Abstract
The alternative transcription factor σB is responsible for transcription in Staphylococcus aureus during the stress response. Many virulence-associated genes are directly or indirectly regulated by σB. We hypothesized that treatment with antibiotics may act as an environmental stressor that induces σB activity in antibiotic-resistant strains. Several antibiotics with distinct modes of action, including ampicillin (12 µg/ml), vancomycin (16 or 32 µg/ml), chloramphenicol (15 µg/ml), ciprofloxacin (0.25 µg/ml), and sulfamethoxazole/trimethoprim (SXT, 0.8 µg/ml), were investigated for their ability to activate this transcription factor. We were especially interested in the stress response in vancomycin-resistant S. aureus (VRSA) strains treated with vancomycin. The transcription levels of selected genes associated with virulence were also measured. Real-time quantitative reverse transcription PCR was employed to evaluate gene transcription levels. Contact hemolytic and cytotoxicity assays were used to evaluate cell damage following antibiotic treatment. Antibiotics that target the cell wall (vancomycin and ampicillin) and SXT induced σB activity in VRSA strains. Expression of σB-regulated virulence genes, including hla and fnbA, was associated with the vancomycin-induced σB activity in VRSA strains and the increase in cytotoxicity upon vancomycin treatment. These effects were not observed in the sigB-deficient strain but were observed in the complemented strain. We demonstrate that sub-minimum inhibitory concentration (sub-MIC) levels of antibiotics act as environmental stressors and activate the stress response sigma factor, σB. The improper use of antibiotics may alter the expression of virulence factors through the activation of σB in drug-resistant strains of S. aureus and lead to worse clinical outcomes.
Introduction
Vancomycin is used to treat health care-associated infections resulting from multidrug-resistant S. aureus, including methicillin-resistant S. aureus (MRSA). The first clinical case of vancomycin-intermediate S. aureus (VISA) was reported in 1997, followed by the appearance of the first vanA-mediated vancomycin-resistant S. aureus (VRSA) clinical isolate in 2002 [1]–[3]. A recent study in Taiwan indicated that 2.9% of the MRSA strains isolated were VISA [4].
We are interested in studying the role of an antibiotic when applied to a resistant strain of bacteria. Such an antibiotic may no longer be lethal (or inhibit growth) but instead acts as a stimulus (stress) to drug-resistant strains. If so, whether this type of stress activates σB and thereby affects the expression of downstream virulence factors remains to be determined. σB is the alternative σ factor that modulates the general stress response in certain Gram-positive bacteria, including Bacillus subtilis, Listeria monocytogenes, and S. aureus [5]. In addition to the general stress response, σB regulates cell wall metabolism, membrane transport processes and virulence in S. aureus [6], [7]. It has also been shown that virulence factors, such as α-hemolysin (encoded by hla) and fibronectin-binding protein A (encoded by fnbA), are likely controlled by σB through the global regulator SarA and/or the agr locus [8], [9]. Recently, it was demonstrated that σB plays a role in central venous catheter (CVC)-associated infections [10].
Concentrations of antibiotics below the minimum inhibitory concentration (MIC) are known to promote a variety of bacterial properties, such as the alternation of virulence; the effects of sub-MICs do not necessarily involve a reduction in the growth rate [11]. It has been reported that sub-MICs of β-lactam antibiotics induce the expression of virulence-associated exotoxin genes in S. aureus [12]. In Clostridium difficile, another opportunistic pathogenic Gram-positive bacterium, the transcription of major virulence factor genes is induced by sub-MICs of antibiotics [13]. However, sub-MICs of protein synthesis-suppressing antibiotics, such as clindamycin, linezolid and quinupristin/dalfopristin, have been shown to inhibit virulence factors released by S. aureus [14]–[16].
In the present study, we hypothesized that σB may respond to antibiotic stress and mediate the stress signal to downstream virulence factors in antibiotic-resistant S. aureus strains. Antibiotics with distinct modes of action were used to investigate their potential in activating σB. The drugs used in this study were ampicillin β-lactam; targets the cell wall), vancomycin (glycopeptide; targets the cell wall), chloramphenicol (suppresses protein synthesis), ciprofloxacin (suppresses DNA synthesis), and SXT (interferes with folic acid metabolism). Because vancomycin is used to treat infections caused by MRSA, the effect of vancomycin treatment on cytotoxicity and the expression of selected virulence genes was tested in VRSA strains.
Materials and Methods
Bacterial strains, plasmids and growth conditions
The bacterial strains, plasmids and primers used in this study are listed in Table 1 and Table 2. All bacterial strains were routinely cultured at 37°C with the specific required antibiotics (Sigma) in BHI broth (for S. aureus), in LB broth (for E. coli) or on agar plates. The plasmids used to transform S. aureus strains were maintained in strain RN4220 prior to conducting the experiments.
Table 1. Bacterial strains and plasmids used in this study.
| Strain or plasmid | Descriptiona | Reference or source |
| Strains | ||
| Escherichia coli | ||
| DH5α | General molecular cloning | Invitrogen |
| Enterococcus faecalis | ||
| HIP12467 | pAM830::Tn1546; VanR | NARSAb [35] |
| Staphylococcus aureus | ||
| RN4220 | Plasmids reservation | NARSA |
| ATCC12598 | Standard strain | ATCC |
| SJC1200 | ATCC12598/pG1546; VanR | This study |
| SJC1205 | SJC1200, ΔsigB::spc; VanR, SpcR | This study |
| SJC1206 | SJC1205, rocA:: sigB operon; VanR, SpcR | This study |
| Plasmids | ||
| pGHL6 | E. coli/S. aureus shuttle vector | [36] |
| pG1546 | pGHL6/ΔluxAB::van operon | This study |
| pMAD | Vector for allelic replacement | [18] |
| pMAsigBD | pMAD/sigB::spc | This study |
| pMAsigBC | pMAD/rocA::sigB operon | This study |
Abbreviations: VanR, vancomycin resistant; SpcR, spectinomycin resistant.
