Abstract
PURPOSE
To describe long-term trends in TB mortality and to compare trends estimated from two different sources of public health surveillance data.
METHODS
Trends and changes in trend were estimated by joinpoint regression. Comparisons between datasets were made by fitting a Poisson regression model.
RESULTS
Since 1900, TB mortality rates estimated from death certificates have declined steeply, except for a period of no change in the 1980s. This decade had long-term consequences resulting in more TB deaths in later years than would have occurred had there been no flattening of the trend. Recent trends in TB mortality estimated from National Tuberculosis Surveillance System (NTSS) data, which record all-cause mortality, differed from trends based on death certificates. In particular, NTSS data showed TB mortality rates flattening since 2002.
CONCLUSIONS
Estimates of trends in TB mortality vary by data source, and therefore interpretation of the success of control efforts will depend upon the surveillance dataset used. The datasets may be subject to different biases that vary with time. One dataset showed a sustained improvement in the control of TB since the early 1990s while the other indicated that the rate of TB mortality was no longer declining.
Keywords: Tuberculosis, Mortality, Trends, United States, Surveillance
INTRODUCTION
Tuberculosis (TB) incidence has been falling for the past 150 years in North America and Europe (1, 2). The mortality associated with TB in the United States has dropped rapidly since 1900, especially since the 1940s when new anti-tuberculous drugs became available (3, 4).
Mortality in patients with TB in the United States has been estimated from death certificates since the beginning of the 20th century. However, death certificates may not give reliable estimates of mortality for specific diseases, especially for respiratory and infectious diseases (5, 6). TB mortality rates since 1993 can also be estimated from the National Tuberculosis Surveillance System (NTSS) which has been collecting data on confirmed deaths of patients diagnosed with active TB disease. NTSS mortality data includes all deaths of TB patients including deaths that occurred just prior to TB diagnosis or during treatment.
We evauated TB mortality in the US from 1900 to 2006 using death certificate data in order to put recent trends in TB mortality in a long-term perspective. In addition, we compared recent trends in TB mortality estimated from death certificates and the NTSS in order to confirm that different surveillance systems give similar estimates of trends.
METHODS
Data
Numbers of deaths associated with TB on death certificates were taken from two sources: (a) Iskrant & Rogot (7) for 1900 to 1950, and (b) national estimates by the National Center for Health Statistics, National Vital Statistics Reports from 1953 to 2006 (8). These figures were used to show the long-term trends in deaths associated with TB in the United States from 1900 through 2006.
The NTSS provided data on the number of deaths from all causes among TB patients in the United States from 1993 to 2006. The NTSS is a nationally standardized system through which state health departments report all known TB cases to the CDC using fixed criteria (Report of a Verified Case of Tuberculosis), and includes both culture proven and clinically proven cases (9). It provides comprehensive data on all patients but over-estimates mortality associated with TB because it records deaths from all causes. NTSS mortality data included deaths that had occurred by the time the diagnosis of TB was confirmed, called “death by diagnosis” (10), and those who died from all causes during their TB therapy, called “death during treatment” (9). We included all deaths in the NTSS database in this analysis. For all years we used census estimates of population size for the United States (11).
Long-term TB Mortality Trends
We plotted trends in TB mortality from death certificate data on a logarithmic scale to illustrate trends in the United States from 1900 to 2006. Mortality was expressed as log(deaths per million) on the graphs to avoid negative numbers. Trends in TB mortality (the number of deaths per 100,000 population), and the years of inflection when trends changed, were estimated by joinpoint regression (12). This is a method for identifying joinpoints, or significant changes in trend, using permutation tests (12). A phase was defined as the years between two inflections when the trend was constant. The joinpoint regression model was only fitted to the data from 1953 to 2006 because those were the years for which contiguous data were available.
Comparison of Death Certificate and NTSS Datasets
To compare mortality trends based on death certificate versus NTSS data, we fitted a Poisson regression model with three predictor variables: time (continuous), data source (binary), and phases defined by the joinpoint regression (categorical). Number of deaths was used for the response variable and the log of population size was the offset. An adjustment was made for over-dispersion (13). Time was represented by years centered on the mid-point of the period covered by the model. The interaction of time by phase accounted for differences between phases. The interaction of time by dataset tested the hypothesis that the rate of change (or trend) in mortality was similar for both datasets. Interaction terms were evaluated with the likelihood ratio test (14).
