Abstract
BACKGROUND
Many states require screening of individuals arrested for driving under the influence of alcohol (DUI) to determine recidivism risk and the need for treatment based on severity of alcohol problems. Several screening instruments use DSM-IV criteria for alcohol abuse and dependence to assess alcohol problems in this population, but whether they adequately measure alcohol problems in individuals with DUIs has not been examined. In addition, gender differences in DUI samples suggest that female offenders have more severe alcohol problems than male offenders. The current study examines differences in alcohol criteria functioning by DUI history and gender using an item response theory (IRT) approach.
METHODS
Data from diagnostic interviews with 8605 participants in the Collaborative Study on the Genetics of Alcoholism, including 1655 who ever reported a DUI arrest (20% women), were used to examine differences in alcohol criteria functioning between men and women with and without DUIs. The factor underlying item response was conceptualized as unidimensional, representing alcohol problem severity.
RESULTS
Social/interpersonal problems, larger/longer, and inability/persistent desire to quit displayed greater discrimination of IRT-defined alcohol problem severity among individuals with DUIs than those without. Irrespective of DUI status, women had a higher threshold than men for time spent drinking or recovering. Women without DUIs had a higher threshold than similar men for social/interpersonal problems. Taken as a whole, the criteria yielded similar amounts of information in all groups.
CONCLUSIONS
DSM-IV criteria for alcohol abuse and dependence adequately detect alcohol problem severity in individuals with DUIs and some are better at detecting severity in this particularly high-risk group than in individuals without DUIs. However, the criteria as a whole are equally effective in measuring alcohol problem severity among individuals with and without DUIs, and may be used with confidence in screening DUI offenders.
Keywords: DUI, Alcohol Use Disorder, Item Response Theory
INTRODUCTION
Individuals arrested for driving under the influence of alcohol (DUI) represent a significant risk to public health, accounting for more than 10,000 crash-related deaths on U.S. highways in 2009, or 32% of all crash-related fatalities (U.S. Department of Transportation, 2009). Many states require screening of DUI arrestees to determine recidivism risk and the need for treatment based on severity of alcohol problems. The accuracy of screening instruments used in this population has been questioned, however, and their ability to detect alcohol-related problems varies (Chang et al., 2002; Lapham et al., 1995). Several screening instruments use Diagnostic and Statistical Manual of Mental Disorders criteria (DSM, American Psychiatric Association, 1994; 1987) to assess alcohol use severity and to categorize abuse and dependence (Kincannon, 1984; ADE Incorporated, 2007; Behavior Data Systems, 1987). According to a review of screening instruments used in DUI populations, these instruments are widely used in judicial settings but have not been sufficiently evaluated (Chang et al., 2002). Furthermore, underreporting of alcohol use and its behavioral consequences is common during court-ordered screening (Lapham et al., 2004). Testing the measurement characteristics of DSM criteria in individuals with histories of DUI, using data obtained outside a criminal justice setting, can contribute to the evaluation of screening instruments in this population.
Women account for an increasing proportion of individuals arrested for DUI. Arrests of women for DUI rose 31% but decreased 11% for men between 2000 and 2009 (Federal Bureau of Investigation, 2009). Previous work has shown that women with DUIs are more likely than their male counterparts to report unsuccessful quit attempts, spending a great deal of time drinking or recovering from drinking, continued alcohol use despite family problems and psychological problems, and withdrawal symptoms (McCutcheon et al., 2009). These gender differences suggest more severe alcohol problems among women than men with DUIs, consistent with studies showing higher rates of alcohol dependence among female than male recidivists (Lapham et al., 2006; Laplante et al., 2008). This evidence for gender differences in alcohol problem severity among DUI offenders, combined with scant evidence for gender differences in other high risk samples (Bucholz et al., 1996; Kahler et al., 2003; Schuckit et al., 1998; Wu et al., 2009), suggests that women with DUIs may represent a particularly severe alcohol use phenotype. There is thus a need to test whether the DSM-IV criteria for alcohol abuse and dependence measure alcohol problems adequately and to a similar degree in men and women with DUI histories. Such evaluation is important given the increasing numbers of women arrested for DUI and the public concern with this trend, as evidenced by frequent news articles about women arrested for DUI (e.g., Flam, 2009; Lundstrom, 2009; Tellier, 2009).
The current study examines differences in DSM-IV alcohol abuse and dependence criteria functioning by gender and by DUI history using an item response theory (IRT) approach. Previous studies using this approach have found differences in measurement characteristics of abuse and dependence criteria by gender (Harford et al., 2009; Kahler and Strong, 2006; Nichol et al., 2007; Saha et al., 2006), treatment group (Wu et al., 2009), and sample ascertainment method (i.e., clinical, adjudicated, or population-based; Gelhorn et al., 2008). Investigating the measurement characteristics of DSM-IV alcohol abuse and dependence criteria in individuals with DUIs will contribute to the evaluation of screening instruments used in this population and also to understanding the functioning of these criteria in a high-risk population.
MATERIALS AND METHODS
Sample
Data were collected from 1287 probands and 7318 relatives of probands who participated in the Collaborative Study on the Genetics of Alcoholism (COGA), a high-risk family study of alcohol dependence (Foroud et al., 2000; Reich et al., 1998). Probands were recruited from treatment settings in 6 catchment areas (Farmington, CT; Brooklyn, NY; Indianapolis; IN, St. Louis, MO; Iowa City, IA; and San Diego, CA) and were required to meet criteria for DSM-III-R alcohol dependence ( American Psychiatric Association, 1987), Feighner definite alcoholism (Feighner et al., 1972), and to have at least two first-degree relatives available for study. The institutional review board at each site approved the protocol, and written informed consent was obtained from all subjects. Details about ascertainment are available from previous studies (Bucholz et al., 1996; Reich et al., 1998). The sample was 51% male, 74% non-Hispanic white, 17% African American, 6% Hispanic white, and 3% other ethnicity, with a mean age of 40.2 (sd = 13.6). Forty-nine percent of participants were married at time of interview, 28% had never been married, and 23% were widowed, separated, or divorced. Approximately half (47%) had greater than a high-school education, 37% had finished high school or passed an equivalency exam, and 16% had less than a high school education. Individuals with DUIs (19.2%) compared to those without DUIs were slightly older (mean (sd) = 41.9 (11.3) vs. 39.7 (14.1), p < .001), less likely to be African American (10.8% vs. 18.4%, p < .001), more likely to be separated or divorced (34.0% vs. 18.2%, p < .001), and more likely to have a yearly household income below $20,000 (35.6% vs. 25.4%, p < .001). Nearly all met criteria for an alcohol use disorder (AUD, = either alcohol abuse or dependence, 98.1% versus 59.9% for individuals without DUIs), and they endorsed a greater number of AUD criteria than individuals with no DUIs (range 0 – 11, DUI, mean (sd) = 8.3 (2.7); No DUI = 3.1 (3.2), p < .001)). The relatively high prevalence of AUDs and high mean symptom count for the non-DUI group reflects the high density of AUDs in the COGA families.
