Abstract
Purpose
The management of calcaneal fractures remains challenging and often controversial. Open reduction and internal fixation with a lateral plate has been established as a standard therapy for displaced articular fractures. However, accurate subtalar joint reduction, while mandatory, is difficult to achieve, requires an extensive lateral approach, and clinical results may not be up to the difficulty of the task.
Methods
We present a treatment using a percutaneous approach and local balloon reduction followed by polymethyl-metacrylate fixation. This technique was used in four patients presenting articular subtalar fractures with displacement.
Results
Reduction was achieved in all cases using a posterior trans-osseous percutaneous approach. Bony fusion with conservation of the subtalar articular reduction was achieved in all cases. We present all cases with a detailed report of outcome.
Conclusions
Clinical outcome after at least three years of follow-up suggests that this technique may be promising and may be used in cases with closed fractures as a primary reduction and fixation tool.
Introduction
Calcaneal fractures are a challenging clinical problem due to the complex anatomy of the os calcis, the frequent subtalar joint involvement and frequent articular displacement [1, 2]. Open reduction and internal fixation with a lateral plate has been established as a standard therapy [3]. However, surgery is difficult and is plagued with potential problems such as skin necrosis, imperfect reduction and subtalar osteoarthritis [3, 4]. Satisfactory reduction can be obtained using less invasive, percutaneous techniques. However, reduction remains difficult and fixation precarious, necessitating multiple screws and multiple incisions [5, 6].
Following numerous attempts to understand the pathophysiology and outcome of these injuries, starting with Essex-Lopresti in 1950 [7], Sanders et al. designed a classification [8] centered exclusively on the posterior thalamic articular surface involvement and its characteristics. Involvement of the posterior thalamic joint is seen in approximately 80% of cases and is a strong predictor of the eventual clinical outcome. However, the extent of the displacement is not taken into account in the Sanders classification. The thalamic fragments are displaced vertically and impacted in the neutral zone at the time of impact [9–11], and surgery aims at reducing the joint fragments and bringing them back into contact with their subtalar counterparts. We looked for a way to provide reduction of these fragments in a simpler and more effective fashion than the open procedure or closed manipulation techniques. Having an extensive experience in kyphoplasty and vertebroplasty techniques in the spine, and confident that such techniques can be used to achieve adequate reduction, as confirmed by the literature [12], we tried to extend its use to the calcaneal fracture patients by using a percutaneous balloon reduction technique similar to that used in vertebral compression fractures. Bano et al. [13], in 2009, published one case treated by a percutaneous technique including a double lateral approach in order to reduce the thalamic surface and the shape of the os calcis, with an excellent outcome. Gupta et al. [14], in 2009, reported three cases using a technique very similar to the one we used, with a good outcome, albeit the indications were different and the follow-up very limited. The technique we used was designed to reduce the thalamic surface percutaneously and to restore the shape of the bone.
Materials and methods
From 2006 to 2007, four patients aged 26–53 years, all of them female, were operated upon for displaced calcaneal fractures with subtalar joint involvement. Details of the different cases are shown in Table 1. Cases were operated upon from two to nine days after the trauma. Reduction of the fracture was assessed postoperatively using CT in all cases. Reduction was deemed satisfactory in all cases with articular defects being less than 1 mm in all planes.
Table 1.
Characteristics of the cases
| Characteristic | Case number | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Gender | Female | Female | Female | Female |
| Age (years) | 29 | 53 | 54 | 26 |
| Mechanism | Fall on staircase | Fall from ladder (5 ft) | Fall from ladder (4 ft) | Fall in swimming pool |
| Side | Right | Right | Left | Left |
| Sanders class | IIC | IIIBC | IIA | IIB |
| Delay (days) | 2 | 9 | 5 | 8 |
| Follow-up (months) | 36 | 35 | 32 | 30 |
| Discharge | POD2 | POD5 | POD2 | POD2 |
| Worker’s compensation | No | No | No | No |
| Reoperation | No | No | No | No |
| Pain at follow-up | Never | Never | Occasional | Occasional |
| Analgesic usage | No | No | No | No |
| ROM, subtalar, 3 months | 5°E/5°I | 0°E/5°I | 5°E/10°I | 10°E/10°I |
| ROM, subtalar, 6 months | 10°E/15°I | 0°E/10°I | 5°E/10°I | 5°E/20°I |
| ROM, subtalar, 12 months | 5°E/25°I | 5°E/10°I | 10°E/15°I | 10°E/20°I |
| ROM, subtalar, 24 months | 15°E/25°I | 10°E/15°I | 10°E/20°I | 15°E/25°I |
POD postoperative day
Technique
Reduction and fixation of the subtalar surface was achieved using four successive operative steps:
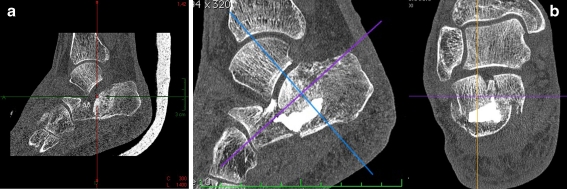
Percutaneous reduction with inflation of a balloon ideally placed just under the thalamic fragments (Fig. 1).