RESULTS
Long-term TB Mortality Trends
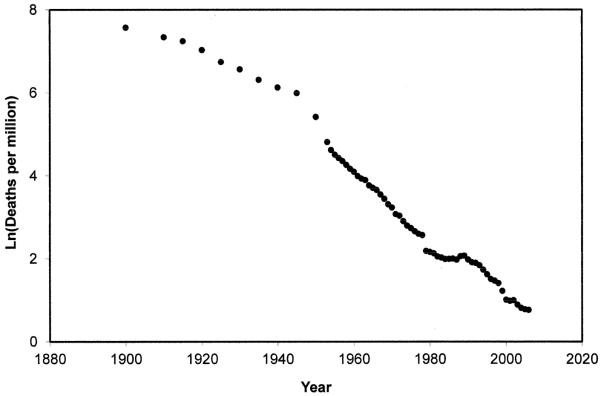
During the first half of the 20th century TB mortality fell steadily and then more rapidly (Figure 1). The steep decline was interrupted by a marked flat phase between 1982 and 1990 (Figure 1 and Table 1). We projected the number of deaths that would have occurred if rates continued to decline and compared it to the actual number of deaths. In the absence of a flat phase, we projected that the total TB deaths between 1982 and 2006 would have been 21,004 (Figure 2). The recorded total during that time was 33,567 deaths---a difference of 60%. In the absence of a flat phase, there would have been 297 deaths in 2006, compared to the 644 that were recorded for that year---a difference of 117%.
FIGURE 1.
Trends in TB mortality rates in the United States from 1900 through 2006 based on death certificates, shown on a logarithmic scale.
TABLE 1.
Trends in mortality associated with TB estimated by joinpoint regression from two sets of surveillance data.
| Variable | Dataset | Phase* | Annual % change (95% CI) |
|---|---|---|---|
| TB mortality since 1953 |
Death certificates |
1953 – 1955 | −14.2 (−18.6, −9.5) |
| 1955 – 1966 | −7.5 (−8.0, −7.0) | ||
| 1966 – 1982 | −9.5 (−10.0, −9.1) | ||
| 1982 – 1990 | 0.1 (−2.1, 2.4) | ||
| 1990 – 2006 | −8.2 (−9.0, −7.4) | ||
| TB mortality since 1993 |
NTSS § | 1993 – 2002 | −13.3 (−13.8, −12.9) |
| 2002 – 2006 | −3.4 (−5.8, −0.9) |
Phases were defined as the years between the inflection points identified by the joinpoint regression.
NTSS: National Tuberculosis Surveillance System.
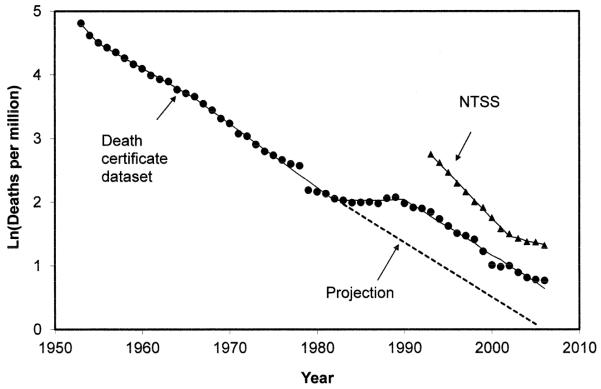
FIGURE 2.
Comparison of mortality trends estimated from death certificates (filled circles) and from the National Tuberculosis Surveillance System (NTSS) (triangles). The solid lines show the fitted joinpoint regression models. The broken line indicates the projected number of deaths from 1982 to 2006, assuming that the mortality rate decreased by 8.2% annually.
The drop in mortality between 1978 and 1979 (Figure 1) followed a change in reporting criteria (8). Consequently the calculation of excess deaths, which treats the decline as real, is likely an underestimate.
