Abstract
Objective
Both peripheral fat loss and central fat gain have been reported in women with HIV infection. We determined the fat changes that are specific to HIV infection in women.
Methods
HIV-infected and control women from the study of Fat Redistribution and Metabolic Change in HIV Infection (FRAM) were compared. Lipoatrophy or lipohypertrophy was defined as concordance between participant report of fat change and clinical examination. Whole-body magnetic resonance imaging measured regional adipose tissue volumes. The relationship among different adipose tissue depots was assessed. Factors associated with individual depots were analyzed using multivariate linear regression.
Results
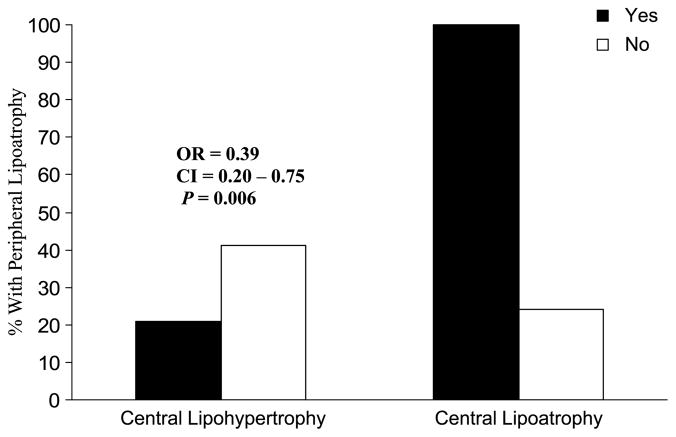
HIV-infected women reported more fat loss than controls in all peripheral and most central depots. Peripheral lipoatrophy was more frequent in HIV-infected women than controls (28% vs. 4%, P < 0.001), whereas central lipohypertrophy was similar (62% vs. 63%). Among HIV-infected women, those with central lipohypertrophy were less likely to have peripheral lipoatrophy (odds ratio, 0.39; 95% confidence interval, 0.20 to 0.75, P = 0.006) than those without central lipohypertrophy. On magnetic resonance imaging, HIV-infected women with clinical peripheral lipoatrophy had less subcutaneous adipose tissue (SAT) in peripheral and central sites and less visceral adipose tissue (VAT) than HIV-infected women without peripheral lipoatrophy. Compared with controls, HIV-infected women had less SAT in the legs, regardless of the presence or absence of lipoatrophy. However, those without lipoatrophy had more VAT and upper trunk SAT than controls. Use of the antiretroviral drug stavudine was associated with less leg SAT but was not associated with VAT. The use of highly active antiretroviral therapy, however, was associated with more VAT.
Conclusions
Peripheral lipoatrophy occurs commonly in HIV-infected women but is not associated with reciprocally increased VAT or trunk fat.
Keywords: HIV, lipodystrophy, lipoatrophy, lipohypertrophy, visceral obesity, fat redistribution, body composition
Fat distribution changes, including fat loss in the face, arms, legs, and buttocks, and fat gain in the upper back, abdomen, viscera, and breast have been reported in HIV infection and are often referred to as “lipodystrophy” or “fat redistribution syndrome.”1–25 Early studies in HIV-infected women suggested that fat gain particularly in the abdomen, breast, and upper back might be the dominant change.12,13 One study also reported that HIV-infected women had a 12% higher prevalence of fat distribution changes than HIV-infected men.26 Understanding the changes in fat that occur in HIV-infected women is critical because these fat changes may be associated with adverse metabolic parameters that predict increased risk of cardiovascular disease.
The lack of consensus defining fat changes in HIV has made research into etiology difficult and led to dilemmas among health care providers as to how to counsel patients regarding fat changes. Most published reports assessed fat changes using a participant’s report of change, confirmed on examination by a health care provider.2,4,6,10–13,15,20,25,27–30 Studies have also used different definitions to define fat changes in HIV. Some defined fat changes as occurring in either peripheral or central body sites,2–4,10,16,25,31 some combined both peripheral and central fat changes into 1 syndrome,11–13,18,20,22,27,28 and others reported separately on lipoatrophy only, lipohypertrophy only, and “combined” syndromes.15,17,21,23,24,29,30 Most studies used unidirectional questionnaires that presumed the presence of anticipated findings of peripheral lipoatrophy and central lipohypertrophy.6,11,12,15,17,21,23,24,27–30,32 Thus, there remains a debate about the definition of the syndrome.1,15,17,20,24,29,30,32–34
Early studies also did not include an HIV-uninfected comparison group. A more recent longitudinal study from the Women’s Interagency HIV Study (WIHS) cohort found that lipoatrophy (defined as participant’s report of body fat loss confirmed by anthropometry) distinguished HIV-infected women from uninfected women.35 In a cross-sectional subset of women from the WIHS, direct measurement of leg and trunk fat using dual x-ray absorptiometry scans demonstrated an inverse association between duration of stavudine use and leg fat.36
The interrelationships among the changes in fat distribution must be defined before prevalence, etiologic factors, and associated metabolic changes can be studied. Therefore, in the study of Fat Redistribution and Metabolic Changes in HIV Infection (FRAM), we evaluated self-reported changes in fat in the context of physical examination by trained observers using bidirectional instruments, and magnetic resonance imaging (MRI) measured regional subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT) volume in HIV-infected and control men and women using the same protocol. We report here our findings in HIV-infected and control women comparing fat distribution as assessed by self-report, physical examination, and MRI. Among the HIV-infected women, we also present our findings on the interrelationships of fat distribution across peripheral and central body regions, and their associations with antiretroviral therapy. Our findings in HIV-infected and control men have previously been reported.37
METHODS
Study Population
Institutional Review Boards at all 18 participating sites (16 HIV and 2 control sites) approved the study protocol and consent process. Between June 2000 and September 2002, 1480 participants (1183 HIV-infected subjects and 297 healthy controls) were enrolled in FRAM. Of the 1480 participants, 33% were women (350 HIV-infected women and 142 controls). The recruitment and data collection procedures for the entire cohort have been described elsewhere.38 Briefly, HIV-infected participants were selected from coded lists of patients seen in 16 HIV or infectious disease clinics or cohorts during 1999. Each list was then randomly ordered and provided back to the sites. Each site then contacted the subjects in consecutive order. Of 1058 women active in HIV or infectious disease clinics or cohorts, 269 did not answer multiple contact attempts; 71 were dead; 156 were ineligible (institutionalized, n = 4; communication difficulty, n = 13; primary care provider did not give permission, n = 13; or excluded by study criteria, n = 126 [age <18 years; and factors that prevented imaging: weight >136 kg, height >6′5″, metal in body, and/or claustrophobia]). The remaining 562 women were approached for informed consent. Of these, 124 declined participation and 88 did not return for data collection. Therefore, examination was completed on 350 women (62.3% of 562 contacted and eligible).