Percutaneous temporary pin fixation of the plantar cortex of the calcaneus in case of a plantar cortical fracture (Fig. 1).
Transcutaneous stabilisation of the lateral cortex using plastic slabs applied laterally to the heel, just under the lateral malleolus, and tightened with a bone clamp. This allows inflation of the balloon under the articular surface to provide reduction without widening the calcaneus bone laterally, and to provide relative stability of the reduction when the balloon is extracted and the bone cement inserted into the calcaneus, by tightening the lateral fragment together with the thalamic fragment. However, this was used in one patient only as a way to improve the anatomical result.
Percutaneous insertion of polymethyl-metacrylate cement. The cement is the same as that used in vertebral balloon reduction; achieving a high viscosity before insertion is mandatory to avoid any intra-articular leak during insertion.
Fig. 1.
Peroperative fluoroscopic view showing plantar K-wires inserted into the cortex to provide an adequate support for reduction, and the inflatable balloon inserted just under the thalamic fragment and ready to be inflated for reduction
The operative procedure was as follows. The patient received either general or regional anaesthesia and was positioned prone, with the operative foot positioned loosely over the end of the table. The contralateral limb was positioned in a slightly lower position to allow easy lateral fluoroscopy visualisation of the injured limb, or positioned with the knee flexed for the same purpose. Two C-arms were positioned in a lateral and frontal way to obtain orthogonal images. The frontal image intensifier was positioned at a 45° angle with the horizontal plane in order to obtain a retro-tibial view in line with the subtalar joint and allow visualisation of the subtalar fragments during reduction. The skin was prepared and the entire foot was draped in sterile sheets on top of the fluoroscopy devices.
The main skin entry point was located in the posterior aspect of the heel. An 11-gauge bone needle was inserted into the calcaneus bone and a K-wire placed into the fracture through the needle. The tip of the wire was inserted into the fracture line just under the thalamic fragments. In case of a plantar cortical fracture, K-wires were driven percutaneously into the plantar cortex starting from the posterior lower aspect of the heel. Two wires were sufficient to achieve enough stability for our purposes. The wires were placed to act as a floor to provide support at the time the balloon was inflated and to direct its effect vertically towards the thalamic articular fragment. The balloon was then inserted and inflated. A pressure of 250 psi and an injected volume of at least 4 mL were usually necessary to obtain any reduction, depending on the age of the fracture. Migration of the thalamic fragment upwards to the inferior aspect of the corresponding surface of the talus was observed on the image intensifiers. Inflation was stopped when the reduction did not improve regardless of how much more pressure was applied. Stabilisation of the lateral cortex was useful at this point in order to prevent lateral displacement and possible impingement on the lateral malleolus or peroneal tendon sheath. Compression using two laterally placed plastic slabs on each side of the heel, held together with a large bone clamp, achieved this. It further stabilised the fracture when the intracalcaneal balloon was extracted in order to introduce the bone cement. The cement injection device was introduced through the cannula and cement was injected slowly under anteroposterior and lateral fluoroscopy control. Bone cement had to be thick enough to prevent any leakage through the fracture lines into the subtalar joint. An amount of 4–6 mL, necessitating the use of two to four bone injection devices, was typically used. The injection cannula and wires were extracted and the skin closed using absorbable sutures. The use of oxyl-2 cyanocrylate on the skin eliminated the need for any other dressing. The foot was maintained postoperatively in an elevated position for 24 hours and mobilisation was started immediately. Weight bearing was delayed until bony union was expected, i.e. two to three months. Early weight-bearing could theoretically be allowed with this technique, but we have no experience of this so far.
