inter-rater reliability analysis was completed using the Kappa statistic. Homework completion ratings were found to be consistent, κ = 0.8 (p < 0.001), 95% CI (0.541, 1.106).
Once homework completion ratings were confirmed, participants were grouped into three categories based on their level of homework compliance (i.e., number of completed assignments divided by 32), including minimum (0–25%), moderate (25.1–75%), or maximum (75.1–100%) assignment completion.
Analysis
Change scores were computed for each outcome variable by subtracting baseline scores from 12-month follow-up scores. A multivariate analysis of covariance (MANCOVA) was used to determine whether homework compliance group (i.e., minimum, moderate, maximum) would influence baseline to 12-month follow-up change scores on the following variables: Physical Functioning, Social Functioning, Role Physical, Role Emotional, Vitality, Mental Health, General Health, Bodily Pain, Fatigue Severity, Cognitive BDI-II factor, and Somatic-Affective BDI-II factor. Wilks’ Lambda F approximation was used for interpretation of multivariate tests. After a significant multivariate effect was found, univariate ANOVAs were examined. Bonferroni post hoc analyses were used to compare mean differences if a significant effect of homework compliance on outcomes was revealed.
No significant differences were found among the three groups on demographic variables, so these variables were not included as covariates in the analysis. A chi-square analysis revealed a significant relationship between the homework compliance grouping and treatment assignment (χ2 (6, n = 82) = 15.63, p = .02). Of those in the maximum group, the highest percentage were in the COG condition (55.6%), and the lowest percentage were in the RELAX condition (5.6%). Of those in the moderate group, the highest percentage were in the CBT condition (33.3%), and the lowest percentage were in the ACT condition (18.8%). Of those in the minimum group, the highest percentage were in the ACT and RELAX (37.5%) conditions, and the lowest percentage were in CBT and COG (12.5%).
Results
Results showed that after for controlling for treatment assignment, there was a significant effect of homework compliance group on the collective outcomes of SF-36, FSS, and BDI-II factor variables, F(22, 136) = 1.65, p = .05. Due to the significant overall effect, univariate effects were examined next. Table 1 shows the mean change scores for the three homework compliance groups.
Table 1.
Differences in outcomes across homework compliance groups
| Outcome (baseline to 12 month follow up change scores) | Homework compliance groupings
|
Sig. | ||
|---|---|---|---|---|
| Minimum (0–25%) n=16 | Moderate (25.1–75%) n=48 | Maximum (75.1–100%) n=18 | ||
| SF-36 | ||||
| Physical Functioning | 6.99 (19.30) | 7.55 (18.85) | 17.50 (18.09) | |
| Role Physical | −1.47 (18.69)a,b | 19.39 (29.43)a | 30.56 (37.92)b | * |
| Role Emotional | −3.92 (51.21) | 10.42 (37.13) | 16.67 (58.58) | |
| Mental Health | −8.71 (22.42)a | 3.35 (19.40) | 9.19 (20.71)a | * |
| General Health | 10.87 (14.55) | 7.59 (21.46) | 15.19 (28.28) | |
| Bodily Pain | 5.35 (23.33) | 8.18 (19.95) | 14.06 (16.13) | |
| Social Functioning | −6.62 (23.01)a,b | 10.71 (25.90)a | 15.97 (24.56)b | * |
| Vitality | 8.82 (13.17) | 7.86 (17.85) | 16.39 (18.13) | |
| Fatigue Severity Scale | −0.17 (0.73) | −0.51 (1.00) | −0.54 (1.09) | |
| Beck Depression Inventory factors† | ||||
| Cognitive | 0.56 (4.94) | −1.50 (2.39) | −1.89 (2.45) | * |
| Somatic-Affective | 0.68 (5.66) b | −1.35 (5.54) b | −5.75 (6.24) a,b | * |
Notes. Treatment assignment included as covariate. Similar letters across rows indicate significant difference. SF-36= Medical Outcomes Survey Short form-36. Higher scores on the SF-36 indicate better functioning. Higher scores on the Fatigue Severity Scale and Beck Depression Inventory factors indicate greater levels of impairment.
