Abstract
The relationship between hiatal hernias and gastroesophageal reflux disease (GERD) has been greatly debated over the past decades, with the importance of hiatal hernias first being overemphasized and then later being nearly neglected. It is now understood that both the anatomical (hiatal hernia) and the physiological (lower esophageal sphincter) features of the gastroesophageal junction play important, but independent, roles in the pathogenesis of GERD, constituting the widely accepted "two-sphincter hypothesis." The gastroesophageal junction is an anatomically complex area with an inherent antireflux barrier function. However, the gastroesophageal junction becomes incompetent and esophageal acid clearance is compromised in patients with hiatal hernia, which facilitates the development of GERD. Of the different types of hiatal hernias (types I, II, III, and IV), type I (sliding) hiatal hernias are closely associated with GERD. Because GERD may lead to reflux esophagitis, Barrett's esophagus and esophageal adenocarcinoma, a better understanding of this association is warranted. Hiatal hernias can be diagnosed radiographically, endoscopically or manometrically, with each modality having its own limitations, especially in the diagnosis of hiatal hernias less than 2 cm in length. In the future, high resolution manometry should be a promising method for accurately assessing the association between hiatal hernias and GERD. The treatment of a hiatal hernia is similar to the management of GERD and should be reserved for those with symptoms attributable to this condition. Surgery should be considered for those patients with refractory symptoms and for those who develop complications, such as recurrent bleeding, ulcerations or strictures.
Keywords: Hiatal hernia, Gastroesophageal reflux disease, Lower esophageal sphincter
INTRODUCTION
Over the past few decades, our understanding on the relationship between hiatal hernia and gastroesophageal reflux disease (GERD) has evolved, shifting from one extreme to the other. Initially it was considered that the presence of hiatal hernia, an anatomical abnormality, was a sine qua non in the pathogenesis of GERD ever since its association was first emphasized by Allison in 1951.1 And for about 20 years that followed, hiatal hernia was used almost synonymously with GERD. However, this concept took a turn to the other direction afterwards to focus on the physiology of lower esophageal sphincter (LES). In the early 1970s, Cohen et al.2,3 reported that instead of the anatomical abnormality as occurs in hiatal hernia, hypotonic LES was indeed associated with GERD. In 1982, the significance of LES physiology was further supported by Dodds et al.4 who highlighted the role of transient LES relaxations (tLESRs) not associated with swallowing as the major contributing factor for GERD. Thus, with the widespread use of esophageal manometry and the development of its techniques, the center of attention shifted to the LES5 and the importance of hiatal hernia became obscure or nearly abandoned so as to be considered an incidental finding during upper gastrointestinal examination. After rigorous investigations in recent years, new insights regarding the pathogenesis of GERD were gained. It is currently understood that in addition to other factors such as esophageal acid clearance, tissue resistance, gastric acid secretion, delayed gastric emptying, etc., both the presence of hiatal hernia and the functional abnormality of LES are independently important,6,7 which are the two fundamental components (intrinsic LES and extrinsic compression by the crural diaphragm) of the now generally accepted "two-sphincter hypothesis."8-10 This review will focus on the clinical significance of hiatal hernia on GERD.
ANATOMY OF GASTROESOPHAGEAL JUNCTION
GERD is believed to occur when there is imbalance between defensive factors and aggressive factors. Defensive factors are gastroesophageal junction (GEJ), esophageal acid clearance and tissue resistance. Aggressive factors are gastric factors such as gastric acid secretion, delayed gastric emptying, etc.
GEJ is the first and primary line of esophageal defense against damage by refluxate, and pathologic reflux is thought to occur when there is impairment in this barrier. GEJ is an anatomically complex region that consists of the intrinsic LES, the crural diaphragm, the intra-abdominal location of the LES, the acute angle of His and the phrenoesophageal ligament/membrane. LES is the distal 3 to 4 cm segment of the esophagus that is tonically contracted at rest, and is the principal component of the antireflux barrier. Normal resting LES pressure varies from 10 to 45 mm Hg relative to the intragastric pressure, and there is a considerable temporal variation in the basal LES tone with it being lowest after meals and highest at night.11 Tone of LES is maintained by the intrinsic tone of the muscle itself and by the extrinsic cholinergic innervation.12 The LES tone is also influenced by many factors such as intra-abdominal pressure, circulating peptides and hormones, foods and many drugs. Progesterone, fatty meal, chocolate, alcohol, peppermint, theophylline, octreotide, anticholiergics, etc. are known to decrease the LES tone.
The mechanism of reflux due to GEJ incompetence can be summed down to three: 1) tLESRs, 2) hypotensive LES, and 3) anatomical defect such as hiatal hernia. For those without structural abnormalities of the antireflux barrier, inappropriate tLESR is the dominant and single most important mechanism, and these patients tend to present with milder disease severity compared to those with severe GERD whose predominant mechanism can be attributed more to the presence of hypotonic LES and/or anatomical defect such as hiatal hernia.4,11,13,14
ANATOMY AND ETIOLOGY OF HIATAL HERNIA
Hiatal hernia is a condition in which parts of the abdominal contents, mainly the GEJ and the stomach, are proximally displaced above the diaphragm through the esophageal hiatus into the mediastinum. Esophageal hiatus is an elliptically shaped opening most commonly formed by elements of the right diaphragmatic crus that encircles the distal portion of the esophagus in a sling-like fashion.15 Normally, the distal portion of the esophagus is anchored to the esophageal hiatus by the phrenoesophageal ligament/membrane (also called the fascia of Laimer) that is formed by the fusion of endothoracic and endoabdominal fascia. The phrenoesophageal ligament/membrane is inserted circumferentially into the esophageal musculature in the close vicinity of the squamocolumnar junction (SCJ).16 This ligament/membrane is essential in maintaining the competence of GEJ and preventing the migration of GEJ and/or stomach into the posterior mediastinum by sealing off potential spaces between the esophageal hiatus and the distal portion of the esophagus.17,18
During normal swallows, the esophageal body shortens due to the contraction of the esophageal longitudinal muscles and the phrenoesophageal ligament/membrane is stretched. As a result, GEJ and a small part the stomach is proximally displaced through the esophageal hiatus. At the end of each swallow, the migrated segment is brought to its normal position by the elastic recoil of the phrenoesophageal ligament/membrane.19 However, the phrenoesophageal ligament/membrane becomes progressively lax by losing the amount of elastic tissues with aging, possibly through wear and tear due to repetitive stress of swallowing, thus predisposing to the development of hiatal hernia.20,21 Loss of elasticity of the phrenoesophageal ligament/membrane may also be caused by excessive contraction of the esophageal longitudinal muscle, increased abdominal pressure as occurs in power atheletes,22 pregnancy,23 genetic predisposition,24,25 and previous surgery. Some propose that instead of hiatal hernia being the cause of reflux esophagitis, reflux esophagitis itself is the primary culprit that initiates and sustains the esophagitis-hernia complex; a study with opossums showed that acidification of the esophageal mucosa induced longitudinal muscle contraction, resulting in shortening of the esophagus.26-28
TYPES OF HIATAL HERNIA
There are two major types of hiatal hernia: sliding hiatal hernia and para-esophageal hiatal hernia. Depending on how one subdivides the para-esophageal hiatal hernias, hiatal hernia can be categorized into three29,30 or four31 types, which would be the most comprehensive classification.
