Abstract
Background/Aims
Percutaneous endoscopic gastrostomy (PEG) has been widely used for patients with swallowing dysfunction. However, its beneficial effects in the treatment of gastroesophageal reflux (GER) are controversial. The aim of this study was to evaluate the effect of PEG on the prevention of GER in patients with nasogastric tube (NGT) feeding.
Methods
Continuous 24-hour pH monitoring was performed prospectively in 21 patients receiving NGT feeding before and 7.3±2.2 days after PEG placement to compare the severity of GER.
Results
We studied 21 patients with a mean age of 59.8±14.1 years. The mean duration of NGT placement was 5.8±5.4 months. The causes of swallowing dysfunction included cerebral infarction, cerebral hemorrhage and other central nervous system (CNS) lesions. When all of the patients were considered, there were no significant differences in reflux parameters after PEG placement compared to before PEG placement. However, all seven patients who had preexisting GER showed significant improvement (p<0.05) of the reflux parameters, including the frequency of acid reflux, duration of acid reflux, total time with a pH below 4.0 and the fraction of time with a pH below 4.0, after PEG placement.
Conclusions
PEG might prevent GER in patients receiving NGT feeding, especially in those patients with GER.
Keywords: Percutaneous endoscopic gastrostomy, Gastroesophageal reflux, Continuous 24-hour pH monitoring
INTRODUCTION
Percutaneous endoscopic gastrostomy (PEG) and nasogastric tube (NGT) feeding are the preferred methods of enteral nutrition in patients with dysphagia. Enteral feeding with NGT is associated with nasal mucosal ulceration, laryngopharyngeal damage and discomfort. Furthermore, there is evidence showing that the presence of a NGT is associated with an increased risk of gastroesophageal reflux (GER) and aspiration pneumonia.1
Although the incidence of gastroesophageal reflux and aspiration pneumonia has not been established, 720 postmortem cases with neurological abnormalities were investigated and reported that the use of NGT feeding increased the risk of aspiration by six fold.2 In 1980, PEG was introduced by Ponsky and Gauderer for the patients with poor oral nutrition, for more than one month that had preserved gastrointestinal (GI) function. Complications associated with PEG placement have included wound infections, clogging, leakage, hemorrhage, ileus, tube malfunction, and peritonitis.3
Aspiration is the most feared and potentially serious complication of enteral nutrition. However, there is controversy about whether PEG can prevent GER and aspiration pneumonia. Some reported that PEG tubes were associated with a significantly reduced rate of regurgitation compared to NGT and that the aspiration rate was reduced in patients with PEG compared to NGT.4 On the other hand, others reported that, in children, PEG reduced the lower esophageal sphincter tone and as a result increased GER significantly. We designed a prospective study to determine whether converting NGT to PEG might be a successful strategy to reduce the risk of GER and aspiration in at risk patients.
MATERIALS AND METHODS
1. Patient selection
From May 2005 to December 2005, total 21 bed-ridden patients with dysphagia due to stroke and other neurological abnormalities were admitted to the Kyung Hee University Medical Center. Having a NGT was the criterion for inclusion in this study (Table 1). The study was reviewed and approved by local Institutional Review Board. Because all patients were bedridden with neurologic dysfunction, we explained our purpose of the procedure to the protectors of participants and provided the written informed consent. Moreover, we got data use agreements from them.
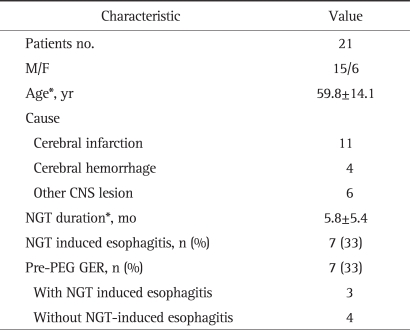
Table 1.
Baseline Clinical Characteristics of the Patients
*Data are expressed as means±SD.
CNS, central nervous system; NGT, nasogastric tube; PEG, percutaneous endoscopic gastrostomy; GER, gastroesophageal reflux.
2. Study design
Continuous 24-hour pH monitoring was performed prospectively in 21 patients with a nasogastric tube before and 7.3±2.2 days after PEG placement to compare the severity of GER.
