Abstract
The macrolide class of antibiotics, including tylosin and tilmicosin, is widely used in the veterinary field for prophylaxis and treatment of mycoplasmosis. In vitro susceptibility testing of 50 strains of M. gallisepticum isolated in Israel during the period 1997-2010 revealed that acquired resistance to tylosin as well as to tilmicosin was present in 50% of them. Moreover, 72% (13/18) of the strains isolated from clinical samples since 2006 showed acquired resistance to enrofloxacin, tylosin and tilmicosin. Molecular typing of the field isolates, performed by gene-target sequencing (GTS), detected 13 molecular types (I-XIII). Type II was the predominant type prior to 2006 whereas type X, first detected in 2008, is currently prevalent. All ten type X strains were resistant to both fluoroquinolones and macrolides, suggesting selective pressure leading to clonal dissemination of resistance. However, this was not a unique event since resistant strains with other GTS molecular types were also found. Concurrently, the molecular basis for macrolide resistance in M. gallisepticum was identified. Our results revealed a clear-cut correlation between single point mutations A2058G or A2059G in domain V of the gene encoding 23S rRNA (rrnA, MGA_01) and acquired macrolide resistance in M. gallisepticum. Indeed, all isolates with MIC ≥ 0.63 μg/mL to tylosin and with MIC ≥ 1.25 μg/mL to tilmicosin possess one of these mutations, suggesting an essential role in decreased susceptibility of M. gallisepticum to 16-membered macrolides.
Introduction
Mycoplasma gallisepticum is the major mycoplasma pathogen in poultry, causing Chronic Respiratory Disease in chickens and Infectious Sinusitis in turkeys [1]. In Israel, due to control measures, M. gallisepticum outbreaks occur infrequently in breeder flocks. However, M. gallisepticum is sometimes present in meat-type turkey flocks or other types of commercial flocks maintained for long growing periods with minimal biosecurity, which thereby may provide reservoirs of infection. Macrolides (tylosin, tilmicosin) and fluoroquinolones (enrofloxacin, difloxacin) are among the antibiotic families most widely used in poultry in many countries [2], including Israel.
Tylosin has been used prophylactically and therapeutically for mycoplasmosis in certain poultry sectors in Israel for more than 40 years [3]. Historically, tylosin was used for eradication of M. gallisepticum by egg-dipping at the same time as being used for control in the progeny, a practice that was linked to the emergence of M. gallisepticum tylosin-resistant strains, initially in turkey breeder flocks and later in broilers and meat-type turkeys [3]. With the successful eradication of M. gallisepticum in breeder flocks, there was a marked decrease in the use of tylosin in poultry and, probably as a consequence, only sporadic detection of M. gallisepticum tylosin-resistant strains [4]. Notably, tylosin-resistant M. gallisepticum strains, all with the same molecular profile identified by random amplification of polymorphic DNA analysis, were consistently isolated in one geographical region of Israel where tylosin-treated commercial flocks served as an environmental reservoir for outbreaks in breeder flocks [5].
The antibacterial activity of macrolides is due to inhibition of bacterial protein synthesis by binding to the 23S rRNA component of the bacterial 50S ribosomal subunit. Usually in bacteria with a small number of rRNA operons, such as mycoplasmas, acquired resistance to macrolides has been associated with mutations within domain II or V of the 23S rRNA genes or in rplD and rplV, genes encoding ribosomal proteins L4 and L22 [6].
Enrofloxacin has a fairly wide spectrum of efficacy and has been used as the routine choice for treatment of a variety of poultry diseases in addition to mycoplasmosis in many countries [2,7] including Israel where it was first introduced in the early 1990s. This practice may account for the relatively rapid emergence of enrofloxacin-resistance in clinical isolates of M. gallisepticum recently reported by our group [8] and others [9]. Molecular characterization of the quinolone resistance-determining regions (QRDRs) of DNA gyrase and topoisomerase IV in M. gallisepticum isolates with different levels of susceptibility to fluoroquinolones showed that enrofloxacin-resistant isolates harbor amino acid substitutions in the QRDRs of each of three proteins (GyrA, GyrB, and ParC) [10].
The present study reports on in vitro susceptibility to two macrolides (tylosin and tilmicosin) and to enrofloxacin in 50 M. gallisepticum clinical strains isolated in Israel during 1997-2010. In addition, by sequence analysis of domains II and V of the 23S rRNA genes as well as genes encoding ribosomal proteins L4 and L22 in clinical isolates with different levels of susceptibility to tylosin and tilmicosin, we investigated the mechanism of M. gallisepticum acquired-resistance to these two 16-membered macrolides. Furthermore, molecular typing by gene targeted sequencing (GTS) [11] was performed to characterize the M. gallisepticum strains isolated in Israel over time, attempting to gain insight into the emergence and dissemination of the resistance phenotype(s) in this population.
Materials and methods
M. gallisepticum strains and growth conditions
A total of 50 M. gallisepticum strains isolated during the period 1997-2010 from 15 meat-type turkey flocks (MT), 7 turkey breeder flocks (TB), 23 broiler breeder flocks (BB), 4 broiler flocks (B) and 1 Leghorn-type breeder flock (LB) were analyzed (Table 1). These include 24 isolates described previously [10]. In addition, reference strains M. gallisepticum PG31 (ATCC 19610), M. gallisepticum S6 (ATCC 15302), prototype pathogen M. gallisepticum R, and Israeli reference strain 227 were included in this study. Samples from breeder flocks (TB, BB and LB) were submitted to the laboratory within the framework of the national mycoplasma control program; clinical signs were not necessarily present. In contrast, samples from MT and B flocks were received by survey of flocks with respiratory disease and/or serological evidence of M. gallisepticum infection. The outbreaks had no known epidemiological link.
Table 1.