Control subjects were recruited from 2 centers of the Coronary Artery Risk Development in Young Adults (CARDIA) study.39,40 CARDIA subjects were originally recruited as a community-based sample of healthy 18- to 30-year-old white and African American men and women from 4 cities in 1986 for a longitudinal study of cardiovascular risk factors. FRAM enrolled 142 control women in 2000 to 2001 from a CARDIA ancillary study, the Visceral Fat and Metabolic Risk in Young Adults Study.41
Our analyses comparing HIV-infected women and controls in the same 33- to 45-year-old age range included 183 HIV-infected women; 6 HIV-infected women were excluded who had an opportunistic infection or malignancy within the same or previous calendar month as the examination (to remove acute changes in fat). Our analyses of HIV-associated factors including antiretroviral therapy in HIV-infected women included 338 women between the ages of 19 and 70 years (mean, 41.5 ± 8.2 years), after excluding 12 women with recent opportunistic infection or malignancy.
Clinical Assessments
HIV-infected and control participants underwent identical standardized questionnaires and examinations. Each participant was asked to report whether she had any change in fat over the last 5 years in the cheeks next to the nose, lateral aspect of the face, legs, arms, buttocks (peripheral sites), back, chest, neck, or abdomen, or change in waist size (central sites). If participants answered yes, they were asked whether the change was an increase or decrease and to grade it as mild, moderate, or severe. Participants could also answer “no change” or “don’t know”; “don’t know” represented less than 10% of responses and was pooled with “no change.” Research associates who were centrally trained were asked to determine whether participants had more or less fat compared with normal healthy people in each of those body areas before the participant filled out the self-administered questionnaire of body fat changes (to keep the research associate blinded to what the participants had reported). For the participants who were determined to have either more or less fat than normal, research associates rated the amount of fat using criteria from the HIV Outpatient Study: mild = only seen if looked for, moderate = easily seen, or severe = obvious immediately.20
Clinical lipoatrophy at each anatomical site was defined as concordance between participant report of loss of fat (mild, moderate, or severe) and examination finding of less fat than a normal healthy person at the same anatomical site. Lipohypertrophy was defined as concordance of self-report of increased fat and examination finding of more fat than normal at the same site.
Physical activity, alcohol intake, smoking, illicit drug use, education, and adequacy of food intake were assessed by standardized instruments.40–43 Menopausal status and history of gynecologic surgery were assessed by interview. Women who reported at least 12 months of amenorrhea or history of bilateral oophorectomy were categorized as being menopausal. Research associates interviewed HIV-infected participants and reviewed medical charts to determine the dates of use of individual antiretroviral medications. Blood was drawn and sent to a central laboratory (COVANCE, Indianapolis, IN) for determination of CD4 cell counts and HIV RNA levels by polymerase chain reaction in HIV-infected women.
Measurements
Height and weight were measured. Body composition was measured by MRI with participants in the supine position, arms extended over head.37,44 Using the intervertebral space between the fourth and fifth lumbar vertebrae as origin, transverse images (10-mm slice thickness) were obtained every 40 mm from the reference point to both the hand (above head) and foot. MRI scans were segmented using image analysis software (Tomovision Inc., Montreal, Quebec, Canada). Tissue areas (cm2) were calculated by summing specific tissue pixels, then multiplying by individual pixel surface area. Volume per slice (cm3) of each tissue was calculated by multiplying area by thickness. Volume of each tissue for the space between 2 consecutive slices was calculated via a mathematical algorithm.45 Volumes were normalized by dividing by height squared with summaries back-transformed to 1.75 m of height. We did not adjust for body mass index (BMI), as BMI is influenced by the very phenomenon being studied: quantity of fat. Using these methods, we quantified adipose tissue volume in the leg, lower trunk (abdomen and back), upper trunk (chest and back), and arm, and VAT.
Statistical Analysis
For comparisons of prevalence, P values were calculated by Fisher exact test. Numerical values were compared by Mann-Whitney test. Associations between dichotomous variables were quantified by odds ratios (OR) from logistic regression models and those between continuous variables by rank correlations.
Multivariate analysis was performed to determine whether factors unrelated to HIV infection and its therapies could account for observed differences in MRI measures between controls, HIV-infected women with peripheral lipoatrophy, and HIV-infected women without clinical peripheral lipoatrophy. Separate analyses were performed for each of the following 5 anatomical sites: visceral, legs, lower trunk, arms, and upper trunk. For each anatomical site, separate comparisons were made of control versus HIV-infected women with lipoatrophy and control versus HIV-infected women without lipoatrophy. These models were fitted to logarithmic transformations of MRI measures divided by height squared, analogous to BMI, to produce estimated percentage differences in height normalized quantity of adipose tissue. Variables controlled for in the models included the following: age, ethnicity, smoking, alcohol intake, illicit drug use (crack/cocaine, marijuana, heroin, and amphetamines/speed), adequacy of food intake, and level of physical activity. As the purpose of these analyses was to examine possible changes in the estimated HIV effects, we included a relatively more expansive set of variables than would be appropriate for building predictive models. Variables selected included those that had P < 0.05 in preliminary (unbootstrapped) multivariate models for any of the 5 anatomical sites considered, along with some that had high a priori plausibility as potential confounders. Confidence intervals (CIs) were determined using the bias-corrected accelerated bootstrap method,46 with P values defined as 1 minus the highest confidence level that still excluded zero. This was necessary because many outcome measures appeared to be non-Gaussian, even after normalization by height squared, log transformation, and controlling for multiple important predictors.
In HIV-infected subjects, multivariate analyses were separately performed to determine which factors were predictive of MRI-measured leg SAT or VAT. Confidence intervals were constructed for the estimated percentage differences from the multivariate models using the bias-corrected accelerated bootstrap model as described above. In addition to the predictors listed above, these models included HIV RNA level (log10), and CD4 count (log2) at the time of study visit. In multivariate models controlling for the above factors, we evaluated total duration of use of each individual antiretroviral drug (ARV), ARV class (nucleoside reverse transcriptase inhibitor [NRTI], nonnucleoside reverse transcriptase inhibitor [NNRTI], and protease inhibitor [PI]) and highly active antiretroviral therapy (HAART) as defined by: (a) 2 or more NRTIs in combination with at least 1 PI or NNRTI, (b) 1 NRTI in combination with at least 1 PI and at least 1 NNRTI, (c) a regimen containing ritonavir and saquinavir in combination with 1 NRTI and no NNRTIs, or (d) an abacavir-containing regimen of 3 or more NRTIs in the absence of both PIs and NNRTIs. We checked linearity by fitting more complex models using linear splines, finding that linearity appeared reasonable in all cases. Duration of each ARV, ARV class, and HAART were added to the model in a forward stepwise manner, and results for each ARV not reaching P < 0.05 are shown controlling for the specific ARVs that were statistically significant predictors.
