Abstract
Prion diseases have been observed to deregulate the transcription of erythroid genes, and prion protein knockout mice have demonstrated a diminished response to experimental anemia. To investigate the role of the cellular prion protein (PrPC) in erythropoiesis, we studied the protein's expression on mouse erythroid precursors in vivo and utilized an in vitro model of the erythroid differentiation of murine erythroleukemia cells (MEL) to evaluate the effect of silencing PrPC through RNA interference.
The expression of PrPC and selected differentiation markers was analyzed by quantitative multicolor flow cytometry, western blot analysis and quantitative RT-PCR. The silencing of PrPC expression in MEL cells was achieved by expression of shRNAmir from an integrated retroviral vector genome. The initial upregulation of PrPC expression in differentiating erythroid precursors was detected both in vivo and in vitro, suggesting PrPC's importance to the early stages of differentiation. The upregulation was highest on early erythroblasts (16200±3700 PrPC / cell) and was followed by the gradual decrease of PrPC level with the precursor's maturation reaching 470±230 PrPC / cell on most mature CD71−Ter119+ small precursors. Interestingly, the downregulation of PrPC protein with maturation of MEL cells was not accompanied by the decrease of PrP mRNA. The stable expression of anti-Prnp shRNAmir in MEL cells led to the efficient (>80%) silencing of PrPC levels. Cell growth, viability, hemoglobin production and the transcription of selected differentiation markers were not affected by the downregulation of PrPC.
In conclusion, the regulation of PrPC expression in differentiating MEL cells mimics the pattern detected on mouse erythroid precursors in vivo. Decrease of PrPC protein expression during MEL cell maturation is not regulated on transcriptional level. The efficient silencing of PrPC levels, despite not affecting MEL cell differentiation, enables created MEL lines to be used for studies of PrPC cellular function.
Introduction
The cellular prion protein (PrPC) is expressed in cells of various origins. It is conserved through the whole vertebrae class, suggesting its importance in cellular physiology[1]. However, its role in physiological processes remains enigmatic although PrPC plays a basic role in the pathogenesis of the fatal neurodegenerative disorders known as Transmissible Spongiform Encephalopathies. Observation of PrPC deficient mice (PrP−/−) did not reveal significant health problems. On the other hand, experiments in cell cultures suggested that PrPC is linked to such processes as the prevention of apoptosis, copper metabolism linked to oxidative stress, iron metabolism, signalization and differentiation[2], [3], [4]. A connection between prion pathogenesis and erythropoiesis was suggested by the downregulation of the α-hemoglobin stabilizing protein (AHSP) mRNA during prion disease[5]. A later study indicated that the disease progression affected the transcription of several other murine erythroid genes, e.g., Kell, GPA, band 3 and ankyrin[6]. A link between PrPC expression and erythropoiesis was also demonstrated in PrP−/− mice after the experimental induction of hemolytic anemia. Upon treatment with phenylhydrazine, PrP−/− mice produced fewer reticulocytes than did PrP+/+ mice. This result was probably due to the reduced level of erythropoietin production and higher percentage of apoptotic erythroid precursors[7]. Apparently, the expression of PrPC is generally important in hematopoiesis. PrPC is present on the surface of mouse long-term hematopoietic stem cells (LT-HSCs) and supports their self-renewal and engraftment during serial transplantation. Quantitatively, 40% of mouse bone marrow (BM) cells express PrPC, and, from this population of cells, 80% are erythroid cells[8]. CD34+ human bone marrow stem cells also express PrPC [9], [10], and circulating human and mouse red blood cells have similarly low levels of PrPC on their cellular membranes[11], [12]. A widely used model for the study of erythroid differentiation in vitro is presented by murine erythroleukemia (MEL) cells. MEL cells are blocked at the proliferative proerythroblast stage, and, after the addition of polar substances, e.g., hexamethylene bisacetamide (HMBA), they lose their proliferative capacity and enter cell-cycle arrest. This process is characterized by structural (decreased cell volume and nuclear condensation) and biochemical changes (activation of erythroid genes, hemoglobin accumulation), which resemble those exhibited by natural erythroid differentiation[13]. Gougoumas and colleagues demonstrated transcriptional activation at the mRNA level of the PrP gene in growth-arrested MEL cells[14]. Our study extends their observations by demonstrating divergences in the regulation of PrPC at the protein and mRNA levels during inducer-mediated erythroid differentiation and cell-growth arrest caused by confluency. In addition, we exploited MEL cell lines with stably downregulated levels of PrPC to study its importance in the differentiation of MEL cells.
Results
Regulation of PrPCexpression on mouse bone marrow and spleen erythroid precursors
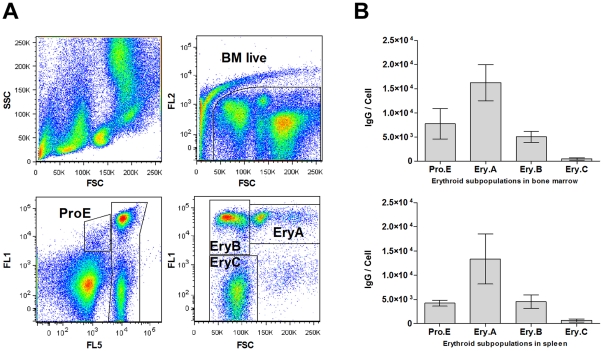
Erythroid precursors were gated according their Ter119 and CD71 signals and the forward scatter (FSC) signals to the proE, EryA, EryB and EryC subpopulations (Fig. 1 A). CD71+Ter119+/− bone marrow proerythroblasts (proE) expressed 7800±3100 PrPC molecules / cell, assuming that one molecule of mAb AH6 binds one molecule of PrPC. The expression of CD71+Ter119+ basophilic erythroblasts (EryA) was elevated to 16200±3700 PrPC / cell and decreased in late basophilic and polychromatic erythroblasts (EryB) to 5100±1100 PrPC / cell and was also diminished in late CD71−Ter119+ small precursors (EryC) (470±230 PrPC / cell). Corresponding erythroid precursors in the spleen expressed 4200±600, 13400±5200, 4600±1400 and 680±280 PrPC / cell, respectively (Fig. 1 B).
Figure 1. The expression of PrPC on mouse bone marrow (BM) and spleen erythroid precursors is upregulated in early erythroblasts and, then, decreases with the cells' maturation.
