Abstract
The purpose of our study was to calculate the optimal tibial resection depth in total knee arthroplasty. The data from 464 navigated total knee arthroplasties were analysed. An implant with a minimum insert thickness of 8 mm was used. Data regarding leg axis, joint line, insert thickness and tibial resection depth were recorded by the navigation device. An algorithm was developed to calculate the optimal tibial resection depth. The required tibial resection significantly correlates with the preoperative leg axis (p < 0.001). In valgus deformities the required resection depth averaged 5.1 mm and was significantly reduced compared to knees with a neutral leg axis (6.8 mm, p < 0.001) and varus deformities (8.0 mm, p < 0.001). Manufacturers recommend undercutting the high side of the tibial plateau to the depth of the thinnest insert available. However, our study demonstrates that in valgus deformities a reduced tibial resection depth is preferable. Hence, unnecessary bone loss can be avoided.
Introduction
The number of primary total knee arthroplasties (TKA) performed in 2003 in the United States was approximately 418,000 and this number is expected to rise exponentially with the aging population [11]. Even with the modest annual revision rates, the number of patients requiring revision knee surgery will increase in a similar fashion [9]. The greatest challenge during revision surgery is the management of bone loss [18]. Therefore, it is a general principle to avoid unnecessary bone loss in primary TKA. Surprisingly, very little data concerning the required tibial resection depth in primary TKA exists. Implant manufacturers and navigation devices recommend undercutting the high side of the tibial plateau to the depth of the thinnest insert available, e.g. our navigation device recommends a resection depth of 8 mm. Contrary to that some experts advise a reduced tibial resection depth in fixed valgus deformities [16]. However, to our knowledge no study has systematically analysed the amount of tibial resection required in primary TKA. Therefore, it was the purpose of our study to calculate the optimal tibial resection depth in total knee arthroplasty.
Materials and methods
The data of 464 consecutive computer navigated primary knee replacements in 443 patients between July 2006 and December 2009 were analysed retrospectively. Exclusion criteria were secondary gonarthrosis due to fracture or trauma, previous osseous operations of the knee joint and revision arthroplasties.
All patients were operated upon using an imageless computer navigation device (CiKnee 1.1.2, Brainlab, Feldkirchen, Germany). All patients received a cemented PFC sigma implant (DePuy, Leeds, England) under general anaesthesia through a standard medial parapatellar approach to the knee joint. The minimum insert thickness of the PFC implant was 8 mm. The tibia first technique with identical ligament balancing procedures was always used. With the navigation device the implant position was planned to achieve a neutral leg axis, a restored joint line and a balanced extension and flexion gap. The computer navigation device was used as the measurement tool. The following data were recorded during the operative procedure: preoperative leg axis, verified resection of the medial and lateral tibial plateau referenced to the mechanical tibial axis, joint line before and after operation in 0° extension, and planned insert thickness.
The following data were recorded after operation: patient’s age, gender, side of the operation, femoral and tibial implant sizes and the insert thickness.
Algorithm of resection depth
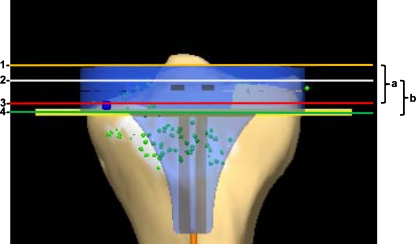
The required resection depth, as shown in Fig. 1, was calculated such that the interval (a) was defined as the distance between the cranial surface of the implanted insert (line 1) and the bottom of the lower side of the tibial plateau (line 3). As the worn out, low side of the tibial plateau (line 3) should be undercut by 2 mm, the minimal resection depth was defined as the interval (a) plus 2 mm. The optimal insert size was identified as the next available insert thickness. The unnecessary bone loss was calculated as the difference between the effectively used insert thickness and the optimal insert thickness. By the use of those data the required tibial resection depth (line 4) was calculated as the difference between the resection performed referencing the high side of the tibial plateau (b) and the unnecessary bone loss.
Fig. 1.
Algorithm of resection depth. The following lines, each of them perpendicular to the mechanical tibial axis, were defined as: 1 cranial surface of the effectively implanted insert, 2 bottom of the intact (high) side of the tibial plateau, 3 bottom of the worn out (low) side of the tibial plateau, and 4 required resection depth. The distance a was defined as the difference between lines 1 and 3; the distance b was defined as the difference between lines 2 and 4
Grouping of the patients
It was the purpose of this study to analyse the required tibial resection depth in comparison to the preoperative leg axis. As the inaccuracy of image free computer navigation in TKA has been proven to be less than 1° [12], patients were grouped as follows: valgus deformities (>1° valgus), varus deformities (>1° varus) and knee joints with a neutral leg axis (1° valgus to 1° varus).
