Abstract
Objective
Both peripheral fat loss and central fat gain have been reported in HIV infection. Which changes are specific to HIV were determined by comparison with control subjects and the associations among different adipose tissue depots were determined.
Methods
Cross-sectional analysis of HIV-positive and control men from the study of Fat Redistribution and Metabolic Change in HIV Infection. Lipoatrophy or lipohypertrophy was defined as concordance between participant report of change and examination. Regional adipose tissue volume was measured by magnetic resonance imaging (MRI).
Results
HIV-positive men reported more fat loss than controls in all peripheral and most central depots. Peripheral lipoatrophy was more frequent in HIV-positive men than in controls (38.3% vs. 4.6%, P < 0.001), whereas central lipohypertrophy was less frequent (40.2% vs. 55.9%, P = 0.001). Among HIV-positive men, the presence of central lipohypertrophy was not positively associated with peripheral lipoatrophy (odds ratio = 0.71, CI: 0.47 to 1.06, P = 0.10). On MRI, HIV-positive men with clinical peripheral lipoatrophy had less subcutaneous adipose tissue (SAT) in peripheral and central sites and less visceral adipose tissue (VAT) than HIV-positive men without peripheral lipoatrophy. HIV-positive men both with and without lipoatrophy had less SAT than controls, with legs and lower trunk more affected than upper trunk. Use of the antiretroviral drugs stavudine or indinavir was associated with less leg SAT but did not appear to be associated with more VAT; nevirapine use was associated with less VAT.
Conclusion
Both peripheral and central subcutaneous lipoatrophy was found in HIV infection. Lipoatrophy in HIV-positive men is not associated with reciprocally increased VAT.
Keywords: HIV infection, lipodystrophy, lipoatrophy, lipohypertrophy, visceral obesity, fat redistribution, body composition
Changes in fat distribution, including peripheral lipoatrophy of face and limbs, appearance of dorsocervical fat pads and multiple lipomas, and increased breast size, abdominal girth, and visceral adipose tissue (VAT) have been reported in HIV infection and are referred to as “lipodystrophy” or “fat redistribution syndrome.”1–25 HIV-associated lipodystrophy has been associated with adverse metabolic parameters that predict increased cardiovascular disease. Changes in fat stigmatize HIV-infected patients and have led patients to stop their antiretroviral (ARV) therapy because they experienced or feared changes in fat.26–28
Most reports have defined lipodystrophy based on self-report of change, confirmed on examination by a health care provider.2,4,6,10–13,15,20,25,29–32 Some studies reported on changes in either peripheral or central body sites,2–4,10,16,25,33 some combine changes into one syndrome,11–13,18,20,22,29,30 and others report separately on lipoatrophy only, lipohypertrophy only, and “combined” syndromes.15,17,21,23,24,31,32 Most studies used unidirectional questions, assessing only the presence of anticipated findings of peripheral lipoatrophy and central lipohypertrophy.6,11,12,15,17,21,23,24,29–32,34 Thus, there is debate about the definition of the syndrome.1,15,17,20,24,31,32,34–36 The few studies that have evaluated population-based control subjects with the same clinical instruments found that lipoatrophy distinguished HIV-infected subjects from control subjects.37,38
The absence of a standardized definition has made research into etiology difficult and prevented healthcare providers from counseling patients. The interrelationships of the changes in fat distribution must be defined before prevalence, etiologic factors, and associated metabolic changes can be studied. Therefore, in the study of Fat Redistribution and Metabolic Changes in HIV Infection (FRAM), we evaluated self-reported changes in fat and physical examination findings by trained observers using bidirectional instruments and measured regional subcutaneous adipose tissue (SAT) and VAT by MRI in HIV-infected subjects and control subjects using identical protocols. Our objectives were to compare fat distribution as assessed by self-report, physical examination, and measurement by MRI in HIV-infected men with that in controls (HIV-uninfected men) and within HIV-infected men, to evaluate the interrelationships of fat distribution across peripheral and central regions, and their associations with ARV therapy.
METHODS
Subjects
The protocol was approved by institutional review boards at all sites. HIV-infected subjects were selected from coded lists of patients seen in 16 HIV or infectious disease clinics or cohorts during 1999. Each list was randomly ordered and grouped into blocks of 5 potential subjects. Sites were given sets of blocks; only after extensive recruitment efforts by multiple methods were completed for a block was a new block provided. Analyses of female participants are incomplete and will be reported subsequently. Of 2094 male patients active in the HIV clinics, 414 did not answer multiple contact attempts; 154 were dead; 269 were ineligible (institutionalized, n = 23; communication difficulty, n = 37; primary care provider refused, n = 13; or excluded by study criteria, n = 196 [age <18 years; factors prevented imaging: weight >136 kg, height >6′5″, metal in body, claustrophobia]). The remaining 1257 eligible men were approached for informed consent. Of those, 279 declined participation and 163 did not return for data collection. Examinations were completed from June 2000–January 2002 on 825 men (65.6% of 1257 contacted and eligible).
Control subjects were recruited from 2 centers of the Coronary Artery Risk Development in Young Adults (CARDIA) study.39,40 CARDIA subjects were originally recruited as a population-based sample of healthy 18- to 33-year-old white and African American men and women from 4 cities in 1986 for a longitudinal study of cardiovascular risk factors. Participants in the CARDIA study were stratified for the 2 races and genders. Of 377 participants who agreed to the year 15 CARDIA examination who were approached to participate in FRAM, 339 (90%) agreed to participate; 28 (7%) did not return for examination; and 14 (4%) were excluded from FRAM for factors preventing imaging. HIV testing was not done in the CARDIA cohort, but the prevalence of HIV infection was estimated to be <1% based on previous data, and no CARDIA participant was taking an ARV medication.
Here we report findings for the 425 HIV-infected men and 152 control men in the 33- to 45-year age range; we excluded 11 HIV-infected men who had an opportunistic infection or malignancy within the same or previous calendar month as the examination, to remove confounders of acute changes in fat.
Clinical Assessments
The HIV-infected and control groups underwent identical standardized questionnaires and examinations performed by uniformly trained research associates (completion rate >99%). Each subject was asked to report whether he had had any change in fat over the past 5 years in the cheeks next to the nose, lateral aspect of the face, legs, arms, buttocks (peripheral sites), back, chest, neck, or abdomen or change in waist size (central sites). If subjects answered yes, they were asked whether the change was an increase or decrease and to grade it as mild, moderate, or severe. Subjects could also answer “No change” or “Don’t know.” “Don’t know” represented <10% of responses and was pooled with “No change.” Research associates were asked to determine whether subjects had more or less fat compared with normal healthy people in each of those body areas, rating amount of fat using criteria from the HIV Outpatient Study (HOPS): mild = only seen if looked for; moderate = easily seen; severe = obvious immediately.20
Clinical lipoatrophy at each anatomic site was defined as concordance between participant report of loss of fat (mild, moderate, or severe) and examination finding of less fat than a normal healthy person at the same anatomic site. Lipohypertrophy was defined as concordance of self-report of increased fat and examination finding of more fat than normal at the same site.
Physical activity, alcohol intake, smoking, illicit drug use, education, and adequacy of food intake were assessed by standardized instruments.40–43 Research associates interviewed HIV-infected subjects and reviewed medical charts to determine the dates of use of individual ARV medications. Blood was drawn for determination of CD4 cell counts and HIV RNA by polymerase chain reaction, which were measured in a single laboratory (Covance, Indianapolis, Indiana).