1. Type I
Type I hiatal hernia is the sliding hiatal hernia (also called concentric or axial hiatal hernia) which accounts for more than 95% of all hiatal hernias with the remaining 5% being paraesophageal hiatal hernias taken together.32 This type is characterized by widening of the esophageal hiatus and laxity of the phrenoesophageal ligament/membrane allowing GEJ and some portion of the stomach, especially the gastric cardia, to be displaced above the diaphragm. Due to the widening of the esophageal hiatus, the caliber of the esophageal luminal opening at this level often approximates the size of esophageal hiatus, becoming evident while observing the cardia during endoscopic examination with sufficient insufflations. However, the orientation of the stomach axis remains unchanged. The sliding hiatal hernia can either be reducible or nonreducible. Since movement of GEJ within the range of 2 cm is considered physiologic, as occurs during normal swallows, it is commonly believed that sliding hiatal hernia should exceed this range to be considered clinically significant. As will be discussed later, sliding hiatal hernia can be diagnosed radiologically using barium swallow examination, endoscopically during upper endoscopy, or manometrically by either conventional or high-resolution esophageal manometry. The significance of sliding hiatal hernia is its relation with GERD in which the symptoms worsen with increasing size of the sliding hiatal hernia.
2. Type II
Type II hiatal hernia is the classic form of para-esophageal hernia in which part of the gastric fundus, and not the GEJ, herniates above the diaphragm alongside the esophagus as a result of localized defect in the phrenoesophageal ligament/membrane. If the herniated segment does not reduce, incarceration can occur. Since the GEJ remains in its normal position fixed to the preaortic fascia and the median arcuate ligament, the stomach is more likely to rotate around its longitudinal or infrequently around its transverse axis during herniation, resulting in an organoaxial volvulus and mesenteroaxial volvulus, respectively.33 The laxity of the gastrosplenic and gastrocolic ligaments, which accompanies this type of hiatal hernia in many instances, further predisposes and facilitates the occurrence of aforementioned variety of volvulus. With time, this type of hiatal hernia progressively enlarges and necessitates operation to bring the herniated portion to its normal position and also to relieve the incarcerated segment.
3. Type III
Type III hiatal hernia is the mixture of type I and II hiatal hernia. In this type, in addition to the para-esophageal hiatal hernia, the GEJ is not fixed but displaced above the diaphragm.
4. Type IV
Type IV hiatal hernia is the herniation of other abdominal organs (spleen, colon, pancreas, etc.) through the esophageal hiatus into the posterior mediastinum. Due to the progressive enlargement of esophageal hiatus and a large defect in the phrenoesophageal ligament/membrane, there is enough space not only for the stomach but also for other abdominal organs to be displaced above the diaphragm. Therefore, it can be viewed as an aggravated form of type III hiatal hernia and some include type IV to type III hiatal hernia.
The remainder of this review will focus on the type I (sliding) hiatal hernia and henceforth use the term "hiatal hernia" to refer to this anatomic abnormality, since this type is the one that is associated with GERD.
DIAGNOSIS
The diagnosis of hiatal hernia can be made through radiographic, endoscopic, and manometric assessment. Whereas large hiatal hernias can be detected and diagnosed without difficulty using either of these methods, diagnosing small hiatal hernias (<2 cm) can be challenging with each modality having its limitations.
1. Radiographic assessment
While performing barium contrast studies of the upper gastrointestinal tract, a globular structure termed "phrenic ampulla" is seen above the diaphragm during swallows.32 This structure has traditionally been considered to be a physiologic finding, but the study using simultaneous fluoroscopy and manometry demonstrated that it corresponded to a small reducing hiatal hernia.16 There are several landmarks of the phrenic ampulla that are worth mentioning. The upper margin of the phrenic ampulla abuts the tubular esophagus forming a structure called "A" ring, which is a muscular ring. This ring corresponds to the upper margin of the LES. The lower margin of the phrenic ampulla is demarcated by the diaphragmatic indentation. Within the phrenic ampulla, a mucosal ring ("B" ring) can be identified, which corresponds to the squamocolumnar junction (Z-line) or the union of the esophagus with the stomach.34 When the "B" ring is prominent, i.e., luminal diameter <13 mm, it is called Schatzki's ring. Radiographically, hiatal hernia is usually defined as the separation of "B" ring and the diaphragmatic indentation of >2 cm (Fig. 1).30,33,34
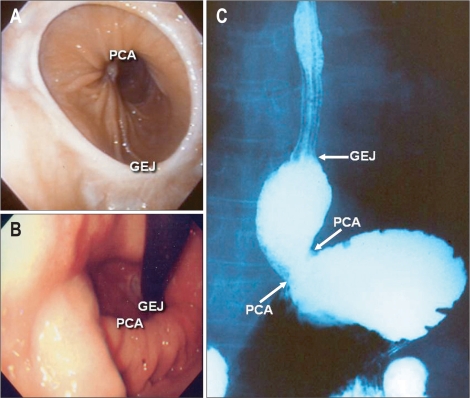
Fig. 1.
Endoscopic and radiologic findings of a sliding type hiatal hernia. A hiatal hernia is a portion of proximal stomach between the gastroesophageal junction (B ring; GEJ) and the diaphragmatic indentation (pinchcock action, PCA). If it is large, a hiatal hernia can be easily observed with a forward or retroflexed view during an upper gastrointestinal endoscopy (A, B) or with barium swallows (C).
The limitation of this method is that it is not always possible to detect all the landmarks of the phrenic ampulla. Defining hiatal hernia especially becomes problematic when the "B" ring, marker necessary for defining the presence of hiatal hernia that is only detectable in about 15% of subjects, cannot be identified. In the absence of the "B" ring, the result of barium contrast studies to diagnose hiatal hernia can become quite inconsistent. In this case, the upper margin of the rugal folds is used instead as the reference point. In addition, the timing of taking images can serve as a source of inaccuracy, since the distance between the "B" ring and the diaphragmatic indentation would vary depending on at which point of swallowing the images were taken. The lack of standardized protocol as to whether examination should be done in upright or supine position etc. also adds to the inconsistency in diagnosing hiatal hernias. Furthermore, in order to observe the relationship between the aforementioned structures and view them under fluoroscopy, the patient should swallow the contrast material. Since swallowing itself distends and shortens the esophageal lumen, diagnosing hiatal hernia <2 cm becomes impractical with barium contrast studies.
2. Endoscopic assessment
The use of endoscopy has become widespread over the past few decades and is now considered the standard modality for diagnosing and treating diseases of the upper gastrointestinal tract. Although barium contrast study has been the most commonly applied method for diagnosing hiatal hernia worldwide, hiatal hernia is increasingly diagnosed with endoscopy (Fig. 1). The most commonly accepted diagnostic criterion of endoscopic hiatal hernia is the proximal dislocation of GEJ of >2 cm above the diaphragmatic indentation. However, controversy still exists as to which marker of GEJ should serve as the reference to diagnose the presence of hiatal hernia: SCJ, the upper margin of the gastric folds or the distal margin of the palisade zone. Therefore, to diagnose hiatal hernia endoscopically, endoscopic definition of GEJ should first be clarified.
