Abstract
The present study examined the potential mediating roles of executive and reactive disinhibition in predicting conduct problems, ADHD symptoms, and substance use among adolescents with and without a family history of substance use disorders. Using data from 247 high-risk adolescents, parents, and grandparents, structural equation modeling indicated that reactive disinhibition, as measured by sensation seeking, mediated the effect of familial drug use disorders on all facets of the adolescent externalizing spectrum. Executive disinhibition, as measured by response disinhibition, spatial short term memory, and “trait” impulsivity, was associated with ADHD symptoms. Moreover, although executive functioning weakness were unrelated to familial substance use disorders, adolescents with familial alcohol use disorders were at risk for “trait” impulsivity marked by a lack of planning. These results illustrate the importance of “unpacking” the broad temperament style of disinhibition and of studying the processes that underlie the commonality among facets of the externalizing spectrum and processes that that predict specific externalizing outcomes.
Introduction
It is well-documented that children of substance-abusing parents are at increased risk for a number of negative outcomes including internalizing and externalizing symptomatology (e.g., Barnard & McKeganey, 2004; Chassin, Pitts, DeLucia, & Todd, 1999; Johnson & Leff, 1999; Nunes, Weissman, Goldstein, McAvay, Beckford, Seracini, Verdeli, & Wickramaratne, 2000; Sher, 1991) and alcohol and drug use disorders (Chassin et al., 1999; Merikangas, Stolar, Stevens, Goulet, Preisig, Fenton et al., 1998; Rounsaville, Kosten, Weissman, Prusoff, Pauls, Anton et al., 1991; Weinberg, Rahdert, Colliver & Glantz, 1998; Zhou, King, & Chassin, 2006). In the case of parental alcoholism, one theoretical mechanism proposed to underlie risk for externalizing disorders among offspring is the “deviance proneness” pathway (Sher, 1991). This empirically supported mechanism (Chartier, Hesselbrock, & Hesselbrock, 2009; Chassin, Pillow, Curran, Molina & Barrera, 1993; Schuckit, Smith, Danko, Trim, Bucholz, Edenberg et al., 2009) proposes that children of alcoholics (COAs) show disinhibited temperament (elevated sensation seeking, impulsivity, lack of constraint, and cognitive dysfunction), which is hypothesized to interact with poor parenting to produce poor academic achievement and affiliation with deviant and substance using peers, who are the proximal influence on offspring substance use.
Recent research suggests that disinhibition confers a broad and general risk for externalizing behaviors among offspring of substance abusers (King, Keyes, Malone, Elkins, Legrand, Iacono, & McGue, 2009). However, less is known about potential unique predictors of different indicators of the externalizing “spectrum” (Krueger, Hicks, Patrick, Carlson, Iacono, & McGue, 2002), and whether different forms of disinhibition predict different externalizing outcomes for children of substance abusers. The overall aim of the present study was to test the potential mediating roles of two forms of disinhibition, namely executive and reactive disinhibition in predicting conduct problems, attention deficit hyperactivity disorder (ADHD) symptomatology, and substance use among children with and without a family history of substance use disorders.
Familial Substance Use Disorders and Offspring Disinhibition
Within the large literature on disinhibition, multiple terms such as impulsivity, behavioral disinhibition and behavioral undercontrol have been used loosely and often interchangeably (see Dick, Smith Olausson, Mitchell, Leeman, O’Malley, & Sher, 2010 for review). Although these constructs are related, they are not identical. Moreover, both human and animal data demonstrate that these broad constructs (i.e., disinhibition, impulsivity, and behavioral undercontrol) are not unitary (see Dick, Smith, Olausson, Mitchell, Leeman, O’Malley, & Sher, 2010 for review). For example, Whiteside and Lynam (2001) found a multifaceted model of propensity to rash action, which included lack of premeditation (i.e., acting without forethought), sensation seeking (i.e., seeking out novel or thrilling experiences), lack of perseverance (i.e., difficulty maintaining sustained attention in the context of distraction) and negative urgency (rash responding in the context of negative affect). Further research (Cyders & Smith, 2007) suggested the addition of positive urgency (rash responding in the context of positive affect).
Other theoretical models have suggested that disinhibition depends on two processes, namely executive disinhibition and reactive disinhibition (Blaskey, Harris, & Nigg, 2008; Nigg, 2000). Executive disinhibition refers to failures of “top-down” effortful cognitive processes to suppress, or intentionally control, a response in order to achieve a higher goal (Nigg, 2000; 2003). Executive disinhibition likely involves lack of both premeditation and perseverance in Whiteside and Lynam’s (2001) model. In contrast, reactive disinhibition (Nigg, 2003; Nigg, 2006), refers to “bottom-up” processes with dysregulations in behavior in the context of novel or affect-laden situations. Both positive and negative urgency as well as sensation seeking might reflect reactive disinhibition. Similar distinctions are represented in models of “hot” and “cold” cognition (Kerr & Zelazo, 2004; Potenza & De Wit, 2010; Rubia, in press), models of “motor impulsivity” and “choice impulsivity” (Urcelay & Dalley, in press), and in Steinberg’s (2010) dual systems model of adolescent risk taking in which impulsivity (an indicator of executive disinhibition) and sensation seeking (an indicator of reactive disinhibition) follow different developmental courses.
Although it is well-documented that children of substance use disordered parents are at-risk for disinhibition (e.g., Edwards, Leonard & Das Eiden, 2001; Sher, Walitzer, Wood,& Brent, 1991; King et al., 2009; Tarter, 1988), it is unclear whether familial substance use disorder confers risk for both executive and reactive disinhibition. Some previous studies have shown that familial substance use disorder is associated with executive disinhibition in the form of poor executive functioning among offspring (Aytaclar, Tarter, Kirisci, & Lu, 1999; Giancola, Moss, Martin, Kirisci, & Tarter, 1996; Harden & Pihl, 1995; Nigg, Glass, Wong, Poon, Jester, Fitzgerald, Puttler, Adams, & Zucker, 2004; Peterson, Finn, & Pihl, 1992). However, findings are not consistent. For example, Corral and colleagues found familial alcoholism effects on working memory but not on Wisconsin Card Sort performance (Corral, Holguín, & Cadaveira, 1999), and found the opposite pattern in a follow-up assessment (Corral, Holguín, & Cadaveira, 2003). Nigg and colleagues (2004) found that boys from families with co-morbid parental alcoholism and antisocial personality disorder did not differ from controls in their executive functioning. Rather, boys with alcoholic but non-antisocial parents had the poorest executive functioning. Moreover, numerous studies have failed to find a relation between executive functioning deficits and familial substance use disorders (Bates & Pandina, 1992; Bauer & Hesselbrock, 1999; Schafer et al., 1991; Schuckit, Butters, Lyn, & Irwin, 1987; Spadoni, Norman, Schweinsburg, & Tapert, 2008; Stevens, Kaplan, & Hesselbrock, 2003; Wiers, Gunning, & Sergeant, 1998; Wilson & Nagoshi, 1988). There are several possible explanations for these inconsistencies including the widely varying measurement of executive functioning (Nigg et al., 2004), inconsistencies in testing the role of parental co-morbidities, and small sample sizes.
Disinhibition and the Externalizing Spectrum
Executive and reactive disinhibition have both been related to externalizing outcomes such as ADHD, conduct problems, and substance use, or what has been called the externalizing spectrum (Krueger, Hicks, Patrick, Carlson, Iacono, & McGue, 2002). These externalizing disorders are frequently co-morbid and there is evidence that the common externalizing factor is highly heritable (Hicks, Krueger, Iacono, McGue, & Patrick, 2004; Kruger et al., 2002; Young, Stallings, Corley, Krauter, & Hewitt, 2000). However, in spite of the high co-morbidity among facets of the externalizing spectrum, there is also evidence for distinction among facets. For instance, Farmer and colleagues (2009) found support for a two-factor model of externalizing behavior in which one factor was characterized by ADHD and ODD symptoms such as inattention, intrusion, impulsivity, and hyperactivity and the second factor was characterized by a general rule-breaking tendency and included symptoms of conduct disorder, antisocial behavior, and substance abuse. Moreover, studies have shown that after controlling for conduct problems, the relation between ADHD and substance use disappears (see Flory & Lynam, 2003 for a review). Taken together these findings suggest that there may be a stronger common diathesis for conduct problems and substance use disorders than for ADHD and substance use disorders.
Moreover, Nigg (2003) proposed that ADHD results from a primary deficit in “top-down” executive inhibition and a secondary weaker deficit in reactive “bottom up” processes, whereas conduct disorder results from a primary reactive disinhibitory process and a secondary weaker executive disinhibition process. Multiple pathway models of ADHD similarly implicate both executive and reactive disinhibition (i.e., Sonuga-Barke, 2003; 2005; Urcelay & Dalley, in press), although the relative importance of reactive disinhibition is still unclear (Blaskey et al., 2008; Wahlstedt, Thorell, & Bohlin, 2008). With regards to conduct problems and substance use disorders, there is empirical support for a reactive disinhibitory pathway (Finn, Mazas, Justus, & Steinmetz, 2002; Herba, Tranah, Rubia & Yule, 2006; Sher, Bartholow & Wood, 2000; Urcelay & Dalley, in press; van Goozen, Cohen-Keetenis, Snoek, Matthys, Swaab-Barneveld, & van Engeland, 2004). However, evidence for an executive disinhibition pathway to conduct problems and substance abuse is less consistent. Specifically, a number of researchers have failed to find a link between executive functioning deficits and conduct problems and substance use (i.e., Giancola & Parker, 2001; Herba, Tranah, Rubia, & Yule, 2006; Oosterlaan, Scheres, & Sergeant, 2005; Nigg, Wong, Martel, Jester, Puttler, Glass, et al., 2006; van Goozen et al., 2004; Wiers et al., 1998). Nigg and colleagues (2006) found that poor performance on the stop task, a measure of executive disinhibition, predicted substance use among adolescents but performance on set-shifting, working memory, and additional neuro-cognitive measures did not.
In addition to theories of direct effects of executive and reactive disinhibition on substance use, Finn (2002) proposed the cognitive-motivational theory (CMT), an interactive model in which working memory capacity moderates the effect of novelty seeking to influence decision making and alcohol use. Specifically, high novelty seeking individuals find rewards to be more salient than punishments and, when they also have low working memory capacity, they are at risk for disinhibition because of difficulty in keeping less salient punishment cues in mind (Finn, Mazas, Justus, & Steinmetz, 2002). This disinhibition then increases risk for alcohol use and problems (Chassin, Pitts, DeLucia, & Todd, 1999). Therefore, the CMT suggests a need to consider the interaction between executive and reactive disinhibition rather than just their individual contributions. Dual process models propose similar interactions between controlled and automatic regulatory processes (Hofman et al., 2009; Grenard et al., 2008).
