Abstract
An understanding of spatial patterns of health facility use allows a more informed approach to the modelling of catchment populations. In the absence of patient use data, an intuitive and commonly used approach to the delineation of facility catchment areas is Thiessen polygons. This study presents a series of methods by which the validity of these assumptions can be tested directly and hence the suitability of a Thiessen polygon catchment model explicitly assessed. These methods are applied to paediatric out-patient origin data from a sample of 81 government health facilities in four districts of Kenya. A geographical information system was used to predict the location of the catchment boundary along a transect between each pair of neighbouring facilities based on patient choice patterns. The mean location of boundaries between facilities of different type was found to be significantly displaced from the Thiessen boundary towards the lower-order facility. The affect of distance on within-catchment utilization rate was assessed by using exclusion buffers to remove the effect of neighbouring facilities. Utilization rate was found to exhibit a slight but steady decrease with distance up to 6 km from a facility. The accuracy of the future modelling of unsampled facility catchments can be increased by the incorporation of these trends.
Keywords: Health services, Fevers, Thiessen polygons, Utilization rate, Kenya
1. Introduction
Government health facilities represent a key source of primary health care for febrile paediatric patients in Kenya (MEASURE DHS+, 2004, http://www.measuredhs.com). Data that are collected routinely at these facilities have the potential to provide a wealth of information about their access and use by the population for treatment and management of febrile and other illnesses. If these data are to be used to model access and use patterns, then the case numbers recorded at each facility must be compared to the total catchment population that the facility is likely to serve. For the majority of cases, no information exists regarding the size of its catchment population and this figure must therefore be estimated. The size of a facility’s catchment population is related to both the spatial extent of the catchment and the pattern of utilization within it. Any model designed to predict catchment populations must therefore address these two factors.
For the majority of government facilities in Kenya, the only information available to assist in estimating catchment population is their location and type (e.g. hospital, health centre, dispensary) (Noor et al., 2004). Given this information, a simple and intuitive means of partitioning a population between a series of facilities is provided by Thiessen polygons. A Thiessen polygon (also referred to as a Dirichlet tile) is defined in this case as the region that incorporates all points that are closer to a given facility than any other. The use of Thiessen polygons in this context is well established (Twigg, 1990; Zwarenstein et al., 1991; Albert et al., 2000; Noor et al., 2003) and is based on two key assumptions which address the two factors stated above:
That all patients choose to utilize the facility nearest to them, regardless of its type, and hence the spatial extent of a facility catchment is determined solely by the proximity of its neighbours.
That per-capita utilization rate is constant throughout a catchment (i.e. that distance does not deter utilization within a catchment).
Previous studies of patient behaviour have allowed inferences to be made about the validity of one or both of these assumptions in various settings, and these are discussed in the following section. This study presents a series of new spatial analytical methods by which the validity of these assumptions can be tested directly and hence the suitability of a Thiessen polygon catchment model explicitly assessed. These methods are applied to paediatric out-patient origin data from a sample of 81 government health facilities in four districts of Kenya, and the observed patient behaviour patterns reported. The success of the methods presented in assessing the validity of the Thiessen polygon assumptions is then discussed.
2. Background
2.1. Patient choice
The actual partitioning of a population between two neighbouring facilities is determined by choices made by care-seeking members of that population. These choices can be based on a wide range of considerations, including social, cultural and religious factors, as well as the nature of the facilities in question (Stock, 1983; Müller et al., 1998; Onokerhoraye, 1999; Deressa et al., 2003). If the two facilities are perceived to be of equal standing by the population, then it would be reasonable to expect care-seekers to base their choice of facility on the relative distance to each. In this idealised case, a theoretical catchment boundary would exist that is equidistant to both facilities. If one facility was perceived as a more attractive option, however, then one might expect care-seekers to be willing to travel relatively further to reach it than its less-favoured neighbour. In these circumstances, the location of the catchment boundary would be shifted towards the latter facility. Various studies into health facility utilization patterns in developing countries have observed differences in the attraction or draw of different facility types. A study in rural Nigeria reported that the perceived lower quality of service available from dispensaries meant that they were less likely to attract patients over longer distances than were the higher-order facilities (Stock, 1983). Similar patterns were also noted in later studies in Nigeria (Onokerhoraye, 1999) and Papua New Guinea (Müller et al., 1998).
