Summary
The mitogenic toxin from Pasteurella multocida (PMT) is a member of the dermonecrotic toxin family, which includes toxins from Bordetella, E. coli and Yersinia. Members of the dermonecrotic toxin family modulate G-protein targets in host cells through selective deamidation and/or transglutamination of a critical active site glutamine residue in the G-protein target, which results in activation of the intrinsic GTPase activity. Structural and biochemical data point to the uniqueness of PMT among these toxins in its structure and action. Whereas the other dermonecrotic toxins act on small Rho GTPases, PMT acts on the α subunits of heterotrimeric Gq, Gi and G12/13 protein families. To date, experimental evidence support a model whereby PMT potently stimulates various mitogenic and survival pathways through activation of Gq and G12/13 signaling, ultimately leading to cellular proliferation, while strongly inhibiting pathways involved in cellular differentiation through activation of Gi signaling. The resulting cellular outcomes account for the global physiological effects observed during infection with toxinogenic P. multocida, as well as hint at potential long-term sequelae that may result from PMT exposure.
Keywords: dermonecrotic toxin, G protein, signal transduction, receptor-mediated endocytosis, deamidation, transglutamination, membrane translocation, cysteine protease, atrophic rhinitis, adipogenesis, mitogenesis, SseI, osteogenesis, pasteurellosis
1. Introduction
Protein toxins have long been known to constitute key virulence determinants for pathogenic bacteria. Recent advances in our understanding of the structural and biochemical basis for the effects of these toxins on various host signaling pathways have provided interesting and sometimes surprising insights into the molecular mechanisms of the pathogenic consequences from exposure to these toxins. Such knowledge has identified toxins as important tools for studying fundamental problems in biology and has also enabled the potential use of these toxins for biomedical applications and as research tools. The emergence of antibiotic resistant, toxin-producing bacteria, along with the heightened awareness of biosecurity threats since 2001, have provided strong impetus to renew our efforts toward understanding toxin-mediated disease processes and discovering alternative antitoxin strategies [1, 2].
A prominent and prevalent group of bacterial toxins is comprised of large multi-partite proteins (called A-B toxins) that act intracellularly on their targets to modulate host signal transduction and physiological processes. The functional B components (domains or subunits) of A-B toxins bind to host cell receptors and facilitate cellular uptake and delivery of the functional A components into the cytosol, where the A components gain access to and interact with their cellular target or targets to cause toxic effects on the host cell. For a large family of A-B toxins, the intracellular targets are G proteins [3], i.e., GTPases that act as regulatory proteins in eukaryotic cell signaling processes by cycling between an inactive GDP-bound state and an active GTP-bound state. Most A-B toxins modulate their G-protein substrates by locking them, through covalent modification, into either an inactive or an active conformation, thus affecting the downstream signaling pathways.
Members of the dermonecrotic toxin family modulate their G-protein targets through selective deamidation and/or transglutamination of an active site glutamine residue, which results in activation of the intrinsic GTPase activity [3]. The cytotoxic necrotizing factors from E. coli (CNF1, CNF2, and CNF3) and Yersinia (CNFY) and the dermonecrotic toxin from Bordetella spp. (DNT) modify and constitutively activate certain members of the Rho family of small regulatory GTPases, namely RhoA, Rac1 and Cdc42 [4–8] [9–12]. Both CNF1 and CNF2, an presumably CNF3, deamidate a specific Gln residue (Gln-63) of RhoA, as well as Gln-61 of Rac1 and Cdc42 [8, 13–15], while CNFY modifies RhoA but not Rac1 or Cdc42 [16] and DNT activates these proteins primarily through transglutamination of the same Gln residue [15, 17]. This active site Gln residue is located in the switch II region of the G protein and is essential for GTPase activity.
Recently, the potent mitogenic toxin from Pasteurella multocida (PMT) joined this group of G-protein-deamidating dermonecrotic toxins, but instead of acting on small Rho GTPases, PMT stimulates various host signal transduction pathways by activating the α subunits of heterotrimeric G proteins of the Gq, Gi and G12/13 families (reviewed in [3]). In these Gα proteins, PMT deamidates an active site Gln residue (Gln-209 in Gαq, Gln-205 in Gαi), which is functionally equivalent to the Gln that is deamidated by the CNFs and DNT [18]. For all of these cases, toxin-catalyzed deamidation or transglutamination of the target inhibits the intrinsic GTPase activity and leads to persistent activation of the regulatory G protein. Although they catalyze the same deamidating reaction on related G-protein targets and with overlapping cellular outcomes, the sequence and structure of the activity domain of PMT differs considerably from that of the other dermonecrotic toxins [3] and points to a clear functional example of convergent toxin evolution. In this review, we will focus on PMT and our current understanding of the structure-function, mechanism of action, and cellular consequences of this newest member of the G-protein-deamidating dermonecrotic toxin family.
2. Epizootic and zoonotic diseases associated with toxinogenic Pasteurella multocida
Toxinogenic P. multocida is associated with the severest forms of dermonecrosis and pasteurellosis in livestock and other domestic and wild animals [19–22], and is the primary etiological agent of progressive atrophic rhinitis (AR), a disease characterized by destruction of the nasal turbinate bones in pigs, rabbits and other animals [20–26]. While in swine the primary disease manifestation is AR [23], in other animals, such as cattle and rabbits, other symptoms may be more pronounced, including respiratory distress in cattle (bovine respiratory disease) or pneumonia (often referred to as pasteurellosis) in rabbits (snuffles) and abscess formation [20, 27–29]. Systemic effects of toxinogenic P. multocida in most animal species include nasal, testicular and splenic atrophy, hepatic necrosis, renal impairment, leukocytosis, symptoms of pneumonia, overall weight loss, growth retardation and death [20, 23, 28, 30–36]. Toxinogenic P. multocida can also affect humans that have contact with infected animals, particularly through respiratory exposure or bite wounds [37–46]. Toxinogenic P. multocida is therefore considered a causative agent of both epizootic and zoonotic diseases [37, 47–50].
3. Pasteurella multocida toxin and disease
A 1285 amino acid (146-kDa) protein toxin (PMT) associated with serotype D and some A strains of Pasteurella multocida is the major virulence factor responsible for bone resorption of nasal turbinates in progressive AR [23, 50], liver necrosis [25, 30, 31, 51], spleen atrophy [23, 31, 52], swelling of the kidneys [25], pneumonia [31], reduced body weight and fat [30, 53], and growth retardation [36, 54, 55]. PMT appears to cause AR through disruption of bone biogenesis and degradation processes, which are mediated by the bone-generating osteoblasts and macrophage-like osteoclasts, respectively [56–58]. In vivo, PMT intoxication stimulates differentiation of preosteoclasts into osteoclasts [59, 60] and promotes osteoclast proliferation, which in turn causes bone resorption [60]. In vitro, PMT stimulates osteoclastic bone resorption [57, 61, 62], while also inhibiting osteoblast differentiation [58, 62–64] and bone regeneration by osteoblasts [57, 58, 64].
4. Cellular activity of PMT
Intoxication of mammalian cells by PMT induces strong mitogenic [65–67] and anti-apoptotic effects [68–70] in various cell lines. The cellular effects of PMT are induced by the activation of heterotrimeric G proteins of at least three different families (Gq, Gi, and G12/13), which lead to mitogenic responses through increased intracellular Ca2+ and inositol phosphate levels due to activation of phospholipase Cβ (PLCβ) [71, 72] and activation of Rho-dependent cytoskeletal signaling [73–75], while concurrently shutting off cAMP-dependent signaling pathways leading to differentiation [68, 76].
Some of the intracellular events that occur upon exposure to PMT are: enhanced hydrolysis of inositolphospholipids to increase the total intracellular content of inositol phosphates [71, 72] increased production of diacylglycerol [77], mobilization of intracellular Ca2+ pools [68, 71, 72, 78]; interconversion of GRP78/BiP [79]; and activation of protein kinase C-dependent and -independent phosphorylation [66, 67, 70, 77, 80–82]. Activation of these pathways leads to subsequent alteration of downstream gene expression by activation of Ca2+ [68, 78, 83], MAPK [66, 67, 83, 84] and JAK/STAT [85–87] signaling pathways and inhibition of Gs-mediated signaling pathways. A summary of the various intracellular signal transduction pathways affected by PMT treatment is shown in Figure 1. We will explore in turn the action of PMT on each of these signaling pathways.
Figure 1. Known intracellular signaling pathways involved in PMT action on host cells.
Overall cellular outcomes that are enhanced by PMT are indicated in red boxes, while outcomes that are blocked by PMT are indicated in blue boxes. Known direct target substrates of PMT (Gαq, Gαi and Gα12/13) are indicated in yellow. Arrows point in the direction of positive/activation of the signaling pathway, while barred lines indicate negative/inhibition of the signaling pathway. Solid lines indicate interactions that are known to be direct, while dashed lines indicate indirect interactions or effects. Pi indicates phosphorylation of the signaling molecule. Abbreviations: GsPCR, Gs-protein coupled receptor; GiPCR, Gi-protein coupled receptor; GqPCR, Gq-protein coupled receptor; G12/13PCR, G12/13-protein coupled receptor; PDGFR, platelet-derived growth factor receptor; EGFR, epidermal growth factor receptor; PPAR, peroxisome-proliferator activated receptor; GIRK, G-protein-coupled inward-rectifying K+ channel; AC, adenylate cyclase; PKA, cAMP-dependent protein serine/threonine kinase A; PKD, DAG-dependent serine/threonine protein kinase D; C/EBP, CAATT-enhancer binding protein; Pref1, preadipocyte factor 1; JAK, Janus tyrosine protein kinase; STAT, signal transducer and activator of transcription; SOCS, suppressors of cytokine signaling; Cox-2, cyclooxygenase-2; Pim-1, Pim serine/threonine protein kinase-1; PI3K, phosphatidylinositol 3-kinase; PDK1, phosphoinositide-dependent protein kinase 1; Akt, (also PKB) serine/threonine protein kinase; Frizzled, Wnt-activated G-protein coupled receptor; β-catenin, subunit of the cadherin adherens junction protein complex; Bcl-2, B-cell lymphoma 2 anti-apoptotic protein; NFAT, nuclear factor of activated T cells transcription factor; CN, calcium-calmodulin-dependent calcineurin protein phosphatase; CaM, calcium-dependent calmodulin; MLCK, myosin light chain kinase (serine/threonine protein kinase); MLCPase, myosin light chain phosphatase; Ras, Ras small regulatory GTPase; RhoA, RhoA small regulatory GTPase; Rac, Rac1 small regulatory GTPase; CDC42, Cdc42 small regulatory GTPase; RhoK, Rho kinase ROKα; FAK, p125FAK focal adhesion tyrosine protein kinase; paxillin, focal adhesion adaptor protein; PLCβ, phosphatidylinositol-dependent phospholipase C β isoform; PKC, calcium-dependent serine/threonine protein kinase C; nPCK, novel PKC; Raf, Ras-activated factor serine/threonine protein kinase; Grb2, growth factor receptor-bound adaptor protein 2; Sos, son of sevenless guanine nucleotide exchange factor for Ras; MAPK, mitogen-activated protein serine/threonine protein kinase; MEK, MAPK serine/threonine protein kinase; Erk1/2, (also p42/p44 MAPK) extracellular signal-regulated serine/threonine protein kinase; JNK, (also MAPK10) c-Jun N-terminal serine/threonine protein kinase; RSK, ribosomal S6 serine/threonine protein kinase; CREB, cAMP responsive element binding protein 1 transcription factor.