Measurements
Height and weight were measured. Body composition was measured by MRI with subjects in the supine position, arms extended over head.44 Using the intervertebral space between the 4th and 5th lumbar vertebrae as origin, transverse images (10-mm slice thickness) were obtained every 40 mm from hand to foot. MRI scans were segmented using image analysis software (Tomovision, Inc., Montreal, Canada). Tissue areas (cm2) were calculated by summing specific tissue pixels, then multiplying by individual pixel surface area. Volume per slice (cm3) of each tissue was calculated by multiplying area by thickness. Volume of each tissue for the space between 2 consecutive slices was calculated via a mathematical algorithm.45 Volumes were normalized by dividing by height2 with summaries back-transformed to 1.75 m of height. We did not adjust to body mass index (BMI), as BMI is influenced by the phenomenon being studied: quantity of fat. However, we also analyzed adipose tissue volume adjusted to the subject’s total lean body mass. Ninety-two percent of participants had MRI performed. Eleven percent of scans had at least one body area outside the field of view. When a single limb was outside the field of view, volume in the measured limb was doubled to obtain total limb volume. Using this method we quantified adipose tissue volume in the leg, lower trunk (abdomen and back), upper trunk (chest and back), arm, and VAT.
Statistical Analysis
For prevalence, P values were calculated by Fisher exact test. Numerical values were compared by Mann–Whitney U test, which can produce small P values even when confidence intervals for medians overlap. Associations between dichotomous variables were quantified by odds ratios (ORs) from logistic regression models and those between numeric variables by rank correlations.
Multivariate analysis was performed to determine whether factors unrelated to HIV infection and its therapies could account for observed differences in MRI measures between the control and HIV-infected groups with and without clinical peripheral lipoatrophy. Separate analyses were performed for each of the following 5 anatomic sites: visceral, legs, lower trunk, arms, and upper trunk. For each anatomic site, separate comparisons were made of control subject vs. HIV infected with lipoatrophy and control vs. HIV infected without lipoatrophy. These models were fitted to logarithmic transformations of MRI measures to produce estimated percentage differences in amounts of adipose tissue. To control for body size, we included logarithm of total lean mass by MRI as a predictor in all models. This appeared to have nonlinear associations with adipose tissue volume in some depots, so we also included the square of log lean mass to model this nonlinearity. Results were very similar when we instead used height to control for body size. We note that controlling for BMI would not be appropriate, because BMI includes the outcomes being modeled as part of its definition. Variables controlled for in the models include the following: age, ethnicity, smoking, alcohol intake, illicit drug use (crack/cocaine, marijuana, heroin, and speed), adequacy of food intake, and level of physical activity. As the purpose of these analyses was to examine possible changes in the estimated HIV effects, we included a relatively more expansive set of variables than would be appropriate for building predictive models. Variables selected included those that had P < 0.05 in preliminary (unbootstrapped) multivariate models for any of the 5 anatomic sites considered, along with some that had high a priori plausibility as potential confounders. Confidence intervals were determined using the bias-corrected accelerated bootstrap method,46 with P values defined as the one minus the highest confidence level that still excluded zero. This was necessary both because many outcome measures appeared to be non-Gaussian, even after log transformation, and to control for multiple important predictors.
Multivariate analyses were separately performed to determine which factors related and unrelated to HIV infection were predictive of lipoatrophy as assessed by leg SAT or of lipohypertrophy as assessed by VAT in HIV-infected subjects. To control for body size, we adjusted for logarithm of total lean mass by MRI as described above. Confidence intervals were constructed for the estimated percentage differences from the multivariate models using the bias-corrected accelerated bootstrap model as described above. In addition to the predictors listed above, these models included HIV RNA level (log 10) and CD4 count (log 2) at the time of study visit. In multivariate models controlling for the above factors, we evaluated total duration of use of each individual ARV drug and ARV class: nucleoside reverse transcriptase inhibitor (NRTI), nonnucleoside reverse transcriptase inhibitor (NNRTI), protease inhibitor (PI), and highly active antiretroviral therapy (HAART) as defined by ≥2 NRTIs in combination with at least one PI or NNRTI; one NRTI in combination with at least one PI and at least one NNRTI; a regimen containing ritonavir and saquinavir in combination with one NRTI and no NNRTIs; or an abacavir-containing regimen of ≥3 NRTIs in the absence of both PIs and NNRTIs. We checked linearity by fitting more complex models using linear splines, finding that linearity appeared reasonable in all cases. Duration of each ARV, ARV class, and HAART was added to the model in a forward stepwise manner, and results for ARV not reaching P < 0.05 are shown controlling for those that did.
RESULTS
Subjects
HIV-infected and control men had similar age ranges and percentage of whites; both groups included significant numbers of African Americans, but the HIV-infected cohort included other ethnic groups (Table 1). Mean height was 2% lower, weight 15% lower, and BMI 11% lower in the HIV-infected men than in control subjects. The dominant HIV risk factor for men was having sex with men. HIV RNA and CD4 counts spanned the full spectrum of HIV infection.
TABLE 1.
Demographics of Men Between the Ages of 33 and 45
| HIV+* | Control | |
|---|---|---|
| n | 425 | 152 |
| Age (y) | ||
| Mean ± SD | 39.6 ± 3.5† | 39.6 ± 3.5 |
| Range | 33.0–45.0 | 33.0–45.0 |
| Race | ||
| White | 57% | 53% |
| African American | 31% | 47% |
| Hispanic | 12% | 0 |
| Asian | 0.5% | 0 |
| Other | 1% | 0 |
| Height (cm) | ||
| Mean ± SD | 175.9 ± 7.1‡ | 178.3 ± 7.4 |
| Median | 175.9 | 178.2 |
| Range | 144.8–194.4 | 155.5–197.7 |
| Weight (kg) | ||
| Mean ± SD | 77.2 ± 13.5§ | 87.7 ± 15.1 |
| Median | 75.4 | 84.7 |
| Range | 47.8–129.3 | 48.3–137.3 |
| BMI (kg/m2) | ||
| Mean ± SD | 24.9 ± 3.9§ | 27.6 ± 4.5 |
| Median | 24.4 | 27.0 |
| Range | 17.2–43.2 | 15.1–41.6 |
| HIV Risk Factors | ||
| MSM | 70% | |
| IDU | 15% | |
| Other | 15% | |
| Duration HIV (y) | ||
| Mean ± SD | 8.6 ± 4.1 | |
| Range | 1.6–21.1 | |
| HIV RNA (1000/mL) | ||
| Median | <0.4 | |
| Range | 0.4–751 | |
| CD4 (cells/μL) | ||
| Mean ± SD | 393 ± 238 | |
| Median | 356 | |
| Range | 3–1267 | |
Men with recent opportunistic infections were excluded.
P = 0.9.
P = 0.001 vs. controls.
P < 0.001 vs. controls.
IDU indicates injecting drug user; MSM, men who have sex with men.
Lipoatrophy and Lipohypertrophy by Self-Report, Examination, and Concordance
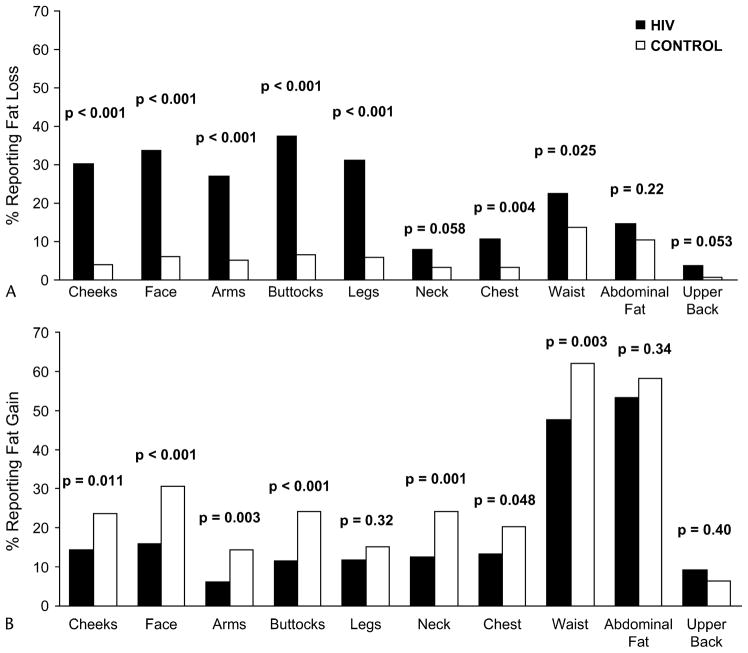
Figure 1A shows that more HIV-infected men than control subjects reported fat losses in the peripheral sites: cheeks, face, arms, buttocks, and legs (all P < 0.001). Half of fat loss changes reported in HIV-infected men were “mild.” Likewise, for central sites, higher proportions of HIV-infected men than control subjects reported decreases in waist size and chest fat and possibly neck and upper back fat. These results indicate that a significantly greater proportion of HIV-infected men lost fat in peripheral and central sites compared with control men.