(A) Gating strategy for erythroid precursors: upper left - scattergram of BM cells; upper right – gating of viable 7-AAD negative cells (BM live); lower left – live BM cells labeled with CD71-FITC (FL1) and Ter119-eFluor450 (FL5): ProE - CD71+Ter119+/− proerythroblasts; Ter119+ cells were further gated on CD71-FITC (FL1) and FSC plot (lower right): EryA - large CD71+ early basophilic erythroblasts, EryB - small CD71+ late basophilic and polychromatic erythroblasts, EryC - small CD71- orthochromatic erythroblasts and reticulocytes. (B) Quantitative FACS analysis of PrPC expression on erythroid precursors in mouse bone marrow and spleen. Expression of PrPC on early basophilic erythroblasts (EryA) is significantly higher (p>0.005, n = 5) in comparison with proerythroblasts (ProE), both in BM (upper) and spleen (lower). The initial increase of expression is followed by its decrease on late basophilic and polychromatic erythroblasts (EryB), and most mature small precursors (EryC) express a low number of PrPC. Quantification is based on assumption that one IgG molecule of MAb AH6 binds to one molecule of PrPC.
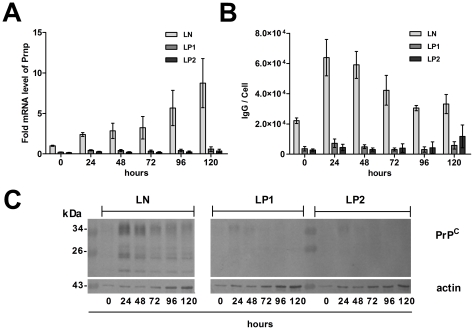
Regulation of PrPC expression during the erythroid differentiation of MEL cells
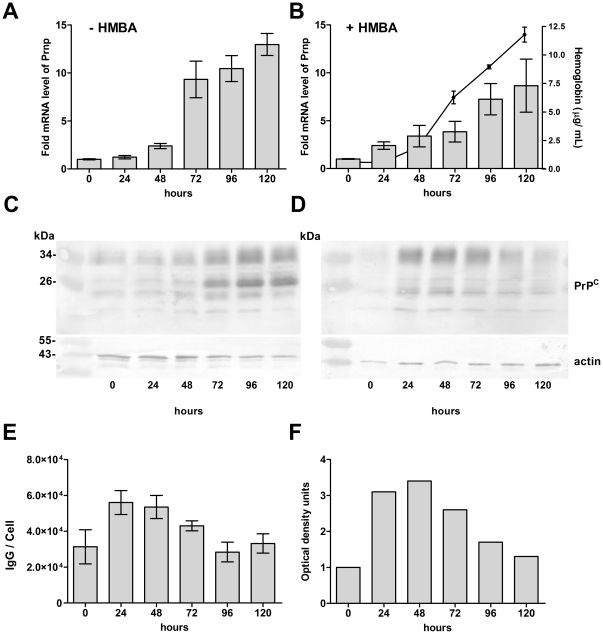
MEL cells were grown for five days in the absence or presence of 5 mM HMBA. The cells increased their expression of Prnp mRNA, reaching 13±1.2 -fold and 8.7±2.8-fold relative expression after 120 hours in uninduced and differentiating cells, respectively (Fig. 2 A and B). While the level of PrP mRNA in the differentiating cells more than doubled within 24 h after induction, a similar increase in the uninduced cells was observed after 48 h in culture when cells were reaching confluency. At the protein level, the uninduced cells increased their PrPC, reaching a maximum expression in confluent culture at 96–120 h (Fig. 2C) which correlated with the expression of Prnp mRNA. In contrast, the expression of the PrPC protein in differentiating cells peaked at 24–48 h post-induction (Fig. 2D) with a subsequent decrease to almost its basal level at 120 h, as demonstrated by densitometry (Fig. 2F). The increased density of the PrPC band on the WB was already visible within 6 h post-induction (not shown). These results were confirmed by quantitative FACS analysis, which demonstrated approximately twofold increase of PrPC membrane expression after 24 h of differentiation, with a subsequent return to the basal level after 96 h (Fig. 2E).
Figure 2. Initial increase of PrPC protein expression in differentiating MEL cells is followed by its downregulation.
(A) Transcriptional activation of the Prnp gene in uninduced MEL cells (- HMBA) correlates with growth arrest in confluent culture at 72 h, as demonstrated by qRT-PCR. A similar, but lower, increase of PrP mRNA is seen in cells induced to erythroid differentiation (+ HMBA) (B). Progress of cell differentiation is monitored by overall hemoglobin level (full line, n = 2, mean ± SD). The amount of PrPC protein on western blots (WB) in uninduced cells (C) correlates with the level of mRNA (A). In contrast, the amount of PrPC protein in differentiating cells (D) is highest 24–48 h after induction and, then, is downregulated, as shown by densitometry (F), despite the level of PrP mRNA continues to rise (B). Blots were developed with a mix of PrPC mAbs (AH6, AG4, 6H4) and actin antibody was used as a loading control. Surface expression of PrPC on HMBA induced differentiating MEL cells (number of mAb AH6 IgG molecules / cell) measured by quantitative flow cytometry (E) correlates with the levels detected by WB (F) (n = 2, means ± range).
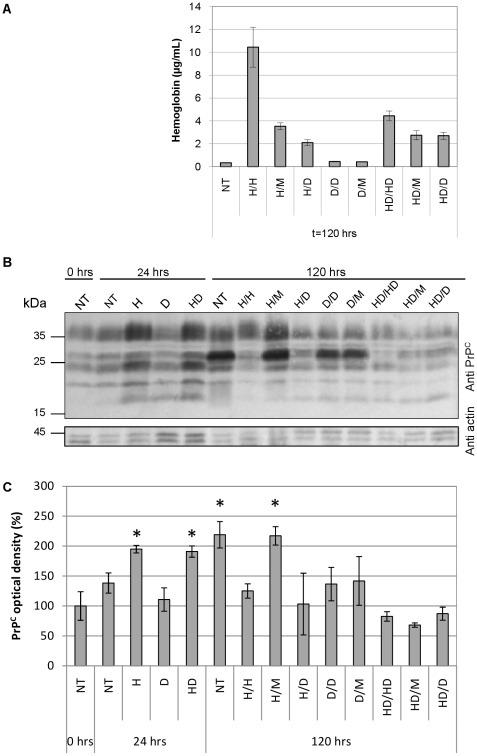
Dexamethasone treatment of MEL cells lowers their expression of PrPC in confluent culture irrespective of production of hemoglobin
Induction of MEL cell differentiation by incubation with HMBA for 24 h with their subsequent incubation in the media without HMBA (H/M), or the inclusion of 4 µM dexamethasone in the medium with HMBA (HD/HD), both led to a comparable (∼60%) reduction of MEL cells hemoglobinization after 120 h of culture (Fig. 3 A). The H/M treatment was connected with the significant increase of PrPC level (∼220%) at 120 h comparable to the increase recorded in non-differentiated confluent cells (NT) (Fig. 3 B, C). At the other hand, HD/HD treatment led to low PrPC level (∼80%), lower than in differentiated fully hemoglobinized MEL cells (H/H). Treatment of MEL cells with up to 40 µM dexamethasone did not influence the initial up-regulation of PrPC in HMBA stimulated cells 24 h post induction, but generally led to lower PrPC levels in comparison with NT cells after 120 h in culture (Fig. 3 B, C). Interestingly, induction of PrPC expression in growth-arrested confluent culture led to a different PrP western blot pattern with predominant ∼26 kDa band which is much less present in both, fully differentiated or actively dividing MEL cells (Fig. 3 B). The detected changes in the levels of PrPC were not caused by differences in gel loading, as demonstrated by actin labeling.