Few studies have attempted to test directly actual patient behaviour patterns in relation to their theoretical choice as defined by Thiessen polygons. A simple means of quantifying this pattern is to determine the proportion of people who have utilized their nearest facility. Previous analysis of the 81-facility patient origin data has shown that this proportion ranges from 56 to 83% over the four districts (Noor et al., 2003). An earlier study in rural South Africa stated that 81% of homesteads utilize their nearest facility (Tanser et al., 2001). These values suggest that, although Thiessen polygons may provide a reasonable approximation of patient behaviour, there is a proportion of patients that base their choice of facility on factors other than distance. Tanser et al. (2001) also compared actual-to-predicted (Thiessen) catchments. They concluded that there was overall agreement between predicted and actual catchments, but that large variation existed.
2.2. Utilization rate
The simple allocation of a population into a series of contiguous facility catchments, such as Thiessen polygons, assumes a uniform utilization rate throughout that population. This implies that, within a catchment, a patient’s likelihood of visiting the facility is not affected by their distance from it. The concept of distance as a primary influence on health facility utilization is well established (Shannon et al., 1969, 1973; Kohli et al., 1995). Previous studies have investigated the relationship between utilization rate and distance in a wide range of settings, and a variety of different trends have been observed. Several studies in rural areas of Ethiopia, for example, have reported distance effects on care-seeking behaviour with steep distance–decay gradients in utilization rate and under-utilization of more rural health services (Kloos, 1990; Deressa et al., 2003). The studies by Stock (1983) and Tanser et al. (2001) both described an exponential decay in utilization rate with distance and this model has commonly been described as a reasonable approximation of the utilization–distance relationship in both developed and developing world settings (Morrill and Earickson, 1968; Ingram et al., 1978). A study in rural Papua New Guinea reported that although utilization rate showed a general decline with distance, this decline was not evident until some distance away from facilities, and a Gaussian curve was therefore proposed as being a more representative model (Müller et al., 1998). A pertinent study in the Kilifi district of Kenya found a decrease in admission rates to the district hospital with distance such that the rate from distances over 25 km from the hospital was one-fifth of that within 5 km (Schellenberg et al., 1998). In contrast, other studies have found distance to have no systematic effect on utilization rate even in rural settings (Girt, 1973; Slack et al., 2002).
3. Methodology
3.1. Approach
The various studies described have reported differing draws from different facility types, significant proportions of patients attending facilities other than their nearest, and decay in utilization rate with distance. Whilst these findings enable an assessment of the suitability of the Thiessen polygon model, they are less able to suggest how such a model could be modified to more accurately represent the patient behaviour observed. In this study, a geographical information system (GIS) was used to predict the catchment boundary along a direct transect between each pair of neighbouring facilities in the sample set based on patient choice patterns (see Fig. 1). Once the location of a catchment boundary can be established along a given transect, this can be compared to that predicted by the theoretical Thiessen polygon boundary. In this way, not only can the validity of the Thiessen boundary be assessed directly, but, if its position is found to be inappropriate, the position of a more realistic boundary can be identified.
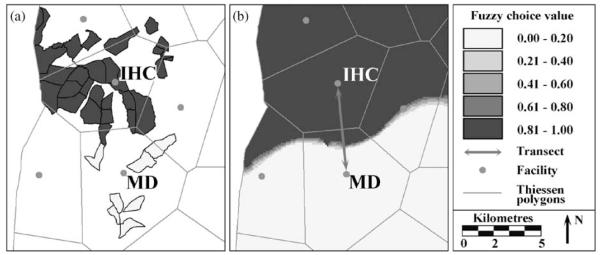
Fig. 1.
Creation of a fuzzy choice surface. This example shows the case of Iyabe health centre (IHC) and Misesi dispensary (MD) in the Greater Kisii district. All enumeration areas contributing one or more patients to either facility were allocated a fuzzy choice value corresponding to the relative proportion attending Iyabe health centre (a). The polygon coverage was then rasterised into a 100 m grid and interpolated using an inverse distance weighting algorithm to predict a choice surface (b). Thiessen polygon boundaries are also shown for reference.
When considering a distance decay effect in utilization rate, it may be difficult to disentangle the influence of neighbouring facilities, especially where they are in relatively close proximity. This can lead to the incorrect conclusion that distance limits access to a facility when, in reality, patients at the periphery of a catchment are simply choosing to utilize a neighbouring facility. These effects can be disentangled, however, if the pattern of patient choice between the two facilities is analysed prior to assessing the utilization rate gradient. If a clear patient choice boundary can be identified, then it is reasonable to interpret any reduction in utilization rate within this boundary as being less influenced by the second facility than that observed outside the boundary. The approach taken in this study was to exclude a buffer around the periphery of each catchment – the width of this buffer being determined by the results of the preceding patient choice analysis.