FIGURE 1.
Prevalence of self-report of change in body fat over the prior 5 years. HIV-infected men (solid bars) and control subjects (open bars) were surveyed for self-reported changes in fat in multiple anatomic areas and in waist size that occurred in the 5 years prior to study. A, Decreased fat. B, Increased fat.
Some HIV-infected men reported gain in fat (Fig. 1B). However, the prevalence of fat gain was significantly lower in HIV-infected men than controls in most central and peripheral sites.
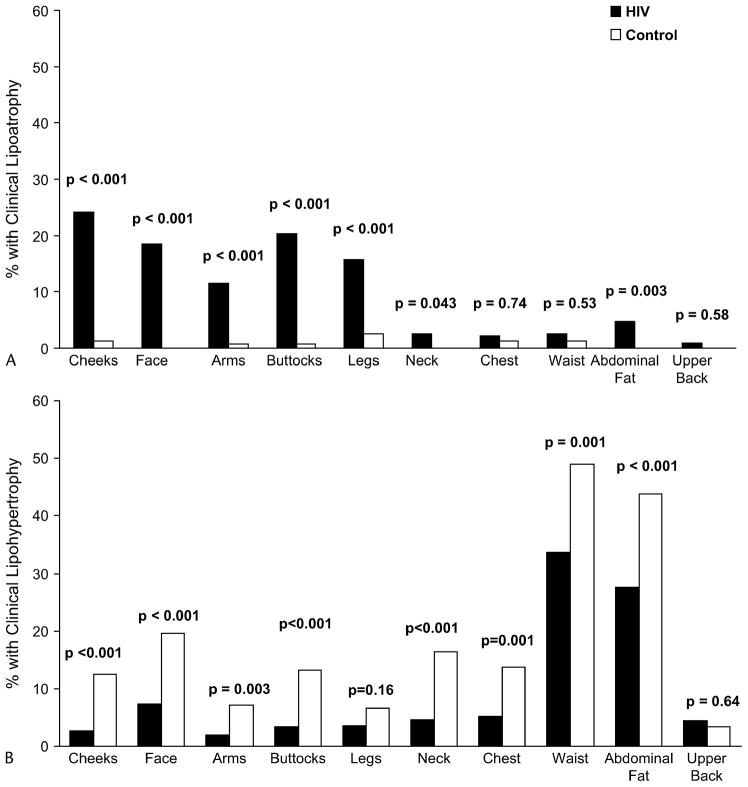
Findings on examination were similar to those from self-report (data not shown). Using the commonly accepted standard of self-report confirmed by physical examination, clinical lipoatrophy was more prevalent in all peripheral sites in HIV-infected men than in controls (Fig. 2A). HIV-infected men were also more likely to have lipoatrophy in the central site of abdominal fat and possibly neck, but the prevalence of central lipoatrophy was much lower than in the periphery. With regard to clinical lipohypertrophy defined as concordance of self-report and examination, HIV-infected men had less lipohypertrophy in the neck, chest, abdomen, waist, cheeks, face, arms, and buttocks compared with controls (Fig. 2B).
FIGURE 2.
A, Prevalence of lipoatrophy by concordance. Subjects who reported loss of fat and had less fat than normal on examination were designated as having clinical lipoatrophy. B, Prevalence of lipohypertrophy by concordance. Subjects who reported gain of fat and had more fat than normal on examination were designated as having clinical lipohypertrophy. HIV-infected (solid bars); control subjects (open bars).
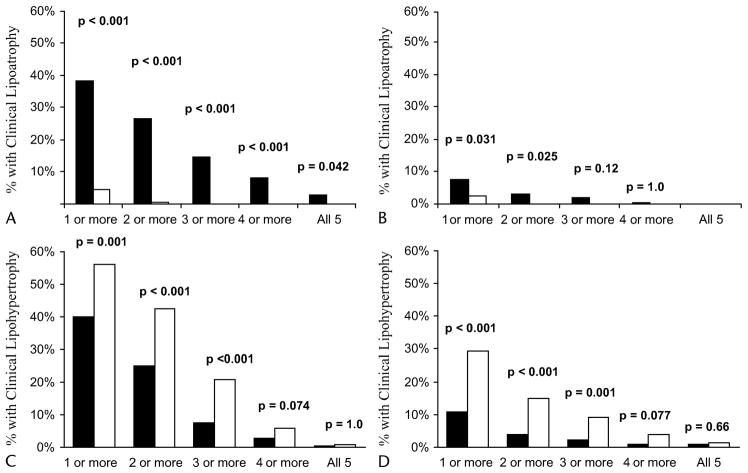
We then separately assessed the prevalence of lipoatrophy and lipohypertrophy at any peripheral or central site (Fig. 3). HIV-infected men were more likely to have peripheral lipoatrophy in at least one site compared with controls (38% vs. 5%; P <0.001, Fig. 3A). HIV-infected men commonly had multiple sites of peripheral lipoatrophy, whereas this was uncommon in controls. More HIV-infected men than controls had clinical central lipoatrophy (8% vs. 3%, P = 0.03, Fig. 3B), although this finding was less common than peripheral lipoatrophy. In contrast, controls were more likely to have lipohypertrophy at one or more sites, be they central or peripheral (Figs. 3C and D).
FIGURE 3.
Prevalence of lipoatrophy (A and B) and lipohypertrophy (C and D) by number of anatomic sites affected in HIV-infected (closed bars) and control subjects (open bars). The percentage of subjects with each number of anatomic sites affected is presented. A and D, Peripheral sites (cheeks, face, arms, buttocks, leg). B and C, Central Sites (neck, chest, upper back, waist, abdominal fat).