In vitro sensitivity, GTS typing and molecular characterization of domain V in the 23S rRNA genes of M. gallisepticum clinical isolates.
| No | Strain | Sector a | Year | Susceptibility | GTS type | Domain V sequenceb | |||
|---|---|---|---|---|---|---|---|---|---|
| Ty | Tm | En | rrnA | rrnB | |||||
| S6 | S | S | S | NA | A2058/A2059 | A2058/A2059 | |||
| R | S | S | S | NA | A2058/A2059 | A2058/A2059 | |||
| PG31 | S | S | S | NA | NA | NA | |||
| 227 | TB | 1978 | R | R | S | I | G2058/- | -/G2059 | |
| 1 | HZ-19 | MT | 1997 | S | S | S* | II | -/- | -/G2059 |
| 2 | NMH-2 | TB | 1997 | R | R | S | III | -/G2059 | -/G2059 |
| 3 | BSY-10 | B | 1998 | S | S | S* | IV | -/- | -/G2059 |
| 4 | TY-6 | MT | 1998 | R | R | S* | IV | -/G2059 | -/G2059 |
| 5 | DSD-4 | MT | 2000 | R | R | S* | II | -/G2059 | -/G2059 |
| 6 | YS | BB | 2001 | S | S | S | II | -/- | -/G2059 |
| 7 | EK | BB | 2001 | S | S | S | II | -/- | -/G2059 |
| 8 | KBR-3 | MT | 2002 | S | S | S* | II | -/- | -/G2059 |
| 9 | KR-11 | MT | 2002 | R | R | S* | II | -/G2059 | -/G2059 |
| 10 | TMM | BB | 2002 | S | S | S | II | -/- | -/G2059 |
| 11 | KSH | BB | 2002 | S | S | S | II | -/- | -/G2059 |
| 12 | SMR | TB | 2002 | S | S | S | V | -/- | -/- |
| 13 | BR | BB | 2002 | S | S | S | II | -/- | -/G2059 |
| 14 | NLP | TB | 2002 | R | R | S | II | -/G2059 | -/G2059 |
| 15 | PYN | BB | 2002 | S | S | S | II | -/- | -/G2059 |
| 16 | SBC | TB | 2002 | R | R | S | II | -/G2059 | -/G2059 |
| 17 | MKK | BB | 2002 | S | S | S | II | -/- | -/G2059 |
| 18 | NR-3 | LB | 2003 | R | R | S* | II | -/G2059 | -/G2059 |
| 19 | NH-7 | TB | 2003 | R | R | S* | II | -/G2059 | -/G2059 |
| 20 | RFG | TB | 2003 | S | S | S | II | -/- | -/G2059 |
| 21 | TR-9 | MT | 2004 | R | R | S* | II | -/G2059 | -/G2059 |
| 22 | ABA-6 | MT | 2005 | S | S | R* | II | -/- | -/G2059 |
| 23 | BAK-2 | BB | 2005 | S | S | S* | II | -/- | -/- |
| 24 | BNC-2 | MT | 2005 | S | S | S* | VI | -/- | -/- |
| 25 | YDK-3 | MT | 2005 | S | S | R* | II | -/- | -/G2059 |
| 26 | MT-13 | B | 2005 | S | S | R* | II | -/- | -/G2059 |
| 27 | MYZ-8 | BB | 2005 | S | S | R* | VII | -/- | -/G2059 |
| 28 | SYR-3 | BB | 2005 | S | S | R* | II | -/- | -/G2059 |
| 29 | MKT-3 | MT | 2005 | S | S | R* | II | -/- | -/G2059 |
| 30 | SM-9 | MT | 2005 | R | R | S* | II | -/G2059 | -/G2059 |
| 31 | MAR-1 | B | 2005 | R | R | R* | II | -/G2059 | -/G2059 |
| 32 | KYN-6 | BB | 2005 | R | R | S* | II | -/G2059 | -/G2059 |
| 33 | MSA-9 | B | 2006 | S | S | R* | II | -/- | -/G2059 |
| 34 | JL-10 | MT | 2006 | S | S | R* | II | -/- | -/G2059 |
| 35 | MDE-3 | BB | 2006 | R | R | R* | VIII | -/G2059 | -/G2059 |
| 36 | RV-2 | BB | 2007 | S | S | S* | IX | -/- | -/- |
| 37 | BLF-6 | BB | 2008 | R | R | R | X | -/G2059 | -/G2059 |
| 38 | KFM | BB | 2009 | R | R | R | X | -/G2059 | -/G2059 |
| 39 | SU | MT | 2009 | R | R | R | XI | -/G2059 | -/G2059 |
| 40 | LH-22 | MT | 2009 | R | R | R | X | -/G2059 | -/G2059 |
| 41 | VR-8 | BB | 2009 | S | S | R | XII | -/- | -/- |
| 42 | KLD-8 | BB | 2009 | R | R | R | X | -/G2059 | -/G2059 |
| 43 | CK-4 | BB | 2009 | R | R | R | X | -/G2059 | -/G2059 |
| 44 | KC-4 | BB | 2009 | R | R | R | X | -/G2059 | -/G2059 |
| 45 | KTY | BB | 2009 | R | R | R | VIII | -/G2059 | -/G2059 |
| 46 | TLS-2 | BB | 2010 | S | S | S | XIII | -/- | -/- |
| 47 | MCK | BB | 2010 | R | R | R | X | -/G2059 | -/- |
| 48 | MAT-394 | BB | 2010 | R | R | R | X | -/G2059 | -/G2059 |
| 49 | MN-2 | MT | 2010 | R | R | R | X | -/G2059 | -/G2059 |
| 50 | NLY | TB | 2010 | R | R | R | X | -/G2059 | -/G2059 |
a B = Broiler; BB = Broiler breeder; LB = Leghorn-type breeder; MT = Meat-type turkey; TB= turkey breeder.
b Nucleotide present at positions 2058 and 2059.
"-", No polymorphism compared to the sequence of the reference strains.
* MIC values for En published in Gerchman et al. [13] and in Lysnyansky et al. [10].
NA = not analyzed.
