Abstract
Purpose
The aim of our study was to review the clinical and radiological outcome of patients who had undergone anterior cruciate ligament (ACL) reconstruction in comparison to a group of non-operatively treated patients.
Methods
In a retrospective study we compared ACL reconstruction using a bone-patellar tendon-bone graft with a non-operatively treated group of patients 17–20 years later. Fifty-four patients that met the inclusion criteria, with arthroscopically proven ACL rupture, were treated between 1989 and 1991. Thirty-three patients underwent ACL reconstruction, forming group one. Eighteen non-reconstructed patients continued with rehabilitation and modification of activities (group two). The International Knee Documentation Committee (IKDC) subjective and objective evaluation forms and the Lysholm and Tegner scale were used to assess the knees at follow-up. Radiographic assessment was performed using the IKDC grading scale.
Results
Follow-up results showed that 83% of reconstructed patients had stable knees and normal or nearly normal IKDC grade. Patients in the non-reconstructed group had unstable knees with 84% having abnormal or severe laxity. The subjective IKDC score was significantly in favour of group one: 83.15 compared to 64.6 in group two. The Lysholm and Tegner score was also significantly better in group one. Conservatively treated patients all had unstable knees and worse scores. The rate of osteoarthritis showed more severe changes in non-reconstructed patients with additional meniscus injury.
Conclusions
We can conclude that 94% of patients who underwent ACL reconstruction had stable knees after 15–20 years and there was a significantly lower percentage of osteoarthritis in comparison to conservatively treated patients.
Introduction
Anterior cruciate ligament (ACL) reconstruction gives very good short- and intermediate-term results, regardless of the graft used [1–4]. Long-term studies report mostly good results ten or more years after surgery [5–9]. It has been reported that degenerative changes of the cartilage become apparent seven years after surgery [10]. They increase with time in long-term follow-up [11].
It seems that medial meniscectomy is an important factor for the onset of degenerative changes over time [12, 13]. Further factors significant for osteoarthritis (OA) are time elapsed between injury and the reconstruction and age of the patient.
There is a dilemma over whether every patient with ACL rupture should be treated operatively or not. Conservatively treated patients often cannot return to the level of their previous sports activities [14, 15]. There are some more optimistic late results with good functional scores, but early activity modification and neuromuscular rehabilitation seem to be important [16].
The aim of our study was to review the clinical and radiological outcome of patients who had undergone ACL reconstruction in comparison to a group of non-operatively treated patients. Twenty years ago almost 40% of our arthroscopically proven ACL injuries were not submitted to surgery. They preferred a modification of activities and physical therapy. Therefore, we have been able to compare operatively versus non-operatively treated patients after a relatively long time. We studied subjective symptoms, knee stability and grade of OA.
Materials and methods
This is a retrospective clinical study of patients with ACL rupture diagnosed 17–20 years ago. We have tried to avoid as much bias as possible, having an unselected population. In the period from 1989 to 1991, there were 86 patients who were treated in our hospital for an ACL injury. Among them we selected 54 patients that met the criteria of the study: acute isolated ACL injury with possible meniscus lesion, no combined or cartilage injury, or previous trauma or surgery. Age was limited up to 40 with no evident OA at the time of injury. The clinical diagnosis was confirmed on arthroscopy in all patients. After the arthroscopy, all patients were advised to undergo open ACL reconstruction. Some patients accepted surgery, and others preferred to continue with conservative treatment and modification of activities.
The study group consisted of 44 male and ten female patients. They were divided in two subgroups: in group one there were 36 patients who had undergone ACL reconstruction in the average period of 19 months after the injury (range 3–24). In group two there were 18 patients who were treated conservatively. The mean age at the time of injury was 25.3 in the first group and 25.5 in the second.
At arthroscopy the diagnosis of complete ACL rupture was confirmed and meniscectomy was performed when there was also a meniscus lesion. All patients were then treated with a plaster cast for three weeks. After that period, patients were sent to rehabilitation for two months. They performed exercises to regain full range of motion and strengthen their quadriceps. After initial rehabilitation, patients who were not operated upon modified their sports or work activities.
Surgical technique
All patients were operated upon using the same technique and by the same team of surgeons: open reconstruction with two skin incisions. The patient was placed in a supine position, with a tourniquet and the knee flexed to 90°. After regional anaesthesia, a free graft of the central third of the patellar ligament was harvested through a vertical skin incision. The graft had bone plugs 10 × 25 mm at each end, and they were secured with non-absorbable sutures. An arthrotomy was performed through the fat pad incision in the defect of the patellar ligament. The remaining tissue of the torn ACL was removed and both tibial and femoral insertion points were determined under direct vision. A second skin incision was made over the lateral femoral epicondyle. A bone tunnel 10 mm in diameter was drilled through the tibial head and the lateral femoral condyle using the C guide. The graft was pulled through from the femoral to the tibial tunnel, and both sides were fixed with non-absorbable sutures over cortical screws. After fixing the femoral side of the graft, ten to 15 full knee flexions were performed before fixing the tibial graft end. After skin closure a plaster cast was applied for two weeks and after that period rehabilitation started.
