Abstract
The aim of this study was to evaluate the long-term results of conservative and surgical fragment excision treatment in patients with Pipkin type 1 fractures of the femoral head associated with posterior dislocation of the hip by a randomised controlled trial. Sixteen patients were randomly divided into two groups: the conservative group was treated by closed reduction, and the surgical group was treated by closed reduction followed with fragment excision. Functional outcome was determined using the Thompson and Epstein score and the Merle d’Aubigne and Postel score. Outcome of the conservative group was worse than that of the surgical group (p = 0.032). The randomised controlled trial proves surgical fragment excision after closed reduction is an effective treatment for Pipkin type 1 fractures.
Introduction
With increasing numbers of road traffic accidents, fracture of the femoral head after hip dislocation is becoming more common. Statistics showed that 11.7% of hip dislocations were associated with a femoral head fracture and that 84% of patients had been victims of an automobile accident [8]. The Pipkin’s classification system is the most commonly used to evaluate these fractures [13]. For Pipkin type 1 fractures, there is still no clear evidence indicating whether to treat the fracture conservatively or operatively. Post-traumatic changes, such as heterotopic ossification, avascular necrosis of the femoral head and osteoarthritis may lead to a restriction in hip function and permanent disability, even in young patients. The choice treatment for Pipkin type 1 fractures remains controversial [10, 11, 14, 17]. The absence of a validated outcome instrument has contributed to the lack of absolute recommendations and indications for the most appropriate treatment of femoral-head fractures associated with hip dislocations [16].
The aim of this study is to evaluate the long-term results of conservative and surgical fragment excision treatment in patients with Pipkin type 1 fractures of the femoral head associated with posterior dislocation of the hip by a randomised controlled trial.
Materials and methods
From 2002 to 2008, we preselected 16 patients with Pipkin type 1 fractures and divided them into two groups randomly, each group comprising eight patients. The conservative group was treated by closed reduction, and the surgical group was treated by surgical fragment excision after closed reduction. Inclusion criteria were patients with Pipkin type 1 fractures of the femoral head associated with posterior dislocation of the hip, aged 18–60 years, less than 12 hours between injury and reduction; no sciatic nerve injury; no previous injury in hip. Exclusion criteria were pathological fracture of the femoral head or associated severe multiple injuries, including brain injury. In the conservative group, immediate closed reduction of the fracture dislocation of the hip was carried out under general or epidural anaesthesia. The limb was put into skeletal traction for six weeks after successful closed reduction to restrict hip movement. Radiographs were taken immediately after successful closed reduction and again at the 12th week, then once every six months. When the radiographs at the 12th week showed fracture healing, progressive weight-bearing and active exercises were started. In the surgical group, management of closed reduction was the same as in the conservatively treated group. Three to five days after injury, operation was performed via a Smith-Petersen approach to excise fragments. Postoperative management was the same as for the conservative group.
All patients were followed up at the study centre for at least two years, Functional outcome was determined using the Thompson and Epstein [18] score and the Merle d’Aubigne and Postel [3] score. Heterotopic ossification was assessed using the Brooker classification [1]. Descriptive statistics were calculated for all continuous and categorical variables. Post hoc analysis included Student’s t tests and Wilcoxon rank sum test. A p value ≤0.05 was considered statistically significant.
Results
From January 2002 to January 2008, eight patients with Pipkin type 1 fractures were treated conservatively with closed reduction and eight were treated operatively by surgical fragment excision within three to five days after closed reduction (Figs. 1, 2, 3, 4). In the conservative group, there were six male and two female patients, and the average age at the time of the accident was 37.6 ± 10.90 (range 19–56) years. Six patients sustained their injuries in a traffic accident, and two patients fell from a height. The interval between injury and successful closed reduction was 4.0 ± 2.14 hours (range 1.5–8.0 h). In the surgical group, the average age of seven male and one female patient was 37.3 ± 12.54 (range 21–59) years. Five patients sustained their injuries during a traffic accident, two from a fall from a height and one was hit by a falling wall. The interval between injury and successful closed reduction was 3.9 ± 1.47 hours (range 1.5–6.0 h). Student’s t tests failed to reach statistical significance for age (p = 0.967) and the average interval between injury and successful closed reduction (p = 0.894) between groups.