RESULTS
Participants
HIV-infected and control women between the ages of 33 and 45 years had similar proportions of African Americans (Table 1). Both groups included significant numbers of whites. The control group was confined to African Americans and whites by design. Control women were on average slightly older. HIV-infected women had lower mean height and weight; however, BMI was similar between HIV-infected and control women. Few HIV-infected and control women reported being postmenopausal (n = 11 and n = 9, respectively). The primary mode of HIV transmission in the HIV-infected women was through heterosexual contact. HIV RNA levels and CD4 counts spanned the full spectrum of HIV infection.
TABLE 1.
Demographic Characteristics of Women Between the Ages of 33 to 45 Years
| Characteristic | HIV+* | Control | P |
|---|---|---|---|
| n | 183 | 142 | |
| Age (y) | |||
| Median | 39.0 | 42.0 | <0.001 |
| Range | 33.0–45.0 | 33.0–45.0 | |
| Race (%) | |||
| White | 32 | 49 | 0.002 |
| African American | 56 | 51 | 0.37 |
| Hispanic | 10 | 0 | — |
| Asian | 1 | 0 | — |
| Native American | 1 | 0 | — |
| Unknown | 1 | 0 | — |
| Height (cm) | |||
| Median | 162.6 | 164.5 | 0.005 |
| Range | 142.5–185.6 | 149.9–192.0 | |
| Weight (kg) | |||
| Median | 71.7 | 75.1 | 0.017 |
| Range | 32.7–140.2 | 42.9–117.7 | |
| BMI (kg/m2) | |||
| Median | 26.4 | 28.0 | 0.16 |
| Range | 13.0–47.7 | 17.5–47.8 | |
| Menopause† (%) | |||
| Yes | 6 | 6 | >0.99 |
| No | 80 | 81 | |
| Missing data | 14 | 13 | |
| HIV risk factor‡ (%) | |||
| Heterosexual contact | 59 | N/A | |
| Injection drug user | 26 | ||
| Other | 15 | ||
| Reported duration of HIV (y) | |||
| Median | 8.5 | N/A | |
| Range | 1.9–17.4 | ||
| HIV RNA (1000/mL) | |||
| Median | 0.8 | N/A | |
| Range | 0.4–751.0 | ||
| CD4 (cells/μL) | |||
| Median | 369 | N/A | |
| Range | 3–1600 | ||
Women with recent opportunistic infections were excluded.
Reported amenorrhea for more than 1 year or bilateral oophorectomy.
Data from 11 participants missing.
N/A indicates not available.
Lipoatrophy and Lipohypertrophy by Self-Report, Examination, and Concordance
More HIV-infected women than controls reported loss of fat in the peripheral sites: cheeks, face, arms, buttocks, and legs (all P < 0.001) (Figure 1A). Likewise, for central sites, significantly higher proportions of HIV-infected women than controls reported decreases in waist size. Similar proportions of HIV-infected and control women reported loss of neck, chest, abdominal fat, and upper back fat, although the proportion for each was slightly higher among HIV-infected women.
FIGURE 1.
Prevalence of self-report of change in body fat over the previous 5 years. HIV-positive subjects and controls were surveyed for self-reported changes in fat in multiple anatomical areas and in waist size that occurred in the 5 years before the study. A, Decreased fat. B, Increased fat. HIV+ (solid bars); controls (open bars).
Many HIV-infected women reported gain in fat (Figure 1B). In all peripheral sites, the prevalence of fat gain was significantly lower in HIV-infected women than controls. For central sites, the proportion of HIV-infected women reporting increases in the chest, waist, and upper back were similar; the prevalence was not higher in HIV-infected women at any site. However, for central sites, fewer HIV-infected women reported increases in neck fat than control women.
Using the commonly accepted standard of self-report confirmed by physical examination to define fat changes, clinical lipoatrophy was more prevalent in all peripheral sites in HIV-infected women compared with controls (Figure 2A). At central sites, clinical lipoatrophy was uncommon in both HIV-infected and control women. Clinical lipohypertrophy was less prevalent in all peripheral sites and in the neck among HIV-infected women compared with controls. The prevalence of clinical lipohypertrophy was not higher in HIV-infected women than controls in any central site (Figure 2B).
FIGURE 2.
A, Prevalence of lipoatrophy by concordance. Subjects who reported loss of fat and had less fat than normal on examination were designated as having clinical lipoatrophy. B, Prevalence of lipohypertrophy by concordance. Subject who reported gain of fat and had more fat than normal on examination were designated as having clinical lipoatrophy. HIV+ (solid bars); controls (open bars).
We separately assessed the prevalence of clinical lipoatrophy and lipohypertrophy at any peripheral or central site. HIV-infected women were more likely to have peripheral lipoatrophy in at least 1 site compared with controls (28% vs. 4%; P < 0.001). The prevalence of clinical central lipoatrophy was low for both HIV and control (6% vs. 3%, respectively, P = 0.44) and the prevalence of central lipohypertrophy in at least 1 site was very high (62% vs. 63%, P = 0.91). Peripheral lipohypertrophy was less common among HIV-infected women compared with controls (35% vs. 62%, P < 0.001).
Magnetic Resonance Imaging Measurement of Regional Adipose Tissue Volumes
We compared adipose tissue volume measured by MRI among HIV-infected women with clinical peripheral lipoatrophy at 1 or more sites to those without clinical peripheral lipoatrophy and to controls (Figure 3). HIV-infected women with clinical peripheral lipoatrophy had less adipose tissue volume in the leg, lower trunk, arms, and upper trunk and less VAT than HIV-infected women without peripheral lipoatrophy. Compared with controls, HIV-infected women had less leg SAT regardless of the presence or absence of peripheral lipoatrophy. HIV-infected women with peripheral lipoatrophy also had less adipose tissue volume in the lower trunk and arms than controls. They appeared to have less upper trunk and VAT than controls, but these comparisons did not reach statistical significance. In contrast, HIV-infected women without peripheral lipoatrophy had more upper trunk SAT and VAT than controls, despite having less leg SAT. Lower trunk and arm SAT were similar.
FIGURE 3.
Adipose tissue volume by MRI. Comparison of controls, HIV-infected women with clinical peripheral lipoatrophy (LA+), and HIV-infected women without clinical peripheral lipoatrophy (LA−). Adipose tissue volume was divided by height squared, medians and CIs were calculated, and these then multiplied by 1.752 to correspond to a typical height. Values are median and CI. Leg is the region from the toes to the slice in which the leg separation is visible and no pubic bone occurs. Lower trunk is the region from the slice above the legs to the last slice where the liver area is greater than the lung. Upper trunk is the region from the first slice where the lung area is greater than the liver to the slice below the one where the arms are separated from torso. Arm is defined as the first slice where the arms are separated from torso to the end of the hands.
