Abstract
Objective
The aims of this paper are as follows: to present past-year prevalence data for DSM-IV disorders in the early elementary school years; to examine the impact of impairment criteria on prevalence estimates; to examine the relation of sociodemographic and psychosocial risk factors to disorders; and to explore associations between ”internalizing” and ”externalizing” disorders and social competence and family burden as further validation of the impairing nature of these disorders.
Method
As part of a longitudinal representative population study of children born healthy between July 1995 and September 1997 in the New Haven–Meriden Standard Metropolitan Statistical Area of the 1990 Census (n = 1,329), parents of a subsample enriched for child psychopathology (n = 442; 77.6% response rate, 69.5% of eligible sample) were interviewed in the child's kindergarten or first-grade year with the Diagnostic Interview Schedule for Children, Version IV (DISC-IV). Parents were surveyed about sociodemographic and psychosocial characteristics, and both parents and teachers were surveyed about social competence.
Results
Approximately one in five (21.6 %) children met criteria for psychiatric disorder(s) with impairment. Sociodemographic and psychosocial correlates included persistent poverty beginning in early childhood, limited parental education, low family expressiveness, stressful life events, and violence exposure. Finally, diagnostic status was significantly associated with poorer social competence and family burden.
Conclusions
That approximately one in five children evidenced a psychiatric disorder with impairment during the transition to formal schooling highlights the importance of integrating psychiatric epidemiological and developmental approaches to inform conversations about school readiness and intervention planning.
Keywords: child psychiatric disorders, prevalence, social competence, family burden, impairment
The transition to formal schooling has been a period of intense focus for developmental investigation; this period is marked by dramatic changes in contextual demands that, together with child cognitive and social capacities, may increase vulnerability to maladjustment.1-3 Multiple studies have documented that children's social competence and behavior problems in kindergarten and first grade are strong predic tors of later social and academic functioning.4-6 Despite intensive study in developmental psychology, to our knowledge, no epidemiological studies have focused on the prevalence of psychopathology during this developmental period. Although categorical diagnostic approaches to psychopathology have limitations,7,8 diagnosis continues to serve as a gateway to mental health services.9 Knowledge of rates in this transitional period can inform identification and intervention efforts.
It is challenging to conduct epidemiological studies of child health in the United States. Numerous barriers to accessing family contact information for population-based samples exist, including the absence of accessible integrated medical records, use of parochial and other private schools, laws protecting health and other personal information, and high household mobility. The majority of studies addressing the prevalence of children's mental health in the United States have ascertained samples through pediatric offices or public school records. For example, the Smokey Mountain Study10 and Caring for Children in the Community Study11 have been successful in ascertaining representative samples through public school records in districts with 99% public school participation. Nationally, however, the percentage of children in parochial and other private schools is approximately 10%, and, among other socio-demographic differences, private school students are less likely to be living in or near poverty than those attending public school. Studies that rely on pediatric samples may represent high users of pediatric services.12,13 Some pediatric studies focused on prevalence of psychopathology have not obtained epidemiologically based samples.14
In contrast, the current sample was ascertained through birth records. As all births are registered, this approach has strong potential for obtaining geographically-representative samples of young children. Birth records also contain key demographic and birth status information, allowing identification of systematic biases in the obtained sample. A high initial response rate in early childhood and strong retention through the transition to schooling result in a unique opportunity to examine psychopathology prevalence.
Irrespective of method of ascertainment, rates of psychopathology ranging from 9.5%15 to 26.4%16 have been reported in clinical and epidemiological prevalence studies of preschoolers and older children.12-14,17-20 The handful using DSM-IV criteria have confirmed earlier rates, with the most comprehensive DSM-IV-TR study showing a total rate of 9.5% overall and of 7.79% among 5- to 7-year-olds in a British sample.15 Only a small number of epidemiological studies have included school-aged children under 9 years of age.13,15,17 Although largely comparable, analyzing prevalence rates within narrow age bands can reveal meaningful differences across development. For example, Costello et al. reported a 19.5% prevalence rate of any diagnosis for 9- to 10-year-olds, but a significantly lower rate of 8.3% in 11- to 12-year-olds.
A major shift in DSM-IV from DSM-III was the requirement of impairment in functioning in the social, academic, and/or employment domain for psychiatric diagnosis.17 Originally introduced in response to implausibly high rates of psychiatric disorder in community samples, impairment criteria were added to DSM-IV to incorporate service need into diagnosis.21 DSM-IV studies of childhood confirm that including impairment dramatically lowers prevalence rates.15,17,19 For example, among 4- to 17-year-olds in Puerto Rico, estimates dropped from 20% to 16.4% when disorder-specific impairment was required and to 6.9% when both disorder-specific and global impairment were required; however no breakdown of prevalence rates for younger children were reported.17 In young children, impairment criteria may, for example, help to distinguish normative misbehavior from non-normative, clinically significant oppositional behavior.19 How-ever, the DSM-IV does not offer developmental guidance in how these criteria should be used, and there is no clear consensus regarding developmental expectations for impaired school and social functioning among young children.22
Across the lifespan, comorbidity, or the cooccurrence of multiple disorders, is generally regarded to be the rule rather than the exception for individuals with psychiatric diagnoses.23 Moreover, the belief that comorbidity reflects lack of differentiation of psychiatric symptoms in young children has been dispelled.24 Historically, children's disorders have been grouped into two domains: internalizing, which includes anxiety and depressive disorders and symptoms; and externalizing, which includes disruptive behavior and attention/hyperactivity disorders and symptoms.7 Comorbidity prevalence has been addressed in several ways, counting as comorbid children with the following: more than one psychiatric disorder, irrespective of type; more than one disorder within a specific domain, or “homotypic comorbidity;” and disorders across the internalizing/externalizing boundary, or “heterotypic comorbidity.”23 Children with comorbid psychiatric disorders are more likely to persist and to be more impaired;23 therefore, estimating comorbidity rates during the transition to school can inform service need.
A large body of developmental research highlights the importance of social competence in successfully negotiating the transition to formal schooling.25-27 Poorer social competence may reflect current impairment in social functioning, as well as increased risk for persistent psychopathology and school failure. Social competence has been linked with dimensional problem behaviors, such as aggression and withdrawal28 and symptoms of attention-deficit disorder.29 Social competence may also be protective.30 Assessing psychopathology prevalence and social competence during the transition to elementary school provides an opportunity to address policy concerns regarding school readiness and to link psychiatric and developmental epistemologies.
An important role of epidemiological studies is to examine contextual factors that may influence rates of disorder, including sociodemographic factors such as child sex, minority status, poverty, and exposure to violence.31 Sociodemographic and structural characteristics of families (e.g., parent education, single-parent status), parental mental health (e.g., parental depression), stressful life events, and family dysfunction have been linked to increased rates of psychiatric disorders across childhood and adolescence.32
This report focuses on a longitudinal healthy birth cohort of children who had recently made the transition to formal schooling. The primary aims of this study were as follows: to document rates of psychiatric disorder assessed with and without impairment criteria; to explore associations between internalizing and externalizing disorders and social competence and family burden; and to identify sociodemographic and psychosocial correlates of internalizing and externalizing disorders.