3.2. Data and study area
This study was based on data acquired by the Government of Kenya (Ministry of Health, Division of Malaria Control) and the Kenya Medical Research Institute/Wellcome Trust Collaborative Program (Zurovac et al., 2002). The four Kenyan districts of Bondo, Greater Kisii (now composed of Kisii Central and Gucha district), Kwale and Makueni were chosen as encompassing a broad range of the most prevalent environmental, demographic and socio-economic conditions found across Kenya. Greater Kisii and Bondo exhibit relatively evenly distributed and high density population, whereas Makueni and Kwale include areas of very low population density. This difference is reflected in the density of health facilities within the districts. The four districts provide representative examples of the main malaria ecologies in Kenya: intense perennial transmission (Bondo), ‘highland’ malaria (Greater Kisii), acute seasonal transmission (Makueni) and intense seasonal transmission (Kwale) (Snow et al., 1998). The districts are described in more detail in Zurovac et al. (2002), Noor et al. (2003) and Amin et al. (2003).
A total of 81 government facilities, consisting of hospitals, health centres and dispensaries, were sampled from the four districts during 2001–2002. Each facility was sampled over 2 days during which time the origin of all febrile paediatric out-patients was determined. The smallest Kenyan census unit is the enumeration area (EA), normally consisting of not more than 100 households, and these were the units by which each child was located.
EA population and out-patient data were compiled into a GIS polygon layer in ArcView 3.2 (ESRI Inc., USA) along with a point coverage of all Government of Kenya (GoK) health facilities. For a full description of out-patient and population data acquisition and digitisation, see Noor et al. (2003).
3.3. Patient choice – creation of fuzzy surfaces
The 81 facilities in the data set represent a sample of the 174 GoK facilities found in total in the four districts. Thiessen polygons were created around all 174 facilities. It was then possible to identify cases where two-sampled facilities were immediately adjacent, that is, they shared a Thiessen boundary. A total of 78 such pairs were identified in the four districts. Analysis was performed along the transect that joined the two facilities in each pair.
Each of the 78 pairs of neighbouring facilities were considered in turn. In each case, a fuzzy choice value was assigned to every EA that contributed one or more patients to either facility in the pair. This value is simply the relative proportion of patients attending each facility from a given EA. The two facilities in each pair were labelled A and B such that values ranged from 1 (all to A) to 0 (all to B). To ease later analysis, facilities were assigned as A or B in a consistent manner depending on the type of facilities in question. This meant that each pair was always classed as either health centre-to-dispensary, dispensary-to-hospital or health centre-to-hospital, and not in the opposite order. The opposite relationships need not be considered separately as they are simply the inverse of those considered. Pairs of matching facility type were also considered, and in these cases, facilities were assigned as A or B arbitrarily. Fuzzy choice values were assigned to the EA polygon coverage (Fig. 1a). These vector layers were converted into 100 m × 100 m raster grids and interpolated using an inverse-distance weighting algorithm. The result is a fuzzy choice surface (Fig. 1b) which represents a continuous prediction of patient choice behaviour between the two facilities in question.
3.4. Utilization rate – creation of study catchments and reduction of overlap effects
To isolate the effect of distance on utilization rate for each facility, it was necessary to define each catchment such that the influence of a neighbouring facility could be considered minor. This was achieved by shrinking the Thiessen polygon boundaries of each catchment such that radii were reduced by approximately 25%. This figure exceeds the largest mean deviation from a Thiessen boundary position found in the analysis of patient choice (see Table 1). This strategy was implemented by creating an exclusion buffer. The buffer width was calculated as a function of the area of each polygon. If polygons can be assumed to be approximately square, then the width W of buffer required to achieve a reduction in radius of 25% can be defined in terms of the polygon area A as
| (1) |
Buffers were created at this width for each catchment.
Table 1.