Measures
The Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA; Bucholz et al., 1994; Bucholz et al., 1995) was used to assess alcohol abuse and dependence symptoms. The SSAGA has shown high reliability and validity in diagnosing alcohol dependence and has good inter-rater reliability for individual alcohol criteria (Bucholz et al., 1994; Bucholz et al., 1995; Hesselbrock et al., 1999). The current study uses lifetime abuse and dependence criteria based on DSM-IV definitions (American Psychiatric Association, 1994). Two criteria, legal problems and time spent, were strictly operationalized in the interview . The dependence criterion for spending “a great deal of time … in activities necessary to obtain the substance or recover from its effects” (American Psychiatric Association, 1994, p. 181) was coded positive for respondents who answered “yes” to the question “Has there ever been a period of several days or more when you spent so much time drinking or recovering from the effects of alcohol that you had little time for anything else?” and also reported 3 or more such periods or a period lasting at least one month. The abuse criterion for legal problems was coded positive for individuals who reported 3 or more arrests for DUI or reported 3 or more arrests in a 12-month period for other drunken behavior. History of DUI was based on self-report in answer to the question “Have you ever been arrested for drunk driving?” and number of times arrested. Of individuals with DUIs, a majority reported one (n=822), 368 reported two, and 465 individuals reported three or more DUIs.
Statistical analysis
Two abuse criteria, hazardous use and legal problems, were excluded from the analysis due to their tautology with DUI status (i.e., arrest for DUI contributes to the legal problems criterion, and accident resulting from drinking and driving contributes to the hazardous use criterion). In order to determine whether arrest for DUI was simply a proxy for alcohol abuse (and thus did not index a group of individuals distinct from other individuals who met abuse criteria), we examined differences in alcohol and drug use and psychiatric disorder between individuals with DUIs and individuals who met abuse criteria but did not endorse arrest for DUI or accident due to drinking and driving.
Exploratory factor analysis (EFA; Fabrigar et al., 1999) was used to determine the number of factors required to explain the covariance across the 2 alcohol abuse (i.e. excluding hazardous use and legal problems) and 7 dependence criteria for all participants and in groups defined by DUI status and gender (men and women with DUIs; men and women with no DUIs) before proceeding with an item response theory (IRT; Muthén and Lehman, 1985) analysis. The EFA results supported the unidimensionality of the criteria and a confirmatory one factor model (using confirmatory factor analysis or CFA) was used for all subsequent models. Parameters from CFA can be converted into a 2 parameter (2P) logistic item response model (Muthén and Lehman, 1985) characterized by discrimination and difficulty. Discrimination represents the ability of a criterion to distinguish individuals at high risk for AUDs from those at relatively lower risk. Difficulty reflects the location along the liability continuum where the criterion has a .50 probability of endorsement. It thus represents the threshold on the alcohol severity continuum where the criterion becomes more likely to be endorsed than not.
The direct effects of gender on AUD criteria in the sample as a whole were tested within the item-response model by regressing each criterion on the alcohol severity factor and gender simultaneously. A significant effect of gender on a criterion beyond that accounted for by underlying mean differences in the alcohol severity factor indicates that the criterion has different measurement characteristics in men and women, or measurement non-equivalence, and that the data should be grouped separately by gender. Similar tests were performed to evaluate direct effects of number of DUIs on AUD criteria using dummy variables representing individuals with 1, 2, and 3 or more DUIs. Based on the results of these tests, a 4-group model, with groups defined by DUI status (yes/no) and gender, was used to test the residual association of each of the 9 criteria with DUI status. In these models, factor means were set to zero for women without DUIs and were freely estimated in the other groups. As there was evidence for unequal variances (X2(4) = 128.54, p < .0001), variances were freely estimated across groups and the discrimination and difficulty parameters for role failure, which showed no evidence of differential criterion functioning (DCF), were constrained across groups to identify the model. The baseline model against which subsequent models were compared constrained the discrimination and difficulty parameters for all criteria across groups. For each criterion individually (except role failure), a model was fit which freed the discrimination and difficulty parameters for individuals with DUIs (male and female DUI groups were equated) and a likelihood ratio test on 2 degrees of freedom was computed using the baseline model for comparison. If this test yielded a statistically significant improvement in fit (based on a p-value of ≤ .01, and calculated using equations available at statmodel.com), 2 additional tests were conducted to assess DCF by gender for individuals with and without DUIs, using the previous model for comparison. If no DCF by DUI status was found, then a single test of DCF by gender was performed, using the baseline model for comparison. The final model incorporated all significant differences between groups.
For criteria showing DCF, effect sizes for were calculated for difficulty parameters showing DCF as the absolute difference in thresholds between groups and item characteristic curves (ICCs) were computed to provide a visual representation of group differences in both discrimination and difficulty (Steinberg and Thissen, 2006). In ICCs, criteria with greater discrimination will have steeper curves (i.e., higher factor loading). Likewise, criteria with greater difficulty will have higher thresholds (i.e., will correspond to higher numbers on the x-axis, representing greater severity) and will appear farther from the y-axis. Conversely, more commonly endorsed criteria tend to have lower difficulty and will appear closer to the y-axis in ICCs. A partial item information curve was also computed from the final model parameters to illustrate the aggregate information about AUD severity gleaned from the criteria showing DCF for each of the 4 groups. In the information curves, the height of the peak corresponds to measurement precision, with higher peaks having greater precision, and the kurtosis corresponds to the range of severity over which liability is measured.
