Abstract
The objective of this study was to compare replacement of the radial head by metal prostheses with open reduction and internal fixation (ORIF) for the treatment of unstable, multi-fragmented radial head fractures. A prospective randomised controlled trial was employed to investigate 45 patients with unstable, multi-fragmented fractures of the radial head, from January 2004 to June 2007. The patients were randomised to two groups: the ORIF group and the radial head replacement group. Over the next two years, follow-up assessments recorded Broberg and Morrey scores and postoperative complication rate. Statistical analysis was performed. According to Broberg and Morrey scores, patients receiving radial head replacement achieved significantly better clinical results with 91% (20/22) good or excellent compared to patients assigned to the ORIF group with 65.2% (15/23) good or excellent results (P < 0.01). Postoperative complication rate of the radial head replacement group (13.6%) was significantly lower than that of the ORIF group (47.9%; P < 0.01). Compared with open reduction and internal fixation, radial head replacement with a metal prostheses resulted in favourable joint function for the unstable, multi-fragmented fractures of the radial head.
Introduction
With the development of techniques and implants for micro-fractures, the important role of the radial head in the elbow joint and stability of the forearm have aroused greater attention. Significant changes have taken place in the treatment of comminuted radial head fractures. The traditional resection of the radial head is seldom adopted due to complications of instability of the elbow joint, muscle force regression and proximal radius dislocation. Another complication of radial head resection is postero-lateral rotatory instability. Hall et al. [1] have identified a series of patients with postero-lateral rotatory instability following radial head resection. Lindenhovius et al. [2] found that radial head excision had a higher risk of subsequent elbow dislocation and long-term arthrosis compared to open reduction and internal fixation (ORIF). Although, there are some reports stating that most patients with an isolated comminuted fracture of the radial head treated nonoperatively or with a radial head excision report no or only minor long-term complaints [3]. Currently, the two major treatments for unstable comminuted radial head fractures are replacement of the radial head with metal prostheses and open reduction and internal fixation (ORIF) of the radial head, each with its successful cases and flaws. The purpose of this study was to compare the therapeutic effects of these two methods on comminuted radial head fractures by analysing the function of the elbow joint and the forearm.
Subjects and methods
A prospective randomised controlled trial was employed in this study to compare the therapeutic effects of radial head replacement by metal prostheses with open reduction and internal fixation of the radial head. All of the patients were followed-up for two years. This study was authorised by the hospital ethics committee. The patients included all signed informed consent documents in the presence of a third party.
All of the patients were randomly divided into the radial head replacement group (22 cases) and the ORIF group (23 cases). The patients of the ORIF group received open reduction and internal fixation of the radial head. The follow-up took four years from January 2004 to January 2009. Each case was reviewed at least at one follow-up. The average length of follow-up was 2.8 years (range, 1–5 years) with no loss of follow-up. All of the reviewers were blinded to evaluate postoperative functions by means of a randomised block design. Of the 45 patients, 76% were men and 24% were women, with an average age of 37 years (range, 19–68). The average delay between injury and surgery was 4.9 days.
Radial head prostheses and internal fixation materials
The patients in the radial head replacement group reveived a monopolar titanium radial head prostheses matched to each individual from Wright Medical Technology. The ORIF group were treated using the AO mini steel plate interfixed system combined with Kirschner wires.
Perioperative management
Under general anaesthesia and using a tourniquets, the radial head replacement operations were performed by the same surgeon. The Kocher approach was used to expose the radial head fractures for radial head excision and implanting the prostheses. A medulla dilation drill was used to enlarge the medulla until the intra-medullary bone cortex was reached. The prostheses were tried from the small size to the large until the right size was determined. Also, clinical and radiological examinations were undertaken to confirm the stability of the elbow joint and the neck and the suitability of the prostheses. After replacement, the annular ligaments were sutured, but not too tight in order not to affect the supination of the forearm. Collateral ulnar ligament complex injuries were fixed and reconstructed operatively. Complicating fractures were dealt with simultaneously. Active exercises were started after three to seven days rest in a splint except for cases of additional elbow injuries. If complicating injuries were present, the elbow joints were rested in a 60° flexion position for three weeks followed by rehabilitation exercises, with gradually increased intensity.