METHOD
Participants
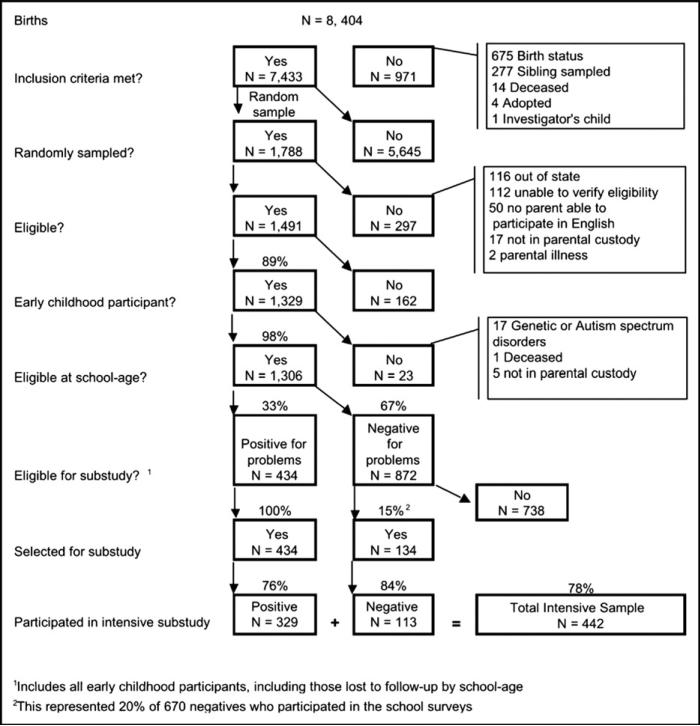
Children were selected from birth records (N = 8,404) provided by the State of Connecticut Department of Public Health for births at Yale-New Haven Hospital from July 1995 to September 1997 (Figure 1). Eligible children were born healthy in the New Haven–Meriden Standard Metropolitan Statistical Area of the 1990 Census. Children who were likely to have developmental delays because of low birthweight (<2,200 g), prematurity (<36 weeks), low APGAR scores (defined as both 1- and 5-minute scores <5), or birth complications (e.g., resuscitation need, anoxia, long hospital stay) were excluded; only one child per family was sampled. Of the 7,433 births meeting these criteria, a random sample of 1,788 was selected, stratified to have equal representation of girls and boys within 3-month age groupings between 11 and 35 months of age. Children were excluded after the initial sampling if any of the following exclusion criteria were met: no parent could participate in English; no biological parent had custody of the child; the family had moved out of Connecticut at the time of the first survey (1998–1999); or eligibility could not be verified. After exclusions, 1,491 subjects were eligible, of whom 1,329 participated in one or more of three early childhood surveys (89.1% response rate). As shown in Table 1, this early childhood sample was similar to the original pool of births (N = 7,433) with respect to sociodemographic characteristics and birth status variables. Although not shown in Table 1, the early childhood sample was also similar to census data for families with young children in the SMSA with respect to single parent status (20.2% versus 18.5%) and race/ethnicity (73.9% versus 76.7% white; 22.1% versus 17.2% African American/black; and 8.2% versus 9.5% Hispanic).
FIGURE 1.
Flowchart of intensive sample recruitment and retention.
TABLE 1.
Intensive sample participants versus original birth cohort and early childhood sample
| Eligible Birth Record Sample (N = 7,433) | Early Childhood Participants (N = 1,329) | Intensive Subsample (N = 442) |
||
|---|---|---|---|---|
| Unweighted Mean (SD) | Unweighted Mean (SD) | Unweighted Mean (SD) | Weighted Mean (SD) | |
| Birthweight (grams) | 3,417.2 (485.1) | 3,425.4 (483.2) | 3,415.8 (494.5) | 3,406.3 (477.4) |
| Paternal age (years) | 31.8 (6.6) | 32.1 (6.5) | 31.9 (6.6) | 32.1 (6.2) |
| Maternal age (years) | 28.8 (6.2) | 29.4 (6.2) | 29.6 (6.4) | 29.7 (6.1) |
| Paternal education (years) | 14.0 (2.5) | 14.1 (2.3) | 14.0 (2.3) | 14.0 (2.6) |
| Maternal education (years) | 13.8 (2.5) | 14.1 (2.4) | 13.9 (2.5) | 14.0 (2.7) |
| Gestational age (days) | 275.4 (9.6) | 275.3 (9.6) | 275.0 (9.8) | 274.7 (9.9) |
| Length of time at address (years) | 3.5 (4.1) | 3.6 (3.9) | 3.6 (4.0) | 3.6 (3.7) |
| % | % | % | % | |
|---|---|---|---|---|
| Boys | 51.6 | 49.1 | 53.4 | 49.5 |
| Girls | 48.4 | 50.9 | 46.6 | 50.5 |
| Caucasian | 72.3 | 73.9 | 74.3 | 74.4 |
| African American | 22.6 | 22.1 | 23.1 | 23.7 |
| Other | 5.0 | 4.0 | 2.6 | 1.9 |
| Hispanic | 11.5 | 8.2 | 7.3 | 4.4 |
| Non-Hispanic | 88.5 | 91.8 | 92.7 | 95.6 |
| Single parent household | – | 20.2 | 22.2 | 18.3 |
| Living in poverty | – | 18.9 | 20.0 | 14.6 |
Before mailing or based on information in the first Early Elementary School survey, 23 children were excluded due to genetic or developmental disorders, death, or loss of parental custody. Parent (n = 1,058) and/or teacher (n = 751) surveys were obtained for 1,078 participants, corresponding to retention of 82.5% of the 1,306 eligible participants from the Early Childhood survey and 73.4% of the eligible original sample (N = 1,468). This sample was comparable to the original sample in terms of child sex, poverty status, single-parent household status, and paternal education (continuity adjusted χ2 ranged from 0.07 to 1.37; NS). There were trend-level differences (p < .10), with small effect sizes (phi ≤0.04), indicating loss of minority children and mothers with a high school education or less.
The focus of this report is on an early elementary school intensive assessment subsample, enriched for psychopathology (n = 567), which was selected for more in-depth diagnostic interviewing and direct child assessment. All children who met any of the following criteria were selected: persistent social–emotional/behavioral problems in early childhood, defined as parent report at 2 and 3 years of age of problems in the subclinical/clinical range on reliable and validated checklist measures appropriate for this age range (Infant–Toddler Social and Emotional Assessment [ITSEA]33 and Child Behavior Checklist/1.5-5 [CBCL/1.5-5])34; social–emotional/behavioral problems in kindergarten or first grade, according to parent and/or teacher report of problems in the subclinical/clinical range (T-score ≥60) on reliable and validated checklists (CBCL and Teacher Report Form [TRF]),34 or parent or teacher report of need for services at school age; and risk for language/learning difficulties, according to parent report of low receptive and expressive language ability at 3 years of age (Child Development Inventory [CDI]),35 defined on the basis of one of the following: as scores <6th percentile; parent or teacher report of low language ability in kindergarten (CDI),35 defined as failing to pass 80% of the items typically passed by 3½-year-old children); parent report of a language delay diagnosis in early childhood; parent report of concern about the child's language abilities in kindergarten (rating of 4 or 5 on a scale from 1 = not at all worried to 5 = extremely worried); or teacher report of that the child had “probable” or “definite” receptive or expressive language problems. Language difficulties were included in these selection criteria because early language delays have been linked to problem behaviors.36,37
Following these selection criteria, 434 children were deemed eligible for the intensive subsample (252 social–emotional problems only, 83 language problems only, and 98 problems in both areas). One child was subsequently deemed ineligible because s/he was not in parental custody. A random sample of 20% of the 670 children whose parents or teachers participated in the Early Elementary School assessment and did not meet any of these inclusion criteria also was selected (n = 134). Of the 567 selected, 541 participated in the Early Elementary School survey and were invited into the intensive study and 442 participated (78% of the eligible). Intensive subsample participants and non-participants did not differ on the sample selection criteria (Rao-Scott χ2 = 1.4369, NS).