All isolates were propagated at 37°C in Frey's broth medium. Isolates of M. gallisepticum were identified by direct immunofluorescence (IMF) of colonies using species-specific conjugated antiserum. Mixed cultures were cloned to IMF homogeneity by microscopic selection of target colonies. Notably, isolates were not filtered cloned in order to avoid inadvertent selection of a non-representative variant [12]. Aliquots of low-passage (3-4 p) cultures were stored at -80°C.
Antimicrobial susceptibility testing
In vitro susceptibility for tylosin (98%, batch RS 0315), tilmicosin (91%, batch RS 0263), kindly provided by Eli Lilly (Indianapolis, IN, USA), and for enrofloxacin (98% active material, Fluka AG, Seelze, Germany) was determined by the microbroth dilution method as previously described [13], following the guidelines recommended by Hannan [14]. Two-fold dilutions of antibiotics from 0.04 - 10 μg/mL were tested. For M. gallisepticum strains sensitive to macrolides or to fluoroquinolones at the lowest concentration in the preliminary test, an additional round of testing with tylosin and tilmicosin or enrofloxacin in the range 0.0008 - 0.2 μg/mL was performed. The microbiological criterion (epidemiological cut-off value) was used for interpretation of MIC results [15].
MIC values for tylosin and tilmicosin in reference strains S6, R and PG31 were 0.0063 μg/mL and 0.0032 μg/mL, respectively for each of the strains (data not shown). The MIC values for enrofloxacin in reference strains S6, R and PG31 were 0.01, 0.005 and 0.01 μg/mL, respectively (data not shown). The MIC values for tylosin, tilmicosin, and enrofloxacin in this study were consistent with the previously published values for these strains [8,16-19].
The MIC values for Israeli reference strain 227 were 1.25 μg/mL for tylosin and tilmicosin and 0.05 μg/mL for enrofloxacin (data not shown).
PCR amplification and sequence analysis of domains II and V of the 23S rRNA genes, rplD and rplV genes
M. gallisepticum genomic DNA was extracted from 10 mL logarithmic-phase broth cultures using the Maxwell® 16 apparatus and Maxwell 16™ Cell DNA Purification Kit (Promega, Madison, USA) according to the manufacturer's instructions. Primers used in this study were designed on the nucleotide sequence of M. gallisepticum strain Rlow (AE015450, [20]) (Table 2). Since the nucleotide sequences of the two M. gallisepticum 23S rRNA genes (MGAr01 (rrnA) and MGAr04 (rrnB)) are highly homologous, four different PCR systems were designed to specifically amplify domains II and V in each gene. One of the primers in each PCR system (initial step) recognizes a sequence in the respective flanking gene (MGA_0754 to amplify domain V and MGA_0746 for domain II of MGAr01; MGA_1046 for domain V and MGAr03 for domain II of MGAr04) (Table 2). The primers MG23S-1F and MG23S-1R (for the nested reactions) contain a nucleotide sequence found in domain V of both MGAr01 and MGAr04 genes. Likewise, primers MG-rRNAII-F and MG-rRNAII-R (nested) recognize a nucleotide sequence in domain II of both MGAr01 and MGAr04 genes (Table 2). In addition, gene-specific primers corresponding to genes rplD and rplV, encoding ribosomal proteins L4 and L22, respectively, were synthesized (Table 2).
Table 2.
Primers used for PCR amplification and sequencing of domains II and V of 23S rRNAs and ribosomal proteins of L4 and L22 in M. gallisepticum.
| Primer designation | Source of primer | Sequence (5'-3') | Nucleotide positiona | Amplicon size (bp) |
|---|---|---|---|---|
| Domain V of MGAr01 | ||||
| MG-23S-1F1 MG-0754-R |
MGAr01 MGA_0754 |
CACAGCTCTATGCTAAATCGC GATAATTGGTGGAGTTGG |
82312-82332 and 324019-324039 83691-83708 |
1396 |
| Nested PCR for domain V of MGAr01 | ||||
| MG-23S-1F1 MG-23S-1R2 |
MGAr01 MGAr01 |
CACAGCTCTATGCTAAATCGC GGTCCTCTCGTACTAAG |
82312-82332 and 324019-324039 83175-83191 and 324882-3244898 |
879 |
| Domain II of MGAr01 | ||||
| MG-mdh-F MG-rRNAII-R3 |
MGA_0746 MGAr01 |
GCAAGCACGGATGGAAGT CCACTGTCTGACTGCAAG |
79928-79945 81483-81500 and 323190-323207 |
1572 |
| Nested PCR fordomain II of MGAr01 | ||||
| MG-rRNAII-F4 MG-rRNAII-R3 |
MGAr01 MGAr01 |
GGTTTAATACCTAGCAGGAT CCACTGTCTGACTGCAAG |
80893-80912 and 322600-322619 81483-81500 and 323190-323207 |
607 |
| Domain V of MGAr04 | ||||
| MG-23S-1F1 MG-1046-R |
MGAr04 MGA_1046 |
CACAGCTCTATGCTAAATCGC GCTAATTGCCTCCTGGTAAC |
324019-324039 and 82312-82332 325669-325688 |
1669 |
| Nested PCR for domain V of MGAr04 | ||||
| MG-23S-1F1 MG-23S-1R2 |
MGAr04 MGAr04 |
CACAGCTCTATGCTAAATCGC GGTCCTCTCGTACTAAG |
324019-324039 and 82312-82332 324882-324898 and 83175-83191 |
879 |
| Domain II of MGAr04 | ||||
| MG-16S-F MG-rRNAII-R3 |
MGAr03 MGAr04 |
GGAATCACTAGTAATCGC CCACTGTCTGACTGCAAG |
321355-321317 323190-323207 and 81483-81500 |
1852 |
| Nested PCR for domain II of MGAr04 | ||||
| MG-rRNAII-F4 MG-rRNAII-R3 |
MGAr04 MGAr04 |
GGTTTAATACCTAGCAGGAT CCACTGTCTGACTGCAAG |
322600-322619 and 80893-80912 323190-323207 and 81483-81500 |
607 |
| rplD (L4) | ||||
| MG-L4-F MG-L4-R |
MGA_0710 MGA_0710 |
CGATTTATCTGGAAAAGTTCAAG GTTCAACCTTTCAACTCAGTTAT |