Under direct vision, the ORIF group also used the Kocher approach to fully expose the radial head and reduction was undertaken. In ten cases, the shattered multi-fragmented bones were arranged externally. After the radial heads were reconstructed, they were fixed with two to three lag screws. Afterwards, two Kirschner wires of 1.8-mm diameter were used to fix the radial head on the neck of the radius. The needle ends were buried beneath the radial head cartilage. Radial head fractures in eight cases were fixed with one to three lag screws and five cases with T-shaped metacarpal bone steel plates. Under direct vision, we could see the fractures with sound apposition and no limit of rotation. The same method was used to fix the annular ligaments in the radial head replacement group. Injuries of the collateral ulnar ligaments complex were reconstructed operatively, and the associated fractures should be managed with the same method used in the radial head replacement group. Postoperatively, for patients with associated injuries, long-arm cast plaster was used to immobilise the elbow at 90°, which was changed to short-arm cast plaster after two weeks. Meanwhile, active rotation of the forearm was allowed. After four weeks, the plaster was removed followed by rehabilitation exercises. For patients without associated injuries, the elbow joints were suspended at 90° for two weeks and active rotational movement of the forearm was undertaken. Two weeks later, active flexion–extension movement was recommended. The whole process was taken with gradually increased intensity.
Clinical evaluation and complications
The postoperative clinical examination followed the Broberg and Morrey System [4–6], an established functional evaluation score for the elbow. The score ranges from 0 to 100 based on four criteria of range of motion, grip strength, functional stability, and pain. Clinical and radiological examinations (flexion, extension, pronation supination and X-ray examinations) were carried out at the fourth to sixth weeks, sixth month and 18th month (average, 26 ± 3.2 months; range, 21–37 months). The flexion–extension examinations were made in the neutral position, and the pronation-supination examinations were measured at 90° flexion of the elbow. A tension meter was used to measure the force of flexion, extension, pronation and supination compared with the unaffected extremities. A goniometer was used to measure the range of flexion–extension and rotation of the elbow. X-ray was used to observe the healing of the fractures and the apposition of the joints. Meanwhile, heterotopic ossification was noted. All clinical assessments in this research were accomplished by independent observers.
In the follow-up, postoperative complications included the following: deep wound infection, range of motion deficit >30°, no or delayed healing, internal fixation failure, secondary fragment displacement, joint stiffness and heterotopic ossification. Restriction of joint movement, which is commonly seen after elbow injuries, was classified as a complication when over 30°.
Statistics
The statistical analysis was performed using SPSS 12.0 (SPSS Inc., Chicago, IL, USA). For the treatment result, differences between the two groups were compared by t test and Chi-square test. In all cases, a p value of 0.05 was assumed to denote statistical significance.
Results
This study selected patients with Mason III type unstable comminuted radial head fractures [7] who visited our hospital from January 2004 to June 2007. The radial head fracture types were based on Mason classification. According to the inclusion and exclusion criteria (Table 1), 48 patients were enrolled in the primary design, among whom, two chose bipolar radial head replacement and one chose radial head resection. Forty-five patients entered the final trial. All the patients were followed-up for two years according to the elbow functional evaluation criteria of Broberg and Morrey (Table 2). The outcome was considered to be satisfactory if the result was good or excellent and unsatisfactory if it was fair or poor. The outcome was satisfactory in 91% of patients in the replacement group and in 65.2% of patients in the ORIF group. The difference was statistically significant (P < 0.01).
Table 1.
Inclusion and exclusion criteria for the radial head fracture study
| Inclusion criteria | Exclusion criteria |
|---|---|
| Mason III type radial head fracture | Mason I, II type radial head fracture |
| Including multiple injuries: collateral ulnar ligament injury | Severely comminuted radial head fracture |
| Ulnar coronoid process fracture | Old radial head fracture |
| Ulnar anconeal process or ulnar proximal end fracture | Children with radial head fracture |
| Interosseous ligament injury | Psychological and/social conditions with poor compliance |
| Posterior cubital articulation dislocation |
Table 2.