Taken together, these studies provide consistent support for an executive disinhibitory pathway to ADHD symptomatology and for a reactive disinhibitory pathway to conduct problems and substance use/abuse. In addition, reactive disinhibition may represent a weaker secondary path to ADHD symptoms and executive disinhibition may represent a weaker secondary path to conduct problems and substance use although findings remain unclear. The current study tested whether indicators of executive and reactive disinhibition predicted distinct facets of the externalizing spectrum among adolescents, namely ADHD symptoms, conduct problems, and substance use. Moreover, we tested whether these indicators mediated the effects of familial alcohol and drug disorders on externalizing outcomes among adolescent offspring. Finally, we tested interactions between executive and reactive disinhibition on externalizing outcomes.
Specificity of the Effects of Familial Alcohol Use Disorder
Previous research clearly indicates that individuals with familial alcohol use disorder (AUD) are at heightened risk for a disinhibited temperament (Sher, Grekin, & Williams, 2005), and that familial alcoholism risk for disinhibition and externalizing problems broadly shows significant heritability (Elkins, McGue, Malone, & Iacono, 2004; Hicks, Krueger, Iacono, McGue, & Patrick, 2004; King et al., 2009). However, studies of familial alcoholism risk often fail to consider commonly co-occurring familial psychopathology, particularly antisociality and drug use disorders (DUD). Because there are differing personality correlates of alcohol disorders witih and without co-occurring antisocial and drug disorders (McGue, Slutske, & Iacono, 1999) as well as differing parenting and family environments (Jacob & Johnson, 1997; Ohannessian, Hesselbrock, Kramer, Kuperman, Bucholz, Schuckit, & Nurnberger, 2004; Wong, Zucker, Puttler, & Fitzgerald, 1999), the mechanisms that mediate the effects of familial AUD versus drug use disorder (DUD) may differ. Indeed, previous studies suggest that parent antisociality and drug disorders exert unique negative effects, over and above co-occurring parent alcohol disorder on child externalizing symptomatology, substance use, and the parent-child relationship (Chassin, Rogosch, & Barrera, 1991; Loukas, Fitzgerald, Zucker, von Eye, 2001). Interestingly, Elkins and colleagues (2004) demonstrated that parental drug disorders had a unique effect on offspring constraint, above and beyond parental alcohol disorders, suggesting that an offspring temperamental style marked by low constraint may be most accurately attributable to familial drug use disorder, that often co-occurs with AUDs, rather than to AUDs in absence of DUDs. Therefore, the present study tested whether familial alcohol and drug use disorder and parental antisocial behavior exerted unique effects on offspring reactive and executive disinhibition and on externalizing outcomes.
In summary, the primary aim of the present study was to test whether executive and reactive disinhibition differentially mediated the influence of familial substance use disorders on three adolescent outcomes from the externalizing spectrum: ADHD symptoms, conduct problems, and substance use while also examining the effects of familial alcoholism in the context of co-occurring DUDs and antisociality
Method
Participants
Participants were drawn from Wave 6 of a larger, ongoing longitudinal study of familial alcoholism across three generations (e.g. Chassin et al., 1991). There were three annual waves of data collection and three additional follow-ups separated by five years. At Wave 1 (1988), the total sample consisted of 454 adolescents (generation 2; “G2s”) and their parents (generation 1; “G1s”). 246 of these adolescents had at least one biological alcoholic parent who was also a custodial parent (COAs), and the remaining 208 adolescents were demographically matched controls without an alcoholic parent (matched on adolescent age, family composition, ethnicity, and socioeconomic status). Beginning at Wave 4 (18–25 years of age), G2 biological siblings within the same age range of the original G2s were also interviewed. At Wave 6, we conducted interviews with their children (generation 3; “G3s”). Sample retention has averaged more than 90% since the advent of the study.
The current analyses used Wave 6 data from a subsample of 247 G3 children who were at least 11.5 years old and had complete data on the three measures of executive disinhibition. We selected those who were at least 11.5 years of age to be appropriate for the substance use outcome. Of the 289 excluded G3s, 206 were excluded because they were younger than 11.5 years old, and 83 were excluded because they were not interviewed in-person and were thus missing data on the cognitive tasks measuring executive disinhibition. Of the G3s included in our analyses, approximately 50.0% were male, 50.0% were non-Hispanic Caucasian, 36.6% were Hispanic, and 13.4% identified themselves as American Indian or some other race/ethnicity. 50.8% of adolescents had at least one biological parent with a lifetime alcohol disorder and 41.0% had at least one biological parent with a lifetime drug disorder (as defined by DSM-IV criteria for abuse or dependence). Of the 41.0% of adolescents with at least one biological drug disordered parent, 79.0% also had at least one biological alcohol disordered parent.
Analyses (chi-square and t-tests) comparing the included and excluded G3 participants on demographic and study variables indicated that included participants were significantly older (by design), scored lower on the IQ measure, were more likely to have used substances, and reported more symptoms of ADHD, higher levels of impulsivity and conduct problems. Moreover, included participants demonstrated stronger performance on all three cognitive executive disinhibition measures. There were no significant differences between included and excluded participants in gender, family structure, parental alcohol and drug disorder status, family history density of alcohol and drug disorders, or sensation seeking.
Recruitment
The original recruitment is described in detail elsewhere (Chassin, Barrera, Bech, and Kossak-Fuller, 1992). COA families were originally recruited using court records, health maintenance organization questionnaires, and community telephone screening. Selection criteria were a child between the ages of 10.5 and 15.5 years, Arizona residence, Hispanic or non-Hispanic Caucasian ethnicity, English-speaking, and no cognitive limitations that would preclude interview. Direct interview was used to confirm that a biological G1 parent met Diagnostic and Statistical Manual of Mental Disorders—Third Edition (DSM-III; American Psychiatric Association, 1980) criteria for lifetime alcohol abuse or dependence. The resulting alcoholic sample had rates of other psychopathology similar to rates reported for a community-dwelling alcoholic sample (Helzer & Pryzbeck, 1988). However, those who refused participation were more likely to be Hispanic, suggesting some caution in generalization. Reverse directories were used to locate non-alcoholic families in the same neighborhood. Controls were screened and recruited via telephone interviews to match alcoholic families in ethnicity, family structure, age (within 1 year), and socioeconomic status (using the property value code from the reverse directory). Interview data confirmed that neither biological parent met DSM-III criteria (or Family History Research Diagnostic Criteria [FH-RDC]; Endicott, Andreason, & Spitzer, 1975) for lifetime alcohol abuse or dependence.
Procedure
At all waves, computer-assisted interviews were conducted either at the family’s residence or at the Arizona State University campus. Parents provided informed consent and adolescents provided assent. To encourage self-disclosure, family members were interviewed simultaneously in separate rooms and a Department of Health and Human Services Certificate of Confidentiality was used to emphasize confidentiality. To maximize privacy, participants could enter their responses on the keyboard rather than verbally.
Measures
Family structure
G3s were categorized as living either in a two-parent home (regardless of the biological relation of the child to the parent, 74.8%) or any other living situation.
G3 adolescent intelligence
G3 adolescents completed the Kaufman Brief Intelligence Test (K-BIT, Kaufman & Kaufman, 1990). The K-BIT score was a composite of the standard scores of two subtests: verbal intelligence, which included expressive vocabulary and word definitions, and nonverbal intelligence, which included a section of Matrices. The mean IQ was 102.52 (SD =11.14).
G3 adolescent family history density of alcohol and drug use disorder
Family history density (FHD) scores were calculated for each G3 adolescent participant based upon the lifetime history of their biological parents (G2s) and grandparents (G1s) using all available direct interview data from the Computerized Diagnostic Interview Schedule (C-DIS; Robins, Cottler, Bucholz, Compton, North, & Rourke, 2000) and family member report using Family History-Research Diagnostic Criteria (FH-RDC; Endicott, Andreason, & Spitzer, 1975). Density scores (separately for alcohol and drug disorders) were calculated using the methods of Stoltenberg and colleagues (1998) and Zucker, Ellis, and Fitzgerald (1994). Parent lifetime diagnoses were weighted by 0.5 and the lifetime disorder variables for grandparents were weighted by 0.25. Each nonalcoholic relative was given a score of 0. The appropriate weighted lifetime disorder variables were summed to create a specific FHD score which ranges in value from 0 to 2. The mean density score for G3 familial alcoholism was .63 (SD = .49) and .36 (SD = .42), for G3 familial drug disorder density.
G2 parent antisociality
Parents (i.e., G2s) antisocial behavior was assessed with the computerized Diagnostic Interview Schedule (C-DIS; Robins et al., 2000). Because this measure did not assess conduct problems before the age of 15, parent antisociality was calculated using a symptom count of endorsed behaviors since age 15. We considered parents who endorsed 5 or more symptoms to show clinically elevated levels of antisociality (11.8%).1
G3 adolescent reactive disinhibition: Sensation seeking
Consistent with Nigg’s (2000) conceptualization of reactive disinhibition as including the propensity to seek out novel experiences, we used sensation seeking as a measure of reactive disinhibition. Because the outcome measures were adolescent-reported, to minimize reporter effects, we used parent report of six items from Zuckerman’s 1979 scale (Zuckerman, 1979). Items included “likes being where there is something going on all the time,” “would do almost anything on a dare,” and “likes to do things on the spur of the moment” (Cronbach alphas of .78 and .87). To minimize missing data, we used the average of mother and father report or either reporter if only one was interviewed (correlation between mother and father reports r=.41, p<.001). We tested our hypothesized one-factor structure using confirmatory factor analysis. Results confirmed the model but indicated that one item did not significantly load (“likes work that has lots of excitement”) and this item was dropped. The remaining five items were used as indicators of the latent sensation seeking construct. Factor loadings ranged from .65 to .77.