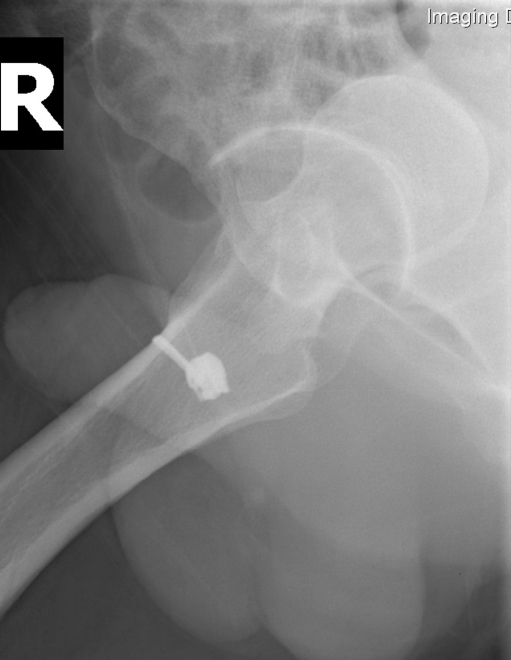
Fig. 1.
X-ray showing Pipkin type 1 fracture associated with posterior dislocation of the hip
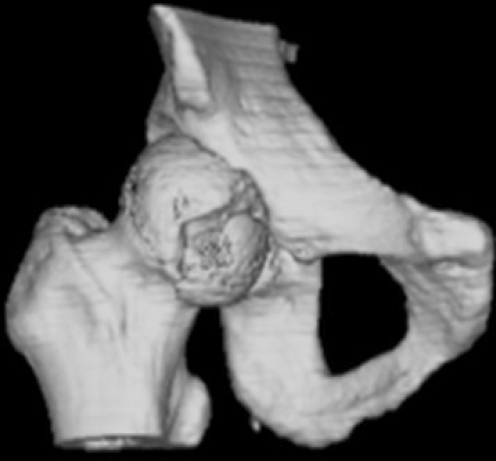
Fig. 2.
Computed tomography scan showing Pipkin type 1 fracture associated with posterior dislocation of the hip
Fig. 3.

X-ray showing Pipkin type 1 fracture after closed reduction
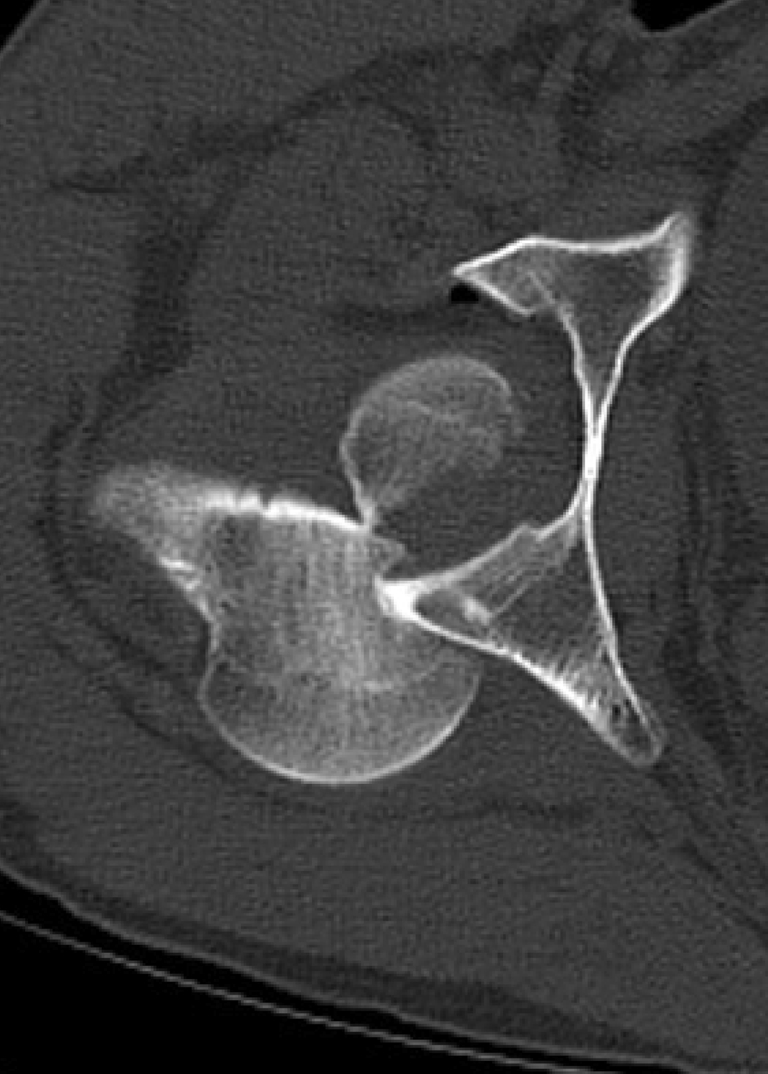
Fig. 4.