Broberg and Morrey elbow scores at two-year follow-up
| Procedure | Elbow score mean ± SD | Number of patients (%) | ||||
|---|---|---|---|---|---|---|
| Excellent | Good | Fair | Poor | Total | ||
| Replacement | 92.1 ± 6.8 | 15 (68.2) | 5 (22.8) | 1 (4.5) | 1 (4.5) | 22 (100) |
| ORIF | 72.4 ± 7.1 | 9 (39.1) | 6 (26.1) | 5 (21.7) | 3 (13.1) | 23 (100) |
SD standard deviation, ORIF open reduction and internal fixation
There was no significant difference in the average scores of the two groups (P < 0.01)
Table 3 shows complications from a total of 45 patients. Among 22 patients in the replacement group, range of motion deficit more than 30° occurred in two cases and joint stiffness occurred in one case due to unsuitable long prostheses. In the ORIF group, one case failed to unite, three cases with internal fixation failure and secondary fragment displacement within an average of six months and four cases with second-stage radial head replacement having good outcomes. Heterotopic ossification was found in two cases on X-ray re-examination two years postoperatively. Internal fixation was removed within eight to ten months in 19 patients out of 23. Complication rates between two groups were 13.6% and 47.9% with statistical significance (P < 0.01).
Table 3.
Post-surgical complications at any follow-up
| Complication type | Replacement, N = 22 | ORIF, N = 23 |
|---|---|---|
| Range of motion deficit >30° | 2 (9.1) | 4 (17.4) |
| Stiffness caused by prostheses | 1 (4.5) | 0 (0) |
| No healing | 0 (0) | 1 (4.3) |
| Secondary fragment displacement | 0 (0) | 3 (13.1) |
| Deep wound infection | 0 (0) | 1 (4.3) |
| Heterotopic ossification | 0 (0) | 2 (8.7) |
| Total | 3 (13.6) | 11 (47.9) |
ORIF open reduction and internal fixation
Data given as number of patients (%)
The prosthesis replacement group had better clinical effects than the ORIF group and the total difference was statistically significant
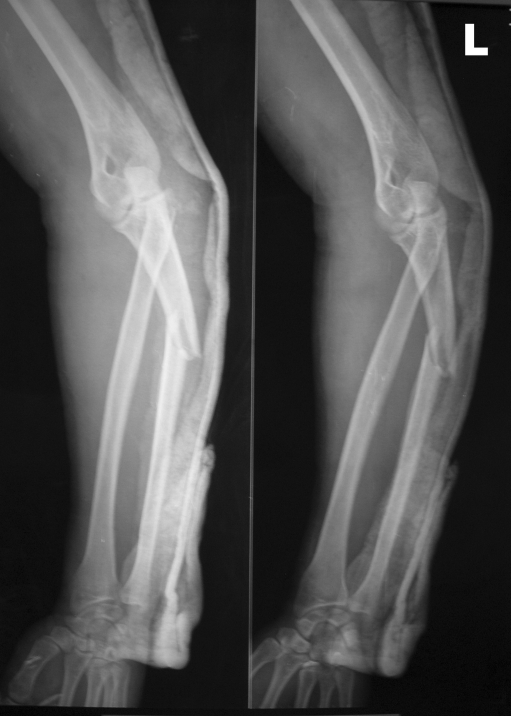
Typical case 1 A 27-year-old man fell from height and sustained a left radial head comminuted fracture associated with a dislocation of the elbow. The fracture type was classified as Mason type III (Fig. 1). On the second day, under brachial plexus anaesthesia, left radial head replacement was undertaken. In the re-examination after 24 months, X-ray showed that the result was satisfactory without obvious heterotopic ossification. The Broberg and Morrey score was 95 (Figs. 2 and 3).
Fig. 1.
A left radial head comminuted fracture associated with a dislocation of the elbow was classified as Mason type III
Fig. 2.
