Abstract
Cholangioscopy not only enables the direct visualization of the biliary tree, but also allows for forceps biopsy to diagnosis early cholangiocarcinoma. Recently, some reports have suggested the clinical usefulness of direct peroral cholangioscopy (POC) using an ultra-slim endoscope with a standard endoscopic unit by a single operator. Enhanced endoscopy, such as narrow band imaging (NBI), can be helpful for detecting early neoplasia in the gastrointestinal tract and is easily applicable during direct POC. A 63-year-old woman with acute cholangitis had persistent bile duct dilation on the left hepatic duct after common bile duct stone removal and clinical improvement. We performed direct POC with NBI using an ultra-slim upper endoscope to examine the strictured segment. NBI examination showed an irregular surface and polypoid structure with tumor vessels. Target biopsy under direct endoscopic visualization was performed, and adenocarcinoma was documented. The patient underwent an extended left hepatectomy, and the resected specimen showed early bile duct cancer confined to the ductal mucosa.
Keywords: Early bile duct cancer, Direct peroral cholangioscopy, Narrow band imaging
INTRODUCTION
The early diagnosis of cholangiocarcinoma (CC) is important because surgery is the only curative treatment. Cholangioscopy not only enables direct visualization of the biliary tree, but also allows forceps biopsy to diagnosis early CC.1-3 However, the clinical use of percutaneous3 or peroral cholangioscopy using a "mother-baby scope"1,4,5 is limited because of its invasiveness or inconvenience. Recently, some reports have indicated the clinical usefulness of direct peroral cholangioscopy (POC) using an ultra-slim endoscope5,6 with a standard endoscopic unit by a single operator. Enhanced endoscopy, such as narrow band imaging (NBI), can be helpful for detecting early neoplasia in the gastrointestinal tract.7-9 NBI is easily applied during direct POC using an ultra-slim endoscope. We report a case of early bile duct cancer diagnosed at direct POC with NBI using an ultra-slim endoscope.
CASE REPORT
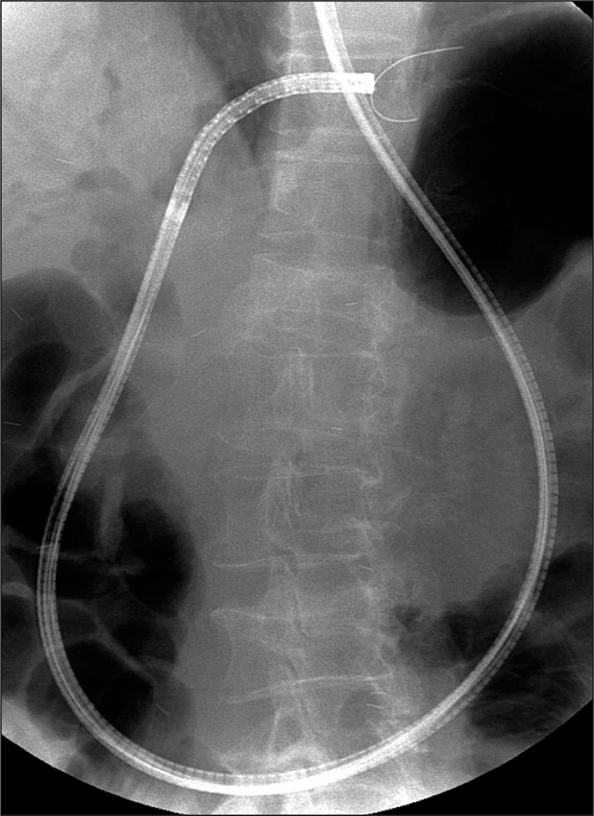
A 63-year-old woman was admitted to the emergency room with right upper quadrant pain with fever over 2 days. Laboratory findings were as follows: white blood cell count 14,400/µL, total/direct bilirubin 2.89/2.09 mg/dL, gamma-glutamyl-transpeptidase 1,470 IU/L, and alkaline phosphatase 1,334 IU/L. Abdominal computed tomography showed bile duct dilation and high density stone on ampullary portion (Fig. 1). After the removal of the impacted stone on the ampullary orifice and nasobiliary drainage, clinical symptoms were improved. On the 3rd hospital day, we performed endoscopic retrograde cholangiography (ERC) to evaluate for remnant stones. ERC showed no remnant stone but duct dilation on left hepatic duct and short segment stricture on the orifice (Fig. 2).
Fig. 1.
Abdominal computed tomography showing abnormal stricture of the intrahepatic duct.
Fig. 2.
Cholangiogram showing stricture of the left hepatic duct with proximal dilatation.