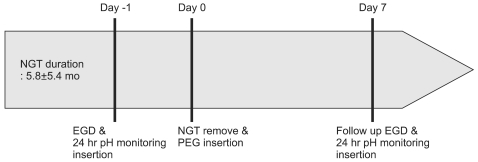
On 1 day before PEG insertion, the NGT were temporally removed after eight hours of fasting. An esophagogastroduodenoscopy (EGD) was performed to evaluate for lesions of the esophagus, stomach and duodenum and to assess the location of the gastroesophageal junction. After the EGD, the NGT were inserted again and continuous 24-hour esophageal pH monitoring was performed. Then the PEG tube was inserted. On the seventh day after PEG tube insertion, continuous 24-hour esophageal pH monitoring was performed again and the extent of the GER was compared (Fig. 1).
Fig. 1.
A schematic plot of study design.
EGD, esophagogastroduodenoscopy; NGT, nasogastric tube.
The PEG (Ponsky Pull PEG kit; Bard, Bellerica, MA, USA) tube was inserted by the pull-through method previously described by Gauderer et al.5 The measurement of esophageal pH was performed with monocrystalline antimony pH electrode catheter (Simline MU; Medtronic A/S, Copenhagen, Denmark) connected with a recorder (Digitrapper pH400; Medtronics Functional Diagnostic A/S, Skovlunde, Denmark). The probe was inserted through the nasal cavity and the distal end was located 5 cm above of the gastroesophageal junction which was estimated by withdrawing the pH catheter from the stomach until there was an abrupt rise in pH. The probes were calibrated in standard buffer solutions at pH 7 and pH 1 before and after each study.
Proton-pump-inhibitor, H2 receptor blockers, prokinetic agents and other drugs that can affect acidity of stomach and GI motility were discontinued seven days before the study.
In this study, acid reflux was defined as a pH below 4 and GER was defined as when the total acid reflux time exceeded five percent of the total monitoring time. The presence of GER and the GER indices were compared between pre-PEG and post-PEG placement by EGD and 24-hour pH monitoring. The reflux indices included: 1) the number of reflux episodes, 2) the number of long durations of acid reflux, 3) the total time the pH was below 4.0, and 4) the fraction of the time the pH was below 4.0.
NGT induced esophagitis was defined as when esophageal mucosal erosion or ulcer was detected in EGD and the lesion was largely due to NGT in this study.
3. Statistical analysis
Data is expressed as the mean±standard deviation. For the analysis of improvement of the GER the Wilcoxon signed rank test with SPSS 11.0 software (SPSS Inc., Chicago, IL, USA) was used. p-values of less than 5% were regarded as significant.
RESULTS
Among 21 patients, 15 males and 6 females were entered into the study; the mean age was 59.8±14.1. The mean duration of NGT placement was 5.8±5.4 months. The causes of swallowing dysfunction were cerebral infarction (n=11), cerebral hemorrhage (n=4), and other CNS lesions (n=6).
On the pre-PEG EGD and 24-hour pH monitoring tests, NGT induced esophagitis was noted in seven (33%) and pre-PEG GER was noted in seven (33%). Among the seven patients that had NGT-induced esophagitis, only three patients had GER. On the other hand, among 14 patients without NGT-induced esophagitis, four patients had GER (Table 1). There was no significant correlation between NGT-induced esophagitis and GER.
There were no aspiration events such as pneumonia during the 7±2 days after changing to PEG.
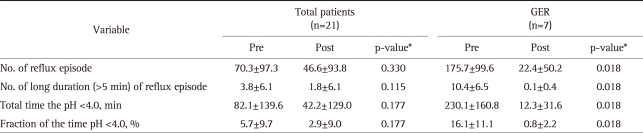
1. Changes of reflux indices
The pre-PEG with post-PEG reflux indices was compared: acid reflux frequency (70.3±97.3 vs 46.6±93.8; p=0.330), long duration of acid reflux (3.8±6.1 vs 1.8±6.1; p=0.115), total time the pH was below 4.0 (82.1±139.6 vs 42.2±129.0; p=0.177) and the fraction of time the pH was below 4.0 (5.7±9.7 vs 2.9±9.0; p=0.177). There were no significant differences in the reflux parameters between the before and after measurements with regard to PEG placement among all patients (p>0.05) (Table 2).