On the second day, left radial head replacement was undertaken. In the reexamination after 24 months, X-ray showed no obvious heterotopic ossification. The Broberg and Morrey score was 95
Fig. 3.

The patient showed normal elbow appearance and excellent functions
Typical case 2 A 35-year-old man sustained a right radial head comminuted fracture associated with a posterior luxation of the elbow due to a traffic accident. The fracture type was classified as Mason type III. On the fifth day, under brachial plexus anaesthesia, right radial head replacement was undertaken. In the re-examination after 26 months, the X-ray showed no obvious heterotopic ossification. The Broberg and Morrey score was 93.
Discussion
Radial head fractures occur in about 17–19% of cases of elbow trauma and account for 33% of elbow fractures [8]. Mason type I fractures can be managed without surgery and Mason type II fractures can be managed with open reduction and internal fixation with excellent results achieved [9, 10]. Most clinicians have personally experienced dissatisfaction with the treatment of radial head fractures of Mason type III, which has many surgical options, and this has resulted in controversy.
The early treatments of unstable and comminuted radial head fractures included excision of the radial head. However, in the follow-up, we found that excision led to a high complication rate. Several significant complications were symptoms at the wrist, degenerative arthritis and so on [11]. With the development the understanding of biomechanics, the role of the radial head in the elbow, mainly force transmission and elbow stability maintenance, are attracting greater attention. Experiments have demonstrated that after radial head excision, elbow extension decreased by 30%. When the collateral ulnar ligaments were injured, the integrity of brachioradial articulation was an important factor for elbow stability maintenance [12–14]. Ring et al. [15] reported that four patients out of 11 who underwent Terrible triad fractures and radial head excision presented with articulation instability. Josefsson et al. [16] reported that out of 19 patients with elbow fractures and dislocation who undertaken radial head excision, three presented with redislocation and outof 15 patients followed-up 11 had post-traumatic arthritis. We found that in radial head fractures associated with collateral ulnar ligament injuries, when the radial heads were excised, even followed by collateral ulnar ligament repair, ligament looseness would occur, leading to increasing probability of rupture.
Increasing popularity of the novel technique—internal fixation—for the treatment of mini fractures and growing importance attached to the radial head result in the tendency to preserve comminuted radial heads by internal fixation. A number of doctors reported that ORIF could achieve satisfactory results in the treatment of comminuted radial heads [17–19]. Nevertheless, we maintain that these results might result from stable comminuted radial head fractures. Recent researches have demonstrated that after internal fixation operations, unstable, dislocated and comminuted radial head fractures tended to develop internal fixation failures, nonunions and forearm rotation impairment. Ring et al. [20] reported the effects of internal fixation for complex radial head fractures. Of 26 patients with Mason III type radial head fractures, ten required revision for fixation failure, healing failure and chronic, persistent pain. In the remaining 16 patients, five reported unsatisfactory results. Heim et al. [21] demonstrated that fractures in six out of 11 patients with ORIF for comminuted radial head fractures failed to heal. Cai et al. [22] reported that results of the follow-up of nine patients with Mason type III radial head fractures, who underwent open reduction and mini-steel plate interfixed operations, achieved only 22% satisfaction rate. In our study, of 23 patients in the ORIF group, one ended with nonunion, two with severe heterotopic ossification and three with internal fixation failure, severely impairing joint functions. The total satisfaction rate was only 65.2%. We believe that for unstable and comminuted radial head fractures, the failure rate of internal fixation is relatively high, which should be taken into account.
Therefore, for comminuted and unstable radial head fractures, radial head replacement with prostheses is an appropriate option to best reconstruct stable structures of the elbow and avoid weakness, pain and instability afterwards. Harrington et al. [23] reported that of 20 cases with titanium radial head replacement and an average 12 (range, 6–9) years’ follow-up, 16 cases reported excellent or good results with no prostheses-related complications. They believed metal radial head replacement was able to restore stability of the elbow and prevent proximal displacement of the radius, thus reducing extension of the elbow and complications of the ulnoradial joint. Grewe et al. [24] believed that standard-designed prostheses for comminuted radial head fractures were safe and effective with satisfactory results and least function impairments.