Comparison of Death Certificate and NTSS Datasets
We compared trends in the most recent phase of the death certificate data (1990 – 2006; Table 1) with the NTSS data for the United States (1993 – 2006; Table 1) by fitting a Poisson regression model. As expected, the mortality estimates were higher (p < 0.001) in the NTSS dataset (Figure 2). A significant (p < 0.001) interaction between time and dataset indicated that estimated mortality trends differed between datasets (Table 1). Consequently, the ratio between the two datasets decreased during the 1990s because of the steeper NTSS slope (Figure 2). Furthermore, the NTSS dataset indicated a change in trend in 2002 (the interaction between time and phase was significant [p < 0.001]) from −13.3% to −3.4% per annum, while the death certificates showed a constant trend with no inflection (Table 1 and Figure 2).
DISCUSSION
Long-term Trends
According to death certificate data, TB mortality fell in the United States during the first half of the 20th century as living standards, public health efforts and TB case finding improved, bovine TB was eradicated and educational campaigns expanded (4, 15, 16). Mortality declined even more steeply after new anti-TB drugs, such as streptomycin (introduced in 1944) and isoniazid (introduced in 1952), were discovered and raised hopes of a dramatic reduction in TB deaths by century’s end (3, 16). However, the mortality decline ended abruptly and unexpectedly in the early 1980s.
This long-term perspective (Figure 1) reveals the 1980s as a “lost decade” for TB control. The resurgence of TB in the 1980s came at a time of reduced spending on public health and TB prevention (17, 18). Immigration was increasing, with many immigrants coming from countries where TB was endemic (19, 20). Injection drug use was also associated with the rise in TB deaths in some northeastern cities (21, 22) while outbreaks of multidrug-resistant TB contributed to the spread of a more lethal form of TB in crowded institutions (23).
Most significantly, the resurgence of TB in the US coincided with the HIV/AIDS epidemic that emerged in the 1980s. HIV increases the probability of TB infection, accelerates the progression of TB disease and significantly increases the probability of death in TB patients (24-27). The first signs of HIV/AIDS were noticed in 1981(28) and correlate well with the inflection in the TB mortality trends observed in this analysis. The change in TB mortality trend (Figure 1) actually began in about 1979, before HIV was discovered, and earlier than the trend in TB incidence which increased in the mid-1980s (29): unrecognized HIV may have been causing additional TB deaths earlier than previously realized. It is likely that it was the synergy of emerging HIV, reduced public health funding, immigration and drug-resistant TB that played a critical role in changing the dynamics of TB mortality in the US in the 1980s.
The steady decline in TB mortality resumed in the 1990s as federal funding increased, new clinics opened, HIV treatment improved, directly observed therapy expanded, and contact tracing increased to interrupt transmission (16). Nevertheless, the flat phase of the 1980s had serious long-term consequences. Even allowing for the uncertainties inherent in projections, annual TB deaths may now be double the number that would have occurred had there been no flattening of the trend in the 1980s.
Comparison of Death Certificate and NTSS Datasets
TB mortality estimates based on death certificates, representing deaths caused by TB or exacerbated by TB, were lower than the NTSS estimates. While differing in absolute number, the two datasets would show parallel trends in mortality if each were a reliable index of TB mortality. However, the mortality rates derived from NTSS data declined more steeply in the 1990s than the death rates based on death certificates, but less steeply after 2002. These differences suggest varying biases in one or both datasets. The NTSS records deaths from all causes in TB patients under treatment and therefore overestimates mortality associated with TB, while death certificates may substantially under-record TB deaths, especially given that a TB diagnosis can take months to complete and is often delivered after a patient has died (5). For example, TB was not recorded on the death certificates of two-thirds of those dying with active TB disease in New York in 1992 (5). Furthermore, the criteria for recording TB on death certificates is not standardized and sometimes changes (8).
Since the NTSS did not identify the exact cause of death in TB patients, trends in other diseases may account for a changing proportion of deaths among TB patients. A major recent change is the increasing prevalence of obesity (30). Associated maladies such as diabetes may be changing the profile of TB patients over time as well as reducing their probability of surviving treatment (31).
The differences between these datasets are important, because interpretation of the success of control efforts will depend upon the surveillance dataset used. For example, the death certificate dataset showed a constant mortality decline from 1990 to 2006, indicating a sustained improvement in TB control measures. In contrast, the flattening in mortality trend since 2002 in the NTSS data suggests a significant change in the epidemiology of TB. This flattening, while only evident in one dataset, is worrying and warrants further investigation.