Table 2.
Changes in Reflux Indices Pre-PEG and Post-PEG
Data are expressed as means±SD.
PEG, percutaneous endoscopic gastrostomy; GER, gastroesophageal reflux; No., number.
*p-values are calculated using the Wilcoxon signed rank test.
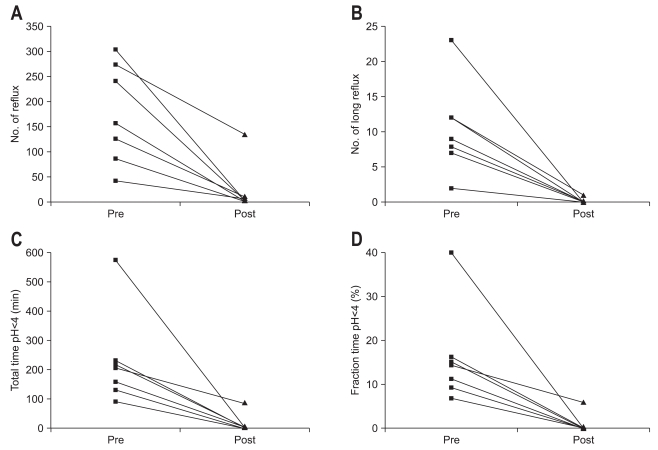
Although, all seven patients that had preexisting GER showed significant improvement of the reflux parameters after PEG placement (p<0.05); including the frequency of acid reflux (175.7±99.6 vs 22.4±50.2; p=0.018), long duration of acid reflux (10.4±6.5 vs 0.1±0.4; p=0.018), total time the pH was below 4.0 (230.1±160.8 vs 12.3±31.6; p=0.018) and the fraction of time the pH was below 4.0 (16.1±11.1 vs 0.8±2.2; p=0.018) (Table 2, Fig. 2), only two out of 14 patients without preexisting GER developed reflux after PEG placement.
Fig. 2.
Comparison of reflux indices in seven patients with gastroesophageal reflux (GER): pre-percutaneous endoscopic gastrostomy (PEG) and post-PEG. (A) Number of reflux episodes. (B) Number of long-duration acid reflux episodes. (C) Total time with a pH below 4.0. (D) Fraction of time with a pH below 4.0; all reflux indices are significantly decreased after PEG placement replaced nasogastric tube (NGT) feeding (p<0.05).
DISCUSSION
Enteral feeding with NGT or PEG is used for patients with dysphagia caused by multiple etiologies frequently associated with neurological abnormalities or head and neck cancers. Such methods of feeding help decrease morbidity and mortality due to malnutrition. However, there are complications that can occur with tube feeding. The most serious complication of enteral tube feeding is aspiration pneumonia. The mortality from aspiration pneumonia associated with tube feeding in the intensive care unit has been reported to be 17% to 62%.6,7
The major risk factors for aspiration are a previous history of aspiration, altered level of consciousness, anatomic abnormality, gastrointestinal disease, neuromuscular disease, severe vomiting or GER, prolonged supine position, and retained gastric material.8 In addition, intermittent feeding of large amounts, poor oral hygiene and advanced age may also increase the risk.
A number of interventions have been proposed to prevent aspiration and GER: maintaining elevation of the head-of-the bed >30 degrees, changing hyper-osmolar formulas to iso-osmolar formulas to prevent delayed gastric emptying, using prokinetics, pump-controlled slow drip formulas, and restriction of night feeding.8 Some reported that early PEG tube feeding was superior to NGT feeding among 30 patients with acute dysphagia due to stroke in a randomized prospective comparison,9 and some reported that among 122 chronically ill patients, the use of PEG was associated with improved survival and was associated with a lower incidence of aspiration.10 However, others have reported that PEG does not affect GER;11,12 and some have reported that it aggravates GER.13 Therefore, the efficacy and risks of these two types of enteral feedings continue to be debated.
Lee et al.14 compared esophageal acidity in 13 brain-injured patients before and after changing NGT to PEG feeding and reported that none of the reflux indices were changed. In our study, seven patients (33%) among 21 patients with NGT had significant GER according to the 24-hour pH monitoring. Among all patients (n=21), after change to PEG, there was no significant improvement in the GER; consistent with the findings reported by Lee et al.14 However, in the seven patients that had GER before changing to PEG, the GER resolved in six patients and the remaining one patient showed improvement of the reflux indices; these differences were statistically significant. These findings suggest that the change to PEG can help prevent GER and aspiration in patients receiving NGT feeding and having GER.