MRI Measurement of Regional Adipose Tissue Volumes
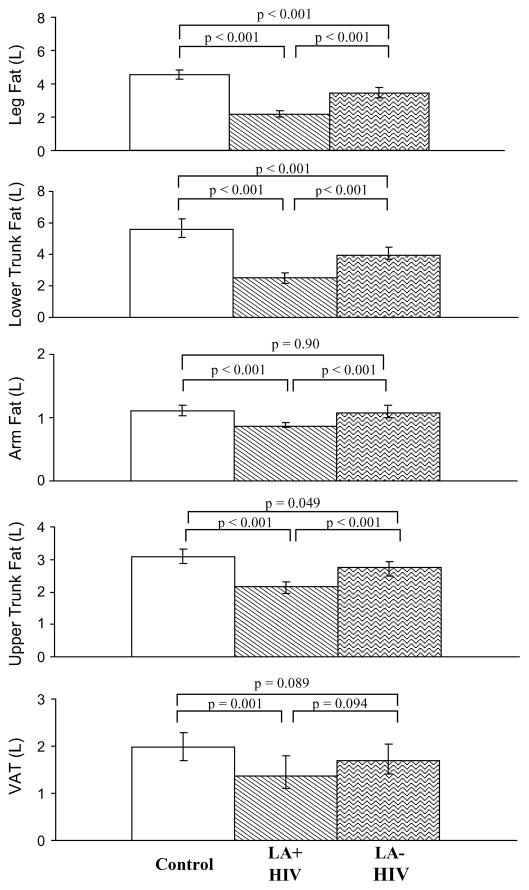
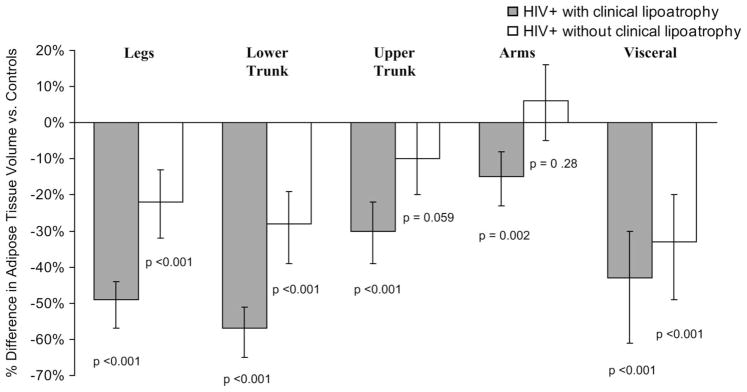
Because peripheral lipoatrophy was the most common characteristic that distinguished HIV-infected men from control subjects and because peripheral lipoatrophy has been reported as a distinct clinical syndrome, we compared adipose tissue volume measured by MRI in HIV-infected men with and without clinical peripheral lipoatrophy and controls. Compared with HIV-infected men without peripheral lipoatrophy, HIV-infected men with clinical peripheral lipoatrophy had less SAT in peripheral depots of legs and arms, but they also had less SAT in central depots of the lower trunk/abdomen and upper trunk/chest, and possibly VAT (Fig. 4). The findings were similar when adipose tissue volume was adjusted per lean body mass rather than height (data not shown).
FIGURE 4.
Adipose tissue volume by MRI. Comparison of control subjects, HIV-infected with clinical peripheral lipoatrophy (LA+) and HIV-infected without clinical peripheral lipoatrophy (LA−). Adipose tissue volume was divided by height squared, medians and confidence intervals were calculated, and these were then multiplied by 1.752 to correspond to a typical height. Values are median and confidence interval. Leg is the region from the toes to the slice in which the leg separation is visible and no pubic bone occurs. Lower trunk is the region from the slice above legs to the last slice where the liver area is greater than lung. Upper trunk is the region from the first slice where the lung area is greater than liver to the slice below the one where the arms are separated from torso. Arm is defined as the first slice where the arms are separated from torso to the end of the hands.
HIV-infected men with clinical lipoatrophy had less adipose tissue than controls in all depots. Furthermore, HIV-infected men who did not have the clinical syndrome of peripheral lipoatrophy also had less SAT in the legs, lower trunk, and upper trunk than controls (Fig. 4). When adipose tissue volume was adjusted per lean body mass rather than height, the findings were similar, except that median VAT volumes, although following the same pattern, were closer together and differences did not reach statistical significance (data not shown).
We also performed an analysis controlling for factors unrelated to HIV infection that might contribute to differences in body composition among HIV-infected men and controls (including lean body mass, age, race, physical activity, and substance abuse) by multivariate adjustment. The amount of adipose tissue adjusted remained significantly lower in all depots in HIV-infected men with peripheral lipoatrophy compared with controls (Fig. 5). HIV-infected men who did not have lipoatrophy also had significantly less adipose tissue in lower trunk, leg, and possibly VAT than controls. HIV-infected men who did not have lipoatrophy had similar upper trunk fat compared with controls and possibly more arm fat. Thus even after adjustment for these factors and lean body mass, there is no evidence for a reciprocal increase in VAT in HIV-infected men with peripheral lipoatrophy.
FIGURE 5.
Comparison of MRI findings in HIV subjects with and without clinical lipoatrophy vs. control subjects: Results of multivariate models adjusting for non–HIV-related factors affecting adipose tissue volume in various fat depots. Percentage effects in HIV-infected groups vs. controls are estimated in multivariate models of logarithmically transformed (adipose tissue by MRI), controlling for logarithm (lean mass) and the square of log (lean mass) (continuous), age (continuous), ethnicity, total physical activity score (categorical by quartile), smoking (current vs. past vs. never), current marijuana use (used 10+ days per month vs. 1–9 days vs. not used), current use of cocaine (crack or other forms, 10+ days per month vs. 1–9 days vs. not used), heroin use (any in past 30 days vs. past use only vs. never used), speed use (any in past 30 days vs. past use only vs. never used), and reported adequacy of food eaten (enough vs. less). Hatched bars: HIV-infected with lipoatrophy (LA+); open bars: HIV-infected no lipoatrophy (LA−). P values are vs. controls.
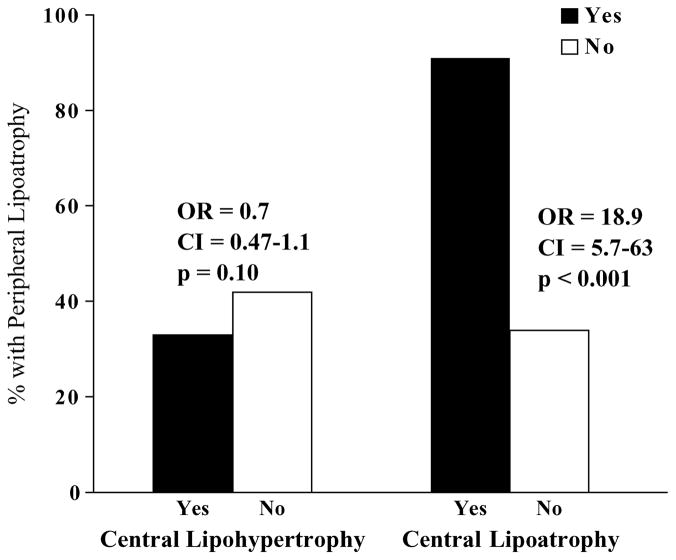
Is Clinical Peripheral Lipoatrophy Associated With Central Lipohypertrophy?
The findings that HIV-infected men with the clinical syndrome of peripheral lipoatrophy have less adipose tissue volume in central sites than HIV-positive men without peripheral lipoatrophy suggested that there was no association of peripheral lipoatrophy with central lipohypertrophy in men with HIV infection. We found evidence against such an association using multiple approaches. First, the amount of adipose tissue measured by MRI in most sites was positively correlated with the amount of adipose tissue in most other sites regardless of whether the sites were peripheral or central, or whether correlations were examined among HIV-infected men with peripheral lipoatrophy, HIV-infected men without peripheral lipoatrophy, or control subjects (data not shown). An interesting exception was that there was no correlation between leg SAT and VAT in HIV-infected men with peripheral lipoatrophy (r = 0.00, P = 0.99); men with low leg SAT had a wide range of VAT.
Likewise, loss of fat in individual peripheral sites by self-report was associated with loss of or less gain in fat at central sites (data not shown). Similarly, less fat in individual peripheral sites on examination was associated with less fat in central sites. As shown in Figure 6, among HIV-infected men, the presence of the clinical syndromes of central lipohypertrophy and peripheral lipoatrophy had no positive association with each other (OR: 0.71, CI: 0.47 to 1.06, P = 0.10). In contrast, the presence of central lipoatrophy was strongly associated with peripheral lipoatrophy (OR: 18.9, CI: 5.7 to 63, P < 0.0001).
FIGURE 6.