Calcium Signaling
Exposure of cultured fibroblasts and osteoblasts to PMT results in the activation of phosphatidylinositol-specific phospholipase C (PLCβ) [58, 71, 77], which in turn triggers hydrolysis of phosphatidylinositol 4,5-bisphosphate (PIP2) to increase intracellular levels of inositol 1,3,5-trisphosphate (IP3) and diacylglycerol (DAG) and stimulates downstream Ca2+ signaling pathways. PMT strongly stimulates primarily PLCβ1 and to a lesser extent PLCβ3, but not PLCβ2 [72]. These findings are consistent with known cellular PLCβ responses elicited through Gαq-coupled receptors [88], and indeed, activation of PLCβ1 occurs through selective action of PMT on the regulatory Gαq subunit, but not the closely related Gα11 subunit [72, 84]. Discrimination between Gα11- and Gαq-mediated activation of PLCβ by PMT was attributed to the helical domain of the heterotrimeric G proteins [89], although it is not clear whether the basis for this discrimination occurs as a result of differential recognition of the Gαq versus Gα11 protein by PMT or through preferential coupling of the Gαq versus Gα11 protein to the downstream PLCβ effector protein.
The PMT-induced PLCβ response was potentiated by release of the Gαq subunit from the heterotrimeric Gαβγ complex through either dissociation of the Gαq subunit from Gβγ by using antibodies against the Gβ subunit or through sequestration of the Gβγ subunits away from the Gαqβγ heterotrimeric complex by treatment with pertussis toxin (PT) [72]. PMT action on Gαq is irreversible and persistent [72, 90] and independent of interaction with G protein-coupled receptors [90]. Indeed, PMT potentiates the PLCβ response elicited by Gαq-coupled receptors upon stimulation with bombesin, vasopressin or endothelin [91]. Furthermore, overexpression of Gαq enhanced the PMT-induced response, while decreased expression of Gαq or treatment with the GDP analogue, GDPβS, which locks G proteins in their inactive form, blocked the PMT-induced response [72], supporting the monomeric form of Gαq as the preferred substrate of PMT. However, after the strong initial PMT-induced response an uncoupling of the Gαq-coupled PLCβ signaling pathway subsequently follows, such that no further stimulation occurs upon additional treatment with PMT [72].
Release of the second messengers IP3 and DAG mediated by PMT leads to stimulation of Ca2+ signaling through mobilization of intracellular Ca2+ stores [71, 72, 78, 84] and activation of Ca2+-dependent protein kinase (PKC)-catalyzed phosphorylations [70, 77], Ca2+-calmodulin (CaM)-calcineurin-dependent nuclear factor of activated T cells (NFAT) signaling [68], and Ca2+-dependent Cl− secretion [72, 92].
Mitogenic Signaling
PMT exhibits proliferative or cytopathic effects on a number of cultured cell lines. In cultured mesenchymal cells, such as murine, rat, and human fibroblasts [65–67], preadipocytes [68], and osteoblasts [57, 58], PMT elicits primarily a proliferative response, leading to the speculation that PMT can promote cancer [87, 93]. Accordingly, PMT initiates intracellular signal transduction events that result in DNA synthesis and cytoskeletal rearrangements. In agreement with these findings, PMT stimulates fibroblastic cells through the cell cycle, moving cells from the G1 phase into and through the S phase without triggering apoptosis [67]. Consistent with these observations, PMT treatment induces the expression of a number of cell cycle markers, including the protooncogene c-Myc, D and E cyclins, PCNA, p21, and the Rb proteins. Yet, continued expression of these markers is not sustained after the initial proliferative response and confluent Swiss 3T3 cells become unresponsive to further PMT treatment [67].
In contrast, PMT causes cytopathic responses in other cell types, such as cultured epithelial cells, including embryonic bovine lung (EBL) cells [94], Vero cells [67, 95, 96], cardiomyocytes [70], and osteosarcoma cells [96]. For example, confluent Vero cells undergo rapid and dramatic morphological changes upon toxin exposure [67, 95, 96]. But, PCNA and cyclins D3 and E are not upregulated in these cells upon PMT treatment, and so no cell cycle progression occurs; instead, cells arrest primarily in G1 [67].
Mitogenic signaling stimulated by PMT appears to be different for different cell types. For example, in HEK-293 cells PMT induces Ras-dependent activation of Erk mitogen-activated protein kinase (MAPK) via Gq-dependent, but PKC-independent transactivation of the epidermal growth factor (EGF) receptor [66], which was blocked by cellular expression of two inhibitors of Gq signaling, a dominant-negative mutant of the G-protein-coupled receptor kinase 2 (GRK2) and a C-terminal peptide of Gαq (residues 305–359). Consistent with this, Erk activation by PMT was insensitive to the PKC inhibitor (GF109203X), but was blocked by tyrphostin (AG1478), an EGF receptor-specific inhibitor, and by dominant negative mutants of mSos1 and Ha-Ras. In cardiac fibroblasts Erk activation by PMT also occurs via transactivation of the EGF receptor, resulting in fibrosis [70].
In cardiomyocytes, however, PMT-induced activation of Erk and to a lesser extent JNK and p38 MAPK occurs via Gq-dependent activation of PLCβ and novel PKC (nPKC) isoforms [70], resulting in cardiomyocyte hypertrophy reminescent of that induced by norepinephrine activation of Gq-coupled receptors [97]. Similar to norepinephrine, PMT suppresses activation of Akt, a serine/threonine protein kinase that is activated by Gβγ subunits and Ras GTPases, and causes apoptosis, albeit not to the extent of norepinephrine [70]. PMT also induces serine phosphorylation of p66Shc, an adapter protein of oxidative stress responses, via PKC and MEK signaling [81], suggesting that p66Shc might be a candidate mediator of PMT-enhanced apoptosis in cardiomyocytes.
On the other hand, PMT also activates anti-apoptotic pathways. For example, PMT activates protein kinase D (PKD) signaling in both cardiac fibroblasts and cardiomyocytes [82], presumably through DAG-dependent phosphorylation by nPKC [98], which leads to phosphorylation of the transcription factor cAMP response element-binding protein (CREB) and increased expression of CREB target genes such as the anti-apoptotic Bcl-2 protein.
Additional evidence pointing to the oncogenic potential of PMT is the finding that PMT treatment leads to activation of JAK/STAT signaling [86, 87]. Treatment of Swiss 3T3 cells with PMT results in Gq-dependent phosphorylation and activation of the Janus tyrosine protein kinases, JAK1 and JAK2 [87]. This is followed by JAK-mediated activation of STAT1, STAT3 and STAT5 through tyrosine phosphorylation, and at least in the case of STAT3 further activation through subsequent serine phosphorylation. PMT-stimulation of phosphorylation of STAT transcription factors leads to upregulation of cyclooxygenase 2 (Cox-2), a pro-inflammatory protein upregulated in many cancers, but downregulation of the transcription factor suppressor of cytokine signaling 3 (SOCS-3) [87]. In HEK-293 cells PMT also increases expression of the serine/threonine protein kinase Pim-1, which phosphorylates and inactivates the transcription factor SOCS-1 [86]. Phosphorylated SOCS-1 can no longer act as an E3 ubiquitin ligase to target JAK proteins for proteosomal degradation, thereby leading to increased levels of JAK.
Cytoskeletal Signaling
PMT initiates cytoskeletal rearrangements, including focal adhesion assembly and actin stress fiber development [11, 80, 99, 100]. These actin cytoskeletal rearrangements appear to be RhoA-dependent [11, 67, 73, 75, 80, 101]; however, PMT does not act directly on RhoA [6, 11, 102]. Instead, RhoA activation occurs through PMT activation of Gα12/13 [74], presumably by interaction of the Gα subunit with the RhoGEFs p115-RhoGEF, PDZ-RhoGEF, LARG, or Dbl [103–106]. RhoA activation indirectly through PMT activation of Gαq [72, 84], presumably by interaction of the Gα subunit with the regulator of G protein signaling (RGS) domain of the Rho guanine nucleotide exchange factor (RhoGEF), p63RhoGEF [107] or Lbc [75]; or. In Gαq/11-deficient fibroblasts, expression of dominant-negative Gα13 inhibited RhoA activation by PMT, whereas in Gα12/13-deficient cells expression of Gα13 restored RhoA activation by PMT [74]. Whether PMT can discriminate between the Gα12 and Gα13 proteins remains to be determined.
PMT-induced RhoA activation subsequently leads to activation of its downstream target Rho kinase (ROKα), which then phosphorylates and inactivates myosin light chain (MLC) phosphatase PP1 and thereby leads to increased levels of MLC phosphorylation [101]. The resulting MLC phosphorylation regulates actin reorganization, increasing stress fiber formation, cell retraction and endothelial cell layer permeability [101]. PMT-mediated RhoA activation also promotes to ROKα-dependent autophosphorylation of focal adhesion kinase (FAK) on Tyr-397, which is an SH2-binding site for Src tyrosine kinase [80, 100]. This binding results in formation of a FAK-Src complex that leads to further tyrosine phosphorylation of downstream adaptor proteins such as paxillin and Cas and facilitates stress fiber formation and focal adhesion assembly [80, 100].
PMT-mediated RhoA activation and subsequent disturbance of endothelial barrier function has been speculated to be responsible for the vascular effects of PMT observed in dermonecrotic lesions from bite wounds [73]. This is consistent with histological observations showing evidence of endothelial damage by influx of neutrophils and increased attachment of thrombocytes to blood vessels surrounding PMT-induced dermal lesions [108].
cAMP signaling
In addition to activation of Gαq and Gα12/13 signaling, PMT treatment inhibits adenylyl cyclase activity through activation of Gαi [76], converting it into a PT-insensitive state. Capitalizing on the fact that the preferred substrate of PT-catalyzed ADP-ribosylation is the heterotrimeric Gαiβγ complex, and not the monomeric Gαi [109], it was found that PMT action on the Gαi protein interferes with the interaction of Gαi and its cognate Gβγ subunits and thereby prevents ADP-ribosylation by PT [76], resulting in activation and subsequent uncoupling of Gαi signaling. In this study, PMT treatment of intact wild-type mouse embryonic fibroblasts, as well as cells deficient in Gαq/11 or Gα12/13, resulted in inhibition of cAMP accumulation through isoproterenol stimulation of Gs-coupled receptors or through forskolin stimulation of adenylate cyclase activity, while enhancing the inhibition of cAMP accumulation by lysophosphatidic acid (LPA) through Gi-coupled receptors. While PT treatment blocked LPA-mediated inhibition of cAMP accumulation, it did not block PMT-mediated activation of Gαi or inhibition of cAMP accumulation. The observation that PMT overrides the action of PT suggests that PMT may also be able to act on the heterotrimeric Gαiβγ complex.
The effect of PMT on the GTPase activity of the Gαi subunit has also been studied. PMT treatment of cells not only reduced both basal and LPA-induced hydrolysis of GTP by the Gαi protein in membrane preparations, but also inhibited LPA-receptor-stimulated binding of GTPγS to Gαi [76], suggesting that PMT locks the Gαi subunit in its monomeric active form. The finding that pretreatment of cells with PMT prevented PT-induced ADP-ribosylation of Gαi2 is in keeping with the proposed model where PMT acts on the Gα subunit to irreversibly convert it into an active state that can no longer interact with its cognate Gβγ subunits [72]. This effectively shifts the equilibrium to dissociate the heterotrimeric complex and release the Gβγ subunits, which can then interact with their downstream effector proteins, such as phosphoinositide 3-kinase γ (PI3Kγ). Activation of PI3Kγ generates PIP3 that activates phosphoinositide-dependent protein kinase 1 (PDK1), which then phosphorylates Akt and upregulates Pim-1 expression, thereby stimulating survival pathways while inhibiting apoptotic pathways [69].