Figure 3. The initial upregulation of PrPC expression after the induction of MEL cells' differentiation by HMBA is not affected by dexamethasone.
(A) Hemoglobin levels 120 hrs post induction of MEL cells differentiation. Cells were treated with HMBA (H), Dexamethasone (D) or the combination thereof (HD). After 24 hrs media were exchanged and the treatment continued, or was changed for different one as shown on x-axis labels (M stands for DMEM medium only). Non-treated (NT) control represents cells kept in DMEM only. Cell lysates were normalized to the total protein content (measured by BCA assay) and hemoglobin was quantified by TMB assay. (B) Western blot analysis of PrPC expression. Samples were harvested after 24 and 120 hrs treatments described above. NT control at 0 hrs represents the initial conditions of MEL culture before treatment. The gel loading was normalized to the total protein content (measured by BCA assay) and controlled by actin staining. The blot is a representative of three independent experiments. (C) Quantification of the PrPC level on western blots by densitometry. Graph columns represent the average density of PrPC bands and error bars represent the standard deviations; PrPC expression level of NT control at 0 hrs was set as 100% (*p<0.05, n = 3).
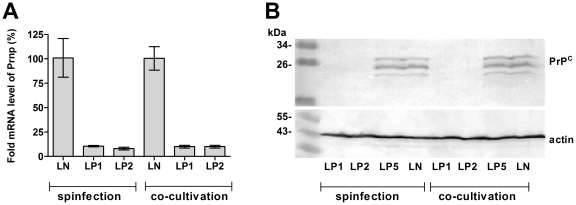
Retroviral vector delivery of anti-Prnp shRNAmir leads to stable and efficient PrPC silencing
Both spinfection and co-cultivation methods led to efficient (∼90%) silencing of PrPC at the mRNA (Fig. 4 A) and protein levels (Fig. 4 B) by LP1 and LP2 constructs in comparison with control construct LN. The LP5 construct did not produce any downregulation of PrPC levels (Fig. 4 B). Retroviral infection of cells did not induce cell-protective effects, as demonstrated by qRT-PCR analysis of chosen interferon-stimulating genes Oas1a, Rnase1 and Eif2ak2 (not shown). The silencing of PrPC in LP1 and LP2 lines was stable during the course of HMBA-induced cell differentiation (Fig 5). In comparison with LN, LP1- and LP2-transduced cells exhibited 79% and 84% inhibition of Prnp mRNA expression at the beginning of differentiation and 93% and 96% after 120 h of differentiation, respectively (Fig. 5 A). The levels of Prnp mRNA and protein during differentiation of the control LN-transduced cells (Fig. 5 A, C) was upregulated similarly as in non-manipulated MEL cells (Fig. 2 B, D). The stability of PrPC silencing was confirmed by quantitative FACS analysis, which demonstrated downregulation of PrPC at the cell membrane ranging from 17% (LP1) and 12% (LP2) to 8% (LP1) and 5% (LP2) of its expression (100%) in LN-transduced cells at the beginning of differentiation and after 48 h, respectively (Fig. 5 B). These results were confirmed by western blot analysis in which we could faintly detect PrPC in LP1 and LP2 cells only after 24 hours, while the protein in LN-transduced cells was readily detected (Fig. 5 C).
Figure 4. Downregulation of PrPC expression by RNAi in MEL cells after selection with puromycin.
(A) Both methods of retroviral vector delivery led to ∼90% silencing of Prnp mRNA in both lines expressing anti-Prnp shRNAmir (LP1 and LP2) when compared with the MEL line expressing nonsilencing shRNAmir (LN), as depicted by qRT-PCR. (B) Confirmation of PrPC downregulation in LP1- and LP2-transduced cells at the protein level by western blot. PrPC was detected by mAb AH6. No silencing was observed in LP5 cell line. Actin was used as a loading control.
Figure 5. Expression of PrPC is stably repressed during the differentiation of MEL cells.
(A) Level of PrP mRNA measured with qRT-PCR in cell lines stably expressing anti-Prnp shRNAmir (LP1 and LP2) is downregulated in comparison with control (LN) during the course of cell differentiation (2 experiments, mean ± SD). (B) The effect of silencing on the level of PrPC on cell membrane estimated by quantitative flow cytometry (four experiments, mean ± SD. (C) Confirmation of stable PrPC silencing on the protein level by western blot. PrPC was detected by mAb mix AH6, AG4 and 6H4. Actin was used as a loading control.