Descriptive statistics were computed using Stata statistical software (StataCorp, 2009), and factor analysis and IRT models were computed using Mplus (Muthen and Muthen, 2007). All models were adjusted for the clustering of family data.
RESULTS
Rates of alcohol dependence for individuals with and without DUIs were 81.3% and 30.8%, respectively; nearly all of these also met criteria for abuse. Seventeen percent of individuals with DUIs and 29.1% of those without DUIs met criteria for abuse only.
DUI versus alcohol abuse with no DUI
Individuals with DUIs (n=1655)were compared to those who met abuse criteria (with or without dependence) but reported no DUIs or accidents due to drinking and driving (n=3852). The purpose of this comparison was to establish that DUI status was not merely a proxy for alcohol abuse but distinguished a group distinct from individuals with abuse but no DUI. Individuals with DUIs, compared to those without, began drinking at a younger age (mean (sd) = 16.9 (4.5) vs. 17.8 (4.7), p < .001), reported a higher lifetime maximum number of drinks in 24 hours (mean (sd) = 34.2 (22.5) vs. 22.2 (21.4), p < .001), and endorsed more AUD criteria (after excluding hazardous use and legal problems from the criterion set; range 0 – 9, mean (sd) = 6.4 (2.7) and 3.8 (2.9), p < .001). Individuals with DUIs also had higher lifetime rates of illicit drug use (77.0% vs. 67.9%, p < .001), major depression (50.6% vs. 45.7%, p < .001), and antisocial personality disorder (ASPD, 29.0% vs. 15.7%, p < .001) and lower rates of conduct disorder without ASPD (3.7% vs. 5.3%, p < .001) than those who met abuse criteria but had no DUIs or car accidents due to drinking and driving. History of DUI thus indexes a greater severity of alcohol problems that is distinct from alcohol abuse without DUI, as reflected in greater alcohol use and symptoms and higher rates of co-occurring drug use and psychiatric disorder.
Unidimensionality
Fit statistics from exploratory factor analysis indicated that a one-factor model was optimal for these data, with a Comparative Fit Index (CFI) =.998, Tucker-Lewis Index (TLI) =.999 and Root Mean Square Error of Approximation (RMSEA) =.034. In each subgroup as well (men with and without DUIs, women with and without DUIs), fit statistics indicated a unidimensional structure provided the best fit to the data, with CFIs and TLIs ranging from .992 to .999 and RMSEAs ranging from .025 to .061.
Tests of measurement non-equivalence by gender and number of DUIs
Tests of direct effects of gender on AUD criteria in the sample as a whole, adjusted for the underlying severity factor, found that women were less likely than men to report social/interpersonal problems (OR = 0.49, 95 % CI = 0.39 – 0.62) and were more likely to report drinking larger amounts than intended or for longer periods of time (OR = 1.32, 95 % CI = 1.09 – 1.61), spending so much time drinking or recovering that there was little time for anything else (OR = 1.38, 95 % CI = 1.08 – 1.76), and continued drinking despite physical or psychological problems (OR = 1.33, 95 % CI = 1.05 – 1.69). In tests evaluating direct effects of number of DUIs on AUD criteria, only the social/interpersonal problems criterion showed differential reporting by number of DUIs. Individuals with 2 (OR = 1.53, 95 % CI = 0.67 – 2.39) and 3 or more DUIs (OR = 1.88, 95 % CI = 0.81 – 2.95) did not differ in rates of endorsement (X2 (1) = 0.45, p = 0.50) but individuals with 1 DUI (OR = 0.55, 95 % CI = 0.15 – 0.94) were less likely to endorse this criterion than those with multiple DUIs (X2 (1) = 14.94, p = .0001). Because this was the only criterion showing differential endorsement by number of DUIs, and because nearly all individuals with 2 or more DUIs endorsed it (95.6 %), we elected to use the more parsimonious model of DUI status as binary (yes/no). A 4-group model was thus used to test whether measurement characteristics for the 9 AUD criteria differed across men with and without DUIs and women with and without DUIs.
Tests of DCF for individual criteria
All criteria were endorsed more frequently by individuals with, than by those without, DUIs (Table 1). Of the criteria included in the IRT analysis, drinking larger amounts or for longer periods of time than intended (larger/longer) was the most commonly endorsed and spending so much time drinking or recovering from drinking that there was little time for anything else (time spent drinking/recovering) was the least frequent. Results of 4-group IRT models testing DCF of individual criteria are reflected in the letter superscripts accompanying the frequencies in Table 1, with different letters across rows indicating significant differences in endorsement after accounting for the alcohol severity factor. The tests revealed DCF by DUI status and gender for social/interpersonal problems and larger/longer; gender differences were significant only among individuals without DUIs. Inability/persistent desire to quit showed DCF by DUI status only while time spent drinking/recovering and physical/psychological problems showed DCF by gender but not by DUI status. There was no evidence of DCF for tolerance, withdrawal, or activities given up, and so the IRT parameters for these criteria were constrained across groups in the final model. Results of the final model accounting for these similarities and differences and for differences in factor means are displayed in Table 2, and item characteristic curves (ICCs) representing group differences for criteria with DCF are displayed in Figure 1.
Table 1.
Lifetime prevalence (%) of DSM-IV alcohol abuse and dependence criteria endorsement, by DUI status and gender
| NO DUI | DUI | |||
|---|---|---|---|---|
| Male (n=3056) | Female (n=3894) | Male (n=1330) | Female (n=325) | |
| Abuse Criteria | ||||
| Role failure | 29.5 A | 19.9 A | 72.6 A | 64.6 A |
| Hazardous use1 | 63.5 | 43.3 | 96.5 | 91.4 |
| Legal problems1 | 5.1 | 1.1 | 42.9 | 21.8 |
| Social/interpersonal problems | 44.8 A | 27.9 B | 88.5 C | 78.8 C |
| Dependence criteria | ||||
| Tolerance | 45.4 A | 33.4 A | 81.9 A | 75.7 A |
| Withdrawal | 18.4 A | 12.1 A | 54.2 A | 45.8 A |
| Larger/longer | 57.8 A | 47.6 B | 90.7 C | 88.6 C |
| Inability/persistent desire to quit | 48.1 A | 35.8 A | 84.7 B | 77.2 B |
| Time spent drinking/recovering | 14.9 A | 10.7 B | 44.5 A | 44.6 B |
| Activities given up | 22.3 A | 14.5 A | 63.1 A | 53.2 A |
| Physical/Psychological problems | 26.4 A | 18.5 B | 66.1 A | 64.0 B |
NOTES:
excluded from IRT analysis due to redundancy with DUI status;
different superscripts across rows indicate differences between groups at p < .01 from tests of DCF for individual criteria, adjusted for underlying alcohol severity factor; same superscript indicates no statistically significant difference
Table 2.