Mean position of catchment boundaries for each transect class (%)
| Transect class | District means |
Overall means (P) | |||
|---|---|---|---|---|---|
| Bondo | Greater Kisii | Kwale | Makueni | ||
| Dispensary-to-dispensary | 57.30 | 49.40 | 42.40 | – | 51.41 (0.7701)a |
| Health centre-to-health centre | – | 52.87 | 20.20 | 56.60 | 49.80 (0.9798)a |
| Health centre-to-dispensary | 61.31 | 55.25 | 62.17 | 54.40 | 58.50 (0.0077)b |
| Dispensary-to-hospital | 37.30 | 39.05 | 38.60 | 46.70 | 39.88 (0.0041)b |
| Health centre-to-hospital | – | 32.75 | – | 50.40 | 38.63 (0.0656)b |
Values of less than 50% are closer to the first facility in the pair while values greater than fifty are closer to the second. A theoretical Thiessen boundary is equidistant to both facilities and would therefore be located at exactly 50%.
Two-tailed single sample t-test for significant difference from 50%.
One-tailed single sample t-test for significant shift from 50% towards lower-order facility.
For each sampled facility, utilization rate was calculated for each EA contributing one or more patients (i.e. excluding those contributing zero patients). This value was obtained simply by dividing the tally of recorded patients from a given EA by its population. When dealing with paediatric data, the use of total population as a denominator is clearly less favourable than child-only totals. Furthermore, these values represent a daily rate that should not be extrapolated across the year. To achieve a more readily comparable value, the absolute EA rate values for each facility were transformed into relative utilization rate (RUR) by dividing each set through by its largest value. These RUR values were linked back to the EA polygon coverage and again rasterised into a 100 m × 100 m grid. The study catchment for each facility was then delineated using the exclusion buffers.
3.5. Analysis of fuzzy choice transects
Each fuzzy choice surface was analysed along the transect between the two facilities in question. Each transect was divided into 100 equally spaced points and the fuzzy choice value recorded at each point. This process was implemented using the ArcView X-Section Utility v.1.0 extension. The catchment ‘choice boundary’ was taken to be located at the point where the fuzzy choice value equalled 0.5. For each of the transect classes, an ‘average’ transect was created by calculating the mean fuzzy choice value for each of the 100 divisions. In this instance, relative distances were considered since the split of patients between neighbouring facilities is of interest, regardless of the absolute distance between them.
The relative location of the 0.5 boundary was also recorded for each transect. A Thiessen polygon boundary would be located at the exact mid-point of a given transect (50%, since transects ran from 0 to 100%). Actual boundary locations less than 50% are closer to facility A, while those greater than 50% are closer to facility B. An overall and district mean transect location was calculated for each transect class. Single sample t-tests were carried out on the overall mean of each class. For the dispensary-to-dispensary and health centre-to-health centre classes, a two-tailed test was applied to test for a significant difference from the Thiessen boundary (i.e. from a mean value of 50%). For the remaining three transect classes, a one-tailed test was used. Hospitals are the highest-order facility followed by health centres and then dispensaries. The expectation is that any deviation from the Thiessen boundary will be due to patients choosing to make a longer journey to reach a higher-order facility, resulting in a displacement from the Thiessen boundary towards the lower-order facility.
3.6. Analysis of within-catchment utilization rate
For each of the 81 study catchments, the RUR value of every grid cell was output along with its six-digit latitude and longitude. The straight line distance between a given facility and the centroid of each non-zero cell in its study catchment was calculated. RUR values were then grouped by distance from facility, and a mean value was calculated for every successive 100 m. An overall mean RUR plot was created along with one for each district. These plots illustrate the influence of distance from facility on RUR. In contrast to the analysis of patient choice, utilization rate is considered with reference to absolute distance.
4. Results
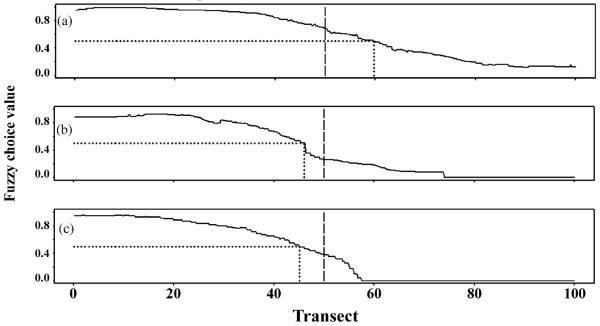
Mean fuzzy choice transects are shown for the three classes of differing facility type that were present: health centre-to-dispensary, dispensary-to-hospital and health centre-to-hospital (Fig. 2). In each case, the position of the 0.5 fuzzy value, taken to represent the catchment choice boundary, is located nearer the lower-order facility. Table 1 lists the overall and district mean boundary locations for all five transect classes. The overall mean boundary locations were 51.41% for dispensary-to-dispensary, 49.80% for health centre-to-health centre, 58.50% for health centre-to-dispensary, 39.88% for dispensary-to-hospital and 38.63% for health centre-to-hospital. Two-tailed single sample t-tests for the dispensary-to-dispensary and health centre-to-health centre classes both revealed no significant difference from the Thiessen boundary location of 50% (P = 0.7701 and 0.9798, respectively). One-tailed single sample t-tests for the remaining three classes revealed that boundary locations were significantly nearer the lower-order facility in each case.