67500-67522 68084-68106 |
606 |
| rplV (L22) | ||||
| MG-L22-F MG-L22-R |
MGA_0716 MGA_0716 |
ATGATCGCAATTGCAAGACAA CTCCGCTAACTGATTGTTTTC |
69631-69651 70034-70054 |
423 |
PCR reaction mixtures contained 50 μL Ready-Mix PCR Master Mix (ABGene, Surrey, UK) with 30 pmol/μL of each primer (Sigma-Aldrich, Rehovot, Israel) and about 100 ng of mycoplasmal DNA. PCR amplifications were carried out in an MJ Research PT200 thermocycler (Waltham MA, USA). PCR conditions for primers MG-23S-1F/MG-0754-R and MG-23S-1F/MG-1046-R were the following: one cycle of 3 min at 95°C, 1 min 45 s at 56°C, 1 min 45 s at 72°C; 30 cycles of 95°C for 45 s, 56°C for 45 s, and 72°C for 1 min 45 s; 72°C for 10 min. To amplify domain II of the 23S rRNA genes (primers MG-mdh-F/MG-rRNAII-R or MG-16S-F/MG-rRNAII-R) the following program was used: one cycle of 3 min at 95°C, 2 min at 52°C, 2 min 30 s at 72°C; 30 cycles of 95°C for 45 s, 52°C for 45 s, and 72°C for 2 min; 72°C for 10 min. When the final PCR product of domain II or V of 23S rRNA was absent or was weak on the agarose gel, it was subjected to semi-nested PCR with primers MG-23S-1F/MG-23S-1R (for domain V) or with primers MG-rRNAII-F/MG-rRNAII-R (for domain II) as follows: one cycle of 3 min at 95°C, 45 s at 50°C, 1 min at 72°C; 30 cycles of 95°C for 30 s, 50°C for 30 s, and 72°C for 1 min; 72°C for 10 min. The nested program was also used for amplification of the rplD (primers MG-L4-F/MG-L4-R) and rplV (primers MG-L22-F/MG-L22-R) genes (Table 2). PCR products were visualized on ethidium bromide stained agarose gels, and then purified from the gel using the QIAquick Gel Extraction kit (QIAGEN, Hilden, Germany).
Sequencing was performed at the DNA Sequencing Unit, Weizmann Institute (Rehovot, Israel), utilizing the Applied Biosystems DNA Sequencer with the ABI BigDye Terminator Cycle Sequencing Kit (Applied Biosystems, Foster City, CA, USA). Sequence editing, consensus, and alignment construction were performed using DNASTAR software, version 5.06/5.51, 2003 (Lasergene, Inc. Madison, Wisconsin, USA).
Numbering of the nucleotide substitutions in domain V of the 23S rRNA sequenced amplicon is according to the sequence of the respective genes in Escherichia coli.
GTS typing
Molecular typing was performed by modified GTS analysis [11]. The pvpA, gapA, and lp (MGA_0319) partial gene sequences were amplified using primers pvpA 4F/3R, gapA 3F/4R, and lp 1F/1R described previously [11]. However, the mgc2 gene was amplified using primers mgc2 2F/2R, previously described by Garcia et al., [21], resulting in an amplicon of about 300 bp. Amplified gene fragments of the respective genes were sequenced as described above.
The sequences obtained from each corresponding forward and reverse primer were assembled using the SeqMan program (Lasergene, DNASTAR) and the extremities showing single strand sequences, as well as aberrant sequences, were trimmed. All sequences obtained for each gene were aligned using Clustal V (Megalign, Lasergene, DNASTAR, Madison, Wisconsin, USA) and trimmed to the same size for diversity analysis. Phylogenetic trees for individual genes were constructed from the Clustal V alignments by the neighbor-joining method and 1000 bootstrap replicate analysis using the MEGA 5 software [22,23]. In contrast with the previously published GTS analysis, in which mgc2 and pvpA gene fragments were 584 bp and 455 bp-long, respectively [11], mgc2 and pvpA sequences were 300 bp and 700 bp-long, respectively (sizes corresponding to the M. gallisepticum Rlow genome [20]). The different sequences obtained for each gene fragment were assigned different allele numbers, designated by Arabic numerals (1, 2, 3, etc; data not shown). The GTS types, based on the allelic profiles of the four genes, were designated by Roman numerals (I, II, III, etc) (Table 1).
The four gene sequences corresponding to each of the GTS types identified amongst the 51 strains analysed, were concatenated head-to-tail for diversity analysis using Darwin 5.0 [24] available at [25]. A distance tree was constructed using the neighbor-joining algorithm with the "simple matching" option (no correction applied to dissimilarities). The "pairwise gap block correction" option was selected with a minimal length for gap blocks of one nucleotide. This implied that all consecutive gaps, starting from one nucleotide, were considered as a single event. A bootstrap analysis with 1000 replicates was performed to test the stability on randomly chosen sets of positions.
Sequences of 50 M. gallisepticum isolates and 1 Israeli reference strain were submitted to GenBank under the following accession numbers: gapA, JN102573-102623; MGA_0319, JN102624-102674; pvpA, JN113291-113341; mgc2, JN 13342-113392.
Results
Antimicrobial susceptibility
An overview of the MIC values, MIC50, and MIC90 for tylosin, tilmicosin, and enrofloxacin for the 50 strains tested is presented in Table 3. Bimodal distribution of MIC was identified for all three antimicrobial agents, indicating acquired resistance in isolates in the higher range of MIC values.
Table 3.