Criterion response parameter estimates from final model, with 95% confidence intervals
| No DUI | DUI | ||||
|---|---|---|---|---|---|
| Discrimination | Difficulty | Discrimination | Difficulty | Effect Size | |
| Role failure | 2.41 (1.78–3.05) | 4.76 (4.18–5.34) | 2.41 (1.78–3.05) | 4.76 (4.18–5.34) | NO DCF |
| Social/interpersonal problems A, B | |||||
| Male | 1.87 (1.37–2.38) | 2.10 (1.65–2.54) | 2.36 (1.56–3.15) | 2.46 (1.52–3.39) | .36 |
| Female | 2.05 (1.40–2.69) | 2.81 (2.37–3.25) | 2.36 (1.56–3.15) | 2.46 (1.52–3.39) | .35 |
| Tolerance | 1.05 (0.77–1.32) | 1.18 (1.01–1.35) | 1.05 (0.77–1.32) | 1.18 (1.01–1.35) | NO DCF |
| Withdrawal | 2.03 (1.54–2.52) | 5.68 (5.13–6.23) | 2.03 (1.54–2.52) | 5.68 (5.13–6.23) | NO DCF |
| Larger/longer A, B | |||||
| Male | 1.25 (0.91–1.59) | 0.45 (0.18–0.71) | 1.55 (1.14–1.95) | 0.68 (0.00–1.36) | .23 |
| Female | 1.15 (0.81–1.49) | 0.18 (0.00–0.36) | 1.55 (1.14–1.95) | 0.68 (0.00–1.36) | .50 |
| Inability/persistent desire to quit A | 1.19 (0.87–1.52) | 1.13 (0.94–1.33) | 1.54 (1.10–1.99) | 1.69 (1.03–2.35) | .56 |
| Time spent drinking/recovering B | |||||
| Male | 1.48 (1.15–1.81) | 4.80 (4.28–5.32) | 1.48 (1.15–1.81) | 4.80 (4.28–5.32) | |
| Female | 1.76 (1.24–2.27) | 5.26 (4.61–5.91) | 1.76 (1.24–2.27) | 5.26 (4.61–5.91) | M:F .46 |
| Activities given up | 2.27 (1.69–2.85) | 5.58 (5.00–6.16) | 2.27 (1.69–2.85) | 5.58 (5.00–6.16) | NO DCF |
| Physical/psychological problems B | |||||
| Male | 1.88 (1.40–2.35) | 4.21 (3.68–4.73) | 1.88 (1.40–2.35) | 4.21 (3.68–4.73) | |
| Female | 1.99 (1.40–2.59) | 4.19 (3.65–4.72) | 1.99 (1.40–2.59) | 4.19 (3.65–4.72) | M:F .02 |
NOTE: letter superscripts indicate group differences by DUI status and/or gender,
parameters vary by DUI status;
parameters vary by gender.
NO DCF = no evidence of DCF (see Table 1) and so IRT parameters were constrained across groups. Effect size compares difficulty parameters across rows unless noted by M:F (denotes male-to-female comparison)
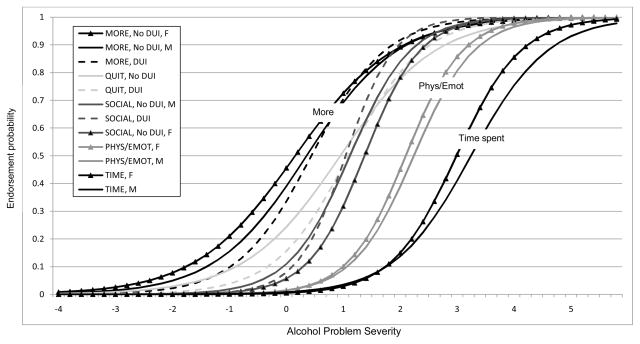
Figure 1.
Item characteristic curves of 5 AUD criteria which displayed DCF in IRT analysis, by DUI status and gender corresponding to DCF findings.
NOTES: Legend entries correspond to curves going from left to right (nearest to farthest from y-axis). Female curves marked with triangles. DUI curves are dashed lines.