Participants in the intensive subsample were diverse with respect to parental education (29.3% of mothers and 29.1% of fathers had education of high school or less), poverty status, ethnicity, and marital status, as well as risks in the areas of parental symptoms, life stress, and family functioning (Tables 1 and 2). Given the time involved in tracking parents and teachers, most assessments occurred when children were in first grade; mean child age was 6.6 years (SD = 0.4). Of the children, 84% were enrolled in public schools, 15% private schools, and 0.9% home-schooled.
TABLE 2.
Rates of Risk Factors and Association with Presence of Any Diagnostic Interview Schedule for Children (DISC) Disorder
| Full Sample (N = 441) % | No Disorder (N = 330) % | Any Disorder (N = 91) % | χ 2 | |
|---|---|---|---|---|
| Sociodemographic factors | ||||
| Child sex (1 = male) | 49.6 | 48.7 | 54.0 | 0.51 |
| Minority ethnicity | 32.9 | 32.7 | 35.1 | 0.12 |
| Kindergarten poverty | 15.0 | 13.2 | 23.2 | 4.46* |
| Early poverty (any) | 18.9 | 15.6 | 33.3 | 10.48** |
| Teenage mother | 3.0 | 2.8 | 4.5 | 0.37 |
| Paternal or maternal education less than high school | 9.3 | 8.7 | 12.3 | 0.88 |
| Single parent home | 18.5 | 16.9 | 26.8 | 3.43† |
| No parent working | 5.5 | 5.7 | 5.3 | 0.02 |
| Birth status variables | ||||
| Birth weight <2,850 g | 10.5 | 9.9 | 9.6 | 0.00 |
| Low 1-minute APGAR score | 1.6 | 1.4 | 2.4 | 0.28 |
| Psychosocial variables | ||||
| Parental anxiety | 5.0 | 3.4 | 11.3 | 7.11** |
| Parental depression | 16.3 | 13.0 | 30.0 | 11.28*** |
| Child life events | 5.6 | 4.5 | 10.1 | 3.86* |
| Parent life events | 11.4 | 11.2 | 12.7 | 0.11 |
| Low social support | 11.8 | 10.9 | 16.3 | 1.64 |
| Violence exposure past year | 6.4 | 4.0 | 15.6 | 14.33"*** |
| FES conflict | 8.3 | 7.2 | 12.1 | 2.13 |
| FES expressiveness | 5.7 | 5.4 | 7.9 | 0.77 |
Note: APGAR scores are derived from observations of infant health at one and five minutes after birth; lower scores reflect health concerns. FES = Family Environment Scale.
p < .05
p < .01
p < .001
p < .10.
Procedure
Subsequent to the initial survey of parents of children 12 to 36 months old in 1998, two annual surveys preceded the Early Elementary School survey. Beginning in 2000/2001 through 2003/2004, families were contacted by mail and phone to identify children who had entered kindergarten. To ensure that teachers had sufficient time to get to know children, surveys were mailed in late winter/early spring of each kindergarten year.
For each survey, eligible parents were invited to participate by mail. Telephone and in-person visits were used to encourage participation. In the Early Elementary School wave, parents were asked for signed permission to invite their child's teacher to complete survey questions. With parental permission, teachers were contacted through the mail with telephone follow-up. Parents received $25 for participating in each of the Early Childhood surveys and $30 for the Early Elementary School survey. Teachers received $25 for participating. Informed consent procedures, approved by two university institutional human subjects review boards, were used. Intensive subsample visits were conducted in project offices or the family home, depending upon family preference. Parents received $100 for participating in the intensive visit.
Measures
One parent per family was interviewed with the Diagnostic Interview Schedule for Children, Version IV (National Institute of Mental Health [NIMH] DISC-IV)38 structured interview. At the end of each diagnos tic section, six question pairs are asked to assess impairment with respect to time involvement and problem intensity across three settings (home, school, other). Diagnostic status is determined using a set of computerized symptom algorithms that either require or do not require impairment criteria. Impairment is defined as present if interference in functioning occurred “some of the time” or “a lot of the time” or caused “bad” or “very bad” problems or feelings in at least one context. To reduce burden on parents, longer diagnostic modules were administered only if the child screened positive for the disorder on the DISC Predictive Scales (DPS) Screener. The DPS screener consists of a series of symptom questions for each diagnostic area and gathers data on symptom presence but not duration, onset, or frequency. An extremely low threshold for screening positive for a disorder is used, requiring only one symptom be reported to maximize sensitivity to disorder.
The Family Life Impairment Scale (FLIS)39 assesses the extent to which parents report that child behavior limits participation in activities typical of families with young children. Items are rated on a three-point scale from “not true” to “very true” and begin with “Because of my child's behavior, personality or special needs, we rarely. . ..” The FLIS has acceptable internal consistency (Cronbach's alpha = 0.81), with item loadings ranging from 0.33 to 0.62.
Children's social competence was measured by parent and teacher ratings on the Adaptive Social Behavior Ratings (ASBR), a research questionnaire comprising items drawn from the Behavior Assessment Scale for Children,40 Child Behavior Scale,41 ITSEA,33 and Teacher Social Competence Rating Scale.34 Items were rated on a four point frequency scale (1 = never, 2 = sometimes; 3 = often, 4 = always). The ASBR Global Score, used in analyses, comprises four first-order constructs: Social Problem-Solving, the use of constructive, prosocial strategies to resolve conflict; Flexibility, the ability to shift behavior in response to social demands; Affiliation, a child's active interest and engagement in social interactions with others; and Consideration, the tendency to take the needs and feelings of others into account. Structural equation models indicated acceptable model fit for a second order global ASBR factor for both parent and teacher models (parent model loadings from 0.57 to 0.87, teacher model loadings from .68-.92). The ASBR Global Score correlated significantly (r = 0.42) with the Vineland Screener Socialization Domain, supporting its validity.
The Vineland Screener42 is a semi-structured parent interview that was developed to gather a quick, reliable and valid assessment of personal and social sufficiency. The 15-item Socialization Domain, used to assess children's adaptive and social skills, has acceptable reliability with the Vineland Survey form (>0.90).
Measures of Risk
Birth Status Variables
Child birth status variables, including low birth weight (<2,850 g), gestational age, and 1-minute APGAR scores (≤5), were collected from birth record data.
Sociodemographic Measures
Poverty was calculated based on federal poverty guidelines: pre-tax annual household income and the number of adults and children in the home or, when income information was not reported, receipt of income-based public assistance. Families with incomes below 100% of the federal poverty line were classified as poor. Early poverty was defined as poor at one or more time points in early childhood (age 1 to 4 years). Child ethnicity was based on birth records and parent surveys. Parents reported maternal education and marital status in surveys.