G3 adolescent executive disinhibition: working memory, spatial short term memory, response inhibition
Working memory
Working memory was assessed with the Letter-Number Sequencing (LNS) subtest from the Weschler Intelligence Scale for Children, Fourth Edition (WISC-IV; Wechsler, 2003). Participants listened to a combination of numbers and letters and then recalled the numbers first in ascending order followed by the letters in alphabetical order. The mean raw score was 18.73 (SD=2.99).2
Spatial short term memory
Spatial short term memory was assessed with the Matrix Span Task (MST; Kane, Hambrick, Tuholski, Wilhelm, Payne, & Engle, 2004). MST is a computerized assessment of attention and memory, specifically in the spatial domain. Participants were briefly presented with 4 × 4 matrices in which one cell was highlighted. They attempted to hold in memory the spatial location of the highlighted cell for later recall. Participants were then shown a series of screens each displaying one matrix (series sizes range from 2–5), and were cued to recall and attempt to mark which cells had been filled in that set on a response sheet. There were a total of 20 trials, divided equally into set sizes of 2, 3, 4, and 5 matrices. The test trials were preceded by 3 practices trials with a set size of 2. We followed Conway and colleagues’ (2005) guidelines for scoring such that partial credit was awarded if the participant correctly selected some elements in the trial, but incorrectly selected other elements in trial. The mean score was 0.60 (SD=.15).
Response inhibition
Response inhibition was assessed with the Immediate Memory Task (IMT; Dougherty, Marsh, & Mathias, 2002) as a measure of response inhibition. In this computerized task a 5 digit number was presented every second and the participant was asked to press a button only if the current number exactly matched the prior number. On a third of the trials the current number was identical to the prior number (target trials); on a third of the trials the current number was different from the prior number on all 5 digits (foil trials); and on a third of the trials the current number was different from the prior number by only one digit (catch trials or commission errors). Commission errors have been interpreted as a measure of impulsive responding (Dougherty et al., 2002; Dougherty, Mathias, Marsh, & Jagar, 2005) and were used in the current analyses. The mean score was 1.46 (SD=.25).
G3 adolescent impulsivity
A measure of G3 adolescent impulsivity was created from parent-report of items adapted from the Junior Eysenck Impulsiveness Questionnaire (J-EIQ; Eysenck, Pearson, Easting, Allsopp, 1985). Exploratory factor analysis was conducted on the original 23 items to extract factors of impulsivity to identify a factor tapping executive disinhibition. The following 6 items were extracted because they mapped most closely onto the construct of the lack of premeditation: generally does and says things without stopping to think; usually thinks carefully before doing anything; mostly speaks before thinking things out; often buys things on impulse; thinks that planning takes the fun out of things; sometimes puts down the first answer that comes into his/her head during a test and forgets to check it later. Confirmatory factor analysis supported this as a single factor: (χ2(9) = 20.91, p = .01, CFI = .98, RMSEA = .06, SRMR = .03) and all factor loadings were significant at p<.001. Standardized factor loadings ranged from .58 to .82.
G3 outcomes: conduct problems, ADHD symptoms, and substance use
Because parents are not good reporters of adolescent substance use and to avoid introducing reporter effects, we used adolescent self report of all externalizing outcomes.
Conduct problems
Adolescents self-reported their conduct problems using 28 items from the rule-breaking and aggression subscales of the Youth Self Report externalizing syndrome scale (YSR; Achenbach & Rescorla, 2001). Response options ranged from 0 “Not True” to 2 “Very True.” “Loud” was dropped because of overlap with the ADHD scale and three substance use items were dropped because they overlapped with the substance use outcome (e.g., drinking alcohol without parents’ approval). Cronbach alpha was .89. The mean score was .28 (SD=.25; range 0–1.29)
ADHD symptoms
Adolescents self-reported on 6 items from the DSM-oriented Attention-Deficit Hyperactivity Problems scale of the Youth Self Report (YSR; Achenbach & Rescorla, 2001). Sample items are: fails to finish, can’t concentrate, and talks too much. Response options ranged from 0 “Not True” to 2 “Very True.” “Loud” was dropped because of overlap with the conduct problems outcome. Cronbach alpha was .77. The mean score was .68 (SD = .51; range 0–2).
Substance use
Adolescents indicated whether they had ever used alcohol, cigarettes, or marijuana. Adolescents were divided into those who had (29.3%) or had not (70.7%) used substances.
Results
Zero-order correlations among study variables are in Table 1. None of the executive disinhibition measures were significantly correlated with family history density of drug disorder or alcohol disorder (with the exception of Letter Number Sequencing). In contrast, high levels of adolescent sensation seeking were related to denser family histories of drug and alcohol disorder (see Table 1).
Table 1.
Zero-order correlations among study variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | -- | ||||||||||||||
| 2. Adolescent age | .01 | -- | |||||||||||||
| 3. Family structure | .13* | −.07 | -- | ||||||||||||
| 4. Intelligence | −.13* | −.11 | .10 | -- | |||||||||||
| 5. FHD-alcohol | .03 | .04 | −.15* | −.14* | -- | ||||||||||
| 6. FHD-drug | −.01 | −.06 | −.17** | −.02 | .47*** | -- | |||||||||
| 7. Parent antisociality | −.05 | .02 | .05 | −.05 | .20** | .23*** | -- | ||||||||
| 8. Sensation seeking | .06 | .12* | .03 | −.08 | .16* | .18** | .07 | -- | |||||||
| 9. MST | −.23*** | −.19** | −.10 | −.44*** | .11 | .04 | .04 | .05 | -- | ||||||
| 10. LNS | .12 | −.19** | −.04 | −.45*** | .14* | .05 | .04 | .07 | .38*** | -- | |||||
| 11. IMT | .22*** | −.25** | .09 | −.15* | .07 | −.05 | −.05 | .10 | .12* | .21** | -- | ||||
| 12. Impulsivity | .15* | .04 | −.04 | −.21** | .24*** | .20** | .02 | .55*** | .11 | .18** | .19** | -- | |||
| 13. ADHD symptoms | −.05 | .11 | −.05 | −.09 | .09 | .07 | .06 | .27*** | .15* | .10 | .13* | .34*** | -- | ||
| 14. Substance Use | −.03 | .40*** | −.21** | −.08 | .20** | .17** | .12 | .26*** | .04 | −.08 | −.13* | .19** | .28*** | -- | |
| 15. Conduct problems | .04 | .27*** | −.11 | −.08 | .17** | .18** | .08 | .31*** | .03 | .04 | .09 | .33*** | .66*** | .43*** | -- |
Note:
p<.05,
p<.01,
p<.001. MST=Matrix Span Task; LNS=Letter Number Sequencing; IMT=Immediate Memory Task. Gender was coded 1=male, 0=female; family structure was coded 1=two-parent home, 0=single parent home or other; parent antisociality was coded 0= no diagnosis, 1= diagnosed; substance use was coded 0=non-users, 1=users; higher scores on FHD-alcohol, FHD-drug, ADHD symptoms, sensation seeking and conduct problems indicate greater levels of the construct; higher scores on MST, LNS, and IMT indicate higher levels of executive disinhibition. The mean of the 5 sensation seeking items was used to include sensation seeking in this table. The 5 sensation seeking items were used as indicators of the latent variable in the final model.
As expected, high family history density of AUD was significantly correlated with high family history density of drug disorder. Although family history density of alcoholism (AUD) was significantly correlated with parent antisociality, this correlation was reduced to non-significance when family history density of DUD was controlled. In contrast, family history density of DUD was significantly correlated with parent antisociality, and remained significantly correlated when family history density of AUD was controlled. These results indicate significant overlap in parent antisociality and family history of DUD, and suggest that the relation between parent antisociality and family history of AUD was accounted for family history of DUD.
With regards to the outcomes, familial alcohol and drug use disorders were significantly related to conduct problems and substance use, but not to ADHD symptoms. Adolescent sensation seeking was related to all of the outcomes. ADHD symptoms were related to poor performance on MST and IMT but not LNS. Conduct problems and substance use were not significantly correlated with poor performance on measures of executive disinhibition except for a surprising association between substance use and stronger performance on the IMT. However, once age was controlled, the relation was no longer significant (pr= −.03; p = n.s).
Model Specification
We tested whether parent-reported sensation-seeking (latent variable) and executive disinhibition (as measured by working memory, spatial short term memory, and response inhibition) mediated the effects of family history densities of alcohol and drug disorders and parent antisocial behavior on three adolescent-reported outcome variables: substance use (dichotomous), ADHD symptoms, and conduct problems. Family history of AUD, DUD and parent antisocial behavior were entered as exogenous predictors, with paths estimated to the 4 mediator variables (sensation seeking and 3 executive disinhibition measures) and all three outcome variables. However because there was no significant unique effects of parent antisociality on the two mediators and three outcome variables, it was trimmed from the final model.
Adolescent age, gender, IQ, and family structure were initially entered as exogenous covariates, with paths estimated to the mediator and outcome variables, and significant paths from covariates to mediators and outcomes were retained in the final model. Preliminary analyses tested all covariate by predictor interactions in predicting mediators and outcomes and also tested mediators by covariate/predictors interactions in predicting outcomes. Because all preliminary interactions were non-significant they were trimmed from the final model. Therefore, in terms of covariates, in our final model, paths were estimated from family structure to substance use, from adolescent IQ to IMT and LNS, and from adolescent age to IMT, LNS, MST, conduct problems, and substance use. Because gender had no significant unique effects and all interactions between gender and predictors/mediators were non-significant, it was trimmed from the final model. Correlations among exogenous variables were modeled and residual variances among the mediators and among the outcome variables were allowed to covary.
Models were tested using MPlus version 6.0 (Muthén & Muthén, 1998–2010). Because the final model included a binary dependent variable (substance use), the weighted least squares estimator with mean and variance adjustments (WLSMV) was used, which computes OLS parameter estimates for continuous outcomes and probit parameter estimates for categorical outcomes. Missing data on endogenous variables were estimated as a function of the observed exogenous variables under the missingness at random assumption (Schafer & Graham, 2002). Because participants were nested within families, standard errors were adjusted for non-independence of observations using the complex function in MPlus.
Model fit was estimated with the robust WLSMV chi-square statistic, comparative fit index (CFI), root mean square error of approximation (RMSEA), and the weighted root mean square residual (WRMR). The robust WLSMV chi-square statistic was developed and shown to have good statistical properties in testing model fit with relatively small sample sizes (N ≈ 200) and categorical outcomes (Nussbeck, Eid, & Lischetzke, 2006). CFI values greater than .95, RMSEA values less than .06, WRMR values less than .90, and a non-significant chi-square statistic were considered to indicate good model fit (Hu & Bentler, 1999; Yu & Muthén, 2002).