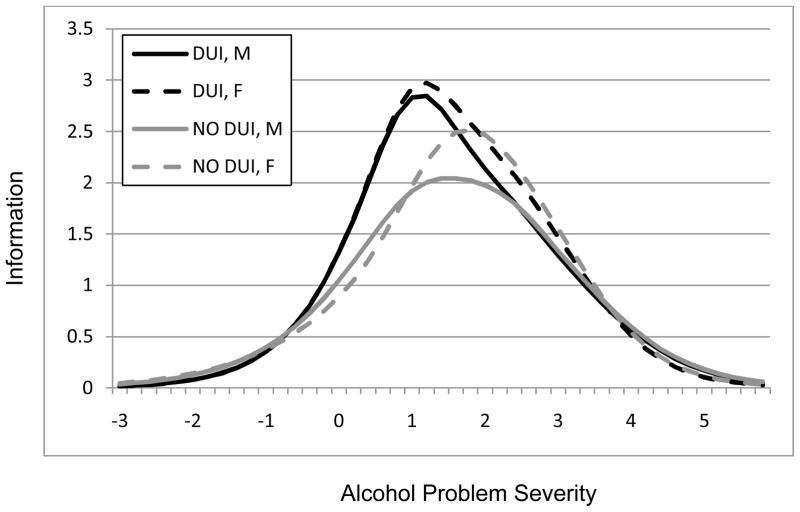
The curve representing Larger/Longer (“More” in the graph) is closest to the y-axis, corresponding to its frequent endorsement in Table 1 and its low difficulty parameters in Table 2, indicating that it is endorsed at lower levels of alcohol problem severity. The slope of the “More” curve for the DUI category is steepest, reflecting its higher discrimination parameter in Table 2. “Time Spent” is farthest from the y-axis, corresponding to its infrequent endorsement in Table 1 and its high difficulty parameters in Table 2, indicating that a high level of severity is needed before it is more likely to be endorsed. The slope of the curve is greater for women than for men, reflecting its greater discrimination among women. A similar gender pattern was observed for Physical/Psychological problems (“Phys/Emot” to the left of “Time Spent”). Sandwiched between “More” and “Phys/Emot” are Social/Interpersonal problems (“Social” in graph) and Inability/Persistent desire to quit (“Quit” in graph). Slopes for the DUI group (dotted lines) were steeper for both these criteria, showing greater discrimination among individuals with than among those without DUIs. The intersection of the lines representing “More,” “Quit,” and “Social” for individuals with DUIs (dotted lines) with the lines for those without DUIs (solid lines) illustrates the greater discrimination of these criteria among individuals with DUIs. Information curves representing the aggregate information gleaned from the 5 criteria showing DCF are displayed in Figure 2, by DUI group and gender. Measurement precision of these criteria was greater in the DUI groups (higher peaks).
Figure 2.
Information curves showing aggregate information from 5 AUD criteria which displayed DCF in IRT analysis (larger/longer, inability/persistent desire to quit, social/interpersonal problems, physical/psychological problems, time spent), by DUI and gender
A total information curve which included all 9 criteria from the final model showed that measurement precision was very similar in all 4 groups. To determine whether the two abuse criteria included in the analysis contributed information beyond that from the dependence items, an item information curve which excluded role failure and social/interpersonal problems was compared to the total information curve. The peaks were uniformly lower in all four groups in the curves which excluded abuse items, indicating that the abuse criteria contributed to identification of AUDs similarly in all groups. For example, the height of the peaks for women with no DUIs before and after excluding the abuse criteria were 5.8 and 4.1, respectively and for women with DUIs were 5.7 and 4.2 (data not shown, available on request). This indicates that the remaining abuse criteria contribute to identification of AUDs, over and above the 7 dependence criteria, and do so similarly across groups.
DISCUSSION
Differences in alcohol criteria functioning by DUI history and gender were examined in the current study using an item response approach. Differential criterion functioning related to DUI status was observed for 3 criteria, social/interpersonal problems, larger/longer, and inability/persistent desire to quit, indicating they were better at discriminating alcohol problem severity in individuals with DUIs than those without. Irrespective of DUI status, women had a higher threshold than men for time spent drinking or recovering and women without DUIs had a higher threshold than similar men for social/interpersonal problems. When considered as a whole, the criteria functioned equally well in all groups, supporting the use of AUD criteria in instruments used to screen individuals with DUIs for alcohol problem severity in judicial settings.
Information on which the AUD criteria were based came from diagnostic interviews in the context of a high risk family study, and thus was not subject to the underreporting of alcohol use and related behaviors noted in DUI samples in court-ordered settings. A study which examined the accuracy of alcohol diagnosis in DUI offenders found a 20.1% rate of alcohol dependence during DUI-related screening; 5 years later this rate was 60.1% based on interviews with the same offenders which queried the same time frame as the previous screening (Lapham et al., 2004). In the current study, 81.3% of DUI offenders met alcohol dependence criteria, consistent with an accurate reporting of symptoms and with high rates of AUD symptoms in other high-risk samples (Hill et al., 2010; Strong et al., 2010).
In parallel with the extant literature, we found evidence for a unidimensional structure underlying AUD criteria in the sample as a whole and in individuals with and without DUIs as well. Unidimensionality in the non-DUI group, which was heterogeneous regarding AUD status in that 40% did not meet criteria for alcohol abuse or dependence, further supports the conceptualization of the criteria as representing a continuum. Not surprisingly, individuals with DUIs scored significantly higher on the underlying alcohol severity factor than those without DUIs, underscoring their high-risk status and consistent with their higher mean number of AUD symptoms.
Three criteria that discriminated at lower levels of alcohol severity, larger/longer, inability/persistent desire to quit, and social/interpersonal problems, showed DCF by DUI status, with higher difficulty parameters in individuals with DUIs than those without. This means that individuals with DUIs were less likely to endorse these criteria, on average, than were individuals without DUIs at the same level of alcohol problem severity. The higher discrimination parameters among individuals with than without DUIs suggests that individuals with DUIs were less likely to endorse these criteria at low levels of alcohol problem severity and more likely to endorse them at higher levels than were individuals with no DUIs. The measurement precision of these criteria was also better in individuals with DUIs, suggesting that they function well in exceptionally high-risk populations. The higher severity threshold required before endorsement by individuals with DUIs may reflect differences in life circumstances, perception, or attitude between the groups. For example, the higher rates of divorce and separation among individuals with DUIs may well be a consequence of excessive alcohol use, however, unless it is perceived as an alcohol-related problem it will not be reported as such. It is possible that individuals with DUIs at lower levels of severity do not recognize or acknowledge social/interpersonal problems as related to alcohol use, but that they acknowledge the association between alcohol use and relational difficulties at higher levels of severity, after an accumulation of negative consequences. Similarly, individuals with DUIs may be less likely to perceive or admit to a need to quit, making them less likely to endorse wanting to quit or being unable to. In fact, a majority of individuals who meet criteria for AUDs do not perceive a need for help (Dawson et al., 2006; Mojtabai et al., 2002; Wu and Ringwalt, 2004). The gender differences observed for social/interpersonal problems and larger/longer among individuals without DUIs were similar to those observed in a population-based sample (Saha et al., 2006), with social/interpersonal problems having a higher threshold and larger/longer having a lower threshold among women. The lack of gender differences in the DUI group suggests that gender differences are minimized in more severely affected samples. This is consistent with a study in a high-risk sample of women and men enrolled in a domestic violence program which found that items in the alcohol dependence scale showed no DCF by gender (Kahler et al., 2003).