Parents completed the Beck Anxiety Inventory (BAI),43 a self-report measure that consists of statements describing common symptoms of anxiety, rated on a four-point scale (“not at all” to “severely bothered”), with adequate psychometric properties.
Parents completed the Center for Epidemiologic Studies Depression Inventory (CES-D),44 a 20-item self-report scale that assesses depressive symptoms in adults with high internal consistency (coefficient alpha from 0.84 to 0.90) and modest test–retest reliability for 2- to 4-week intervals.
Parents completed the Expressiveness and Conflict subscales of the Family Environment Scale (FES),45 comprising 18 items. These scales have demonstrated adequate reliability and validity.
Parents rated their child's experience in the last year on the Child Life Events and Violence Exposure46 scales, developed for this study, using check-boxes for events that may be stressful for young children: accidents, injuries, prolonged separation from parent, parental divorce or separation, death of a loved one, serious illness, or hospitalization. Examples of violence items include: “seen someone hit, push or kick a family member” and “seen someone use a weapon to threaten or hurt a family member.” Test–retest reliability (κ = 0.78 over 2 to 4 weeks) and mother–father agreement (κ = 0.40) are adequate.47 Parent-reported exposures were associated with child behavior problems and trauma-related symptoms in early childhood. Two dichotomous variables were derived: Child Life Events, coded as positive if any nonviolent life event was endorsed; and Violence Exposure, coded as positive if any violence exposure was endorsed.
Parents completed the Life Events Inventory (LEI)48 derived from the Schedule of Recent Life Experiences.49 The version used includes the 40 LEI items that have the highest severity weights and greatest applicability to parents of young children.
Parents completed the 24-item Medical Outcomes Study Survey Social Support (MOS),50 which assesses tangible (or concrete, material assistance) and emotional/informational support (or coping assistance). The MOS has adequate psychometric properties, including modest 1-year stability.
Analytic Approach
Analyses were conducted in SAS version 9.1 and SPSS version 14. Prevalence estimates were examined using two diagnostic algorithms (i.e., with and without disorder-specific impairment) for boys and girls using robust variance estimates. Weights were applied in all analyses to adjust for unequal probabilities of selection and retention through the study period to represent rates of disorder in the target population (N = 7,433). These weights adjusted for the probability of selection as a result of oversampling high-risk children for the intensive subsample, and adjusted for differential non-response and attrition on the basis of background characteristics such as gestational age, birth weight, mother's and father's age, and mother's education, available from birth records. Our two-stage sampling approach resulted in a reduction in statistical precision (i.e., increase in sampling variance), as evidenced by a design effect (DEFF) of 1.95, using the Kish approximation. Thus, standard errors are twice as large as would be expected, had a simple random sample of the same size been used.
Bivariate statistics (e.g., Rao-Scott χ2, continuity adjusted χ2, and Fisher's exact test) were calculated to identify sociodemographic and psychosocial factors associated with the presence of disorder with impairment. The bivariate association of risk factors with the following group membership was examined: no disorder, internalizing only, and externalizing only. Given our interest in determining specificity in risk factors for internalizing versus externalizing disorders, children with heterotypic comorbidity (i.e., co-occurring internalizing and externalizing disorders) (n = 15) were excluded from risk analyses;32 this group is not analyzed independently because of limited power. Finally, multivariate analysis of covariance (MANCOVA) was conducted to test whether there were significant differences across the three diagnostic groups (No Disorder, Internalizing Only, and Externalizing Only) in social competence reported by parents and teachers on the ASBR and by parents on the Vineland Socialization Domain and FLIS. Child age and sex were included as covariates in the MANCOVA models. Effect sizes for MANCOVA effects are reported as partial eta squared values, which are interpreted as “small” at 0.01 to 0.05, “medium” at 0.06 to 0.13, and “large” at or above the 0.14 level.51
RESULTS
Prevalence of DISC Disorders
Rates of DISC disorder varied depending on whether impairment criteria were employed (Table 3). When impairment was not required for diagnosis, 32.0% of children met criteria for “any” disorder, 14.3% had one or more externalizing disorders, and 22.5% had one or more internalizing disorders. Without requiring impairment, the most common disorder was Specific Phobia (20.0%), and the majority of children who met criteria for this disorder (69.7%) did not have any other disorder. When impairment was required, 21.6% met criteria for any disorder, 13.8% met criteria for an externalizing disorder, and 11.1% met criteria for an internalizing disorder. In addition, 9% met criteria for Specific Phobia (64.7% of these children did not meet criteria for any other disorder with impairment). All subsequent analyses use diagnostic criteria with impairment required.
TABLE 3.
Prevalence Estimates for Diagnostic Interview Schedule for Children (DISC) Disorders According to Level of Impairment Required for Diagnosis
| Impairment Not Required |
Impairment Required |
|||||||
|---|---|---|---|---|---|---|---|---|
| Unweighted |
Weighted |
Weighted |
||||||
| N | % | Total % (SE) | Boys % (SE) | Girls % (SE) | Total % (SE) | Boys % (SE) | Girls % (SE) | |
| Any disorder | 169 | 39.9 | 32.0 (2.9) | 34.8 (3.8) | 29.3 (9.2) | 21.6 (2.5) | 23.4 (3.1) | 19.8 (3.8) |
| Any externalizing | 84 | 19.8 | 14.3 (2.1) | 18.2 (2.8) | 10.6 (3.1) | 13.8 (2.1) | 17.4 (2.7) | 10.4 (3.1) |
| Any internalizing | 110 | 26.4 | 22.5 (2.6) | 20.8 (3.2) | 24.1 (4.0) | 11.1 (1.9) | 7.9 (1.9) | 14.3 (3.3) |
| Two or more disorders | 50 | 11.8 | 8.6 (1.6) | 8.8 (1.7) | 8.3 (2.7) | 5.8 (1.4) | 5.3 (1.3) | 6.3 (2.5) |
| Individual disorders | ||||||||
| ADHD | 59 | 13.8 | 9.2 (1.6) | 12.0 (2.2) | 6.5 (2.4) | 8.7 (1.6) | 11.1 (2.1) | 6.3 (2.4) |
| Oppositional Defiant | 39 | 9.2 | 8.4 (1.8) | 8.6 (2.1) | 8.1 (3.0) | 8.4 (1.8) | 8.6 (2.1) | 8.1 (3.0) |
| Conduct disorder | 9 | 2.1 | 1.2 (0.5) | 2.1 (0.9) | 0.3 (0.2) | 1.2 (0.5) | 2.1 (0.9) | 0.3 (0.2) |
| Separation anxiety | 18 | 4.2 | 3.8 (1.2) | 3.2 (1.2) | 4.4 (2.0) | 2.2 (0.9) | 1.5 (0.7) | 2.8 (1.7) |
| Social phobia | 3 | 0.7 | 0.3 (0.2) | 0.4 (0.3) | 0.1 (0.1) | 0.3 (0.2) | 0.4 (0.3) | 0.1 (0.1) |
| Specific phobia | 100 | 23.6 | 20.0 (2.4) | 18.9 (3.1) | 21.1 (3.7) | 9.0 (1.7) | 7.4 (1.9) | 10.6 (2.8) |
| Agoraphobia | 2 | 0.5 | 0.3 (0.2) | 0.2 (0.2) | 0.3 (0.3) | 0.1 (0.1) | 0.2 (0.2) | 0.0 (0.0) |
| General anxiety | 3 | 0.7 | 0.3 (0.2) | 0.7 (0.4) | 0.0 (0.0) | 0.2 (0.1) | 0.4 (0.3) | 0.0 (0.0) |
| OCD | 1 | 0.2 | 0.2 (0.2) | 0.0 (0.0) | 0.3 (0.3) | 0.2 (0.2) | 0.0 (0.0) | 0.3 (0.3) |
| PTSD | 2 | 0.5 | 0.3 (0.2) | 0.2 (0.2) | 0.4 (0.4) | 0.3 (0.2) | 0.2 (0.2) | 0.4 (0.4) |
| MDD/dysthymia | 1 | 0.2 | 0.1 (0.1) | 0.2 (0.2) | 0.0 (0.0) | 0.1 (0.1) | 0.2 (0.2) | 0.0 (0.0) |
| Tic disorder | 15 | 3.4 | 3.6 (1.2) | 4.5 (1.5) | 2.8 (2.0) | 1.7 (0.9) | 1.5 (0.6) | 1.8 (1.8) |
Note: Unless othewise noted, rates are weighted estimates. ADHD = attention-deficit/hyperactivity disorder; MDD = major depressive disorder; OCD = obsessive-compulsive disorder; PTSD = posttraumatic stress disorder; SE = standard error of the prevalence.