Final Model
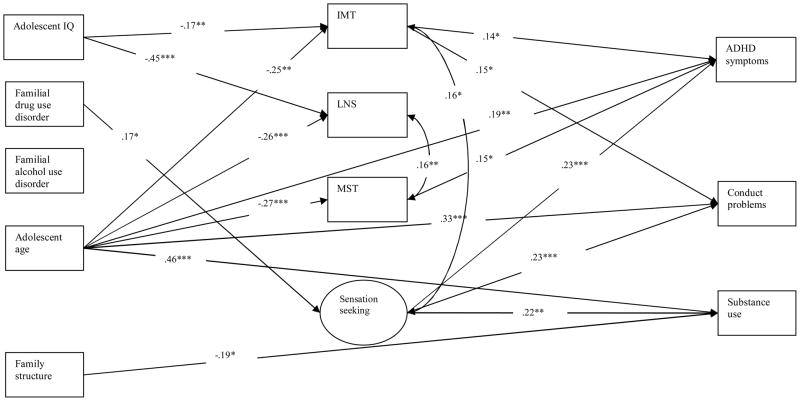
The final model (see Figure 1) showed good fit to the data (χ2(61) = 70.25, p = .20, CFI = .98, RMSEA = .02, WRMR = .62). For ease of presentation, Figure 1 does not show non-significant paths. However, all significant and non-significant standardized path coefficients are presented in Table 2.
Figure 1.
Results of final structural equation model-task model
Notes: *p<.05, **p<.01, ***p<.001; IMT=Immediate Memory Task; LNS=Letter Number Sequencing; MST=Matrix Span Task; Family structure is coded 1=two-parent home and 0=single parent home or other living situation; IMT and MST was coded such that high scores indicate poor performance. Sensation seeking was coded such that high scores indicate high levels of sensation seeking; High scores on ADHD symptoms and conduct problems indicate more endorsed symptoms.
Table 2.
Standardized path coefficients for final structural equation model
| Predictors | Mediators | |||
|---|---|---|---|---|
| Sensation seeking | MST | LNS | IMT | |
| FHD-alc | .11 | .07 | .09 | .12 |
| FHD-drug | .17* | −.02 | −.02 | −.12 |
| Adolescent IQ | -- | -- | −.45*** | −.17** |
| Family structure | -- | -- | -- | -- |
| Adolescent age | -- | −.27*** | −.27*** | −.25*** |
| Predictors/Mediators | Outcomes | ||
|---|---|---|---|
| ADHD symptoms | Conduct problems | Substance use | |
| FHD-alc | −.01 | .04 | .13 |
| FHD-drug | .03 | .12 | .12 |
| Adolescent IQ | -- | -- | -- |
| Family structure | -- | -- | −.19* |
| Adolescent age | .18* | .33*** | .46*** |
| Sensation seeking | .23** | .23** | .22** |
| MST | .15* | .04 | .12 |
| LNS | .02 | .01 | −.11 |
| IMT | .14* | .15* | −.03 |
Note: The standardized path coefficient is reported first, followed by the standard error in parentheses. MST=Matrix Span Task; LNS=Letter Number Sequencing; IMT=Immediate Memory Task;
p<.05,
p<.01,
p<.001
Results indicated that older adolescents exhibited lower levels of executive disinhibition on all three measures (i.e. IMT, LNS, MST), reported more ADHD symptoms and conduct problems and were also more likely to have used substances. Adolescents with higher IQs showed less executive disinhibition on LNS and IMT. Adolescents from single-parent families were more likely to have used substances than were adolescents from two-parent homes.
Adolescents with higher density of familial drug use disorders showed higher levels of adolescent sensation seeking. Familial drug disorders were unrelated to executive disinhibition and did not have any unique effects on outcomes above and beyond the mediators. Density of familial alcoholism did not uniquely predict sensation seeking or executive disinhibition mediators, nor did it have a unique effect on the outcomes.
An examination of the effects of the mediators on the three outcomes indicated that higher levels of sensation seeking significantly predicted higher levels of ADHD symptoms, higher levels of conduct problems, and higher likelihood of lifetime substance use. Weaker performance on MST and IMT, but not LNS, predicted ADHD symptoms. Executive disinhibition task performance did not uniquely predict conduct problems or substance use, with the exception that poorer IMT performance predicted more conduct problems.
Mediation Analyses
To test the indirect effect of family history density of drug disorders on the three outcome variables via sensation-seeking, 95% asymmetric confidence limits were used (MacKinnon, Lockwood, & Williams, 2004). Confidence intervals that do not include the value zero indicate significant mediation. Results indicated that sensation seeking significantly mediated the effect of family history density of drug disorders on adolescent substance use (CI.95 = .008; .260), ADHD symptoms (CI.95 = .004; .105), and conduct problems (CI.95 = .002; .052).3
Moderation Analyses
To examine the interactive effect of executive disinhibition and sensation seeking in predicting adolescent externalizing outcomes, we specified three multiple group models testing sensation seeking as a mediator. Sensation seeking was converted to a manifest variable (i.e. mean score of five items). High and low levels of each of the three executive disinhibition tasks were used as grouping variables in three separate analyses. That is, we tested whether the effects of sensation seeking on the adolescent outcomes were the same across adolescents’ high and low scores on each of the tasks measuring executive disinhibition. We used a mean split to dichotomize adolescents as scoring either high or low on each of three tasks. For the LNS and MST tasks, there was no evidence of moderation. That is, there were no significant improvements in model fit when the paths from sensation seeking to the outcome variables were allowed to vary across high/low levels of the LNS or MST tasks, compared to models in which all paths were constrained to be equal across high/low levels of these tasks. In contrast, performance on the IMT showed evidence of moderation in that there was significant improvement in model fit when the paths from sensation seeking to the outcome variables were allowed to vary for low and high IMT scores (Δ χ2(2)= 15.07, p < .000). Sensation seeking significantly predicted higher levels of all externalizing outcomes for adolescents who performed poorly on the IMT, but not for adolescents who performed well on the IMT.4
Other Operationalizations of Executive Disinhibition
The use of three separate correlated measures of executive disinhibition may have underestimated the effects of executive disinhibition by testing unique effects of each one over the other rather than the effects of what they have in common. Accordingly, we tested a model in which the three executive disinhibition tasks were specified as indicators of a latent variable. The model showed fair fit to the data (χ2(72) = 129.37, p <.001, CFI = .86, RMSEA = .05, WRMR = .99). The pattern of results was the same as the final model presented above with the following differences: 1) the latent variable for executive disinhibition marginally significantly predicted ADHD symptoms (p=.08) and 2) the latent variable for executive disinhibition did not significantly predict CD symptoms.5
“Trait” Impulsivity Model
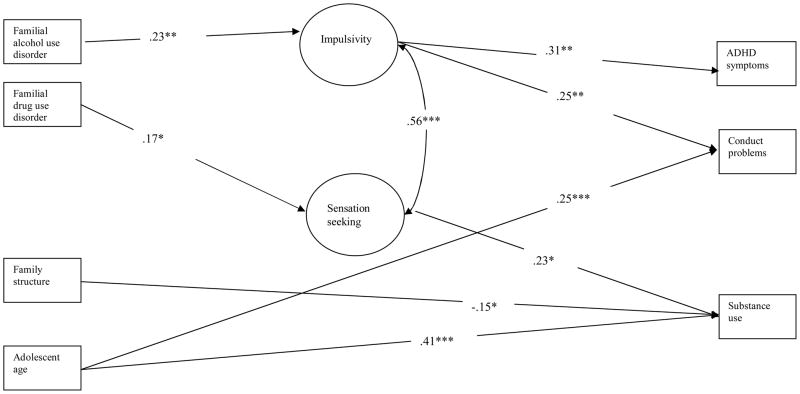
Another possible reason that sensation seeking showed significant effects on all outcomes whereas executive disinhibition did not predict substance use might be shared method variance. That is, both the externalizing outcomes and the sensation seeking mediator were measured by reports about behavior whereas executive disinhibition was measured by cognitive tasks. Although the use of different reporters (parent-reported sensation seeking and adolescent-reported substance use) reduces shared method variance, we tested an additional model using parent reports of adolescent impulsivity in place of the cognitive tasks to indicate executive disinhibition. Model specification was as described above with the following exceptions: 1) parent-reported impulsivity (latent variable) replaced the executive disinhibition mediators in the previous model; 2) adolescent IQ was trimmed from this model because it did not uniquely predict the mediators or outcome variables; 3) the path from adolescent age to parent-reported impulsivity was non-significant and was therefore trimmed from this model. Finally, this model had a larger sample size (n=310) because participants who were not interviewed in person (and thus lacked data on the cognitive tasks) still had data on parent-reported impulsivity. This larger sample might also allow for detection of executive disinhibition effects that would be missed by the cognitive task models presented above.
This model (see Table 3 and Figure 2) also showed good fit to the data (χ2(113) = 144.74, p = .02, CFI = .96, RMSEA = .02, WRMR = .74). For ease of presentation, Figure 2 does not show non-significant paths. The main findings from the cognitive task model were replicated. That is, executive disinhibition (impulsivity) predicted ADHD symptomatology and conduct problems but not substance use and reactive disinhibition (sensation seeking) predicted substance use. There were some differences between this model and the cognitive task model: 1) familial alcohol use disorder uniquely predicted parent-reported impulsivity; 2) parent-reported sensation seeking no longer uniquely predicted ADHD symptoms and conduct problems.6
Table 3.
Standardized path coefficients for “trait” impulsivity model
| Predictors | Mediators | |
|---|---|---|
| Sensation seeking | Impulsivity | |
| FHD-alc | .12 | .23** |
| FHD-drug | .17* | .08 |
| Predictors/Mediators | Outcomes | ||
|---|---|---|---|
| ADHD symptoms | Conduct problems | Substance use | |
| FHD-alc | −.03 | .02 | .17† |
| FHD-drug | .02 | .10 | .13 |
| Family structure | -- | -- | −.15* |
| Adolescent age | -- | .25** | .41*** |
| Sensation seeking | .05 | .10 | .23* |
| Impulsivity | .31** | .25** | .01 |
Note: The standardized path coefficient is reported first, followed by the standard error in parentheses.
p<.06; p<.05,
p<.01,
p<.001
Figure 2.
Results of “trait” impulsivity model
Notes: *p<.05, **p<.01, ***p<.001; Family structure is coded 1=two-parent home and 0=single parent home or other living situation; Impulsivity was coded such that high scores indicate high levels of impulsivity; Sensation seeking was coded such that high scores indicate high levels of sensation seeking; High scores on ADHD symptoms and conduct problems indicate more endorsed symptoms.