Adipogenesis
PMT prevents adipocyte differentiation and blocks adipogenesis [68]. After hormonal stimulation with a combination of insulin, dexamethasone and isobutylmethylxanthine, confluent 3T3-L1 fibroblastic preadipocyte cells are induced to differentiate by first entering a mitotic clonal expansion stage with increased expression of cell cycle markers such as cyclins and c-Myc, which is then followed by subsequent growth arrest and terminal differentiation into mature adipocytes containing abundant lipid droplets [110], which are visualized by Oil Red O staining. PMT completely blocks this process in 3T3-L1 cells [68].
During adipocyte differentiation Notch1 signaling plays a pivotal role in regulating expression of adipocyte-specific markers [111]. The transcription factors peroxisomal proliferator-activated receptor (PPARγ) and CAATT enhancer-binding protein (C/EBPα), are upregulated [110], while preadipocyte-specific markers, such as Pref1 [112], and Wnt/β-catenin signaling [113] are downregulated. PMT prevents expression of PPARγ and C/EBPα in 3T3-L1 preadipocytes and downregulated expression of PPARγ and C/EBPα in mature adipocytes [68]. PMT completely downregulates Notch1 levels, yet maintains high levels of Pref1 and β-catenin [68].
Although the connection between Gq-dependent Ca2+ signaling and Notch1 signaling in adipogenesis is not fully understood, Gq-mediated Ca2+ signaling blocks adipogenesis through activation of the Ca2+/calmodulin-dependent serine/threonine phosphatase calcineurin [114, 115]. However, the inhibitory effects of PMT on differentiation and Notch1 could not be reversed by treatment with the calcineurin inhibitor cyclosporin A, suggesting that PMT-mediated blockade of adipocyte differentiation must occur through multiple pathways. PMT activation of Gi signaling, which would block Gs-mediated differentiation, might account for these inhibitory effects. These results regarding PMT action on adipogenesis may account in part for the decreased weight gain and growth retardation observed in animals exposed to PMT [30, 36, 53–55, 96].
Osteogenesis
Natural or experimental exposure to PMT in animals causes bone loss in nasal turbinates [116, 117], calvaria [61] and long bones [60]. In tissue culture, PMT stimulates proliferation of primary mouse calvaria and bone marrow cells [57, 58, 60], while inhibiting differentiation of osteoblasts to bone nodules through activation of the RhoA-ROKα signaling pathway [63]. PMT downregulates the expression of several markers of osteoblast differentiation, including alkaline phosphatase and type I collagen [57]. Overall bone loss mediated by osteoclasts appears to require interaction of PMT-stimulated osteoblasts [58], presumably through cytokines released by activation of the osteoblasts [62]. While PMT appears to stimulate preosteoclasts (bone marrow progenitor cells) to differentiate into osteoclasts [59], it was recently shown that PMT-induced osteoclastogenesis is mediated indirectly through a subset of B cells that are activated by PMT to produce osteoclastogenic factors and cytokines [85].
The Notch1 signaling pathway also plays an important role in regulation of osteogenesis by blocking osteoblastic cell differentiation [111, 118]. The observation that PMT downregulates Notch1, while maintaining β-catenin levels to blocking adipogenesis [68], suggests that these signaling pathways may also play a role in PMT-induced bone resorption.
Immune Signaling
Even though immunization with PMT toxoid affords protection [119–124], naturally occurring AR is characterized by an overall lack of immune response against PMT [125–128]. Immunization with killed toxigenic P. multocida bacteria generated only low levels of toxin-neutralizing antibodies [53, 120, 129]. Although PMT activates dendritic cells [125, 130], it is a poor immunogen and appears to suppress the antibody response in vivo [125–127] and inhibits immune cell differentiation and dendritic cell migration [63, 125, 130]. Vaccination with PMT showed lower IgG antibody responses against other antigens, including limpet hemocyanin, ovalbumin, and tetanus toxoid [126, 127], suggesting a possible role for PMT as an immunomodulator in pathogenesis.
5. PMT structure and enzyme activity
Dermonecrotic toxin family
One question of interest is the relationship between the structural similarities and the activities of PMT with the related DNT and CNFs. All three toxins cause similar, but not identical, effects on cultured cells [6, 11, 80, 99, 102]. Although there is no crystal structure for any of the full-length proteins, sequence comparisons and biochemical studies provide insights into the functional organization of these toxins. Although the precise localization of the domains responsible for receptor binding and translocation activities remains unclear, these domains are located in the N terminus of each of these toxins and share limited sequence similarities with each other [131–137] and will be discussed in more detail later in section 6. On the other hand, more is known about the intracellular activity domain, which resides in the C terminus of each toxin [14, 83, 132, 133, 138, 139]. Crystal structures of C-terminal fragments of PMT (PDB 2EBF) [139] and CNF1 (PDB 1HQ0) [138] are available and have revealed that they are quite different from each other.
The deamidase activity of CNF1 involves two essential C-terminal Cys and His residues [140], which are conserved in all members of the CNF/DNT family (Cys-866 and His-881 in CNF1, Cys-1305 and His-1320 in DNT). Since DNT and the CNFs share sequence similarity in their C-terminal domains (residues 720–1014 in the CNFs, 1176–1464 in DNT) and have common G protein targets, it is presumed that their activity domains have similar overall structures. PMT does not share any discernable sequence similarity with the C-terminal regions of DNT or the CNFs and the solved crystal structure of a biologically active C-terminal fragment of PMT (PMT-C) consisting of residues 575–1285 also showed no structural similarity [139]. The structure of PMT-C revealed three distinct domains: a C1 domain (residues 575–719) with sequence and structural similarity to the membrane-targeting domain of the clostridial toxin TcdB [141, 142]; a C2 domain (residues 720–1104) of as-yet unknown function; and a C3 domain (residues 1105–1285) with a papain-like cysteine protease structural fold that was subsequently shown to harbor the minimal domain responsible for toxin-mediated activation of Ca2+ and mitogenic signaling [83].
Comparison of PMT-C3 with TGase (Pf01841) and NAT (Pf00797) families
PMT-C3 has structural similarity with the catalytic core of transglutaminases (TGase family Pf01841) and arylamine N-acetyltransferases (NAT family Pf00797) [18]. The spatial arrangement of the active site Cys-His-Asp triad of PMT-C3 is nearly superimposable with members of the TGase and NAT families [3], including the human blood-clotting factor XIII (PDB 1FIE) [143], fish-derived TGase from red sea bream (PDB 1G0D) [144], putative TGase-like cysteine protease from Cytophaga hutchinsonnii (PDB 3ISR), and the arylamine N-acetyltransferase (NAT) from Salmonella enterica serovar Typhimurium (PDB 1E2T) [145]. The structure of PMT-C3 most closely resembles that of the protein glutaminase from Chryseobacterium proteolyticum (PDB 2ZK9) [146], which shares some weak sequence similarity with PMT-C3 and also has a Cys-His-Asp triad superimposable with this group of proteins, but does not belong to either of the TGase or NAT families. The crystal structures of another family of bacterial type 3 secretion system (T3SS) effector proteins, called CIF (cycle inhibiting factor) from E. coli (PDB 3EFY)[147] and CIF homologs from Burkholderia pseudomallai (CHBP, PDB 3EIT) [148, 149], Photorhabdus luminescens (PDB 3GQJ) [149], and Yersinia species [149], have revealed active site Cys-His-Gln/Asp motifs associated with CIF-mediated actin stress fiber formation and cell cycle arrest [150, 151]. Recently, CIF and CHBP were shown to selectively deamidate Gln-40 in ubiquitin and the ubiquitin-like protein NEDDS, thereby blocking the ubiquitination-proteosome pathway [152].
Other PMT-C3-related bacterial proteins
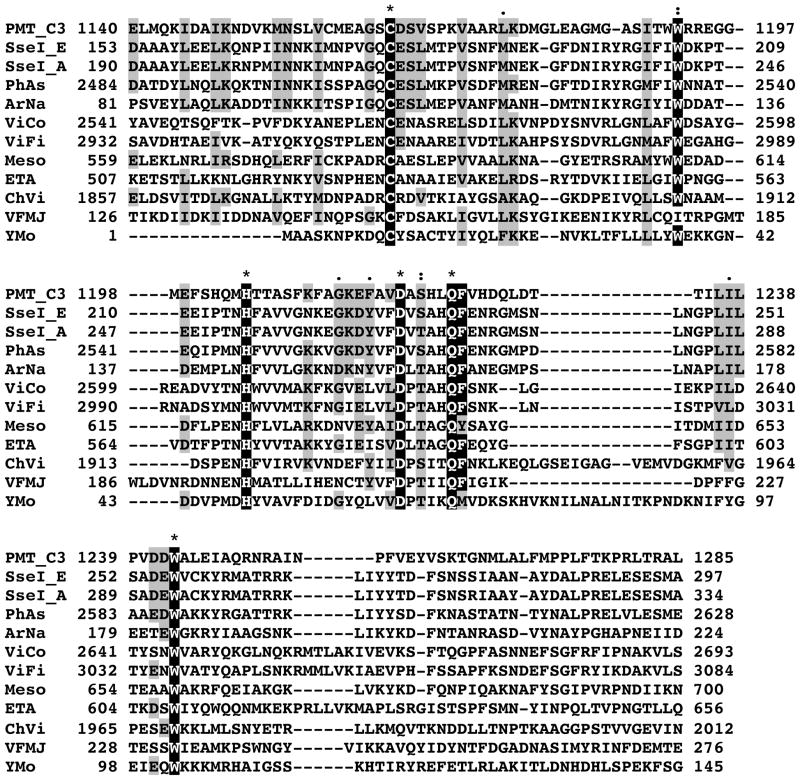
A striking finding about the group of proteins with Cys-His-Asp triads similar to that of PMT-C3 is that at the sequence level there is no discernable similarity of PMT-C3 to the proteins, with the exception of the Cryseobacterium protein glutaminase. On the other hand, there are a group of proteins with activity domains that have recognizable sequence similarity to PMT-C3 (Figure 2), even though there is no structural confirmation of this yet. Most notable are several related SPI-2 T3SS effector proteins from Salmonella enterica serovars and Arsenophonus nasoniae, an insecticidal toxin from Photorhabdus asymbiotica, and a number of hypothetical bacterial proteins from Vibrio coralliilyticus, Vibrio fischeri, Erwinia tasmaniensis, Mesorhizobium sp., Chromobacterium violaceum, and Yersinia mollaretii. Among these are the recently characterized T3SS effector proteins SseI (also called SrfH) from S. enterica serovar Typhimurium [153] and its close homologs. SseI binds to and inhibits the host factor, IQ motif-containing GTPase-activating protein 1 (IQGAP1), which in turn inhibits cytoskeletal signaling and migration of macrophages and dendritic cells, thereby preventing bacterial clearance during infection [153]. Each of these proteins share the highly conserved active site Cys-His-Asp triad found in PMT-C3, as well as additional conserved Trp and Gln-Phe residues (highlighted in Figure 2). Mutation of the active site Cys-178 to Ala in SseI results in loss of function, but not binding to IQGAP1 [153].
Figure 2. Alignment of amino acid sequences with similarity to PMT-C3.
The protein sequences were obtained from NCBI; PMT_C3: C3 domain of Pasteurella multocida toxin; SseI_E: SseI from Salmonella enterica serovar Enteritidis; SseI_A: SseI from Salmonella enterica serovar Arizonae; PhAs: insecticidal toxin from Photorhabdus asymbiotica; ArNa: secreted effector protein from Arsenophonus nasoniae; ViCo: hypothetical protein VIC_001387 from Vibrio coralliilyticus; ViFi: hypothetical protein VF_A1129 from Vibrio fischeri strain ES114; Meso: hypothetical protein Meso_3517 from Mesorhizobium sp. Strain BNC1; ETA: hypothetical protein ETA_29930 from Erwinia tasmaniensis strain Et1/99; ChVi: hypothetical protein CV_2593 from Chromobacterium violaceum; VFMJ: hypothetical protein VFMJ11_A0013 from Vibrio fischeri strain MJ11; YMo: hypothetical protein ymoll0001_35050 from Yersinia mollaretii. The numbers at the ends of each line correspond to the amino acid position in the indicated protein. The catalytic Cys-His-Asp triad as well as the highly conserved Trp and Gln-Phe residues are highlighted in black, “*” denotes identical amino acid residues; “:” denotes highly conserved residues; “.” denotes conserved residues.