Comorbidity
The prevalence of general comorbidity (i.e., two or more disorders of any type) was 5.8% (SE =1.4). Among children with any disorder, 70.2% had one disorder, 13.7% had two disorders, and 16.2% had three or more disorders. The prevalence of heterotypic comorbidity was 3.5% (SE = 1.3, weighted n = 15).
Risk Factors Associated with Any Disorder
Of the sociodemographic and birth risk factors assessed, only early childhood and early elementary school poverty were significantly associated with the presence of any disorder (odds ratios [OR] = 2.23, 95% confidence intervals [CI] = 1.21 to 4.11, p = .0092; and OR = 1.99, 95% CI = 1.04 to 3.81, p = .0355, respectively) (Table 2). Among psychosocial risks, disorder status was significantly associated with high levels of parental depressive and anxiety symptoms (OR = 2.87, 95% CI = 1.52 to 5.39, p = .0008, OR = 3.60, 95% CI = 1.33 to 9.74, p = .0076, respectively), child stressful life events (OR = 2.40, 95% CI = 0.98 to 5.86, p = .0494), and child exposure to violence (OR = 4.43, 95% CI = 1.93 to 10.14, p = .0002). Not associated with disorder status were child sex, child race/ethnicity, paternal education, marital status, social support, birth status, and family expressiveness and conflict.
Risk Factors Associated with Internalizing and Externalizing Disorders
Children with externalizing disorders only were more likely to be male compared with children with no disorder (OR = 2.76, 95% CI: 1.00 to 7.60, p = .0435) or internalizing disorders only (OR = 5.03, 95% CI = 1.39 to 18.17, p = .0168) (Table 4). The likelihood of externalizing disorders was greater among children who had experienced stressful life events (OR = 3.76, 95% CI = 1.27-11.16, p = .0115), had low family expressiveness (OR = 3.19, 95% CI = 1.11 to 9.21, p = .0245), or were not of minority race/ethnicity (OR = 2.20, 95% CI = 1.01 to 4.78, p = .0373). Children with internalizing disorders were significantly more likely than children with no disorder (OR = 3.7, 95% CI = 1.34 to 10.25, p = .0079) or externalizing disorders (OR = 5.6, 95% CI = 1.38 to 22.50, p = .0077) to have parents with lower education. Children with internalizing disorders also were more likely than those with no disorder (OR = 8.93, 95% CI = 3.03 to 26.31, p < .0001) and externalizing disorders (OR = 5.45, 95% CI = 1.45 to 20.46, p = .0047) to have been exposed to violence in the previous year. In addition, increased risk for internalizing disorders relative to no disorder was associated with concurrent poverty (OR = 2.85, 95% CI = 1.14 to 7.16, p = .0209), early poverty (OR = 3.12, 95% CI = 1.31 to 7.46, p = .0076), and high parental anxiety symptoms (OR = 3.85, 95% CI = 1.14 to 12.92, p = .0205).
TABLE 4.
Sociodemographic and Psychosocial Factors Associated with Internalizing (Intern) and Externalizing (Extern) Disorders
| No Disorder (N = 331) | Intern Only (N = 26) | Extern Only (N = 37) | |
|---|---|---|---|
| Sociodemographic factors | % | % | % |
| Child sex (1 = male) | 48.9a | 34.4a | 72.5b |
| Minority ethnicity | 32.8a | 39.2ab | 18.1b |
| Kindergarten poverty | 13.1a | 30.1b | 15.7ab |
| Early poverty any | 15.7a | 36.7b | 18.4ab |
| Born to a teenage mother | 2.8 | 8.6 | 1.1 |
| Paternal or maternal education less than high school | 8.7a | 26.1b | 6.0a |
| Single parent home | 17.0 | 26.5 | 23.2 |
| No parent working | 5.7 | 1.5 | 6.9 |
| Birth status factors | |||
| Low birthweight | 10.0 | 10.0 | 12.9 |
| Low APGAR score | 1.4 | 1.7 | 2.3 |
| Family risk factors | |||
| Parental anxiety | 3.4a | 11.9b | 2.7ab |
| Parental depression | 13.1a | 23.3ab | 16.6ab |
| Child life events | 4.5a | 5.4ab | 14.9b |
| Parent life events | 11.3 | 6.9 | 14.1 |
| Low social support | 10.9 | 14.5 | 11.9 |
| Violence exposure | 4.0a | 27.2b | 6.4a |
| FES conflict | 7.4 | 6.0 | 16.5 |
| FES expressiveness | 5.4a | 3.7ab | 15.4b |
Note: Pairwise differences within row are noted by different subscripts (p < .05). FES = Family Environment Scale.
Social Competence and Family Burden Across the Diagnostic Groups
A MANCOVA was used to test for differences in social competence, Vine-land socialization, and FLIS family life impairment across the three diagnostic groups (no disorder, internalizing, and externalizing). Child sex was covaried in this model because of its association with both social competence and externalizing disorders and age was covaried to be conservative. The overall model was significant (Wilk's lambda = 0.88, F(8,588) = 5.033, p < .0001), with a moderate overall effect size (partial eta squared = 0.064). Examination of univariate effects indicated small effect sizes for each of the measures examined (Table 5). Results of pairwise tests indicated that parents and teachers reported lower social and adaptive competence on the ASBR and Vineland Socialization in children with externalizing disorders, as compared with children with no disorder or internalizing disorders. Teachers reported greater social competence among children with internalizing disorders relative to children without disorders. Finally, parents reported that both children with internalizing and externalizing disorders evidenced greater family life impairment than children with no disorder.
TABLE 5.