Twenty two cases were involved with two years’ follow-up. According to Broberg and Morrey scores, 91% presented with excellent or good results. Based on our experience, prosthesis replacement should abide by the following rules. Radial head prosthesis replacement should be restricted to its indications, mainly the unstable and comminuted radial head fractures, including Mason type III radial head fractures associated with collateral ulnar ligaments injury or Essex-Lopresti injury, ulnar coronoid process fractures, proximal ulnar fractures or ulnar anconeal process fractures and severely comminuted radial head fractures. For those relatively stable, comminuted radial head fractures devoid of associated fractures and ligament injury, i.e. less than three bone fragments, radial heads should be preserved. Because prostheses have problems of loosening, wearing and matching with neighbouring articulations. Researches by Pomianowski et al. [25] revealed that no prosthesis could fully restore the articular stability. Thus, it is necessary to strictly evaluate the indications. Second, during the operation, it is mandatory to determine the position for the radial head amputation. Accurate evaluation should be made using prostheses models to avoid too much bone being excised. Harrington et al. [23] reported that of 20 cases with titanium radial head replacement, four cases with unsatisfactory results were closely related to the inappropriate length of the radius neck. After elongating (2.5 mm and 5.0 mm) and shortening (2.5 mm and 5 mm) the radius necks, Glabbbeek et al. [26] evaluated effects of the length of the prosthetic radius neck on movement of the elbow and the pressure of the articulation. Results suggested that accurately restoring the length of the radius was of overriding importance. Kinematical parameters and pressure of the brachioradial articulation would change when elongating or shortening distance was over 2.5 mm. Too much excision would result in semi dislocation while too little would cause articular pain and stiffness. Third, it is significant to choose the right surgery time. Prosthesis replacement operations should be reserved for those with the correct indications. Some doctors believe that ORIF could be taken at the first stage. If it is unsatisfactory, prosthesis replacement could be done at the second stage. We think that contraction of soft tissue scars by multiple operations will greatly affect functions of the elbow. Also, multiple operations will increase the risk of heterotopic ossification.
We conclude that, in this study, metal prosthetic radial head replacement was more effective than traditional open reduction and internal fixation in clinical practice. However, prostheses have problems of aging, looseness and wear. Because this technique has only been in use clinically for a relatively short time, there is no information about durability. Furthermore in view of problems with wear and loosening further studies are required.
Acknowledgments
Conflicts of interest The authors declare they have no conflicts of interest.
Footnotes
Xiao Chen and Si-cheng Wang contributed equally to this work.
Contributor Information
Xiao Chen, Phone: +86-135-64661943, Email: sirchenxiao@126.com.
Jia-can Su, Email: sujiacan@yahoo.com.cn, Email: trauma8888@yahoo.com.cn.
References
- 1.Hall JA, McKee MD. Postero-lateral rotatory instability of the elbow following radial head resection. J Bone Joint Surg Am. 2005;87:1571–1579. doi: 10.2106/JBJS.D.02829. [DOI] [PubMed] [Google Scholar]
- 2.Lindenhovius AL, Felsch Q, Doornberg JN, et al. Open reduction and internal fixation compared with excision for unstable displaced fractures of the radial head. J Hand Surg Am. 2007;32(5):630–636. doi: 10.1016/j.jhsa.2007.02.016. [DOI] [PubMed] [Google Scholar]
- 3.Karlsson MK, Herbertsson P, Nordqvist A, et al. Comminuted fractures of the radial head. Acta Orthop. 2010;81(2):226–229. doi: 10.3109/17453671003717815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68:669–674. [PubMed] [Google Scholar]