Mediation Analyses
To test the indirect effect of family history density of drug and alcohol disorders on the externalizing outcome variables via sensation-seeking and impulsivity, 95% asymmetric confidence limits were again used (MacKinnon et al., 2004). Confidence intervals that do not include the value zero indicate significant mediation. Consistent with the previous model, results indicated that sensation-seeking significantly mediated the effect of family history density of drug disorders on adolescent substance use (CI.95 = .004; .275). Interestingly, parent-reported impulsivity significantly mediated the effect of family history of alcohol use disorders on adolescent ADHD symptoms (CI.95 = .021; .137) and conduct problems (CI.95 = .008; .052).
Moderation Analyses
We also tested this trait model for a potential sensation seeking by executive disinhibition (i.e., parent-reported impulsivity) interaction. A multi-group model tested whether the effects of parent-reported sensation seeking (specified as a manifest variable) on the three adolescent externalizing outcomes varied across high and low levels of parent-reported impulsivity (mean split). There was not a significant improvement in model fit when the three paths from sensation seeking to the outcome variables were allowed to vary across high and low levels of impulsivity (Δ χ2(2)= 4.23, p = .121). Therefore, the influences of sensation seeking on the adolescent outcomes did not significantly vary across parent-reported impulsivity.7
Discussion
The present study examined executive and reactive disinhibition as mechanisms underlying familial substance use disorder risk for adolescent externalizing outcomes, and tested whether executive and reactive disinhibition differentially predicted different facets of the externalizing spectrum. Our results demonstrated that adolescent reactive disinhibition, as measured by sensation seeking, was a mediator of the influence of familial drug disorders on adolescent substance use (over and above the effects of executive disinhibition). In contrast, executive disinhibition, as measured by three executive functioning tasks, was not predicted by familial alcohol or drug use disorders or parent antisociality (although trait impulsivity was related to familial alcohol use disorder), and executive disinhibition was not a unique predictor of adolescent substance use. Rather, poor spatial short term memory, response disinhibition and trait impulsivity were significant unique predictors of ADHD symptoms, and response disinhibition and trait impulsivity were significant unique predictors of conduct problems. These results provide clear support for Nigg’s (2000; 2003) theorized distinction between executive and reactive disinhibition and illustrate the importance of “unpacking” the broad temperament style of “undercontrol.” Not only were the two types of disinhibition differentially predicted by familial risk, but they conferred risk differentially to different forms of adolescent externalizing behaviors
Relation of reactive and executive disinhibition to density of familial alcohol and drug disorders
The current findings showed that adolescents with higher levels of reactive disinhibition as measured by sensation seeking also had more dense family histories of drug disorders. However, although sensation seeking was related to familial drug disorders it was not uniquely related to density of familial alcoholism. In interpreting this finding, it is important to remember that adolescents with more drug disordered relatives are also more likely to have denser histories of familial alcoholism, whereas adolescents with alcohol disordered relatives do not necessarily have as high a likelihood of having drug disordered relatives. This asymmetry in the overlap of alcohol and drug disorders seen in the current study is also evident in epidemiological data, which show that individuals with drug disorders are more likely to have comorbid alcohol disorders whereas individuals with alcohol disorders are less likely to show comorbid drug disorders (Kessler, 2007). In addition, high familial drug disorder density likely reflects a more severe family history risk (including drug disorders, alcohol disorders, and antisociality) than does high familial alcohol disorder density (Dick et al., 2007). Interestingly, previous research also indicates that alcohol disorder comorbid with drug disorder is more likely to result from pathways related to lack of constraint whereas alcohol disorder in the absence of drug disorder is more likely to reflect pathways involving negative emotionality or physiological responses to alcohol (McGue et al., 1999; Chassin et al., 2004; Grekin, Sher, & Wood, 2006). Thus, our finding that adolescents with high familial drug disorder densities show high levels of reactive disinhibition may reflect risk pathways involving lack of constraint. Moreover, our finding that adolescents with particularly severe familial risk show elevated reactive disinhibition is consistent with the findings of Nigg and colleagues (2004) who found that sons of antisocial alcoholic parents, but not sons of non-antisocial alcoholic parents, exhibited deficits in regulatory control in the context of rewards.
In contrast, (with the exception of a relation between familial alcohol density and trait impulsivity), our results did not show a relation between executive disinhibition and either familial alcohol or drug disorders. Specifically, performance on cognitive tasks reflecting executive functions was not predicted by familial alcohol or drug disorders, or parental antisociality. Interestingly, when IQ was not controlled, familial alcoholism was related to executive functioning tasks, suggesting that relations between familial alcoholism and executive functioning may be spurious or better accounted for by the third variable of IQ. In fact, research findings concerning executive functioning deficits associated with familial alcoholism risk is decidedly mixed. Consistent with our findings, a number of researchers have also failed to find familial alcoholism effects on executive functioning (i.e., Spadoni et al., 2008; Stevens et al., 2003; Wiers et al., 1998). However, others have found evidence of an association (i.e. Corral et al, 1999; 2003; Nigg et al., 2004). A possible explanation for the differing findings may be differences in tasks designed to tap executive functioning. For example, Nigg et al. (2004) found differences between sons of non-antisocial alcoholics and controls on tasks designed to tap response suppression and response regulation, but not on tasks tapping set shifting and working memory and visual working memory planning which may be more analogous to our measures of executive disinhibition.
Although familial alcoholism was not related to executive disinhibition as measured by cognitive tasks, familial alcoholism was related to “trait” impulsivity. Many other studies have also noted differences in findings produced by “task” and “trait” measures (see Dick et al., 2010 for a recent review). Our results may suggest that although adolescents with familial alcohol and drug use disorders may not be at risk for specific executive functioning weakness, those with familial alcohol use disorders may be at risk for a broader temperamental style marked by a lack of planning or premeditation. Alternatively, however, given that trait impulsivity was parent-reported, the relation found between familial alcoholism and offspring trait impulsivity might also reflect shared measurement variance.
Relations of executive and reactive disinhibition to adolescent externalizing outcomes
The central finding of the current study was that executive and reactive disinhibition differentially predicted different facets of the externalizing spectrum. Most important, as predicted, adolescent substance use was related only to reactive disinhibition, and not to executive disinhibition. This was true regardless of whether executive disinhibition was operationalized as performance on cognitive tasks or as trait impulsivity, so that the findings were robust and could not be accounted for by shared method variance. Thus, our results clearly indicate a reward-driven risk pathway, rather than an executive dysfunction pathway, to adolescent substance use. This finding is consistent with a number of recent studies demonstrating the association between reward response weakness, or sensation seeking, and substance use (e.g., Castellanos-Ryan, Rubia, & Conrod, 2010; Cyders, Flory, Rainer, & Smith, 2009; Magid, Maclean, & Colder, 2007; Urcelay & Dalley, in press; Whiteside & Lynam, 2003; Whiteside, Lynam, Miller, & Reynolds, 2005). For example, consistent with our findings, Cyders and colleagues (2009) found that sensation seeking, but not planning or perseverance, was associated with college student drinking. Similarly, Castellanos-Ryan and colleagues (2010) found that response disinhibition among adolescents was associated with conduct problems, whereas “hot” reward response weakness was associated with binge drinking. Our results corroborate their claims that adolescents who become dysregulated in the context of “hot” rewards or motivation are at risk for substance use and extend this work to suggest that “cold” executive functioning weakness, may not be a primary pathway to adolescent substance use. Therefore, adolescent substance use may be better conceptualized as a result of difficulty “putting on the breaks,” when rewards are present, rather than difficulty with thoughtful planning or persistence in working toward a goal. Given that substance use is associated with physiological responses that may be temporarily rewarding, it makes sense that individuals who demonstrate disinhibition in the context of rewards may be particularly vulnerable to substance use.
Steinberg’s (2010) dual systems model of adolescent risk taking describes the differential development of reward sensitivity and cognitive control such that around the time of puberty, adolescents experience a dramatic increase in reward sensitivity, whereas the development of impulse control appears to be a more gradual process occurring slowly throughout adolescence and emerging adulthood. Consequently, risky behavior may increase during adolescence because of the gap between elevated reward sensitivity and immature cognitive control. Moreover, because peer social interactions are particularly rewarding for adolescents, they may show most risk-taking in peer contexts (Steinberg, 2010). Because adolescent substance use typically occurs in a peer context, disruptions of adolescent self-regulation in highly rewarding contexts may be particularly relevant for adolescent substance use.
With regards to the relations between disinhibition and ADHD symptoms, ADHD symptoms were predicted by trait impulsivity, poor spatial working memory, and response disinhibition and inconsistently predicted by sensation seeking (in the model including cognitive tasks but not in the model including trait impulsivity). Our findings that executive functioning and trait impulsivity predict ADHD symptoms are consistent with a large body of research showing executive disinhibition deficits in ADHD (e.g., Barkley, 1997; Willcutt, Doyle, Nigg, Faraone, & Pennington, 2005). Also, the relations between ADHD and sensation seeking are consistent with some research that suggests a weaker secondary pathway of reactive disinhibition to ADHD (Nigg, 2003; Sonuga-Barke, 2003; 2005; Urcelay & Dalley, in press). Because studies do not consistently find relations between ADHD and sensation seeking (see e.g., Blaskey et al., 2008), more work is needed to understand the role of sensation seeking, or “bottom-up” reactive processes, in the development of ADHD.
Our results also showed that conduct problems were associated with response disinhibition and trait impulsivity, and inconsistently associated with sensation seeking. That is, sensation seeking predicted conduct problems in the cognitive task model but not when trait impulsivity was considered. Although it is possible that trait impulsivity is a more salient underlying pathway to conduct problems than is sensation seeking, future research is necessary to more fully clarify these mechanisms given the inconsistent findings for sensation seeking.
Further research is also needed to understand the extent to which ADHD and conduct problems share a common diathesis in terms of executive and reactive disinhibition, or are affected to different degrees by executive and reactive disinhibition, or differ in their diatheses. Of course, other influences may also determine whether an individual develops ADHD or conduct problems or both. For example, some researchers have suggested that ADHD and conduct disorder share a common diathesis but that the quality of parenting influences the nature of the resulting symptomatology(see Beauchaine, Hinshaw, & Pang, 2010 for a review). Further study to understand the overlap and diatheses between ADHD and conduct problems, and the heterogeneity of each is warranted, especially with regards to dimensions of disinhibition.
