Abstract
Dieulafoy disease is an uncommon cause of gastrointestinal system bleeding. Although the exact cause is not known, it is characterized by bleeding from abnormal submucosal vessels. There are many methods for diagnosis and treatment. In this case, a patient with a long-time undiagnosed stomach Dieulafoy lesion had a surgical resection. During the postoperative period the patient was discharged without any complication.
Key words: Dieulafoy lesion, Gastrointestinal system bleeding
Case Report
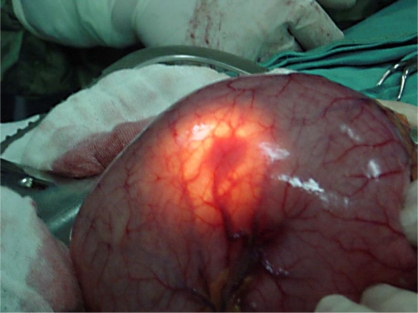
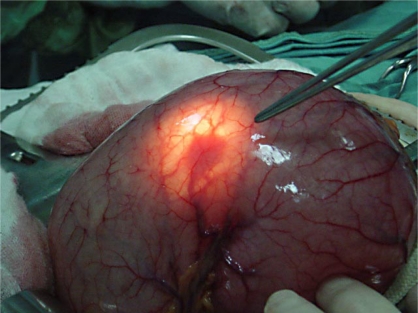
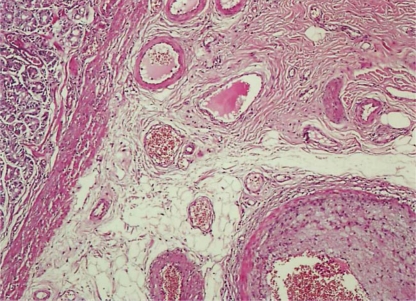
A 75-year-old woman with melena-like defecations over a three- to four-day period on a monthly basis had been evaluated at different hospitals for gastrointestinal system hemorrhage during a period of 16 years. She had been given over 100 units of blood because of low hematocrit. The patient had been suffering from bronchial asthma for 46 years and had been using levothyroxine because of total thyroidectomy 15 years earlier. Her last upper gastrointestinal system endoscopy had shown an ulceration in 2 cm bouffant floor with vessels visible in the crater proximal to the corpoantral junction in the greater curvature between the piles. Physical examination was normal except for her melena at rectal examination. Blood pressure and pulse were stable. Hematocrit was 24.4% and hemoglobin 7.77 g/dl. The erythrocyte sedimentation rate was 47 mm in the 1st hour (normal value 0–20 mm/h); gastrin was 124 pg/ml (normal value 0–150 pg/ml). After 5 units of blood transfusion, hematocrit was 33.5% and hemoglobin 10.4 g/dl. Abdominal CT scans were normal, and her tentative diagnosis were arteriovenous malformation or gastrointestinal system stromal tumor. At exploration during surgery, there was no gross pathology or free fluid in the abdomen. Intraoperative gastroscopy showed a smooth-surfaced vascular lesion with a diameter of 1.5 cm located at the front surface of the corpoantral junction (fig. 1); a wedge resection was performed. Macroscopic examination revealed that there was a 1 cm diameter, crater-shaped mucosal erosion lined by a vascular structure (fig. 2). After histopathologic examination, it was reported as a submucosal dilated, thrombotic vascular structure (fig. 3). The patient's melena stopped and her hemoglobin and hematocrit values reverted to normal ranges. She was discharged healthy from hospital after the 5th postoperative day and re-examined during the 1st, 3rd and 6th months after discharge. During 7 months follow-up no recurrence of symptoms was detected.
Fig. 1.
Intraoperative illuminational view of Dieulafoy lesion.
Fig. 2.
Intraoperative illuminational view of Dieulafoy lesion.
Fig. 3.
Microscopic view of Dieulafoy lesion.
Discussion
Dieulafoy lesion was first described by Gallard in 1884 as ‘millier aneurysm of stomach’. At 1898 Dieulafoy described this as ‘l'exulceratio simple’. This encompasses approximately 4% of upper gastrointestinal system hemorrhage and can cause, for example, hematemesis, hemotochezia and melena.