- 5.Geel C, Palmer A, Ruedi T, Leutenegger A. Internal fixation of proximal radial head fractures. J Orthop Trauma. 1990;4:270–274. doi: 10.1097/00005131-199004030-00006. [DOI] [PubMed] [Google Scholar]
- 6.Geel CW, Palmer AK. Radial head fractures and their effect on the distal radioulnar joint. A rationale for treatment. Clin Orthop Rel Res. 1992;275:79–84. [PubMed] [Google Scholar]
- 7.Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg. 1959;42:123–132. doi: 10.1002/bjs.18004217203. [DOI] [PubMed] [Google Scholar]
- 8.Morrey BF. Radial head fracture. In: Merrey BF, editor. The elbow and its disorders. 2. Philadelphia: WB Saunder; 2000. pp. 341–364. [Google Scholar]
- 9.Dooley JF, Angus PDRS. The importance of elbow aspiration when treating radial head fractures. Arch Emerg Med. 1991;8:117–121. doi: 10.1136/emj.8.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prokop A, Jubel A, Helling HJ, et al. New biodegradable polylactide implants (Polypin C) in therapy for radial head fractures. Chirurg. 2002;73:997–1004. doi: 10.1007/s00104-002-0545-y. [DOI] [PubMed] [Google Scholar]
- 11. Lu YP, Xu ST (1991) Orthopaedic surgery. People's Military Medical Press 449
- 12.Hotchkiss RN. Fracture of the radial head and related instabilits and contracture of the forearm. Instr Course Lect. 1998;47:173–177. [PubMed] [Google Scholar]
- 13.Hotchkiss RN. Displaced fractures of the radial head internal fixation or excision? J Am Acad Orthop Surg. 1997;5:1–10. doi: 10.5435/00124635-199701000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Morrey BF, Chao EY, Hui FG. Biomechanical study of the elbow following excision of the radial head. J Bone Joint Surg Am. 1979;61:63–68. [PubMed] [Google Scholar]
- 15.Ring D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am. 2002;84:547–551. doi: 10.2106/00004623-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Josefsson PO, Gentz CF, Johnell O, et al (1989) Dislocations of the elbow and intraarticular fractures. Clin Orthop Relat Res 246:126–130 [PubMed]
- 17.Geel CW, Palmer AK, Rüedi T, Leutenegger AF. Internal fixation of proximal radial head fractures. J Orthop Trauma. 1990;4:270–274. doi: 10.1097/00005131-199004030-00006. [DOI] [PubMed] [Google Scholar]
- 18.Kelberine F, Basseres B, Curvale G, et al. Fractures of the radial head: an analysis of 62 surgically treated cases. Rev Chir Orthop. 1991;77:322–328. [PubMed] [Google Scholar]
- 19.Pearce MS, Gallannaugh SC. Mason type II radial head fractures fixed with Herbert bone screws. J R Soc Med. 1996;89:340–344. doi: 10.1177/014107689608900616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ring D, Quintero J, Jupiter JB. Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg Am. 2002;84:1811–1815. doi: 10.2106/00004623-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Heim U. Surgical treatment of radial head fracture. Z Unfallchir Versicherungsmed. 1992;85:3–11. [PubMed] [Google Scholar]
- 22.Cai PH, Mei HG, Fan Yi C, et al. Clinical efficacy of internal fixation on Mason type III radial head fractures. Chin J Orthop Trauma. 2004;5:496–498. [Google Scholar]
- 23.Harrington U, Sekyi-Otu A, Barrington TW, et al. The functional outcome with metallic radial head implants in the treatment of unstable elbow fractures: a long-term review. J Trauma. 2001;50:46. doi: 10.1097/00005373-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Grewel R, MacDermid J, Faber K, et al. Comminuted radial head fractures treated with a modular metallic radial head arthroplasty: a study of outcomes. J Bone Joint Surg Am. 2006;88:2191–2200. doi: 10.2106/JBJS.E.00962. [DOI] [PubMed] [Google Scholar]
- 25.Pomianowski S, Morrey BF, Neale PG, et al. J Bone Joint Surg Am. 2001;83(12):l829–l834. doi: 10.2106/00004623-200112000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Glabbeek F, Riet RP, Baumfeld JA, et al. Detrimental effects of overstuffing or understuffing with a radial head replacement in the medial collateral-ligament deficient elbow. J Bone Joint Surg Am. 2004;86(12):2629. doi: 10.2106/00004623-200412000-00007. [DOI] [PubMed] [Google Scholar]