We found only limited evidence for Finn’s (2002) cognitive-motivational theory, which posits that working memory interacts with novelty seeking to influence alcohol use. Our findings indicated that for adolescents with response inhibition weakness, sensation seeking was a significant predictor of all three facets of the adolescent externalizing spectrum (i.e., ADHD symptoms, conduct problems, and substance use) whereas for adolescents with strong response inhibition, sensation seeking did not significantly predict outcomes. Other substance use researchers (e.g., Grenard et al., 2008) also suggest that strong executive functioning allows for “cool” reflective controlled processes to over-ride the effects of reactive disinhibition on substance use outcomes. The lack of broader support for these interaction effects in the current data may be due to statistical limitations of the multiple group model tests which dichotomize task performance as well as the low statistical power associated with interaction tests.
Executive and reactive disinhibition as mediators of familial risk for adolescent externalizing outcomes
We found that reactive disinhibition, but not executive disinhibition, mediated the influence of familial drug disorder risk on adolescent externalizing outcomes, supporting a novelty-driven disinhibitory pathway of familial drug disorder risk. However, our findings are not definitive about whether this reactive disinhibitory pathway (indicated by sensation seeking) raises risk broadly for all externalizing outcomes or only for substance use. When executive disinhibition was operationalized by cognitive task performance, our results are consistent with sensation-seeking as a broad diathesis of externalizing spectrum risk (Iacono, Malone, & McGue, 2008). However, when executive disinhibition was conceptualized as parent-reported impulsivity, sensation seeking predicted only substance use outcomes, supporting a much more specific pathway underlying familial risk for adolescent substance use outcomes. What is clear in both cases, however, is that reactive disinhibition and not executive disinhibition, predicted adolescent substance use. Thus, in terms of mediators of intergenerational transmission of risk for adolescent substance use, it may be a propensity for disinhibition in the “hot” context of novelty rather than a “cool” executive functioning weakness that is the pathway of risk.
Although the present study makes new contributions to the literature on the risk mechanisms underlying the adolescent externalizing spectrum, several limitations should be noted. First, our data are cross-sectional. Although reverse directions of effect are unlikely (e.g., adolescent cognitive task performance is not likely to influence family history density of substance use disorders and the low levels of substance use in these young adolescents are not likely to substantially influence their executive and reactive disinhibition), longitudinal data are important to further our understanding of these risk pathways. Moreover, different forms of disinhibition may be important for different stages of substance use from initiation to maintenance, the development of clinical substance use disorder or cessation (Urcelay & Dalley, in press). Also, we did not measure clinically diagnosed parent or grandparent antisocial personality disorder, and relied on a proxy measure which might underestimate the unique effects of familial antisociality. Finally, it would be useful to have additional measures of reactive disinhibition.
In summary, the current study was the first to examine both executive and reactive disinhibition, in one model, as potential mechanisms underlying familial substance use disorder risk for multiple facets of the adolescent externalizing spectrum. Our results provide clear evidence for Nigg’s (2000; 2003) proposed distinction between executive and reactive disinhibition as well as for similar models that distinguish between “cold” and “hot” failures of self-regulation (e.g., Kerr & Zelazo, 2004; Potenza & De Wit, 2010; Rubia, in press; Steinberg, 2010). Executive and reactive disinhibition were not only differentially predicted by familial risk, but they conferred risk differentially to different facets of the externalizing spectrum. Specifically, reactive disinhibition significantly mediated the effect of familial drug use disorder on adolescent substance use. In contrast, executive disinhibition, as measured by response disinhibition, spatial short-term memory, and working memory was not associated with familial substance use disorders, and did not predict adolescent substance use, although executive disinhibition was related to ADHD and conduct problems. Moreover, executive disinhibition, as measured by “trait” impulsivity or a lack of planning or premeditation, was associated with familial alcohol use disorder, adolescent ADHD symptoms, and conduct problems, but not with adolescent substance use. These findings illustrate the importance of “unpacking” the broad construct of disinhibition and of studying the processes that underlie the commonality among facets of the externalizing spectrum as well as processes that that predict specific externalizing outcomes.
Acknowledgments
This study was supported by a grant from the National Institute on Alcohol Abuse (NIAAA AA016213).
Footnotes
To select a cut-off of 5 symptoms, we examined early conduct problems among our original target participants at wave 3 (average age 15.2). Those with externalizing symptoms 1 standard deviation above the mean were considered to have conduct problems before age 15. Using this cut-off, 7.8% of original target participants were classified as demonstrating antisocial behavior at wave 6. We then determined that a CDIS cut-off of 5 ASP symptoms yielded approximately the same prevalence of antisocial behavior in the larger sample. Because the gender and family history of alcoholism of original target participants, their siblings, and spouses are relatively similar, we deemed this an appropriate cut-off for the sample.
In the current sample, raw scores were used for analyses because the other 2 measures of executive disinhibition were not scaled for age. Accordingly, age was used as a covariate in the model.
Given the lack of a significant unique effect of family history of alcohol use disorders on any of the outcomes, and the lack of an effect of family history of alcohol use disorders on sensation seeking, we did not test the indirect effect of family history of alcohol use disorders on the outcomes.
We also tested moderation following the Aiken and West (1991) method by creating interaction terms using the cross-product of each cognitive task multiplied by sensation seeking. There was no evidence of significant moderation using this method.
Because IQ was correlated with executive disinhibition, we also estimated a model without covarying IQ. The model fit the data well (χ2(52) = 69.81, p = .05, CFI = .95, RMSEA = .04, WRMR = .65) and results for the final model reported above were replicated, with the following differences: 1) high levels of family history of DUD were marginally related to sensation seeking (p=.07); 2) and high levels of family history of AUD significantly predicted poor performance on MST and IMT.
This trait model was also estimated using the restricted subsample of adolescents who were included in the cognitive task model and showed good fit to the data χ2(113) = 140.27, p <.05, CFI = .96, RMSEA = .03, WRMR = .71. The pattern of results was the same as with the larger sample except that sensation seeking marginally significantly predicted substance use (p=.07).
We also tested for moderation using the Aiken and West (1991) method by computing the cross-product of sensation seeking and impulsivity. There was no evidence of significant moderation using this method.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ABN
References
- Achenbach TM, Rescorla LA. Manual for ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- American Psychiatic Association. Diagnostic and Statistical Manual of Mental Disorders. 3. Washington, DC: Author; 1980. [Google Scholar]
- Aytaclar S, Tarter RE, Kirisci L, Lu S. Association between hyperactivity and executive cognitive functioning in childhood and substance use in early adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:172–178. doi: 10.1097/00004583-199902000-00016. [DOI] [PubMed] [Google Scholar]
- Barkley R. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychological Bulletin. 1997;121:65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- Barnard M, McKeganey N. The impact of parental problem drug use on children: What is the problem and what can be done to help? Addiction. 2004;99:552–559. doi: 10.1111/j.1360-0443.2003.00664.x. [DOI] [PubMed] [Google Scholar]
- Bates ME, Pandina RJ. Familial alcoholism and premorbid cognitive deficit: A failure to replicate subtype differences. Journal of Studies on Alcohol. 1992;53:320–327. doi: 10.15288/jsa.1992.53.320. [DOI] [PubMed] [Google Scholar]
- Bauer LO, Hesselbrock VM. Subtypes of family history and conduct disorder: Effects on P300 during the stroop test. Neuropsychopharmacology. 1999;21:51–62. doi: 10.1016/S0893-133X(98)00139-0. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Hinshaw SP, Pang KL. Comorbidity of attention-deficit/hyperactivity disorder and early-onset conduct disorder: Biological, environmental, and developmental mechanisms. Clinical Psychology Science and Practice. 2010;17:327–336. [Google Scholar]
- Blaskey LG, Harris L, Nigg J. Are sensation seeking and emotion processing related to or distinct from cognitive control in children with ADHD? Child Neuropsychology. 2008;14:353–371. doi: 10.1080/09297040701660291. [DOI] [PubMed] [Google Scholar]
- Castellanos-Ryan N, Rubia K, Conrod P. Sensation seeking and common and unique variance in conduct disorder and substance misuse. Alcoholism: Clinical and Experimental Research. 2011;35:1–15. doi: 10.1111/j.1530-0277.2010.01331.x. [DOI] [PubMed] [Google Scholar]
- Chartier KG, Hesselbrock MN, Hesselbrock VM. Ethnicity and adolescent pathways to alcohol use [Special Issue] Journal of Studies on Alcohol and Drugs. 2009;70:337–345. doi: 10.15288/jsad.2009.70.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Barrera M, Bech K, Kossak-Fuller J. Recruiting a community sample of adolescent children of alcoholics: A comparison of three subject sources. Journal of Studies on Alcohol. 1992;53:316–319. doi: 10.15288/jsa.1992.53.316. [DOI] [PubMed] [Google Scholar]