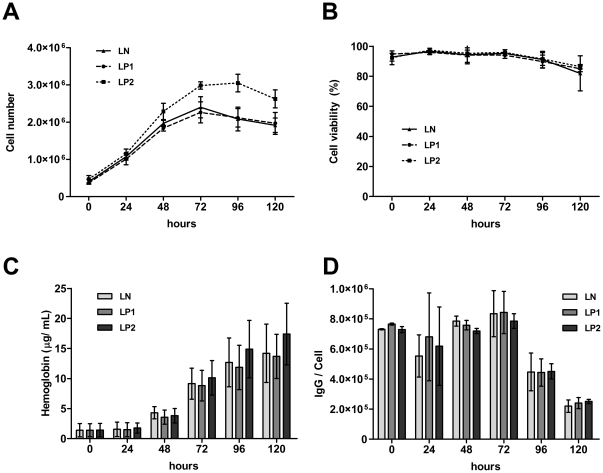
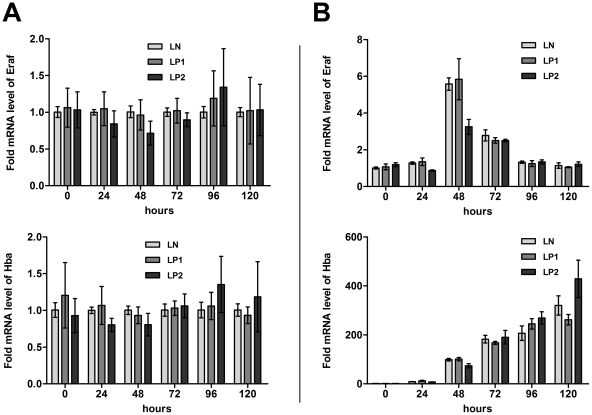
Silencing of the Prnp gene by RNAi does not affect HMBA-induced differentiation of MEL cells
Cell numbers in differentiating LN and LP1 lines increased similarly, reaching 2.4×106 cells/mL at 72 h. The LP2-transduced cell line produced slightly more cells, with a maximum of 3.0×106 cells/mL at 72 h (Fig. 6 A). In a Trypan Blue exclusion assay, all cell lines demonstrated a similar viability (∼94%) over a 72-h post-induction period and, also, a similar slight decrease of viability after 96 and 120 h (Fig. 6 B). We did not detect any differences in the transcriptional levels of proapoptotic Bax (not shown). The dynamic of hemoglobin production was comparable in all cell lines, irrespective of the level of PrPC (Fig. 6 C). Similarly, surface expression of the transferrin receptor (CD71) was similarly regulated in all cell lines (Fig. 6 D). Also, no difference was demonstrated in the levels of c-myb mRNA, which were downregulated approximately eightfold after 24 h post-induction in all lines. After 48 h, c-myb mRNA was downregulated to ∼2% of the starting level and remained silenced until the end of the experiment (not shown). Similarly, monitoring of the erythroid markers Eraf and Hba (Fig. 7A and B) and GATA-1 (not shown) during the differentiation of cells at the transcriptional level indicated analogous expression in all lines, irrespective of PrPC levels.
Figure 6. Differentiating MEL cells display similar characteristics irrespective to the level of PrPC expression.
(A) Growth curves of LP1, LP2 and control LN lines during erythroid differentiation induced by HMBA. (B) Cell viability based on a Trypan Blue exclusion assay. (C) Concentration of total hemoglobin in the cells per 100 µg/mL of total cell proteins. (D) Number of CD71 (transferrin receptor) molecules per cell, analyzed by quantitative flow cytometry, based on assumption that one anti- CD71-PE mAb binds one molecule of transferrin receptor.
Figure 7. Transcriptional levels of selected erythroid markers in differentiating MEL cells indicate a similar pattern, irrespective to PrP silencing.
(A) Expression of Eraf (α-hemoglobin stabilizing protein) and Hba (Hemoglobin α) in LP1- and LP2-transduced cells was compared with the level in the control LN-transduced cell line on individual days, as measured by qRT-PCR (n = 4, mean ± SD). (B) Representative pattern of Eraf and Hba expression during differentiation. The level of expression in individual days was normalized to the level in the LN-transduced cell line in day 0.
Discussion
The role of PrPC in cellular physiology has been proposed for a variety of processes, but with no prevailing consensus to date[1]. The downregulation of erythroid genes during prion infection has established a link between the peripheral pathogenesis of prion diseases and erythropoiesis. However, it is not clear if the effect is caused by direct interaction of prion particles with erythroid cells or if it is triggered by some yet unknown humoral response to the infection. The expression of PrPC on circulating red blood cells (RBCs) of closely related nonhuman primates varies from several thousand per cell to zero[15], implying that its function on mature erythrocytes is not conserved. Griffiths et al. demonstrated the regulation of PrPC expression during the differentiation of cultured human erythroblasts in vitro, indicating that it may play a role in the differentiation of erythroid precursors. PrPC was found mostly in the perinuclear region of proerythroblasts, and the amount of PrPC declined as erythroid cells matured[16]. Human and mouse RBCs express approximately 200 PrPC molecules per cell[11], suggesting a similar regulation of its expression in the erythroid lineage in both species. In this study, we demonstrated that the surface expression of PrPC on erythroid precursors in the mouse bone marrow and spleen follows a similar pattern as the cells mature. The protein's levels first increase with basophilic erythroblasts, expressing more than twice as much PrPC as proerythroblasts, and then declines significantly in late basophilic and polychromatic erythroblasts, with most mature small erythroid precursors expressing only around 500 PrPC molecules per cell. This pattern of expression is suggestive of PrPC's involvement in the early stages of erythroid differentiation. The differentiation of MEL cells in culture is known to resemble the in vivo process, with similar maturation stages: proerythroblast-like, erythroblasts-like and, occasionally, reticulocyte-like[16], [17]. The surface expression of PrPC on uninduced MEL cells in the exponential phase of growth was approximately six times higher than that observed on proerythroblasts in the mouse bone marrow or spleen. However, the induction of differentiation led to nearly doubling of the PrPC number on MEL cell membranes within 24 h, which resembled a similar increase of PrPC expression on basophilic erythroblasts in vivo. In agreement with previous observations in vivo, we found that this initial upregulation was followed by a gradual downregulation of PrPC surface levels along with the progression of MEL cells' differentiation. This decrease did not reach the degree observed in small CD71-Ter119+ erythroid precursors in vivo, which is in line with the limited ability of differentiating MEL cells to reach this stage of maturation. The differentiation of MEL cells is composed of two separate events, growth arrest and terminal differentiation. Both processes are characterized by the activation of early (cell-cycle control) and late (morphological changes) genes[17]. The first period lasts approximately 12 hours, after which the first committed cells materialize. The majority of cells are terminally differentiated between 24 and 50 h[18]. In agreement with previous studies by Gougomas et al.[14], we found that the Prnp gene in MEL cells is transcriptionally activated both during inducer-mediated differentiation and in confluent cells undergoing cell-cycle arrest. In addition, we were able to demonstrate the regulation of PrPC at the protein level by western blot. Interestingly and in accordance with the flow cytometry results, in differentiating cells, the expression of the protein was downregulated after an initial increase, even though the level of PrP mRNA continued to rise. This result suggests that MEL cells' differentiation leads to a translational regulation of PrPC levels[19] not seen in uninduced cells undergoing cell-cycle arrest. Alternatively, more differentiated cells could degrade PrPC at an increased rate, as has been proposed to explain the disparity between PrP protein and mRNA levels in different types of neuronal cells[20]. The downregulation of PrPC protein during the differentiation of highly responsive subclones of MEL cells was recently reported by Otsuka et al.