Substrate specificity of PMT
The active site Gln residue located in the switch II region of GTPases serves to stabilize the pentavalent transition state for GTP hydrolysis and serves to orient the water nucleophile. Deamidation of this Gln in Gαi or Gαq by PMT constitutively activates and releases the Gα subunit from the respective heterotrimeric Gαβγ complex [18]. So far, detection of PMT-catalyzed deamidase activity of Gα proteins in vitro has proven to be a challenge, and most biochemical studies to date have relied on whole cell studies to address questions regarding substrate specificity and effects of PMT action on Gα protein interactions with its cognate Gβγ subunits, receptors, effectors, and/or regulators.
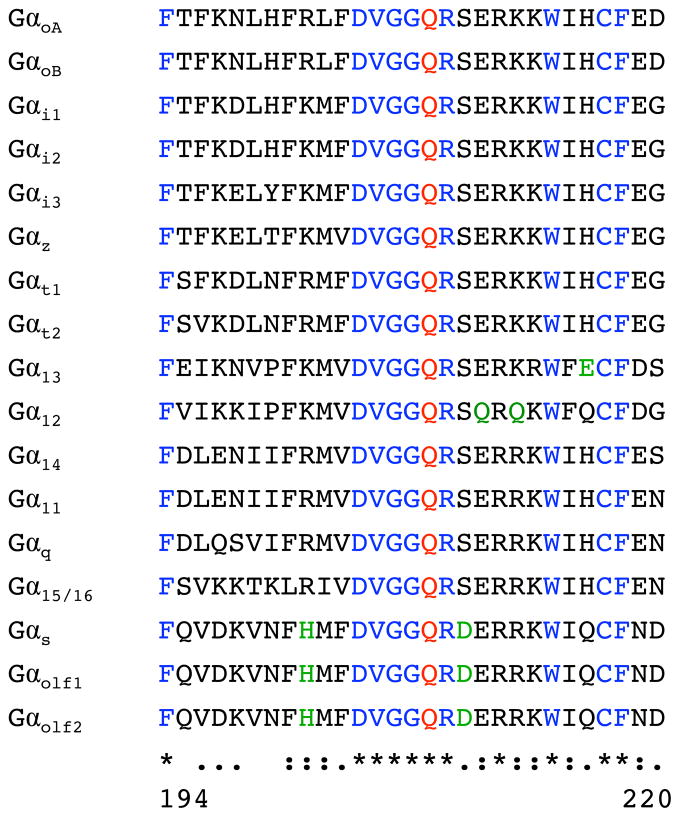
One enigmatic aspect of PMT action on its G protein substrates is the ability of PMT to discriminate among the different Gα isoforms since all of the Gα subunits have analogous active site Gln residues (equivalent to Gln-204 of Gαi1, Gln-205 of Gαi2, Gln-229 of Gα12/13, and Glu-209 of Gαq/11) and share significant sequence similarity in the flanking sequences of the switch II region (see Figure 3). It is noteworthy that Gαq and Gα11 share considerable amino acid identity (88% overall) with each other, including the switch II Gln-209 residue, yet only Gαq is a substrate for PMT [18, 84]. The reason for this difference in substrate specificity between Gαq and Gα11 is not known; however, there is some evidence that differences in substrate recognition of Gαq versus Gα11 by PMT may reside in the helical domain of the Gαprotein [89].
Figure 3. Alignment of amino acid sequences of the switch II region in the α subunits of heterotrimeric GTPases.
The protein sequences were obtained from NCBI; Gαt1 (NP_032166), Gαt2 (NP_032167), Gαi1 (NP_034435), Gαi2 (AAH65159), Gαi3 (NP_034436), GαoA (NP_034438), GαoB (P18873.3), Gαz (NP_034441), Gαs (P63094), Gαolf1 (NP_034437), Gαolf2 (NP_796111), Gα11 (NP_034431), Gαq (NP_032165), Gα14 (NP_032163), Gα15 (NP_034434), Gα12 (NP_034432), and Gα13 (NP_034433). The numbers below the alignment correspond to the amino acid positions of Gαq. The active site Gln (at position 209 in Gαq) is indicated in red, identical flanking residues in blue, and flanking residues that result in notable charge differences are indicated in green. “*” denotes identical amino acid residues; “:” denotes highly conserved residues; “.” denotes conserved residues.
Although direct deamidation of Gα12 or Gα13 by PMT has not yet been demonstrated, exogenous expression of Gα13 restored RhoA activation by PMT in Gα12/13-deficient cells in the presence of the specific Gαq inhibitor YM-254890 [74], indicating that Gα13 can serve as a substrate for PMT. PMT-mediated activation of Gα12 signaling was not tested in this study, but since both Gα12 and Gα13 share 67% overall amino acid identity and nearly identical switch II regions (Figure 3), it is possible that they could both serve as a target for PMT-mediated deamidation. However, considering that Gαq and Gα11 share even greater similarity, yet Gα11 is not a substrate of PMT, it will be interesting to see whether Gα12 is a substrate for PMT. It also remains to be determined which of the other G protein α subunits might also be targets for deamidation by PMT.
6. Cellular intoxication of PMT
Little is known about the cellular uptake mechanisms of PMT. Bacterial protein toxins are known to utilize a number of different entry routes. And, the nature of the receptor often dictates what route is taken. It has been suggested that the cellular receptor for PMT might be a ganglioside [96, 99], but the identity of the receptor(s) responsible for PMT binding to host cells remains unclear. Once PMT binds to cells, it is internalized through a receptor-mediated endocytic pathway involving a pH-dependent step [62, 65, 96]. Although the detailed mechanism of this process is lacking, the toxin is translocated from the endocytic vesicles into the cytosol, where the C-terminal activity domain gains access to its target to activate intracellular signaling.
Weak bases such as NH4Cl, chloroquine, and methylamine, which buffer the acidification of endosomes, block PMT activity on cells [65]. Bafilomycin A1, a potent and specific inhibitor of the vacuolar H+-ATPase responsible for endosomal acidification, was also found to inhibit PMT activity [154, 155]. Involvement of a low pH-dependent membrane translocation event in PMT action was further supported by entry of cell surface-bound PMT directly into cells by a low pH pulse at 4°C in the presence of bafilomycin A1 [154]. There is some evidence that a predicted helix-loop-helix motif, entailing two hydrophobic helices (residues 402–423 and 437–457) linked by a hydrophilic loop (residues 424–436), may be part of a pH-sensitive membrane translocation domain of PMT [154]. Double mutation of Asp-373 and Asp-379 in the corresponding helix-loop-helix of CNF1 resulted in complete loss of biological activity [136]. Substitution of putative pH-sensitive acidic residues in the loop (Asp-425, Asp-431, Glu-434) of PMT with Lys resulted in reduction in toxin activity, whereas mutation of Asp-401 in PMT, which is outside of the helix-loop-helix motif, completely abolished PMT activity [154].
A recent study showed that endocytosis and trafficking of PMT is dependent on the small regulatory GTPase Arf6 [155]. In this study, PMT was found to share an initial entry pathway through Arf6-containing endosomes with transferrin and cholera toxin. However, the trafficking pathways subsequently diverge, as transferrin is trafficked to recycling endosomes, cholera toxin is trafficked retrograde to the ER, and PMT is trafficked to late endosomes. Nocodazole, which causes disassembly of microtubules important for trafficking from early to late endosomes, and cytochalasin D, which disrupts actin polymerization, blocked PMT activity [155], suggesting that membrane translocation and cytotoxicity of PMT is dependent on its trafficking to late acidic endosomes. Interestingly, disruption of Golgi-ER trafficking with brefeldin A increased PMT activity, suggesting that inhibiting PMT trafficking to non-productive compartments that do not lead to translocation, enhances PMT translocation and activity.
7. Perspective
A large number of bacterial toxins act on host cell G proteins that regulate a myriad of cellular signaling pathways. Many do so through covalent modification of their targets, such as ADP-ribosylation, monoglucosylation, phosphorylation, proteolysis, deamidation or transglutamination, while others do so through noncovalent interactions involving GEF-like, GAP-like, GDI-like or GDF-like activities [3]. In the case of signaling by heterotrimeric G-protein-coupled receptors, CT directly activates Gs and PT directly inhibits Gi and Go, thereby indirectly potentiating Gs signaling, while PMT directly activates Gi, thereby indirectly inhibiting Gs signaling. PMT also directly activates a number of other signaling pathways, including Gq, G12/13, and possibly others that have not been delineated yet. CT and PT modify their targets through ADP-ribosylation, but PMT does so by deamidation.
The realization that a number of bacteria, including known pathogens such as Pasteurella, Bordetella, Yersinia, Salmonella, Burkholderia and E. coli, produce deamidases/TGases that affect cytoskeletal and mitogenic signaling, suggests that there may be additional bacteria that produce such factors to modulate host signaling during infection. Modification of heterotrimeric G proteins through deamidation so far is unique to PMT. The finding that SseI may also be a deamidase, sharing partial amino acid sequence similarity with PMT in addition to the same catalytic triad, supports this notion. Availability of current genomic sequences and structural databases may enable further discoveries through gene and protein sequence comparisons, particularly with use of the Cys-His-Asp triad motif to point toward potential candidates. One difficulty encountered in finding more potential deamidase/TGase-like bacterial factors is detection of the modification, which involves detection of a molecular mass change of 1 dalton in a relatively large protein substrate (20–45 kDa). Another challenge is development of an in vitro assay for studying the enzyme activity of these proteins.
Although PMT has multiple intracellular G protein targets, the overall outcome (summarized in Figure 1) is downregulation of differentiation, such as adipogenesis and osteogenesis, with concomitant upregulation of mitogenesis and cell growth, without inducing apoptosis. The cellular actions of several bacterial toxins, including PMT, have been linked to their effects on mitogenic signaling, and have been speculated as potential contributors to cancer predisposition as long-term sequelae to bacterial infection [87, 93, 156]. Further exploration of toxin action may provide additional insights into the regulation of cellular processes and cell fate decisions.
Acknowledgments
Some of the work reported here was supported by grants from the National Institutes of Health (NIH/NIAID AI038396) and from the U. S. Department of Agriculture (NRI 1999-02295) (to B.A.W.).