- Chassin L, Flora DB, King KM. Trajectories of alcohol and drug use and dependence from adolescence to adulthood: The effects of familial alcoholism and personality. Journal of Abnormal Psychology. 2004;113:483–498. doi: 10.1037/0021-843X.113.4.483. [DOI] [PubMed] [Google Scholar]
- Chassin L, Pillow D, Curran P, Molina B, Barrera M. Relation of parental alcoholism to early adolescent substance use: A test of three mediating mechanisms. Journal of Abnormal Psychology. 1993;102:3–19. doi: 10.1037//0021-843x.102.1.3. [DOI] [PubMed] [Google Scholar]
- Chassin L, Pitts SC, DeLucia C, Todd M. A longitudinal study of children of alcoholics: Predicting young adult substance use disorders, anxiety, and depression. Journal of Abnormal Psychology. 1999;108:106–119. doi: 10.1037//0021-843x.108.1.106. [DOI] [PubMed] [Google Scholar]
- Chassin L, Rogosch F, Barrera M. Substance use and symptomology among adolescent children of alcoholics. Journal of Abnormal Psychology. 1991;100:449–463. doi: 10.1037//0021-843x.100.4.449. [DOI] [PubMed] [Google Scholar]
- Conway ARA, Kane MJ, Bunting MF, Hambrick DZ, Wilhelm O, Engle RW. Working memory span tasks: A methodological review and user’s guide. Psychonomic Bulletin and Review. 2005;12:769–786. doi: 10.3758/bf03196772. [DOI] [PubMed] [Google Scholar]
- Corral MM, Holguín SR, Cadaveira F. Neuropsychological characteristics of young children from high-density alcoholism families: A three-year follow-up. Journal of Studies on Alcohol. 2003;64:195–199. doi: 10.15288/jsa.2003.64.195. [DOI] [PubMed] [Google Scholar]
- Corral MM, Holguín SR, Cadaveira F. Neuropsychological characteristics in children of alcoholics: Familial density. Journal of Studies on Alcohol. 1999;60:509–513. doi: 10.15288/jsa.1999.60.509. [DOI] [PubMed] [Google Scholar]
- Cyders MA, Flory K, Rainer S, Smith GT. The role of personality dispositions to risky behavior in predicting first year college drinking. Addiction. 2009;104:193–202. doi: 10.1111/j.1360-0443.2008.02434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Smith GT. Mood-based rash action and its components: Positive and negative urgency. Personality and Individual Differences. 2007;43:839–850. [Google Scholar]
- Dick DM, Agrawal A, Wang JC, Hinrichs A, Bertelsen S, Bucholz KK, Schukit M, Kramer J, Nurnberger J, Tischfield J, Edenberg HA, Goate A, Bierut LJ. Alcohol dependence with comorbid drug dependence: Genetic and phenotypic associations suggest a more severe form of the disorder with stronger genetic contribution to risk. Addiction. 2007;102:1131–1139. doi: 10.1111/j.1360-0443.2007.01871.x. [DOI] [PubMed] [Google Scholar]
- Dick DM, Smith G, Olausson P, Mitchell SH, Leeman RF, O’Malley SS, Sher K. Review: Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addiction Biology. 2010;15:217–226. doi: 10.1111/j.1369-1600.2009.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Marsh DM, Mathias CW. Immediate and delayed memory tasks: A computerized behavioral measure of memory, attention, and impulsivity. Behavior Research Methods, Instruments and Computers. 2002;34:391–398. doi: 10.3758/bf03195467. [DOI] [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, Marsh DM, Jagar AA. Laboratory behavioral measures of impulsivity. Behavior Research Methods. 2005;37:82–90. doi: 10.3758/bf03206401. [DOI] [PubMed] [Google Scholar]
- Edwards EP, Leonard KE, Das Eiden R. Temperament and behavioral problems among infants in alcoholic families. Infant Mental Health Journal. 2001;22:374–392. doi: 10.1002/imhj.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endicott J, Andreason N, Spitzer R. Family history research diagnostic criteria. New York State Psychiatric Institute, Biometrics Research Department; New York: 1975. [Google Scholar]
- Elkins IJ, McGue M, Malone S, lacono WG. The effect of parental alcohol and drug disorders on adolescent personality. American Journal of Psychiatry. 2004;161:670–676. doi: 10.1176/appi.ajp.161.4.670. [DOI] [PubMed] [Google Scholar]
- Eysenck SB, Pearson PR, Easting G, Allsopp JF. Age norms for impulsiveness, venturesomeness, and empathy in adults. Personality and Individual Differences. 1985;6:613–619. [Google Scholar]
- Farmer RF, Seeley JR, Kosty DB, Lewinsohn PM. Refinements in the hierarchical structure of externalizing psychiatric disorders: Patterns of lifetime liability from mid-adolescence through early adulthood. Journal of Abnormal Psychology. 2009;118:699–710. doi: 10.1037/a0017205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn PR. Motivation, working memory, and decision making: A cognitive-motivational theory of personality vulnerability to alcoholism. Behavioral and Cognitive Neuroscience Reviews. 2002;1:183–205. doi: 10.1177/1534582302001003001. [DOI] [PubMed] [Google Scholar]
- Finn PR, Mazas CA, Justus AN, Steinmetz J. Early-onset alcoholism with conduct disorder: Go/no go learning deficits, working memory capacity, and personality. Alcoholism: Clinical and Experimental Research. 2002;26:186–206. [PubMed] [Google Scholar]
- Flory K, Lynam DR. The relation between attention deficit hyperactivity disorder and substance abuse: What role does conduct disorder play? Clinical Child and Family Psychology Review. 2003;6:1–16. doi: 10.1023/a:1022260221570. [DOI] [PubMed] [Google Scholar]
- Giancola PR, Moss HB, Martin CS, Kirisci L, Tarter RE. Executive cognitive functioning predicts reactive aggression in boys at high risk for substance abuse: A prospective study. Alcoholism: Clinical and Experimental Research. 1996;20:740–744. doi: 10.1111/j.1530-0277.1996.tb01680.x. [DOI] [PubMed] [Google Scholar]
- Giancola P, Parker A. A six-year prospective study of pathways toward drug use in adolescent boys with and without a family history of a substance use disorder. Journal of Studies on Alcohol. 2001;62:166–178. doi: 10.15288/jsa.2001.62.166. [DOI] [PubMed] [Google Scholar]
- Grekin E, Sher K, Wood P. Personality and substance dependence symptoms: modeling substance-specific traits. Psychology of Addictive Behaviors. 2006;20:415–24. doi: 10.1037/0893-164X.20.4.415. [DOI] [PubMed] [Google Scholar]
- Grenard J, Ames S, Wiers R, Thush C, Sussman S, Stacy A. Working memory capacity moderates the predictive effects of drug-related associations on substance use. Psychology of Addictive Behaviors. 2008;22:426–32. doi: 10.1037/0893-164X.22.3.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harden PW, Pihl RO. Cognitive function, cardiovascular reactivity, and behavior in boys at high risk for alcoholism. Journal of Abnormal Psychology. 1995;104:94–103. doi: 10.1037//0021-843x.104.1.94. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Pryzbeck TR. The co-occurrence of alcoholism with other psychiatric disorders in the general population and its impact on treatment. Journal of Studies on Alcohol. 1988;49:219–244. doi: 10.15288/jsa.1988.49.219. [DOI] [PubMed] [Google Scholar]
- Herba CM, Tranah T, Rubia K, Yule W. Conduct problems in adolescence: Three domains of inhibition and effect of gender. Developmental Neuropsychology. 2006;30:659–695. doi: 10.1207/s15326942dn3002_2. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Krueger RF, lacono WG, McGue M, Patrick CJ. Family transmission and heritability of externalizing disorders: A twin-family study. Archives of General Psychiatry. 2004;61:922–928. doi: 10.1001/archpsyc.61.9.922. [DOI] [PubMed] [Google Scholar]
- Hofmann W, Friese M, Strack F. Impulse and self-control from a dual-systems perspective. Perspectives on Psychological Science. 2009;4:162–176. doi: 10.1111/j.1745-6924.2009.01116.x. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler P. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Iacono W, Malone S, McGue M. Behavioral disinhibition and the development of early-onset addiction: Common and specific influences. Annual Review of Clinical Psychology. 2008;4:325–348. doi: 10.1146/annurev.clinpsy.4.022007.141157. [DOI] [PubMed] [Google Scholar]
- Jacob T, Johnson S. Parenting influences on the development of alcohol abuse and dependence. Alcohol Health and Research World. 1997;21:204–209. [PMC free article] [PubMed] [Google Scholar]
- Johnson JL, Leff M. Children of substance abusers: Overview of research findings. Pediatrics. 1999;103:1085–1099. [PubMed] [Google Scholar]
- Kane MJ, Hambrick DZ, Tuholski SW, Wilhelm O, Payne TW, Engle RW. The generality of working memory capacity: A latent variable approach to verbal and visuospatial memory span and reasoning. Journal of Experimental Psychology: General. 2004;133:189–217. doi: 10.1037/0096-3445.133.2.189. [DOI] [PubMed] [Google Scholar]
- Kaufman AS, Kaufman NL. Kaufman Brief Intelligence Test Manual. American Guidance Service; Circle Pines, MN: 1990. [Google Scholar]
- Kerr A, Zelazo PD. Development of hot executive function: the children’s gambling task. Brain and Cognition. 2004;55:148–157. doi: 10.1016/S0278-2626(03)00275-6. [DOI] [PubMed] [Google Scholar]
- Kessler R. The prevalence of psychiatric comorbidity. In: Wetzler S, Sanderson WC, editors. Treatment Strategies for Patients with Psychiatric Comorbidity. New York: Wiley; 1997. pp. 23–48. [Google Scholar]
- King SM, Keyes M, Malone SM, Elkins I, Legrand LN, Iacono WG, McGue M. Parental alcohol dependence and the transmission of adolescent behavioral disinhibition: A study of adoptive and non-adoptive families. Addiction. 2009;104:578–586. doi: 10.1111/j.1360-0443.2008.02469.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Loukas A, Fitzgerald HE, Zucker RA, von Eye A. Parental alcoholism and co-occurring antisocial behavior: Prospective relationships to externalizing behaviors problems in their young sons. Journal of Abnormal Child Psychology. 2001;29:91–106. doi: 10.1023/a:1005281011838. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavior Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magid V, Maclean MG, Colder CR. Differentiating between sensation seeking and impulsivity through their mediated relations with alcohol use and problems. Addictive Behaviors. 2007;32:2046–2061. doi: 10.1016/j.addbeh.2007.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGue M, Slutske W, Iacono WG. Personality and substance use disorders: II. Alcoholism versus drug use disorders. Journal of Consulting and Clinical Psychology. 1999;67:394–404. doi: 10.1037//0022-006x.67.3.394. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Stolar M, Stevens DE, Goulet J, Preisig MA, Fenton B, Zhang H, O’Malley SS, Rounsaville BJ. Familial transmission of substance use disorders. Archives of General Psychiatry. 1998;55:973–979. doi: 10.1001/archpsyc.55.11.973. [DOI] [PubMed] [Google Scholar]
- Muthén BO, Muthén LK. Mplus Version 5.0, Computer Software and Manual. Los Angeles, CA: Muthén and Muthén; 1998–2010. [Google Scholar]