Distribution of minimal inhibitory concentration (MIC) for tylosin, tilmicosin, and enrofloxacin among 50 M.gallisepticum field strains, determined by the microbroth dilution method.
| Number of isolates with MIC (μg/mL) of | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antimicrobial agent | ≤0.0032 | 0.0063 | 0.0125 | 0.025 | 0.05 | 0.1 | 0.25 | 0.63 | 1.25 | 2.5 | 5 | ≥10 | MIC50 | MIC90 | % Resistance |
| Tylosin | 1 | 11 | 10 | 2 | 1 | 3 | 8 | 13 | 1 | 0.05 | 2.5 | 50 | |||
| Tilmicosin | 16 | 6 | 2 | 1 | 3 | 7 | 15 | 0.1 | ≥10 | 50 | |||||
| Enrofloxacin* | 3 | 10 | 9 | 5 | 2 | 11 | 8 | 2 | 0.25 | 5 | 46 | ||||
M. gallisepticum strains considered to have acquired resistance according to the microbiological criterion are represented in bold.
* MIC values for enrofloxacin are presented for 26 M. gallisepticum strains tested in this study and for 24 strains tested by the same method with the same reference strains and controls and published previously [6,8].
In Table 1 susceptibility data are presented on an individual strain basis indicating year of isolation and poultry sector of origin.
The molecular basis of macrolide resistance in M. gallisepticum clinical isolates
No nucleotide mutations associated with decreased susceptibility to macrolides were identified in the rlpD and rlpV genes or in domain II of the 23S rRNA genes (data not shown). However, sequence analysis of domain V revealed that all 25 M. gallisepticum tylosin and tilmicosin-resistant clinical isolates had nucleotide transitions in one or both 23S rRNA genes (Table 1). Twenty-four tylosin and tilmicosin-resistant M. gallisepticum strains showed an A2059G transition in both rrnA and rrnB and strain MCK showed an rrnA A2059G transition (Table 1). The Israeli reference strain 227 with MIC of 1.25 μg/mL to tylosin and to tilmicosin had rrnA A2058G and rrnB A2059G transitions. In the cohort of 25 tylosin- and tilmicosin-susceptible clinical isolates, 19 possessed only the rrnB A2059G substitution and 6 did not show any substitution (Table 1). Notably, no increase in the MIC values was found between cohorts of M. gallisepticum isolates showing the genotype found in reference strains S6 and R (rrnA A2058A/A2059A and rrnB A2058A/A2059A) and M. gallisepticum strains possessing the single nucleotide substitution A2059G in rrnB (Table 1).
Molecular typing of M. gallisepticum clinical isolates
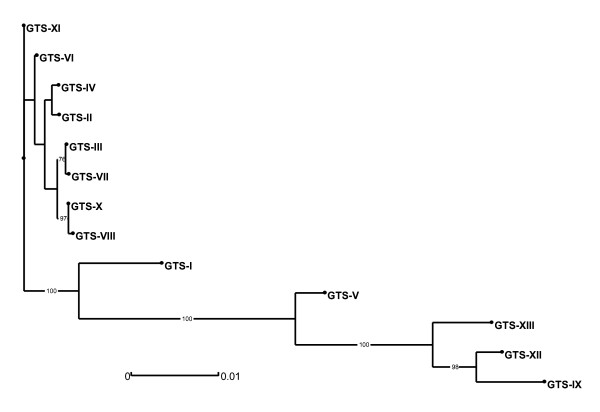
The genetic variability of Israeli M. gallisepticum strains was assessed by a modification of the previously described GTS method [11]. Overall, 13 GTS groups, arbitrarily designated I through XIII, were distinguished by analysis of the partial gene sequences of mgc2, pvpA, gapA, and lp (Table 1 and Figure 1). The results show that 38 of the 51 strains analyzed belong to two major groups: GTS type II, comprising 28 isolates, and GTS type X, with ten isolates. Type II was identified in 28/35(80%) of M. gallisepticum strains isolated between 1997 and 2006 and was not identified after 2006 (Table 1, No. 1-35). Type X, first detected in 2008, was found in 10/14 (71%) of the strains isolated since then (Table 1, No. 37-50). Type X differs from type II by the nucleotide sequences of three genes (mgc2, pvpA, and lp). Two isolates each possess GTS type IV and GTS type VIII. The remaining nine strains were found to have unique patterns. Interestingly, GTS type X is very closely related to type VIII (Figure 1). They diverge only by a single nucleotide polymorphism (SNP) in the pvpA sequence, namely by 1 out of 1837 nt of the concatenated sequences analyzed (0.054% divergence). GTS type VIII was first identified in 2006 and was found again in 2009.
Figure 1.
Phylogenetic tree derived from distance analysis of the four concatenated GTS partial gene sequences. The tree was constructed using the neighbor-joining algorithm (Darwin 5.0). A single sequence representing each of the 13 GTS types (I to XIII, Table 1) is displayed. Bootstrap percentage values were calculated from 1000 resamplings and values over 70% are displayed. The scale bar shows the distance equivalent to 1 substitution per 1000 nucleotide positions.
Notably, the susceptibility profiles of M. gallisepticum strains presented in Table 1 show that isolates with molecular type II vary with respect to susceptibility to tylosin and enrofloxacin (11 strains susceptible to both antibiotics, nine resistant to tylosin and susceptible to enrofloxacin, seven susceptible to tylosin and resistant to enrofloxacin, and one resistant to both antibiotics). In contrast, all the M. gallisepticum strains with molecular types VIII and X were resistant to enrofloxacin as well as to tylosin and to tilmicosin (Table 1).