Fig. 2.
Mean fuzzy choice transects for all neighbouring facility pairs of class health centre-to-dispensary (a), dispensary-to-hospital (b) and health centre-to-hospital (c), illustrating the relative draw of different facility types. The location of the theoretical Thiessen boundary is marked at the mid-point (dashed line) along with the location of the observed 0.5 fuzzy choice value (dotted line).
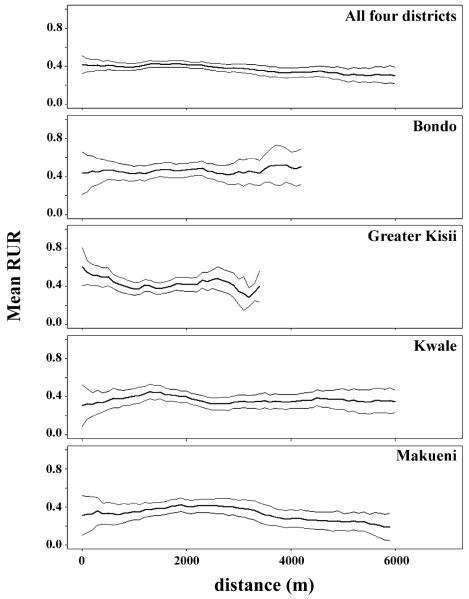
Relative utilization plots are shown in Fig. 3. These include a mean plot for each district as well as an overall mean. Mean plots are accompanied by 95% confidence intervals. Each of the district plots extends to a different length, which corresponds to the most distant non-zero pixels found in any of the study catchments in each district. The districts of Bondo and Greater Kisii are characterised by a relatively dense network of facilities, corresponding to a higher population density. Catchments are, therefore, smaller than some of those found in the more rural Kwale and Makueni districts. For Bondo, RUR fluctuates but exhibits no systematic trend with distance. For Greater Kisii, RUR decreases with distance. For both Kwale and Makueni, RUR increases up to around 2 km, and then levels off (Kwale) or steadily declines (Makueni). Overall, there exists a slight but steady decrease in RUR with distance up to 6 km.
Fig. 3.
Mean overall and district relative utilization rate (RUR) plots. Thick lines show the mean RUR value of all sampled 100 m × 100 m grid cells within every study catchment at each distance. 95% confidence intervals are also shown (fine lines).
5. Discussion
5.1. Patient choice
The construction of fuzzy patient choice surfaces is presented as a robust means of assessing patient behaviour for two neighbouring health facilities and identifying the location and nature of the choice boundary between them. This method represents the conversion of two separate facility-based variables (attendance per EA) into a single facility pair-based variable (fuzzy choice) that describes the spatial partitioning of patients between the two facilities in question. By analysing patient choice along a transect between two neighbouring facilities, the influence of other facilities is minimized. The mean fuzzy choice transects for each transect class (Fig. 2) suggest a smooth gradient of choice between the two facility types in question. This is not, however, representative of the shape of most of the 78 individual choice transects (not shown). These exhibited a much sharper transition from high to low choice values indicating a crisper boundary. Although this characteristic of the individual plots is smoothed in the averaging process, the mean transects are useful for illustrating the relative drawing power of the different facility types as a whole, especially with reference to the Thiessen boundary. The calculation of mean boundary locations, along with the use of appropriate significance tests (Table 1), provides a means of comparing directly the observed behaviour patterns to those assumed in a Thiessen polygon catchment model.
For the Kenyan data set used in this study, the results suggest that the Thiessen polygon model does not provide a realistic division of a population into facility catchments when dealing with facilities of different type and that a greater level of model accuracy would be achieved if boundaries were shifted away from the higher-order facility towards the lower-order facility. Whilst these results reveal trends in patient choice between formal sector options, the omission of non-GoK facilities in the analysis means that they must be considered with caution when extrapolated to a wider setting. In many cases, the presence of mission, private or informal sector options will influence patient choice. Further analysis of more complex data from community surveys and positions of these broader service providers will be explored elsewhere (Noor et al., in preparation).