Preliminary tests of DCF performed prior to the 4-group model produced evidence that, irrespective of DUI status, women were more likely than men to report drinking larger amounts or for longer periods of time than intended, spending so much time drinking or recovering that there was little time for anything else, and continued drinking despite physical or psychological problems, and less likely than men to report social or interpersonal problems due to drinking. Similar evidence of measurement non-equivalence for drinking despite psychological and physical problems was found in a population-based sample using measures based on the previous 12 months, with females more likely than males at similar levels of alcohol problem severity to endorse it (Harford et al., 2009). This criterion also showed gender heterogeneity with regard to cannabis abuse and dependence criteria in the NESARC (Agrawal and Lynskey, 2007). This consistency across samples and substances warrants examination of drinking despite physical or psychological problems to elucidate reasons for this gender difference which could potentially help improve treatment outcomes for women.
Even after removing the abuse criteria confounded with DUI, hazardous use and legal problems, the two remaining abuse criteria included in the analysis, role failure and social/interpersonal problems, did contribute to the overall measurement of the criteria in all groups. It is possible that hazardous use and legal problems would show greater discrimination and higher thresholds among individuals without DUIs than those with, since they are much less frequently endorsed by individuals without DUIs. Inclusion of these criteria, however, is not warranted in the current analysis due to their redundancy with DUI status. Had they been included, it is unlikely they would alter the overall conclusion of the analysis.
As one would expect, the findings from this high-risk sample are more consistent with similar analyses in clinical samples than in population-based samples. Time spent drinking or recovering and giving up activities were the two most severe criteria in the current study and in a study using data from a multisite treatment sample (Wu et al., 2009), suggesting that these criteria map higher ranges of severity in exceptionally high-risk samples. Giving up activities was also among the more severe criteria in clinical, adjudicated, and community samples of adolescents (Gelhorn et al., 2008). In a population-based study, giving up activities was the most severe criterion and difficulty quitting and larger/longer were least severe (Saha et al., 2006), similar to the current study, but the severity ranking of the other criteria was quite different. In another population-based study, time spent was the least severe criterion among individuals aged 18 and older (Harford et al., 2009); in the current study it was the most severe criterion for men and second most severe for women, perhaps reflecting greater habituation to alcohol use in this high-risk sample. The strict operationalization of time spent as spending “so much time drinking or recovering from the effects of alcohol that you had little time for anything else” in the current study may also contribute to the discrepant findings. The qualifier “little time for anything else” may cause respondents to interpret the question as a more severe drinking-related behavior, resulting in lower endorsement and higher severity. For women, time spent was as severe a criterion as giving up activities to drink. In other studies in high risk (Wu et al., 2009; Gelhorn et al., 2008) and population-based samples (Saha et al., 2006) giving up activities is a more severe criterion than time spent.
Limitations of the study include the use of a family study with a high genetic loading for alcohol dependence, which means that these results may not generalize to other samples that are not high-risk. Heightened risk for social and environmental adversity that often accompany familial risk for alcohol dependence, such as childhood trauma, may not generalize to other samples. Variation in abuse/dependence status in the non-DUI group may have obscured some distinctions that might have become apparent with further stratification by abuse and dependence status. However, because our aim was to examine AUD criteria functioning in individuals with versus those without DUIs, regardless of AUD status and consistent with current findings of a continuum of alcohol problem severity, we elected not to stratify the data further.
The current study has highlighted some areas where alcohol criteria may function differently in the particularly high-risk group of individuals with DUIs, and where examination of differences could yield information useful for the study and treatment of individuals at the more severe end of the alcohol use spectrum. The adequate functioning of the criteria as a whole, however, supports the use of AUD criteria in instruments used to screen individuals with DUIs for alcohol problem severity in judicial settings.
Acknowledgments
Funding for this study was provided by NIH grants AA018146, AA12640, AA11998, DA14363, DA23668, DA25886, K05AA17688, U10AA008401
COGA
The Collaborative Study on the Genetics of Alcoholism (COGA), Principal Investigators B. Porjesz, V. Hesselbrock, H. Edenberg, L. Bierut, includes ten different centers: University of Connecticut (V. Hesselbrock); Indiana University (H.J. Edenberg, J. Nurnberger Jr., T. Foroud); University of Iowa (S. Kuperman, J. Kramer); SUNY Downstate (B. Porjesz); Washington University in St. Louis (L. Bierut, A. Goate, J. Rice, K. Bucholz); University of California at San Diego (M. Schuckit); Rutgers University (J. Tischfield); Southwest Foundation (L. Almasy), Howard University (R. Taylor) and Virginia Commonwealth University (D. Dick). Other COGA collaborators include: L. Bauer (University of Connecticut); D. Koller, S. O’Connor, L. Wetherill, X. Xuei (Indiana University); Grace Chan (University of Iowa); N. Manz, M. Rangaswamy (SUNY Downstate); A. Hinrichs, J. Rohrbaugh, J-C Wang (Washington University in St. Louis); A. Brooks (Rutgers University); and F. Aliev (Virginia Commonwealth University). A. Parsian and M. Reilly are the NIAAA Staff Collaborators. We continue to be inspired by our memories of Henri Begleiter and Theodore Reich, founding PI and Co-PI of COGA, and also owe a debt of gratitude to other past organizers of COGA, including Ting-Kai Li, currently a consultant with COGA, P. Michael Conneally, Raymond Crowe, and Wendy Reich, for their critical contributions. This national collaborative study is supported by NIH Grant U10AA008401 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the National Institute on Drug Abuse (NIDA).