Follow-up
Follow-up examination consisted of a questionnaire, clinical examination and radiographic evaluation. The contralateral knee of the same patient served as a control. The final examination was performed by an independent observer (HJ).
The self-administrated questionnaire provided information for the subjective International Knee Documentation Committee (IKDC) score and the Tegner and Lysholm knee scores. All patients filled in our questionnaire with questions about their activities and the grade of symptoms connected with these activities. According to the answers, the IKDC subjective score was calculated for each patient. From all results, a median score was calculated for each group of patients. Another questionnaire was used for Lysholm knee score and Tegner activity scale. [17].
The functional outcome was evaluated using the IKDC evaluation form [18]. Range of motion was measured with a standard goniometer. Knee stability was tested using the manual Lachman test and KT 2000 arthrometer (MEDmetric, San Diego, CA, USA). The Lachman test was graded as negative (grade A of the IKDC scale) or positive 3–5 mm (grade B), 6–10 mm (grade C), > 10 mm (grade D). Collateral ligaments were tested manually. In all patients we tested the injured knee and the contralateral knee as a control. Radiographic assessment was done according to the IKDC evaluation form and by an independent radiologist. Bilateral weight-bearing anterior posterior, lateral and skyline patellar views were made. According to the IKDC score radiographs were classified as A, normal; B, nearly normal: minimal changes in joint space narrowing; C, abnormal: moderate changes with joint space narrowing up to 50%; and D, severely abnormal: severe changes in the whole joint with axis deviation and subluxation.
Statistical method
The outcomes between the two groups were calculated by chi-square test. P ≤ 0.05 was considered to indicate statistical significance. To search for relations between variables correlation analysis (Pearson) was applied. The average value of the Tegner activity scale was calculated as the arithmetic mean; deviation of individual patients within the group from the average value was calculated as standard deviation and coefficient of variation.
Results
Among the patients in group one, 13 (36%) had isolated ACL injury, ten (28%) had associated injury to the medial meniscus and 13 (36%) had both medial and lateral meniscus injury. In the second group (conservatively treated patients), seven patients (39%) had isolated ACL injury, while six (33%) had injury to the medial meniscus and five patients (28%) had a lesion to both menisci. There were no cases of lateral meniscus injury alone.
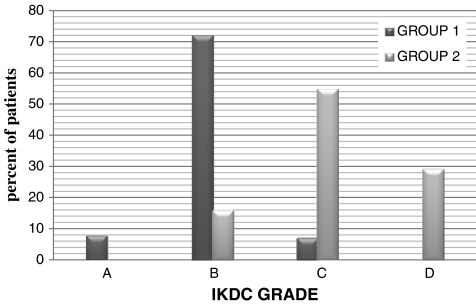
In the group of reconstructed patients, 11% had a negative anterior drawer test and 72% of patients had 0–5 mm on the anterior drawer test, graded as normal or nearly normal knees. Subjectively 83% of patients felt they had good stability in walking or sports activities. They had no pain or swelling and all had full range of motion. In the group of non-reconstructed patients only 16% had nearly normal drawer test results, but others had 10–15 mm on the anterior drawer test. They had little pain or swelling, but felt unstable in sports activities or heavy labour.
The final objective IKDC score is shown in Fig. 1.
Fig. 1.
Overall IKDC score
The subjective IKDC score showed significant differences between the two groups: in group one, the median score was 83.15 and in group two it was 64.6 (P < 0.05). It is evident that patients with a stable knee had better function and sports activity levels.
The Tegner activity scale showed that the patients in the first group had an average preinjury activity level of 6 (range 6–9) compared to 5 (range 2–9) in group two. There was no significant difference in preinjury activity level between the two groups (P < 0.05).
After surgery, there was a shift; the average activity level in group one decreased to 5 (range 2–9), meaning that some of the patients dropped one or two levels. In the group of non-operated patients, the average level after the injury was 4 (range 2–6). The Tegner activity scale showed a significantly lower level of activity after the injury in group two compared to group one (P < 0.05)
The results in the Lysholm knee scale regarding limping, swelling, instability, walking on stairs and pain showed significant differences between the two groups: the median score in group one was 84.3 = good, and in group two it was 53.3 = poor (P < 0.05). As most of the patients in group two had evident anterior translation, they also had more pain, swelling and giving way.