Social Competence and Family Burden According to Diagnostic Status
| No Disorder |
Internalizing Disorder Only |
Externalizing Disorder Only |
||||||
|---|---|---|---|---|---|---|---|---|
| Estimated Marginal Mean | SE | Estimated Marginal Mean | SE | Estimated Marginal Mean | SE | F | Partial η2 | |
| Parent-reported social competence (ASBR)1 | 3.09a | 0.03 | 3.10a | 0.10 | 2.81b | 0.09 | 4.47* | 0.03 |
| Teacher-reported social competence (ASBR)1 | 2.76a | 0.03 | 3.02b | 0.12 | 2.38c | 0.11 | 8.12*** | 0.05 |
| Vineland socialization1 | 95.21a | 0.73 | 94.44a | 2.67 | 85.88b | 2.44 | 7.21** | 0.04 |
| Family burden (FLIS)1 | 1.06a | 0.12 | 2.17b | 0.45 | 2.38b | 0.41 | 6.87** | 0.05 |
Note: ASBR = Adaptive Social Behavior Rating; FLIS = Family Life Impairment Scale; SE = standard error.
Mean differences are noted by different subscripts in the same row.
p < .05
p < .01
p < .001.
DISCUSSION
Prevalence rates for psychopathology in these young, school-aged children ascertained from birth records in a Northeastern urban and suburban SMSA are consistent with previous estimates of preschool children,12,14,16,19 older children, and adolescents11,15,17,18 and suggest that as children transition to formal schooling, approximately one in five (21.6%) will have a psychiatric disorder with impairment and may benefit from services. The estimated prevalence of psychiatric disorder was 13.8% for externalizing disorders and 11.1% for internalizing disorders. Inclusion of impairment criteria significantly decreased overall prevalence estimates of DSM-IV diagnoses, in a manner consistent with previous studies (32.0% to 21.6%).15,17 Impairment criteria affected rates of internalizing disorders more than externalizing disorders, which may reflect parents’ decreased awareness to the more subtle impairments associated with internalizing versus externalizing disorders. For example, parents may be less aware of internal distress and limitations in peer participation associated with fear or low motivation than they are of the impairing effects of rule-breaking, defiance and aggression. It is important to consider impairment criteria when estimating prevalence, as impairment predicts service use beyond all other factors.17
Comorbidity
Highlighting the complexity of treatment needs in this age range, 5.8% of the total sample, or 30% of children with any disorder met criteria for multiple psychiatric disorders. In addition, heterotypic comorbidity, or the presence of cooccurring internalizing and externalizing disorders, was observed in 3.5% of the total sample or approximately 62% of children who had more than one psychiatric disorder. That this form of comorbidity is not higher supports the differen tiation of psychopathology in this age range.52 Many empirically validated treatments focus on a particular disorder, yet, as these data reveal, children often present with multiple problems and disorders.53,54 This complexity in presentation is frequently cited as a reason for the poor uptake of evidence-based treatments in usual care settings.55
Risk
Relatively few sociodemographic risk factors were associated with disorder status. Boys were more likely than girls to evidence externalizing disorders, consistent with some previous epidemiological work,13,17 including work suggesting that the sex difference in disruptive behavior disorders emerges in early childhood11; others have not observed sex differences in early childhood.19 The lack of sex differences in internalizing disorders is consistent with studies that show sex differences emerging in adolescence.56 Sex differences also might be evident in patterns of individual symptom profiles or developmental pathways.56,57
Poverty in early childhood and early elementary school were associated with elevated rates of disorder. This adds to a large body of literature documenting the deleterious impact of poverty on young children's development.58 Further, consistent with Mesman and Koot's findings among 10- and 11-year-olds, stressful life events were associated with higher rates of externalizing problems.20 Although not consistently observed by others,13,17 parents with more limited education were more likely to report their children as meeting criteria for internalizing disorders.
Social Competence and Family Burden
A clear pattern linking externalizing diagnostic status with deficits in social competence emerged. These results are particularly significant given that social relationships during this entry-to-school period are protective for cognitive, social and academic trajectories.3-5,59 In contrast to expectations, teachers reported higher rates of social competence among children with internalizing disorders compared with children without disorders. These teacher ratings of interpersonal competence may contribute to lower rates of referral to mental services and children with internalizing disorders suffering in silence.52,60 Parents did not rate children with internalizing disorders lower or higher in social competence than nondisordered children. However, greater family burden was reported by parents of children with internalizing and externalizing disorders alike, relative to parents of nondisordered children, validating the impairing nature of these disorders.
This study has several limitations. First, in part because of children's young age, we relied on a single parent informant for diagnostic information. Although teachers provided dimensional reports on children's behavior problems and social competence, the lack of teacher diagnostic data may have depressed rates of ADHD and CD.15 Moreover, although children in this age range do not provide reliable information on the DISC,61 the lack of child data may have depressed rates of depression and anxiety disorders other than specific phobias, which are more likely to be observed by parents. The rate of specific phobias was higher than that observed in comparable studies in this age range.13,15
Second, we relied on a structured, respondent-based interview that does not provide opportunities for clarification of symptom or impairment criteria. This may be particularly problematic at young ages, as normative expectations for adaptive school and social functioning are more variable.22 Although comparable to Canino et al.,17 use of a respondent-based interview makes comparisons with interviewer based studies11,12,18 or to clinical review of structured interviews15 difficult. Had we, like Ford et al.,15 required impairment that “merited clinical intervention” versus a single parent indicating that disorder symptoms occurred “some of the time” or “a lot of the time” or caused “bad” or “very bad” problems or feelings in at least one context, our rates would likely be closer to the 10% they reported. Because of interest in examining associations with risk factors, we did not address higher levels of impairment.
Third, our initial exclusions likely introduce a number of biases. Specifically, sampling healthy, full-term births likely results in lower estimates than would be expected without exclusions used; although somewhat controversial, children born preterm and/or small for gestational age are at higher risk for ADHD and other disorders.62 In addition, excluding families who could not participate in English excluded an important segment of the Hispanic population, likely biasing toward higher acculturation.
Fourth, given that we have sampled only from one Northeastern Metropolitan Statistical Area, the application of these results to other regions should be approached with caution.
Fifth, our two-stage sampling approach, which used oversampling based on broad selection criteria including early and concurrent emotional and behavioral and language problems, reduced statistical precision relative to a simple random sample of the same size. Finally, it will be important to extend these cross-sectional findings to capitalize on our longitudinal data from early childhood.
In conclusion, this study examined prevalence rates of DSM-IV childhood disorders in a representative population sample of children during the transition to formal schooling, a sensitive developmental period that has been the focus of intensive study in the developmental literature.3-5 Despite multiple methodological limitations and differences from previous prevalence studies, rates of psychopathology in this sample (21.6%) are consistent with those reported for older and younger children. Among children with a disorder, comorbidity was not the rule but was not uncommon (30%), highlighting differentiation of psychopathology in this age range and the complexity of mental health needs. Teachers and parents reported limitations in social competence among children with externalizing disorders, and parents reported elevated family burden for children with internalizing and externalizing disorders.
Epidemological data on prevalence and risk co-incidence with disorders during the transition to school can and should inform conversations about psychosocial school readiness, early intervention, and prevention programming. Moreover, given compelling evidence that difficulty in social competencies in the transition to school is associated with later school functioning,4,6,59 intervening at only the level of disorder or symptomatology may not be sufficient. Rather, intervention should also take into account the social context, not only within the school setting but also with respect to risk factors in the home and broader community. &
Acknowledgments
Support for this research came from a grant to the first author from the National Institute of Mental Health (R01MH55278), the MRSA/ MCHB LEND project (HERSA/MCHB T73MC00020l; Dr. David Helm, PI), and the Mental Health/Developmental Disabilities at Children's Hospital Boston (National Institute of Mental Health/ National Institutes of Health R25 MH0171286; Dr. Kerim Munir, PI).