Clinical peripheral lipoatrophy is not associated with central lipohypertrophy. The prevalence of peripheral lipoatrophy is presented on the y-axis for those with (closed bars) or without (open bars) central lipohypertrophy (left side) or central lipoatrophy (right side).
Factors Associated With Leg SAT and VAT
Finally, we assessed (Table 2) whether similar factors were associated with leg SAT (the most affected subcutaneous depot) and VAT (an important central depot that is associated with metabolic changes) in HIV-infected men by a multivariate model that included CD4 cell count, HIV RNA level, and ARV therapy duration, as well as the non–HIV-related predictors used above. The effects of race, smoking, and physical activity all followed known patterns in the general population.43 Of note, age was associated with less leg SAT, but more VAT, in HIV-infected subjects. Higher current HIV RNA levels were associated with more leg SAT but did not appear to be associated with VAT. Duration of use of stavudine was strongly associated with less leg SAT, as was that of indinavir. There was a trend for an association of duration of use of didanosine with less leg fat. However, stavudine and indinavir were not associated with more VAT. No ARV was estimated to have a substantial positive association with VAT; the largest point estimate for an ARV was much smaller in magnitude than those for race, age, or physical activity. In contrast, duration of nevirapine use was associated with less VAT. There were no apparent associations with any ARV class or HAART after adjusting for stavudine and indinavir for leg SAT or nevirapine for VAT.
TABLE 2.
Results of Multivariate Models Assessing Association of HIV-Related and Non–HIV-Related Factors With Adipose Tissue Volume of Leg SAT and VAT in HIV-Positive Men
| Leg SAT
|
VAT
|
|||||||
|---|---|---|---|---|---|---|---|---|
| % Effect | 95% CI
|
P value | % Effect | 95% CI
|
P value | |||
| Lower | Upper | Lower | Upper | |||||
| Ethnicity | ||||||||
| African American vs. Caucasian | 16.9 | 6.6 | 28.3 | 0.001 | −55.9 | −63.5 | −46.6 | <0.0001 |
| Hispanic vs. Caucasian | 13.3 | −3.0 | 30.3 | 0.12 | −0.9 | −26.7 | 24.5 | 0.87 |
| Other vs. Caucasian | −7.7 | −24.1 | 16.8 | 0.50 | −13.8 | −40.5 | 30.5 | 0.45 |
| Age (per decade) | −5.2 | −9.1 | −1.2 | 0.012 | 32.8 | 23.1 | 44.6 | <0.0001 |
| Current smoker vs. non-smoker | 1.4 | −7.1 | 9.7 | 0.79 | −14.8 | −26.9 | −2.1 | 0.022 |
| Physical activity | ||||||||
| 2nd quartile vs. 1st | −2.7 | −12.0 | 7.5 | 0.62 | −15.1 | −30.5 | 3.4 | 0.12 |
| 3rd quartile vs. 1st | −1.1 | −11.0 | 10.2 | 0.86 | −5.8 | −22.6 | 14.2 | 0.52 |
| 4th quartile vs. 1st | −18.0 | −25.7 | −9.3 | <0.0001 | −24.9 | −39.4 | −8.5 | 0.001 |
| Current HIV viral load (log 10) | 6.3 | 1.4 | 11.5 | 0.010 | −0.6 | −7.9 | 8.3 | 0.94 |
| Current CD4 100 (log 2) | 0.0 | −3.4 | 3.3 | 1.00 | 4.5 | −2.0 | 12.4 | 0.19 |
| ARVs reaching significance (per year of use) | ||||||||
| Stavudine | −6.0 | −8.1 | −4.1 | <0.0001 | ||||
| Indinavir | −3.9 | −6.4 | −1.6 | 0.002 | ||||
| Nevirapine | −13.2 | −25.3 | −2.8 | 0.012 | ||||
| ARVs not reaching significance (per year of use) | ||||||||
| HAART | −1.5 | −4.2 | 1.2 | 0.29 | −0.5 | −4.8 | 4.0 | 0.82 |
| NRTIs | −0.8 | −2.4 | 0.8 | 0.31 | 1.1 | −1.9 | 4.1 | 0.48 |
| Stavudine | 0.9 | −3.5 | 4.7 | 0.73 | ||||
| Zidovudine | −0.5 | −2.2 | 1.2 | 0.53 | 0.7 | −2.2 | 3.8 | 0.60 |
| Lamivudine | 0.0 | −2.3 | 2.2 | 0.99 | 2.0 | −1.8 | 6.5 | 0.28 |
| Didanosine | −3.2 | −6.4 | 0.1 | 0.062 | 0.1 | −5.1 | 6.1 | 0.94 |
| Zalcitabine | −2.1 | −11.1 | 6.1 | 0.61 | 7.4 | −6.3 | 20.3 | 0.29 |
| Abacavir | −2.3 | −7.0 | 3.1 | 0.38 | −6.1 | −16.1 | 2.9 | 0.18 |
| PIs | 0.3 | −2.5 | 3.2 | 0.81 | −1.8 | −6.3 | 2.3 | 0.35 |
| Indinavir | −1.0 | −6.2 | 3.3 | 0.59 | ||||
| Saquinavir | 0.1 | −3.7 | 3.9 | 1.00 | −0.9 | −8.5 | 6.5 | 0.84 |
| Ritonavir | 1.7 | −1.9 | 5.8 | 0.33 | 3.4 | −3.1 | 10.9 | 0.27 |
| Nelfinavir | −0.7 | −3.7 | 2.6 | 0.74 | −4.1 | −10.7 | 1.6 | 0.16 |
| Lopinavir/ritonavir | 0.8 | −16.5 | 21.5 | 0.95 | −7.5 | −27.6 | 19.1 | 0.53 |
| Amprenavir | −1.9 | −11.5 | 9.7 | 0.72 | 0.0 | −17.8 | 23.1 | 1.00 |
| NNRTIs | −1.3 | −4.4 | 2.8 | 0.56 | 0.9 | −7.9 | 9.2 | 0.82 |
| Delavirdine | 10.3 | −11.0 | 32.8 | 0.36 | 0.4 | −16.7 | 43.5 | 0.90 |
| Efavirenz | −1.4 | −5.4 | 3.0 | 0.51 | 0.7 | −9.4 | 8.9 | 0.92 |
| Nevirapine | −2.1 | −6.6 | 2.9 | 0.36 | ||||
Outcome is Log (AT depot). Model controls for alcohol, crack/cocaine, heroin, marijuana, and lean mass (plus quadratic effect) as well as factors listed in top part of table. For bottom half of table, the values are the boot strapped outcome for that ARV plus the above factors.
DISCUSSION
Our study demonstrates that HIV-infected men who had the clinical syndrome of peripheral lipoatrophy had less adipose tissue in each peripheral and central depot than HIV-infected men without peripheral lipoatrophy. Furthermore, HIV-infected men with or without the clinical syndrome of peripheral lipoatrophy had less adipose tissue in both peripheral and central subcutaneous sites compared with control subjects, with lower body more affected than upper body using direct measurements of adipose tissue volume. Clinically, HIV-infected men were more likely to have peripheral lipoatrophy than controls, but they also had more central lipoatrophy and less central lipohypertrophy. The findings from self-report also show that loss of fat in peripheral and most central subcutaneous depots distinguished all HIV-infected men from controls. Furthermore, use of stavudine or indinavir was associated with less leg SAT, but the use of these drugs did not appear to be associated with more VAT.