In an environment of overall declining TB mortality, the flat phases are of great consequence because they result in more deaths in the long-term. If one accepts that the recent inflection in the trend is real, even though it was evident in only one dataset, then it will result in more deaths in the future than would have been the case had mortality continued to decline steadily. These results demonstrate that it is important to document trends in TB mortality consistently and to identify changes early in order to discover their likely causes. Starting in 2009, the Report of Verified Case of Tuberculosis, on which the NTSS data is based, was amended to include information on whether or not a death was due to or related to TB. This improvement will enable future trends in TB deaths to be estimated more accurately.
Limitations of this study include the accuracy with which death certificates are completed and the proportion of NTSS subjects lost to follow up whose deaths were not recorded. Furthermore, trends in other diseases afflicting TB patients would also have influenced the rate of all-cause mortality in the NTSS data.
Acknowledgments
This work was supported by California HIV/AIDS Research Program at the University of California (fellowship CF07-SD-302), the National Institutes of Health (grant T32DA023356) and the National Institute of Allergy and Infectious Diseases (grant K01AI083784) to T.C. Rodwell. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases, the National Institutes of Health or the Centers for Disease Control and Prevention.
Selected Abbreviations and Acronyms
- TB
Tuberculosis
- NTSS
National Tuberculosis Surveillance System
- CDC
Centers for Disease Control and Prevention
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Daniel TM. Captain of death: the story of tuberculosis. University of Rochester Press; Rochester, New York: 2002. [Google Scholar]
- 2.Grigg ER. The arcana of tuberculosis, with a brief epidemiological history of the disease in the USA. Am Rev Tuberc Pulm. 1958;78(2):151–72. doi: 10.1164/artpd.1958.78.2.151. [DOI] [PubMed] [Google Scholar]
- 3.Doege TC. Tuberculosis mortality in the United States, 1900 to 1960. JAMA. 1965;192(12):103–6. doi: 10.1001/jama.1965.03080250023005. [DOI] [PubMed] [Google Scholar]
- 4.Wilson LG. The historical decline of tuberculosis in Europe and America: its causes and significance. J Hist Med Allied Sci. 1990;45:366–96. doi: 10.1093/jhmas/45.3.366. [DOI] [PubMed] [Google Scholar]
- 5.Washko RM, Frieden TR. Tuberculosis surveillance using death certificate data, New York City, 1992. Public Health Rep. 1996;111:251–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Drummond MB, Wise RA, John M, Zvarich MT, McGarvey LP. Accuracy of death certificates in COPD: analysis from the TORCH trial. COPD. 2010;7:179–85. doi: 10.3109/15412555.2010.481695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iskrant AP, Rogot E. Trends in tuberculosis mortality in continental United States. Public Health Rep. 1953;68(9):911–9. [PMC free article] [PubMed] [Google Scholar]
- 8.CDC . Mortality trends tables United States. Centers for Disease Control and Prevention; 2008. http://www.cdc.gov/tb/statistics/reports/2008/pdf/4_MorbTrend.pdf. [Google Scholar]
- 9.CDC Decrease in reported tuberculosis cases---United States, 2009. MMWR. 2010;59(10):289–94. [PubMed] [Google Scholar]
- 10.CDC . CDC WONDER on-line Database. Centers for Disease Control and Prevention, Division of TB Elimination; 2007. Online Tuberculosis Information System (OTIS), National Tuberculosis Surveillance System, United States, 1993-2007. http://wonder.cdc.gov/tb-v2007.html. [Google Scholar]
- 11.U.S. Bureau of the Census National population estimates. http://www.census.gov/popest/estimates.html.