5.2. Utilization rate
The method presented allows the effect of distance on utilization rate to be studied in isolation from the possible influence of surrounding facilities. Although one consequence of the use of exclusion buffers is that the maximum distance over which this relationship can be studied for any given set of sample facilities is inevitably reduced, it provides a means of elucidating the influence of distance alone. The degree of confidence associated with each of the mean plots in Fig. 3 follows a similar pattern – wide confidence intervals at small distances, which narrow through medium distances before widening once more at the larger distances. This consistent pattern can be explained largely by changes in sample size. Only those EAs that contributed patients to the sample could be included in the analysis, and this represented a relatively sparse sample (between 13 and 28% of EAs across the four districts). The successive 100 m distance bands (over which RUR values were averaged) can be considered as a series of concentric bands of equal width and, as such, their area increases linearly with distance from facility. Distance bands close to the facility are, therefore, smaller and less likely to contain as many non-zero RUR pixels as those further away, with a corresponding effect on sample size. When considering the largest distances in each district, the sample size is likely to be small, since there are few examples of catchments that extend to this distance.
Individual district plots display considerable high-frequency spatial variation, which can be attributed to the relatively sparse number of contributing EAs. A general decrease in RUR is evident, however, with distance up to around 6 km. This suggests that, for the data set studied, the assumption of uniform within-catchment utilization rate is sub-optimal. The observed decline with distance is consistent with most other low-income country studies (Stock, 1983; Kloos, 1990; Müller et al., 1998; Schellenberg et al., 1998; Tanser et al., 2001; Deressa et al., 2003), although the observed decline is far less pronounced than many of those reported. A reasonable explanation for this difference is that the influence of neighbouring facilities is often manifested as a reduction in RUR towards the periphery of a catchment and this effect has not been removed adequately in many studies leading to their over-reporting of decline in RUR with distance.
Whilst knowledge of the within-catchment pattern of RUR is vital in the formulation of a modelling strategy, it falls some way short of explaining the absolute pattern of facility usage. This shortfall arises because a significant proportion of paediatric fevers are treated outside the formal sector due to a plethora of factors of which distance is only one (Snow et al., 2003; Amin et al., 2003). If catchment population estimates made without consideration of this non-attendance are then used as denominators (with facility disease incidence data as numerator) to estimate disease rate, then rates may be under-estimated. Whilst this work presents methods to account for the influence of distance on utilization, future work must consider ways to quantify the influence of other factors. Data obtained from household surveys, for example, can allow a more thorough assessment of care-seeking behaviour than facility-based data alone, and this will be explored in a subsequent study (Noor et al., in preparation).
5.3. Euclidean distance
Euclidean distance is simply the straight-line distance between two points. When considering distances on the ground, an alternative metric is the financial or time cost of making the journey between two points. Various studies have investigated the correspondence between Euclidean distance and journey cost (e.g. Perry and Gesler, 2003; Costa et al., 2003), and the extent to which the two concur is dependent on factors, such as the density and quality of transport networks, the nature of topography, and features such as rivers and swamps. Whilst Thiessen polygons are defined in terms of Euclidean distance, their validation using geo-referenced patient-use data does not explicitly use any distance metric as it relies solely on the positions of patients in Cartesian space and their choice of health facility. A consideration of the discrepancy between journey cost and Euclidean distance becomes important, however, when attempting to explain the reasons for the observed shifts in boundary positions towards lower-order facilities. A situation may exist, for example, whereby the quality of transport networks around hospitals allows more efficient journeys than that around health centres and dispensaries. In this case, if care-seekers based their choice of facility entirely on journey cost, then one would expect a relative increase in the spatial extent of hospital catchments. This explanation has some grounding in that hospitals are generally located in urban areas, where one might expect transport networks to be most efficient. However, given that the majority of patients made the journey to seek treatment on foot, and that populated non-urban areas generally have comprehensive road, track and footpath networks, it is unlikely that this effect is responsible for all of the observed shift in boundary location. These issues do, however, underline the importance of considering journey cost when attempting to predict patient behaviour, and this is the subject of work currently in progress (Noor et al., in preparation).