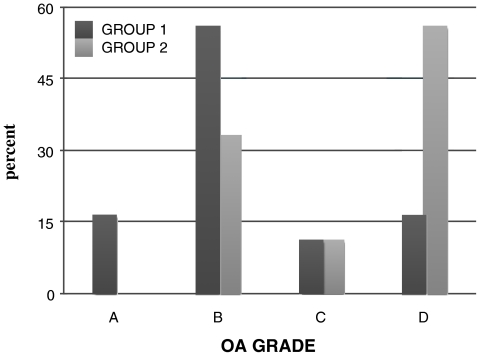
The development of degenerative changes is shown in Fig. 2.
Fig. 2.
Distribution of OA at follow-up
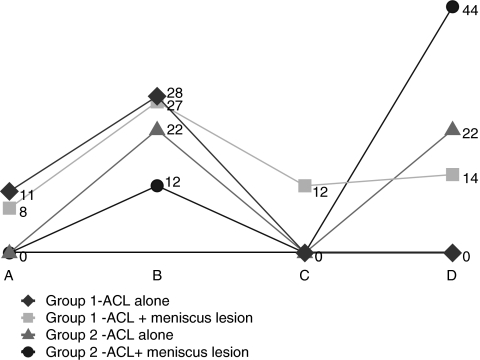
Half of the patients in group one had mild degenerative changes but 16.5% had severe OA. In conservatively treated patients there were no normal knees; 56% of the patients had severe OA, which is a statistically significant difference (P < 0.05). The distribution of OA in relation to associated meniscus injury showed a scattered pattern. Still, the highest percentage was present in conservatively treated patients with meniscus lesion (Fig. 3).
Fig. 3.
Distribution of OA incorrelation to meniscus injury
Discussion
This retrospective clinical study is a comparison of reconstructed and non-reconstructed ACL injuries with long-term results with a follow-up 17–20 years. Our results show that the majority of reconstructed patients had stable knees and a good functional score. In the mid-1980s in our region many patients decided against operation and preferred conservative treatment with a modification of activities. This is why about 40% of the patients were not treated surgically. We have tried to avoid the bias of a heterogenic population. There was no significant difference in age, occupation or sports activities between the two groups before injury (P < 0.05).
At follow-up non-operated patients had worse subjective and objective scores. They were free of symptoms in daily walking, but experienced difficulties in going down stairs, felt giving way while walking on uneven grounds and could not jump on the involved leg. The majority had increased laxity with Lachman over 10 mm. We find it logical that knees with unreconstructed ACL would have increased anterior laxity even 20 years after injury. The Tegner activity scale showed that three of eight competitive athletes maintained the same level of sports after the ACL reconstruction. Others switched two levels down and continued with recreational activities. A further seven patients participating in recreational sports (level 6 activities) maintained the same level after the surgery. On the other hand, in non-operated patients there were two competitive athletes who gave up sports completely and reduced activities to level 4. Nevertheless, six of eight patients with level 6 were able to maintain the same level of recreational activities. Sometimes athletes with good objective scores after ACL reconstruction do not return to the same level of competition, explaining it as a “fear of a second injury” [19]. Streich et al. [20] published a similar report, comparing operative versus conservative treatment of ACL deficiency, but their results differ strongly. They found no significant difference in subjective scores between two groups, and surprisingly their overall IKDC score showed 40% nearly normal in reconstructed patients and 42.5% nearly normal knees in non-reconstructed patients. The rate of OA was higher in patients with positive pivot shift test, but there was no significant difference in severe OA between the two groups. Previous publications have reported that a variety of OA grade was found at long-term follow-up, depending on the patient’s age, the time elapsed from injury to the reconstruction, residual laxity or meniscectomy [4, 7, 8, 11]. However, in the early years of ACL reconstruction, the time from injury to the surgery was often over 18 months. None of our patients had osteoarthritic changes at the time of injury. At the follow-up we found that even patients with stable knees after ACL reconstruction develop degenerative changes after 15–20 years, mostly mild, but in 16.5% the changes were severe. In the literature the percentage and grade of OA are vaguely described. We discovered that non-reconstructed knees showed a higher prevalence of severe OA. Our study also confirms the importance of an additional meniscus lesion. In the group of reconstructed patients there was a significant prevalence of severe OA (P < 0.5) in cases with an additional medial lesion or lesion to both menisci. In non-reconstructed knees this prevalence was even higher, rising to 44%. Mild degenerative changes were present in 28% of isolated ACL tears in reconstructed patients and in 22% of non-reconstructed knees. We have addressed the residual knee laxity and meniscectomy as principal factors for the onset of OA. We did not take other potential factors into consideration (body mass index, gender or genetic factors).
Our conclusion is that conservatively treated patients had unstable knees with increased anterior laxity and higher rate of severe degenerative changes. We also found that reconstruction of ACL cannot prevent OA; it can only lead to a lower prevalence of its onset.