- Nigg JT. On inhibition/disinhibition in developmental psychopathology: Views from cognitive and personality psychology and a working inhibition taxonomy. Psychological Bulletin. 2000;126:220–246. doi: 10.1037/0033-2909.126.2.220. [DOI] [PubMed] [Google Scholar]
- Nigg JT. Response inhibition and disruptive behaviors: Toward a multiprocess conception of etiological heterogeneity for ADHD combined type and conduct disorder early-onset type. In: King JA, Ferris CF, Lederhendler II, editors. Roots of mental illness in children. New York, NY: New York Academy of Sciences; 2003. pp. 170–182. [DOI] [PubMed] [Google Scholar]
- Nigg JT. Temperament and developmental psychopathology. Journal of Child Psychology and Psychiatry. 2006;47:395–422. doi: 10.1111/j.1469-7610.2006.01612.x. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Glass JM, Wong MM, Poon E, Jester JM, Fitzgerald HE, Puttler LI, Adams KM, Zucker RA. Neuropsychological executive functioning in children at elevated risk for alcoholism: Findings in early adolescence. Journal of Abnormal Psychology. 2004;113:302–314. doi: 10.1037/0021-843X.113.2.302. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Wong MM, Martel MM, Jester JM, Puttler LI, Glass JM, et al. Poor response inhibition as a predictor of problem drinking and illicit drug use in adolescents at risk for alcoholism and other substance use disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:468–475. doi: 10.1097/01.chi.0000199028.76452.a9. [DOI] [PubMed] [Google Scholar]
- Nunes EV, Weissman MM, Goldstein R, McAvay G, Beckford C, Seracini A, Verdeli H, Wickramaratne P. Psychiatric disorders and impairment in the children of opiate addicts: Prevalences and distribution by ethnicity. American Journal on Addictions. 2000;9:232–241. doi: 10.1080/10550490050148062. [DOI] [PubMed] [Google Scholar]
- Nussbeck FW, Eid M, Lischetzke T. Analysing multitrait-multimethod data with structural equation models for ordinal variables applying the WLSMV estimator: What sample size is needed for valid results? British Journal of Mathematical and Statistical Psychology. 2006;59:195–213. doi: 10.1348/000711005X67490. [DOI] [PubMed] [Google Scholar]
- Ohannessian CM, Hesselbrock VM, Kramer J, Kuperman S, Bucholz KK, Schuckit MA, Nurnberger JI. The relationship between parental alcoholism and adolescent psychopathology: A systematic examination of parental comorbid psychopathology. Journal of Abnormal Child Psychology. 2004;32:519–533. doi: 10.1023/b:jacp.0000037781.49155.a6. [DOI] [PubMed] [Google Scholar]
- Oosterlaan J, Scheres A, Sergeant JA. Which executive functioning deficits are associated with AD/HD, ODD/CD and comorbid AD/HD+ODD/CD? Journal of Abnormal Child Psychology. 2005;33:69–85. doi: 10.1007/s10802-005-0935-y. [DOI] [PubMed] [Google Scholar]
- Peterson JB, Finn PR, Pihl RO. Cognitive dysfunction and the inherited predisposition to alcoholism. Journal of Studies on Alcohol. 1992;53:154–160. doi: 10.15288/jsa.1992.53.154. [DOI] [PubMed] [Google Scholar]
- Potenza M, De Wit H. Control Yourself: Alcohol and Impulsivity. Alcoholism: Clinical and Experimental Research. 2010;34:1303–1305. doi: 10.1111/j.1530-0277.2010.01214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins LN, Cottler LB, Bucholz KK, Compton WM, North CS, Rourke KM. Diagnostic Interview Schedule for the DSM-IV (DIS-IV) St. Louis, MO: Washington University School of Medicine; 2000. [Google Scholar]
- Rounsaville BJ, Kosten TR, Weissman MM, Prusoff B, Pauls D, Anton SF, Merikangas K. Psychiatric disorders in relatives of probands with opiate addiction. Archives of General Psychiatry. 1991;48:33–42. doi: 10.1001/archpsyc.1991.01810250035004. [DOI] [PubMed] [Google Scholar]
- Rubia K. “Cool” inferior frontostriatal dysfunction in attention-deficit/hyperactivity disorder versus “hot” ventromedial orbitofrontal-limbic dysfunction in conduct disorder: A review. Biological Psychiatry. doi: 10.1016/j.biopsych.2010.09.023. in press. [DOI] [PubMed] [Google Scholar]
- Schafer K, Butters N, Smith T, Irwin M, Brown S, Hanger P, Grant I, Shuckit M. Cognitive performance of alcoholics: A longitudinal evaluation of the role of drinking history, depression, liver function, nutrition, and family history. Alcoholism: Clinical and Experimental Research. 1991;15:653–660. doi: 10.1111/j.1530-0277.1991.tb00574.x. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Schuckit MA, Butters N, Lyn L, Irwin MR. Neuropsychological deficits and the risk for alcoholism. Neuropsychopharmacology. 1987;1:45–53. doi: 10.1016/0893-133x(87)90009-1. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, Danko GP, Trim R, Bucholz KK, Edenberg HJ, Hesselbrock V, Kramer JJ, Dick DM. An evaluation of the full level of response to alcohol model of heavy drinking and problems in COGA offspring [Special Issue] Journal of Studies on Alcohol and Drugs. 2009;70:436–445. doi: 10.15288/jsad.2009.70.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher KJ. Children of alcoholics: A critical appraisal of theory and research. Chicago, IL: University of Chicago Press; 1991. [Google Scholar]
- Sher KJ, Bartholow BD, Wood MD. Personality and substance use disorders: A prospective study. Journal of Consulting and Clinical Psychology. 2000;68:818–829. [PubMed] [Google Scholar]
- Sher KJ, Grekin ER, Williams NA. The development of alcohol use disorders. Annual Review of Clinical Psychology. 2005;1:493–523. doi: 10.1146/annurev.clinpsy.1.102803.144107. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Walitzer KS, Wood PK, Brent EE. Characteristics of children of alcoholics: Putative risk factors, substance use and abuse, and psychopathology. Journal of Abnormal Psychology. 1991;100:427–448. doi: 10.1037//0021-843x.100.4.427. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS. The dual pathway model of AD/HD: An elaboration of neuro-developmental characteristics [Special Issue] Neuroscience and Biobehavioral Reviews. 2003;27:593–604. doi: 10.1016/j.neubiorev.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS. Causal models of attention-Deficit/Hyperactivity disorder: From common simple deficits to multiple developmental pathways. Biological Psychiatry. 2005;57:1231–1238. doi: 10.1016/j.biopsych.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Spadoni AD, Norman AL, Schweinsburg AD, Tapert SF. Effects of family history of alcohol use disorders on spatial working memory bold response in adolescents [Special Issue] Alcoholism: Clinical and Experimental Research. 2008;32:1135–1145. doi: 10.1111/j.1530-0277.2008.00694.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L. A dual systems model of adolescent risk-taking. Developmental Psychobiology. 2010;52:216–224. doi: 10.1002/dev.20445. [DOI] [PubMed] [Google Scholar]
- Stevens MC, Kaplan RF, Hesselbrock VM. Executive-cognitive functioning in the development of antisocial personality disorder. Addictive Behaviors. 2003;28:285–300. doi: 10.1016/s0306-4603(01)00232-5. [DOI] [PubMed] [Google Scholar]
- Tarter R. Are there inherited behavioral traits that predispose to substance abuse? Journal of Consulting and Clinical Psychology. 1988;56:189–196. doi: 10.1037//0022-006x.56.2.189. [DOI] [PubMed] [Google Scholar]
- Urcelay GP, Dalley JW. Linking ADHD, impulsivity, and drug abuse: A neuropsychological perspective. Current Topics in Behavioral Neuroscience. doi: 10.1007/7854_2011_119. in press. [DOI] [PubMed] [Google Scholar]
- van Goozen SHM, Cohen-Kettenis PT, Snoek H, Matthys W, Swaab-Barneveld H, van Engeland H. Executive functioning in children: A comparison of hospitalised ODD and ODD/ADHD children and normal controls. Journal of Child Psychology and Psychiatry. 2004;45:284–292. doi: 10.1111/j.1469-7610.2004.00220.x. [DOI] [PubMed] [Google Scholar]
- Wahlstedt C, Thorell LB, Bohlin G. ADHD symptoms and executive function impairment: Earlier predictors of later behavioral problems. Developmental Neuropsychology. 2008;33:160–178. doi: 10.1080/87565640701884253. [DOI] [PubMed] [Google Scholar]
- Wechsler D. WISC-IV technical and interpretive manual. San Antonio, TX: Psychological Corporation; 2003. [Google Scholar]
- Weinberg NZ, Rahdert E, Colliver JD, Glantz MD. Adolescent substance abuse: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:252–261. doi: 10.1097/00004583-199803000-00009. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–689. [Google Scholar]
- Whiteside SP, Lynam DR. Understanding the role of impulsivity in alcohol abuse: Application of the UPPS Impulsive Behavior Scale. Experimental and Clinical Psychopharmacology. 2003;11:210–217. doi: 10.1037/1064-1297.11.3.210. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR, Miller JD, Reynolds SK. Validation of the UPPS Impulsive Behaviour Scale: A Four-factor Model of Impulsivity. European Journal of Personality. 2005;19:559–574. [Google Scholar]
- Wiers RW, Gunning WB, Sergeant JA. Is a mild deficit in executive functions in boys related to childhood ADHD or to parental multigenerational alcoholism? Journal of Abnormal Child Psychology. 1998;26:415–430. doi: 10.1023/a:1022643617017. [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biological Psychiatry. 2005;57:1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]
- Wilson JR, Nagoshi CT. Adult children of alcoholics: Cognitive and psychomotor characteristics. Journal of Studies on Alcohol. 1988;48:437–442. doi: 10.1111/j.1360-0443.1988.tb00516.x. [DOI] [PubMed] [Google Scholar]
- Wong M, Zucker R, Puttler L, Fitzgerald H. Heterogeneity of risk aggregation for alcohol problems between early and middle childhood: nesting structure variations. Development and Psychopathology. 1999;11:727–744. doi: 10.1017/s0954579499002291. [DOI] [PubMed] [Google Scholar]
- Young SE, Stallings MC, Corley RP, Krauter KS, Hewitt JK. Genetic and environmental influences on behavioral disinhibition. American Journal of Medical Genetics (Neuropsychiatric Genetics) 2000;96:684–695. [PubMed] [Google Scholar]
- Yu CY, Muthe’n BO. Evaluation of model fit indices for latent variable models with categorical and continuous outcomes (Technical Report) Los Angeles: University of California at Los Angeles, Graduate School of Education & Information Studies; 2002. [Google Scholar]
- Zhou Q, King KM, Chassin L. The roles of familial alcoholism and adolescent family harmony in young adults’ substance dependence disorders: Mediated and moderated relations. Journal of Abnormal Psychology. 2006;115:320–331. doi: 10.1037/0021-843X.115.2.320. [DOI] [PubMed] [Google Scholar]
- Zuckerman Marvin. Sensation Seeking: Beyond the Optimal Level of Arousal. Hillsdale, NJ: L4wrence Erlbaum Associates; 1979. [Google Scholar]