Footnotes
The authors thank all of the children and families who participated.
Disclosure: Drs. Carter and Briggs-Gowan receive royalties from the sale of the Infant Toddler Social and Emotional Assessment from Pearson Assessment. Drs. Wagmiller and Horwitz and Ms. Gray and McCarthy report no biomedical financial interests or potential conflicts of interest.
REFERENCES
- 1.Cairns RB, Cairns BD. Lifelines and Risks: Pathways of Youth in Our Time. Cambridge University Press; Cambridge, UK: 1994. [Google Scholar]
- 2.Coie JD, Watt NF, West SG, et al. The science of prevention: a conceptual framework and some directions for a national research program. Am Psychol. 1993;48:1013–1022. doi: 10.1037//0003-066x.48.10.1013. [DOI] [PubMed] [Google Scholar]
- 3.La Paro KM, Pianta RC. Predicting children's competence in the early school years: a meta-analytic review. Rev Educ Res. 2000;70:443–484. [Google Scholar]
- 4.McClelland MM, Morrison FJ, Holmes D. Children at risk for early academic problems: the role of learning-related social skills. Early Childhood Res Q. 2000;15:307–329. [Google Scholar]
- 5.Hamre B, Pianta RC. Early teacher-child relationships and children's social and academic outcomes through eighth grade. Child Dev. 2000;72:625–638. doi: 10.1111/1467-8624.00301. [DOI] [PubMed] [Google Scholar]
- 6.Burchinal MR, Peisner-Feinberg ES, Pianta RC, Howes C. Development of academic skills from preschool through second grade: family and classroom predictors of developmental trajectories. J Sch Psychol. 2002;40:415–436. [Google Scholar]
- 7.Achenbach TM, Edelbrock CS. Taxonomic issues in child psychopathology. In: Ollendick TH, Hersen M, editors. Handbook of Child Psychopathology. Plenum Press; New York: 1983. pp. 65–93. [Google Scholar]
- 8.Lopez SJ, Edwards LM, Pedrotti JT, et al. Beyond the DSM-IV: assumptions, alternatives, and alterations. J Counsel Dev. 2006;84:259–267. [Google Scholar]
- 9.Farmer EM, Burns BJ, Phillips SD, Angold A, Costello EJ. Pathways into and through mental health services for children and adolescents. Psychiatr Serv. 2003;54:50–66. doi: 10.1176/appi.ps.54.1.60. [DOI] [PubMed] [Google Scholar]
- 10.Costello EJ, Angold A, Burns BJ, et al. The Great Smoky Mountains Study of Youth: goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry. 1996;53:1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- 11.Angold A, Erkanli A, Farmer EM, et al. Psychiatric disorder, impairment, and service use in rural African American and white youth. Arch Gen Psychiatry. 2002;59:893–901. doi: 10.1001/archpsyc.59.10.893. [DOI] [PubMed] [Google Scholar]
- 12.Egger HL, Erkanli A, Keeler GP, Potts E, Walter BK, Angold A. Test-retest reliability of the Preschool Age Psychiatric Assessment (PAPA). J Am Acad Child Adolesc Psychiatry. 2006;45:538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- 13.Briggs-Gowan MJ, Owens PL, Schwab-Stone ME, Leventhal JM, Leaf PJ, Horwitz SM. Persistence of psychiatric disorders in pediatric settings. J Am Acad Child Adolesc Psychiatry. 2003;42:1360–1369. doi: 10.1097/01.CHI.0000084834.67701.8a. [DOI] [PubMed] [Google Scholar]
- 14.Lavigne JV, Gibbons RD, Christoffel KK, et al. Prevalence rates and correlates of psychiatric disorders among preschool children. J Am Acad Child Adolesc Psychiatry. 1996;35:204–214. doi: 10.1097/00004583-199602000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Ford T, Goodman R, Meltzer H. The British Child and Adolescent Mental Health Survey 1999: the prevalence of DSM-IV disorders. J Am Acad Child Adolesc Psychiatry. 2003;42:1203–1211. doi: 10.1097/00004583-200310000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Keenan K, Shaw DS, Walsh B, Delliquadri E, Giovannellie J. DSM-III-R disorders in preschool children from low-income families. J Am Acad Child Adolesc Psychiatry. 1997;36:620–627. doi: 10.1097/00004583-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Canino G, Shrout PE, Rubio-Stipec M, et al. The DSM-IV rates of child and adolescent disorders in Puerto Rico. Arch Gen Psychiatry. 2004;61:85–93. doi: 10.1001/archpsyc.61.1.85. [DOI] [PubMed] [Google Scholar]
- 18.Costello EJ, Mustillo S, Erkanli A, Keeler GP, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 19.Lavigne JV, LeBailly SA, Hopkins J, Gouze KR, Binns HJ. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. J Child Adolesc Psychol. 2009;38:315–328. doi: 10.1080/15374410902851382. [DOI] [PubMed] [Google Scholar]
- 20.Mesman J, Koot HM. Early preschool predictors of preadolescent internalizing and externalizing DSM-IV diagnoses. J Am Acad Child Adolesc Psychiatry. 2001;40:1029–1036. doi: 10.1097/00004583-200109000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Regier DA, Narrow WE. Defining clincially significant psychopathology with epidemiologic data. In: Helzer JE, Hudziak JJ, editors. Defining Psychopathology in the 21st Century: DSM-V and Beyond. American Psychiatric Publishing; Washington, DC: 2002. [Google Scholar]
- 22.Carter AS, Briggs-Gowan MJ, Davis AS. Assessment of young children's social-emotional development and psychopathology: recent advances and recommendations for practice. J Child Psychol Psychiatry. 2004;45:109–134. doi: 10.1046/j.0021-9630.2003.00316.x. [DOI] [PubMed] [Google Scholar]
- 23.Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- 24.Carter AS, Briggs-Gowan MJ, Jones SM, Little TD. The Infant-Toddler Social and Emotional Assessment (ITSEA): factor structure, reliability, and validity. J Abnorm Child Psychol. 2003;53:495–514. doi: 10.1023/a:1025449031360. [DOI] [PubMed] [Google Scholar]
- 25.Rimm-Kaufman SE, Pianta RC. An ecological perspective on the transition to kindergarten: a theoretical framework to guide empirical research. J Appl Dev Psychol. 2000;21:491–511. [Google Scholar]
- 26.Ladd GW. Having friends, keeping friends, making friends, and being liked by peers in the classroom: predictors of children's early school adjustment? Child Dev. 1990;61:1081–1110. [PubMed] [Google Scholar]
- 27.Strormshak EA, Webster-Stratton C. The qualitative interactions of children with conduct problems and their peers: differential correlates with self-report measures, home behavior, and school behavior problems. J Appl Dev Psychol. 1999;20:295–317. [Google Scholar]
- 28.Ladd GW, Burgess KB. Charting the relationship trajectories of aggressive, withdrawn, and aggressive/withdrawn children during early grade school. Child Dev. 1999;70:910–929. doi: 10.1111/1467-8624.00066. [DOI] [PubMed] [Google Scholar]