As derived from Arnau, R., Meagher, M., Norris, M., & Bramson, R. (2001). Psychometric evaluation of the Beck Depression Inventory-II with primary care medical patients. Health Psychology, 20, 112–119.
Statistically significant univariate effect at the p < .05 level.
Significant univariate effects were found between groups for Role Physical, F(2,78) = 5.02, p = .01; Social Functioning, F(2,78)= 3.89, p =.02; Mental Health, F(2,78) = 3.52, p = .03; the Somatic-Affective BDI-II factor, F(2,78) = 5.76, p = .01; and the Cognitive BDI-II factor, F(2,78) = 3.84, p =.03, scores. Bonferroni post hoc analyses revealed that those completing moderate and maximum amounts of homework were significantly more improved in Role Physical and Social Functioning compared to those completing minimum amounts of homework. A significant difference was also found for Mental Health, such that those completing maximum amounts of homework improved more than those completing minimum amounts of homework. In addition, those completing maximum amounts of homework were significantly more improved in the Somatic-Affective BDI-II factor symptoms than those completing minimum and moderate amounts of homework. No significant post hoc differences were revealed for the Cognitive BDI-II factor. No significant univariate effects were found for Physical Functioning, Vitality, General Health, Bodily Pain, and Role Emotional. A significant univariate effect was not observed for Fatigue Severity. Directionally, increased homework compliance was associated with more positive improvements on all outcomes with the exception of General Health and Vitality.
Because participants who missed sessions were counted as also missing homework assignments, homework compliance and session attendance were not fully independent of one another. Consequently, we were unable to examine homework compliance exclusive of session attendance. In an attempt to address whether session attendance alone had an effect on outcomes, a multiple regression was conducted with number of sessions attended included as the dependent variable and change scores included as predictor variables, no significant relationships were found among the change scores and the number of sessions attended (β = .001 to .067; p = .21 to .97).
Discussion
After controlling for treatment condition, this study found that those who completed a moderate or maximum amount of homework had the greatest amount of improvement in SF-36 Role Physical functioning and Social Functioning compared to those who completed a minimum amount of homework. For Role Physical, improvements suggest participants reduced the amount of interference with work or daily activities due to health problems. For Social Functioning, improvements indicate that participants were able to engage in social activities with less interference due to health or emotional problems. Those completing a maximum amount of homework also had more improvement in SF-36 Mental Health scores than those who did a minimum amount of homework, indicating a reduction in depressed and anxious mood. Also, those who completed maximum amounts of homework had greater improvement in Somatic-Affective BDI-II factor symptoms as compared to those completing moderate or minimum amounts of homework. The improvement in the Somatic-Affective BDI-II factor suggests relief in symptoms such as loss of pleasure, tiredness or fatigue, and concentration difficulty. While there was an overall effect for Cognitive BDI-II factor symptoms, there were no significant differences between homework compliance groups. Interestingly, session attendance alone was unrelated to outcomes, suggesting that homework compliance has a particular influence on outcomes in non-pharmacological interventions for ME/CFS.
Studies have shown that non-pharmacological interventions for ME/CFS can help reduce fatigue and improve levels of physical functioning (Price et al., 2008; Whiting et al., 2001). Findings from non-pharmacological clinical trials for other chronic illnesses, such as cancer and HIV, have also shown positive effects on mental health, fatigue, and physiology (Antoni et al., 2006a; Antoni et al., 2006b; Penedo et al., 2006; Redinbaugh et al., 2004). Findings from this study suggest that homework compliance has an active role in improving functioning and symptoms in some domains for participants with ME/CFS. However, because the effects of non-pharmacological interventions do not produce an overall recovery for participants with most chronic illnesses, a multidisciplinary approach to treatment is often recommended (Redinbaugh et al., 2004; Sayger, Bowersox, & Steinberg, 1996). With this in mind, future research should consider providing treatment across multiple domains for participants with ME/CFS (i.e., integrating the best of both biological and non-biological approaches) in order to provide support for the many detriments caused by this illness (Goudsmit et al., 2009; Jason et al., 2007; Van Houdenhove & Luyten, 2008). In addition, recognition of individual patient differences may help to tailor treatment protocols for participants with ME/CFS and elicit the most improvement.