Series
Four consecutive cases were treated using this technique with a follow-up of three years or more. All were female. The mean age was 40.5 years. The procedure was performed after a mean of six days after the trauma.
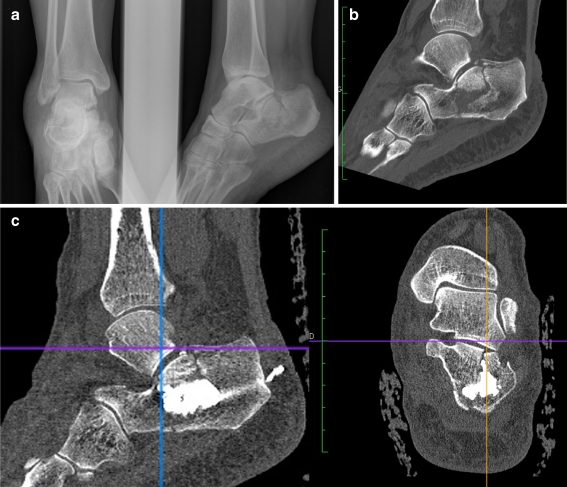
First case
A 29-year-old female working as a bartender suffered a right displaced calcaneal fracture with subtalar involvement and a vertical displacement of the subtalar fragment following a fall on the heel from a flight of stairs (Fig. 2a). X-ray films and CT scan showed an additional fracture of the plantar cortex. The fracture was a “tongue type” and was classified as a type IIC according to Sanders et al. The procedure was performed two days after the injury with no particular difficulty. The control postoperative CT scan showed reduction of the vertically displaced thalamic fragment up to the subtalar joint level (Fig. 2b). Swelling subsided two days after the procedure; pain decreased markedly postoperatively and any pain had disappeared after eight days. Early mobilisation was begun and weight-bearing was delayed until two months after the fracture. The patient resumed full-time employment in the same occupation three months after the accident, with no pain except for slight occasional weather-related discomfort. Full function and freedom from pain are maintained after three years of follow-up (Fig. 2c).
Fig. 2.
a Lateral preoperative radiographs of a type IIC thalamic fracture with vertical displacement of the thalamic fragment. b Postoperative CT scan of the same patient showing reduction of the thalamic joint surface. c Lateral radiograph of the same patient two years after the procedure showing persistent restoration and no subtalar joint space narrowing
Second case
A 53-year-old female was admitted following a fall from a five-foot ladder at home, presenting with a displaced Sanders IIIBC left calcaneal fracture with slight comminution (Fig. 3a). The procedure was performed in the same way nine days after the accident. Reduction of the thalamic fragments was obtained up to the subtalar joint (Fig. 3b) and mobilisation started the day after the procedure. The patient returned to work as a self-employed fashion designer after only 15 days. Full weight-bearing was allowed only two months after the operation, with no pain and mild swelling initially. Full function and absence of pain are maintained three years after the procedure.
Fig. 3.
a Preoperative CT scan reconstruction showing vertical displacement of the thalamic joint surface in a Sanders IIIBC fracture. b Postoperative CT scan reconstruction showing reduction of the thalamic surface in the same patient as in (a)
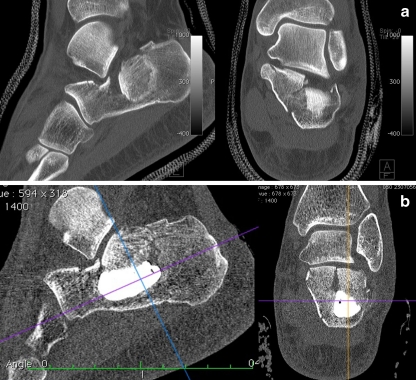
Third case
A 54-year-old female working as an administrative manager was admitted after a fall from a four-foot ladder at home with a right Sanders type IIA fracture (Fig. 4a, b). The procedure was performed five days after admission. Reduction of the thalamic fragment was obtained, although the CT scan showed a slight widening of the thalamic fracture site (Fig. 4c). Also, slight leakage of bone cement in the heel’s soft tissue appeared on the radiographs. The patient resumed full weight-bearing three months after the procedure and work after five months. Local pain due to inflammation of the fibular tendons’ sheath was experienced after three months but subsided after two local steroid infiltrations were performed. Full function is maintained three years after the procedure with no residual pain. Cement leakage in the heel had apparently no consequences.