After multivariate analysis, HIV-infected women with peripheral lipoatrophy had significantly lower quantities of adipose tissue in leg, lower trunk, and arm than controls (Figure 4); the amount of VAT was similar. HIV-infected women without peripheral lipoatrophy also had significantly less adipose tissue in the legs than controls; the amount of VAT remained higher.
FIGURE 4.
Comparison of MRI findings in HIV subjects with and without clinical lipoatrophy versus controls. Results of multivariate models adjusting for non-HIV–related factors affecting adipose tissue volume in various fat depots. Percentage effects in HIV-infected groups versus controls are estimated in multivariate models of logarithmically transformed (adipose tissue per height squared by MRI), controlling for age (continuous), ethnicity, total physical activity score (categorical by quartile), smoking (current vs. past vs. never), current marijuana use (used 10+ days per month vs. 1 to 9 days vs. not used), current use of cocaine (crack or other forms, 10+ days per month vs. 1 to 9 vs. not used), heroin use (any in last 30 days vs. past use only vs. never used), speed use (any in last 30 days vs. past use only vs. never used), and reported adequacy of food eaten (enough vs. less). Hatched bars, HIV+ with lipoatrophy (LA+); open bars, HIV+ no lipoatrophy (LA−). P are versus controls.
Is Clinical Peripheral Lipoatrophy Associated With Central Lipohypertrophy?
We found evidence against any association linking peripheral lipoatrophy with central lipohypertrophy in women with HIV infection. The amount of adipose tissue measured by MRI in most sites was positively correlated with the amount of adipose tissue in most other sites regardless of whether the sites were peripheral or central, or whether correlations were examined among HIV-infected women with peripheral lipoatrophy, HIV-infected women without peripheral lipoatrophy, or controls (data not shown). For example, there was a positive correlation between leg SAT and lower trunk SAT in HIV-infected women with peripheral lipoatrophy (r = 0.48, P = 0.002) and HIV-infected women without peripheral lipoatrophy (r = 0.69, P < 0.001). Interesting exceptions were the lack of a correlation between leg SAT and VAT in either HIV-infected women with peripheral lipoatrophy (r = 0.09, P = 0.57) or those without peripheral lipoatrophy (r = 0.07, P = 0.48); women with low leg SAT had a wide range of VAT. Additionally, there was no substantial correlation between leg SAT and upper trunk SAT in HIV-infected women with peripheral lipoatrophy (r = 0.07, P = 0.68). However, there were no inverse correlations to suggest reciprocal changes of peripheral and central fat.
Likewise, loss of fat in individual peripheral sites by self-report was for the most part associated with loss of or less gain in fat at central sites (data not shown). An exception was that we found little correlation between self-report of fat change in the lower body (hips, buttocks, and legs) and fat change in the upper back. Again, there were no inverse correlations. When clinical examination data on fat were analyzed, less fat in individual peripheral sites was associated with less fat at all central sites studied.
As shown in Figure 5, among HIV-infected women, the presence of the clinical syndrome of central lipohypertrophy was strongly associated with a reduced likelihood of peripheral lipoatrophy (OR = 0.39; 95% CI, 0.20 to 0.75, P = 0.006). In contrast, every woman with central lipoatrophy also had peripheral lipoatrophy.
FIGURE 5.
Clinical peripheral lipoatrophy is not associated with central lipohypertrophy. The prevalence of peripheral lipoatrophy is presented on the y axis for those with (closed bars) or without (open bars) central lipohypertrophy (left side) or central lipoatrophy (right side).
Factors Associated With Leg SAT and VAT
Finally, we assessed (Table 2) whether similar factors were associated with leg SAT (the most affected subcutaneous depot) and VAT (an important central depot that is associated with metabolic changes) among HIV-infected women using multivariate analysis. HIV-infected African American women had more leg SAT than HIV-infected white women. This difference was similar to that seen in our control women (African American women had 17% more leg SAT; 95% CI, 1.8 to 36.6, P = 0.027). Age was associated with more VAT and smoking with less VAT.
TABLE 2.
Results of Multivariate Models* Assessing Association of HIV-Related and Non–HIV-Related Factors With Adipose Tissue Volume of Leg SAT and VAT in HIV-Infected Women†
| Leg SAT‡ |
VAT‡ |
|||||
|---|---|---|---|---|---|---|
| % Effect§ | 95% CI | P | % Effect§ | 95% CI | P | |
| Ethnicity (vs. white) | ||||||
| African American | 44 | 23 to 72 | <0.0001 | −21 | −38 to 2 | 0.089 |
| Hispanic | 12 | −16 to 49 | 0.40 | 6 | −32 to 56 | 0.78 |
| Other | −15 | −43 to 18 | 0.29 | 1 | −61 to 81 | 0.95 |
| Age (y, per decade) | −6 | −14 to 2 | 0.13 | 18 | 2 to 35 | 0.031 |
| Current smoker vs. nonsmoker | −10 | −23 to 7) | 0.26 | −32 | −47 to −11 | <0.0001 |
| Physical activity (vs. first quartile) | ||||||
| Second Quartile | 10 | −7 to 30 | 0.27 | 2 | −20 to 31 | 0.79 |
| Third Quartile | 2 | −23 to 33 | 0.93 | −12 | −44 to 37 | 0.57 |
| Fourth Quartile | −20 | −38 to 3 | 0.070 | −21 | −52 to 24 | 0.32 |
| Current HIV viral load (log10) | −2 | −11 to 7 | 0.58 | −2 | −17 to 15 | 0.84 |
| Current CD4 (per doubling)|| | −3 | −8 to 3 | 0.41 | 12 | −1 to 26 | 0.096 |
| ARVs reaching statistical significance for either depot (per y of use) | ||||||
| Stavudine | −9 | −12 to −5 | <0.0001 | 1 | −5 to 7 | 0.78 |
| NNRTI | −6 | −12 to −1 | 0.027 | 0 | −9 to 8 | 0.88 |
| HAART | −0.6 | −5 to 4 | 0.83 | 7 | 1 to 13 | 0.033 |
Values are the bootstrapped outcome for the ARV plus the HIV-related and non–HIV-related factors.
Excludes participants with recent opportunistic infections.
Outcome is log (adipose tissue depot/height squared). Model controls for alcohol, crack/cocaine, heroin, and marijuana.
Percent effect describes the estimate of the percentage differences in the quantity of adipose tissue normalized by height that is caused by the specific factor.
CD4 log transformed for analysis.