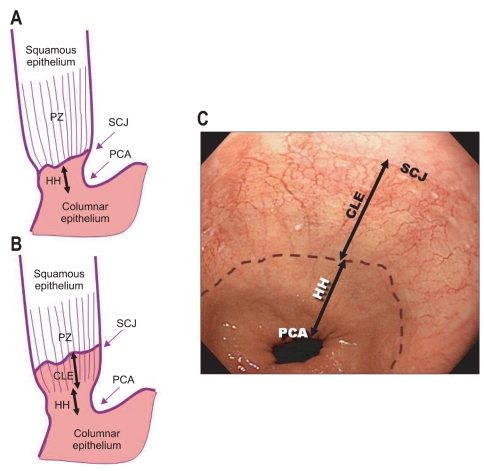
SCJ is the circumferential margin that is formed by the pinkish gray colored squamous epithelium of the esophagus and the reddish orange colored columnar epithelium of the stomach. This transition zone is also called the "Z-line" and can vary in contour.35 SCJ usually corresponds to GEJ in normal subjects and many consider that hiatal hernia is present when there is separation of >2 cm between the SCJ and the diaphragmatic indentation.29 However in the presence of columnar-lined esophagus or Barrett's esophagus, SCJ is moved cranially and thus cannot serve as a reliable marker. The upper margin of the gastric folds is also a generally accepted marker used to identify GEJ.36,37 Nevertheless, endoscopists sometimes have difficulty identifying this marker clearly. Another option is to use the distal margin of the palisade zone to depict the GEJ. Palisade zone is the longitudinally parallel capillaries running underneath the most distal 2 to 3 cm of the esophageal epithelium.38 In 1966, de Carvalho took a special interest in this vascular anatomy and schematically illustrated its angioarchitecture dividing it into four distinct zones.39 These zones were later named as truncal zone, perforating zone, palisade zone and gastric zone.40,41 Based on this anatomy, Hoshihara classified the patterns of GEJ into four types according to the relationship among the distal margin of the palisade zone, SCJ and the diaphragmatic indentation.42 In the first type, the distal margin of the palisade zone, SCJ and the diaphragmatic indentation (or pinchcock action) all fall at the same level. In the second type, the distal margin of the palisade zone and the diaphragmatic indentation lie at the same level but SCJ is proximally located. In third type, the distal margin of the palisade zone and SCJ coincides but the diaphragmatic indentation is found distal in relation to them. In fourth type, SCJ is situated proximal to both the distal margin of the palisade zone and the diaphragmatic indentation. Since the distal margin of the palisade zone is known to correspond to the GEJ,37,40,41 the third and fourth types can be thought to meet the definition of hiatal hernia (Fig. 2). However, the palisade zone may not be visible in the presence of inflammation of the squamous epithelium that overlies the vasculature. In normal subjects, the SCJ, the upper margin of the gastric fold and the distal margin of the palisade zone generally coincide and approximate the GEJ. Therefore, either of these markers would be suitable for diagnosing hiatal hernia endoscopically, but in the presence of columnar-lined esophagus and/or Barrett's esophagus, the distal margin of the palisade zone would be more appropriate whenever it can be identified.
Fig. 2.
Endoscopic diagnosis of short segment hiatal hernias using lower esophageal capillary patterns as guides. Endoscopic identification of the gastroesophageal junction is occasionally difficult, especially in patients with short segment hiatal hernias (HHs). Using the distal margin of longitudinally arrayed subepithelial capillaries (palisade zone, PZ) as a landmark for the gastroesophageal junction, patterns can be classified according to the relationships between the distal end of the PZ with the squamocolumnar junction (SCJ) and the diaphragmatic indentation (pinchcock action, PCA). (A) The PCA is distal to the other two markers that are at the same level. (B) The SCJ is proximal to the distal end of the PZ, which is proximal to the PCA. The HH is the area between the distal margin of the PZ and the PCA, and the columnar-lined esophagus (CLE) is in the area between the SCJ and the distal margin of the PZ.
There are many limitations in using endoscopes to diagnose hiatal hernia. Measuring the size of hiatal hernia with incisor as the reference point and using centimeter markings on the scope that is spaced every 5 cm as a ruler can be said to lack in precision. The mouthpiece or bite block also hinders viewing the location of the incisor if it not transparent. Since the esophageal hiatus is elliptically shaped and obliquely located, the distance from the tip of the scope to incisor would vary along the circumference of the opening. Although we usually look for the presence and evaluate the extent of hiatal hernia during insertion of the endoscopes with minimum insufflations of air, there are still confusions as to when (during insertion or removal of the endoscopes) or at which phase of respiration measurements should be made, or how much air should be insufflated. To make to matters worse, retching or belching of the patients during examination can alter the location and anatomy of GEJ. Furthermore, even when the measurements are made, there can be a great degree of inter- and intra-observer variation among endoscopists, thus lacking in reproducibility.43 Due to these limitations, some advocate observing the GEJ by retroflexing the scope in the stomach to assess its appearance (gastroesophageal flap valve) and grade the severity of hiatal hernia,44-46 but further study is warranted to ascertain its clinical implication.
3. Manometric assessment
Esophageal manometry measures intraluminal pressures and coordinated contractile movements of the esophageal musculature. Therefore, it is most commonly applied for assessing peristaltic function of the esophagus and measuring the LES pressure and relaxation, thus aiding in the evaluation of esophageal motility disorders. Although esophageal manometry is generally not indicated and plays a minimal role in diagnosing GERD, it can be used for establishing the presence of a hiatal hernia.
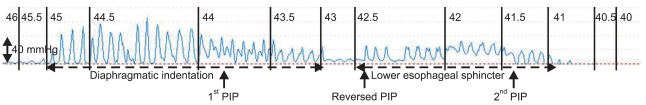
Two important landmarks for defining hiatal hernia are the presence of high-pressure zone separation and the location of the respiratory pressure inversion (or reversal) point. During deep inspiration, the abdominal pressure rises and the intrathoracic pressure decreases. Therefore, the part of the manometry probe that is located in the gastric lumen translates this pressure change as a positive deflection whereas that located in the intrathoracic portion of the esophageal lumen records it as a negative deflection. Since the diaphragm descends during inspiration, the manometry probe situated at the level of the diaphragm first shows a positive deflection then a negative deflection, as the probe that was intragastric becomes intrathoracic. This is called the respiratory pressure inversion point. During a pull-through tracing in normal subjects, only one high-pressure zone that corresponds to the pressure made by the LES and the diaphragmatic indentation can be observed. In this situation, the proximal margin of LES is located at or below the pressure inversion point. However in patients with hiatal hernia, high pressure zone is separated into two zones with the proximal corresponding to the LES and the distal to the diaphragmatic indentation (Fig. 3). In this case, the LES becomes situated above the pressure inversion point. Thus, when there are two definite high-pressure zones as occurs in overt hiatal hernia, it is not difficult to make the diagnosis of a hiatal hernia, but this finding cannot always be demonstrated and the distance between the two high-pressure zones changes with degree of respiration unless the hiatal hernia is sufficiently large. Therefore, using esophageal manometry in diagnosing small hiatal hernias would neither be accurate nor practical.
Fig. 3.
Conventional manometric identification of a hiatal hernia. In a pressure tracing over the distal end of the esophagus generated by the station pull-through technique; the high pressure zone is separated into two zones with the proximal zone corresponding to the lower esophageal sphincter and the distal zone corresponding to the diaphragmatic indentation. The respiratory pressure inversion point (PIP) is sometimes observed twice. The numbers on the upper part of the tracing indicate the distance in centimeters from the nostril.