Network on Antimicrobial Resistance in Staphylococcus aureus (NARSA).
Table 2. Primers used in this study.
| Primer | Sequence (5′ → 3′)a |
| Cloning | |
| Tn-SphI-F | AAAGCATGCAGGAATGAATTATGCGG |
| Tn-KpnI-R | CACTTGGTACCTACGGGCGAGTTTC |
| RsbU-BglII-F | CGGAAGATCTGACTGAAGCTAG |
| SigB-NcoI-R | GCTCAGGTGAAACTTCCATGGCTGATTTC |
| SigB-SalI-F | CGTCGACTAAGAAATTACAAGAAGCAGC |
| SA2151-BamHI-R | TTCTTGACGTGCAATGGGATCCTCAC |
| SigBop-SalI-F | CGGTCGACTATTGAAAATGACACACCATC |
| SigBop-NcoI-R | AACCATGGCGTCTATTATATGTATTTTTCAGAG |
| RocA-BamHI-F | CCTGGATCCACACCTAAGATGTG |
| RocA-SalI-R | CATGTGAATGGTCGACATTTAAAC |
| RocA-NcoI-F | CTGTTATGCATATACCATGGTC |
| RocA-BglII-R | GCATTAGAACAGATCTGAAACAACC |
| qRT-PCR | |
| sigB-F | TGGCGAAAGAGTCGAAATCAGC |
| sigB-R | TCAGCGGTTAGTTCATCGCTCAC |
| asp23-F | AAAATTGCTGGTATCGCTGC |
| asp23-R | TGTAAACCTTGTCTTTCTTGGT |
| fnbA-F | ACTGGCGCAGTGAGCGACCA |
| fnbA-R | GCACTTCTGGCGTTGGCGGT |
| hla-F | CCTGGCCTTCAGCATTTAAG |
| hla-R | GGTCCCCAATTTTGATTCAC |
| dnaA-F | TCCACATGCAGCGAGTTTAG |
| dnaA-R | GGTGGTCGATCACTCGAAAT |
Incorporated restriction sites are underlined.
The vancomycin-resistant S. aureus strain SJC1200 was generated by introducing a vancomycin resistance-carrying plasmid (pG1546) into strain ATCC 12598 as described previously [17]. The PRvanRSPHHAXPYvanYPZvanZ gene cluster (the van operon within Tn1546) in E. faecalis HIP12467 was amplified using the primer pair Tn-SphI-F and Tn-KpnI-R, which contained restriction sites for SphI and KpnI. The 7075-bp PCR product was then cloned into pGHL6 from which the luxAB gene was removed by digestion with the same restriction enzymes (New England Biolabs) to generate pG1546. VRSA strains, approved by the Chang Gung University biosafety committee, were used strictly in a P2 level laboratory, and all lab equipment and surfaces were sterilized by bleach and/or autoclaved immediately after the experiments were performed.
Allelic replacement of the sigB gene by a spectinomycin cassette (spc) was performed by introducing the pMASigBD plasmid into strain SJC1200 to generate the sigB mutant strain SJC1205, as described previously [18]. A spectinomycin cassette restricted by NcoI and SalI was flanked by the upstream and downstream arms of the PCR product. The 1115-bp upstream arm originating from the 5′ end of the sigB was amplified using the primer pair RsbU-BglII-F and SigB-NcoI-R, which contained BglII and NcoI restriction sites, respectively. The 1183-bp downstream arm restricted by SalI and BamHI was amplified using the primer pair SigB-SalI-F and SA2151-BamHI-R from the 3′ end of sigB. The constructed upstream arm-spc-downstream arm DNA fragment restricted by BglII and BamHI was then cloned into pMAD, yielding pMASigBD.
Complementation of the sigB mutation in strain SJC1205 was performed by inserting the full-length rsbU and sigB operon (PUrsbUPVrsbVWsigB), including the promoter region, into the rocA gene via homologous recombination to generate SJC1206 [19]. The 3277-bp PUrsbUPVrsbVWsigB DNA fragment restricted by SalI and NcoI was amplified using the primer pair SigBop-SalI-F and SigBop-NcoI-R and was flanked by parts of the 5′ and 3′ ends of rocA. The 484-bp 5′ region was amplified using the primer pair RocA-BamHI-F and RocA-SalI-R, whereas the 489-bp 3′ region was amplified using RocA-NcoI-F and RocA-BglII-R. The 5′ region-PUrsbUPVrsbVWsigB-3′ region DNA fragment was cloned into pMAD, yielding pMAsigBC, which was then used to transform into SJC1205. The sigB-complemented colonies were selected using blue-white screening at the non-permissive temperature [18]. The insertion of rocA by PUrsbUPVrsbVWsigB was confirmed by PCR and DNA sequencing.