References
- 1.Wilson BA. Global biosecurity in a complex, dynamic world. Complexity. 2008;14:71–88. doi: 10.1002/cplx.20246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson BA, Salyers AA. Ecology and physiology of infectious bacteria--implications for biotechnology. Curr Opin Biotechnol. 2002;13:267–274. doi: 10.1016/s0958-1669(02)00312-9. [DOI] [PubMed] [Google Scholar]
- 3.Wilson BA, Ho M. Recent insights into Pasteurella multocida toxin and other G-protein-modulating bacterial toxins. Future Microbiol. 2010;5:1185–1201. doi: 10.2217/fmb.10.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fiorentini C, Fabbri A, Flatau G, Donelli G, Matarrese P, Lemichez E, Falzano L, Boquet P. Escherichia coli cytotoxic necrotizing factor 1 (CNF1), a toxin that activates the Rho GTPase. J Biol Chem. 1997;272:19532–19537. doi: 10.1074/jbc.272.31.19532. [DOI] [PubMed] [Google Scholar]
- 5.Flatau G, Lemichez E, Gauthier M, Chardin P, Paris S, Fiorentini C, Boquet P. Toxin-induced activation of the G protein p21 Rho by deamidation of glutamine. Nature. 1997;387:729–733. doi: 10.1038/42743. [DOI] [PubMed] [Google Scholar]
- 6.Horiguchi Y. Escherichia coli cytotoxic necrotizing factors and Bordetella dermonecrotic toxin: the dermonecrosis-inducing toxins activating Rho small GTPases. Toxicon. 2001;39:1619–1627. doi: 10.1016/s0041-0101(01)00149-0. [DOI] [PubMed] [Google Scholar]
- 7.Oswald E, Sugai M, Labigne A, Wu HC, Fiorentini C, Boquet P, O’Brien AD. Cytotoxic necrotizing factor type 2 produced by virulent Escherichia coli modifies the small GTP-binding proteins Rho involved in assembly of actin stress fibers. Proc Natl Acad Sci U S A. 1994;91:3814–3818. doi: 10.1073/pnas.91.9.3814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmidt G, Sehr P, Wilm M, Selzer J, Mann M, Aktories K. Gln 63 of Rho is deamidated by Escherichia coli cytotoxic necrotizing factor-1. Nature. 1997;387:725–729. doi: 10.1038/42735. [DOI] [PubMed] [Google Scholar]
- 9.Horiguchi Y, Inoue N, Masuda M, Kashimoto T, Katahira J, Sugimoto N, Matsuda M. Bordetella bronchiseptica dermonecrotizing toxin induces reorganization of actin stress fibers through deamidation of Gln-63 of the GTP-binding protein Rho. Proc Natl Acad Sci U S A. 1997;94:11623–11626. doi: 10.1073/pnas.94.21.11623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horiguchi Y, Senda T, Sugimoto N, Katahira J, Matsuda M. Bordetella bronchiseptica dermonecrotizing toxin stimulates assembly of actin stress fibers and focal adhesions by modifying the small GTP-binding protein rho. J Cell Sci. 1995;108 (Pt 10):3243–3251. doi: 10.1242/jcs.108.10.3243. [DOI] [PubMed] [Google Scholar]
- 11.Ohnishi T, Horiguchi Y, Masuda M, Sugimoto N, Matsuda M. Pasteurella multocida toxin and Bordetella bronchiseptica dermonecrotizing toxin elicit similar effects on cultured cells by different mechanisms. J Vet Med Sci. 1998;60:301–305. doi: 10.1292/jvms.60.301. [DOI] [PubMed] [Google Scholar]
- 12.Masuda M, Minami M, Shime H, Matsuzawa T, Horiguchi Y. In vivo modifications of small GTPase Rac and Cdc42 by Bordetella dermonecrotic toxin. Infect Immun. 2002;70:998–1001. doi: 10.1128/iai.70.2.998-1001.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flatau G, Landraud L, Boquet P, Bruzzone M, Munro P. Deamidation of RhoA glutamine 63 by the Escherichia coli CNF1 toxin requires a short sequence of the GTPase switch 2 domain. Biochem Biophys Res Commun. 2000;267:588–592. doi: 10.1006/bbrc.1999.1904. [DOI] [PubMed] [Google Scholar]
- 14.Sugai M, Hatazaki K, Mogami A, Ohta H, Peres SY, Herault F, Horiguchi Y, Masuda M, Ueno Y, Komatsuzawa H, et al. Cytotoxic necrotizing factor type 2 produced by pathogenic Escherichia coli deamidates a gln residue in the conserved G-3 domain of the rho family and preferentially inhibits the GTPase activity of RhoA and rac1. Infect Immun. 1999;67:6550–6557. doi: 10.1128/iai.67.12.6550-6557.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoffmann C, Schmidt G. CNF and DNT. Rev Physiol Biochem Pharmacol. 2004;152:49–63. doi: 10.1007/s10254-004-0026-4. [DOI] [PubMed] [Google Scholar]
- 16.Hoffmann C, Pop M, Leemhuis J, Schirmer J, Aktories K, Schmidt G. The Yersinia pseudotuberculosis cytotoxic necrotizing factor (CNFY) selectively activates RhoA. J Biol Chem. 2004;279:16026–16032. doi: 10.1074/jbc.M313556200. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt G, Goehring UM, Schirmer J, Uttenweiler-Joseph S, Wilm M, Lohmann M, Giese A, Schmalzing G, Aktories K. Lysine and polyamines are substrates for transglutamination of Rho by the Bordetella dermonecrotic toxin. Infect Immun. 2001;69:7663–7670. doi: 10.1128/IAI.69.12.7663-7670.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Orth JH, Preuss I, Fester I, Schlosser A, Wilson BA, Aktories K. Pasteurella multocida toxin activation of heterotrimeric G proteins by deamidation. Proc Natl Acad Sci U S A. 2009;106:7179–7184. doi: 10.1073/pnas.0900160106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ackermann MR, DeBey MC, Register KB, Larson DJ, Kinyon JM. Tonsil and turbinate colonization by toxigenic and nontoxigenic strains of Pasteurella multocida in conventionally raised swine. J Vet Diagn Invest. 1994;6:375–377. doi: 10.1177/104063879400600318. [DOI] [PubMed] [Google Scholar]
- 20.Deeb BJ, DiGiacomo RF, Bernard BL, Silbernagel SM. Pasteurella multocida and Bordetella bronchiseptica infections in rabbits. J Clin Microbiol. 1990;28:70–75. doi: 10.1128/jcm.28.1.70-75.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DiGiacomo RF, Deeb BJ, Brodie SJ, Zimmerman TE, Veltkamp ER, Chrisp CE. Toxin production by Pasteurella multocida isolated from rabbits with atrophic rhinitis. Am J Vet Res. 1993;54:1280–1286. [PubMed] [Google Scholar]
- 22.Magyar T. Study of the toxin-producing ability of Pasteurella multocida in mice. Acta Vet Hung. 1989;37:319–325. [PubMed] [Google Scholar]
- 23.Foged NT. Pasteurella multocida toxin. The characterisation of the toxin and its significance in the diagnosis and prevention of progressive atrophic rhinitis in pigs. APMIS Suppl. 1992;25:1–56. [PubMed] [Google Scholar]
- 24.Frymus T, Bielecki W, Jakubowski T. Toxigenic Pasteurella multocida in rabbits with naturally occurring atrophic rhinitis. Zentralbl Veterinarmed B. 1991;38:265–268. doi: 10.1111/j.1439-0450.1991.tb00870.x. [DOI] [PubMed] [Google Scholar]
- 25.Lax AJ, Chanter N. Cloning of the toxin gene from Pasteurella multocida and its role in atrophic rhinitis. J Gen Microbiol. 1990;136:81–87. doi: 10.1099/00221287-136-1-81. [DOI] [PubMed] [Google Scholar]
- 26.Williams PP, Hall MR, Rimler RB. Host response to Pasteurella multocida turbinate atrophy toxin in swine. Can J Vet Res. 1990;54:157–163. [PMC free article] [PubMed] [Google Scholar]
- 27.Digiacomo RF, Allen V, Hinton MH. Naturally acquired Pasteurella multocida subsp. multocida infection in a closed colony of rabbits: characteristics of isolates. Lab Anim. 1991;25:236–241. doi: 10.1258/002367791780808365. [DOI] [PubMed] [Google Scholar]
- 28.DiGiacomo RF, Xu YM, Allen V, Hinton MH, Pearson GR. Naturally acquired Pasteurella multocida infection in rabbits: clinicopathological aspects. Can J Vet Res. 1991;55:234–238. [PMC free article] [PubMed] [Google Scholar]
- 29.Kielstein P. On the occurrence of toxin-producing Pasteurella multocida strains in atrophic rhinitis and in pneumonias of swine and cattle. Zentralbl Veterinarmed B. 1986;33:418–424. doi: 10.1111/j.1439-0450.1986.tb00052.x. [DOI] [PubMed] [Google Scholar]
- 30.Cheville NF, Rimler RB. A protein toxin from Pasteurella multocida type D causes acute and chronic hepatic toxicity in rats. Vet Pathol. 1989;26:148–157. doi: 10.1177/030098588902600208. [DOI] [PubMed] [Google Scholar]
- 31.Chrisp CE, Foged NT. Induction of pneumonia in rabbits by use of a purified protein toxin from Pasteurella multocida. Am J Vet Res. 1991;52:56–61. [PubMed] [Google Scholar]
- 32.Glavits R, Magyar T. The pathology of experimental respiratory infection with Pasteurella multocida and Bordetella bronchiseptica in rabbits. Acta Vet Hung. 1990;38:211–215. [PubMed] [Google Scholar]
- 33.Hoskins IC, Thomas LH, Lax AJ. Nasal infection with Pasteurella multocida causes proliferation of bladder epithelium in gnotobiotic pigs. Vet Rec. 1997;140:22. doi: 10.1136/vr.140.1.22. [DOI] [PubMed] [Google Scholar]
- 34.Klein NC, Cunha BA. Pasteurella multocida pneumonia. Semin Respir Infect. 1997;12:54–56. [PubMed] [Google Scholar]
- 35.Magyar T, Glavits R. Immunopathological changes in mice caused by Bordetella bronchiseptica and Pasteurella multocida. Acta Vet Hung. 1990;38:203–210. [PubMed] [Google Scholar]
- 36.Ackermann MR, Register KB, Stabel JR, Gwaltney SM, Howe TS, Rimler RB. Effect of Pasteurella multocida toxin on physeal growth in young pigs. Am J Vet Res. 1996;57:848–852. [PubMed] [Google Scholar]
- 37.Arashima Y, Kumasaka K. Pasteurellosis as zoonosis. Intern Med. 2005;44:692–693. doi: 10.2169/internalmedicine.44.692. [DOI] [PubMed] [Google Scholar]
- 38.Garcia VF. Animal bites and Pasturella infections. Pediatr Rev. 1997;18:127–130. doi: 10.1542/pir.18-4-127. [DOI] [PubMed] [Google Scholar]
- 39.Griego RD, Rosen T, Orengo IF, Wolf JE. Dog, cat, and human bites: a review. J Am Acad Dermatol. 1995;33:1019–1029. doi: 10.1016/0190-9622(95)90296-1. [DOI] [PubMed] [Google Scholar]
- 40.Kobayaa H, Souki RR, Trust S, Domachowske JB. Pasteurella multocida meningitis in newborns after incidental animal exposure. Pediatr Infect Dis J. 2009;28:928–929. doi: 10.1097/INF.0b013e3181a81f0f. [DOI] [PubMed] [Google Scholar]
- 41.Migliore E, Serraino C, Brignone C, Ferrigno D, Cardellicchio A, Pomero F, Castagna E, Osenda M, Fenoglio L. Pasteurella multocida infection in a cirrhotic patient: case report, microbiological aspects and a review of literature. Adv Med Sci. 2009;54:109–112. doi: 10.2478/v10039-009-0005-8. [DOI] [PubMed] [Google Scholar]