Some reported that in critically ill patients on mechanical ventilation in the intensive care unit, the mean frequency of regurgitation per patient was 31.3% and the mean frequency of aspiration per patient was 22.1%.4 They showed that even though all episodes of GER did not induce aspiration, most of them were associated with aspiration. Given these findings, the decreasing tendency for GER and improved reflux indices after changing to PEG suggests that PEG is a reasonable approach to preventing aspiration.
This prospective study was limited by the small sample size (n=21). In addition, it was not possible to examine the long term effects of PEG because of the short follow-up period. Among the interventions associated complications, and the post PEG complications, GER and aspiration pneumonia have been reported with variable frequency ranging from 8% to 56%.15,16 These variations can be attributed to the differences in the follow-up periods. A long follow-up duration was associated with an increasing tendency for GER.17 As mentioned above, the short follow-up period is the shortcoming of this study. If we had had a long term follow-up of esophageal pH monitoring for GER, the result would have gotten more strength. However, longer examination for these bed-ridden patients was actually impossible. In fact, the physiologic changes of feeding will affect more to the amount of acid reflux to esophagus than the periods of feeding time. So we compared the difference of acid reflux between before and after changing to PEG in same patient, even though the follow-up periods were short. Therefore, these results would provide clinical evidence for the superiority of PEG in prevention of GER among patients who had GER with NGT. Many factors are associated with the pathogenesis of aspiration pneumonia such as host immunity, GER, and toxicity of pathogens. The results of this study show that PEG could prevent aspiration pneumonia by preventing GER. A large scale and long term follow-up study is now needed to confirm these findings and further define the effect of PEG on the morbidity and mortality of patients from aspiration pneumonia.
All patients that were enrolled in this study were bed-ridden and had maintained elevation of the head-of-the bed by more than 45 degrees from the start of feeding to one hour after finishing feeding. However, the personal differences such as body mass index and clinical findings such as a cough might have increased the abdominal pressure and GER. Although the amount and method of feeding before and after changing to PEG was controlled and the same for each patient, the feeding calories (500 to 1,800 kcal) and the frequencies (3 to 4 times) differed among the patients. Some studies have reported that the form and location of PEG can also affect the development of GER.18,19 In this study, all PEG placements were located at the anterior wall side of the mid-body of the stomach.
In summary, seven patients (33%) among 21 patients with NGT had significant GER based on 24-hour pH monitoring; among these patients GER resolved in six and the reflux indices improved in all seven after changing from NGT feeding to PEG feeding. In conclusion, PEG feeding did not aggravate GER in patients receiving NGT feeding; changing enteral feeding to PEG feeding might prevent GER, especially in patients that had GER with NGT feedings.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Gomes GF, Pisani JC, Macedo ED, Campos AC. The nasogastric feeding tube as a risk factor for aspiration and aspiration pneumonia. Curr Opin Clin Nutr Metab Care. 2003;6:327–333. doi: 10.1097/01.mco.0000068970.34812.8b. [DOI] [PubMed] [Google Scholar]
- 2.Olivares L, Segovia A, Revuelta R. Tube feeding and lethal aspiration in neurological patients: a review of 720 autopsy cases. Stroke. 1974;5:654–657. doi: 10.1161/01.str.5.5.654. [DOI] [PubMed] [Google Scholar]