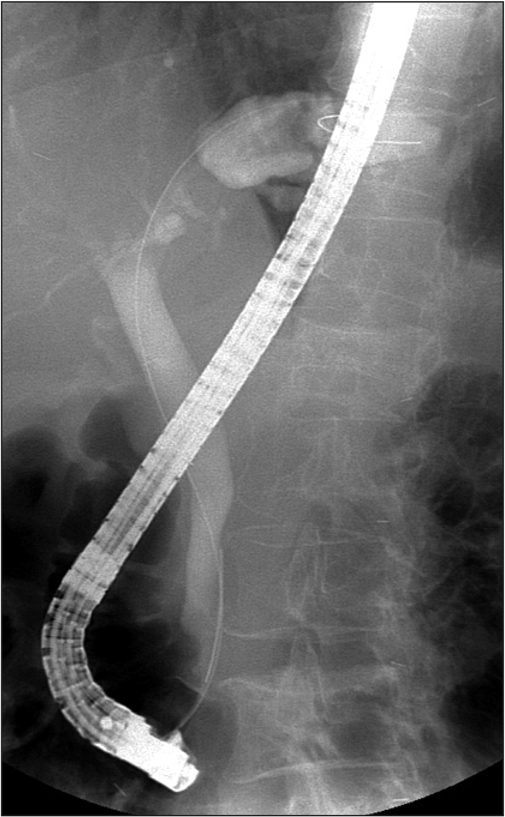
We examined the stricture under endoscopic visualization using intraductal balloon-guided direct POC using an ultra-slim upper endoscope (GIF-XP260N; Olympus, Tokyo, Japan) as our previous report.6 The endoscope was inserted into the ampulla of Vater. After advancing the 5 F balloon catheter (MTW Endoskopie, Wesel, Germany) through the stricture via the guidewire, the balloon was inflated to anchor it inside the left hepatic duct. The endoscope was advanced over the balloon catheter into the proximal bile duct using the ropeway method (Fig. 3). We observed the stricture under white light (WL) and NBI (Evis Lucera 260 System; Olympus) examination.
Fig. 3.
Fluoroscopy image of the direct peroral cholangioscopy with an ultra-slim endoscope showing the advance of the endoscope into the left intrahepatic duct.
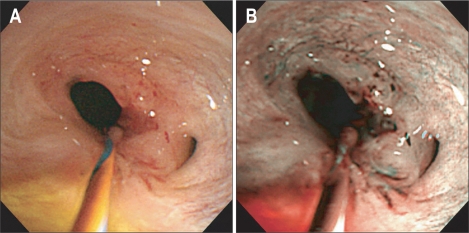
The WL examination showed ill-defined hyperemia at the stricture site. NBI showed better contrast than did the WL examination, with a well-defined margin and prominent, thickened vascular markings (Fig. 4). We performed a target biopsy of the lesion using biopsy forceps (FB-19K-1; Olympus). Histopathological examination revealed a well-differentiated adenocarcinoma. The patient underwent an extended left hepatectomy. Histopathologically, the resected specimen showed focal papillary adenocarcinoma confined to the ductal mucosa (Fig. 5).
Fig. 4.
White light (A) and narrow-band imaging (B) of the stricture in the left hepatic duct.
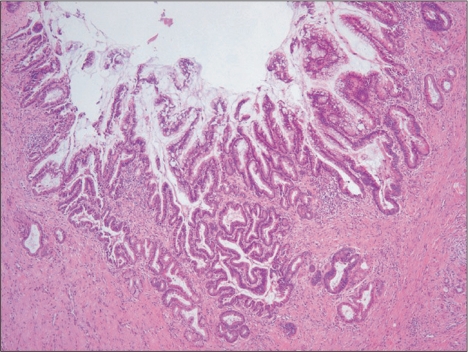
Fig. 5.
Histopathologically, the resected specimen shows focal papillary adenocarcinoma confined to the mucosa (H&E stain, ×20).
DISCUSSION
Cholangioscopy provides advantages over endoscopic retrograde cholangiopancreatography (ERCP) for the diagnosis of lesions in the bile duct. Visual information from the endoscope disclose characteristics of filling defects or stricture site, which enables us not only to differentiate between benign and malignant strictures, but also to apply treatment or to biopsy in some cases.1 Direct POC with ultra-slim upper endoscope has been proposed as a potential solutions for the direct visual examination of the biliary tree.5 In this case, there were persistent bile duct stricture after stone removal. At present, there are some limitation of the cholangiogram or cytology study including brush cytology to differentiate between benign and malignancy. We evaluated the stricture site by using the direct POC with ultra-slim endocope. It provides white light image of the lesion and NBI, thus enable to target biopsy for proper diagnosis.