- 42.Waldor M, Roberts D, Kazanjian P. In utero infection due to Pasteurella multocida in the first trimester of pregnancy: case report and review. Clin Infect Dis. 1992;14:497–500. doi: 10.1093/clinids/14.2.497. [DOI] [PubMed] [Google Scholar]
- 43.Frederiksen W. Ecology and significance of Pasteurellaceae in man--an update. Zentralbl Bakteriol. 1993;279:27–34. doi: 10.1016/s0934-8840(11)80488-3. [DOI] [PubMed] [Google Scholar]
- 44.Donnio PY, Allardet-Servent A, Perrin M, Escande F, Avril JL. Characterisation of dermonecrotic toxin-producing strains of Pasteurella multocida subsp. multocida isolated from man and swine. J Med Microbiol. 1999;48:125–131. doi: 10.1099/00222615-48-2-125. [DOI] [PubMed] [Google Scholar]
- 45.Donnio PY, Lerestif-Gautier AL, Avril JL. Characterization of Pasteurella spp. strains isolated from human infections. J Comp Pathol. 2004;130:137–142. doi: 10.1016/j.jcpa.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 46.Holst E, Rollof J, Larsson L, Nielsen JP. Characterization and distribution of Pasteurella species recovered from infected humans. J Clin Microbiol. 1992;30:2984–2987. doi: 10.1128/jcm.30.11.2984-2987.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Henderson SR, Shah A, Banford KB, Howard LS. Pig trotters lung--novel domestic transmission of Pasteurella multocida. Clin Med. 2010;10:517–518. doi: 10.7861/clinmedicine.10-5-517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Iaria C, Cascio A. Please, do not forget Pasteurella multocida. Clin Infect Dis. 2007;45:940. doi: 10.1086/521247. [DOI] [PubMed] [Google Scholar]
- 49.Satomura A, Yanai M, Fujita T, Arashima Y, Kumasaka K, Nakane C, Ito K, Fuke Y, Maruyama T, Maruyama N, et al. Peritonitis associated with Pasteurella multocida: molecular evidence of zoonotic etiology. Ther Apher Dial. 2010;14:373–376. doi: 10.1111/j.1744-9987.2009.00788.x. [DOI] [PubMed] [Google Scholar]
- 50.Wilson BA, Ho M. Pasteurella multocida toxin. In: Alouf JE, Popoff MR, editors. The Comprehensive Sourcebook of Bacterial Protein Toxins. Elsevier Science Publishers B. V.; Amsterdam: 2006. pp. 430–447. [Google Scholar]
- 51.Cheville NF, Rimler RB, Thurston JR. A toxin from Pasteurella multocida type D causes acute hepatic necrosis in pigs. Vet Pathol. 1988;25:518–520. doi: 10.1177/030098588802500617. [DOI] [PubMed] [Google Scholar]
- 52.Nakai T, Sawata A, Tsuji M, Kume K. Characterization of dermonecrotic toxin produced by serotype D strains of Pasteurella multocida. Am J Vet Res. 1984;45:2410–2413. [PubMed] [Google Scholar]
- 53.Thurston JR, Rimler RB, Ackermann MR, Cheville NF. Use of rats to compare atrophic rhinitis vaccines for protection against effects of heat-labile protein toxin produced by Pasteurella multocida serogroup D. Vet Immunol Immunopathol. 1992;33:155–162. doi: 10.1016/0165-2427(92)90042-o. [DOI] [PubMed] [Google Scholar]
- 54.Ackermann MR, Stabel JR, Pettit RK, Jacobson CD, Elmquist JK, Register KB, Rimler RB, Hilton JH. Reduced physeal area and chondrocyte proliferation in Pasteurella multocida toxin-treated rats. Vet Pathol. 1995;32:674–682. doi: 10.1177/030098589503200609. [DOI] [PubMed] [Google Scholar]
- 55.Al-Haddawi MH, Jasni S, Israf DA, Zamri-Saad M, Mutalib AR, Sheikh-Omar AR. Ultrastructural pathology of nasal and tracheal mucosa of rabbits experimentally infected with Pasteurella multocida serotype D:1. Res Vet Sci. 2001;70:191–197. doi: 10.1053/rvsc.2001.0459. [DOI] [PubMed] [Google Scholar]
- 56.Kimman TG, Lowik CW, van de Wee-Pals LJ, Thesingh CW, Defize P, Kamp EM, Bijvoet OL. Stimulation of bone resorption by inflamed nasal mucosa, dermonecrotic toxin-containing conditioned medium from Pasteurella multocida, and purified dermonecrotic toxin from P. multocida. Infect Immun. 1987;55:2110–2116. doi: 10.1128/iai.55.9.2110-2116.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mullan PB, Lax AJ. Pasteurella multocida toxin is a mitogen for bone cells in primary culture. Infect Immun. 1996;64:959–965. doi: 10.1128/iai.64.3.959-965.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mullan PB, Lax AJ. Pasteurella multocida toxin stimulates bone resorption by osteoclasts via interaction with osteoblasts. Calcif Tissue Int. 1998;63:340–345. doi: 10.1007/s002239900537. [DOI] [PubMed] [Google Scholar]
- 59.Jutras I, Martineau-Doize B. Stimulation of osteoclast-like cell formation by Pasteurella multocida toxin from hemopoietic progenitor cells in mouse bone marrow cultures. Can J Vet Res. 1996;60:34–39. [PMC free article] [PubMed] [Google Scholar]
- 60.Martineau-Doize B, Caya I, Gagne S, Jutras I, Dumas G. Effects of Pasteurella multocida toxin on the osteoclast population of the rat. J Comp Pathol. 1993;108:81–91. doi: 10.1016/s0021-9975(08)80230-7. [DOI] [PubMed] [Google Scholar]
- 61.Felix R, Fleisch H, Frandsen PL. Effect of Pasteurella multocida toxin on bone resorption in vitro. Infect Immun. 1992;60:4984–4988. doi: 10.1128/iai.60.12.4984-4988.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gwaltney SM, Galvin RJ, Register KB, Rimler RB, Ackermann MR. Effects of Pasteurella multocida toxin on porcine bone marrow cell differentiation into osteoclasts and osteoblasts. Vet Pathol. 1997;34:421–430. doi: 10.1177/030098589703400506. [DOI] [PubMed] [Google Scholar]
- 63.Harmey D, Stenbeck G, Nobes CD, Lax AJ, Grigoriadis AE. Regulation of osteoblast differentiation by Pasteurella multocida toxin (PMT): a role for Rho GTPase in bone formation. J Bone Miner Res. 2004;19:661–670. doi: 10.1359/JBMR.040105. [DOI] [PubMed] [Google Scholar]
- 64.Sterner-Kock A, Lanske B, Uberschar S, Atkinson MJ. Effects of the Pasteurella multocida toxin on osteoblastic cells in vitro. Vet Pathol. 1995;32:274–279. doi: 10.1177/030098589503200309. [DOI] [PubMed] [Google Scholar]
- 65.Rozengurt E, Higgins T, Chanter N, Lax AJ, Staddon JM. Pasteurella multocida toxin: potent mitogen for cultured fibroblasts. Proc Natl Acad Sci U S A. 1990;87:123–127. doi: 10.1073/pnas.87.1.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Seo B, Choy EW, Maudsley S, Miller WE, Wilson BA, Luttrell LM. Pasteurella multocida toxin stimulates mitogen-activated protein kinase via G(q/11)-dependent transactivation of the epidermal growth factor receptor. J Biol Chem. 2000;275:2239–2245. doi: 10.1074/jbc.275.3.2239. [DOI] [PubMed] [Google Scholar]
- 67.Wilson BA, Aminova LR, Ponferrada VG, Ho M. Differential modulation and subsequent blockade of mitogenic signaling and cell cycle progression by Pasteurella multocida toxin. Infect Immun. 2000;68:4531–4538. doi: 10.1128/iai.68.8.4531-4538.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Aminova LR, Wilson BA. Calcineurin-independent inhibition of 3T3-L1 adipogenesis by Pasteurella multocida toxin: suppression of Notch1, stabilization of beta-catenin and pre-adipocyte factor 1. Cell Microbiol. 2007;9:2485–2496. doi: 10.1111/j.1462-5822.2007.00975.x. [DOI] [PubMed] [Google Scholar]
- 69.Preuss I, Hildebrand D, Orth JH, Aktories K, Kubatzky KF. Pasteurella multocida toxin is a potent activator of anti-apoptotic signalling pathways. Cell Microbiol. 2010;12:1174–1185. doi: 10.1111/j.1462-5822.2010.01462.x. [DOI] [PubMed] [Google Scholar]
- 70.Sabri A, Wilson BA, Steinberg SF. Dual actions of the Galpha(q) agonist Pasteurella multocida toxin to promote cardiomyocyte hypertrophy and enhance apoptosis susceptibility. Circ Res. 2002;90:850–857. doi: 10.1161/01.RES.0000016165.23795.1F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Staddon JM, Barker CJ, Murphy AC, Chanter N, Lax AJ, Michell RH, Rozengurt E. Pasteurella multocida toxin, a potent mitogen, increases inositol 1,4,5-trisphosphate and mobilizes Ca2+ in Swiss 3T3 cells. J Biol Chem. 1991;266:4840–4847. [PubMed] [Google Scholar]
- 72.Wilson BA, Zhu X, Ho M, Lu L. Pasteurella multocida toxin activates the inositol triphosphate signaling pathway in Xenopus oocytes via G(q)alpha-coupled phospholipase C-beta1. J Biol Chem. 1997;272:1268–1275. doi: 10.1074/jbc.272.2.1268. [DOI] [PubMed] [Google Scholar]
- 73.Aepfelbacher M, Essler M. Disturbance of endothelial barrier function by bacterial toxins and atherogenic mediators: a role for Rho/Rho kinase. Cell Microbiol. 2001;3:649–658. doi: 10.1046/j.1462-5822.2001.00145.x. [DOI] [PubMed] [Google Scholar]
- 74.Orth JH, Lang S, Taniguchi M, Aktories K. Pasteurella multocida toxin-induced activation of RhoA is mediated via two families of G{alpha} proteins, G{alpha}q and G{alpha}12/13. J Biol Chem. 2005;280:36701–36707. doi: 10.1074/jbc.M507203200. [DOI] [PubMed] [Google Scholar]
- 75.Sagi SA, Seasholtz TM, Kobiashvili M, Wilson BA, Toksoz D, Brown JH. Physical and functional interactions of Galphaq with Rho and its exchange factors. J Biol Chem. 2001;276:15445–15452. doi: 10.1074/jbc.M008961200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Orth JH, Fester I, Preuss I, Agnoletto L, Wilson BA, Aktories K. Activation of Galpha (i) and subsequent uncoupling of receptor-Galpha(i) signaling by Pasteurella multocida toxin. J Biol Chem. 2008;283:23288–23294. doi: 10.1074/jbc.M803435200. [DOI] [PubMed] [Google Scholar]
- 77.Staddon JM, Chanter N, Lax AJ, Higgins TE, Rozengurt E. Pasteurella multocida toxin, a potent mitogen, stimulates protein kinase C-dependent and -independent protein phosphorylation in Swiss 3T3 cells. J Biol Chem. 1990;265:11841–11848. [PubMed] [Google Scholar]
- 78.Luo S, Ho M, Wilson BA. Application of intact cell-based NFAT-beta-lactamase reporter assay for Pasteurella multocida toxin-mediated activation of calcium signaling pathway. Toxicon. 2008;51:597–605. doi: 10.1016/j.toxicon.2007.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Staddon JM, Bouzyk MM, Rozengurt E. Interconversion of GRP78/BiP. A novel event in the action of Pasteurella multocida toxin, bombesin, and platelet-derived growth factor. J Biol Chem. 1992;267:25239–25245. [PubMed] [Google Scholar]
- 80.Lacerda HM, Lax AJ, Rozengurt E. Pasteurella multocida toxin, a potent intracellularly acting mitogen, induces p125FAK and paxillin tyrosine phosphorylation, actin stress fiber formation, and focal contact assembly in Swiss 3T3 cells. J Biol Chem. 1996;271:439–445. doi: 10.1074/jbc.271.1.439. [DOI] [PubMed] [Google Scholar]