Fig. 4.
a Anteroposterior and lateral radiograph of a type IIA fracture with vertical displacement of the thalamic surface. b Preoperative CT scan reconstruction in the sagittal plane showing displacement on the thalamus. c Postoperative CT scan reconstruction showing some improvement in the position of the thalamic surface
Fourth case
A 26-year-old female working as a manager in a private company experienced a fall in a swimming pool while on vacation and was admitted with a left Sanders type IIB fracture (Fig. 5a). The procedure was performed eight days after the fracture. Postoperative CT scan showed thalamic reduction with a slight widening of the calcaneal body (Fig. 5b). Pain and swelling subsided after eight days. The patient returned to work six weeks later with crutches and full weight-bearing was allowed after two months. No residual pain is present after three years after the procedure and the patient resumed all social activities including dancing. The patient says she can dance with no pain and can walk with high heels for up to two hours.
Fig. 5.
a Preoperative CT scan reconstruction showing a Sanders type IIB fracture with vertical displacement of the thalamic fragment. b Same patient as in (a) showing postoperative CT scan reconstruction and restoration of the thalamic surface, although some widening of the os calcis and the sagittal fracture line remains
Results
After two years of follow-up, no patient required further surgical treatment and none has evident radiographic subtalar joint space narrowing as a sign of arthritis. All patients resumed social and professional activities with no limping during regular walking. Characteristics of the patients are shown in Table 1. Range of motion of the subtalar joint at the different time points is shown in Table 1.
Discussion
The standard procedure for calcaneal fractures has been open reduction followed by internal fixation for a number of years [15]. The technique is difficult and accurate reduction is clearly a major factor in the functional result [16]. Additional factors depend on the patient (i.e. work-related and workers’ compensation status) [17] and the fracture type, with open fractures carrying a worse prognosis.
Operative reduction and fixation has been likened to “nailing a custard pie to the wall” [7], and was initially strongly discouraged until modern fixation techniques and suitable devices were developed. Even then, operative open reduction and fixation requires an extensive approach and much surgical skill. This may render the technique difficult should any soft tissue involvement be present; and complications [18] due to the surgical approach are not uncommon in clinical practice [19].
The aim of the operative technique is to achieve perfect reduction. This is a difficult task that is achieved only in some cases, even in trained hands, as can be inferred from the literature [20]. Approximately 80% of cases obtain the required perfect reduction in series with numerous cases treated by experienced surgeons. Cases where less-than-perfect reduction is obtained clearly develop inferior outcomes that bring into question the surgical indication [21].
Percutaneous reduction and fixation techniques were described as a means to obviate the need for dissection, with extensive additional damage to the tissues and the peroneal tendon sheath [22]. Satisfactory reduction can be obtained using these techniques. However, reduction remains a difficult goal and fixation is precarious, necessitating multiple screws and thus multiple incisions [5, 6]. The learning curve for these techniques is steep, with unsatisfactory results being difficult to manage and ultimately a number of patients needing subtalar fusion as a salvage procedure.
Percutaneous reduction techniques using balloons inflated with contrast medium as a means of reduction have been used for a number of years in the spine [12], initially as a treatment of osteoporotic fractures and more recently in the setting of acute traumatology [23]. The technique is of widespread use in many countries and is gaining momentum, although two recent studies claimed it is no better than sham surgery [24, 25]. The balloon was designed to provide upward lifting of the vertebral endplate in the context of a vertebral body compression fracture. This may be achieved completely, mainly in acute fractures, and provides accurate reduction. The underlying rationale for lifting the vertebral plateau in a vertebral compression fracture and providing immediate fixation through the use of cement is not unlike that of a calcaneus fracture, where an articular surface is smashed into the bone and the best treatment option is to provide as good a reduction as possible. We applied the principles of percutaneous balloon reduction to the treatment of calcaneal fractures as a technique for reduction and fixation in four cases with subtalar articular involvement and herein describe the technique and outcome of these patients.
The series demonstrates the feasibility of percutaneous reduction using solely balloon reduction and cement injection. This was controlled by performing a CT scan examination postoperatively in all patients. We also describe additional manoeuvres that allowed us to obtain a better reduction peroperatively. This description of a new percutaneous technique has several limitations: it is a small series that includes no patient with factors associated with a poor outcome, all of them were female, and there was no history of heavy physical work and no workers’ compensation history.