Detection of gene expression and real-time quantitative reverse transcription PCR (qRT-PCR)
The activity of σB upon treatment with antibiotics with distinct modes of action was detected using RT-PCR by assaying the transcription of asp23, a gene encoding an alkaline shock protein, which is directly activated by σB [20]. The MICs of the antibiotics used in the present study were determined by an E-test and a microdilution broth method according to CLSI guidelines [21]. The MICs of the antibiotics for strain SJC1200, and the final concentrations used in the qRT-PCR assay are provided in Table 3. Antibiotics were added to bacterial cultures at the indicated concentrations at OD600 = 0.6. Antibiotic-treated or untreated bacterial cells were collected and pelleted at a given time and frozen on dry ice immediately. Total RNA was extracted from cell pellets using TRIzol (Invitrogen) followed by RQ1 RNase-free DNase (Promega) treatment to eliminate any remaining DNA. An RT-PCR time course was performed, and the results were visualized using agarose gel electrophoresis to determine the time points for subsequent qRT-PCR analysis. The mRNA levels, including those of sigB, asp23, fnbA and hla, upon vancomycin treatment (32 µg/ml) were determined by qRT-PCR with the KAPA™ SYBR® qPCR Kit (Kapa Biosystems) in a Roche LightCycler (LC-32). All samples were tested in triplicate in three independent experiments. The expression levels of different genes were normalized against the dnaA expression level. The fold change of each transcript was determined by the 2−ΔΔCT method compared with the untreated cells [22].
Table 3. MICs of antibiotics for strain SJC1200 and the final concentrations treated in qRT-PCR for all of the tested strains.
| Antibiotica | |||||
| Van | Amp | Cm | Cip | SXT | |
| MICb (µg/ml) | >256 | 32 | 64 | 0.8 | 2 |
| Treated concentrationc (µg/ml) | 16 or 32 | 12 | 16 | 0.25 | 0.8 |
Abbreviations: Van: vancomycin; Amp: ampicillin; Cm: chloramphenicol; Cip: ciprofloxacin; SXT: sulfamethoxazole/trimethoprim.
The MICs of antibiotics for strains SJC1205 and 1206 were the same as for SJC1200.
The concentrations used were based on the therapeutic levels except for SXT.
Contact hemolysis
Contact hemolysis was performed as described elsewhere [23]. The bacteria were cultured overnight, diluted to OD600 = 0.1 and subcultured in 20 ml of fresh LB Broth for about three hours at 37°C at which point the culture was in log phase (OD600 = 0.6∼0.8). The bacterial cultures were collected by centrifugation at 10,000×g for 10 minutes at 4°C and resuspended in 20 ml of cold PBS. Sheep blood was washed three times in PBS by centrifugation at 1,500×g for five minutes at 4°C and diluted to a final concentration of 8%. A 100 µl aliquot of bacterial culture was mixed with 900 µl of 8% red blood cells (10-fold dilution of bacteria) in a 1.5 ml centrifuge tube and incubated at 37°C for three hours. Finally, the mixtures were centrifuged at 1,500×g for 10 min at 4°C, and the OD450 was measured using a Novaspec II spectrophotometer (Pharmacia Biotech). The positive control sample contained erythrocytes that had been lysed by SDS. One unit of hemolytic activity was defined as half of the total erythrocytes lysed by hemolysin relative to the positive control at OD450, followed by multiplication by the dilution factor to obtain the final hemolytic unit.
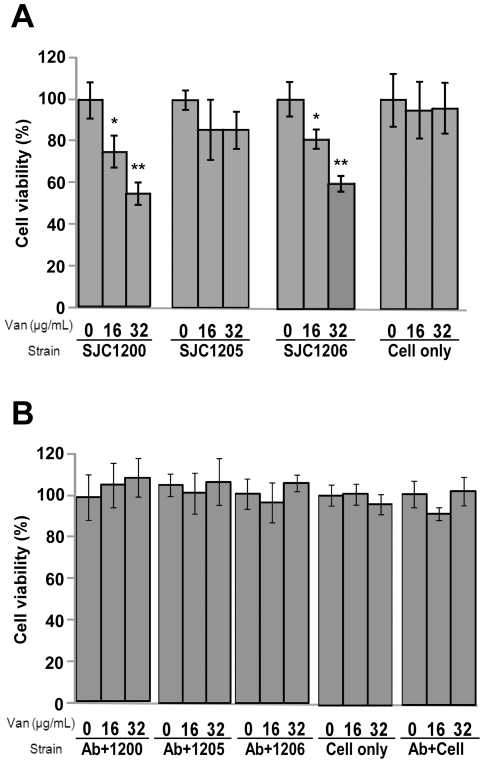
Cytotoxicity assay
The cytotoxicity assay was performed by evaluating the cell viability of BEAS-2B cells (human bronchial epithelial cells) co-cultured with S. aureus in the presence of different concentrations of vancomycin. BEAS-2B cells were maintained in RPMI-1640 medium (Gibco BRL) supplemented with 10% fetal bovine serum, 10% glycine and 1% penicillin and streptomycin at 37°C in a humidified atmosphere of air and 5% CO2. Cell viability tests were performed using the MTT assay with the cell proliferation reagent MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl tetrazolium bromide; Sigma), as described previously [24]. The MTT tetrazolium ring is cleaved only by active mitochondria, yielding purple formazan crystals whose amount directly correlates with the viable cell count. Cells were inoculated with different S. aureus strains (multiplicity of infection of 100) in the presence of different concentrations of vancomycin. In a parallel experiment, polyclonal fibronectin antibodies (5 µg/ml; Abcam) were added to block the interaction between fibronectin-binding proteins and cells. After six hours of exposure, 10 µl of a 5 mg/ml MTT solution was added into each well, and the plates were incubated at 37°C for 2.5 hours. The purple formazan crystals were dissolved by adding 100 µl of MTT solubilization solution (Sigma), and the absorbance at A570 was spectrophotometrically measured with a reference wavelength of A690. The results were expressed as the percent absorbance of the vancomycin-treated cultures versus the untreated control cultures. Three wells per dose were counted in three independent experiments.
Statistical analysis
A Student's t-test was used to analyze the experimental data and to compare means. P values of less than 0.05 were considered statistically significant.