To overcome the effect of respiration during pull-through method in order to correctly detect the separation of high-pressure zones and delineate the location of the respiratory inversion point, the intraluminal pressure would have to be observed in real-time and this has become feasible with high resolution manometry. High resolution manometry is equipped with 32 or 36 circumferentially sensitive manometric pressure sensors closely spaced at 1 cm intervals and enables simultaneous luminal pressure monitoring and pressure topography plotting of the entire esophagus from the pharynx to the stomach in realtime.47,48
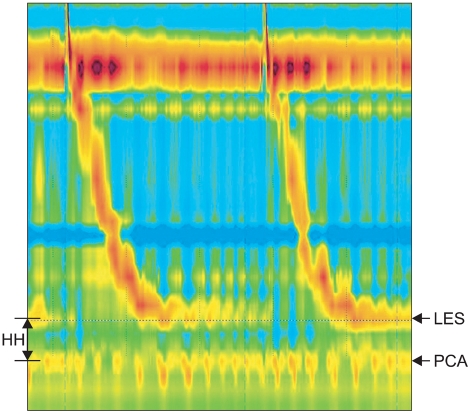
With high resolution manometry, GEJ pressure pattern can be classified into three types (type I, II, and III) based on the extent of separation between the LES and the crural diaphragm; type III is further classified as type IIIa and IIIb.31 In type I, which is normal, there is a complete overlap between the LES and the crural diaphragm both during inspiration and expiration with resultant increase in GEJ pressure. The superimposed peaks move downward during inspiration. In this type, the respiratory inversion point is located at the proximal margin of the GEJ. In type II, there is a small but noticeable separation (1 to 2 cm) between the LES and the crural diaphragm, especially during inspiration, but the lowest pressure between the separated peaks is still higher than the gastric pressure. In this case, the pressure inversion point in typically situated within the GEJ at the proximal border of the crural diaphragm. Type III is diagnostic of hiatal hernia and downward movement of the LES during inspiration is no longer seen. In type IIIa, the separation of two peaks made by the LES and the crural diaphragm is evident with the distance between them being >2 cm (Fig. 4). In this situation, the pressure inversion point lies proximal to the crural diaphragm. Type IIIb is characterized by indistinguishable or absence of the pressure peak made by the crural diaphragm due the presence of a very large hiatal hernia, with resultant shifting of the pressure inversion point to above the peak made by the LES. Thus, high resolution manometry with topographic plotting has opened the door to accurately and objectively detecting and diagnosing hiatal hernias <2 cm, which had not been possible neither through radiographic, endoscopic nor conventional manometric assessment. The advent of high resolution manometry has added new dimension to our knowledge on the esophageal physiology, and the long disputed role of hiatal hernia on GERD is sure to be fully unraveled in the near future.
Fig. 4.
High resolution manometric identification of a hiatal hernia. A hiatal hernia (HH) can be identified between the two high-pressure zones of the lower esophageal sphincter (LES) and the diaphragmatic indentation (PCA).
CLINICAL SIGNIFICANCE OF HIATAL HERNIA
Many studies have demonstrated that hiatal hernia is closely related to reflux symptoms, reflux esophagitis, Barrett's esophagus and esophageal adenocarcinoma. Patients with hiatal hernia are significantly more likely to present with GERD symptoms than those without hiatal hernia, and symptomatic GERD patients are more likely to have hiatal hernias compared to those without symptoms.49-51 In addition, studies from the Western countries showed that over half of patients (50% to 94%) with reflux esophagitis that was diagnosed either endoscopically or radiologically had concomitant hiatal hernias, whereas the prevalence of hiatal hernia was lower (13% to 59%) in the control subjects.34,50-54 Furthermore, both the presence and size of the hiatal hernia were important, with majority of patients with severe esophagitis having hiatal hernia.50,54-57 This association between hiatal hernia and reflux esophagitis could also be observed in the studies from Eastern countries where the prevalence of GERD and reflux esophagitis is considered to be lower.58-62 As for Barrett's esophagus, it is strongly related to hiatal hernia,63 with hiatal hernia being present in a great majority (72% to 96%) of patients with Barrett's esophagus.51,64 The prevalence of hiatal hernia also increased with the length of Barrett's esophagus and the size of hiatal hernia was larger in those with Barrett's esophagus compared to those without.64 Moreover, it was shown that development and progression to Barrett's esophagus with high-grade dysplasia or adenocarcinoma was significantly and independently related to the size of hiatal hernia,63,65 and that the presence of hiatal hernia more than doubled the risk of developing adenocarcinoma of the esophagus and gastric cardia.66 In a population-based case-control study, the risk of esophageal adenocarcinoma increased even up to 8-fold when both hiatal hernia and reflux symptoms were present.67
These above mentioned associations between hiatal hernia and reflux symptoms, reflux esophagitis, Barrett's esophagus and esophageal adenocarcinoma are largely due to the disruption of many of the antireflux mechanisms that leads to increased esophageal acid exposure. These impairments can largely be divided into incompetence of GEJ, relationship with tLESRs, and compromise of esophageal acid clearance.
1. Incompetence of gastroesophageal junction
As mentioned above, GEJ is an anatomically complex area consisting of the intrinsic LES, the crural diaphragm, the intraabdominal location of the LES, the acute angle of His and the phrenoesophageal ligaments/membrane. Among these components, the intrinsic LES and the crural diaphragm are the two major components of the "two-sphincter hypothesis" in which both the LES (smooth muscle) and the crural diaphragm (striated muscle) are considered to serve as sphincters.8-10 Under normal circumstances, these two sphincters are superimposed, and the tonically contracted LES and the extrinsic compression by the diaphragm create a resting LES pressure of 10 to 45 mm Hg, which is sufficiently higher than the naturally occurring positive pressure gradient of about 5 mm Hg across the GEJ to prevent reflux of gastric contents into the esophagus. The contribution of the crural diaphragm in increasing the LES pressure can be appreciated in many instances. During manometry, there is a rhythmic increase in the resting LES pressure of about 5 to 10 mm Hg with its pressure being highest at the end of inspiration and lowest at the end of expiration. The LES pressure also has been shown to augment in direct proportion to the depth of inspiration, often reaching 50 to 150 mm Hg with deep inspiration.9 These increases in the LES pressure are largely attributable to the contraction of the diaphragmatic crus. The role of crural diaphragm in increasing the LES pressure becomes particularly more pronounced during periods of elevated intra-abdominal pressures such as coughing, abdominal straining and abdominal compression.68,69 However in hiatal hernia, the LES is displaced proximally, and this leads to spatial separation of the intrinsic LES from the extrinsic compression by the diaphragm, which results in decreased resting LES pressure in proportion to the size of the hiatal hernia.6,68,70 The proximal displacement of the LES in hiatal hernia further compromises the competence of the GEJ due to the loss of the intra-abdominal segment of the LES, because the intra-abdominal location of the LES per se is considered to serve as a valve by being exposed to the positive abdominal pressure.71,72 Loss of the acute angle of His in hiatal hernia is also thought to add to the incompetence of GEJ possibly due to the compromise of the flap valve effect of the structure. Due to the laxity of the phrenoesophageal ligaments/membrane and widening of the esophageal hiatus, the cross-sectional area of the GEJ opening increases as has been demonstrated in a study using modified barostat technique.7 This increase in the luminal cross-sectional area of the opening allows larger amount of refluxate to be regurgitated, and facilitates reflux of not only gas but also liquids and solids which have higher viscosity.