[21]; however, their study did not detect an initial increase of PrPC expression, most likely due to the different status of cells at the point of induction. Stimulation of the glucocorticoid receptor by dexamethasone induces the proliferation and expansion of erythroid progenitors and delays the terminal differentiation of erythrocytes[22]. In our hands, dexamethasone did not prevent the HMBA-induced initial upregulation of PrPC in MEL cells, suggesting that it precedes the effect of dexamethasone, which is known to suppress the HMBA-mediated commitment to terminal cell division at a relatively late step in this process[23]. However, dexamethasone prevented the increase of PrPC protein levels in confluent MEL cells after 120 h of culture, demonstrating that the activation of the glucocorticoid receptor can interfere with the transcriptional activation of the Prnp gene mediated by cell-cycle arrest. The mechanism of dexamethasone's action on the prevention PrPC protein upregulation in confluent MEL cells is unknown at present. Dexamethasone has been shown to induce cell-cycle arrest in number of various cell lines[24], but not in MEL cells, in which it increases cell viability[25], both in induced and uninduced culture. In summary, our results demonstrate that the regulation of PrPC levels in differentiating MEL cells resembles, at least in part, its regulation in maturing mouse erythroid precursors in vivo. To learn more about the importance of PrPC in the process of MEL cells' differentiation, we created cell lines using RNAi to stably inhibit expression of the protein. RNAi administered by shRNA from a retrovector had previously been employed efficiently to inhibit PrPC expression in vitro and in vivo [26], [27]. The main objective for using RNAi to suppress PrPC was to study its therapeutic potential in preventing propagation of infectious prions. To the best of our knowledge, our model is the first murine cell line of non-neuronal origin with stably silenced PrPC expression. Inhibition of the protein's expression at both the mRNA and protein levels was efficiently maintained during the differentiation of MEL cells, although it varied between 75 and 95% in individual time points. Despite the silencing, the induction of differentiation led to a detectable increase of PrPC signal on blots after 24 h, suggesting that the regulation of the protein's expression in LP1- and LP2-transduced cell lines follows similar pattern as in unmodified MEL cells, although at a suppressed level. Growth curve and viability of LP1-, LP2- and control LN-transduced cell lines after the induction of differentiation was similar, although the LP2-transduced cell line exhibited a higher proliferation capacity. Since the LP1-transduced cell line did not differ from control LN-transduced cell line, we could not assign the LP2-transduced cell line's divergence solely to PrPC silencing. All cell lines observed here demonstrated similar dynamics and level of hemoglobinization and regulation of the transferrin receptor on their cell membranes. This finding suggested that silencing of PrPC in MEL cells does not lead to gross perturbation of iron homeostasis, although the involvement of PrPC in iron-cell uptake was described recently[28], [29]. Similarly, the level of the protooncogene c-myb, expression of which is characteristic of the proliferative state and has been demonstrated to block MEL cells' differentiation[30], [31], decreased upon induction similarly in all created cell lines and remained low during the entire course of the experiment. Monitoring of selected erythroid markers (AHSP, Hba and GATA-1) on the transcriptional level also did not reveal significant differences among LP1-transduced, LP2-transduced and LN-transduced cell lines, confirmingthat PrPC silencing does not appear disturb the differentiation of MEL cells. In many cell cultures, the enhanced expression of PrPC was proposed to facilitate cytoprotective effects[32]. However, overexpression of exogenously delivered PrPC in MEL cells did not protect the cells against apoptosis initiated by serum withdrawal[33]. We also found that silencing of PrPC did not seem to sensitize cells to apoptosis during differentiation, as demonstrated by a Trypan Blue exclusion assay and by monitoring of Bax expression by qRT-PCR. This result is concurrent with Christensen and Harris, who reevaluated former assays reporting a protective activity of PrPC and suggested that the presence of PrPC has only a modest effect in cytoprotection in vitro [34].
Taken together, our results imply that, under normal conditions, PrPC seems dispensable for the erythroid differentiation of MEL cells. The pattern of PrPC regulation on erythroid precursors in vivo suggests that PrPC may play a role in the maturation of erythroblasts in erythroblastic islands. We can speculate that PrPC, which was shown to bind both laminin and the laminin receptor[35], [36], can be involved in cell-cell contacts in an erythroblastic niche, or with a surrounding extracellular matrix. Downregulation of PrPC, then, could play a role in the dissociation of matured reticulocytes from the erythroblastic niche. Such a role for PrPC is unlikely to be detected by the MEL cell model. Another explanation could be that PrPC exerts its function only under stress conditions. This hypothesis is consistent with the documented poor recovery of PrP−/− mice from experimental anemia[7]. Finally, it is possible that the effect of PrPC silencing was compensated for by an unknown pathway or that the remaining expression is sufficient to sustain its role.
In conclusion, we created model cell lines with efficiently silenced expression of PrPC, which are the first of their kind and may serve as a valuable tool in subsequent searches for the function of PrPC beyond the erythroid differentiation.
Materials and Methods
Flow cytometry of mouse bone marrow and spleen erythroid precursors
The study was approved by the Committee on the Ethics of Animal Experiments of the First Faculty of Medicine, Charles University in Prague (Permit Number: 217/07). Bone marrow (BM) cells were isolated from the femurs of PrP+/+ mice (C57BL/6×129/SvxCD1 mixed background) by washing with PBS, 1% BSA and 2 mM EDTA, pH 7.4 (PBS-BE). Spleen and BM cells were passed through a 40-µm cell strainer (Becton Dickinson, San Diego, CA, USA) to eliminate stroma and debris. The cells were labeled (30 min, 4°C) with saturating concentration of monoclonal antibodies (mAbs): anti-mouse Ter-119 eFluor 450, anti-mouse CD71-FITC (both eBioscience, San Diego, CA, USA) and AH6 (TSE Resource Center, Roslin, UK), custom conjugated to PE (Exbio, Vestec, Czech Republic). Labeled cells were washed and resuspended in PBS-BE, and their fluorescence was analyzed on a BD FACSCanto II flow cytometer equipped with BD FACSDiva Software v6.0 (Becton Dickinson). Dead cells were excluded from the analysis by 7-aminoactinomycin D (7-AAD) (Molecular Probes, Eugene, OR, USA) labeling, and the fluorescence of live cells (105) was analyzed. Erythroblast subpopulations were resolved according Ter119, CD71 and forward-scatter (FSC) signals. Proerythroblasts (proE) were identified as Ter119medium CD71+ cells. Ter119high cells were divided using both the CD71 and FSC parameters into three populations, labeled EryA, EryB and EryC, as described previously[37], and the binding of the prion mAb AH6 was quantified using Standard Quantum R-PE MESF beads (Bangs Laboratories, Fishers, IN, USA)[11], [15].