Results
Effect of antibiotic treatment on the expression of σB
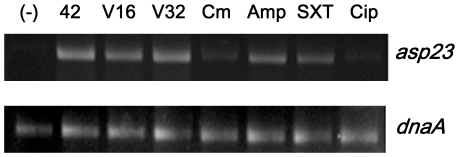
Strain SJC1200 was treated with antibiotics with distinct modes of action at sub-inhibitory concentrations as shown in Table 3. Bacterial growth was assessed by monitoring the growth curve spectrophotometrically at OD600. The plateau level was not affected by antibiotic treatment, but the stationary phase was reached later than in the drug-free condition (data not shown). The expression of asp23, which is directly activated by σB, was increased at 10 minutes post-treatment with ampicillin, vancomycin, and SXT (Fig. 1).
Figure 1. Effects of different antibiotics with distinct modes of action on asp23 transcription.
(-): sample without treatment (negative control); 42: heat shock at 42°C for five minutes (positive control); V16 and V32: vancomycin at the concentrations of 16 and 3 µg/ml, respectively.
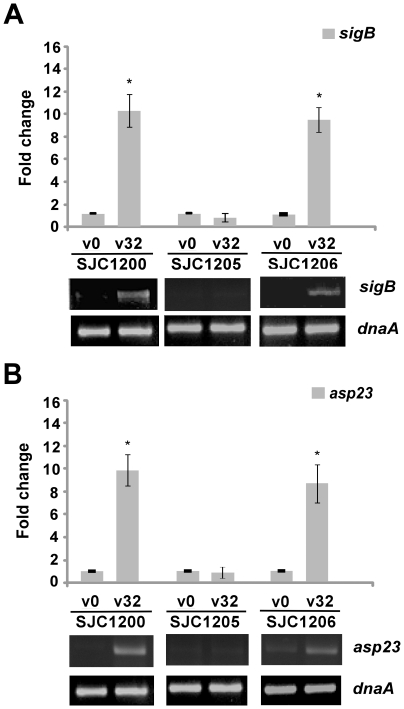
We next focused on the effects of vancomycin treatment on the expression of sigB using real-time qRT-PCR. It had been recommended that the appropriate therapeutic range of vancomycin concentrations in the serum is 15 to 20 µg/ml for through levels and 20 to 40 µg/ml for peak levels [25]. A recent study also indicated that 74% of heteroresistant VISA (hVISA) strains and 15% of wild-type S. aureus strains were tolerant to the effects of vancomycin (minimum bactericidal concentration of ≧ 32 µg/ml) [26]. Therefore, the maximum concentration of vancomycin used in our experiments was 32 µg/ml. Over the time course examined, the RT-PCR results showed that the peak expression of sigB and asp23 was five and 10 minutes after vancomycin treatment, respectively, and samples were collected for subsequent qRT-PCR assays at these time points (Fig. S1). The results shown in Fig. 2A indicate that the expression of sigB was significantly increased (10.2-fold) five minutes after vancomycin treatment. The transcription of sigB was not detected in SJC1205 (sigB-deficient strain) and was restored in SJC1206 (sigB-complemented strain). To further confirm the activation of σB, asp23 mRNA levels were quantified. Consistent with the expression of sigB, the expression of asp23 was significantly increased (9.8-fold) in strain SJC1200 10 minutes after vancomycin treatment, suggesting that σB was activated (Fig. 2B). The activation of asp23 was abolished in strain SJC1205 and was restored in SJC1206. Vancomycin-stimulated σB activation was also observed in VRSA strains derived from the strain COL and ATCC 49476 genetic backgrounds and in the VISA strain Mu50 at the concentrations of 32 and 4 µg/ml, respectively (data not shown).
Figure 2. Expression of sigB upon vancomycin treatment.
Changes in the transcription levels of the (A) sigB and (B) asp23 genes upon vancomycin treatment determined using qRT-PCR. Representative agarose gel electrophoresis images of RT-PCR assays are shown below the bar chart. V0 and V32: 0 and 32 µg/ml vancomycin, respectively. * P<0.05 compared to the untreated control cells.
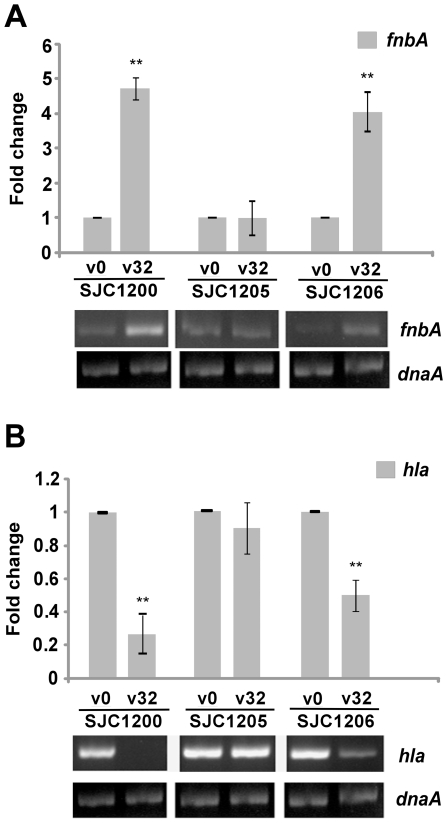
Effect of vancomycin on the expression of virulence-associated genes
The transcription of hla and fnbA mRNA over time in response to vancomycin treatment was investigated using RT-PCR. The greatest difference in the expression levels of fnbA and hla between drug-treated and untreated cells was observed one hour after vancomycin treatment, and this time point was used for further qRT-PCR assays (Fig. S2). A significant increase in the transcription level of fnbA (4.8-fold) was observed one hour after treatment of vancomycin in strain SJC1200. The increased fnbA expression was abolished in strain SJC1205 and was restored in SJC1206 (Fig. 3A). However, hla expression was significantly decreased (0.2-fold) after one hour of vancomycin treatment. The decreased hla expression was not observed in strain SJC1205 and was restored in SJC1206 (Fig. 3B).