Discussion
In the present study, the microbiological criterion was used for interpretation of MIC results, since no Clinical and Laboratory Standards Institute breakpoints for tylosin, tilmicosin and enrofloxacin are available for the avian pathogen M. gallisepticum [26]. The bimodal distribution of the cohort of strains tested (Table 3) allows wild-type susceptible populations of bacteria to be distinguished from those with acquired resistance [15,27]. Indeed, according to the data presented in Table 3, M. gallisepticum field strains with MIC of ≥ 0.63 μg/mL to tylosin, ≥ 1.25 μg/mL to tilmicosin and ≥ 1.25 μg/mL to enrofloxacin should be considered as resistant strains. The difference between susceptible and resistant populations for macrolides is more than tenfold (0.05 vs. ≥ 0.63). Using this criterion, 50% of all M. gallisepticum strains checked in this study were resistant to tylosin and tilmicosin and 46% were resistant to enrofloxacin (Table 3). Moreover, 12/14 (86%) and 13/14 (93%) of recently isolated M. gallisepticum strains (2008-2010) were resistant to tylosin and tilmicosin and to enrofloxacin, respectively (Table 1). Resistance to tylosin is not a new phenomena in Israel, being present at least sporadically since the 1970s [3]. Moreover, tylosin-resistant M. gallisepticum strains have been previously isolated under field conditions in many countries [9,19,28-30]. In contrast, although enrofloxacin has been used in local poultry since the early 1990s, enrofloxacin-resistant M. gallisepticum strains were first detected in 2005. However since then, 23/29 (79%) of the M. gallisepticum field strains tested were resistant to enrofloxacin (Table 1). The emergence of widespread resistance to tylosin and tilmicosin in clinical isolates of M. gallisepticum in Israel, often together with resistance to enrofloxacin, may confound treatment of mycoplasma infection in poultry.
The data presented herein demonstrate that a single point mutation in domain V of the 23S rRNA gene of operon rrnA is highly correlated with decreased susceptibility of M. gallisepticum to 16-membered macrolides (Table 1). Indeed, with one exception, all isolates with a MIC of ≥ 0.63 μg/mL to tylosin and a MIC of ≥ 1.25 μg/mL to tilmicosin show the transition A2059G in the rrnA. Interestingly, the single exception is M. gallisepticum strain 227 that has the nucleotide transition A2058G in domain V of 23S rRNA gene of rrnA (Table 1). This strain was isolated more than 30 years ago and possesses a unique GTS-pattern. No correlation between the presence of nucleotide substitution A2059G in rrnB and acquired resistance or decreased susceptibility to tylosin was found in this study.
It has been shown previously that tylosin-resistant M. gallisepticum mutants selected in vitro by erythromycin harbored an A2058G substitution in one of the two 23S rRNA genes [31]. However, since the authors did not use the designation rrnA and rrnB, it was not possible to clarify in which 23S rRNA gene the A2058G mutation was identified. In addition, among the tylosin-resistant mutants selected by erythromycin, a G2057A mutation and an A2059G mutation were found in one of the 23S rRNA genes. In the same study, in M. gallisepticum tilmicosin-selected tylosin-resistant mutants, two mutations, A2058G and A2503U, occurred in one of the two 23S rRNA genes and those mutants were characterized by markedly high resistance [31]. In another study, in vitro selection of M. gallisepticum mutants resistant to tiamulin, a member of the pleuromutilin family of antibiotics that also bind at the peptidyl transfer site in the 23S rRNA, resulted in nucleotide substitutions within domain V of the 23S rRNA genes [32]. Mutants with the A2058G or the A2059G mutation showed cross-resistance to erythromycin, tilmicosin and tylosin. Interestingly, 1/3 of these mutants harbored A2058G substitution in the rrnB gene, while the other two have A2058G or A2059G in the rrnA gene [32]. The nt substitutions at 2058 or at 2059 have been previously reported as hot spots for macrolide resistance in other bacteria and mycoplasmas [6,33-39].
Molecular typing of the 50 Israeli isolates analyzed in this study revealed the presence of two predominant types: GTS type II dominated until 2006 and type X has been dominant since first detected in 2008. By molecular analysis of the nucleotide sequences of pvpA, lp, and mgc2 genes, type X is relatively distant from type II but very closely related to VIII and may be considered as part of the same clonal complex.
Interestingly, all M. gallisepticum strains of the currently dominant GTS type X (as well as type VIII) are resistant to tylosin, tilmicosin, and enrofloxacin, suggesting clonal dissemination of this phenotype (Table 1). However, this apparently was not a unique occurrence, as evidenced by the presence of a resistant strain with a different GTS pattern (Table 1, No.39).
In conclusion, our study shows the recent emergence of acquired resistance to both the macrolide and fluoroquinolone classes of antibiotics in M. gallisepticum, mainly present in field isolates closely related by molecular typing. A comparison between cohorts of M. gallisepticum tylosin- and tilmicosin-resistant and -susceptible field strains revealed that acquired resistance to tylosin and tilmicosin may be attributed to mutations A2058G or A2059G in domain V of 23S rRNA gene (operon rrnA). This is the first report of a mechanism for macrolide-resistance in M. gallisepticum clinical isolates. A comparison of MIC in organisms with genetically characterized resistance mutation/s may offer a feasible way to validate MIC breakpoint values. Therefore, the data presented in this paper may help establish a workable breakpoint for macrolides in M. gallisepticum. Characterization of domain V of the 23S rRNA genes in a greater number of M. gallisepticum macrolide-resistant clinical isolates, especially those originating from other countries, will help elucidate whether the nt mutations observed in this study are characteristic only of this cohort of strains or are the universal markers for macrolide resistance in this pathogenic mycoplasma.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
IG carried out MIC assays, molecular analyses and participated in sequence processing. SL participated in the design of the study, manuscript preparation and its editing. IM participated in molecular analyses and PCR testing. LM-S performed diversity analyses and construction of phylogenetic trees and participated in manuscript preparation. IL designed and coordinated the study and drafted the manuscript. All authors read and approved the final version of the manuscript.
Contributor Information
Irena Gerchman, Email: irenag@moag.gov.il.
Sharon Levisohn, Email: sharon-l@013.net.
Inna Mikula, Email: innam@moag.gov.il.
Lucía Manso-Silván, Email: lucia.manso-silvan@cirad.fr.
Inna Lysnyansky, Email: innal@moag.gov.il.
Acknowledgements
This research was supported by Research Grant No. 847-0346 from the Israel Egg and Poultry Board.