Dieulafoy lesion is seen infrequently and can result in life-threatening situations [1]. The lesion is generally seen in the stomach and especially within 6 cm of the gastroesophageal junction in the lesser curvature. It occurs at all ages but generally after the age of 60. Male gender is dominant. One third of cases occur outside the stomach, the duedonum and colon being commonly affected. The lesion can rupture spontaneously and without known cause, resulting in gross hemorrhage. The hemorrhage frequently comes from the submucosal eroded artery at the proximal stomach [2]. Endoscopy is used frequently in diagnosis, but unfortunately because of size and hidden location, diagnosis is difficult. The typical endoscopic view is of an artery that is located in a solitary, round mucosal defect [1]. There is no peripheral ulceration. Angiography may also be useful at diagnosis [2, 3].
The treatment modalities are various [4]. Endoscopic band ligation is prevalent [5]. Xavier et al. successfully performed band ligations in all Dieulafoy patients in their series [5]. Ertekin et al. also performed a band ligation in a 25-year-old woman with Dieulafoy lesion [6]. Parra-Blanco et al. used endoscopic hemoclips in their treatment of Dieulafoy lesion and stated that endoscopy must first be undertaken [7]. Alshumrani et al. treated a 77-year-old man with endovascular embolisation [2]. Baettig et al. found that 20 patients (95%) treated with endoscopic norepinephrine and polidocanol for Dieulafoy hemorrhage had no recurrence [8]. Yilmaz et al. successfully treated 26 of 28 (92.8%) such patients by endoscopic injection sclerotherapy [9].
Surgery is an option for treatment: coagulation or vessel ligation, proximal gastric resection and wedge resection may be used. When using wedge resection, diagnosis may be confirmed with the help of pathologic-anatomic examination. In our case we chose curative surgery by wedge resection because there was chronic hemorrhaging lesion and the diagnosis was not certain.
Conclusion
Dieulafoy lesion is seen infrequently, may cause severe gastrointestinal system hemorrhage and can be difficult to diagnose. Endoscopy or surgery can be curative after diagnosis.
References
- 1.Apiratpracha W, Ho JK, Powell JJ, Yoshida EM. Acute lower gastrointestinal bleeding from a dieulafoy lesion proximal to the anorectal junction post-orthotopic liver transplant. World J Gastroenterol. 2006;12:7547–7548. doi: 10.3748/wjg.v12.i46.7547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alshumrani G, Almuaikeel M. Angiographic findings and endovascular embolization in Dieulafoy disease: a case report and literature review. Diagn Interv Radiol. 2006;12:151–154. [PubMed] [Google Scholar]
- 3.Lee KS, Moon YJ, Lee SI, Park IS, Sohn SK, Yu JS, Kie JH. A case of bleeding from the Dieulafoy lesion of the jejunum. Yonsei Med J. 1997;38:240–244. doi: 10.3349/ymj.1997.38.4.240. [DOI] [PubMed] [Google Scholar]
- 4.Veldhuyzen van Zanten SJ, Bartelsman JF, Schipper ME, Tytgat GN. Recurrent massive haematemesis from Dieulafoy vascular malformations – a review of 101 cases. Gut. 1986;27:213–222. doi: 10.1136/gut.27.2.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xavier S. Band ligation of Dieulafoy lesions. Indian J Gastroenterol. 2005;24:114–115. [PubMed] [Google Scholar]
- 6.Ertekin C, Barbaros U, Taviloglu K, Güloglu R, Kasoglu A. Dieulafoy's lesion of esophagus. Surg Endosc. 2002;16:219. doi: 10.1007/s00464-001-4204-z. [DOI] [PubMed] [Google Scholar]
- 7.Parra-Blanco A, Takahashi H, Mendez Jerez PV, Kojima T, Aksoz K, Kirihara K, Pamerin J, Takekuma Y, Fujita R. Endoscopic management of Dieulafoy lesions of the stomach: a case study of 26 patients. Endoscopy. 1997;29:834–839. doi: 10.1055/s-2007-1004317. [DOI] [PubMed] [Google Scholar]
- 8.Baettig B, Haecki W, Lammer F, Jost R. Dieulafoy's disease: endoscopic treatment and follow up. Gut. 1993;34:1418–1421. doi: 10.1136/gut.34.10.1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yilmaz M, Ozütemiz O, Karasu Z, Ersöz G, Günsar F, Batur Y, Aydin A, Tekesin O, Yönetici N, Ilter T. Endoscopic injection therapy of bleeding Dieulafoy lesion of the stomach. Hepatogastroenterology. 2005;52:1622–1625. [PubMed] [Google Scholar]