References
- ADE Incorporated. The Substance Abuse/Life Circumstances Evaluation Reference Guide [Online] Clarkston, MI: ADE; 2007. [[Accessed 2/3/2011 2011]]. Available: http://www.adeincorp.com/SALCE_Ref_Guide.pdf. [Google Scholar]
- Agrawal A, Lynskey MT. Does gender contribute to heterogeneity in criteria for cannabis abuse and dependence? Results from the national epidemiological survey on alcohol and related conditions. Drug Alcohol Depend. 2007;88:300–7. doi: 10.1016/j.drugalcdep.2006.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-IV) Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Association, A. P. Diagnostic and statistical manual of mental disorders (DSM-III- R) Washington, DC: American Psychiatric Association; 1987. [Google Scholar]
- Borges G, Ye Y, Bond J, Cherpitel CJ, Cremonte M, Moskalewicz J, Swiatkiewicz G, Rubio-Stipec M. The dimensionality of alcohol use disorders and alcohol consumption in a cross-national perspective. Addiction. 2010;105:240–54. doi: 10.1111/j.1360-0443.2009.02778.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JIJ, Reich T, Schmidt I, Schuckit MA. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. J Stud Alcohol. 1994;55:149–58. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Heath AC, Reich T, Hesselbrock VM, Kramer JR, Nurnberger JIJ, Schuckit MA. Can we subtype alcoholism? A latent class analysis of data from relatives of alcoholics in a multicenter family study of alcoholism. Alcohol Clin Exp Res. 1996;20:1462–71. doi: 10.1111/j.1530-0277.1996.tb01150.x. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Hesselbrock VM, Shayka JJ, Nurnberger JIJ, Schuckit MA, Schmidt I, Reich T. Reliability of individual diagnostic criterion items for psychoactive substance dependence and the impact on diagnosis. J Stud Alcohol. 1995;56:500–5. doi: 10.15288/jsa.1995.56.500. [DOI] [PubMed] [Google Scholar]
- Chang I, Gregory C, Lapham SC. Review of screening instruments and procedures for evaluating DWI (driving while intoxicated/impaired) offenders. Washington, DC: AAA Foundation for Trafiic Safety; 2002. [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Estimating the effect of help-seeking on achieving recovery from alcohol dependence. Addiction. 2006;101:824–34. doi: 10.1111/j.1360-0443.2006.01433.x. [DOI] [PubMed] [Google Scholar]
- Fabrigar LR, Wegener DT, Maccallum RC, Strahan EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychological Methods. 1999;4:272–299. [Google Scholar]
- Federal Bureau of Investigation. [Accessed February 4 2011];Uniform Crime Reports, Ten-Year Arrest Trends by Sex, 2000–2009. Available: http://www2.fbi.gov/ucr/cius2009/data/table_33.html.
- Feighner JP, Robins E, Guze SB, Woodruff RA, Wimokur G, Munoz R. Diagnostic criteria for use in psychiatric research. Archives of General Psychiatry. 1972;26:57–63. doi: 10.1001/archpsyc.1972.01750190059011. [DOI] [PubMed] [Google Scholar]
- Flam L. [Accessed Feb. 5, 2010];Women drinking more, DUI arrests up, experts say. 2009 [Online]. Available: http://www.dallasnews.com/sharedcontent/dws/news/nation/stories/DN-womendrinkers_07nat.ART.State.Edition1.3c7e443.html (Archived by WebCiteR at http://www.webcitation.org/5nJvliGcP)
- Foroud T, Edenberg HJ, Goate A, Rice J, Flury L, Koller DL, Bierut LJ, Conneally PM, Nurnberger JI, Bucholz KK, Li TK, Hesselbrock V, Crowe R, Schuckit M, Porjesz B, Begleiter H, Reich T. Alcoholism susceptibility loci: confirmation studies in a replicate sample and further mapping. Alcoholism-Clinical and Experimental Research. 2000;24:933–45. [PubMed] [Google Scholar]
- Gelhorn H, Hartman C, Sakai J, Stallings M, Young S, Rhee SH, Corley R, Hewitt J, Hopfer C, Crowley T. Toward DSM-V: an item response theory analysis of the diagnostic process for DSM-IV alcohol abuse and dependence in adolescents. J Am Acad Child Adolesc Psychiatry. 2008;47:1329–39. doi: 10.1097/CHI.0b013e318184ff2e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harford TC, Yi HY, Faden VB, Chen CM. The dimensionality of DSM-IV alcohol use disorders among adolescent and adult drinkers and symptom patterns by age, gender, and race/ethnicity. Alcohol Clin Exp Res. 2009;33:868–78. doi: 10.1111/j.1530-0277.2009.00910.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesselbrock M, Easton C, Bucholz KK, Schuckit M, Hesselbrock V. A validity study of the SSAGA--a comparison with the SCAN. Addiction. 1999;94:1361–70. doi: 10.1046/j.1360-0443.1999.94913618.x. [DOI] [PubMed] [Google Scholar]
- Hill SY, Tessner KD, Mcdermott MD. Psychopathology in offspring from families of alcohol dependent female probands: A prospective study. J Psychiatr Res. 2010 doi: 10.1016/j.jpsychires.2010.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Strong DR. A Rasch model analysis of DSM-IV alcohol abuse and dependence items in the National Epidemiological Survey on Alcohol and Related Conditions. Alcoholism-Clinical and Experimental Research. 2006;30:1165–1175. doi: 10.1111/j.1530-0277.2006.00140.x. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, Stuart GL, Moore TM, Ramsey SE. Item functioning of the alcohol dependence scale in a high-risk sample. Drug Alcohol Depend. 2003;72:183–92. doi: 10.1016/s0376-8716(03)00199-6. [DOI] [PubMed] [Google Scholar]
- Kincannon J. Minnesota Assessment of Chemical Health (MACH) Chaska, MN: International Professional Services, Inc; 1984. [Google Scholar]
- Lapham SC, C’de Baca J, Mcmillan G, Hunt WC. Accuracy of alcohol diagnosis among DWI offenders referred for screening. Drug Alcohol Depend. 2004;76:135–41. doi: 10.1016/j.drugalcdep.2004.04.020. [DOI] [PubMed] [Google Scholar]
- Lapham SC, C’de Baca J, Mcmillan GP, Lapidus J. Psychiatric disorders in a sample of repeat impaired-driving offenders. J Stud Alcohol. 2006;67:707–13. doi: 10.15288/jsa.2006.67.707. [DOI] [PubMed] [Google Scholar]