References
- Ley DH, Yoder HW. In: Diseases of Poultry. 10. Calnek BW,Barnes HJ,Beard C,McDougald LR,Saif YM, editor. London: Mosby-Wolfe; 1997. Mycoplasma gallisepticum Infection; pp. 194–207. [Google Scholar]
- Hofacre CL. In: Antimicrobial Therapy in Veterinary Medicine. 4. Giguere S,Prescott JF,Baggot JD,Walker RD,Dowling PM, editor. Oxford: Wiley Blackwell; 2007. Antimicrobial drug use in poultry; pp. 545–553. [Google Scholar]
- Levisohn S. Antibiotic sensitivity patterns in field isolates of Mycoplasma gallisepticum as a guide to chemotherapy. Isr J Med Sci. 1981;17:661–666. [PubMed] [Google Scholar]
- Levisohn S, Gerchman I. Epidemiology of tylosin-resistant Mycoplasma gallisepticum strains in Israel. American Association of Avian Pathologists 1996; Louisville, Kentucky. 1996. p. 388.
- Levisohn S, Gerchman I, Berkhoff JE, Ley DH. Molecular tracking of Mycoplasma gallisepticum infection by random amplification of polymorphic DNA. World Veterinary Poultry Association: Aug. 18-22, 1997 1997; Budapest, Hungary. 1997. p. 68.
- Vester B, Douthwaite S. Macrolide resistance conferred by base substitutions in 23S rRNA. Antimicrob Agents Chemother. 2001;45(1):1–12. doi: 10.1128/AAC.45.1.1-12.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gberindyer FA, Wannang N, Akiwuobu CA. Comparative pharmacokinetics/pharmacodynamic modeling on three brands of 10% enrofloxacin oral formulations in broiler chickens. Int J Poul Sci. 2010;9(3):273–277. [Google Scholar]
- Gerchman I, Lysnyansky I, Perk S, Levisohn S. In vitro susceptibilities to fluoroquinolones in current and archived Mycoplasma gallisepticum and Mycoplasma synoviae isolates from meat-type turkeys. Vet Microbiol. 2008;131:266–276. doi: 10.1016/j.vetmic.2008.04.006. [DOI] [PubMed] [Google Scholar]
- Pakpinyo S, Sasipreeyajan J. Molecular characterization and determination of antimicrobial resistance of Mycoplasma gallisepticum isolated from chickens. Vet Microbiol. 2007;125:59–65. doi: 10.1016/j.vetmic.2007.05.011. [DOI] [PubMed] [Google Scholar]
- Lysnyansky I, Gerchman I, Perk S, Levisohn S. Molecular characterization and typing of enrofloxacin-resistant clinical isolates of Mycoplasma gallisepticum. Avian Dis. 2008;52:685–689. doi: 10.1637/8386-063008-RESNOTE.1. [DOI] [PubMed] [Google Scholar]
- Ferguson NM, Hepp D, Sun S, Ikuta N, Levisohn S, Kleven SH, Garcia M. Use of molecular diversity of Mycoplasma gallisepticum by gene-targeted sequencing (GTS) and random amplified polymorphic DNA (RAPD) analysis for epidemiological studies. Microbiology. 2005;151(6):1883–1893. doi: 10.1099/mic.0.27642-0. [DOI] [PubMed] [Google Scholar]
- Rosengarten R, Yogev D. Variant colony surface antigenic phenotypes within mycoplasma strain populations: Implications for species diagnosis and strain standardization. J Clin Microbiol. 1996;34:149–158. doi: 10.1128/jcm.34.1.149-158.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerchman I, Levisohn S, Mikula I, Lysnyansky I. In vitro antimicrobial susceptibility Mycoplasma bovis isolated in Israel from local and imported cattle. Vet Microbiol. 2009;137:268–275. doi: 10.1016/j.vetmic.2009.01.028. [DOI] [PubMed] [Google Scholar]
- Hannan PC. Guidelines and recommendations for antimicrobial minimum inhibitory concentration (MIC) testing against veterinary mycoplasma species. Vet Res. 2000;31(4):373–395. doi: 10.1051/vetres:2000100. [DOI] [PubMed] [Google Scholar]
- Turnidge J, Paterson DL. Setting and revising antibacterial susceptibility breakpoints. Clin Microbiol Rev. 2007;20(3):391–408. doi: 10.1128/CMR.00047-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannan PCT, Windsor GD, de Jong A, Schmeer N, Stegemann H. Comparative susceptibilities of various animal-pathogenic mycoplasmas to fluoroquinolones. Antimicrob Agents Chemother. 1997;41(9):2037–2040. doi: 10.1128/aac.41.9.2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan FTW, Forrester CA, Ripley PH, Burch DG. In vitro and in vivo comparisons of valnemulin, tiamulin, tylosin, enrofloxacin, and lincomycin/spectinomycin against Mycoplasma gallisepticum. Avian Dis. 1998;42(4):738–745. doi: 10.2307/1592709. [DOI] [PubMed] [Google Scholar]
- Kempf I, Reeve-Johnson L, Gesbert F, Guittet M. Efficacy of tilmicosin in the control of experimental Mycoplasma gallisepticum infection in chickens. Avian Dis. 1997;41:802–807. doi: 10.2307/1592332. [DOI] [PubMed] [Google Scholar]
- Jordan FTW, Horrocks BK. The minimum inhibitory concentration of Tilmicosin and Tylosin for Mycoplasma gallisepticum and Mycoplasma synoviae and a comparison of their efficacy in the control of Mycoplasma gallisepticum infection in broiler chicks. Avian Dis. 1996;40:326–334. doi: 10.2307/1592228. [DOI] [PubMed] [Google Scholar]
- Papazisi L, Gorton TS, Kutish G, Markham PF, Browning GF, Nguyen DK, Swartzell S, Madan A, Mahairas G, Geary SJ. The complete genome sequence of the avian pathogen Mycoplasma gallisepticum strain R(low) Microbiology. 2003;149(Pt 9):2307–2316. doi: 10.1099/mic.0.26427-0. [DOI] [PubMed] [Google Scholar]