Figure 3. Expression of virulence genes upon vancomycin treatment.
Changes in the transcription levels of (A) fnbA and (B) hla genes upon vancomycin treatment determined using qRT-PCR. Representative agarose gel electrophoresis images of RT-PCR assays are shown below the bar chart. * P<0.05 and ** P<0.005 compared to the untreated control cells.
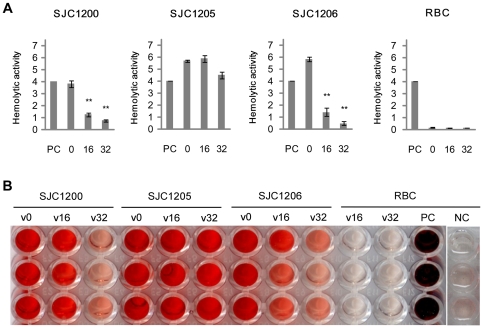
Effect of vancomycin on the hemolytic activity
The decreased hla expression suggests that the hemolytic activity of S. aureus is impaired following vancomycin treatment. A hemolytic assay measuring contact hemolysis was performed to evaluate the effect of vancomycin-induced σB activity on hemolysis. As expected, vancomycin treatment significantly suppressed hemolysis by strains SJC1200 and SJC1206 and mildly reduced hemolysis in the sigB-deficient strain SJC1205 (Fig. 4A and 4B).
Figure 4. Effect of vancomycin on hemolytic activity.
(A) Quantitative hemolytic unit. (B) Hemolysis was observed in a flat-bottom 96-well microtiter plate. Numerals shown on the figure represent the vancomycin concentration (µg/ml). PC: positive control; NC: negative control (erythrocyte suspensions without bacterial inoculation). ** P<0.005 compared to the untreated control cells.
Effect of vancomycin-induced σB activity on cytotoxicity
The pathogenicity of S. aureus involves the net expression of different exotoxins and cell wall components. Whether the vancomycin-induced σB activity affected S. aureus pathogenicity was investigated by a cytotoxicity assay. Because S. aureus is a major pathogen of the airway, cytotoxicity was evaluated in BEAS-2B cells using the MTT assay. When strains SJC1200 and SJC1206 were challenged with vancomycin, the cell viability was significantly decreased in a dose-dependent manner (Fig. 5A). The viability of BEAS-2B cells co-cultured with SJC1200 decreased to 74% (P<0.05) upon treatment with vancomycin at 16 µg/ml and further decreased to 57% (P<0.005) at 32 µg/ml. No considerable cytotoxicity was detected by challenging strain SJC1205 under the same conditions.
Figure 5. Effect of vancomycin-treated VRSA on the cytotoxicity.
Cytotoxicity toward BEAS-2B cells inoculated with S. aureus strains in the presence of different concentrations of vancomycin (A) without or (B) with polyclonal fibronectin antibodies. “Cell only” indicates cells cultured without bacteria to evaluate the cytotoxicity of vancomycin. “Ab+cell” indicates cells cultured with polyclonal fibronectin antibodies to evaluate the cytotoxicity of the antibodies. * P<0.05 and ** P<0.005 compared to the untreated control cells.
Vancomycin-enhanced fnbA expression suggests that the increased cytotoxicity may result from an increase in bacterial attachment to cells. A parallel cytotoxicity experiment was performed in which the target of fibronectin-binding proteins, fibronectin was blocked using antibodies. Vancomycin-enhanced cytotoxicity was abolished among all of the three strains in the presence of fibronectin antibodies (Fig. 5B). Cytotoxicity was not observed in control cells cultured with different concentrations of vancomycin or polyclonal fibronectin antibodies in the absence of bacteria (Fig. 5A and 5B).
Discussion
In the present study, we demonstrated that σB was activated when S. aureus was exposed to sub-inhibitory concentrations of antibiotics that target the cell wall (ampicillin and vancomycin) or SXT. In particular, we focused on the effects of vancomycin treatment on a VRSA strain. We demonstrated that vancomycin-stimulated σB is involved in the expression of virulence-associated genes and the increase in cytotoxicity. A recent study also indicated that the alternative sigma factor σE, which is responsible for the surface stress response, is activated by vancomycin in Mycobacterium tuberculosis [27].
We demonstrated that only the cell-wall active antibiotics and SXT acted as environmental stressors that induced σB transcription (Fig. 1). It has been reported that treatment with protein-suppressing agents may not cause significant differences in the expression of virulence factors in S. aureus [14], [15]. We propose that cell wall-targeting antibiotics and SXT trigger unknown receptors that induce σB activity. Activation of σB by vancomycin was observed in the SJC1200 strain (ATCC 12598 derivative), in the VISA strain Mu50, and in all of the tested VRSA strains derived from the strain COL and the ATCC 49476 genetic backgrounds (data not shown), suggesting that antibiotic-induced σB activity occurs frequently. Strain 12598 was chosen for subsequent studies because of its strong hemolysis and cytotoxicity in our previous study. DNA sequence analysis indicated that there were no mutations in the sigB operon of strain 12598 (data not shown).