An important aspect of treatment delivery in this study was that the four interventions were guided by their respective frameworks, but they also allowed for flexibility in determining the appropriate intensity of homework to assign. This is in contrast to rigid, manualized interventions that prescribe the same amount of activity for all patients regardless of ability level. Individuals with ME/CFS who experience high levels of disability may be unable to comply with homework assignments. Consequently, the benefits of these otherwise effective interventions may be restricted to individuals with higher functioning. Non-pharmacological interventions may need to incorporate self management practices, such as pacing or staying within their energy envelopes, into the protocol in order to respect a patient’s level of limitation and further aid in energy maintenance (Goudsmit & Howes, 2008; Jason et al., 2007).
Upon examination of the level of homework compliance across treatment conditions, it was found that those in the COG condition were more likely to complete maximum amounts of homework, those in the CBT condition were more likely to complete moderate amounts of homework, and those in the ACT and RELAX conditions were more likely to complete minimum amounts of homework. The original findings from Jason et al. (2007) showed that across conditions participants experienced some improvement, but those in the COG condition had the highest number of positive changes, and those in CBT, ACT, and RELAX successively following with number of positive changes. The relationship between homework compliance and treatment condition is not explicitly clear, but could be due to a number of factors, such as theoretical implication of the treatments. For example, unlike the other conditions, the COG condition did not require any type of activity increase, so participants may have found it easier to complete homework assignments. Similarly, since the CBT condition involved therapeutic techniques that were similar to the COG condition but also required mild activity increases, participants’ may have found some assignments easier to complete than others. Additionally, the influence of external factors, such as symptom variation, experienced reductions, or satisfaction with treatment, may have played a role in determining the amount of homework participants were able to complete.
Limitations in the present study include collapsing the four different treatment conditions. In doing so we were unable to determine effects of homework compliance between interventions. In addition, the small sample sizes in homework compliance groupings used for statistical comparisons suggests future studies should expand upon these findings in order to increase external validity of homework compliance effects. Moreover, level of completion could have been examined more thoroughly by assessing the effort put into each assignment; however, this study considered any form of compliance as in accordance with therapist ratings. And while qualitative feedback was unavailable for the analysis of homework compliance, future studies should take participant explanations for noncompliance into consideration. In the process of evaluating homework completion from session notes, we were unable to determine if participants completed homework when sessions were missed. Future research should address this problem by tracking homework completion using electronic diaries with time stamps. Finally, it should be noted that 11 outcomes were evaluated in this study at the p < .05 significance level, making the findings vulnerable to Type I error.
It is important to understand aspects of non-pharmacological interventions for ME/CFS that are associated with functional improvements. Some writers question whether non-pharmacological interventions are appropriate for participants with ME/CFS (Twisk & Maes, 2009). But sensitively delivered non-pharmacologic interventions might represent one component within future multidisciplinary rehabilitation programs. The present study found no differential improvements in physical and fatigue functioning based on level of homework compliance, and this suggests a need for more extensive and possibly biologically-based treatment approaches that can elicit improvement in these areas.
Figure 1.
CONSORT Diagram
Acknowledgments
The authors appreciate the financial assistance provided by the National Institute of Allergy and Infectious Diseases (grant numbers AI36295 and AI49720).