The recently introduced NBI is helpful for diagnosing early gastrointestinal neoplasia due to its ability to yield clear images of the surface structure and microvessels.7-9 Although it has not become established in biliary disease, Itoi et al.10 reported the usefulness of NBI for the diagnosis of biliary disease using POC with a mother-baby system and video cholangioscope (CHF-B260; Olympus), which may increase the detectability of biliary-tract disease, even of minute lesions. However, POC with the mother-baby scope system is cumbersome, which limits its clinical use. Direct POC using an ultra-slim endoscope can be performed by a single endoscopist; it is not only provide superior endoscopic images with a standard endoscopy unit, but NBI can also be performed easily during the endoscope examination.5,6,11,12
Although it was difficult to see an objective difference between the WL and NBI examinations in this case, the NBI examination suggested a malignant stricture rather than a benign one because it showed abnormal superficial mucosal change, with irregularly dilated vessels. Based on this finding, we could target a biopsy of the suspicious lesion precisely.
Our procedure has several limitations. It needs specialized accessories, such as an intraductal balloon, and a skilled endoscopist. In addition, optical magnification for enhancing NBI cannot be used with the existing ultra-slim endoscope and it is time consuming to clear the bile duct because bile on the NBI is recognized as a reddish fluid.1
In conclusion, our case demonstrated the possibility of detecting early bile duct cancer using NBI under direct POC.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Shim CS, Neuhaus H, Tamada K. Direct cholangioscopy. Endoscopy. 2003;35:752–758. doi: 10.1055/s-2003-41580. [DOI] [PubMed] [Google Scholar]
- 2.Fukuda Y, Tsuyuguchi T, Sakai Y, Tsuchiya S, Saisyo H. Diagnostic utility of peroral cholangioscopy for various bile-duct lesions. Gastrointest Endosc. 2005;62:374–382. doi: 10.1016/j.gie.2005.04.032. [DOI] [PubMed] [Google Scholar]
- 3.Nimura Y, Shionoya S, Hayakawa N, Kamiya J, Kondo S, Yasui A. Value of percutaneous transhepatic cholangioscopy (PTCS) Surg Endosc. 1988;2:213–219. doi: 10.1007/BF00705323. [DOI] [PubMed] [Google Scholar]
- 4.Bogardus ST, Hanan I, Ruchim M, Goldberg MJ. "Mother-baby" biliary endoscopy: the University of Chicago experience. Am J Gastroenterol. 1996;91:105–110. [PubMed] [Google Scholar]
- 5.Larghi A, Waxman I. Endoscopic direct cholangioscopy by using an ultra-slim upper endoscope: a feasibility study. Gastrointest Endosc. 2006;63:853–857. doi: 10.1016/j.gie.2005.07.050. [DOI] [PubMed] [Google Scholar]
- 6.Moon JH, Ko BM, Choi HJ, et al. Intraductal balloon-guided direct peroral cholangioscopy with an ultraslim upper endoscope (with videos) Gastrointest Endosc. 2009;70:297–302. doi: 10.1016/j.gie.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 7.Machida H, Sano Y, Hamamoto Y, et al. Narrow-band imaging in the diagnosis of colorectal mucosal lesions: a pilot study. Endoscopy. 2004;36:1094–1098. doi: 10.1055/s-2004-826040. [DOI] [PubMed] [Google Scholar]
- 8.Nakayoshi T, Tajiri H, Matsuda K, Kaise M, Ikegami M, Sasaki H. Magnifying endoscopy combined with narrow band imaging system for early gastric cancer: correlation of vascular pattern with histopathology (including video) Endoscopy. 2004;36:1080–1084. doi: 10.1055/s-2004-825961. [DOI] [PubMed] [Google Scholar]
- 9.Kara MA, Ennahachi M, Fockens P, ten Kate FJ, Bergman JJ. Detection and classification of the mucosal and vascular patterns (mucosal morphology) in Barrett's esophagus by using narrow band imaging. Gastrointest Endosc. 2006;64:155–166. doi: 10.1016/j.gie.2005.11.049. [DOI] [PubMed] [Google Scholar]
- 10.Itoi T, Sofuni A, Itokawa F, et al. Peroral cholangioscopic diagnosis of biliary-tract diseases by using narrow-band imaging (with videos) Gastrointest Endosc. 2007;66:730–736. doi: 10.1016/j.gie.2007.02.056. [DOI] [PubMed] [Google Scholar]
- 11.Brauer BC, Fukami N, Chen YK. Direct cholangioscopy with narrow-band imaging, chromoendoscopy, and argon plasma coagulation of intraductal papillary mucinous neoplasm of the bile duct (with videos) Gastrointest Endosc. 2008;67:574–576. doi: 10.1016/j.gie.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 12.Choi HJ, Moon JH, Ko BM, et al. Overtube-balloon-assisted direct peroral cholangioscopy by using an ultra-slim upper endoscope (with videos) Gastrointest Endosc. 2009;69:935–940. doi: 10.1016/j.gie.2008.08.043. [DOI] [PubMed] [Google Scholar]