- 81.Obreztchikova M, Elouardighi H, Ho M, Wilson BA, Gertsberg Z, Steinberg SF. Distinct signaling functions for Shc isoforms in the heart. J Biol Chem. 2006;281:20197–20204. doi: 10.1074/jbc.M601859200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ozgen N, Obreztchikova M, Guo J, Elouardighi H, Dorn GW, 2nd, Wilson BA, Steinberg SF. Protein kinase D links Gq-coupled receptors to cAMP response element-binding protein (CREB)-Ser133 phosphorylation in the heart. J Biol Chem. 2008;283:17009–17019. doi: 10.1074/jbc.M709851200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Aminova LR, Luo S, Bannai Y, Ho M, Wilson BA. The C3 domain of Pasteurella multocida toxin is the minimal domain responsible for activation of Gq-dependent calcium and mitogenic signaling. Protein Sci. 2008;17:945–949. doi: 10.1110/ps.083445408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zywietz A, Gohla A, Schmelz M, Schultz G, Offermanns S. Pleiotropic effects of Pasteurella multocida toxin are mediated by Gq-dependent and -independent mechanisms. involvement of Gq but not G11. J Biol Chem. 2001;276:3840–3845. doi: 10.1074/jbc.M007819200. [DOI] [PubMed] [Google Scholar]
- 85.Hildebrand D, Heeg K, Kubatzky KF. Pasteurella multocida toxin-stimulated osteoclast differentiation is B cell dependent. Infect Immun. 2010;79:220–228. doi: 10.1128/IAI.00565-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hildebrand D, Walker P, Dalpke A, Heeg K, Kubatzky KF. Pasteurella multocida Toxin-induced Pim-1 expression disrupts suppressor of cytokine signalling (SOCS)-1 activity. Cell Microbiol. 2010;12:1732–1745. doi: 10.1111/j.1462-5822.2010.01504.x. [DOI] [PubMed] [Google Scholar]
- 87.Orth JH, Aktories K, Kubatzky KF. Modulation of host cell gene expression through activation of STAT transcription factors by Pasteurella multocida toxin. J Biol Chem. 2007;282:3050–3057. doi: 10.1074/jbc.M609018200. [DOI] [PubMed] [Google Scholar]
- 88.Sternweis PC, Smrcka AV. Regulation of phospholipase C by G proteins. Trends Biochem Sci. 1992;17:502–506. doi: 10.1016/0968-0004(92)90340-f. [DOI] [PubMed] [Google Scholar]
- 89.Orth JH, Lang S, Aktories K. Action of Pasteurella multocida toxin depends on the helical domain of Galphaq. J Biol Chem. 2004;279:34150–34155. doi: 10.1074/jbc.M405353200. [DOI] [PubMed] [Google Scholar]
- 90.Orth JH, Lang S, Preuss I, Milligan G, Aktories K. Action of Pasteurella multocida toxin on Galpha(q) is persistent and independent of interaction with G-protein-coupled receptors. Cell Signal. 2007;19:2174–2182. doi: 10.1016/j.cellsig.2007.06.016. [DOI] [PubMed] [Google Scholar]
- 91.Murphy AC, Rozengurt E. Pasteurella multocida toxin selectively facilitates phosphatidylinositol 4,5-bisphosphate hydrolysis by bombesin, vasopressin, and endothelin. Requirement for a functional G protein. J Biol Chem. 1992;267:25296–25303. [PubMed] [Google Scholar]
- 92.Hennig B, Orth J, Aktories K, Diener M. Anion secretion evoked by Pasteurella multocida toxin across rat colon. Eur J Pharmacol. 2008;583:156–163. doi: 10.1016/j.ejphar.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 93.Lax AJ. Opinion: Bacterial toxins and cancer--a case to answer? Nat Rev Microbiol. 2005;3:343–349. doi: 10.1038/nrmicro1130. [DOI] [PubMed] [Google Scholar]
- 94.Rutter JM, Luther PD. Cell culture assay for toxigenic Pasteurella multocida from atrophic rhinitis of pigs. Vet Rec. 1984;114:393–396. doi: 10.1136/vr.114.16.393. [DOI] [PubMed] [Google Scholar]
- 95.Pennings AM, Storm PK. A test in vero cell monolayers for toxin production by strains of Pasteurella multocida isolated from pigs suspected of having atrophic rhinitis. Vet Microbiol. 1984;9:503–508. doi: 10.1016/0378-1135(84)90071-3. [DOI] [PubMed] [Google Scholar]
- 96.Pettit RK, Ackermann MR, Rimler RB. Receptor-mediated binding of Pasteurella multocida dermonecrotic toxin to canine osteosarcoma and monkey kidney (vero) cells. Lab Invest. 1993;69:94–100. [PubMed] [Google Scholar]
- 97.Adams JW, Sakata Y, Davis MG, Sah VP, Wang Y, Liggett SB, Chien KR, Brown JH, Dorn GW., 2nd Enhanced Galphaq signaling: a common pathway mediates cardiac hypertrophy and apoptotic heart failure. Proc Natl Acad Sci U S A. 1998;95:10140–10145. doi: 10.1073/pnas.95.17.10140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wang QJ. PKD at the crossroads of DAG and PKC signaling. Trends Pharmacol Sci. 2006;27:317–323. doi: 10.1016/j.tips.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 99.Dudet LI, Chailler P, Dubreuil JD, Martineau-Doize B. Pasteurella multocida toxin stimulates mitogenesis and cytoskeleton reorganization in Swiss 3T3 fibroblasts. J Cell Physiol. 1996;168:173–182. doi: 10.1002/(SICI)1097-4652(199607)168:1<173::AID-JCP21>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 100.Thomas W, Pullinger GD, Lax AJ, Rozengurt E. Escherichia coli cytotoxic necrotizing factor and Pasteurella multocida toxin induce focal adhesion kinase autophosphorylation and Src association. Infect Immun. 2001;69:5931–5935. doi: 10.1128/IAI.69.9.5931-5935.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Essler M, Hermann K, Amano M, Kaibuchi K, Heesemann J, Weber PC, Aepfelbacher M. Pasteurella multocida toxin increases endothelial permeability via Rho kinase and myosin light chain phosphatase. J Immunol. 1998;161:5640–5646. [PubMed] [Google Scholar]
- 102.Lacerda HM, Pullinger GD, Lax AJ, Rozengurt E. Cytotoxic necrotizing factor 1 from Escherichia coli and dermonecrotic toxin from Bordetella bronchiseptica induce p21(rho)-dependent tyrosine phosphorylation of focal adhesion kinase and paxillin in Swiss 3T3 cells. J Biol Chem. 1997;272:9587–9596. doi: 10.1074/jbc.272.14.9587. [DOI] [PubMed] [Google Scholar]
- 103.Buhl AM, Johnson NL, Dhanasekaran N, Johnson GL. G alpha 12 and G alpha 13 stimulate Rho-dependent stress fiber formation and focal adhesion assembly. J Biol Chem. 1995;270:24631–24634. doi: 10.1074/jbc.270.42.24631. [DOI] [PubMed] [Google Scholar]
- 104.Goulimari P, Knieling H, Engel U, Grosse R. LARG and mDia1 link Galpha12/13 to cell polarity and microtubule dynamics. Mol Biol Cell. 2008;19:30–40. doi: 10.1091/mbc.E06-11-1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jin S, Exton JH. Activation of RhoA by association of Galpha(13) with Dbl. Biochem Biophys Res Commun. 2000;277:718–721. doi: 10.1006/bbrc.2000.3744. [DOI] [PubMed] [Google Scholar]
- 106.Tanabe S, Kreutz B, Suzuki N, Kozasa T. Regulation of RGS-RhoGEFs by Galpha12 and Galpha13 proteins. Methods Enzymol. 2004;390:285–294. doi: 10.1016/S0076-6879(04)90018-3. [DOI] [PubMed] [Google Scholar]
- 107.Lutz S, Freichel-Blomquist A, Yang Y, Rumenapp U, Jakobs KH, Schmidt M, Wieland T. The guanine nucleotide exchange factor p63RhoGEF, a specific link between Gq/11-coupled receptor signaling and RhoA. J Biol Chem. 2005;280:11134–11139. doi: 10.1074/jbc.M411322200. [DOI] [PubMed] [Google Scholar]
- 108.Elling F, Pedersen KB, Hogh P, Foged NT. Characterization of the dermal lesions induced by a purified protein from toxigenic Pasteurella multocida. APMIS. 1988;96:50–55. doi: 10.1111/j.1699-0463.1988.tb05267.x. [DOI] [PubMed] [Google Scholar]
- 109.Katada T, Oinuma M, Ui M. Two guanine nucleotide-binding proteins in rat brain serving as the specific substrate of islet-activating protein, pertussis toxin. Interaction of the alpha-subunits with beta gamma-subunits in development of their biological activities. J Biol Chem. 1986;261:8182–8191. [PubMed] [Google Scholar]
- 110.Rosen ED, Spiegelman BM. Molecular regulation of adipogenesis. Annu Rev Cell Dev Biol. 2000;16:145–171. doi: 10.1146/annurev.cellbio.16.1.145. [DOI] [PubMed] [Google Scholar]
- 111.Nuttall ME, Gimble JM. Controlling the balance between osteoblastogenesis and adipogenesis and the consequent therapeutic implications. Curr Opin Pharmacol. 2004;4:290–294. doi: 10.1016/j.coph.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 112.Sul HS, Smas C, Mei B, Zhou L. Function of pref-1 as an inhibitor of adipocyte differentiation. Int J Obes Relat Metab Disord. 2000;24(Suppl 4):S15–19. doi: 10.1038/sj.ijo.0801494. [DOI] [PubMed] [Google Scholar]
- 113.Ross SE, Hemati N, Longo KA, Bennett CN, Lucas PC, Erickson RL, MacDougald OA. Inhibition of adipogenesis by Wnt signaling. Science. 2000;289:950–953. doi: 10.1126/science.289.5481.950. [DOI] [PubMed] [Google Scholar]
- 114.Liu L, Clipstone NA. Prostaglandin F2alpha inhibits adipocyte differentiation via a G alpha q-calcium-calcineurin-dependent signaling pathway. J Cell Biochem. 2007;100:161–173. doi: 10.1002/jcb.21044. [DOI] [PubMed] [Google Scholar]
- 115.Neal JW, Clipstone NA. Calcineurin mediates the calcium-dependent inhibition of adipocyte differentiation in 3T3-L1 cells. J Biol Chem. 2002;277:49776–49781. doi: 10.1074/jbc.M207913200. [DOI] [PubMed] [Google Scholar]
- 116.DiGiacomo RF, Deeb BJ, Giddens WE, Jr, Bernard BL, Chengappa MM. Atrophic rhinitis in New Zealand white rabbits infected with Pasteurella multocida. Am J Vet Res. 1989;50:1460–1465. [PubMed] [Google Scholar]
- 117.Elling F, Pedersen KB. The pathogenesis of persistent turbinate atrophy induced by toxigenic Pasteurella multocida in pigs. Vet Pathol. 1985;22:469–474. doi: 10.1177/030098588502200506. [DOI] [PubMed] [Google Scholar]
- 118.Sciaudone M, Gazzerro E, Priest L, Delany AM, Canalis E. Notch 1 impairs osteoblastic cell differentiation. Endocrinology. 2003;144:5631–5639. doi: 10.1210/en.2003-0463. [DOI] [PubMed] [Google Scholar]
- 119.Bording A, Foged NT. Characterization of the immunogenicity of formaldehyde detoxified Pasteurella multocida toxin. Vet Microbiol. 1991;29:267–280. doi: 10.1016/0378-1135(91)90134-2. [DOI] [PubMed] [Google Scholar]
- 120.Chanter N, Rutter JM. Colonisation by Pasteurella multocida in atrophic rhinitis of pigs and immunity to the osteolytic toxin. Vet Microbiol. 1990;25:253–265. doi: 10.1016/0378-1135(90)90082-7. [DOI] [PubMed] [Google Scholar]