Cheung and colleagues demonstrated the hyper-production of α-hemolysin in a sigB mutant, implying a negative effect of σB on hla expression [28]. Restoring σB activity to a σB-impaired strain decreased Hla expression [8]. Consistent with these findings, vancomycin-activated σB significantly suppressed hla expression, thereby reducing hemolysis. In addition to exotoxins such as hemolysins, cell wall-associated proteins, such as fibronectin-binding proteins (FnBPs), are important virulence determinants. The surface levels of FnBP were lower in a sigB-deficient strain, suggesting that σB regulates FnBP expression [29]. It has been shown that the increased expression of FnBPs is related to the diminished expression of Hla [30], [31]. Our results are consistent with previous findings in that increased fnbA transcription was associated with decreased hla. Thus, the interplay between σB activation and the expression of hla and fnbA is associated with vancomycin treatment. Although the expression of many virulence factors in S. aureus is regulated by the agr-mediated temporal and cell density-dependent regulatory pathways [9], vancomycin treatment still had a significant and immediate effect on the expression levels of virulence factors during the exponential growth phase (Fig. S2). The rapid activation of σB in response to vancomycin stress may force virulence expression through cell density-independent pathways. Generally speaking, the expression of fnbA was increased over time in sigB + strains with or without vancomycin treatment, whereas hla was increased up to two hours after vancomycin treatment (Fig. S2).
A striking finding of the present study is that σB was activated by cell wall-targeting antibiotics and SXT in drug-resistant S. aureus strains. This sigma factor may mediate the antibiotic-activated signal, as well as other environmental stresses, to downstream virulence determinants, leading to worse outcomes in the clinical environment. The results from the cytotoxicity assays reported herein reflect this concern. A significant decrease in cell viability upon administration of increased concentrations of vancomycin in the presence of drug-resistant S. aureus was observed (Fig. 5). Cytotoxicity induced by vancomycin was not observed when BEAS-2B cells were co-cultured with the sigB-deficient S. aureus strain SJC1205, suggesting the key role of σB in responding to antibiotic stress. The rapid increase in the prevalence of multidrug-resistant pathogenic bacteria and the appearance of resistant strains following continuous selective pressure suggest that improper antibiotic use may occur in the clinical environment. Such improper use may be the result of unsuitable initial antibiotic treatment, the development of drug-resistant strains during long-term selective pressure or inappropriate treatment following misdiagnosis. Regardless, antibiotic-enhanced pathogenicity makes subsequent treatment much more difficult. A recent study indicated that the highest mean steady-state concentrations of vancomycin for continuous and intermittent infusion regimens were 24.88±12.75 and 55.02±17.36 µg/ml, respectively, whereas the lowest concentrations were 19.89±10.15 and 12.43±12.86 µg/ml, respectively, in serum [32]. Concentrations are expected to be even lower in tissues. As a result, VISA strains could survive and enhance pathogenicity. Our results indicate that σB was activated in strain Mu50 after treatment with a lower concentration of vancomycin (4 µg/ml, data not shown), suggesting that the expression of σB-associated virulence genes might be altered.
The model strain used in the present study was derived from the ATCC 12598 (Cowan I) genetic background, which has been recognized as a protein A-overproducing and archetypal adherent strain. This strain is also known to lack a variety of exotoxins such as most staphylococcal enterotoxins, exfoliative toxins and toxic shock syndrome toxin 1 [33]. Strain ATCC 12598 is often used as a control strain in determining the invasive capacity and cytotoxicity of other strains. It has been demonstrated that FnBP expression is highly associated with the invasion of host cells, particularly during the study of ATCC 12598 [34]. Following vancomycin treatment, no obvious increase in exoprotein secretion by strain SJC1200 was observed by SDS PAGE analysis (data not shown), but there was a decrease in Hla expression. This result suggests that the cytotoxicity caused by SJC1200 was mainly due to the σB-activated cell wall components, possibly FnBPs, upon vancomycin treatment. A parallel study was performed using a VRSA strain derived from the strain COL genetic background, and similar cytotoxicity results were observed. Based on many studies, fnbA could have some role in invasion, but the overall cytotoxicity (cell invasion and damage) is governed by various toxins. Because SDS-PAGE is not a sensitive determinant of protein secretion, the expression of trace exoproteins stimulated by vancomycin may not be observable using a gel. In addition, BEAS-2B cells may not be the best model for analyzing virulence, particularly because they are less sensitive to Hla. However, the blockage of fibronectin by antibodies leading to subsequent reduction of cytotoxicity implies that vancomycin-enhanced bacterial attachment plays an important role in pathogenesis, at least in bronchial epithelial cells (Fig. 5B). The role of toxins underlying cytotoxicity after bacterial attachment and invasion needs to be investigated. Nevertheless, we propose that other σB-regulated exotoxins are overexpressed upon antibiotic treatment in other drug-resistant strains.
In conclusion, we hypothesize that sub-MICs of antibiotics may act as environmental stresses to activate the stress response sigma factor, σB. Although it has been reported that a number of virulence-associated genes are regulated by σB, the complexity of the downstream global regulatory pathways shows the diversity of virulence gene expression levels, not only within a single strain but also among different lineages. The pathogenicity of S. aureus will be the net effect of virulence-associated regulatory pathways and strain dependence. Although we cannot give a definitive warning about the antibiotic-triggered σB-associated virulence factor expression in pathogenic S. aureus because of strain variation, the risk should be taken into consideration.
Supporting Information
Evaluation of the expression levels of sigB and asp23 over time using RT-PCR. The agarose gel electrophoresis image shows the time course of the expression of sigB and asp23 in strains SJC1200, SJC1205, and SJC1206 without (V0) or with (V32) vancomycin treatment using RT-PCR.
(TIF)
Evaluation of the expression levels of fnbA and hla over time using RT-PCR. The agarose gel electrophoresis image shows the time course of the expression of fnbA and hla in strains SJC1200, SJC1205, and SJC1206 without (V0) or with (V32) vancomycin treatment using RT-PCR.