Among the ARVs evaluated, stavudine was significantly associated with less leg SAT. After adjustment for stavudine, no other individual ARV was associated. However, the ARV class NNRTI was associated with less leg SAT. We did not adjust for the NRTI class because stavudine is a NRTI, and no other NRTIs were found to be associated with leg SAT. HAART was found to be associated with more VAT. Individual ARV drugs not reaching significance for leg SAT and VAT are listed in the appendix.
DISCUSSION
In this multicenter study of HIV-infected women and controls, we made several important observations. First, HIV-infected women who had the clinical syndrome of peripheral lipoatrophy had less adipose tissue in each peripheral and each central depot than HIV-infected women without the syndrome of peripheral lipoatrophy. Second, HIV-infected women had less SAT in the legs than control women, regardless of the presence or absence of the clinical syndrome of lipoatrophy. Third, the clinical syndrome of peripheral lipoatrophy was not associated with the clinical syndrome of lipohypertrophy. However, HIV-infected women without the clinical syndrome of lipoatrophy had more VAT and upper trunk SAT than control women. Finally, among the individual ARVs and ARV classes evaluated, use of stavudine and the ARV class NNRTI were associated with less leg SAT, whereas the use of HAART was associated with more VAT.
Our results argue against previous descriptions of a “lipodystrophy syndrome” in which peripheral fat loss is accompanied by central fat gain, including increased VAT. Likely reasons for the observed differences in our study and previous reports6,11,12,15,17,21,23,24,27–30,32 include our use of bidirectional questions to assess fat changes, our direct measurements of regional adipose tissue by MRI, and the comparison of HIV-infected and control women.
Our study found that peripheral lipoatrophy was not associated with central lipohypertrophy whether determined by self-report, examination, or concordance. Measurement by MRI also found that the clinical syndrome of peripheral lipoatrophy was not associated with increased VAT. However, our findings that upper trunk SAT and VAT was significantly higher in HIV-infected women without the clinical syndrome of peripheral lipoatrophy, who also had less leg SAT, may explain the previously proposed association of peripheral lipoatrophy with central lipohypertrophy.11–13,15,17,18,20,21,23,24,27–30 Interestingly, we found that in HIV-infected men,37 VAT was similar between those with the clinical syndrome of peripheral lipoatrophy and those without the clinical syndrome of peripheral lipoatrophy. Although upper trunk SAT was higher in HIV-infected men without the clinical syndrome of peripheral lipoatrophy compared with those with the clinical syndrome, contrary to what we found in women, the amount of upper trunk SAT in both groups of HIV-infected men was less than in control men. The sex differences observed may be caused by the fact that women have more total body fat than men. Thus, although the clinical syndrome of peripheral lipoatrophy is not associated with the clinical syndrome of central lipohypertrophy, some women will have both a high amount of VAT and a low amount of leg SAT.
Our findings may also explain previous reports that HIV-infected women experience more central lipohypertrophy. First, only 28% of our HIV-infected women had the clinical syndrome of peripheral lipoatrophy by the accepted clinical approach of self report confirmed by examination compared with nearly 40% of FRAM HIV-infected men.37 Second, those without the clinical syndrome of lipoatrophy had more upper trunk SAT and VAT, yet direct measures of fat on MRI demonstrated less leg fat in all HIV-infected women compared with controls. Conversely, those with the clinical syndrome of lipoatrophy appear to represent those most severely affected with peripheral fat loss. Categorizing HIV-infected women by a clinical syndrome of peripheral lipoatrophy may underestimate the fat changes that occur.
Therefore, we used actual adipose tissue volumes in the leg and VAT to assess the associated factors. We found that the factors associated with leg SAT differed from those associated with VAT. Among the individual ARVs studied, the findings that stavudine was strongly associated with less leg SAT, but apparently not VAT, support the contention that HIV-related lipoatrophy is not linked to visceral obesity. The findings with stavudine confirm what we found in HIV-infected men from our cohort. However, the use of NNRTI as a class predicted less leg SAT in women (−6.0%; 95% CI, −11.5% to −0.8%, P = 0.026), but appeared to be more weakly associated with leg SAT in HIV-infected men from our cohort (−2.5%; 95% CI, −5.6% to 1.0%, P = 0.15). Similarly, indinavir use was associated with less leg SAT in men (−3.3%; 95% CI, −5.4% to −1.0%, P = 0.004), but may be less associated with reduced leg SAT in women (−2.5%; 95% CI, −7.5% to 3.6%, P = 0.50). These data could represent similar trends, but may suggest a sex-specific effect of NNRTI, which has not previously been reported. Most studies in women have not examined the association between the use of NNRTI and leg fat. These results should be examined in a randomized, prospective study of NNRTI use in a large cohort of women using direct measures of fat.
Our findings are different from another study in HIV-infected women,12 which reported an association between lamivudine and a clinical syndrome of both peripheral lipoatrophy and central lipohypertrophy. We found that the use of any form of HAART was associated with increased VAT; lamivudine is a common component of most HAART regimens. In the study of Gervasoni et al,12 most women with the clinical syndrome were also concurrently on stavudine. Because fat redistribution changes were defined as women with both peripheral lipoatrophy and central lipohypertrophy in that study, the independent effects of stavudine and lamivudine could not be determined. Combining findings that are inversely correlated with each other (peripheral lipoatrophy and central lipohypertrophy) could have led to misunderstandings.
Our findings are consistent with those of the WIHS, which found an increased incident risk of lipoatrophy in both peripheral and central sites in HIV-infected compared with uninfected women, but similar risk of central lipohypertrophy.47 WIHS also used bidirectional questions to ascertain body fat change. However, the clinical syndrome was defined using participant’s self report of fat change confirmed by a change in anthropometric measurement in the same direction. Therefore, VAT could not be assessed and regional SAT depots were not directly measured. Interestingly, the BMI in HIV-infected women in the WIHS was significantly lower than their controls, whereas HIV-infected women in FRAM had similar BMI to controls. In a cross-sectional subset of WIHS women, stavudine was found to be associated with decreased leg fat on dual x-ray absorptiometry scans.36
The primary limitation of our study was its cross-sectional design. We were not able to study changes in adipose tissue distribution over time. However, our study was performed approximately 5 years after the introduction of combination antiretroviral therapy, which is adequate time to observe the evolution of the syndromes studied by others. Most women in our study were exposed to antiretroviral therapy, and so we were not able to address regional body composition in HIV-infected women not previously exposed to antiretroviral therapy. Our controls were not selected from women with similar risk behaviors as our HIV-infected women, as were the controls in the WIHS. Rather, we recruited women from a community-based study of healthy young whites and African Americans in the United States whose BMI measurements are similar to the larger, nationally representative NHANES III.