Statistics
The data was tested for normality using the Kolmogorov-Smirnov test. A Levene's test was performed to test the equality of variances. Depending on those test results, the Students t-test or the Kruskal–Wallis test were used to determine significance which was set at 0.05. Correlations were evaluated using Pearson's correlation coefficient. The software SPSS statistics 18.0 (SPSS Inc., Chicago, IL, USA) for Windows was used for statistical analysis.
Results
Data was complete in 413 of 464 operative procedures (89.01%). With regard to the preoperative leg axis a valgus deformity >1° was assessed in 93 knee joints, a neutral axis (1° valgus to 1° varus) in 36 knee joints and a varus deformity >1° in 284 knee joints. Details of the study population are shown in Table 1.
Table 1.
Details of the study population
| Parameter | Valgus deformity | Neutral axis | Varus deformity | Total |
|---|---|---|---|---|
| Number of operative procedures (n) | 93 | 36 | 284 | 413 |
| Age (years) | 68 (11; 41–96) | 66 (10; 46–92) | 69 (8; 46–90) | 69 (9; 41–96) |
| Gender (% female) | 84 | 57 | 59 | 65 |
| Side (% left) | 39 | 31 | 51 | 46 |
| Leg axis (° varus) | −4 (2; −1 to −15) | 0 (1; −1–1) | 6 (3; 1–20) | 3 (15, −15–20) |
Values given as mean (standard deviation; range)
The high percentage of female patients in the study population and their further elevated proportion in the valgus deformity group represents the well-known epidemiology of knee osteoarthritis [8, 14].
Intraoperative data
The joint line was reconstructed with an average inaccuracy of 0.4 mm and did not significantly differ between the three groups. In valgus deformities significantly thicker inserts were used and significantly less tibial bone was resected. The difference between the resection depth of the medial and lateral tibial plateau in valgus knee joints averaged 1.4 mm and was significantly less when comparing knees with a neutral axis (2.3 mm) and varus deformities (4.5 mm). Further details concerning the intraoperative data are shown in Table 2.
Table 2.
Details of the study population
| Parameter | Grouping | Level of significance: p-values | ||||
|---|---|---|---|---|---|---|
| Valgus | Neutral | Varus | Valgus vs. varus | Valgus vs. neutral | Neutral vs. varus | |
| Femoral implant size | 3.9 (0.8; 2–6) | 3.8 (0.8; 2–5) | 4.1 (1.0; 2–6) | 0.104a | 0.960a | 0.258a |
| Tibial implant size | 3.2 (0.7; 2–5) | 3.3 (0.8: 2–5) | 3.5 (0.9; 2–5) | 0.004a | 0.518a | 0.211a |
| Insert size (mm) | 11.6 (2.4; 8–17.5) | 9.8 (2.3; 8–17.5) | 10.2 (2.2; 8–17.5) | <0.001a | <0.001a | 0.193a |
| Joint line elevation (mm) | 0.4 (1.6; −4–4) | 0.1 (1.7; −3–3) | 0.5 (1.6; −4–4) | 0.643a | 0.460a | 0.263a |
| Resection of the high side of the tibia plateau (mm) | 7.5 (1.0; 5–12) | 7.9 (0.9; 6–10) | 8.5 (1.4; 5–17) | <0.001a | <0.001a | 0.031a |
| Resection of the low side of the tibia plateau (mm) | 6.1 (1.4; 3–9) | 5.6 (1.6; 3–9) | 4.0 (1.8; −1–9) | <0.001b | 0.063b | <0.001b |
| Difference between high and low side of tibia plateau (mm) | 1.4 (1.0; 0–4) | 2.3 (1.4; 0–5) | 4.5 (2.4; 0–13) | <0.001a | <0.001a | <0.001a |
Values given as mean (standard deviation; range). Significant p-values in bold
a Kruskal–Wallis test
b Student's t-test
Calculation of the optimal resection depth
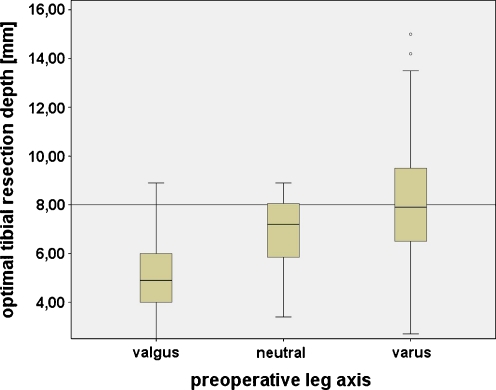
The optimal resection depth was calculated by the above-mentioned algorithm. In valgus deformities the optimal resection depth with reference to the high side of the tibia plateau averaged 5.1 mm (standard deviation [SD] 1.5, range 2.5–8.9) and was significantly reduced when comparing neutral knees (6.8 mm, SD 1.6, range 3.4–8.9; p < 0.001 [Kruskal–Wallis test]) and varus deformities (8.0 mm, SD 2.3, range 2.7–17; p < 0.001, Fig. 2). Similarly, statistical analysis resulted in a significant difference between the optimal resection depth in knee joints with a neutral axis and varus deformities (p = 0.004). As a minimum insert thickness of 8 mm was used, the optimal tibial resection depth in valgus deformities corresponded to the smallest insert thickness minus 3 mm. In varus knee joints the optimal resection depth was identical to the thinnest insert size.