Thus, our results argue against the proposals in earlier reports of a reciprocal syndrome of lipodystrophy in which peripheral fat loss is accompanied by central fat gain, including increased VAT. Likely reasons for these differences between our study and prior reports include our use of bidirectional scales (most studies only inquired about peripheral fat loss and central fat gain6,11,12,15,17,21,23,24,29–32,34), our highly accurate regional measurements of affected adipose tissue depots, and the comparison of HIV-infected men with a control group. A recent study of anthropometric measurements in HIV-infected and control men also found that waist, hip, arm, and thigh circumferences were lower in HIV-infected men compared with HIV-negative controls, although their examiners reported more fat accumulation in the abdomen.38
Our study evaluated the associations between peripheral fat and central fat without assuming a link between loss of peripheral fat and gain of central fat. We found that peripheral lipoatrophy was not associated with central lipohypertrophy, whether determined by self-report, examination, or concordance. Furthermore, measurement by MRI found that the clinical syndrome of peripheral lipoatrophy was not associated with increased VAT. Finally, the factors associated with leg SAT were not the same as those associated with VAT. For example, the use of stavudine or indinavir was associated with less leg SAT. In contrast, neither of these ARVs appeared to be associated with more VAT. Nevirapine use was associated with less VAT. Combining findings that are inversely correlated with each other (peripheral lipoatrophy and central lipohypertrophy) could lead to misunderstandings of their prevalence, causes, and consequences.
Our finding that leg fat was much lower in HIV-infected men compared with controls, whereas upper trunk fat was relatively spared, may explain the proposed association of peripheral lipoatrophy with central lipohypertrophy.11–13,15,17,18,20,21,23,24,29–32 Furthermore, the finding that even HIV-infected men without clinical peripheral lipoatrophy had less SAT in most depots than controls, especially in the legs and lower trunk, suggests that the clinical syndrome of lipoatrophy underestimates the extent of adipose tissue loss in HIV-infected men. Indeed, the qualitative comparisons vs. controls were similar among HIV-infected men both with and without the clinical syndrome, differing only in the extent of decreased fat. In both HIV-infected groups, lower body adipose tissue depots were affected more than upper body depots or VAT (Fig. 5).
We found evidence against any reciprocal increase in VAT in HIV-infected with peripheral lipoatrophy; indeed VAT was slightly lower in HIV-infected with peripheral lipoatrophy compared with HIV-infected without peripheral lipoatrophy. There were positive, not negative, correlations between VAT and SAT in most peripheral depots (data not shown). These results argue against a single syndrome of peripheral fat loss and central fat gain. We found relative sparing of VAT in HIV-infected men with lower quantity of leg SAT, consistent with other smaller studies in HIV infection15,47 and with what is seen with fat loss in cancer and anorexia nervosa.48,49 Although increased VAT is not statistically associated with decreased adipose tissue in the periphery, individual patients may have high VAT and low subcutaneous fat.
Therefore, we used actual adipose tissue volumes in the leg and VAT to assess the associated factors. The findings that stavudine or indinavir use was associated with less leg SAT, but apparently not with more VAT, also supports the contention that HIV-related lipoatrophy is not linked to visceral obesity, thus contradicting the concept of an HIV-specific reciprocal syndrome of fat redistribution. Conversely, older age, a factor unrelated to HIV infection, was associated both with less leg SAT and with more VAT.
Given our findings that HIV-infected men report more fat loss and have lower adipose tissue volumes in most subcutaneous sites than control men, it is not surprising that BMI was lower in HIV-infected men than controls. We did not control for or match by BMI, as BMI is influenced by the phenomenon being studied: quantity of fat. Thus matching for BMI would constitute overcontrolling and could lead to erroneous comparisons. For example, if HIV caused loss of fat in a single depot, with no change in other depots, then BMI matching would lead to an apparent, but artifactual, increase in nonaffected depots. We controlled for body size by normalizing to height squared, analogous to BMI. An alternative way to account for body size while avoiding overcontrolling is to normalize for lean body mass; this analysis produced similar results.
We chose a control group that was representative of whites and African Americans in the United States 15 years earlier, whose BMI is similar to the larger, nationally representative National Health and Nutrition Examination Survey (NHANES) III. BMI in FRAM CARDIA participants is similar to values in the entire CARDIA cohort (data not shown). It is difficult to find control subjects that are identical to HIV-infected men in all aspects except HIV infection. Two recent reports from the Multicenter AIDS Cohort Study (MACS) and the Woman’s Interagency HIV Study also found that HIV-infected participants had lower BMI than their HIV-negative controls, who were selected from similar demographic groups.37,38 Both groups reported that lipoatrophy, using anthropometrics, was the dominant feature distinguishing HIV-infected men from controls. In the MACS report, demographically matched HIV-negative subjects had average BMI that was higher than the national average in NHANES III.38 The controls in FRAM have a BMI that is closer to that of the subjects in NHANES. Thus the finding of lower BMI in HIV-infected subjects may be common. Furthermore the similarity of conclusions from comparing HIV-infected men with clinical lipoatrophy and HIV-infected men without lipoatrophy, as well as comparing HIV-infected men with controls, provides strong support for the concept that peripheral lipoatrophy is not linked to central lipohypertrophy. Finally, multivariate adjustment for differences in race, illicit drug use, food adequacy, smoking, and other factors that differed between groups found that such factors did not appear to account for the differences in body composition between HIV-infected men and controls.
There are several limitations to our data. We report only on men here. This is a cross-sectional study, so further changes in adipose tissue distribution may occur over time. However, the study was done approximately 5 years after the introduction of highly active ARV therapy, which is more than adequate time to see the syndromes studied by others. It is not possible to determine what regional body composition would have been in the HIV-infected group in the absence of HIV infection or the syndrome of lipoatrophy.
In summary, we find evidence for a syndrome of subcutaneous lipoatrophy in HIV-infected men, with lower body depots affected more than upper body depots. There is no association of peripheral lipoatrophy with central lipohypertrophy or increased VAT; our use of bidirectional scales and rigorous measurements produces findings that argue against the existence of a single syndrome with reciprocal changes in fat. Compared with controls, the similar pattern of decreased fat seen in HIV-infected men both with and without the clinical syndrome of lipoatrophy suggests that the clinical syndrome of lipoatrophy represents only the most severely affected group of the spectrum. Finally, ARV drugs that were associated with lipoatrophy, as assessed by volume of subcutaneous adipose tissue in the leg, did not appear to be associated with central lipohypertrophy, as assessed by volume of VAT. Thus, these data suggest that future research studies of fat distribution in HIV-infected persons should focus on subcutaneous lipoatrophy and that direct measurements of regional adipose tissue (rather than surveys or subjective examination) should be used to determine cause and associated metabolic findings.
Acknowledgments
Supported by National Institutes of Health grants RO1-DK57508, HL74814, HL 53359, and AI 027767 and NIH GCRC grants M01-RR00036, RR00051, RR00052, RR00054, RR0636, and RR00865. The funding agency reviewed the study design but played no role in collection, management, analysis, or interpretation of the data or in preparation of the manuscript. NIH personnel participated as members of the CARDIA
APPENDIX
Writing Team
Peter Bacchetti, Barbara Gripshover, Carl Grunfeld, Steven Heymsfield, Heather McCreath, Dennis Osmond, Michael Saag, Rebecca Scherzer, Michael Shlipak, Phyllis Tien.
Sites and Investigators
University Hospitals of Cleveland (Barbara Gripshover); Tufts University (Abby Shevitz and Christine Wanke); Stanford University (Andrew Zolopa and Lisa Gooze); University of Alabama at Birmingham (Michael Saag and Barbara Smith); John Hopkins University (Joseph Cofrancesco and Adrian Dobs); University of Colorado Heath Sciences Center (Constance Benson and Lisa Kosmiski); University of North Carolina at Chapel Hill (Charles van der Horst); University of California at San Diego (W. Christopher Matthews and Daniel Lee); Washington University (William Powderly and Kevin Yarasheski); VA Medical Center, Atlanta (David Rimland); University of California at Los Angeles (Judith Currier and Matthew Leibowitz); VA Medical Center, New York (Michael Simberkoff and Juan Bandres); VA Medical Center, Washington, DC (Cynthia Gibert and Fred Gordin); St. Luke’s-Roosevelt Hospital Center (Donald Kotler and Ellen Engelson); University of California at San Francisco (Morris Schambelan and Kathleen Mulligan); Indiana University (Michael Dube); Kaiser Permanente, Oakland (Stephen Sidney); University of Alabama at Birmingham (Cora E. Lewis).