In summary, we find evidence for a syndrome of subcutaneous lipoatrophy in HIV-infected women. Peripheral lipoatrophy was not associated with central lipohypertrophy or increased VAT. Women who did not have the clinical syndrome of peripheral lipoatrophy had more VAT than controls. Thus, our findings are contrary to previous observations of a single syndrome of peripheral lipoatrophy and clinical lipohypertrophy. Likewise, antiretroviral drugs that were associated with lipoatrophy, as assessed by volume of leg fat, did not appear associated with central lipohypertrophy, as assessed by volume of VAT. Rather, any form of HAART was associated with increased VAT. These results indicate that future research studies of fat distribution in HIV-infected women should focus on measurements of fat, not clinical syndromes. Our finding that HIV-infected women without clinical peripheral lipoatrophy have more upper trunk SAT and VAT than control women, whereas HIV-infected men do not, highlights the need to study individual adipose tissue depots in women to determine their etiology and associated metabolic findings.
Acknowledgments
Supported by the National Institutes of Health grants RO1-DK57508, HL74814, HL 53359, and AI 027767, and National Institutes of Health GCRC grants M01-RR00036, RR00051, RR00052, RR00054, RR00083, RR0636, and RR00865.
The funding agency reviewed the study design but played no role in collection, management, analysis, or interpretation of the data or in the preparation of the manuscript. The National Institutes of Health personnel participated as members of the Coronary Artery Risk Development in Young Adults Publications Committee that reviewed and approved the manuscript.
APPENDIX
Writing Team
Peter Bacchetti, Joseph Cofrancesco, Steven Heymsfield, Cora E. Lewis, Rebecca Scherzer, Michael Shlipak, and Phyllis C. Tien.
Sites and Investigators
University Hospitals of Cleveland (Barbara Gripshover); Tufts University (Abby Shevitz and Christine Wanke); Stanford University (Andrew Zolopa and Lisa Gooze); University of Alabama at Birmingham (Michael Saag and Barbara Smith); John Hopkins University (Joseph Cofrancesco and Adrian Dobs); University of Colorado Heath Sciences Center (Constance Benson and Lisa Kosmiski); University of North Carolina at Chapel Hill (Charles van der Horst); University of California at San Diego (W. Christopher Matthews and Daniel Lee); Washington University (William Powderly and Kevin Yarasheski); Veterans Affairs Medical Center, Atlanta (David Rimland); University of California at Los Angeles (Judith Currier and Matthew Leibowitz); Veterans Affairs Medical Center, New York (Michael Simberkoff and Juan Bandres); Veterans Affairs Medical Center, Washington, DC (Cynthia Gibert and Fred Gordin); St Luke’s-Roosevelt Hospital Center (Donald Kotler and Ellen Engelson); University of California at San Francisco (Morris Schambelan and Kathleen Mulligan); Indiana University (Michael Dube); Kaiser Permanente, Oakland (Stephen Sidney); and University of Alabama at Birmingham (Cora E. Lewis).
Data Coordinating Center
University of Alabama, Birmingham (O. Dale Williams, Heather McCreath, Charles Katholi, George Howard, Tekeda Ferguson, and Anthony Goudie).
Image Reading Center
St Luke’s-Roosevelt Hospital Center (Steven Heymsfield, Jack Wang, and Mark Punyanitya).
Office of the Principal Investigator
University of California, San Francisco, Veterans Affairs Medical Center and the Northern California Institute for Research and Development (Carl Grunfeld, Phyllis Tien, Peter Bacchetti, Dennis Osmond, Andrew Avins, Michael Shlipak, Rebecca Scherzer, Mae Pang, and Heather Southwell).
TABLE A1.
ARVs Not Reaching Significance (Per Year of Use) or Not Adjusted for in Multivariate Models* Assessing Association of HIV-Related and Non–HIV-Related Factors With Adipose Tissue Volume of Leg SAT and VAT in HIV-Infected Women†
| Leg SAT‡ |
VAT‡ |
|||||
|---|---|---|---|---|---|---|
| % Effect | 95% CI | P | % Effect | 95% CI | P | |
| NRTI§ | −3 | −6 to 0 | 0.038 | −1 | −7 to 4 | 0.61 |
| Zidovudine | −2 | −5 to 1 | 0.25 | −2 | −7 to 3 | 0.54 |
| Lamivudine | −3 | −7 to 1 | 0.11 | 3 | −6 to 12 | 0.53 |
| Didanosine | 5 | −2 to 14 | 0.12 | 6 | −6 to 16 | 0.34 |
| Zalcitabine | −3 | −13 to 3 | 0.25 | −4 | −22 to 7 | 0.44 |
| Abacavir | −5 | −15 to 5 | 0.28 | −4 | −19 to 10 | 0.56 |
| PI | −3 | −7 to 1 | 0.16 | 4 | −4 to 11 | 0.36 |
| Indinavir | −3 | −8 to 4 | 0.49 | −2 | −10 to 7 | 0.67 |
| Saquinavir | −2 | −9 to 1 | 0.12 | 4 | −4 to 13 | 0.31 |
| Ritonavir | 3 | −4 to 11 | 0.45 | 10 | −2 to 22 | 0.091 |
| Nelfinavir | −2 | −8 to 5 | 0.59 | −1 | −10 to 8 | 0.78 |
| Lopinavir | −15 | −35 to 13 | 0.29 | 12 | −25 to 57 | 0.55 |
| Amprenavir | −15 | −41 to 29 | 0.32 | 55 | −6 to 120 | 0.072 |
| NNRTI | ||||||
| Delavirdine | −9 | −36 to 25 | 0.43 | −14 | −57 to 103 | 0.48 |
| Efavirenz | −4 | −14 to 9 | 0.56 | 0 | −15 to 15 | 0.98 |
| Nevirapine | 6 | −6 to 18 | 0.35 | 1 | −9 to 10 | 0.91 |
Values are the bootstrapped outcome for the ARV plus the HIV-related and non–HIV-related factors.
Excludes participants with recent opportunistic infections.
Outcome is log (adipose tissue depot/height squared). Model also controls for alcohol, crack/cocaine, heroin, and marijuana.
Multivariate model of leg fat did not adjust for NRTI class because stavudine is a NRTI; no other NRTIs were significant.