- Lapham SC, Skipper BJ. Does screening classification predict long-term outcomes of DWI offenders? Am J Health Behav. 2010;34:737–49. doi: 10.5993/ajhb.34.6.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapham SC, Skipper BJ, Owen JP, Kleyboecker K, Teaf D, Thompson B, Simpson G. Alcohol abuse screening instruments: normative test data collected from a first DWI offender screening program. Journal of Studies on Alcohol. 1995;56:51–9. doi: 10.15288/jsa.1995.56.51. [DOI] [PubMed] [Google Scholar]
- Lapham SC, Smith E, C’de Baca J, Chang I, Skipper BJ, Baum G, Hunt WC. Prevalence of psychiatric disorders among persons convicted of driving while impaired. Arch Gen Psychiatry. 2001;58:943–9. doi: 10.1001/archpsyc.58.10.943. [DOI] [PubMed] [Google Scholar]
- Laplante DA, Nelson SE, Odegaard SS, Labrie RA, Shaffer HJ. Substance and psychiatric disorders among men and women repeat driving under the influence offenders who accept a treatment-sentencing option. J Stud Alcohol Drugs. 2008;69:209–17. doi: 10.15288/jsad.2008.69.209. [DOI] [PubMed] [Google Scholar]
- Lundstrom M. [Accessed: 2010-02-05]; [Accessed Feb. 5, 2010];Female DUI arrests soar in state, capital area. 2009 [Online]. Available: http://www.sacbee.com/ourregion/story/2019267-p3.html. (Archived by WebCiteR at http://www.webcitation.org/5nJy7ue5H)
- McCutcheon VV, Heath AC, Edenberg HJ, Grucza RA, Hesselbrock VM, Kramer JR, Bierut LJ, Bucholz KK. Alcohol criteria endorsement and psychiatric and drug use disorders among DUI offenders: greater severity among women and multiple offenders. Addict Behav. 2009;34:432–9. doi: 10.1016/j.addbeh.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellenbergh GJ. Generalized Linear Item Response Theory. Psychological Bulletin. 1994;115:300–307. [Google Scholar]
- Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Arch Gen Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- Muthén B, Lehman J. Multiple Group IRT Modeling: Applications to Item Bias Analysis. Journal of Educational Statistics. 1985;10:133–142. [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. 5. Los Angeles, CA: Muthen & Muthen; 1998–2007. [Google Scholar]
- Nichol PE, Krueger RF, Iacono WG. Investigating gender differences in alcohol problems: a latent trait modeling approach. Alcohol Clin Exp Res. 2007;31:783–94. doi: 10.1111/j.1530-0277.2007.00375.x. [DOI] [PubMed] [Google Scholar]
- Programs), A. I. a. a. C. M. S. F. S. A. The Substance Abuse/Life Circumstances Evaluation Reference Guide [Online] Clarkston, MI: ADE; 2007. [Accessed 2/3/2011 2011]. Available: http://www.adeincorp.com/SALCE_Ref_Guide.pdf. [Google Scholar]
- Reich T, Edenberg HJ, Goate A, Williams JT, Rice JP, Van Eerdewegh P, Foroud T, Hesselbrock V, Schuckit MA, Bucholz K, Porjesz B, Li TK, Conneally PM, Nurnberger JI, Tischfield JA, Crowe RR, Cloninger CR, Wu W, Shears S, Carr K, Crose C, Willig C, Begleiter H. Genome-wide search for genes affecting the risk for alcohol dependence. American Journal of Medical Genetics. 1998;81:207–215. [PubMed] [Google Scholar]
- Saha TD, Chou SP, Grant BF. Toward an alcohol use disorder continuum using item response theory: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2006;36:931–41. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- Saha TD, Stinson FS, Grant BF. The role of alcohol consumption in future classifications of alcohol use disorders. Drug Alcohol Depend. 2007;89:82–92. doi: 10.1016/j.drugalcdep.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA, Daeppen JB, Tipp JE, Hesselbrock M, Bucholz KK. The clinical course of alcohol-related problems in alcohol dependent and nonalcohol dependent drinking women and men. J Stud Alcohol. 1998;59:581–90. doi: 10.15288/jsa.1998.59.581. [DOI] [PubMed] [Google Scholar]
- Shaffer HJ, Nelson SE, Laplante DA, Labrie RA, Albanese M, Caro G. The epidemiology of psychiatric disorders among repeat DUI offenders accepting a treatment-sentencing option. J Consult Clin Psychol. 2007;75:795–804. doi: 10.1037/0022-006X.75.5.795. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 11.0. College Station, TX: StataCorp; 2009. [Google Scholar]
- Steinberg L, Thissen D. Using effect sizes for research reporting: Examples using item response theory to analyze differential item functioning. Psychological Methods. 2006;11:402–415. doi: 10.1037/1082-989X.11.4.402. [DOI] [PubMed] [Google Scholar]
- Strong DR, Caviness C, Anderson B, Brown RA, Stein M. Assessing the Severity of Hazardous Drinking and Related Consequences Among Incarcerated Women. Alcoholism: Clinical and Experimental Research. 2010;34:907–914. doi: 10.1111/j.1530-0277.2010.01163.x. [DOI] [PubMed] [Google Scholar]
- Tellier S. [Accessed: 2010-02-05]; [[Accessed Feb. 5, 2010].];Women make up larger percentage of DUI arrests. 2009 [Online]. Available: http://www.wlky.com/news/21398202/detail.html. (Archived by WebCiteR at http://www.webcitation.org/5nJxWFk4O)
- U.S. Department of Transpotation, National Highway Traffic Safety Administration. [Accessed February 4, 2011];Traffic Safety Facts 2009. 2009 Available: http://www-nrd.nhtsa.dot.gov/Pubs/811402EE.pdf.
- Wu LT, Pan JJ, Blazer DG, Tai B, Stitzer ML, Brooner RK, Woody GE, Patkar AA, Blaine JD. An item response theory modeling of alcohol and marijuana dependences: a National Drug Abuse Treatment Clinical Trials Network study. J Stud Alcohol Drugs. 2009;70:414–25. doi: 10.15288/jsad.2009.70.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Ringwalt CL. Alcohol dependence and use of treatment services among women in the community. Am J Psychiatry. 2004;161:1790–7. doi: 10.1176/appi.ajp.161.10.1790. [DOI] [PMC free article] [PubMed] [Google Scholar]