Data Coordinating Center
University of Alabama, Birmingham (O. Dale Williams, Heather McCreath, Charles Katholi, George Howard, Tekeda Ferguson, and Anthony Goudie).
Image Reading Center
St. Luke’s-Roosevelt Hospital Center (Steven Heymsfield, Jack Wang, Mark Punyanitya).
Office of the Principal Investigator
University of California, San Francisco, Veterans Affairs Medical Center, and the Northern California Institute for Research and Development (Carl Grunfeld, Phyllis Tien, Peter Bacchetti, Dennis Osmond, Andrew Avins, Michael Shlipak, Rebecca Scherzer, Mae Pang, Heather Southwell).
References
- 1.Safrin S, Grunfeld C. Fat distribution and metabolic changes in patients with HIV infection. AIDS. 1999;13:2493–2505. doi: 10.1097/00002030-199912240-00002. [DOI] [PubMed] [Google Scholar]
- 2.Lo JC, Mulligan K, Tai VW, et al. “Buffalo hump” in men with HIV-1 infection. Lancet. 1998;351:867–870. doi: 10.1016/S0140-6736(97)11443-X. [DOI] [PubMed] [Google Scholar]
- 3.Miller KD, Jones E, Yanovski JA, et al. Visceral abdominal-fat accumulation associated with use of indinavir. Lancet. 1998;351:871–875. doi: 10.1016/S0140-6736(97)11518-5. [DOI] [PubMed] [Google Scholar]
- 4.Miller KK, Daly PA, Sentochnik D, et al. Pseudo-Cushing’s syndrome in human immunodeficiency virus-infected patients. Clin Infect Dis. 1998;27:68–72. doi: 10.1086/514638. [DOI] [PubMed] [Google Scholar]
- 5.Viraben R, Aquilina C. Indinavir-associated lipodystrophy. AIDS. 1998;12:F37–F39. doi: 10.1097/00002030-199806000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Carr A, Samaras K, Burton S, et al. A syndrome of peripheral lipodystrophy, hyperlipidaemia and insulin resistance in patients receiving HIV protease inhibitors. AIDS. 1998;12:F51–F58. doi: 10.1097/00002030-199807000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Striker R, Conlin D, Marx M, et al. Localized adipose tissue hypertrophy in patients receiving human immunodeficiency virus protease inhibitors. Clin Infect Dis. 1998;27:218–220. doi: 10.1086/517682. [DOI] [PubMed] [Google Scholar]
- 8.Shaw AJ, McLean KA, Evans BA. Disorders of fat distribution in HIV infection. Int J STD AIDS. 1998;9:595–599. doi: 10.1258/0956462981921189. [DOI] [PubMed] [Google Scholar]
- 9.Engelson ES, Kotler DP, Tan Y, et al. Fat distribution in HIV-infected patients reporting truncal enlargement quantified by whole-body magnetic resonance imaging. Am J Clin Nutr. 1999;69:1162–1169. doi: 10.1093/ajcn/69.6.1162. [DOI] [PubMed] [Google Scholar]
- 10.Saint-Marc T, Partisani M, Poizot-Martin I, et al. A syndrome of peripheral fat wasting (lipodystrophy) in patients receiving long-term nucleoside analogue therapy. AIDS. 1999;13:1659–1667. doi: 10.1097/00002030-199909100-00009. [DOI] [PubMed] [Google Scholar]
- 11.Madge S, Kinloch-de-Loes S, Mercey D, et al. Lipodystrophy in patients naive to HIV protease inhibitors. AIDS. 1999;13:735–737. doi: 10.1097/00002030-199904160-00020. [DOI] [PubMed] [Google Scholar]
- 12.Gervasoni C, Ridolfo AL, Trifiro G, et al. Redistribution of body fat in HIV-infected women undergoing combined antiretroviral therapy. AIDS. 1999;13:465–471. doi: 10.1097/00002030-199903110-00004. [DOI] [PubMed] [Google Scholar]
- 13.Dong KL, Bausserman LL, Flynn MM, et al. Changes in body habitus and serum lipid abnormalities in HIV-positive women on highly active antiretroviral therapy (HAART) J Acquir Immune Defic Syndr. 1999;21:107–113. [PubMed] [Google Scholar]
- 14.Christeff N, Melchior JC, de Truchis P, et al. Lipodystrophy defined by a clinical score in HIV-infected men on highly active antiretroviral therapy: correlation between dyslipidaemia and steroid hormone alterations. AIDS. 1999;13:2251–2260. doi: 10.1097/00002030-199911120-00007. [DOI] [PubMed] [Google Scholar]
- 15.Saint-Marc T, Partisani M, Poizot-Martin I, et al. Fat distribution evaluated by computed tomography and metabolic abnormalities in patients undergoing antiretroviral therapy: preliminary results of the LIPOCO study. AIDS. 2000;14:37–49. doi: 10.1097/00002030-200001070-00005. [DOI] [PubMed] [Google Scholar]
- 16.Mallal SA, John M, Moore CB, et al. Contribution of nucleoside analogue reverse transcriptase inhibitors to subcutaneous fat wasting in patients with HIV infection. AIDS. 2000;14:1309–1316. doi: 10.1097/00002030-200007070-00002. [DOI] [PubMed] [Google Scholar]
- 17.Thiebaut R, Daucourt V, Mercie P, et al. Lipodystrophy, metabolic disorders, and human immunodeficiency virus infection: Aquitaine Cohort, France, 1999. Groupe d’Epidemiologie Clinique du Syndrome d’Immunodeficience Acquise en Aquitaine. Clin Infect Dis. 2000;31:1482–1487. doi: 10.1086/317477. [DOI] [PubMed] [Google Scholar]
- 18.Tsiodras S, Mantzoros C, Hammer S, et al. Effects of protease inhibitors on hyperglycemia, hyperlipidemia, and lipodystrophy: a 5-year cohort study. Arch Intern Med. 2000;160:2050–2056. doi: 10.1001/archinte.160.13.2050. [DOI] [PubMed] [Google Scholar]
- 19.Polo R, Verdejo J, Martinez-Rodriguez S, et al. Lipoatrophy, fat accumulation, and mixed syndrome in protease inhibitor-naive HIV-infected patients. J Acquir Immune Defic Syndr. 2000;25:284–286. doi: 10.1097/00126334-200011010-00014. [DOI] [PubMed] [Google Scholar]
- 20.Lichtenstein KA, Ward DJ, Moorman AC, et al. Clinical assessment of HIV-associated lipodystrophy in an ambulatory population. AIDS. 2001;15:1389–1398. doi: 10.1097/00002030-200107270-00008. [DOI] [PubMed] [Google Scholar]
- 21.Martinez E, Mocroft A, Garcia-Viejo MA, et al. Risk of lipodystrophy in HIV-1-infected patients treated with protease inhibitors: a prospective cohort study. Lancet. 2001;357:592–598. doi: 10.1016/S0140-6736(00)04056-3. [DOI] [PubMed] [Google Scholar]
- 22.van der Valk M, Gisolf EH, Reiss P, et al. Increased risk of lipodystrophy when nucleoside analogue reverse transcriptase inhibitors are included with protease inhibitors in the treatment of HIV-1 infection. AIDS. 2001;15:847–855. doi: 10.1097/00002030-200105040-00005. [DOI] [PubMed] [Google Scholar]
- 23.Chene G, Angelini E, Cotte L, et al. Role of long-term nucleoside-analogue therapy in lipodystrophy and metabolic disorders in human immunodeficiency virus-infected patients. Clin Infect Dis. 2002;34:649–657. doi: 10.1086/338811. [DOI] [PubMed] [Google Scholar]