References
- Addis ME, Jacobson NS. A closer look at the treatment rationale and homework compliance in cognitive behavioral therapy for depression. Cognitive Therapy and Research. 2000;24(3):313–326. [Google Scholar]
- Anderson JS, Ferrans CE. The quality of life of persons with chronic fatigue syndrome. Journal of Nervous and Mental Disease. 1997;185(6):359–367. doi: 10.1097/00005053-199706000-00001. [DOI] [PubMed] [Google Scholar]
- Antoni MH, Carrico AW, Duran RE, Spitzer S, Penedo F, Ironson G, Schneiderman N. Randomized clinical trial of cognitive behavioral stress management on human immunodeficiency virus viral load in gay men treated with highly active antiretroviral therapy. Psychosomatic Medicine. 2006a;68:143–151. doi: 10.1097/01.psy.0000195749.60049.63. [DOI] [PubMed] [Google Scholar]
- Antoni MH, Lechner SC, Kazi A, Wimberly SR, Sifre T, Urcuyo KR, Carver CS. How stress management improves quality of life after treatment for breast cancer. Journal of Consulting and Clinical Psychology. 2006b;74:1143–1152. doi: 10.1037/0022-006X.74.6.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnau R, Meagher M, Norris M, Bramson R. Psychometric evaluation of the Beck Depression Inventory-II with primary care medical participants. Health Psychology. 2001;20:112–119. doi: 10.1037//0278-6133.20.2.112. [DOI] [PubMed] [Google Scholar]
- Bazelmans E, Prins J, Bleijenberg G. Cognitive behavior therapy for relatively active and for passive chronic fatigue syndrome patients. Cognitive and Behavioral Practice. 2006;13:157–166. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio: Psychological Corporation; 1996. [Google Scholar]
- Black CD, O’Connor PJ, McCully KK. Increased daily physical activity and fatigue symptoms in chronic fatigue syndrome. Dynamic Medicine. 2005;4:3. doi: 10.1186/1476-5918-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black CD, McCully KK. Time course of exercise induced alterations in daily activity in chronic fatigue syndrome. Dynamic Medicine. 2005;4:10. doi: 10.1186/1476-5918-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchwald D, Pearlman T, Umali J, Schmaling K, Katon W. Functional status in participants with chronic fatigue syndrome, other fatiguing illnesses, and healthy individuals. American Journal of Medicine. 1996;101:364–370. doi: 10.1016/S0002-9343(96)00234-3. [DOI] [PubMed] [Google Scholar]
- Burns DD, Spangler DL. Does psychotherapy homework lead to improvements in depression in cognitive-behavioral therapy or does improvement lead to increased homework compliance? Journal of Consulting and Clinical Psychology. 2000;68(1):46–56. doi: 10.1037//0022-006x.68.1.46. [DOI] [PubMed] [Google Scholar]
- Chalder T, Berelowitz G, Pawlikowska J, Watts L, Wessely D. Development of a fatigue scale. Journal of Psychosomatic Research. 1993;37:147–153. doi: 10.1016/0022-3999(93)90081-p. [DOI] [PubMed] [Google Scholar]
- Cooper L. Report of survey members of local ME groups. Perspectives 2001 [Google Scholar]
- Friedberg F. Chronic fatigue syndrome: A new clinical application. Professional Psychology: Research and Practice. 1996;27:487–494. [Google Scholar]
- Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: A comprehensive approach to its definition and study. Annals of Internal Medicine. 1994;121(12):953–959. doi: 10.7326/0003-4819-121-12-199412150-00009. [DOI] [PubMed] [Google Scholar]
- Goudsmit EM, Howes S. Pacing: A strategy to improve energy management in chronic fatigue syndrome. Health Psychology Update. 2008;17:46–52. [Google Scholar]
- Goudsmit EM, Ho-Yen DO, Dancey CP. Learning to cope with chronic illness. Efficacy of a multi-component treatment for people with chronic fatigue syndrome. Patient Education and Counseling. 2009;77:231–236. doi: 10.1016/j.pec.2009.05.015. [DOI] [PubMed] [Google Scholar]
- Jason LA, Torres-Harding S, Friedberg F, Corradi K, Njoku MG, Donalek J, Papernik M. Non-pharmacologic interventions for ME/CFS: A randomized trial. Journal of Clinical Psychology in Medical Settings. 2007;14:275–296. [Google Scholar]