Reduction was achieved in a satisfactory fashion in all cases. Thalamic surface fragments were lifted in contact with their subtalar counterpart in all cases and remained at this anatomical site as maintained by the polymethyl metacrylate bone cement. In some cases, a slight widening of the vertical fracture site was observed, as the balloon is designed to provide expansion in all directions and not only vertically to provide the reduction. Further improvements, such as maintaining the heel between plastic slabs under compression at the time of expansion, were implemented with success. However, this clearly remains a concern that should be addressed in further refinements of the technique. In any case, good clinical and radiological results were maintained for three years after the procedure with no additional surgical intervention. This suggests that the reduction that was rated as satisfactory on initial radiographs translated into an adequate restoration of the subtalar joint.
The cement we used was a polymethyl-metacrylate compound largely used in vertebral reduction techniques. Its clinical properties are well known and include an important haemostatic effect as well as immediate analgesic properties observed immediately in the vertebral setting, due to the denervation caused by the exothermic polymerisation. This effect was observed in our series, showing a very fast postoperative recovery and an excellent analgesic effect. The effect persisted after healing of the fracture with no patient showing limping or residual pain two years after the procedure.
The rationale for inserting methyl-metacrylate cement in a fracture site in young patients may be questioned. Clearly, excellent bone reduction and immediate fixation was obtained in all cases with minimal soft tissue damage. The biocompatibility of the polymethyl-metacrylate has been shown for over 50 years in the joint replacement setting and shows no long-term adverse effects [23]. Furthermore, cement augmentation has been used in conjunction with open reduction and internal fixation in at least one series with excellent results and no complication due to the cement [26]. However, cement injection may pose a risk should postoperative infection happen. In this case, extraction of the cement would be difficult and necessitate an extensive approach. This is, however, a theoretical risk. This concern should be addressed with the patient before the procedure. Use of bioadsorbable phosphocalcic cement may be an interesting alternative, although the biomechanical properties of the currently available compounds are much weaker than that of regular methyl-metacrylate cement.
Calcaneal fractures are a challenging problem and a number of patients have poor outcomes, even with the best techniques currently available. That is why we felt that new methods of reduction and fixation should be developed and may be of value. We remain aware that describing an application in a small series of patients without risk factors associated with a bad outcome assesses only the feasibility of the technique, and that the end-results after three years after the procedure, even if very satisfactory, are to be evaluated on a larger cohort. However, the technique provided an excellent outcome in all cases that was maintained at the latest follow-up.
Conclusion
A two-year follow-up in a limited series showing excellent outcome suggests that percutaneous balloon reduction and cement fixation of calcaneal fractures may be a promising technique that may be proposed in cases with closed fractures as a primary reduction and fixation tool. We are working on further developments to improve the technique.
References
- 1.Bajammal S, Tornetta P, 3rd, Sanders D, Bhandari M. Displaced intra-articular calcaneal fractures. J Orthop Trauma. 2005;19(5):360–364. [PubMed] [Google Scholar]
- 2.Huang PJ, Huang HT, Chen TB, Chen JC, Lin YK, Cheng YM, Lin SY. Open reduction and internal fixation of displaced intra-articular fractures of the calcaneus. J Trauma. 2002;52(5):946–950. doi: 10.1097/00005373-200205000-00021. [DOI] [PubMed] [Google Scholar]
- 3.Bezes H, Massart P, Delvaux D, Fourquet JP, Tazi F. The operative treatment of intraarticular calcaneal fractures. Indications, technique, and results in 257 cases. Clin Orthop Relat Res. 1993;290:55–59. [PubMed] [Google Scholar]