- 121.Foged NT, Nielsen JP, Jorsal SE. Protection against progressive atrophic rhinitis by vaccination with Pasteurella multocida toxin purified by monoclonal antibodies. Vet Rec. 1989;125:7–11. doi: 10.1136/vr.125.1.7. [DOI] [PubMed] [Google Scholar]
- 122.Frymus T, Muller E, Franz B, Petzoldt K. Protection by toxoid-induced antibody of gnotobiotic piglets challenged with the dermonecrotic toxin of Pasteurella multocida. Zentralbl Veterinarmed B. 1989;36:674–680. doi: 10.1111/j.1439-0450.1989.tb00661.x. [DOI] [PubMed] [Google Scholar]
- 123.Pettit RK, Rimler RB, Ackermann MR. Protection of Pasteurella multocida dermonecrotic toxin-challenged rats by toxoid-induced antibody. Vet Microbiol. 1993;34:167–173. doi: 10.1016/0378-1135(93)90170-c. [DOI] [PubMed] [Google Scholar]
- 124.Suckow MA. Immunization of rabbits against Pasteurella multocida using a commercial swine vaccine. Lab Anim. 2000;34:403–408. doi: 10.1258/002367700780387769. [DOI] [PubMed] [Google Scholar]
- 125.Bagley KC, Abdelwahab SF, Tuskan RG, Lewis GK. Pasteurella multocida toxin activates human monocyte-derived and murine bone marrow-derived dendritic cells in vitro but suppresses antibody production in vivo. Infect Immun. 2005;73:413–421. doi: 10.1128/IAI.73.1.413-421.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Hamilton TD, Roe JM, Hayes CM, Webster AJ. Effect of ovalbumin aerosol exposure on colonization of the porcine upper airway by Pasteurella multocida and effect of colonization on subsequent immune function. Clin Diagn Lab Immunol. 1998;5:494–498. doi: 10.1128/cdli.5.4.494-498.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Jordan RW, Hamilton TD, Hayes CM, Patel D, Jones PH, Roe JM, Williams NA. Modulation of the humoral immune response of swine and mice mediated by toxigenic Pasteurella multocida. FEMS Immunol Med Microbiol. 2003;39:51–59. doi: 10.1016/S0928-8244(03)00201-3. [DOI] [PubMed] [Google Scholar]
- 128.van Diemen PM, de Vries Reilingh G, Parmentier HK. Effect of Pasteurella multocida toxin on in vivo immune responses in piglets. Vet Q. 1996;18:141–146. doi: 10.1080/01652176.1996.9694636. [DOI] [PubMed] [Google Scholar]
- 129.Thurston JR, Rimler RB, Ackermann MR, Cheville NF, Sacks JM. Immunity induced in rats vaccinated with toxoid prepared from heat-labile toxin produced by Pasteurella multocida serogroup D. Vet Microbiol. 1991;27:169–174. doi: 10.1016/0378-1135(91)90008-4. [DOI] [PubMed] [Google Scholar]
- 130.Blocker D, Berod L, Fluhr JW, Orth J, Idzko M, Aktories K, Norgauer J. Pasteurella multocida toxin (PMT) activates RhoGTPases, induces actin polymerization and inhibits migration of human dendritic cells, but does not influence macropinocytosis. Int Immunol. 2006;18:459–464. doi: 10.1093/intimm/dxh386. [DOI] [PubMed] [Google Scholar]
- 131.Kashimoto T, Katahira J, Cornejo WR, Masuda M, Fukuoh A, Matsuzawa T, Ohnishi T, Horiguchi Y. Identification of functional domains of Bordetella dermonecrotizing toxin. Infect Immun. 1999;67:3727–3732. doi: 10.1128/iai.67.8.3727-3732.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lemichez E, Flatau G, Bruzzone M, Boquet P, Gauthier M. Molecular localization of the Escherichia coli cytotoxic necrotizing factor CNF1 cell-binding and catalytic domains. Mol Microbiol. 1997;24:1061–1070. doi: 10.1046/j.1365-2958.1997.4151781.x. [DOI] [PubMed] [Google Scholar]
- 133.Pullinger GD, Sowdhamini R, Lax AJ. Localization of functional domains of the mitogenic toxin of Pasteurella multocida. Infect Immun. 2001;69:7839–7850. doi: 10.1128/IAI.69.12.7839-7850.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Fabbri A, Gauthier M, Boquet P. The 5′ region of cnf1 harbours a translational regulatory mechanism for CNF1 synthesis and encodes the cell-binding domain of the toxin. Mol Microbiol. 1999;33:108–118. doi: 10.1046/j.1365-2958.1999.01453.x. [DOI] [PubMed] [Google Scholar]
- 135.Meysick KC, Mills M, O’Brien AD. Epitope mapping of monoclonal antibodies capable of neutralizing cytotoxic necrotizing factor type 1 of uropathogenic Escherichia coli. Infect Immun. 2001;69:2066–2074. doi: 10.1128/IAI.69.4.2066-2074.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Pei S, Doye A, Boquet P. Mutation of specific acidic residues of the CNF1 T domain into lysine alters cell membrane translocation of the toxin. Mol Microbiol. 2001;41:1237–1247. doi: 10.1046/j.1365-2958.2001.02596.x. [DOI] [PubMed] [Google Scholar]
- 137.Matsuzawa T, Kashimoto T, Katahira J, Horiguchi Y. Identification of a receptor-binding domain of Bordetella dermonecrotic toxin. Infect Immun. 2002;70:3427–3432. doi: 10.1128/IAI.70.7.3427-3432.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Buetow L, Flatau G, Chiu K, Boquet P, Ghosh P. Structure of the Rho-activating domain of Escherichia coli cytotoxic necrotizing factor 1. Nat Struct Biol. 2001;8:584–588. doi: 10.1038/89610. [DOI] [PubMed] [Google Scholar]
- 139.Kitadokoro K, Kamitani S, Miyazawa M, Hanajima-Ozawa M, Fukui A, Miyake M, Horiguchi Y. Crystal structures reveal a thiol protease-like catalytic triad in the C-terminal region of Pasteurella multocida toxin. Proc Natl Acad Sci U S A. 2007;104:5139–5144. doi: 10.1073/pnas.0608197104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Schmidt G, Selzer J, Lerm M, Aktories K. The Rho-deamidating cytotoxic necrotizing factor 1 from Escherichia coli possesses transglutaminase activity. Cysteine 866 and histidine 881 are essential for enzyme activity. J Biol Chem. 1998;273:13669–13674. doi: 10.1074/jbc.273.22.13669. [DOI] [PubMed] [Google Scholar]
- 141.Geissler B, Tungekar R, Satchell KJ. Identification of a conserved membrane localization domain within numerous large bacterial protein toxins. Proc Natl Acad Sci U S A. 2010;107:5581–5586. doi: 10.1073/pnas.0908700107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kamitani S, Kitadokoro K, Miyazawa M, Toshima H, Fukui A, Abe H, Miyake M, Horiguchi Y. Characterization of the membrane-targeting C1 domain in Pasteurella multocida toxin. J Biol Chem. 2010;285:25467–25475. doi: 10.1074/jbc.M110.102285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yee VC, Pedersen LC, Le Trong I, Bishop PD, Stenkamp RE, Teller DC. Three-dimensional structure of a transglutaminase: human blood coagulation factor XIII. Proc Natl Acad Sci U S A. 1994;91:7296–7300. doi: 10.1073/pnas.91.15.7296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Noguchi K, Ishikawa K, Yokoyama K, Ohtsuka T, Nio N, Suzuki E. Crystal structure of red sea bream transglutaminase. J Biol Chem. 2001;276:12055–12059. doi: 10.1074/jbc.M009862200. [DOI] [PubMed] [Google Scholar]
- 145.Sinclair JC, Sandy J, Delgoda R, Sim E, Noble ME. Structure of arylamine N-acetyltransferase reveals a catalytic triad. Nat Struct Biol. 2000;7:560–564. doi: 10.1038/76783. [DOI] [PubMed] [Google Scholar]
- 146.Yamaguchi S, Jeenes DJ, Archer DB. Protein-glutaminase from Chryseobacterium proteolyticum, an enzyme that deamidates glutaminyl residues in proteins. Purification, characterization and gene cloning. Eur J Biochem. 2001;268:1410–1421. doi: 10.1046/j.1432-1327.2001.02019.x. [DOI] [PubMed] [Google Scholar]
- 147.Hsu Y, Jubelin G, Taieb F, Nougayrede JP, Oswald E, Stebbins CE. Structure of the cyclomodulin Cif from pathogenic Escherichia coli. J Mol Biol. 2008;384:465–477. doi: 10.1016/j.jmb.2008.09.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Yao Q, Cui J, Zhu Y, Wang G, Hu L, Long C, Cao R, Liu X, Huang N, Chen S, et al. A bacterial type III effector family uses the papain-like hydrolytic activity to arrest the host cell cycle. Proc Natl Acad Sci U S A. 2009;106:3716–3721. doi: 10.1073/pnas.0900212106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Crow A, Race PR, Jubelin G, Varela Chavez C, Escoubas JM, Oswald E, Banfield MJ. Crystal structures of Cif from bacterial pathogens Photorhabdus luminescens and Burkholderia pseudomallei. PLoS One. 2009;4:e5582. doi: 10.1371/journal.pone.0005582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Samba-Louaka A, Nougayrede JP, Watrin C, Jubelin G, Oswald E, Taieb F. Bacterial cyclomodulin Cif blocks the host cell cycle by stabilizing the cyclin-dependent kinase inhibitors p21 and p27. Cell Microbiol. 2008;10:2496–2508. doi: 10.1111/j.1462-5822.2008.01224.x. [DOI] [PubMed] [Google Scholar]
- 151.Chavez CV, Jubelin G, Courties G, Gomard A, Ginibre N, Pages S, Taieb F, Girard PA, Oswald E, Givaudan A, et al. The cyclomodulin Cif of Photorhabdus luminescens inhibits insect cell proliferation and triggers host cell death by apoptosis. Microbes Infect. 2010;12:1208–1218. doi: 10.1016/j.micinf.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 152.Cui J, Yao Q, Li S, Ding X, Lu Q, Mao H, Liu L, Zheng N, Chen S, Shao F. Glutamine deamidation and dysfunction of ubiquitin/NEDD8 induced by a bacterial effector family. Science. 2010;329:1215–1218. doi: 10.1126/science.1193844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.McLaughlin LM, Govoni GR, Gerke C, Gopinath S, Peng K, Laidlaw G, Chien YH, Jeong HW, Li Z, Brown MD, et al. The Salmonella SPI2 effector SseI mediates long-term systemic infection by modulating host cell migration. PLoS Pathog. 2009;5:e1000671. doi: 10.1371/journal.ppat.1000671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Baldwin MR, Lakey JH, Lax AJ. Identification and characterization of the Pasteurella multocida toxin translocation domain. Mol Microbiol. 2004;54:239–250. doi: 10.1111/j.1365-2958.2004.04264.x. [DOI] [PubMed] [Google Scholar]
- 155.Repella TL, Ho M, Chong TPM, Bannai Y, Wilson BA. Arf6-dependent intracellular trafficking of Pasteurella multocida toxin and pH-dependent translocation from late endosomes. Toxins. 2011;3:218–241. doi: 10.3390/toxins3030218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Oswald E, Nougayrede JP, Taieb F, Sugai M. Bacterial toxins that modulate host cell-cycle progression. Curr Opin Microbiol. 2005;8:83–91. doi: 10.1016/j.mib.2004.12.011. [DOI] [PubMed] [Google Scholar]