- 29.Thorell LB, Rydell AM. Behaviour problems and social competence deficits associated with symptoms of attention-deficit/hyperactivity disorder: effects of age and gender. Child Care Health Dev. 2008;34:584–595. doi: 10.1111/j.1365-2214.2008.00869.x. [DOI] [PubMed] [Google Scholar]
- 30.Messer J, Goodman R, Rowe R, Meltzer H, Maughan B. Preadolescent conduct problems in girls and boys. J Am Acad Child Adolesc Psychiatry. 2006;45:184–191. doi: 10.1097/01.chi.0000186403.13088.d8. [DOI] [PubMed] [Google Scholar]
- 31.Costello EJ, Egger HL, Angold A. 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry. 2005;44:972–986. doi: 10.1097/01.chi.0000172552.41596.6f. [DOI] [PubMed] [Google Scholar]
- 32.Shanahan L, Copeland W, Costello EJ, Angold A. Specificity of putative psychosocial risk factors for psychiatric disorders in children and adolescents. J Child Psychol Psychiatry. 2008;49:34–42. doi: 10.1111/j.1469-7610.2007.01822.x. [DOI] [PubMed] [Google Scholar]
- 33.Carter AS, Briggs-Gowan MJ. Manual for the Infant-Toddler Social & Emotional Assessment (ITSEA)–Version 2. Psychological Corporation, Harcourt Press; San Antonio, TX: 2006. [Google Scholar]
- 34.Achenbach TM, Rescorla L. Manual for the ASEBA Preschool Forms and Profiles. University of Vermont; Burlington, VT: 2000. [Google Scholar]
- 35.Ireton H. Child Development Inventory. Behavior Science Systems; Minneapolis, MN: 1992. [Google Scholar]
- 36.Redmond SM, Rice ML. The socioemotional behaviors of children with SLI. J Speech Language Hearing Res. 1998;41:688–700. doi: 10.1044/jslhr.4103.688. [DOI] [PubMed] [Google Scholar]
- 37.Irwin J, Carter AS, Briggs-Gowan MJ. The social-emotional development of ”late-talking” toddlers. J Am Acad Child Adolesc Psychiatry. 2002;41:1324–1332. doi: 10.1097/00004583-200211000-00014. [DOI] [PubMed] [Google Scholar]
- 38.Schaffer D, Fisher P, Dulcan MK, Davies M, Piacentini J, Schwab-Stone ME. The NIMH Diagnostic Interview Schedule for Children, Verson 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA study. J Am Acad Child Adolesc Psychiatry. 1996;35:865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- 39.Briggs-Gowan MJ, Horwitz SM, Carter AS. The Family Life Impairment Scale. Yale University, Department of Psychology; New Haven, CT: 1997. [Google Scholar]
- 40.Reynolds CR, Kamphaus RW. Behavior Assessment System for Children (BASC) American Guidance Service; Circle Pines, MN: 1992. [Google Scholar]
- 41.Ladd GW, Profilet SM. The child behavior scale: a teacher-report measure of young children's aggressive, withdrawn, adn prosocial behaviors. Dev Psychol. 1996;32:1008–1024. [Google Scholar]
- 42.Sparrow SS, Carter AS, Cicchetti DV. Vineland screener: record booklets, administration and scoring. Yale University Child Study Center; New Haven, CT: 1993. [Google Scholar]
- 43.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 44.Radloff LS. The CES-D scale. Appl Psychol Measure. 1977;1:385–401. [Google Scholar]
- 45.Moos R, Moos B. Family Environment Scale Manual. 2nd ed. Consulting Psychologists Press; Palo Alto, CA: 1986. [Google Scholar]
- 46.Carter AS, Briggs-Gowan MJ. Child Life Events Screener. Yale University; New Haven, CT: 1998. [Google Scholar]
- 47.Mongillo EA, Briggs-Gowan MJ, Ford JD, Carter AS. Impact of traumatic life events in a community sample of toddlers. J Abnorm Child Psychol. 2009;37:455–468. doi: 10.1007/s10802-008-9283-z. [DOI] [PubMed] [Google Scholar]
- 48.Cochrane R, Robertson A. The life events inventory: a measure of the relative severity of psycho-social stressors. J Psychosom Res. 1973;17:135–140. doi: 10.1016/0022-3999(73)90014-7. [DOI] [PubMed] [Google Scholar]
- 49.Holmes TH, Rahe RH. The Social Readjustment Rating Scale. J Psychosom Res. 1967;11:213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 50.Sherbourne CD, Stewart A. The MOS Social Support Survey. Soc Sci Med. 1991;32:706–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 51.Murphy KR, Myors B. Statistical power analysis: a simple and general model for traditional and modern hypothesis tests. 2 ed. Lawrence Erlbaum; Mahwah, NJ: 2004. [Google Scholar]
- 52.Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: presentation, nosology, and epidemiology. J Child Psychol Psychiatry. 2006;47:313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- 53.Goldfried MR, Wolfe BE. Toward a more clinically valid approach to therapy research. J Consult Clin Psychol. 1998;66:143–150. doi: 10.1037//0022-006x.66.1.143. [DOI] [PubMed] [Google Scholar]
- 54.Newman DL, Moffitt TE, Caspi A, Silva PA. Comorbid mental distorders: implications for treatment and sample selection. J Abnorm Psychol. 1998;107:305–311. doi: 10.1037//0021-843x.107.2.305. [DOI] [PubMed] [Google Scholar]
- 55.Weisz JR, Donenberg GR, Han SS, Weiss B. Bridging the gap between laboratory and clinic in child and adolescent psychotherapy. J Consult Clin Psychol. 1995;63:688–701. doi: 10.1037//0022-006x.63.5.688. [DOI] [PubMed] [Google Scholar]
- 56.Crick NR, Zahn-Waxler C. The development of pyschopathology in females and males: current progress and future challenges. Dev Psychopathol. 2003;15:719–742. [PubMed] [Google Scholar]
- 57.Mesman J, Bongers IL, Koot HM. Preschool developmental pathways to preadolescent internalizing and externalizing problems. J Child Psychol Psychiatry. 2001;42:679–689. [PubMed] [Google Scholar]
- 58.McLoyd VC. Socioeconomic disadvantage and child development. Am Psychologist. 1998;53:185–204. doi: 10.1037//0003-066x.53.2.185. [DOI] [PubMed] [Google Scholar]
- 59.Hamre B, Pianta RC. Early teacher-child relationships and the trajectory of children's school outcomes through eighth grade. Child Dev. 2001;72:625–638. doi: 10.1111/1467-8624.00301. [DOI] [PubMed] [Google Scholar]
- 60.Zahn-Waxler C, Klimes-Dougan B, Slattery MJ. Internalizing problems of chlidhood and adolescence: prospects, pitfalls, and progress in understanding the development of anxiety and depression. Dev Psychopathol. 2000;12:443–466. [PubMed] [Google Scholar]
- 61.Schwab-Stone ME, Fallon T, Briggs M, Crowther B. Reliability of diagnostic reporting for children aged 6-11: a test-retest study of the Diagnostic Interview Schedule for Children–Revised. Am J Psychiatry. 1994;151:1048–1054. doi: 10.1176/ajp.151.7.1048. [DOI] [PubMed] [Google Scholar]
- 62.Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJS. Cognitive and behavioral outcomes of school-aged children who were born preterm. J Am Med Assoc. 2002;288:728–737. doi: 10.1001/jama.288.6.728. [DOI] [PubMed] [Google Scholar]