(TIF)
Acknowledgments
We thank the kind gift of bacterial strains from Network on Antimicrobial Resistance in Staphylococcus aureus (NARSA).
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was supported by the National Science Council of the Republic of China (Taiwan) (grant number NSC96-2320-B-182-014-MY3); and Research Program for Chang Gung Memorial Hospital (grant numbers CMRPD160411∼3), Taoyuan 333, Taiwan. The funder's website: http://web1.nsc.gov.tw/mp.aspx?mp=7 and http://www.cgmh.org.tw/eng2002/index.asp. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Hiramatsu K, Hanaki H, Ino T, Yabuta K, Oguri T, et al. Methicillin-resistant Staphylococcus aureus clinical strain with reduced vancomycin susceptibility. J Antimicrob Chemother. 1997;40:135–136. doi: 10.1093/jac/40.1.135. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Staphylococcus aureus resistant to vancomycin—United States, 2002. Morb Mortal Wkly Rep. 2002;51:565–567. [PubMed] [Google Scholar]
- 3.Weigel LM, Clewell DB, Gill SR, Clark NC, McDougal LK, et al. Genetic analysis of a high-level vancomycin-resistant isolate of Staphylococcus aureus. Science. 2003;302:1569–1571. doi: 10.1126/science.1090956. [DOI] [PubMed] [Google Scholar]
- 4.Hsueh PR, Lee SY, Perng CL, Chang TY, Lu JJ. Clonal dissemination of meticillin-resistant and vancomycin-intermediate Staphylococcus aureus in a Taiwanese hospital. Int J Antimicrob Agents. 2010;36:307–312. doi: 10.1016/j.ijantimicag.2010.06.035. [DOI] [PubMed] [Google Scholar]
- 5.van Schaik W, Abee T. The role of σB in the stress response of Gram-positive bacteria – targets for food preservation and safety. Curr Opin Biotechnol. 2005;16:218–224. doi: 10.1016/j.copbio.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 6.Pane-Farre J, Jonas B, Forstner K, Engelmann S, Hecker M. The σB regulon in Staphylococcus aureus and its regulation. Int J Med Microbiol. 2006;296:237–258. doi: 10.1016/j.ijmm.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 7.Nielsen JS, Christiansen MH, Bonde M, Gottschalk S, Frees D, et al. Searching for small σB-regulated genes in Staphylococcus aureus. Arch Microbiol. 2011;193:23–34. doi: 10.1007/s00203-010-0641-1. [DOI] [PubMed] [Google Scholar]
- 8.Horsburgh MJ, Aish JL, White IJ, Shaw L, Lithgow JK, et al. σB modulates virulence determinant expression and stress resistance: characterization of a functional rsbU strain derived from Staphylococcus aureus 8325-4. J Bacteriol. 2002;184:5457–5467. doi: 10.1128/JB.184.19.5457-5467.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheung AL, Bayer AS, Zhang G, Gresham H, Xiong YQ. Regulation of virulence determinants in vitro and in vivo in Staphylococcus aureus. FEMS Immunol Med Microbiol. 2004;40:1–9. doi: 10.1016/S0928-8244(03)00309-2. [DOI] [PubMed] [Google Scholar]
- 10.Lorenz U, Huttinger C, Schafer T, Ziebuhr W, Thiede A, et al. The alternative sigma factor σB of Staphylococcus aureus modulates virulence in experimental central venous catheter-related infections. Microbes Infect. 2008;10:217–223. doi: 10.1016/j.micinf.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Lorian V. Medical relevance of low concentrations of antibiotics. J Antimicrob Chemother 31. 1993. pp. 137–148. [DOI] [PubMed]
- 12.Stevens DL, Ma Y, Salmi DB, McIndoo E, Wallace RJ, et al. Impact of antibiotics on expression of virulence-associated exotoxin genes in methicillin-sensitive and methicillin-resistant Staphylococcus aureus. J Infect Dis. 2007;195:202–211. doi: 10.1086/510396. [DOI] [PubMed] [Google Scholar]
- 13.Gerber M, Walch C, Loffler B, Tischendorf K, Reischl U, et al. Effect of sub-MIC concentrations of metronidazole, vancomycin, clindamycin and linezolid on toxin gene transcription and production in Clostridium difficile. J Med Microbiol. 2008;57:776–783. doi: 10.1099/jmm.0.47739-0. [DOI] [PubMed] [Google Scholar]
- 14.Ohlsen K, Ziebuhr W, Koller KP, Hell W, Wichelhaus TA, et al. Effects of subinhibitory concentrations of antibiotics on α-toxin (hla) gene expression of methicillin-sensitive and methicillin-resistant Staphylococcus aureus isolates. Antimicrob Agents Chemother. 1998;42:2817–2823. doi: 10.1128/aac.42.11.2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernardo K, Pakulat N, Fleer S, Schnaith A, Utermohlen O, et al. Subinhibitory concentrations of linezolid reduce Staphylococcus aureus virulence factor expression. Antimicrob Agents Chemother. 2004;48:546–555. doi: 10.1128/AAC.48.2.546-555.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koszczol C, Bernardo K, Kronke M, Krut O. Subinhibitory quinupristin/dalfopristin attenuates virulence of Staphylococcus aureus. J Antimicrob Chemother. 2006;58:564–574. doi: 10.1093/jac/dkl291. [DOI] [PubMed] [Google Scholar]
- 17.Schenk S, Laddaga RA. Improved method for electroporation of Staphylococcus aureus. FEMS Microbiol Lett. 1992;73:133–138. doi: 10.1016/0378-1097(92)90596-g. [DOI] [PubMed] [Google Scholar]
- 18.Arnaud M, Chastanet A, Debarbouille M. New vector for efficient allelic replacement in naturally nontransformable, low-GC-content, gram-positive bacteria. Appl Environ Microbiol. 2004;70:6887–6891. doi: 10.1128/AEM.70.11.6887-6891.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bae T, Schneewind O. Allelic replacement in Staphylococcus aureus with inducible counter-selection. Plasmid. 2006;55:58–63. doi: 10.1016/j.plasmid.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 20.Gertz S, Engelmann S, Schmid R, Ohlsen K, Hacker J, et al. Regulation of σB-dependent transcription of sigB and asp23 in two different Staphylococcus aureus strains. Mol Gen Genet. 1999;261:558–566. doi: 10.1007/s004380051001. [DOI] [PubMed] [Google Scholar]
- 21.CLSI Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. 2009. Approved standard, M07-A8 ed. Wayne, PA: CLSI.