- 3.McClave SA, Ritchie CS. The role of endoscopically placed feeding or decompression tubes. Gastroenterol Clin North Am. 2006;35:83–100. doi: 10.1016/j.gtc.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 4.McClave SA, Lukan JK, Stefater JA, et al. Poor validity of residual volumes as a marker for risk of aspiration in critically ill patients. Crit Care Med. 2005;33:324–330. doi: 10.1097/01.ccm.0000153413.46627.3a. [DOI] [PubMed] [Google Scholar]
- 5.Gauderer MW, Ponsky JL, Izant RJ., Jr Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15:872–875. doi: 10.1016/s0022-3468(80)80296-x. [DOI] [PubMed] [Google Scholar]
- 6.DiSario JA, Foutch PG, Sanowski RA. Poor results with percutaneous endoscopic jejunostomy. Gastrointest Endosc. 1990;36:257–260. doi: 10.1016/s0016-5107(90)71018-8. [DOI] [PubMed] [Google Scholar]
- 7.Kirby DF, Delegge MH, Fleming CR. American Gastroenterological Association technical review on tube feeding for enteral nutrition. Gastroenterology. 1995;108:1282–1301. doi: 10.1016/0016-5085(95)90231-7. [DOI] [PubMed] [Google Scholar]
- 8.McClave SA, DeMeo MT, DeLegge MH, et al. North American Summit on Aspiration in the Critically Ill Patient: consensus statement. JPEN J Parenter Enteral Nutr. 2002;26(6 Suppl):S80–S85. doi: 10.1177/014860710202600613. [DOI] [PubMed] [Google Scholar]
- 9.Norton B, Homer-Ward M, Donnelly MT, Long RG, Holmes GK. A randomized prospective comparison of percutaneous endoscopic gastrostomy and nasogastric tube feeding after acute dysphagic stroke. BMJ. 1996;312:13–16. doi: 10.1136/bmj.312.7022.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dwolatzky T, Berezovski S, Friedmann R, et al. A prospective comparison of the use of nasogastric and percutaneous endoscopic gastrostomy tubes for long-term enteral feeding in older people. Clin Nutr. 2001;20:535–540. doi: 10.1054/clnu.2001.0489. [DOI] [PubMed] [Google Scholar]
- 11.Samuel M, Holmes K. Quantitative and qualitative analysis of gastroesophageal reflux after percutaneous endoscopic gastrostomy. J Pediatr Surg. 2002;37:256–261. doi: 10.1053/jpsu.2002.30267. [DOI] [PubMed] [Google Scholar]
- 12.Launay V, Gottrand F, Turck D, Michaud L, Ategbo S, Farriaux JP. Percutaneous endoscopic gastrostomy in children: influence on gastroesophageal reflux. Pediatrics. 1996;97:726–728. [PubMed] [Google Scholar]
- 13.Grunow JE, al-Hafidh A, Tunell WP. Gastroesophageal reflux following percutaneous endoscopic gastrostomy in children. J Pediatr Surg. 1989;24:42–44. doi: 10.1016/s0022-3468(89)80298-2. [DOI] [PubMed] [Google Scholar]
- 14.Lee JK, Jang YS, Kim MK, et al. The changes in esophageal acidity during percutaneous endoscopic gastrostomy feeding. Korean J Gastrointest Motil. 2003;9:12–17. [Google Scholar]
- 15.Sanders DS, Carter MJ, D'Silva J, McAlindon ME, Willemse PJ, Bardham KD. Percutaneous endoscopic gastrostomy: a prospective analysis of hospital support required and complications following discharge to the community. Eur J Clin Nutr. 2001;55:610–614. doi: 10.1038/sj.ejcn.1601197. [DOI] [PubMed] [Google Scholar]
- 16.Ciocon JO, Silverstone FA, Graver LM, Foley CJ. Tube feedings in elderly patients: indications, benefits, and complications. Arch Intern Med. 1988;148:429–433. [PubMed] [Google Scholar]
- 17.Nishiwaki S, Araki H, Goto N, et al. Clinical analysis of gastroesophageal reflux after PEG. Gastrointest Endosc. 2006;64:890–896. doi: 10.1016/j.gie.2006.06.086. [DOI] [PubMed] [Google Scholar]
- 18.Seekri IK, Rescorla FJ, Canal DF, Zollinger TW, Saywell R, Jr, Grosfeld JL. Lesser curvature gastrostomy reduces the incidence of postoperative gastroesophageal reflux. J Pediatr Surg. 1991;26:982–984. doi: 10.1016/0022-3468(91)90847-m. [DOI] [PubMed] [Google Scholar]
- 19.Razeghi S, Lang T, Behrens R. Influence of percutaneous endoscopic gastrostomy on gastroesophageal reflux: a prospective study in 68 children. J Pediatr Gastroenterol Nutr. 2002;35:27–30. doi: 10.1097/00005176-200207000-00007. [DOI] [PubMed] [Google Scholar]