2. Relationship with transient lower esophageal sphincter relaxations
In addition to the aforementioned factors related to the incompetence of GEJ, hiatal hernia also seems to be associated to some degree with tLESRs. In brief, tLESR is a phenomenon mediated via vagal pathways that occurs in response to distended gastric cavity, especially the fundus, by food or gas.14 It is well known that tLESRs are differentiated from swallow-induced LES relaxations in several ways: tLESRs occur independently of swallowing, are unaccompanied by esophageal peristalsis, persist for longer duration (>10 seconds) than swallow-induced LES relaxations, are accompanied by inhibition of the crural diaphragm and are associated with distal esophageal shortening by contraction of its longitudinal muscle.14,73,74 tLESR is a normal occurrence during digestion and a physiological mechanism of belching. In a study that employed gas insufflations to distend the stomach in order to see its effect on reflux and tLESRs in GERD patients, it was demonstrated that the frequency of tLESRs increased in direct proportion to the size of the hiatal hernia, plausibly due to the reduced threshold for eliciting tLESRs.75 However, this finding could not be observed in another study in which the frequency of tLESRs and the proportion tLESRs that translated into true acid reflux was shown to be comparable in those with hiatal hernia to those without.76 Nevertheless, those with hiatal hernia did have greater number of reflux episodes associated with low LES pressure, swallow-induced LES relaxations, and straining during periods of low LES pressure.76 The conflicting results from these two studies seems to have resulted from differences in their study design and thus, further investigation is needed to clarify the the role of tLESRs in patients with hiatal hernia.
3. Compromise of esophageal acid clearance
In addition to the increase in the frequency of reflux and volume of refluxate, there is also a delay in esophageal acid clearance among those with hiatal hernia,77,78 which all promote the increase in esophageal acid exposure.79 In patients with hiatal hernia, a hernia sac (or phrenic ampulla) that is formed by the upper margin of the LES and the diaphragmatic indentation is present. After an episode of reflux, the refluxate is cleared from the esophagus by secondary esophageal peristalsis into the stomach but a small amount of acid gets entrapped in this sac. Subsequently, the retained fluid regurgitates into the esophagus during swallow-induced LES relaxation. Since this sequence can be repeated, it can markedly prolong esophageal acid clearance. This finding has been demonstrated and supported by several studies. According to a study that employed simultaneous esophageal pH recordings and radionuclide studies after instilling acid into the esophagus, it was demonstrated that each swallow resulted in the clearance of acid with restoration to normal esophageal pH in subjects without hiatal hernia. However, subjects with hiatal hernia showed a biphasic response: initial swallow-induced reflux followed by acid clearance with resultant initial drop in pH followed by restoration of pH towards normal, consistent with aforementioned sequence.77 In another study using concurrent videofluoroscopy and manometry, complete esophageal emptying without retrograde flow was seen in 86% of test swallows in normal subjects (maximal phrenic ampullary length <2 cm), in 66% of swallows in subjects with reducing hiatal hernia and in 32% of swallows in those with non-reducing hiatal hernia; swallow-induced reflux being evident and more pronounced in those with non-reducing hiatal hernia than in those with reducing hiatal hernia.78
Another factor that could further compromise esophageal acid clearance in hiatal hernia is defective esophageal peristalsis;70,80 patients with larger hiatal hernia presented with less effective peristalsis, shown by decreased distal esophageal peristaltic amplitude, than those with small or no hiatal hernia.70 However, there still are controversies as to whether peristaltic dysfunction is primarily due to hiatal hernia itself or secondary to ensuing reflux esophagitis.
TREATMENT
The presence of hiatal hernia per se is not an indication for treatment, and therapy should be given to those with symptoms attributable to this condition. Since GERD is the most common clinical manifestation in patients with hiatal hernia, lifestyle modifications (weight loss, elevation of head of bed, etc.) should be encouraged and medications (antacids, prokinetics, H2-receptor antagonists and proton pump inhibitors) should first be prescribed to the symptomatic patients, with acid suppression using proton pump inhibitors being the cornerstone of therapy.81,82
Unlike paraesophageal hiatal hernias that need surgical repair even in the absence of symptoms due to its potential for development of complications such as bleeding, incarceration, obstruction and perforation,83-85 isolated sliding hiatal hernias itself usually do not require surgical treatment. However, surgical therapy (either open or laparoscopic) could be given to hiatal hernia patients with severe and refractory GERD symptoms based on the generally accepted indications for antireflux surgery: poor compliance to long-term medical therapy, requirement of high doses of drugs and young patients wishing to avoid lifetime medical treatment.86 In addition, hiatal hernia patients can also resort to surgery if they develop complications such as recurrent bleeding, ulcerations, strictures, etc. Surgical management should encompass both the correction of hiatal hernia by restoring the intra-abdominal esophagus and reconstructing the diaphragmatic hiatus, and reinforcement of the LES by antireflux procedure with Nissen fundoplication being the most frequently employed measure. Although several endoscopic techniques have been introduced to manage GERD, these techniques are unlikely to be effective in those with hiatal hernia since underlying anatomic abnormality cannot be corrected.
SUMMARY AND PERSPECTIVES