- Kazantzis N, Whittington C, Dattilio F. Meta-analysis of homework effects in cognitive and behavioral therapy: A replication and extension. Clinical Psychology Science and Practice. 2010;17:144–156. [Google Scholar]
- Komaroff AL, Fagioli LR, Geiger AM, Doolittle TH, Lee J, Kornish RJ, Guerriero RT. An examination of the working case definition of chronic fatigue syndrome. American Journal of Medicine. 1996;100(1):56–64. doi: 10.1016/s0002-9343(96)90012-1. [DOI] [PubMed] [Google Scholar]
- Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The Fatigue Severity Scale: Application to patents with multiple sclerosis and systemic Lupus erythematosus. Archives of Neurology. 1989;46:1121–1123. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- McHorney CA, Ware JE, Lu AW, Sherbourne CD. The MOS 36-item Short Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- Neimeyer RA, Feixas G. The role of homework and skill acquisition in the outcome of group cognitive therapy for depression. Behavioral Therapy. 1990;21(3):281–292. doi: 10.1016/j.beth.2016.08.013. [DOI] [PubMed] [Google Scholar]
- Penedo FJ, Molton I, Dahn JR, Shen BJ, Kinsigner MS, Traeger L, Antoni MH. A randomized clinical trial of group-based cognitive-behavioral stress management in localized prostate cancer: Development of stress management skills improves quality of life and benefit finding. Annals of Behavioral Medicine. 2006;31:261–270. doi: 10.1207/s15324796abm3103_8. [DOI] [PubMed] [Google Scholar]
- Pepper CM, Krupp LB, Friedberg F, Doscher C, Coyle PK. A comparison of neuropsychiatric characteristics in chronic fatigue syndrome, multiple sclerosis, and major depression. The Journal of Neuropsychiatry and Clinical Neurosciences. 1993;5:200–205. doi: 10.1176/jnp.5.2.200. [DOI] [PubMed] [Google Scholar]
- Preliminary Report. The severely affected. Action for ME. 2001 Feb;28:2001. [Google Scholar]
- Price JR, Mitchell E, Tidy E, Hunot V. Cognitive behavior therapy for chronic fatigue syndrome in adults. Cochrane Database of Systematic Reviews. 2008:3. doi: 10.1002/14651858.CD001027.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins JB, Bleijenberg G, Bazelmans E, Elving LD, de Boo TM, Severens JL, van der Meer JWM. Cognitive behavior therapy for chronic fatigue syndrome: A multicentre randomized controlled trial. The Lancet. 2001;357:841–847. doi: 10.1016/S0140-6736(00)04198-2. [DOI] [PubMed] [Google Scholar]
- Redinbaugh EM, Creola D, Arnold J, Baum A. Behavioral medicine approaches to assessing and treating cancer pain. The Journal of Psychological Practice. 2004;10(1):45–59. [Google Scholar]
- Sayger TV, Bowersox MP, Steinberg EB. Family therapy and the treatment of chronic illness in a multidisciplinary world. The Family Journal. 1996;4(1):12–21. [Google Scholar]
- Taylor RR, Jason LA, Torres A. Fatigue rating scales: An empirical comparison. Psychological Medicine. 2000;30:849–856. doi: 10.1017/s0033291799002500. [DOI] [PubMed] [Google Scholar]
- Twisk FNM, Maes M. A review on cognitive behavioral therapy (CBT) and graded exercise therapy (GET) in myalgic encephalomyelitis (ME)/chronic fatigue syndrome (CFS): CBT/GET is not only ineffective and not evidence-based, but also potentially harmful for many participants with ME/CFS. Neuroendocrinology Letters. 2009;30:284–299. [PubMed] [Google Scholar]
- Van Houdenhove B, Luyten P. Customizing treatment of chronic fatigue syndrome and fibromyalgia: The role of perpetuating factors. Psychosomatics. 2008;49:470–477. doi: 10.1176/appi.psy.49.6.470. [DOI] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-item shortform health survey. Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Whiting P, Bagnall AM, Snowden AJ, Cornell JE, Mulrow CD, Ramirez G. Interventions for the treatment and management of chronic fatigue syndrome. A systematic review. Journal of the American Medical Association. 2001;286:1360–1368. doi: 10.1001/jama.286.11.1360. [DOI] [PubMed] [Google Scholar]