Fig. 2.
The optimal tibial resection depth related to the preoperative leg axis. The axis was grouped as valgus (>1° valgus), neutral (1° valgus to 1° varus) and varus deformities (>1° varus)
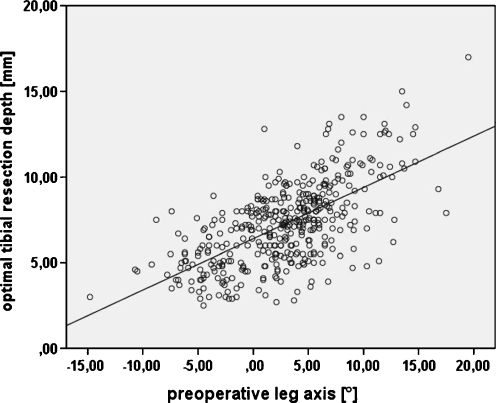
A correlation analysis was performed to further investigate the relationship between preoperative leg axis and optimal tibial resection depth. It resulted in a significant correlation between preoperative leg axis and the optimal tibial resection depth (Pearson's correlation coefficient 0.64, p < 0.001; Fig. 3).
Fig. 3.
Scatterplot of the optimal tibial resection depth in relation to the preoperative leg axis. The diagrammed line represents the linear regression line (regression coefficient 0.30, p < 0.001)
Discussion
In recent decades numerous studies dealing with improved implantation techniques of TKA have been undertaken. Most of them have analysed different ligament balancing procedures, computer navigation support or minimal invasive surgery [2, 5, 17]. The increasing knowledge about TKA allows surgeons the use of better proven procedures. However, few studies included bone resection amounts in TKA [1, 4, 5, 15], and none of them systematically analysed the required or optimal tibial resection depth. Therefore, it remains difficult to follow the primary arthroplasty principle and avoid unnecessary bone loss.
Therefore, surgeons could rely on two sources: first, recommendations of implant manufacturers and second, annotations of experienced surgeons. Implant manufacturers recommend undercutting the high side of the tibial plateau to the depth of the thinnest insert available [10]. By contrast our clinical experience leads to the hypothesis that standard resections in valgus knees lead to unnecessary bone loss and therefore higher insert sizes. Our assumption is strongly supported by this study as significantly reduced tibial resection depths and higher insert thicknesses have been found in TKA of valgus knees. In support of our hypothesis, Ekus et al. and Ranawat et al. reported a follow-up study for TKA in severe valgus knees and recommended a reduced resection depth in tibia and femur if a valgus deformity exists [6, 16]. However, no study including more precise information about the optimal tibial resection depth in TKA has been found.
Why is it important to resect as much tibial bone as required but as little as possible? First, a reduced level of bone resection during primary knee arthroplasty allows a successful revision arthroplasty as sufficient bone stock is preserved. The second reason was investigated by Berend et al. [3]—as resection depth is increased in the tibia during TKA, the surface at the tibial plateau is reduced, leading to the implantation of smaller tibial components. In addition, a more posterior position is required to maintain component placement within the tibial metaphysis. The combination of a small, posteriorly positioned tibial component contributes to increased strains. Hence an increased level of tibial resection may create an elevated risk of posteromedial bony failure and early aseptic loosening.