- Garcia M, Ikuta N, Levisohn S, Kleven SH. Evaluation and comparison of various PCR methods for detection of Mycoplasma gallisepticum infection in chickens. Avian Dis. 2005;49:125–132. doi: 10.1637/7261-0812204R1. [DOI] [PubMed] [Google Scholar]
- Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. MEGA5: Molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Biol Evol. 2011. 2011. [DOI] [PMC free article] [PubMed]
- The Molecular Evolutionary Genetics Analysis (MEGA 5) http://www.megasoftware.net
- Perrier X, Flori A, Bonnot F. In: Genetic diversity of cultivated tropical plants. Hamon P,Seguin M,Perrier X,Glaszmann JC, editor. Enfield: Science Publishers; 2003. Data analysis methods; pp. 43–76. [Google Scholar]
- The Dissimilarity Analysis and Representation for Windows. http://darwin.cirad.fr/darwin/
- Watts JL, Shryock TR, Apley M, Bade DJ, Brown SD, Gray JT, Heine H, Hunter RP, Mevius DJ, Papich MG, Silley P, Zurenko GE. Performance standards for antimicrobial disk and dilution susceptibility tests for bacteria isolated from animals; Approved standard-third edition (M31-A3) CLSI. 2008;28(8) [Google Scholar]
- Dung TT, Haesebrouck F, Tuan NA, Sorgeloos P, Baele M, Decostere A. Antimicrobial susceptibility pattern of Edwardsiella ictaluri isolates from natural outbreaks of bacillary necrosis of Pangasianodon hypophthalmus in Vietnam. Microb Drug Resist. 2008;14(4):311–316. doi: 10.1089/mdr.2008.0848. [DOI] [PubMed] [Google Scholar]
- Kuniyasu C, Yoshida Y, Takano M. Spiramycin- and tylosin-resistant strains of Mycoplasma gallisepticum isolated from breeding chickens and pipped eggs. Natl Inst Anim Health Q. 1974;14:48–53. [PubMed] [Google Scholar]
- Hinz KH. In vitro susceptibility of Mycoplasma gallisepticum field strains to tiamulin and tylosin. Deutsche Tierarztliche Wochenschrift. 1980;87:220–223. (in German) [PubMed] [Google Scholar]
- Bradbury JM, Yavari CA, Giles CJ. In vitro evaluation of various antimicrobials against Mycoplasma gallisepticum and Mycoplasma synoviae by the micro-broth method, and comparison with a commercially-prepared test system. Avian Pathol. 1994;23:105–115. doi: 10.1080/03079459408418978. [DOI] [PubMed] [Google Scholar]
- Wu CM, Wu H, Ning Y, Wang J, Du X, Shen J. Induction of macrolide resistance in Mycoplasma gallisepticum in vitro and its resistance-related mutations within domain V of 23S rRNA. FEMS Microbiol Lett. 2005;247(2):199–205. doi: 10.1016/j.femsle.2005.05.012. [DOI] [PubMed] [Google Scholar]
- Li BB, Shen JZ, Cao XY, Wang Y, Dai L, Huang SY, Wu CM. Mutations in 23S rRNA gene associated with decreased susceptibility to tiamulin and valnemulin in Mycoplasma gallisepticum. FEMS Microbiol Lett. 2010;308:144–149. doi: 10.1111/j.1574-6968.2010.02003.x. [DOI] [PubMed] [Google Scholar]
- Pereyre S, Gonzalez P, De Barbeyrac B, Darnige A, Renaudin H, Charron A, Raherison S, Bebear C, Bebear CM. Mutations in 23S rRNA account for intrinsic resistance to macrolides in Mycoplasma hominis and Mycoplasma fermentans and for acquired resistance to macrolides in M. hominis. Antimicrob Agents Chemother. 2002;46(10):3142–3150. doi: 10.1128/AAC.46.10.3142-3150.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereyre S, Charron A, Renaudin H, Bebear C, Bebear CM. First report of macrolide resistant strains and description of a novel nucleotide sequence variation in the P1 adhesin gene in Mycoplasma pneumoniae clinical strains isolated in France over 12 years. J Clin Microbiol. 2007;45(11):3534–3539. doi: 10.1128/JCM.01345-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi H, Nakajima H, Shimizu Y, Eguchi M, Hata E, Yamamoto K. Macrolides and lincomycin susceptibility of Mycoplasma hyorhinis and variable mutation of domain II and V in 23S ribosomal RNA. J Vet Med Sci. 2005;67(8):795–800. doi: 10.1292/jvms.67.795. [DOI] [PubMed] [Google Scholar]
- Morozumi M, Hasegawa K, Kobayashi R, Inoue N, Iwata S, Kuroki H, Kawamura N, Nakayama E, Tajima T, Shimizu K, Ubukata K. Emergence of macrolide-resistant Mycoplasma pneumoniae with a 23S rRNA gene mutation. Antimicrob Agents Chemother. 2005;49(6):2302–2306. doi: 10.1128/AAC.49.6.2302-2306.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucier TS, Heitzman K, Liu S, Hu PC. Transition mutants in the 23S rRNA of erthromycin-resistant mutants of Mycoplasma pneumoniae. Antimicrob Agents Chemother. 1995;39:2770–2773. doi: 10.1128/aac.39.12.2770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuoka M, Narita M, Okazaki N, Ohya H, Yamazaki T, Ouchi K, Suzuki I, Andoh T, Kenri T, Sasaki Y. et al. Characterization and molecular analysis of macrolide-resistant Mycoplasma pneumoniae clinical isolates obtained in Japan. Antimicrob Agents Chemother. 2004;48(12):4624–4630. doi: 10.1128/AAC.48.12.4624-4630.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stakenborg T, Vicca J, Butaye P, Maes D, Minion FC, Peeters J, De Kruif A, Haesebrouck F. Characterization of in vivo acquired resistance of Mycoplasma hyopneumoniae to macrolides and lincosamides. Microb Drug Resist. 2005;11(3):290–294. doi: 10.1089/mdr.2005.11.290. [DOI] [PubMed] [Google Scholar]