After having swerved to the right and to the left during the past decades regarding the association between hiatal hernia and GERD, we are finally on the path again with "two-sphincter hypothesis" sitting behind the steering wheel. We now understand that the underlying pathophysiology of GERD related to hiatal hernia is multifactorial, and acknowledge the close relationship between hiatal hernia and reflux esophagitis, Barrett's esophagus and esophageal adenocarcinoma. There still are controversies as to which is the initiating factor that sustains the esophagitis-hernia complex: hiatal hernia or reflux esophagitis. It could remain as a baffling question as it still is with the long-disputed argument "what came first, the chicken or the egg?" Meanwhile, to make further progress in our understanding on hiatal hernia, accurately diagnosing hiatal hernia would be fundamental, and this is now possible with the introduction of high resolution manometry. High-resolution manometry seems to hold the key to future studies on hiatal hernia and it is beckoning us to cast the probe deep into the esophagus. With the help of this magnificent apparatus that enables simultaneous luminal pressure monitoring and pressure topography plotting of the entire esophagus from the pharynx to the stomach in real-time, the clinical significance of hiatal hernias measuring less than 2 cm in length, which has long been considered to be insignificant, will also be elucidated in the near future.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Allison PR. Reflux esophagitis, sliding hiatal hernia, and the anatomy of repair. Surg Gynecol Obstet. 1951;92:419–431. [PubMed] [Google Scholar]
- 2.Cohen S, Harris LD. Does hiatus hernia affect competence of the gastroesophageal sphincter? N Engl J Med. 1971;284:1053–1056. doi: 10.1056/NEJM197105132841902. [DOI] [PubMed] [Google Scholar]
- 3.Cohen S, Harris LD. The lower esophageal sphincter. Gastroenterology. 1972;63:1066–1073. [PubMed] [Google Scholar]
- 4.Dodds WJ, Dent J, Hogan WJ, et al. Mechanisms of gastroesophageal reflux in patients with reflux esophagitis. N Engl J Med. 1982;307:1547–1552. doi: 10.1056/NEJM198212163072503. [DOI] [PubMed] [Google Scholar]
- 5.Holloway RH, Dent J. Pathophysiology of gastroesophageal reflux: lower esophageal sphincter dysfunction in gastroesophageal reflux disease. Gastroenterol Clin North Am. 1990;19:517–535. [PubMed] [Google Scholar]
- 6.Sloan S, Rademaker AW, Kahrilas PJ. Determinants of gastroesophageal junction incompetence: hiatal hernia, lower esophageal sphincter, or both? Ann Intern Med. 1992;117:977–982. doi: 10.7326/0003-4819-117-12-977. [DOI] [PubMed] [Google Scholar]
- 7.Pandolfino JE, Shi G, Trueworthy B, Kahrilas PJ. Esophagogastric junction opening during relaxation distinguishes nonhernia reflux patients, hernia patients, and normal subjects. Gastroenterology. 2003;125:1018–1024. doi: 10.1016/s0016-5085(03)01210-1. [DOI] [PubMed] [Google Scholar]
- 8.Boyle JT, Altschuler SM, Nixon TE, Tuchman DN, Pack AI, Cohen S. Role of the diaphragm in the genesis of lower esophageal sphincter pressure in the cat. Gastroenterology. 1985;88:723–730. doi: 10.1016/0016-5085(85)90143-x. [DOI] [PubMed] [Google Scholar]
- 9.Mittal RK, Rochester DF, McCallum RW. Electrical and mechanical activity in the human lower esophageal sphincter during diaphragmatic contraction. J Clin Invest. 1988;81:1182–1189. doi: 10.1172/JCI113433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mittal RK, Rochester DF, McCallum RW. Sphincteric action of the diaphragm during a relaxed lower esophageal sphincter in humans. Am J Physiol. 1989;256(1 Pt 1):G139–G144. doi: 10.1152/ajpgi.1989.256.1.G139. [DOI] [PubMed] [Google Scholar]
- 11.Dent J, Dodds WJ, Friedman RH, et al. Mechanism of gastroesophageal reflux in recumbent asymptomatic human subjects. J Clin Invest. 1980;65:256–267. doi: 10.1172/JCI109667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goyal RK, Rattan S. Genesis of basal sphincter pressure: effect of tetrodotoxin on lower esophageal sphincter pressure in opossum in vivo. Gastroenterology. 1976;71:62–67. [PubMed] [Google Scholar]
- 13.Barham CP, Gotley DC, Mills A, Alderson D. Precipitating causes of acid reflux episodes in ambulant patients with gastro-oesophageal reflux disease. Gut. 1995;36:505–510. doi: 10.1136/gut.36.4.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mittal RK, Holloway RH, Penagini R, Blackshaw LA, Dent J. Transient lower esophageal sphincter relaxation. Gastroenterology. 1995;109:601–610. doi: 10.1016/0016-5085(95)90351-8. [DOI] [PubMed] [Google Scholar]
- 15.Marchand P. The anatomy of esophageal hiatus of the diaphragm and the pathogenesis of hiatus herniation. J Thorac Surg. 1959;37:81–92. [PubMed] [Google Scholar]
- 16.Lin S, Brasseur JG, Pouderoux P, Kahrilas PJ. The phrenic ampulla: distal esophagus or potential hiatal hernia? Am J Physiol. 1995;268(2 Pt 1):G320–G327. doi: 10.1152/ajpgi.1995.268.2.G320. [DOI] [PubMed] [Google Scholar]
- 17.Bombeck CT, Dillard DH, Nyhus LM. Muscular anatomy of the gastroesophageal junction and role of phrenoesophageal ligament; autopsy study of sphincter mechanism. Ann Surg. 1966;164:643–654. doi: 10.1097/00000658-196610000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eliska O. Phreno-oesophageal membrane and its role in the development of hiatal hernia. Acta Anat (Basel) 1973;86:137–150. [PubMed] [Google Scholar]
- 19.Edmundowicz SA, Clouse RE. Shortening of the esophagus in response to swallowing. Am J Physiol. 1991;260(3 Pt 1):G512–G516. doi: 10.1152/ajpgi.1991.260.3.G512. [DOI] [PubMed] [Google Scholar]
- 20.Wolf BS. Sliding hiatal hernia: the need for redefinition. Am J Roentgenol Radium Ther Nucl Med. 1973;117:231–247. doi: 10.2214/ajr.117.2.231. [DOI] [PubMed] [Google Scholar]
- 21.Friedland GW. Progress in radiology: historical review of the changing concepts of lower esophageal anatomy: 430 B.C.--1977. AJR Am J Roentgenol. 1978;131:373–378. doi: 10.2214/ajr.131.3.373. [DOI] [PubMed] [Google Scholar]
- 22.Smith AB, Dickerman RD, McGuire CS, East JW, McConathy WJ, Pearson HF. Pressure-overload-induced sliding hiatal hernia in power athletes. J Clin Gastroenterol. 1999;28:352–354. doi: 10.1097/00004836-199906000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Rigler LG, Eneboe JB. Incidence of hiatus hernia in pregnant women and its significance. J Thoracic Surg. 1935;4:262–268. [Google Scholar]
- 24.Goodman RM, Wooley CF, Ruppert RD, Freimanis AK. A possible genetic role in esophageal hiatus hernia. J Hered. 1969;60:71–74. doi: 10.1093/oxfordjournals.jhered.a107936. [DOI] [PubMed] [Google Scholar]
- 25.Carré IJ, Johnston BT, Thomas PS, Morrison PJ. Familial hiatal hernia in a large five generation family confirming true autosomal dominant inheritance. Gut. 1999;45:649–652. doi: 10.1136/gut.45.5.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Christensen J. Hypothesis: how might oesophagitis cause hiatus hernia? Neurogastroenterol Motil. 2003;15:567–569. doi: 10.1046/j.1365-2982.2003.00436.x. [DOI] [PubMed] [Google Scholar]
- 27.Paterson WG, Kolyn DM. Esophageal shortening induced by short-term intraluminal acid perfusion in opossum: a cause for hiatus hernia? Gastroenterology. 1994;107:1736–1740. doi: 10.1016/0016-5085(94)90814-1. [DOI] [PubMed] [Google Scholar]
- 28.Dunne DP, Paterson WG. Acid-induced esophageal shortening in humans: a cause of hiatus hernia? Can J Gastroenterol. 2000;14:847–850. doi: 10.1155/2000/438981. [DOI] [PubMed] [Google Scholar]