As far as we know our study analysed the optimal tibial resection depth for the first time. The optimal resection depth correlates with the preoperative leg axis. In valgus deformities, defined as a mechanical leg axis >1° valgus, an average resection depth of 5.1 mm was found to be enough to restore the joint line and permit a balanced extension and flexion gap. As a minimum insert thickness of 8 mm was used, an average resection depth corresponding to the smallest insert thickness minus 3 mm was enough. As some authors defined a valgus deformity as a mechanical leg axis with more than 3° valgus [8], a subgroup analysis of those patients was undertaken. Similarly, the optimal resection depth in valgus knees >3° averaged 5.0 mm. Hence our results affirm the above-cited follow-up study and technical instruction for severe valgus knee deformities stating that a reduced tibial resection depth is advisable [6, 16]. Furthermore, it demonstrates that the general recommendation of the implant manufacturers concerning the tibial resection depth is incorrect for valgus knees. For the interpretation of our results, understanding the anatomical situation in valgus knees is essential, i.e. the anatomy of the distal femur is altered in the valgus knee. The lateral femoral condyle is abnormally small, and therefore is considered to be dysplastic [7]. Instead of the normal angular relationship of the distal femur relative to the femoral shaft (average 9°) the alignment of condyles in a valgus knee is commonly 12–20° valgus to the anatomical axis of the femur. Besides this the medial ligaments are stretched and the lateral ligaments contracted. During the operative treatment of those valgus deformities the leg axis is mainly corrected by an asymmetrical resection of the femoral condyles—large resections of bone from the medial femoral condyle accompany small bone resections from the lateral femoral condyle to restore correct axial alignment of the knee [7]. Ligament balancing of those deformed knee joints is the essence of a successful TKA. Load transfer through a correctly aligned and balanced knee will optimise the longevity of the knee arthroplasty and minimise polyethylene wear [7]. Therefore, a ligament release of the contracted lateral soft tissue is always performed in valgus deformities. As the medial collateral ligaments are stretched, the result is a fairly large joint gap. It is important to emphasise that axis deformity in valgus knees is only rarely on the tibial side. Our study indicates no major deformity of the tibia plateau in valgus knees as the difference between medial and lateral tibial plateau in relation to the mechanical tibial axis averaged 1.4 mm. In summary, a reduction of the tibial resection depth in valgus deformities is possible as no tibial deformity has to be undercut and, moreover, it is reasonable to compensate the widened extension gap created by the asymmetrical femoral resection and the ligament balancing procedure.
It is important to highlight the effect of a reduced tibial resection to the joint line. In valgus deformities the reduced tibial resection leads solely to a reduction of the insert thickness. Our study indicated that the joint line in valgus knees was accurately reconstructed as the joint line shift during the operative procedure averaged 0.4 mm.
With regard to varus deformities our study resulted in conflicting findings, i.e. the optimal resection depth in varus deformities corresponded to the smallest available insert thickness. Further analysis of our data indicated that the deformity in varus knees is mainly located in the tibia; the mean height difference between the lateral and medial tibial plateau amounted to 4.5 mm. For this reason a reduced tibial resection is not reasonable in varus deformities. On the one hand, the cut would not be located below the medial bone defect and on the other hand, the reduced tibial resection would lead to increased femoral resection and therefore a joint line elevation. If the joint line is not reconstructed precisely, it may affect the knee kinematics in a negative way [13].
Limitations of our study
Our algorithm calculated the required tibial resection depth by use of the deepest point of the medial and lateral tibial plateau. These landmarks were registered during the navigation procedure. If these landmarks were marked incorrectly the algorithm results would be falsified. To minimise these potential sources of error we registered multiple points in the region of interest. The navigation device selected the deepest of those points. By use of our algorithm these landmarks were referenced to the mechanical tibial axis. This axis was defined as the line between the centre of the talus and the centre of the proximal tibia. Incorrect registration of these landmarks might also falsify the results of our calculation. These potential sources of error were investigated by Yau et al. [19]. Even sizeable registration errors of the tibial landmarks up to 9.6 mm produced only small axis deviations around 1.5°. In summary, we believe that potential registration errors of the tibial landmarks did not substantially falsify our results.
Conclusions
In TKA of valgus deformities a reduced tibial resection depth, lying about 3 mm below the thinnest insert, is usually adequate to restore the joint line. The reduced resection depth preserves adequate bone stock for eventual later revision arthroplasties and furthermore decreases the risk of aseptic implant loosing. In varus deformities a resection depth corresponding to the thinnest insert available is mostly required to undercut the medial bone defects of the tibia and to reconstruct the joint line. As that information may prevent unnecessary bone loss in valgus knee joints it should be included in operation manuals and computer navigation software.