Computed tomography showing Pipkin type 1 fracture after closed reduction
All patients were followed up from 25 to 52 months, with an average of 39.3 ± 8.91 months in the conservative group ;and from 28 to 60 months, with an average of 39.5 ± 12.82 months in the surgical group (p = 0.982). Outcome by the Thompson and Epstein score and the Merle d’Aubigne and Postel score was classified equally. Treatment results were divided into four grades. In the conservative group, one was excellent, three were good, two were fair and two were poor. In the surgical group, five were excellent, two were good, one was fair and none were graded as poor. A Wilcoxon rank sum test analysis of these data reached statistical significance (p = 0.032). Heterotopic ossification was found in five cases: one in the conservative group and four in the surgical group. Avascular necrosis of the femoral head was found in two cases in the conservative group. Patient demographics and results are summarised in Tables 1, 2, 3.
Table 1.
Patient demographics and results of conservative group
| Case | Age | Sex | Time–C (hours) | Follow-up (months) | Complications | Heterotopic ossification (Brooker) | Outcome (Thompson and Epstein) | Outcome (Merle d’ Aubigne and Postel) |
|---|---|---|---|---|---|---|---|---|
| 1 | 31 | M | 3.5 | 52 | — | 0 | Fair | Fair |
| 2 | 38 | M | 8.0 | 32 | HO, AVN | I | Poor | Poor |
| 3 | 43 | W | 5.5 | 39 | — | 0 | Good | Good |
| 4 | 35 | M | 3.0 | 48 | — | 0 | Fair | Fair |
| 5 | 56 | M | 2.0 | 46 | — | 0 | Good | Good |
| 6 | 34 | M | 3.5 | 36 | — | 0 | Good | Good |
| 7 | 19 | M | 1.5 | 37 | — | 0 | Excellent | Excellent |
| 8 | 45 | W | 5.5 | 25 | AVN | 0 | Poor | Poor |
Time–C interval between injury and successful closed reduction in conservative group, HO heterotopic ossification, AVN avascular necrosis of the femoral head
Table 2.
Patient demographics and results of the surgical group
| Case | Age | Sex | Time–S (hours) | Follow-up (months) | Complications | Heterotopic ossification (Brooker) | Outcome (Thompson and Epstein) | Outcome (Merle d’ Aubigne and Postel) |
|---|---|---|---|---|---|---|---|---|
| 1 | 32 | M | 4.0 | 54 | HO | III | Fair | Fair |
| 2 | 26 | M | 6.0 | 60 | HO | II | Good | Good |
| 3 | 31 | M | 1.5 | 35 | — | 0 | Excellent | Excellent |
| 4 | 49 | M | 3.5 | 49 | HO | I | Excellent | Excellent |
| 5 | 21 | M | 4.0 | 28 | — | 0 | Excellent | Excellent |
| 6 | 43 | W | 2.5 | 32 | — | 0 | Excellent | Excellent |
| 7 | 59 | M | 5.5 | 28 | HO | II | Good | Good |
| 8 | 38 | M | 4.5 | 30 | — | 0 | Excellent | Excellent |
Time–S interval between injury and successful closed reduction in surgical group, HO heterotopic ossification
Table 3.