- 12.Kim H-J, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–51. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 13.McCullagh P, Nelder JA. Generalized linear models. 2nd ed. Chapman & Hall; London: 1989. [Google Scholar]
- 14.SAS . SAS/STAT 9.1 User’s Guide. SAS Institute Inc; Cary, NC: 2004. [Google Scholar]
- 15.Myers JA. Captain of all these men of death: Tuberculosis historical highlights. Warren H. Green Inc.; St Louis, Missouri: 1977. [Google Scholar]
- 16.Snider GL. Tuberculosis then and now: a personal perspective on the last 50 years. Ann Intern Med. 1997;126(3):237–43. doi: 10.7326/0003-4819-126-3-199702010-00011. [DOI] [PubMed] [Google Scholar]
- 17.Brudney K, Dobkin J. Resurgent tuberculosis in New York City: human immunodeficiency virus, homelessness, and the decline of tuberculosis control programs. Am Rev Respir Dis. 1991;144:745–9. doi: 10.1164/ajrccm/144.4.745. [DOI] [PubMed] [Google Scholar]
- 18.Reichman L. The U-shaped curve of concern. Am Rev Respir Dis. 1991;144:741–2. doi: 10.1164/ajrccm/144.4.741. [DOI] [PubMed] [Google Scholar]
- 19.Rieder HL, Cauthen GM, Kelly GD, Bloch AB, Snider DE. Tuberculosis in the United States. JAMA. 1989;262(3):385–9. [PubMed] [Google Scholar]
- 20.Cain KP, Haley CA, Armstrong LR, Garman KN, Wells CD, Iademarco MF, et al. Tuberculosis among foreign-born persons in the United States: achieving tuberculosis elimination. Am J Respir Crit Care Med. 2007 Jan 1;175(1):75–9. doi: 10.1164/rccm.200608-1178OC. [DOI] [PubMed] [Google Scholar]
- 21.Reichman LB, Felton CP, Edsall JR. Drug dependence, a possible new risk factor for tuberculosis disease. Arch Intern Med. 1979;139:337–9. [PubMed] [Google Scholar]
- 22.Friedman LN, Williams MT, Singh TP, Frieden TR. Tuberculosis, AIDS, and death among substance abusers on welfare in New York City. N Engl J Med. 1996;334(13):828–33. doi: 10.1056/NEJM199603283341304. [DOI] [PubMed] [Google Scholar]
- 23.Frieden T, Sherman L, Maw K, Fujiwara P, Crawford J, Nivin B, et al. A multi-institutional outbreak of highly drug-resistant tuberculosis. JAMA. 1996;276(15):1229–35. [PubMed] [Google Scholar]
- 24.Braun MM, Coté TR, Rabkin CS. Trends in death with tuberculosis during the AIDS era. JAMA. 1993;269(22):2865–8. [PubMed] [Google Scholar]
- 25.Pablos-Mendez A, Sterling TR, Frieden TR. The relationship between delayed or incomplete treatment and all-cause mortality in patients with tuberculosis. JAMA. 1996;276(15):1223–8. doi: 10.1001/jama.1996.03540150025026. [DOI] [PubMed] [Google Scholar]
- 26.Shah S, Cain KP, Marks S, Cavanaugh J. Mortality among patients with tuberculosis and associations with HIV status---United States, 1993-2008. MMWR. 2010;59(46):1509–13. [PubMed] [Google Scholar]
- 27.Sterling TR, Zhao Z, Khan A, Chaisson RE, Schluger NW, Mangura B, et al. Mortality in a large tuberculosis treatment trial: modifiable and non-modifiable risk factors. Int J Tuberc Lung Dis. 2006;10(5):542–9. [PubMed] [Google Scholar]
- 28.Gottlieb MS, Schanker HM, Fan PT, Saxon A, Weisman JD, Pozalski I. Pneumocystis Pneumonia---Los Angeles. MMWR. 1981 June 5;30(21):1–3. 1981. [Google Scholar]
- 29.Cantwell MF, Snider DE, Cauthen GM, Onorato IA. Epidemiology of tuberculosis in the United States, 1985 through 1992. JAMA. 1994;272(7):535–9. [PubMed] [Google Scholar]
- 30.Flegal K, Carroll M, Ogden C, Curtin L. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303(3):235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 31.Dooley K, Chaisson R. Tuberculosis and diabetes mellitus: convergence of two epidemics. Lancet Infect Dis. 2009;9:737–46. doi: 10.1016/S1473-3099(09)70282-8. [DOI] [PMC free article] [PubMed] [Google Scholar]