- 29.Mittal RK. Hiatal hernia: myth or reality? Am J Med. 1997;103(5A):33S–39S. doi: 10.1016/s0002-9343(97)00318-5. [DOI] [PubMed] [Google Scholar]
- 30.Dodds WJ. 1976 Walter B. Cannon Lecture: current concepts of esophageal motor function--clinical implications for radiology. AJR Am J Roentgenol. 1977;128:549–561. doi: 10.2214/ajr.128.4.549. [DOI] [PubMed] [Google Scholar]
- 31.Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol. 2008;22:601–616. doi: 10.1016/j.bpg.2007.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kahrilas PJ. Hiatus hernia causes reflux: fact or fiction? Gullet. 1993;3(1 Suppl):21–30. [Google Scholar]
- 33.Ott DJ, Gelfand DW, Chen YM, Wu WC, Munitz HA. Predictive relationship of hiatal hernia to reflux esophagitis. Gastrointest Radiol. 1985;10:317–320. doi: 10.1007/BF01893120. [DOI] [PubMed] [Google Scholar]
- 34.Ott DJ, Gelfand DW, Wu WC, Castell DO. Esophagogastric region and its rings. AJR Am J Roentgenol. 1984;142:281–287. doi: 10.2214/ajr.142.2.281. [DOI] [PubMed] [Google Scholar]
- 35.Wallner B, Sylvan A, Janunger KG. Endoscopic assessment of the "Z-line" (squamocolumnar junction) appearance: reproducibility of the ZAP classification among endoscopists. Gastrointest Endosc. 2002;55:65–69. doi: 10.1067/mge.2002.119876. [DOI] [PubMed] [Google Scholar]
- 36.McClave SA, Boyce HW, Jr, Gottfried MR. Early diagnosis of columnar-lined esophagus: a new endoscopic diagnostic criterion. Gastrointest Endosc. 1987;33:413–416. doi: 10.1016/s0016-5107(87)71676-9. [DOI] [PubMed] [Google Scholar]
- 37.Boyce HW. Endoscopic definitions of esophagogastric junction regional anatomy. Gastrointest Endosc. 2000;51:586–592. doi: 10.1016/s0016-5107(00)70295-1. [DOI] [PubMed] [Google Scholar]
- 38.Choi DW, Oh SN, Baek SJ, et al. Endoscopically observed lower esophageal capillary patterns. Korean J Intern Med. 2002;17:245–248. doi: 10.3904/kjim.2002.17.4.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de Carvalho CA. Sur l'angio-architecture veineuse de la zone de transition oesophago-gastrique et son interpretation functionnelle. Acta Anat (Basel) 1966;64:125–162. [Google Scholar]
- 40.Spence RA. The venous anatomy of the lower oesophagus in normal subjects and in patients with varices: an image analysis study. Br J Surg. 1984;71:739–744. doi: 10.1002/bjs.1800711002. [DOI] [PubMed] [Google Scholar]
- 41.Vianna A, Hayes PC, Moscoso G, et al. Normal venous circulation of the gastroesophageal junction: a route to understanding varices. Gastroenterology. 1987;93:876–889. doi: 10.1016/0016-5085(87)90453-7. [DOI] [PubMed] [Google Scholar]
- 42.Hoshihara Y. Complications of gastroesophageal reflux disease. 2. Endoscopic diagnosis of Barrett esophagus--can Barrett esophagus be diagnosed by endoscopic observation alone? Nippon Naika Gakkai Zasshi. 2000;89:85–90. [PubMed] [Google Scholar]
- 43.Bytzer P. Information bias in endoscopic assessment. Am J Gastroenterol. 2007;102:1585–1587. doi: 10.1111/j.1572-0241.2006.00911.x. [DOI] [PubMed] [Google Scholar]
- 44.Johnson LF, DeMeester TR, Haggitt RC. Endoscopic signs for gastroesophageal reflux objectively evaluated. Gastrointest Endosc. 1976;22:151–155. doi: 10.1016/s0016-5107(76)73731-3. [DOI] [PubMed] [Google Scholar]
- 45.Hill LD, Kozarek RA, Kraemer SJ, et al. The gastroesophageal flap valve: in vitro and in vivo observations. Gastrointest Endosc. 1996;44:541–547. doi: 10.1016/s0016-5107(96)70006-8. [DOI] [PubMed] [Google Scholar]
- 46.Seltman AK, Kahrilas PJ, Chang EY, Mori M, Hunter JG, Jobe BA. Endoscopic measurement of cardia circumference as an indicator of GERD. Gastrointest Endosc. 2006;63:22–31. doi: 10.1016/j.gie.2005.07.030. [DOI] [PubMed] [Google Scholar]
- 47.Kahrilas PJ, Sifrim D. High-resolution manometry and impedance-pH/manometry: valuable tools in clinical and investigational esophagology. Gastroenterology. 2008;135:756–769. doi: 10.1053/j.gastro.2008.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fox MR, Bredenoord AJ. Oesophageal high-resolution manometry: moving from research into clinical practice. Gut. 2008;57:405–423. doi: 10.1136/gut.2007.127993. [DOI] [PubMed] [Google Scholar]
- 49.Stål P, Lindberg G, Ost A, Iwarzon M, Seensalu R. Gastroesophageal reflux in healthy subjects: significance of endoscopic findings, histology, age, and sex. Scand J Gastroenterol. 1999;34:121–128. doi: 10.1080/00365529950172952. [DOI] [PubMed] [Google Scholar]
- 50.Petersen H, Johannessen T, Sandvik AK, et al. Relationship between endoscopic hiatus hernia and gastroesophageal reflux symptoms. Scand J Gastroenterol. 1991;26:921–926. doi: 10.3109/00365529108996243. [DOI] [PubMed] [Google Scholar]
- 51.Zagari RM, Fuccio L, Wallander MA, et al. Gastro-oesophageal reflux symptoms, oesophagitis and Barrett's oesophagus in the general population: the Loiano-Monghidoro study. Gut. 2008;57:1354–1359. doi: 10.1136/gut.2007.145177. [DOI] [PubMed] [Google Scholar]
- 52.Ronkainen J, Aro P, Storskrubb T, et al. High prevalence of gastroesophageal reflux symptoms and esophagitis with or without symptoms in the general adult Swedish population: a Kalixanda study report. Scand J Gastroenterol. 2005;40:275–285. doi: 10.1080/00365520510011579. [DOI] [PubMed] [Google Scholar]
- 53.Wright RA, Hurwitz AL. Relationship of hiatal hernia to endoscopically proved reflux esophagitis. Dig Dis Sci. 1979;24:311–313. doi: 10.1007/BF01296546. [DOI] [PubMed] [Google Scholar]
- 54.Berstad A, Weberg R, Frøyshov Larsen I, Hoel B, Hauer-Jensen M. Relationship of hiatus hernia to reflux oesophagitis: a prospective study of coincidence, using endoscopy. Scand J Gastroenterol. 1986;21:55–58. doi: 10.3109/00365528609034622. [DOI] [PubMed] [Google Scholar]
- 55.Sontag SJ, Schnell TG, Miller TQ, et al. The importance of hiatal hernia in reflux esophagitis compared with lower esophageal sphincter pressure or smoking. J Clin Gastroenterol. 1991;13:628–643. doi: 10.1097/00004836-199112000-00006. [DOI] [PubMed] [Google Scholar]
- 56.Jones MP, Sloan SS, Rabine JC, Ebert CC, Huang CF, Kahrilas PJ. Hiatal hernia size is the dominant determinant of esophagitis presence and severity in gastroesophageal reflux disease. Am J Gastroenterol. 2001;96:1711–1717. doi: 10.1111/j.1572-0241.2001.03926.x. [DOI] [PubMed] [Google Scholar]
- 57.Massey BT. Acid clearance, hiatal hernia size and oesophagitis: redress the egress regress. Neurogastroenterol Motil. 2002;14:607–609. doi: 10.1046/j.1365-2982.2002.00372.x. [DOI] [PubMed] [Google Scholar]
- 58.Kang JY, Ho KY. Different prevalences of reflux oesophagitis and hiatus hernia among dyspeptic patients in England and Singapore. Eur J Gastroenterol Hepatol. 1999;11:845–850. doi: 10.1097/00042737-199908000-00006. [DOI] [PubMed] [Google Scholar]