Flow cytometry of cell cultures
Cells were washed with 1% BSA-PBS, pH 7.4 (PBS-B) and labeled for 20 min at RT with saturating concentrations of the AH6-PE or anti-mouse CD71-PE (eBioscience) mAbs. Next, washed cells were resuspended in PBS-B and analyzed using a flow cytometer to standardize the fluorescence readings and to allow for the quantification of PrPC and CD71 expression Standard Quantum R-PE MESF beads were run as a separate sample. Viable cells were identified as a 7-AAD-negative population.
Cell cultures
The MEL cell line (clone 707, ECACC, Salisbury, UK) and packaging cell line HEK293 GP2 (Clontech, Mountain View, CA USA) were maintained in DMEM growth medium containing high glucose (4.5 g/L), L- glutamine, sodium pyruvate, 10% fetal bovine serum and puromycin/streptamycin (all reagents from PAA, Pasching, Austria). Cells were cultured at 37°C in a humidified atmosphere containing 5% CO2. For all experiments, MEL cells between the second and fourth passages were seeded at a density of 105 cells/mL 24 h before induction of differentiation by 5 mM HMBA (final concentration). In some instances, 4 µM dexamethasone (Sigma-Aldrich, Prague, Czech Republic) was used to block the commitment of MEL cells. The cells were incubated with either HMBA, HMBA and dexamethasone or dexamethasone alone for 24 h, and then the medium was changed, and the cells were grown in the presence of either HMBA, dexamethasone, HMBA and dexamethasone, or in medium only.
Cloning
For the silencing of cellular prion expression, we used shRNAmir sequences HP_285770 (LP1) and HP_288208 (LP2), which are available in the RNAi codex database (http://cancan.cshl.edu/cgi-bin/Codex/Codex.cgi). The shRNAs, together with the control nonsilencing shRNAmir (LN), were ordered in the pSM2 retro vectors V2MM_66187, V2MM_63696 and RHS1707 (Open Biosystems, Huntsville, AL, USA)[38]. The third anti- Prnp mRNA sequence (LP5), adopted from Pfeifer et al., was purchased as an oligonucleotide[27]. All sequences were cloned into the LMP retrovector MSCV/LTRmiR30-PIG (Open Biosystems). Constructs created in this study were verified by sequencing.
RNAi of Prnp expression
Packaging HEK293 GP2 cells were seeded at a density of approximately 1.5×105 cells/well (24-well plate). After 24 h, the cells were transfected with a mixture of the VSV-G plasmid, coding the envelope protein of the vesicular stomatitis virus (Clontech), and the appropriate LMP retrovector (LN, LP1, LP2 or LP5). Plasmids were delivered in a ratio of 9:1 with the Arrest-in transfection agent (Open Biosystems). Three days after transfection, media containing retroviral particles were centrifuged (400 g, 4°C) to pellet eventual cell contaminants, and the infectious supernatant, containing 4 µg/mL Polybrene (Sigma-Aldrich), was added to MEL cells in a 1:1 ratio. Subsequently, transduced MEL cells were spun down at 450 g for 90 min at RT (a method known as spinfection). In a second approach, the MEL cells were infected by co-cultivation with a packaging cell line. In this method, medium in HEK293 GP2 cells was aspirated 24 h postinfection, and 2×104 MEL cells/well were added inside the 0.4-µm-pore translucent polyphthalate insert (Becton Dickinson) in a 0.7 mL total volume of fresh media containing 4 µg/mL Polybrene. After 48 (co-cultivation) or after 72 (spinfection) hours of incubation, the cells were diluted with fresh medium, and selection started the next day through the addition of puromycin (Sigma) at a final concentration of 0.5 µg/mL. The percentage of cells with an integrated retrovector genome was monitored by FACS utilizing eGFP positivity. Cell lines prepared by both methods were mixed after three weeks after reaching >95% eGFP positivity and were frozen in aliquots.
Western blot and densitometry
Cells were washed in PBS and lysed with 1% TX-100, 0.5% sodium deoxycholate and 0.1% SDS in 150 mM NaCl, 2 mM MgCl2 and 50 mM Tris, pH 8.0, supplemented with 12 units/µL benzonase (Sigma) and the EDTA-free protease inhibitor Complete (Roche Diagnostics, Basel, Switzerland). Protein concentration was measured by BCA assay (Thermo Fisher Scientific, Rockford, IL, USA), and 20 µg proteins/lane were loaded for SDS-PAGE analysis. Separated proteins were blotted to nitrocellulose membranes (Bio-Rad, Hercules, CA, USA) and PrPC detected with a mix of the mAbs AH6, AG4 (both 1 µg/mL, TSE resource center) and 6H4 (0.05 µg/mL, Prionics AG, Zurich, Switzerland). The anti-actin polyclonal Ab I-19 (Santa Cruz, Santa Cruz, CA, USA) (0.5 µg/mL) was used as a loading control. Secondary antibodies were goat anti mouse IgG F(ab)2 alkaline phosphatase (Biosource) and goat anti rabbit IgG F(ab)2 alkaline phosphatase (Caltag, Buckhingham, UK), both at a dilution of 1: 4000. BCIP/NBT (Caltag) was used as a chromogen. The density of bands on blots was quantified using MiniLumi densitometer software (DNR Bio-Imaging Systems Ltd., Israel).