Patient demographics and results of conservative and surgical groups
| Group | Age | Time–C/S (h) | Follow-up (months) | Complications | Outcome | ||||
|---|---|---|---|---|---|---|---|---|---|
| HO | AVN | Excellent | Good | Fair | Poor | ||||
| C group | 37.6 ± 10.90 | 4.0 ± 2.14 | 39.3 ± 8.91 | 1 | 2 | 1 | 3 | 2 | 2 |
| S group | 37.3 ± 12.54 | 3.9 ± 1.47 | 39.5 ± 12.82 | 4 | 0 | 5 | 2 | 1 | 0 |
C group conservative group, S group surgical group, Time–C/S interval between injury and successful closed reduction, HO heterotopic ossification, AVN avascular necrosis of the femoral head
Discussion
Recommended treatment methods have varied between closed reduction or fragment excision after closed reduction for Pipkin type 1 fractures. Chakraborti S et al. [2] suggested that conservative methods should be considered initially, although treatment of this injury is difficult. However, Epstein et al. [5] suggest that all traumatic dislocations of the hip must be treated as surgical emergencies, that multiple attempts at closed reduction are contraindicated and that the good results after primary open reduction were better than those of closed or closed followed by open reduction. Anatomical reduction of hip dislocation and femoral-head fracture is difficult by closed reduction. Henle et al. [9] showed that only one in 12 patients showed an anatomically correct fracture position after closed reduction. Intra-articular soft tissue, small intra-articular bone fragments and malunion can lead to osteoarthritis and avascular necrosis of the femoral head. Biomechanical cadaveric studies [10] indicate that excision of a small part (<1/3) of the non-weight-bearing surface of the femoral head (as for Pipkin 1) does not lead to adverse long-term clinical implications. Our study shows that surgical fragment excision after closed reduction for Pipkin type 1 fractures has better outcome than closed reduction (p = 0.032). Therefore, we recommend surgical fragment excision when dealing with Pipkin type 1 fractures.
One study [5] indicated that reduction within 24 hours gives better results than late reduction. However, another [12] showed that the joint should be relocated within six hours, and failure to do so increases the risk of avascular necrosis of the femoral head with resultant early degenerative joint disease, often in an otherwise fit young patient. It was difficult to ensure the safe interval time elapsing between injury and reduction of traumatic dislocation of the hip joint. Our study shows that successful closed reduction within six hours followed by surgical fragment excision is safe for Pipkin type 1 fractures associated with posterior dislocation of the hip.
There have been differences of opinion about the operative approach for Pipkin type 1 fractures. Some studies [4, 5] advocate the Kocher–Langenbeck approach and strongly advise against the Smith–Petersen approach, indicating that the latter would damage any residual blood supply to the femoral head. Nevertheless, one study [16] showed that when evaluated with an odds ratio analysis, the Kocher–Langenbeck posterior approach was associated with a 3.2 times higher incidence of avascular necrosis compared with the Smith–Petersen approach. Anatomical study [7] showed that the main source of femoral-head vascular supply is the medial femoral circumflex artery, particularly its deep branch. Studies [11, 16, 17] showed that there is a significant decrease in operative time, estimated blood loss and improved visualisation with the anterior approach. The drawback in patients treated with an anterior approach was the development of more functionally significant heterotopic ossification, and prophylaxis with indomethacin or low-dose radiation should be considered to minimise heterotopic ossification. Recently, an trochanteric flip osteotomy approach was recommended for femoral-head fracture [6, 9, 15]. However, this approach increases the risk of nonunion of the greater trochanter. Due to these findings, we recommend treatment of Pipkin type 1 fractures by the Smith–Petersen approach.
Summary
This study showed the outcome of closed reduction followed by surgical fragment excision for Pipkin type 1 fractures is better than closed reduction alone. The incidence of heterotopic ossification was high; treatment such as indomethacin or low-dose radiation could be used to minimise heterotopic ossification. Successful closed reduction within six hours of trauma, followed by surgical fragment excision, is a safe and effective for treating Pipkin type 1 fractures associated with posterior dislocation of the hip.