Acknowledgments
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Bae DK, Song SJ, Yoon KH. Total knee arthroplasty following closed wedge high tibial osteotomy. Int Orthop. 2010;34:283–287. doi: 10.1007/s00264-009-0749-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bathis H, Shafizadeh S, Paffrath T, Simanski C, Grifka J, Luring C. Are computer assisted total knee replacements more accurately placed? A meta-analysis of comparative studies. Orthopade. 2006;35:1056–1065. doi: 10.1007/s00132-006-1001-3. [DOI] [PubMed] [Google Scholar]
- 3.Berend ME, Small SR, Ritter MA, Buckley CA. The effects of bone resection depth and malalignment on strain in the proximal tibia after total knee arthroplasty. J Arthroplasty. 2009;25:314–318. doi: 10.1016/j.arth.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 4.Brooks P. Seven cuts to the perfect total knee. Orthopedics. 2009;32:27. doi: 10.3928/01477447-20090101-28. [DOI] [PubMed] [Google Scholar]
- 5.Chiu KY, Yau WP, Ng TP, Tang WM. The accuracy of extramedullary guides for tibial component placement in total knee arthroplasty. Int Orthop. 2008;32:467–471. doi: 10.1007/s00264-007-0354-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elkus M, Ranawat CS, Rasquinha VJ, Babhulkar S, Rossi R, Ranawat AS. Total knee arthroplasty for severe valgus deformity. Five to fourteen-year follow-up. J Bone Jt Surg Am. 2004;86:2671–2676. doi: 10.2106/00004623-200412000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Engh GA (2003) The difficult knee: severe varus and valgus. Clin Orthop Relat Res 416:58–63 [DOI] [PubMed]
- 8.Favorito PJ, Mihalko WM, Krackow KA. Total knee arthroplasty in the valgus knee. J Am Acad Orthop Surg. 2002;10:16–24. doi: 10.5435/00124635-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Fehring TK, Christie MJ, Lavernia C, Mason JB, McAuley JP, MacDonald SJ, Springer BD. Revision total knee arthroplasty: planning, management, and controversies. Instr Course Lect. 2008;57:341–363. [PubMed] [Google Scholar]
- 10.Hartel MJ, Loosli Y, Gralla J, Kohl S, Hoppe S, Roder C, Eggli S. The mean anatomical shape of the tibial plateau at the knee arthroplasty resection level: an investigation using MRI. Knee. 2009;16:452–457. doi: 10.1016/j.knee.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 11.Lee K, Goodman SB. Current state and future of joint replacements in the hip and knee. Expert Rev Med Devices. 2008;5:383–393. doi: 10.1586/17434440.5.3.383. [DOI] [PubMed] [Google Scholar]
- 12.Lustig S, Fleury C, Goy D, Neyret P, Donell ST (2010) The accuracy of acquisition of an imageless computer-assisted system and its implication for knee arthroplasty. Knee. doi:10.1016/j.knee.2009.12.010 [DOI] [PubMed]
- 13.Martin JW, Whiteside LA (1990) The influence of joint line position on knee stability after condylar knee arthroplasty. Clin Orthop Relat Res 259:146–156 [PubMed]
- 14.Pape D, Kohn D. Soft tissue balancing in valgus gonarthrosis. Orthopade. 2007;36:657–658. doi: 10.1007/s00132-007-1104-5. [DOI] [PubMed] [Google Scholar]
- 15.Patil S, D’Lima DD, Fait JM, Colwell CW., Jr Improving tibial component coronal alignment during total knee arthroplasty with use of a tibial planing device. J Bone Joint Surg Am. 2007;89:381–387. doi: 10.2106/JBJS.F.00204. [DOI] [PubMed] [Google Scholar]
- 16.Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am. 2005;87(Suppl 1):271–284. doi: 10.2106/JBJS.E.00308. [DOI] [PubMed] [Google Scholar]
- 17.Schnurr C, Nessler J, Konig DP. Is referencing the posterior condyles sufficient to achieve a rectangular flexion gap in total knee arthroplasty? Int Orthop. 2009;33:1561–1565. doi: 10.1007/s00264-008-0656-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whittaker JP, Dharmarajan R, Toms AD. The management of bone loss in revision total knee replacement. J Bone Joint Surg Br. 2008;90:981–987. doi: 10.1302/0301-620X.90B8.19948. [DOI] [PubMed] [Google Scholar]
- 19.Yau WP, Leung A, Liu KG, Yan CH, Wong LL, Chiu KY. Interobserver and intra-observer errors in obtaining visually selected anatomical landmarks during registration process in non-image-based navigation-assisted total knee arthroplasty. J Arthroplasty. 2007;22:1150–1161. doi: 10.1016/j.arth.2006.10.010. [DOI] [PubMed] [Google Scholar]