Reverse transcription and quantitative PCR
RNA was isolated using the RNA Blue solution according to the manufacturer's manual (Top-Bio, Prague, Czech Republic). Contaminating genomic DNA was degraded by treatment with TURBO DNase (Ambion, Austin, TX, USA). RNA integrity was evaluated by electrophoresis, and 0.5 µg RNA was reverse-transcribed with the RevertAid first-strand cDNA synthesis kit (Fermentas, Burlington, ON, Canada) according to the manufacturer's manual. Complementary DNA was tenfold diluted, and 2 µL were used for qRT-PCR performed in an ABI 7300 PCR System using TaqMan primers, probes and the Universal PCR Master Mix (Applied Biosystems, Carlsbad, CA, USA). We monitored the expression of the following genes: glyceraldehyde-3-phosphate dehydrogenase (Gapdh), the prion protein (Prnp), the hemoglobin alpha adult chain 1 (Hba-a1), the myeloblastosis oncogene (Myb), the α-hemoglobin stabilizing protein (Eraf), the GATA-binding protein 1 (GATA-1), 2′-5′ oligoadenylate synthetase 1A (Oas1a), ribonuclease L (Rnase1), the eukaryotic translation initiation factor 2-alpha kinase 2 (Eif2ak2) and the BCL2-associated X protein (Bax). Relative expression levels were calculated using the 2-ΔΔCT method[39] and normalized to the reference Gapdh gene. Expression quantities were normalized as described in results.
Spectrophotometric determination of hemoglobin content
The hemoglobin concentration in MEL cell lysates was measured with the TMB assay as described previously, with adjustments for 96-well plates[40]. The cell lysates were diluted to contain 100 µg of protein per mL, and their absorbance at 660 nm was measured using a VICTOR2 D fluorometer (PerkinElmer, Waltham, Massachusetts, USA). The amount of hemoglobin was subtracted from the calibration curve composed of serial dilutions of purified hemoglobin (Sigma).
Acknowledgments
We would like to thank Jana Cmejlova, Ph.D. and Radek Cmejla, Ph.D. (Institute of Hematology and Blood Transfusion, Prague) and Peter Svoboda, Ph.D. (Institute of Molecular Genetics of the ASCR, Prague) for helpful discussions. We acknowledge the TSE Resource Centre (The Roslin Institute, University of Edinburgh) for the donation of the antibodies AG4 and AH6.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was supported by Czech Science Foundation: project GACR 310/08/0878; Grant Agency of Charles University: projects GAUK 86408, GAUK 203429 and SVV-2010-260506; and by Ministry of Education of the Czech Republic: project MSM0021620806. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Linden R, Martins VR, Prado MA, Cammarota M, Izquierdo I, et al. Physiology of the prion protein. Physiol Rev. 2008;88:673–728. doi: 10.1152/physrev.00007.2007. [DOI] [PubMed] [Google Scholar]
- 2.Roucou X, Gains M, LeBlanc AC. Neuroprotective functions of prion protein. J Neurosci Res. 2004;75:153–161. doi: 10.1002/jnr.10864. [DOI] [PubMed] [Google Scholar]
- 3.Singh A, Kong Q, Luo X, Petersen RB, Meyerson H, et al. Prion protein (PrP) knock-out mice show altered iron metabolism: a functional role for PrP in iron uptake and transport. PLoS One. 2009;4:e6115. doi: 10.1371/journal.pone.0006115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nicolas O, Gavin R, del Rio JA. New insights into cellular prion protein (PrPc) functions: the “ying and yang” of a relevant protein. Brain Res Rev. 2009;61:170–184. doi: 10.1016/j.brainresrev.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 5.Miele G, Manson J, Clinton M. A novel erythroid-specific marker of transmissible spongiform encephalopathies. Nat Med. 2001;7:361–364. doi: 10.1038/85515. [DOI] [PubMed] [Google Scholar]
- 6.Brown AR, Blanco AR, Miele G, Hawkins SA, Hopkins J, et al. Differential expression of erythroid genes in prion disease. Biochem Biophys Res Commun. 2007;364:366–371. doi: 10.1016/j.bbrc.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 7.Zivny JH, Gelderman MP, Xu F, Piper J, Holada K, et al. Reduced erythroid cell and erythropoietin production in response to acute anemia in prion protein-deficient (Prnp-/-) mice. Blood Cells Mol Dis. 2008;40:302–307. doi: 10.1016/j.bcmd.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Zhang CC, Steele AD, Lindquist S, Lodish HF. Prion protein is expressed on long-term repopulating hematopoietic stem cells and is important for their self-renewal. Proc Natl Acad Sci U S A. 2006;103:2184–2189. doi: 10.1073/pnas.0510577103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dodelet VC, Cashman NR. Prion protein expression in human leukocyte differentiation. Blood. 1998;91:1556–1561. [PubMed] [Google Scholar]
- 10.Risitano AM, Holada K, Chen G, Simak J, Vostal JG, et al. CD34+ cells from paroxysmal nocturnal hemoglobinuria (PNH) patients are deficient in surface expression of cellular prion protein (PrPc). Exp Hematol. 2003;31:65–72. doi: 10.1016/s0301-472x(02)01011-1. [DOI] [PubMed] [Google Scholar]
- 11.Holada K, Vostal JG. Different levels of prion protein (PrPc) expression on hamster, mouse and human blood cells. Br J Haematol. 2000;110:472–480. doi: 10.1046/j.1365-2141.2000.02158.x. [DOI] [PubMed] [Google Scholar]
- 12.Panigaj M, Brouckova A, Glierova H, Dvorakova E, Simak J, et al. Underestimation of the expression of cellular prion protein on human red blood cells. Transfusion. 2010;51:1012–1021. doi: 10.1111/j.1537-2995.2010.02924.x. [DOI] [PubMed] [Google Scholar]
- 13.Marks PA, Rifkind RA. Induced differentiation of erythroleukemia cells by hexamethylene bisacetamide: a model for cytodifferentiation of transformed cells. Environ Health Perspect. 1989;80:181–188. doi: 10.1289/ehp.8980181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gougoumas DD, Vizirianakis IS, Tsiftsoglou AS. Transcriptional activation of prion protein gene in growth-arrested and differentiated mouse erythroleukemia and human neoplastic cells. Exp Cell Res. 2001;264:408–417. doi: 10.1006/excr.2001.5151. [DOI] [PubMed] [Google Scholar]