- 24.Saves M, Raffi F, Capeau J, et al. Factors related to lipodystrophy and metabolic alterations in patients with human immunodeficiency virus infection receiving highly active antiretroviral therapy. Clin Infect Dis. 2002;34:1396–1405. doi: 10.1086/339866. [DOI] [PubMed] [Google Scholar]
- 25.Lichtenstein KA, Delaney KM, Armon C, et al. Incidence of and risk factors for lipoatrophy (abnormal fat loss) in ambulatory HIV-1-infected patients. J Acquir Immune Defic Syndr. 2003;32:48–56. doi: 10.1097/00126334-200301010-00007. [DOI] [PubMed] [Google Scholar]
- 26.Collins E, Wagner C, Walmsley S. Psychosocial impact of the lipodystrophy syndrome in HIV infection. AIDS Read. 2000;10:546–550. [PubMed] [Google Scholar]
- 27.Duran S, Saves M, Spire B, et al. Failure to maintain long-term adherence to highly active antiretroviral therapy: the role of lipodystrophy. AIDS. 2001;15:2441–2444. doi: 10.1097/00002030-200112070-00012. [DOI] [PubMed] [Google Scholar]
- 28.Ammassari A, Antinori A, Cozzi-Lepri A, et al. Relationship between HAART adherence and adipose tissue alterations. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S140–S144. doi: 10.1097/00126334-200212153-00011. [DOI] [PubMed] [Google Scholar]
- 29.Carr A, Samaras K, Thorisdottir A, et al. Diagnosis, prediction, and natural course of HIV-1 protease-inhibitor-associated lipodystrophy, hyperlipidaemia, and diabetes mellitus: a cohort study. Lancet. 1999;353:2093–2099. doi: 10.1016/S0140-6736(98)08468-2. [DOI] [PubMed] [Google Scholar]
- 30.Carr A, Miller J, Law M, et al. A syndrome of lipoatrophy, lactic acidaemia and liver dysfunction associated with HIV nucleoside analogue therapy: contribution to protease inhibitor-related lipodystrophy syndrome. AIDS. 2000;14:F25–F32. doi: 10.1097/00002030-200002180-00001. [DOI] [PubMed] [Google Scholar]
- 31.Galli M, Ridolfo AL, Adorni F, et al. Body habitus changes and metabolic alterations in protease inhibitor-naive HIV-1-infected patients treated with two nucleoside reverse transcriptase inhibitors. J Acquir Immune Defic Syndr. 2002;29:21–31. doi: 10.1097/00126334-200201010-00003. [DOI] [PubMed] [Google Scholar]
- 32.Galli M, Cozzi-Lepri A, Ridolfo AL, et al. Incidence of adipose tissue alterations in first-line antiretroviral therapy: the LipoICoNa Study. Arch Intern Med. 2002;162:2621–2628. doi: 10.1001/archinte.162.22.2621. [DOI] [PubMed] [Google Scholar]
- 33.Carr A, Samaras K, Chisholm DJ, et al. Pathogenesis of HIV-1-protease inhibitor-associated peripheral lipodystrophy, hyperlipidaemia, and insulin resistance. Lancet. 1998;351:1881–1883. doi: 10.1016/S0140-6736(98)03391-1. [DOI] [PubMed] [Google Scholar]
- 34.Carr A, Emery S, Law M, et al. An objective case definition of lipodystrophy in HIV-infected adults: a case-control study. Lancet. 2003;361:726–735. doi: 10.1016/s0140-6736(03)12656-6. [DOI] [PubMed] [Google Scholar]
- 35.Carter VM, Hoy JF, Bailey M, et al. The prevalence of lipodystrophy in an ambulant HIV-infected population: it all depends on the definition. HIV Med. 2001;2:174–180. doi: 10.1046/j.1468-1293.2001.00073.x. [DOI] [PubMed] [Google Scholar]
- 36.Moyle G. Lipodystrophy: lack of agreement on definition and etiology presents a challenge to research and therapy. AIDS Read. 2002;12:438, 440–432. [PubMed] [Google Scholar]
- 37.Tien PC, Cole SR, Williams CM, et al. Incidence of lipoatrophy and lipohypertrophy in the Women’s Interagency HIV Study. J Acquir Immune Defic Syndr. 2003;34:461–466. doi: 10.1097/00126334-200312150-00003. [DOI] [PubMed] [Google Scholar]
- 38.Palella FJ, Jr, Cole SR, Chmiel JS, et al. Anthropometrics and examiner-reported body habitus abnormalities in the multicenter AIDS cohort study. Clin Infect Dis. 2004;38:903–907. doi: 10.1086/381684. Epub 2004 Mar 2001. [DOI] [PubMed] [Google Scholar]
- 39.Hughes GH, Cutter G, Donahue R, et al. Recruitment in the Coronary Artery Disease Risk Development in Young Adults (Cardia) Study. Control Clin Trials. 1987;8(4 Suppl):68S–73S. doi: 10.1016/0197-2456(87)90008-0. [DOI] [PubMed] [Google Scholar]
- 40.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 41.Sidney S, Jacobs DR, Jr, Haskell WL, et al. Comparison of two methods of assessing physical activity in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Epidemiol. 1991;133:1231–1245. doi: 10.1093/oxfordjournals.aje.a115835. [DOI] [PubMed] [Google Scholar]
- 42.Hoegerman GS, Lewis CE, Flack J, et al. Lack of association of recreational cocaine and alcohol use with left ventricular mass in young adults. The Coronary Artery Risk Development in Young Adults (CARDIA) study. J Am Coll Cardiol. 1995;25:895–900. doi: 10.1016/0735-1097(94)00469-7. [DOI] [PubMed] [Google Scholar]
- 43.Hill JO, Sidney S, Lewis CE, et al. Racial differences in amounts of visceral adipose tissue in young adults: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Am J Clin Nutr. 1999;69:381–387. doi: 10.1093/ajcn/69.3.381. [DOI] [PubMed] [Google Scholar]
- 44.Gallagher D, Belmonte D, Deurenberg P, et al. Organ-tissue mass measurement allows modeling of REE and metabolically active tissue mass. Am J Physiol. 1998;275:E249–E258. doi: 10.1152/ajpendo.1998.275.2.E249. [DOI] [PubMed] [Google Scholar]
- 45.Shen W, Wang Z, Tang H, et al. Volume estimates by imaging methods: model comparisons with visible woman as the reference. Obes Res. 2003;11:217–225. doi: 10.1038/oby.2003.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Efron B, Tibshirani R. An Introduction to the Bootstrap. London: Chapman and Hall; 1993. [Google Scholar]
- 47.Kotler DP, Rosenbaum K, Wang J, et al. Studies of body composition and fat distribution in HIV-infected and control subjects. J Acquir Immune Defic Syndr Hum Retrovirol. 1999;20:228–237. doi: 10.1097/00042560-199903010-00003. [DOI] [PubMed] [Google Scholar]
- 48.Ogiwara H, Takahashi S, Kato Y, et al. Diminished visceral adipose tissue in cancer cachexia. J Surg Oncol. 1994;57:129–133. doi: 10.1002/jso.2930570211. [DOI] [PubMed] [Google Scholar]
- 49.Zamboni M, Armellini F, Turcato E, et al. Body fat distribution before and after weight gain in anorexia nervosa. Int J Obes Relat Metab Disord. 1997;21:33–36. doi: 10.1038/sj.ijo.0800357. [DOI] [PubMed] [Google Scholar]