References
- 1.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg AM. 1973;55:1629–1632. [PubMed] [Google Scholar]
- 2.Chakraborti S, Miller IM. Dislocation of the hip associated with fracture of the femoral head. Injury. 1975;7:134–142. doi: 10.1016/0020-1383(75)90011-X. [DOI] [PubMed] [Google Scholar]
- 3.D’aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg AM. 1954;36A:451–475. [PubMed] [Google Scholar]
- 4.Epstein HC. Traumatic dislocations of the hip. Clin Orthop Relat Res. 1973;92:116–142. doi: 10.1097/00003086-197305000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Epstein HC, Wiss DA, Cozen L. Posterior fracture dislocation of the hip with fractures of the femoral head. Clin Orthop Relat Res. 1985;201:9–17. [PubMed] [Google Scholar]
- 6.Gardner MJ, Suk M, Pearle A, Buly RL, Helfet DL, Lorich DG. Surgical dislocation of the hip for fractures of the femoral head. J Orthop Trauma. 2005;19:334–342. [PubMed] [Google Scholar]
- 7.Gautier E, Ganz K, Krügel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82:679–683. doi: 10.1302/0301-620X.82B5.10426. [DOI] [PubMed] [Google Scholar]
- 8.Giannoudis PV, Kontakis G, Christoforakis Z, Akula M, Tosounidis T, Koutras C. Management, complications and clinical results of femoral head fractures. Injury. 2009;40:1245–1251. doi: 10.1016/j.injury.2009.10.024. [DOI] [PubMed] [Google Scholar]
- 9.Henle P, Kloen P, Siebenrock KA. Femoral head injuries: Which treatment strategy can be recommended? Injury. 2007;38:478–488. doi: 10.1016/j.injury.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 10.Holmes WJ, Solberg B, Bay BK, Laubach JE, Olson SA. Biomechanical consequences of excision of displaced Pipkin femoral head fractures. J Orthop Trauma. 2000;14:149–150. doi: 10.1097/00005131-200002000-00071. [DOI] [Google Scholar]
- 11.Marchetti ME, Steinberg GG, Coumas JM. Intermediate- term experience of Pipkin fracture-dislocations of the hip. J Orthop Trauma. 1996;10:455–461. doi: 10.1097/00005131-199610000-00002. [DOI] [PubMed] [Google Scholar]
- 12.McMurtry IA, Quaile A. Closed reduction of the traumatically dislocated hip: a new technique. Injury. 2001;32:162–164. doi: 10.1016/S0020-1383(00)00152-2. [DOI] [PubMed] [Google Scholar]
- 13.Pipkin G. Treatment of grade IV fracture-dislocation of the hip. J Bone Joint Surg AM. 1957;39-A:1027–1042. [PubMed] [Google Scholar]
- 14.Roeder LF, Jr, DeLee JC. Femoral head fractures associated with posterior hip dislocation. Clin Orthop Relat Res. 1980;147:121–130. [PubMed] [Google Scholar]
- 15.Solberg BD, Moon CN, Franco DP. Use of a trochanteric flip osteotomy improves outcomes in Pipkin IV fractures. Clin Orthop Relat Res. 2009;467:929–933. doi: 10.1007/s11999-008-0505-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stannard JP, Harris HW, Volgas DA, Alonso JE. Functional outcome of patients with femoral head fractures associated with hip dislocations. Clin Orthop Relat Res. 2000;377:44–56. doi: 10.1097/00003086-200008000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Swiontkowski MF, Thorpe M, Seiler JG, Hansen ST. Operative management of displaced femoral head fractures: case-matched comparison of anterior versus posterior approaches for Pipkin I and Pipkin II fractures. J Orthop Trauma. 1992;6:437–442. doi: 10.1097/00005131-199212000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Thompson VP, Epstein HC. Traumatic dislocation of the hip; a survey of two hundred and four cases covering a period of twenty-one years. J Bone Joint Surg AM. 1951;33A:746–778. [PubMed] [Google Scholar]