- 15.Holada K, Simak J, Brown P, Vostal JG. Divergent expression of cellular prion protein on blood cells of human and nonhuman primates. Transfusion. 2007;47:2223–2232. doi: 10.1111/j.1537-2995.2007.01451.x. [DOI] [PubMed] [Google Scholar]
- 16.Griffiths RE, Heesom KJ, Anstee DJ. Normal prion protein trafficking in cultured human erythroblasts. Blood. 2007;110:4518–4525. doi: 10.1182/blood-2007-04-085183. [DOI] [PubMed] [Google Scholar]
- 17.Hyman T, Rothmann C, Heller A, Malik Z, Salzberg S. Structural characterization of erythroid and megakaryocytic differentiation in Friend erythroleukemia cells. Exp Hematol. 2001;29:563–571. doi: 10.1016/s0301-472x(01)00616-6. [DOI] [PubMed] [Google Scholar]
- 18.Fibach E, Reuben RC, Rifkind RA, Marks PA. Effect of hexamethylene bisacetamide on the commitment to differentiation of murine erythroleukemia cells. Cancer Res. 1977;37:440–444. [PubMed] [Google Scholar]
- 19.Schroder B, Nickodemus R, Jurgens T, Bodemer W. Upstream AUGs modulate prion protein translation in vitro. Acta Virol. 2002;46:159–167. [PubMed] [Google Scholar]
- 20.Ford MJ, Burton LJ, Li H, Graham CH, Frobert Y, et al. A marked disparity between the expression of prion protein and its message by neurones of the CNS. Neuroscience. 2002;111:533–551. doi: 10.1016/s0306-4522(01)00603-0. [DOI] [PubMed] [Google Scholar]
- 21.Otsuka Y, Ito D, Katsuoka K, Arashiki N, Komatsu T, et al. Expression of alpha-hemoglobin stabilizing protein and cellular prion protein in a subclone of murine erythroleukemia cell line MEL. Jpn J Vet Res. 2008;56:75–84. [PubMed] [Google Scholar]
- 22.Chute JP, Ross JR, McDonnell DP. Minireview: Nuclear receptors, hematopoiesis, and stem cells. Mol Endocrinol. 2010;24:1–10. doi: 10.1210/me.2009-0332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaneda T, Murate T, Sheffery M, Brown K, Rifkind RA, et al. Gene expression during terminal differentiation: dexamethasone suppression of inducer-mediated alpha 1- and beta maj-globin gene expression. Proc Natl Acad Sci U S A. 1985;82:5020–5024. doi: 10.1073/pnas.82.15.5020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mattern J, Buchler MW, Herr I. Cell cycle arrest by glucocorticoids may protect normal tissue and solid tumors from cancer therapy. Cancer Biol Ther. 2007;6:1345–1354. doi: 10.4161/cbt.6.9.4765. [DOI] [PubMed] [Google Scholar]
- 25.Osborne HB, Bakke AC, Yu J. Effect of dexamethasone on hexamethylene bisacetamide-induced Friend cell erythrodifferentiation. Cancer Res. 1982;42:513–518. [PubMed] [Google Scholar]
- 26.Tilly G, Chapuis J, Vilette D, Laude H, Vilotte JL. Efficient and specific down-regulation of prion protein expression by RNAi. Biochem Biophys Res Commun. 2003;305:548–551. doi: 10.1016/s0006-291x(03)00805-2. [DOI] [PubMed] [Google Scholar]
- 27.Pfeifer A, Eigenbrod S, Al-Khadra S, Hofmann A, Mitteregger G, et al. Lentivector-mediated RNAi efficiently suppresses prion protein and prolongs survival of scrapie-infected mice. J Clin Invest. 2006;116:3204–3210. doi: 10.1172/JCI29236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singh A, Mohan ML, Isaac AO, Luo X, Petrak J, et al. Prion protein modulates cellular iron uptake: a novel function with implications for prion disease pathogenesis. PLoS One. 2009;4:e4468. doi: 10.1371/journal.pone.0004468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh A, Beveridge AJ, Singh N. Decreased CSF Transferrin in sCJD: A Potential Pre-Mortem Diagnostic Test for Prion Disorders. PLoS One. 2011;6:e16804. doi: 10.1371/journal.pone.0016804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clarke MF, Kukowska-Latallo JF, Westin E, Smith M, Prochownik EV. Constitutive expression of a c-myb cDNA blocks Friend murine erythroleukemia cell differentiation. Mol Cell Biol. 1988;8:884–892. doi: 10.1128/mcb.8.2.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen J, Kremer CS, Bender TP. A Myb dependent pathway maintains Friend murine erythroleukemia cells in an immature and proliferating state. Oncogene. 2002;21:1859–1869. doi: 10.1038/sj.onc.1205003. [DOI] [PubMed] [Google Scholar]
- 32.Roucou X, LeBlanc AC. Cellular prion protein neuroprotective function: implications in prion diseases. J Mol Med. 2005;83:3–11. doi: 10.1007/s00109-004-0605-5. [DOI] [PubMed] [Google Scholar]
- 33.Gougoumas DD, Vizirianakis IS, Triviai IN, Tsiftsoglou AS. Activation of Prn-p gene and stable transfection of Prn-p cDNA in leukemia MEL and neuroblastoma N2a cells increased production of PrP(C) but not prevented DNA fragmentation initiated by serum deprivation. J Cell Physiol. 2007;211:551–559. doi: 10.1002/jcp.20969. [DOI] [PubMed] [Google Scholar]
- 34.Christensen HM, Harris DA. Prion protein lacks robust cytoprotective activity in cultured cells. Mol Neurodegener. 2008;3:11. doi: 10.1186/1750-1326-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gauczynski S, Peyrin JM, Haik S, Leucht C, Hundt C, et al. The 37-kDa/67-kDa laminin receptor acts as the cell-surface receptor for the cellular prion protein. EMBO J. 2001;20:5863–5875. doi: 10.1093/emboj/20.21.5863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Graner E, Mercadante AF, Zanata SM, Forlenza OV, Cabral AL, et al. Cellular prion protein binds laminin and mediates neuritogenesis. Brain Res Mol Brain Res. 2000;76:85–92. doi: 10.1016/s0169-328x(99)00334-4. [DOI] [PubMed] [Google Scholar]
- 37.Liu Y, Pop R, Sadegh C, Brugnara C, Haase VH, et al. Suppression of Fas-FasL coexpression by erythropoietin mediates erythroblast expansion during the erythropoietic stress response in vivo. Blood. 2006;108:123–133. doi: 10.1182/blood-2005-11-4458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang K, Elledge SJ, Hannon GJ. Lessons from Nature: microRNA-based shRNA libraries. Nat Methods. 2006;3:707–714. doi: 10.1038/nmeth923. [DOI] [PubMed] [Google Scholar]
- 39.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 40.Petrak J, Myslivcova D, Man P, Cmejlova J, Cmejla R, et al. Proteomic analysis of erythroid differentiation induced by hexamethylene bisacetamide in murine erythroleukemia cells. Exp Hematol. 2007;35:193–202. doi: 10.1016/j.exphem.2006.10.007. [DOI] [PubMed] [Google Scholar]