6. Conclusions
The methods presented in this study allow the two key assumptions inherent in a Thiessen polygon modelling approach to be tested directly using patient origin data and, where these assumptions are found to be invalid, provide guidance as to how the approach can be refined to better represent the patient behaviour observed. For the four Kenyan districts studied, the two assumptions were found to be invalid. In the 78 cases of neighbouring facilities considered, mean boundary locations were found to be significantly closer to lower-order facilities than predicted by Thiessen polygons. This implies that the relative draw of facilities of different types is different and as such patients are willing to travel some distance further to reach a higher-order facility than a neighbouring lower-order facility. Analysis of mean within-catchment utilization rate revealed that, for distances up to 6 km from a facility, a steady decline in utilization rate with distance was present. This implies that it is sub-optimal to model utilization rate as uniform within a catchment. The accuracy of the future modelling of unsampled facility catchments can be increased by the incorporation of these trends.
Acknowledgements
PWG gratefully acknowledges support from the University of Southampton ECS Doctoral Training Account and School of Geography. This study received financial support from The Wellcome Trust, UK (#058922), the Roll Back Malaria Initiative, AFRO (AFRO/WHO/RBM #AF/ICP/CPC/400/XA/00) and the Kenya Medical Research Institute. The authors are grateful to Mr. David Nalo, Head of the Central Bureau of Statistics, for helping with the provision of census data. The authors are also grateful to Abdinasir Amin for his help in the repeat field visits, Priscilla Wairimu, Lydiah Mwangi and Lucy Muhunyo for assistance with data handling and linkage. D.Z. is grateful for support provided by Médicins Sans Frontière. S.I.H. is a Research Career Development Wellcome Trust Fellow (#056642) and R.W.S. a Senior Wellcome Trust Fellow (#058992). We are grateful to Green College, University of Oxford, for the visiting scholarship to P.M.A. and to the Department of Zoology, University of Oxford, for hosting P.M.A. during 2002–2003. This paper is published with the permission of the director, KEMRI.
References
- Albert DP, Gesler WM, Levergood B. Spatial Analysis, GIS, and Remote Sensing Applications in the Health Sciences. Ann Arbor Press; Michigan: 2000. [Google Scholar]
- Amin AA, Marsh V, Noor AM, Ochola SA, Snow RW. The use of formal and informal curative services in the management of paediatric fevers in four districts of Kenya. Trop. Med. Int. Health. 2003;8:1143–1152. doi: 10.1046/j.1360-2276.2003.01140.x. [DOI] [PubMed] [Google Scholar]
- Costa LS, Nassi CD, Pinheiro RS, Almeida RMVR. Accessibility of selected hospitals and medical procedures by means of aerial and transit network-based measures. Health Serv. Manage. Res. 2003;16:136–140. doi: 10.1258/095148403321591456. [DOI] [PubMed] [Google Scholar]
- Deressa W, Ali A, Enqusellassie F. Self-treatment of malaria in rural communities, Butajira, southern Ethiopia. B. World Health Organ. 2003;81:261–268. [PMC free article] [PubMed] [Google Scholar]
- Girt JL. Distance to general medical practice and its effect on revealed ill health in a rural environment. Can. Geogr. 1973;17:154–166. [Google Scholar]
- Ingram DR, Clarke DR, Murdie RA. Distance and the decision to visit an emergency department. Soc. Sci. Med. 1978;12:55–62. [PubMed] [Google Scholar]
- Kloos H. Utilization of selected hospitals, health centres and health stations in central, southern and western Ethiopia. Soc. Sci. Med. 1990;31:101–114. doi: 10.1016/0277-9536(90)90052-t. [DOI] [PubMed] [Google Scholar]
- Kohli S, Sahlén K, Sivertun Å, Löfman O, Trell E, Wigertz O. Distance from the primary health centre: a GIS method to study geographical access to health care. J. Med. Sys. 1995;19:425–436. doi: 10.1007/BF02260846. [DOI] [PubMed] [Google Scholar]
- MEASURE DHS+ The Demographic and Health Surveys for Sub-Saharan Africa Databases Derived Using STATCompiler. [Online] available: http://www.measuredhs.com. [Google Scholar]