- 4.Zwipp H, Rammelt S, Barthel S. Calcaneal fractures—open reduction and internal fixation (ORIF) Injury. 2004;35(Suppl 2):SB46–SB54. doi: 10.1016/j.injury.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 5.Schuberth JM, Cobb MD, Talarico RH. Minimally invasive arthroscopic-assisted reduction with percutaneous fixation in the management of intra-articular calcaneal fractures: a review of 24 cases. J Foot Ankle Surg. 2009;48(3):315–322. doi: 10.1053/j.jfas.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Weber M, Lehmann O, Sagesser D, Krause F. Limited open reduction and internal fixation of displaced intra-articular fractures of the calcaneum. J Bone Joint Surg Br. 2008;90(12):1608–1616. doi: 10.1302/0301-620X.90B12.20638. [DOI] [PubMed] [Google Scholar]
- 7.Essex-Lopresti P (1952) The mechanism, reduction technique and results in fractures of the os calcis. Br J Surg 39(157):395–419 [DOI] [PubMed]
- 8.Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. 1993;290:87–95. [PubMed] [Google Scholar]
- 9.Heger L, Wulff K, Seddiqi MS. Computed tomography of calcaneal fractures. AJR Am J Roentgenol. 1985;145(1):131–137. doi: 10.2214/ajr.145.1.131. [DOI] [PubMed] [Google Scholar]
- 10.Janzen DL, Connell DG, Munk PL, Buckley RE, Meek RN, Schechter MT. Intraarticular fractures of the calcaneus: value of CT findings in determining prognosis. AJR Am J Roentgenol. 1992;158(6):1271–1274. doi: 10.2214/ajr.158.6.1590122. [DOI] [PubMed] [Google Scholar]
- 11.Koval KJ, Sanders R. The radiologic evaluation of calcaneal fractures. Clin Orthop Relat Res. 1993;290:41–46. [PubMed] [Google Scholar]
- 12.Muijs SP, Nieuwenhuijse MJ, Erkel AR, Dijkstra PD. Percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures: evaluation after 36 months. J Bone Joint Surg Br. 2009;91(3):379–384. doi: 10.1302/0301-620X.91B3.20970. [DOI] [PubMed] [Google Scholar]
- 13.Bano A, Pasku D, Karantanas A, Alpantaki K, Souvatzis X, Katonis P. Intra-articular calcaneal fracture: closed reduction and balloon-assisted augmentation with calcium phosphate cement: a case report. Cases J. 2009;2:9290. doi: 10.1186/1757-1626-2-9290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta AK, Gluck GS, Parekh SG (2011) Balloon reduction of displaced calcaneus fractures: surgical technique and case series. Foot Ankle Int 32(2):205–210 [DOI] [PubMed]
- 15.Sanders R. Displaced intra-articular fractures of the calcaneus. J Bone Joint Surg Am. 2000;82(2):225–250. doi: 10.2106/00004623-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Rammelt S, Zwipp H. Calcaneus fractures: facts, controversies and recent developments. Injury. 2004;35(5):443–461. doi: 10.1016/j.injury.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 17.Buckley R, Tough S, McCormack R, Pate G, Leighton R, Petrie D, Galpin R. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2002;84-A(10):1733–1744. doi: 10.2106/00004623-200210000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Court-Brown CM, Schmidt M, Schutte BG (2009) Factors affecting infection after calcaneal fracture fixation. Injury 40(12):1313–1315 [DOI] [PubMed]
- 19.Buckley RE, Meek RN. Comparison of open versus closed reduction of intraarticular calcaneal fractures: a matched cohort in workmen. J Orthop Trauma. 1992;6(2):216–222. doi: 10.1097/00005131-199206000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Potter MQ, Nunley JA. Long-term functional outcomes after operative treatment for intra-articular fractures of the calcaneus. J Bone Joint Surg Am. 2009;91(8):1854–1860. doi: 10.2106/JBJS.H.01475. [DOI] [PubMed] [Google Scholar]
- 21.Rammelt S, Gavlik JM, Zwipp H. Historical and current treatment of calcaneal fractures. J Bone Joint Surg Am. 2001;83-A(9):1438. doi: 10.2106/00004623-200109000-00040. [DOI] [PubMed] [Google Scholar]
- 22.Schepers T, Schipper IB, Vogels LM, Ginai AZ, Mulder PG, Heetveld MJ, Patka P. Percutaneous treatment of displaced intra-articular calcaneal fractures. J Orthop Sci. 2007;12(1):22–27. doi: 10.1007/s00776-006-1076-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Longo UG, Denaro V. Spinal augmentation: what have we learnt? Lancet. 2009;373(9679):1947. doi: 10.1016/S0140-6736(09)61065-5. [DOI] [PubMed] [Google Scholar]
- 24.Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, Graves S, Staples MP, Murphy B. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361(6):557–568. doi: 10.1056/NEJMoa0900429. [DOI] [PubMed] [Google Scholar]
- 25.Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, Edwards R, Gray LA, Stout L, Owen S, Hollingworth W, Ghdoke B, Annesley-Williams DJ, Ralston SH, Jarvik JG. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361(6):569–579. doi: 10.1056/NEJMoa0900563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kiyoshige Y, Takagi M, Hamasaki M. Bone-cement fixation for calcaneus fracture—a report on 2 elderly patients. Acta Orthop Scand. 1997;68(4):408–409. doi: 10.3109/17453679708996190. [DOI] [PubMed] [Google Scholar]