References
- 1.Safrin S, Grunfeld C. Fat distribution and metabolic changes in patients with HIV infection. AIDS. 1999;13(18):2493–2505. doi: 10.1097/00002030-199912240-00002. [DOI] [PubMed] [Google Scholar]
- 2.Lo JC, Mulligan K, Tai VW, et al. “Buffalo hump” in men with HIV-1 infection. Lancet. 1998;351(9106):867–870. doi: 10.1016/S0140-6736(97)11443-X. [DOI] [PubMed] [Google Scholar]
- 3.Miller KD, Jones E, Yanovski JA, et al. Visceral abdominal-fat accumulation associated with use of indinavir. Lancet. 1998;351(9106):871–875. doi: 10.1016/S0140-6736(97)11518-5. [DOI] [PubMed] [Google Scholar]
- 4.Miller KK, Daly PA, Sentochnik D, et al. Pseudo-Cushing’s syndrome in human immunodeficiency virus-infected patients. Clin Infect Dis. 1998;27(1):68–72. doi: 10.1086/514638. [DOI] [PubMed] [Google Scholar]
- 5.Viraben R, Aquilina C. Indinavir-associated lipodystrophy. AIDS. 1998;12(6):F37–F39. doi: 10.1097/00002030-199806000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Carr A, Samaras K, Burton S, et al. A syndrome of peripheral lipodystrophy, hyperlipidaemia and insulin resistance in patients receiving HIV protease inhibitors. AIDS. 1998;12(7):F51–F58. doi: 10.1097/00002030-199807000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Striker R, Conlin D, Marx M, et al. Localized adipose tissue hypertrophy in patients receiving human immunodeficiency virus protease inhibitors. Clin Infect Dis. 1998;27(1):218–220. doi: 10.1086/517682. [DOI] [PubMed] [Google Scholar]
- 8.Shaw AJ, McLean KA, Evans BA. Disorders of fat distribution in HIV infection. Int J STD AIDS. 1998;9(10):595–599. doi: 10.1258/0956462981921189. [DOI] [PubMed] [Google Scholar]
- 9.Engelson ES, Kotler DP, Tan Y, et al. Fat distribution in HIV-infected patients reporting truncal enlargement quantified by whole-body magnetic resonance imaging. Am J Clin Nutr. 1999;69(6):1162–1169. doi: 10.1093/ajcn/69.6.1162. [DOI] [PubMed] [Google Scholar]
- 10.Saint-Marc T, Partisani M, Poizot-Martin I, et al. A syndrome of peripheral fat wasting (lipodystrophy) in patients receiving long-term nucleoside analogue therapy. AIDS. 1999;13(13):1659–1667. doi: 10.1097/00002030-199909100-00009. [DOI] [PubMed] [Google Scholar]
- 11.Madge S, Kinloch-de-Loes S, Mercey D, et al. Lipodystrophy in patients naive to HIV protease inhibitors. AIDS. 1999;13(6):735–737. doi: 10.1097/00002030-199904160-00020. [DOI] [PubMed] [Google Scholar]
- 12.Gervasoni C, Ridolfo AL, Trifiro G, et al. Redistribution of body fat in HIV-infected women undergoing combined antiretroviral therapy. AIDS. 1999;13(4):465–471. doi: 10.1097/00002030-199903110-00004. [DOI] [PubMed] [Google Scholar]
- 13.Dong KL, Bausserman LL, Flynn MM, et al. Changes in body habitus and serum lipid abnormalities in HIV-positive women on highly active antiretroviral therapy (HAART) J Acquir Immune Defic Syndr. 1999;21(2):107–113. [PubMed] [Google Scholar]
- 14.Christeff N, Melchior JC, de Truchis P, et al. Lipodystrophy defined by a clinical score in HIV-infected men on highly active antiretroviral therapy: correlation between dyslipidaemia and steroid hormone alterations. AIDS. 1999;13(16):2251–2260. doi: 10.1097/00002030-199911120-00007. [DOI] [PubMed] [Google Scholar]
- 15.Saint-Marc T, Partisani M, Poizot-Martin I, et al. Fat distribution evaluated by computed tomography and metabolic abnormalities in patients undergoing antiretroviral therapy: preliminary results of the LIPOCO study. AIDS. 2000;14(1):37–49. doi: 10.1097/00002030-200001070-00005. [DOI] [PubMed] [Google Scholar]
- 16.Mallal SA, John M, Moore CB, et al. Contribution of nucleoside analogue reverse transcriptase inhibitors to subcutaneous fat wasting in patients with HIV infection. AIDS. 2000;14(10):1309–1316. doi: 10.1097/00002030-200007070-00002. [DOI] [PubMed] [Google Scholar]
- 17.Thiebaut R, Daucourt V, Mercie P, et al. Lipodystrophy, metabolic disorders, and human immunodeficiency virus infection: Aquitaine Cohort, France, 1999. Groupe d’Epidemiologie Clinique du Syndrome d’Immunodeficience Acquise en Aquitaine. Clin Infect Dis. 2000;31(6):1482–1487. doi: 10.1086/317477. [DOI] [PubMed] [Google Scholar]
- 18.Tsiodras S, Mantzoros C, Hammer S, et al. Effects of protease inhibitors on hyperglycemia, hyperlipidemia, and lipodystrophy: a 5-year cohort study. Arch Intern Med. 2000;160(13):2050–2056. doi: 10.1001/archinte.160.13.2050. [DOI] [PubMed] [Google Scholar]
- 19.Polo R, Verdejo J, Martinez-Rodriguez S, et al. Lipoatrophy, fat accumulation, and mixed syndrome in protease inhibitor-naive HIV-infected patients. J Acquir Immune Defic Syndr. 2000;25(3):284–286. doi: 10.1097/00126334-200011010-00014. [DOI] [PubMed] [Google Scholar]
- 20.Lichtenstein KA, Ward DJ, Moorman AC, et al. Clinical assessment of HIV-associated lipodystrophy in an ambulatory population. AIDS. 2001;15(11):1389–1398. doi: 10.1097/00002030-200107270-00008. [DOI] [PubMed] [Google Scholar]
- 21.Martinez E, Mocroft A, Garcia-Viejo MA, et al. Risk of lipodystrophy in HIV-1-infected patients treated with protease inhibitors: a prospective cohort study. Lancet. 2001;357(9256):592–598. doi: 10.1016/S0140-6736(00)04056-3. [DOI] [PubMed] [Google Scholar]
- 22.van der Valk M, Gisolf EH, Reiss P, et al. Increased risk of lipodystrophy when nucleoside analogue reverse transcriptase inhibitors are included with protease inhibitors in the treatment of HIV-1 infection. AIDS. 2001;15(7):847–855. doi: 10.1097/00002030-200105040-00005. [DOI] [PubMed] [Google Scholar]
- 23.Chene G, Angelini E, Cotte L, et al. Role of long-term nucleoside-analogue therapy in lipodystrophy and metabolic disorders in human immunodeficiency virus-infected patients. Clin Infect Dis. 2002;34(5):649–657. doi: 10.1086/338811. [DOI] [PubMed] [Google Scholar]