- Morrill RL, Earickson R. Variation in the character and use of Chicago area hospitals. Health Serv. Res. 1968;3:224–238. [PMC free article] [PubMed] [Google Scholar]
- Müller I, Smith T, Mellor S, Rare L, Genton B. The effect of distance from home on attendance at a small rural health centre in Papua New Guinea. Int. J. Epidemiol. 1998;27:878–884. doi: 10.1093/ije/27.5.878. [DOI] [PubMed] [Google Scholar]
- Noor AM, Zurovac D, Hay SI, Ochola SA, Snow RW. Defining equity in physical access to clinical services using geographical information systems as part of malaria planning and monitoring in Kenya. Trop. Med. Int. Health. 2003;8:917–926. doi: 10.1046/j.1365-3156.2003.01112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noor AM, Gikandi PW, Hay SI, Muga RO, Snow RW. Creating spatially defined databases for equitable health service planning in resource poor countries: the example of Kenya. Acta Trop. 2004 doi: 10.1016/j.actatropica.2004.05.003. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onokerhoraye AG. Access and Utilisation of Modern Health Care Facilities in the Petroleum-Producing Region of Nigeria: the Case of Bayelsa State. Takemi Program in International Health, Harvard School of Public Health; Boston: 1999. [Google Scholar]
- Perry B, Gesler W. Physical access to primary health care in Andean Bolivia. Soc. Sci. Med. 2003;50:1177–1188. doi: 10.1016/s0277-9536(99)00364-0. [DOI] [PubMed] [Google Scholar]
- Schellenberg JA, Newell JN, Snow RW, Mung’ala V, Marsh K, Smith PG, Hayes RJ. An analysis of the geographical distribution of severe malaria in children in Kilifi District, Kenya. Int. J. Epidemiol. 1998;27:323–329. doi: 10.1093/ije/27.2.323. [DOI] [PubMed] [Google Scholar]
- Shannon GW, Bashshur RL, Metzner CA. The concept of distance as a factor in accessibility and utilisation of health care. Med. Care Rev. 1969;26:143–161. [Google Scholar]
- Shannon GW, Skinner JL, Bashshur RL. Time and distance: the journey for medical care. Int. J. Health Serv. 1973;3:237–244. doi: 10.2190/FK1K-H8L9-J008-GW65. [DOI] [PubMed] [Google Scholar]
- Slack A, Cumming J, Maré D, Timmins J. Variations in Secondary Care Utilisation and Geographic Access – Trends and Variations in Health Care Utilisation in New Zealand 1991–96. Motu/Health Services Research Centre; University of Wellington, New Zealand: 2002. [Google Scholar]
- Snow RW, Gouws E, Omumbo J, Rapuoda B, Craig MH, Tanser FC, le Sueur D, Ouma J. Models to predict the intensity of Plasmodium falciparum transmission: applications to the burden of disease in Kenya. T. Roy. Soc. Trop. Med. H. 1998;92:601–606. doi: 10.1016/s0035-9203(98)90781-7. [DOI] [PubMed] [Google Scholar]
- Snow RW, Eckert E, Teklehaimanot A. Estimating the needs for artesunate based combination therapy for malaria case-management in Africa. Trends Parasitol. 2003;19:363–369. doi: 10.1016/s1471-4922(03)00168-5. [DOI] [PubMed] [Google Scholar]
- Stock R. Distance and the utilisation of health facilities in rural Nigeria. Soc. Sci. Med. 1983;17:563–570. doi: 10.1016/0277-9536(83)90298-8. [DOI] [PubMed] [Google Scholar]
- Tanser FC, Hosegood V, Benzler J, Solarsh G. New approaches to spatially analyse primary health care usage patterns in rural South Africa. Trop. Med. Int. Health. 2001;6:826–838. doi: 10.1046/j.1365-3156.2001.00794.x. [DOI] [PubMed] [Google Scholar]
- Twigg L. Health based geographical information systems: their potential examined in the light of existing data sources. Soc. Sci. Med. 1990;30:143–155. doi: 10.1016/0277-9536(90)90337-r. [DOI] [PubMed] [Google Scholar]
- Zurovac D, Midia B, Ochola SA, Barake Z, Snow RW. Evaluation of Malaria Case Management of Sick Children Presenting in Outpatient Departments in Government Health Facilities in Kenya. Division of Malaria Control, Ministry of Health; Nairobi: 2002. pp. 1–37. [Google Scholar]
- Zwarenstein M, Krige D, Wolff B. The use of a geographical information-system for hospital catchment-area research in Natal Kwazulu. S. Afr. Med. J. 1991;80:497–500. [PubMed] [Google Scholar]