References
- 1.Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR. Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31:2–11. doi: 10.1177/03635465030310011501. [DOI] [PubMed] [Google Scholar]
- 2.Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564–574. doi: 10.1177/0363546506296042. [DOI] [PubMed] [Google Scholar]
- 3.Salmon LJ, Russel VJ, Refshuage K, Kader D, Conolly C, Linklater J, Pincewski LA. Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med. 2006;34:721–732. doi: 10.1177/0363546505282626. [DOI] [PubMed] [Google Scholar]
- 4.Zaffagnini S, Marcacci M, Lo Presti M, Giordano G, Iacono F, Neri MP. Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc. 2006;14:1060–1069. doi: 10.1007/s00167-006-0130-x. [DOI] [PubMed] [Google Scholar]
- 5.Asik M, Sen C, Tuncay I, Erdil M, Avci C, Taser OF. The mid- to long-term results of the anterior cruciate ligament reconstruction with hamstring tendons using Transfix technique. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):965–972. doi: 10.1007/s00167-007-0344-6. [DOI] [PubMed] [Google Scholar]
- 6.Jäger A, Welsch F, Braune C, Eberhard C, Kappler C. 10-Jahres-Ergebnisse nach arthroskopischer vorderer Kreuzbandrekonstruction mit dem Patellarsehnentransplantat. Z Orthop Ihre Grenzgeb. 2003;141:42–47. doi: 10.1055/s-2003-37361. [DOI] [PubMed] [Google Scholar]
- 7.Jomha NM, Borton DC, Clingeleffer AJ, Pincewski LA. Long-term osteoarthritic changes in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1999;358:188–193. doi: 10.1097/00003086-199901000-00023. [DOI] [PubMed] [Google Scholar]
- 8.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756–1769. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 9.Maletius W, Messner K. Eighteen- to twenty-four-year follow-up after complete rupture of the anterior cruciate ligament. Am J Sports Med. 1999;27:711–717. doi: 10.1177/03635465990270060501. [DOI] [PubMed] [Google Scholar]
- 10.Ait Si Selmi T, Fithian D, Neyret P. The evolution of osteoarthritis in 103 patients with ACL reconstruction at 17 years follow-up. Knee. 2006;13(5):353–358. doi: 10.1016/j.knee.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 11.Ferretti A, Conteduca F, Carli A, Fontana M, Mariani PP. Osteoarthritis of the knee after ACL reconstruction. Int Orthop. 1991;15:367–371. doi: 10.1007/BF00186881. [DOI] [PubMed] [Google Scholar]
- 12.Cohen M, Amaro JT, Ejnisman B, Carvalho RT, Nakano KK, Peccin MS, Teixeria R, et al. Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthrosis. Arthroscopy. 2007;23(6):629–634. doi: 10.1016/j.arthro.2007.03.094. [DOI] [PubMed] [Google Scholar]
- 13.Järvelä T, Kannus P, Järvinen M. Anterior cruciate ligament reconstruction in patients with or without accompanying injuries: a re-examination of subjects 5 to 9 years after reconstruction. Arthroscopy. 2001;17:818–825. doi: 10.1016/S0749-8063(01)90004-0. [DOI] [PubMed] [Google Scholar]
- 14.Kannus P, Järvinen M. Conservatively treated tears of the anterior cruciate ligament. Long term results. J Bone Joint Surg Am. 1987;69(7):1007–1012. [PubMed] [Google Scholar]
- 15.Scavenius M, Bak K, Hansen S, Nørring K, Jensen KH, Jørgensen U. Isolated total ruptures of the anterior cruciate ligament—a clinical study with long-term follow-up of 7 years. Scand J Med Sci Sports. 1999;9(2):114–119. doi: 10.1111/j.1600-0838.1999.tb00219.x. [DOI] [PubMed] [Google Scholar]
- 16.Kostogiannis I, Ageberg E, Neuman P, Dahlberg L, Fridén T, Roos H. Activity level and subjective knee function 15 years after anterior cruciate ligament injury: a prospective, longitudinal study of nonreconstructed patients. Am J Sports Med. 2007;35(7):1135–1143. doi: 10.1177/0363546507299238. [DOI] [PubMed] [Google Scholar]
- 17.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 18.Irrgang JJ, Ho H, Harner CD, Fu FH. Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6:107–114. doi: 10.1007/s001670050082. [DOI] [PubMed] [Google Scholar]
- 19.Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc. 2006;14(10):1021–1028. doi: 10.1007/s00167-006-0050-9. [DOI] [PubMed] [Google Scholar]
- 20.Streich N, Zimmermann D, Bode G, Schmitt H. Reconstructive versus non-reconstructive treatment of anterior cruciate ligament insufficiency. A retrospective matched-pair long-term follow-up. Int Orthop. 2010 doi: 10.1007/s00264-010-1174-6. [DOI] [PMC free article] [PubMed] [Google Scholar]