- 24.Saves M, Raffi F, Capeau J, et al. Factors related to lipodystrophy and metabolic alterations in patients with human immunodeficiency virus infection receiving highly active antiretroviral therapy. Clin Infect Dis. 2002;34(10):1396–1405. doi: 10.1086/339866. [DOI] [PubMed] [Google Scholar]
- 25.Lichtenstein KA, Delaney KM, Armon C, et al. Incidence of and risk factors for lipoatrophy (abnormal fat loss) in ambulatory HIV-1-infected patients. J Acquir Immune Defic Syndr. 2003;32(1):48–56. doi: 10.1097/00126334-200301010-00007. [DOI] [PubMed] [Google Scholar]
- 26.Galli M, Veglia F, Angarano G, et al. Gender differences in antiretroviral drug-related adipose tissue alterations. J Acquir Immune Defic Syndr. 2003;34(1):58–61. doi: 10.1097/00126334-200309010-00008. [DOI] [PubMed] [Google Scholar]
- 27.Carr A, Samaras K, Thorisdottir A, et al. Diagnosis, prediction, and natural course of HIV-1 protease-inhibitor-associated lipodystrophy, hyperlipidaemia, and diabetes mellitus: a cohort study. Lancet. 1999;353(9170):2093–2099. doi: 10.1016/S0140-6736(98)08468-2. [DOI] [PubMed] [Google Scholar]
- 28.Carr A, Miller J, Law M, et al. A syndrome of lipoatrophy, lactic acidaemia and liver dysfunction associated with HIV nucleoside analogue therapy: contribution to protease inhibitor-related lipodystrophy syndrome. AIDS. 2000;14(3):F25–F32. doi: 10.1097/00002030-200002180-00001. [DOI] [PubMed] [Google Scholar]
- 29.Galli M, Ridolfo AL, Adorni F, et al. Body habitus changes and metabolic alterations in protease inhibitor-naive HIV-1-infected patients treated with two nucleoside reverse transcriptase inhibitors. J Acquir Immune Defic Syndr. 2002;29(1):21–31. doi: 10.1097/00126334-200201010-00003. [DOI] [PubMed] [Google Scholar]
- 30.Galli M, Cozzi-Lepri A, Ridolfo AL, et al. Incidence of adipose tissue alterations in first-line antiretroviral therapy: the LipoICoNa Study. Arch Intern Med. 2002;162(22):2621–2628. doi: 10.1001/archinte.162.22.2621. [DOI] [PubMed] [Google Scholar]
- 31.Carr A, Samaras K, Chisholm DJ, et al. Pathogenesis of HIV-1-protease inhibitor-associated peripheral lipodystrophy, hyperlipidaemia, and insulin resistance. Lancet. 1998;351(9119):1881–1883. doi: 10.1016/S0140-6736(98)03391-1. [DOI] [PubMed] [Google Scholar]
- 32.Carr A, Emery S, Law M, et al. An objective case definition of lipodystrophy in HIV-infected adults: a case-control study. Lancet. 2003;361(9359):726–735. doi: 10.1016/s0140-6736(03)12656-6. [DOI] [PubMed] [Google Scholar]
- 33.Carter VM, Hoy JF, Bailey M, et al. The prevalence of lipodystrophy in an ambulant HIV-infected population: it all depends on the definition. HIV Med. 2001;2(3):174–180. doi: 10.1046/j.1468-1293.2001.00073.x. [DOI] [PubMed] [Google Scholar]
- 34.Moyle G. Lipodystrophy: lack of agreement on definition and etiology presents a challenge to research and therapy. AIDS Read. 2002;12(10):438, 440–442. [PubMed] [Google Scholar]
- 35.Tien PC, Cole SR, Williams CM, et al. Incidence of lipoatrophy and lipohypertrophy in the women’s interagency HIV study. J Acquir Immune Defic Syndr. 2003;34(5):461–466. doi: 10.1097/00126334-200312150-00003. [DOI] [PubMed] [Google Scholar]
- 36.Mulligan K, Anastos K, Justman J, et al. Fat distribution in HIV-infected women in the United States: DEXA substudy in the Women’s Interagency HIV Study. J Acquir Immune Defic Syndr. 2005;38(1):18–22. doi: 10.1097/00126334-200501010-00004. [DOI] [PubMed] [Google Scholar]
- 37.FRAM Study Investigators. Fat Distribution in Men with HIV Infection. J Acquir Immune Defic Syndr. 2005;40(2):121–131. doi: 10.1097/01.qai.0000182230.47819.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tien PC, Benson C, Zolopa AR, et al. The study of fat redistribution and metabolic change in HIV infection (FRAM): methods, design, and sample characteristics. Am J Epidemol. 2006;163:860–869. doi: 10.1093/aje/kwj111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hughes GH, Cutter G, Donahue R, et al. Recruitment in the Coronary Artery Disease Risk Development in Young Adults (CARDIA) study. Control Clin Trials. 1987;8(suppl 4):68S–73S. doi: 10.1016/0197-2456(87)90008-0. [DOI] [PubMed] [Google Scholar]
- 40.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41(11):1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 41.Hill JO, Sidney S, Lewis CE, et al. Racial differences in amounts of visceral adipose tissue in young adults: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Am J Clin Nutr. 1999;69(3):381–387. doi: 10.1093/ajcn/69.3.381. [DOI] [PubMed] [Google Scholar]
- 42.Sidney S, Jacobs DR, Jr, Haskell WL, et al. Comparison of two methods of assessing physical activity in the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Epidemiol. 1991;133(12):1231–1245. doi: 10.1093/oxfordjournals.aje.a115835. [DOI] [PubMed] [Google Scholar]
- 43.Hoegerman GS, Lewis CE, Flack J, et al. Lack of association of recreational cocaine and alcohol use with left ventricular mass in young adults. The Coronary Artery Risk Development in Young Adults (CARDIA) study. J Am Coll Cardiol. 1995;25(4):895–900. doi: 10.1016/0735-1097(94)00469-7. [DOI] [PubMed] [Google Scholar]
- 44.Gallagher D, Belmonte D, Deurenberg P, et al. Organ-tissue mass measurement allows modeling of REE and metabolically active tissue mass. Am J Physiol. 1998;275(2 pt 1):E249–E258. doi: 10.1152/ajpendo.1998.275.2.E249. [DOI] [PubMed] [Google Scholar]
- 45.Shen W, Wang Z, Tang H, et al. Volume estimates by imaging methods: model comparisons with visible woman as the reference. Obes Res. 2003;11(2):217–225. doi: 10.1038/oby.2003.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Efron B, Tibshirani R. An Introduction to the Bootstrap. London, UK: Chapman and Hall; 1993. [Google Scholar]
- 47.Palella FJ, Jr, Cole SR, Chmiel JS, et al. Anthropometrics and examiner-reported body habitus abnormalities in the multicenter AIDS cohort study. Clin Infect Dis. 2004;38(6):903–907. doi: 10.1086/381684. [Epub 2004 Mar 2001] [DOI] [PubMed] [Google Scholar]