- 22.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 23.Bernheimer AW. Assay of hemolytic toxins. Methods Enzymol. 1988;165:213–217. doi: 10.1016/s0076-6879(88)65033-6. [DOI] [PubMed] [Google Scholar]
- 24.Mosmann T. Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods. 1983;65:55–63. doi: 10.1016/0022-1759(83)90303-4. [DOI] [PubMed] [Google Scholar]
- 25.Rybak M, Lomaestro B, Rotschafer JC, Moellering R, Jr, Craig W, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm. 2009;66:82–98. doi: 10.2146/ajhp080434. [DOI] [PubMed] [Google Scholar]
- 26.Jones RN. Microbiological features of vancomycin in the 21st century: minimum inhibitory concentration creep, bactericidal/static activity, and applied breakpoints to predict clinical outcomes or detect resistant strains. Clin Infect Dis. 2006;42(Suppl 1):S13–24. doi: 10.1086/491710. [DOI] [PubMed] [Google Scholar]
- 27.Provvedi R, Boldrin F, Falciani F, Palu G, Manganelli R. Global transcriptional response to vancomycin in Mycobacterium tuberculosis. Microbiology. 2009;155:1093–1102. doi: 10.1099/mic.0.024802-0. [DOI] [PubMed] [Google Scholar]
- 28.Cheung AL, Chien YT, Bayer AS. Hyperproduction of α-hemolysin in a sigB mutant is associated with elevated SarA expression in Staphylococcus aureus. Infect Immun. 1999;67:1331–1337. doi: 10.1128/iai.67.3.1331-1337.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li D, Renzoni A, Estoppey T, Bisognano C, Francois P, et al. Induction of fibronectin adhesins in quinolone-resistant Staphylococcus aureus by subinhibitory levels of ciprofloxacin or by σB transcription factor activity is mediated by two separate pathways. Antimicrob Agents Chemother. 2005;49:916–924. doi: 10.1128/AAC.49.3.916-924.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vann JM, Proctor RA. Cytotoxic effects of ingested Staphylococcus aureus on bovine endothelial cells: role of S. aureus α-hemolysin. Microb Pathog. 1988;4:443–453. doi: 10.1016/0882-4010(88)90029-0. [DOI] [PubMed] [Google Scholar]
- 31.Vaudaux P, Francois P, Bisognano C, Kelley WL, Lew DP, et al. Increased expression of clumping factor and fibronectin-binding proteins by hemB mutants of Staphylococcus aureus expressing small colony variant phenotypes. Infect Immun. 2002;70:5428–5437. doi: 10.1128/IAI.70.10.5428-5437.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jaruratanasirikul S, Julamanee J, Sudsai T, Saengsuwan P, Jullangkoon M, et al. Comparison of continuous infusion versus intermittent infusion of vancomycin in patients with methicillin-resistant Staphylococcus aureus. J Med Assoc Thai. 2010;93:172–176. [PubMed] [Google Scholar]
- 33.Becker K, Roth R, Peters G. Rapid and specific detection of toxigenic Staphylococcus aureus: use of two multiplex PCR enzyme immunoassays for amplification and hybridization of staphylococcal enterotoxin genes, exfoliative toxin genes, and toxic shock syndrome toxin 1 gene. J Clin Microbiol. 1998;36:2548–2553. doi: 10.1128/jcm.36.9.2548-2553.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sinha B, Francois P, Que YA, Hussain M, Heilmann C, et al. Heterologously expressed Staphylococcus aureus fibronectin-binding proteins are sufficient for invasion of host cells. Infect Immun. 2000;68:6871–6878. doi: 10.1128/iai.68.12.6871-6878.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Flannagan SE, Chow JW, Donabedian SM, Brown WJ, Perri MB, et al. Plasmid content of a vancomycin-resistant Enterococcus faecalis isolate from a patient also colonized by Staphylococcus aureus with a VanA phenotype. Antimicrob Agents Chemother. 2003;47:3954–3959. doi: 10.1128/AAC.47.12.3954-3959.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin TP, Chen CL, Chang LK, Tschen JS, Liu ST. Functional and transcriptional analyses of a fengycin synthetase gene, fenC, from Bacillus subtilis. J Bacteriol. 1999;181:5060–5067. doi: 10.1128/jb.181.16.5060-5067.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Evaluation of the expression levels of sigB and asp23 over time using RT-PCR. The agarose gel electrophoresis image shows the time course of the expression of sigB and asp23 in strains SJC1200, SJC1205, and SJC1206 without (V0) or with (V32) vancomycin treatment using RT-PCR.
(TIF)
Evaluation of the expression levels of fnbA and hla over time using RT-PCR. The agarose gel electrophoresis image shows the time course of the expression of fnbA and hla in strains SJC1200, SJC1205, and SJC1206 without (V0) or with (V32) vancomycin treatment using RT-PCR.
(TIF)