- 59.Yeom JS, Park HJ, Cho JS, Lee SI, Park IS. Reflux esophagitis and its relationship to hiatal hernia. J Korean Med Sci. 1999;14:253–256. doi: 10.3346/jkms.1999.14.3.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hyun JJ, Kim JH, Yeon JE, et al. Short segment hiatal hernia: is it a clinically significant entity? J Neurogastroenterol Motil. 2010;16:35–39. doi: 10.5056/jnm.2010.16.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kang JY, Tay HH, Yap I, Guan R, Lim KP, Math MV. Low frequency of endoscopic esophagitis in Asian patients. J Clin Gastroenterol. 1993;16:70–73. doi: 10.1097/00004836-199301000-00019. [DOI] [PubMed] [Google Scholar]
- 62.Kim JH, Hwang JK, Kim J, et al. Endoscopic findings around the gastroesophageal junction: an experience from a tertiary hospital in Korea. Korean J Intern Med. 2008;23:127–133. doi: 10.3904/kjim.2008.23.3.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Weston AP, Badr AS, Hassanein RS. Prospective multivariate analysis of clinical, endoscopic, and histological factors predictive of the development of Barrett's multifocal high-grade dysplasia or adenocarcinoma. Am J Gastroenterol. 1999;94:3413–3419. doi: 10.1111/j.1572-0241.1999.01602.x. [DOI] [PubMed] [Google Scholar]
- 64.Cameron AJ. Barrett's esophagus: prevalence and size of hiatal hernia. Am J Gastroenterol. 1999;94:2054–2059. doi: 10.1111/j.1572-0241.1999.01277.x. [DOI] [PubMed] [Google Scholar]
- 65.Avidan B, Sonnenberg A, Schnell TG, Chejfec G, Metz A, Sontag SJ. Hiatal hernia size, Barrett's length, and severity of acid reflux are all risk factors for esophageal adenocarcinoma. Am J Gastroenterol. 2002;97:1930–1936. doi: 10.1111/j.1572-0241.2002.05902.x. [DOI] [PubMed] [Google Scholar]
- 66.Chow WH, Finkle WD, McLaughlin JK, Frankl H, Ziel HK, Fraumeni JF., Jr The relation of gastroesophageal reflux disease and its treatment to adenocarcinomas of the esophagus and gastric cardia. JAMA. 1995;274:474–477. [PubMed] [Google Scholar]
- 67.Wu AH, Tseng CC, Bernstein L. Hiatal hernia, reflux symptoms, body size, and risk of esophageal and gastric adenocarcinoma. Cancer. 2003;98:940–948. doi: 10.1002/cncr.11568. [DOI] [PubMed] [Google Scholar]
- 68.Kahrilas PJ, Lin S, Chen J, Manka M. The effect of hiatus hernia on gastro-oesophageal junction pressure. Gut. 1999;44:476–482. doi: 10.1136/gut.44.4.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mittal RK, Fisher M, McCallum RW, Rochester DF, Dent J, Sluss J. Human lower esophageal sphincter pressure response to increased intra-abdominal pressure. Am J Physiol. 1990;258(4 Pt 1):G624–G630. doi: 10.1152/ajpgi.1990.258.4.G624. [DOI] [PubMed] [Google Scholar]
- 70.Patti MG, Goldberg HI, Arcerito M, Bortolasi L, Tong J, Way LW. Hiatal hernia size affects lower esophageal sphincter function, esophageal acid exposure, and the degree of mucosal injury. Am J Surg. 1996;171:182–186. doi: 10.1016/S0002-9610(99)80096-8. [DOI] [PubMed] [Google Scholar]
- 71.DeMeester TR, Lafontaine E, Joelsson BE, et al. Relationship of a hiatal hernia to the function of the body of the esophagus and the gastroesophageal junction. J Thorac Cardiovasc Surg. 1981;82:547–558. [PubMed] [Google Scholar]
- 72.Fein M, Ritter MP, DeMeester TR, et al. Role of the lower esophageal sphincter and hiatal hernia in the pathogenesis of gastroesophageal reflux disease. J Gastrointest Surg. 1999;3:405–410. doi: 10.1016/s1091-255x(99)80057-2. [DOI] [PubMed] [Google Scholar]
- 73.Pandolfino JE, Zhang QG, Ghosh SK, Han A, Boniquit C, Kahrilas PJ. Transient lower esophageal sphincter relaxations and reflux: mechanistic analysis using concurrent fluoroscopy and high-resolution manometry. Gastroenterology. 2006;131:1725–1733. doi: 10.1053/j.gastro.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 74.Holloway RH, Penagini R, Ireland AC. Criteria for objective definition of transient lower esophageal sphincter relaxation. Am J Physiol. 1995;268(1 Pt 1):G128–G133. doi: 10.1152/ajpgi.1995.268.1.G128. [DOI] [PubMed] [Google Scholar]
- 75.Kahrilas PJ, Shi G, Manka M, Joehl RJ. Increased frequency of transient lower esophageal sphincter relaxation induced by gastric distention in reflux patients with hiatal hernia. Gastroenterology. 2000;118:688–695. doi: 10.1016/s0016-5085(00)70138-7. [DOI] [PubMed] [Google Scholar]
- 76.van Herwaarden MA, Samsom M, Smout AJ. Excess gastroesophageal reflux in patients with hiatus hernia is caused by mechanisms other than transient LES relaxations. Gastroenterology. 2000;119:1439–1446. doi: 10.1053/gast.2000.20191. [DOI] [PubMed] [Google Scholar]
- 77.Mittal RK, Lange RC, McCallum RW. Identification and mechanism of delayed esophageal acid clearance in subjects with hiatus hernia. Gastroenterology. 1987;92:130–135. doi: 10.1016/0016-5085(87)90849-3. [DOI] [PubMed] [Google Scholar]
- 78.Sloan S, Kahrilas PJ. Impairment of esophageal emptying with hiatal hernia. Gastroenterology. 1991;100:596–605. doi: 10.1016/0016-5085(91)80003-r. [DOI] [PubMed] [Google Scholar]
- 79.Jones MP, Sloan SS, Jovanovic B, Kahrilas PJ. Impaired egress rather than increased access: an important independent predictor of erosive oesophagitis. Neurogastroenterol Motil. 2002;14:625–631. doi: 10.1046/j.1365-2982.2002.00362.x. [DOI] [PubMed] [Google Scholar]
- 80.Kahrilas PJ, Dodds WJ, Hogan WJ. Effect of peristaltic dysfunction on esophageal volume clearance. Gastroenterology. 1988;94:73–80. doi: 10.1016/0016-5085(88)90612-9. [DOI] [PubMed] [Google Scholar]
- 81.Bak YT. Management strategies for gastroesophageal reflux disease. J Gastroenterol Hepatol. 2004;19(Suppl 3):S49–S53. doi: 10.1111/j.1440-1746.2004.03587.x. [DOI] [PubMed] [Google Scholar]
- 82.Fock KM, Talley NJ, Fass R, et al. Asia-Pacific consensus on the management of gastroesophageal reflux disease: update. J Gastroenterol Hepatol. 2008;23:8–22. doi: 10.1111/j.1440-1746.2007.05249.x. [DOI] [PubMed] [Google Scholar]
- 83.Menguy R. Surgical management of large paraesophageal hernia with complete intrathoracic stomach. World J Surg. 1988;12:415–422. doi: 10.1007/BF01655690. [DOI] [PubMed] [Google Scholar]
- 84.Walther B, DeMeester TR, Lafontaine E, Courtney JV, Little AG, Skinner DB. Effect of paraesophageal hernia on sphincter function and its implication on surgical therapy. Am J Surg. 1984;147:111–116. doi: 10.1016/0002-9610(84)90043-6. [DOI] [PubMed] [Google Scholar]
- 85.Oddsdóttir M. Paraesophageal hernia. Surg Clin North Am. 2000;80:1243–1252. doi: 10.1016/s0039-6109(05)70222-x. [DOI] [PubMed] [Google Scholar]
- 86.Mattioli S, Lugaresi ML, Pierluigi M, Di Simone MP, D'Ovidio F. Review article: indications for anti-reflux surgery in gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2003;17(Suppl 2):60–67. doi: 10.1046/j.1365-2036.17.s2.4.x. [DOI] [PubMed] [Google Scholar]